Summary:
Knee arthroplasty, both total knee and unicompartmental, has had a significant impact on millions of patients globally. Although satisfaction is usually high, complications such as periprosthetic fracture are increasingly common. Distal femur periprosthetic fractures are relatively well researched and understood in comparison with periprosthetic proximal tibia fractures (PTFs). The management of PTFs is essentially an evidence-free area. This review explores the literature (or lack thereof) and integrates cases from Australia and Japan. As it stands, there is scant literature relating to all facets of PTFs, including, most concerningly, the management of them. Larger studies are required to help further investigate this important interface between arthroplasty and orthopaedic trauma. As a guide, those with loose prostheses will likely benefit most from revision total knee arthroplasty, while those with well-fixed prostheses can be managad according to the fracture with homage paid to the presence of the prosthesis. The use of periarticular locked plates is likely a better option over conventional large or small fragment plates. Nonoperative management is a viable option for selected individuals and can be associated with favorable outcomes.
Keywords: periprosthetic tibia fracture, periprosthtiec knee fracture, open reduction and internal fixation, revision arthroplasty
1. Introduction
Total knee arthroplasty (TKA) and unicompartmental knee arthroplasty (UKA) have had a significant impact on millions of patients globally. Generally, satisfaction rates are high after TKA, with patients noting an improved quality of life and improved functional outcomes.1 The number of TKA's being performed each year in many countries around the globe has increased since their inception at the end of the 1960s, and more recently, the number of UKAs has been rising.2,3 However, because the global population continues to age and become increasingly comorbid, managing the increasing number of complications is becoming more challenging.4 One such complication is periprosthetic fractures, which are increasingly common and technically challenging to manage, especially in the context of revision TKA (rTKA).5 Although there is a well-established literature pool that guides the management for periprosthetic femur fractures, periprosthetic tibia fractures (PTFs) are less common and poorly researched. As a result, there is not a well-developed approach to the management of PTFs.
2. Epidemiology
The overall incidence of periprosthetic fracture after primary TKA has been reported to be between 0.3% and 5.5% and as high was 38% after rTKA in 1 case series.6–8 Periprosthetic fractures around a TKA are commonly believed to be more frequently encountered on the femoral side as opposed to the tibial side; however, the rates seem to be relatively similar in the literature, 0.3%–2.5% versus 0.4%–1.7%, respectively.9 In addition, PTFs can also occur after primary UKA, a recent meta-analysis showed an incidence of between 1.2% and 1.6%.10 The mechanism of injury specific to PTFs is poorly described in the literature; however, low energy trauma is commonly cited and fractures sustained intraoperatively.11 While malalignment of the tibial component is frequently believed to increase the risk of PTF, there is little evidence to support this claim with modern prostheses nor the variations in practice such as improved cementing techniques and prosthesis alignment.7,12 Prosthesis design likely plays a key role in the risk of PTFs, including the use of tibial stems and cones/sleeves; however, there are limited data on the topic, and the selection bias in these patients may explain the anecdotal increased risk noted by many surgeons. Risk factors for periprosthetic fractures around a TKA include the presence of osteoporosis, increasing age, revision surgery, osteolysis, and being from the female sex; however, these are not specific to PTFs.13
3. Fracture patterns
The most commonly used classification system in the literature was developed by Felix et al in 1997.14 In this system, the location of the fracture is separated into (1) those that extend partially across the plateau, (2) those that extend across the entire plateau, (3) those that are distal to the prosthesis (including any stems), and (4) fractures of the tibial tuberosity. The stability is then assessed into (1) stable, (2) unstable, and (3) fractures which occur intraoperatively. A systematic review on PTFs in 2015 showed that based on a cohort of 144 fractures, 19% are type A, 44% are type B, and 37% are Type C.11 Based on fracture location, 55% were type I, 21% were type II, 21% were type III, and 2% were type IV.11 More recently, the OTA/AO universal classification system for periprosthetic fractures was published, although it has not yet been widely adopted within the literature.15 This classifies nondisplaced avulsion type tibial plateau/tubercle fractures as V.4-A (which includes selected Felix IA/IVA), a fracture around a stable tibial component with good bone stock as a V.4-B1 (which includes selected Felix IA/IIA), a fracture around a loose tibial component with good bone stock V.4-B2 (selected Felix IB/IIB), and those with a loose tibial component with poor bone stock V.4-B3. Fractures distal to the tibial component/stem are classified as a V.4-C.15
4. Treatment options
4.1. General principles
The Felix system is commonly used to guide treatment, albeit rather dogmatically because of poor evidence on the treatment of PTFs.14 It is important to note that the cohort of PTFs is a diverse group from younger, healthier patients with higher energy mechanisms all the way to older patients with fragility, pathological, or insufficiency fractures. There are no data on the age distribution of patients with PTF. Treatment should be tailored to the specific needs of the patient with consideration taken to allow for an early functional recovery and minimizing the risk of complications. Treatment success is generally regarded as patients returning to their preinjury ambulatory status without pain with radiographic features of union.11,16
Arguably, the stability of the implant plays the greatest role in deciding what treatment pathway is taken and then a consideration for the location of the fracture. Type A fractures can generally be treated in a fashion that is consistent with the location and nature of the fracture, without any significant consideration for the tibial component other than registering its existence. It is worth noting that the stability of an implant can be difficult to discern clinically or radiographically. Type B fractures generally require revision of the tibial component in addition to the treatment required for the fracture. Type C fractures can generally be both diagnosed and addressed intraoperatively. Of some 54 cases of Type C fractures published in the literature, 22% required internal fixation or bone grafting, while most were managed with weight-bearing restrictions or with supplemental casting or bracing. Regarding the location of the fracture, those which involve the plateau (types I + II) with stable prosthesis can be managed according to their fracture morphology and patient factors.
4.2. Operative treatment
Ideally, a patient would be able to range their knee immediately postoperatively and begin weight bearing as soon as possible; however, restricted weight bearing may be required in situations where the construct is believed to not be able to withstand the forces of mobilization. Surgeons should consider that if a fracture and the prosthesis appear stable and they do not feel that the patient will be able to range nor bear weight postoperatively, a nonoperative treatment pathway may reduce their risk of complications and follow a “first-do-no-harm” mantra.
Plate constructs likely offer the best option for IA and IIA PTFs; however, the plate should be selected to optimize the number of screws/cortices in the proximal fragment. Locking constructs, especially the use of locking screws in the proximal fragment, are generally advisable. Furthermore, consideration must be given to the skin bridges and soft tissues when planning approaches, and surgeons should be cognizant of minimally invasive techniques to reduce soft tissue compromise. The following cases were provided with written informed consent from the patient and local ethics committee approval (National Hospital Organization Okayama 2022-027/028/029 and AU20222007-03).
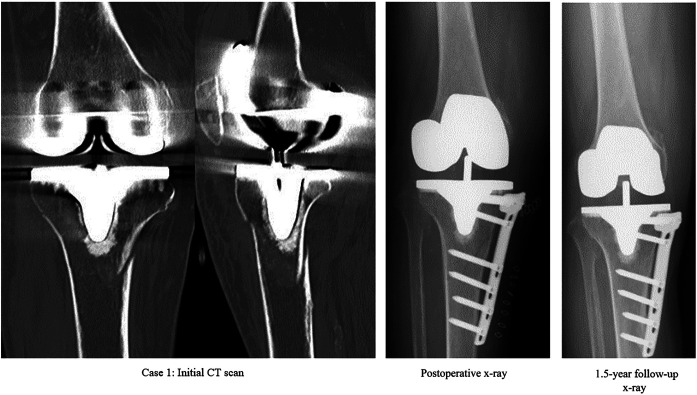
Case 1: a 79-year-old woman who sustained a Right Felix IIA fracture. Owing to concerns for her soft tissues, it was decided to proceed with a medial minimally invasive locking plate construct (TomoFix, DePuy Synthes, West Chester, PA). Care was taken when placing the locking screws around the tibial component and stem (see Fig. 1).
FIGURE 1.
Case 1.
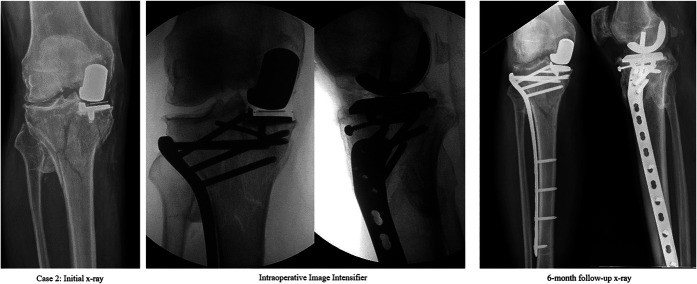
Case 2: a 75-year-old man who sustained a compound Right Felix IIA fracture around a medial UKA from a bulldozer accident. His knee, prosthesis, and fracture were grossly contaminated with stagnant water from a fresh water creek. He underwent a debridement of his open fracture and knee as well as ORIF with the lateral Less Invasive Stabilisation System (DePuy Synthes, West Chester PA, Synthes). A rafting screw was also placed under the tibial component. He was allowed to partial weight bear postoperatively and was managed in a manner similar to a prosthetic joint infection postoperatively with a prolonged course of antibiotics with input from infectious diseases. At 12 weeks, he was weight bearing fully, with preinjury range of motion. At 6 months postoperatively, he was walking unaided 1–2 kilometers per day with no evidence of infection (see Fig. 2).
FIGURE 2.
Case 2.
For IB and IIB PTFs, these are typically believed to benefit from revision arthroplasty, with consideration made during the rTKA about fracture fixation, typically with long tibial stems and supplemented with plate constructs. While revision arthroplasty is associated with higher rates of complications when compared with primary TKA, it is more likely to allow for immediate mobilization in this patient group than a IB/IIB managed in any other way.17 Regarding type IIIA fractures, fracture morphology and surgeon experience play a role in deciding between nonoperative, intramedullary fixation, plate constructs, or combined intramedullary nail and plate constructs. The presence of the tibial component can hinder the passage of intramedullary nails, although it is possible.18 If electing for plate constructs for IIIA fractures, Kim et al19 reported on 10 type IIIa PFTs managed with locked plate constructs, 2 of these patients who both underwent single plate fixation experienced hardware failure, one required a revision to dual plate construct and the other developed a varus malunion. The following cases were provided with written informed consent from the patient and local ethics committee approval (National Hospital Organization Okayama 2022-027/028/029 and AU20222007-03).
Case 3: an 85-year-old woman who sustained a Left Felix IIIA. She underwent an ORIF with a large fragment Locking Compression Plate with a combination of locking and cortical screws. Owing to the fracture pattern, 2 cortical screws and 1 locking screw were placed into the proximal fragment. At 5 months, the patient was ambulating well, with a visible fracture line still on x-ray. At 9 months postoperatively, she had significant callus and was clinically doing well (see Fig. 3).
FIGURE 3.
Case 3.
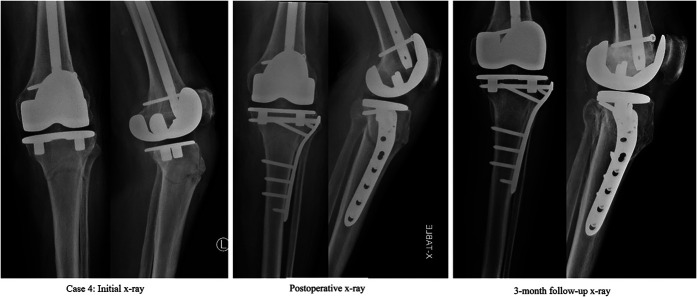
Case 4: an 89-year-old man who fell from standing height and sustained a Felix IIIA. He had a large proximal medial leg skin tear with surrounding threatened skin. He had a history of an ipsilateral mid shaft femur fracture, heart failure, and hypertension, and he was independent of his activities of daily living. He underwent a closed reduction and internal fixation with the lateral Less Invasive Stabilisation System (DePuy Synthes, West Chester PA Synthes). Additional medial fixation was not possible due to soft tissue concerns. He was allowed unrestricted knee range of motion and to weight bear as tolerated immediately. By his 3-month follow-up, he was back to his baseline mobility with a range of motion from 5 to 110 degrees (see Fig. 4).
FIGURE 4.
Case 4.
Type IIIB almost always require rTKA with a long-stemmed tibial component and supplemental internal fixation with plate constructs or consideration for a mega-prosthesis. While both options are not without risk, a proximal tibia replacement does not rely on union for its stability and is a valid option, especially in complex, comminuted fractures. The following case was provided with written informed consent from the patient and local ethics committee approval (AU20222007-03).
Case 5: a 71-year-old woman who fell from standing height with concomitant respiratory sepsis and contralateral ankle fracture dislocation. She sustained a comminuted Felix IIB + IIIB + IV fracture. She had psoriatic arthritis and fibromyalgia, was a nonsmoker and lived independently. Owing to significant comminution in the proximal fragment, the surgeon was unable to reconstruct the proximal metaphyseal tibia with osteosynthesis and proceeded with a proximal tibia replacement and the extensor mechanism reconstruction. The patient was placed in an extension knee splint but allowed to weight bear as tolerated from day 1 postoperatively. At the 2-week mark, the patient was changed into a range of motion brace from 0 to 60 degrees until 6 weeks postoperatively when it was unlocked before being removed at the 10-week mark. Her rehabilitation was significantly delayed by the contralateral ankle; however, at 14 weeks postoperatively, she was living at home again (see Fig. 5).
FIGURE 5.
Case 5.
The literature pool for Type IV fractures is poor; however, an intact extensor mechanism is essential for a good functional outcome, especially in patients with knee arthroplasty. Care should be taken during any operation to fix these or reconstruct the extensor mechanism to not disrupt the tibial component or the cement mantle (if present).
4.3. Nonoperative treatment
Nonoperative treatment can yield excellent results in selected patients with PTFs. While there are patients who are unable to undergo a procedure for personal or medical reasons, in selected patients with IA/IIA fracture patterns in particular, nonoperative management can safely and efficiently manage their fracture. There is no evidence on the optimal casting time or period of non–weight-bearing, and this is likely best guided by serial clinical examinations and imaging. The following case was provided with written informed consent from the patient and local ethics committee approval (AU20222007-03).
Case 6: a 79-year-old woman fell from standing height and sustained a Felix IIA + IV fracture. Her TKA was at 8 years with a range of motion from 0 to 90 degrees. She had type 2 diabetes, osteoporosis, and hypertension, and she was a nonsmoker and lived independently. After x-ray and CT evaluation, she proceeded to OT for an examination under anaesthesia. Under image intensifier, the fracture was stable in varus and valgus as well as in full extension, a full leg cast was applied, and she was non–weight-bearing for 6 weeks after which time she transitioned into a range of motion brace locked at 0–20 degrees weight bearing as tolerated before the brace was unlocked from the 10-week mark. She reached full weight bearing 3 months postfracture and was back to her usual level of function and range of motion by 5 months (see Fig. 6).
FIGURE 6.
Case 6.
5. Discussion
The outcome of PTFs varies widely as it reflects a heterogenous group of varying ages, mechanisms, and patterns. The literature suggests that Felix A fractures heal similarly to those without a TKA.11 Managing PTFs may be more challenging by virtue of the presence of the tibial prosthesis which may increase the risk of adverse outcomes when compared with nonperiprosthetic fractures. For instance, the entry point for a tibial intramedullary nail or screw positioning around tibial stems or cement mantles add complexity to the situation. Care should be taken when selecting implants; while all tibial fractures are at risk of nonunion, the limited published cases on this topic suggest that single plate constructs may not provide the fracture with the stability needed for union, a sentiment echoed in case 3 where a conventional locking compression plate was selected and the patient had a delay to union.19 However, cases 1 and 2 contradict this notion slightly; this may be anecdotal or due to the use of locked plate constructs in each case, which help to more rigidly fix the fracture, while affording surgeons more proximal screw holes to capture the proximal fragment. Intramedullary nailing is reasonable for fractures distal enough to the stem to allow for a more distal entry point and proximal screw placement. It is important to also remember that nonoperative management is an option for some fractures, and surgeons may want to consider an examination under anesthesia to determine whether a nonoperative treatment course is wise. While cast immobilization generally means prolonged non–weight-bearing, the first do-no-harm principle applies. Case 6 echoes this sentiment nicely.
Some evidence suggests that for Type B fractures, those treated with rTKA fare much better than those who do not.7,11 While the literature pool is limited, those treated without rTKA initially had a complication rate (including instability, malunion, nonunion, and need for revision surgery) of greater than 80%.11 While the conventional teaching is a long tibial stem that bridges the fracture, with augmented internal fixation if needed to create a stable proximal metaphysis, in patients with poor bone quality or with significant comminution, a proximal tibia replacement could be an option as was chosen in case 5.
For Type C fractures, patients seem to do quite well, granted less well than those who do not sustain a periprosthetic fracture intraoperatively.11 Care should be taken during primary and rTKAs to minimize the risk of PTF. However, if it is identified and addressed during the same operation, patients seem to recover well.11 The specific treatment for the fracture follows the same philosophy as with Types A and B fractures.
6. Future directions
As TKAs and UKAs become an increasing prevalent operation, so too will the rate of PTFs. As it stands, there is very scant evidence relating to all facets of PTFs, including, most concerningly, the management of them. Although a handful of authors have published small case series and cohorts of PTFs, larger studies are needed in this area to better guide our understanding and treatment. In the interim, care should be taken at all stages of arthroplasty to prevent a PTF. As a guide, those with loose prostheses will benefit most from rTKA, while those with well-fixed prostheses can be managed according to the fracture with homage paid to the presence of the prosthesis. Nonoperative management is a viable option for selected individuals with favorable outcomes.
Footnotes
There is no relevant conflict of interest for all authors, nor was any funding received for this project
Contributor Information
Daniel P. Lewis, Email: daniel.lewis@health.nsw.gov.au.
Seth M. Tarrant, Email: sethtarrant@gmail.com.
Stuart MacKenzie, Email: stuart@hunterboneandjoint.com.au.
Lachlan Cornford, Email: lachlancornford@gmail.com.
Toru Sato, Email: tsato6789@outlook.jp.
Naofumi Shiota, Email: naofumi@mx1.tiki.ne.jp.
References
- 1.Canovas F, Dagneaux L. Quality of life after total knee arthroplasty. Orthop Traumatol Surg Res. 2018;104:S41–S46. [DOI] [PubMed] [Google Scholar]
- 2.AOANJRR. Hip, Knee and Shoulder Arthroplasty: 2019 Annual Report. Adelaide, Australia: Australian Orthopaedic Association; 2019. [Google Scholar]
- 3.AOANJRR. Hip, Knee and Shoulder Arthroplasty: 2022 Annual Report. Adelaide, Australia: Australian Orthopaedic Association; 2022. [Google Scholar]
- 4.Losina E, Thornhill TS, Rome BN, et al. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012;94:201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benkovich V, Klassov Y, Mazilis B, et al. Periprosthetic fractures of the knee: a comprehensive review. Eur J Orthop Surg Traumatol. 2020;30:387–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Delanois RE, Mistry JB, Gwam CU, et al. Current epidemiology of revision total knee arthroplasty in the United States. J Arthroplasty. 2017;32:2663–2668. [DOI] [PubMed] [Google Scholar]
- 7.Parvizi J, Jain N, Schmidt AH. Periprosthetic knee fractures. J Orthop Trauma. 2008;22:663–671. [DOI] [PubMed] [Google Scholar]
- 8.Smolle MA, Hörlesberger N, Maurer-Ertl W, et al. Periprosthetic fractures of hip and knee–A morbidity and mortality analysis. Injury. 2021;52:3483–3488. [DOI] [PubMed] [Google Scholar]
- 9.Canton G, Ratti C, Fattori R, et al. Periprosthetic knee fractures. A review of epidemiology, risk factors, diagnosis, management and outcome. Acta Biomed. 2017;88:118–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burger JA, Jager T, Dooley MS, et al. Comparable incidence of periprosthetic tibial fractures in cementless and cemented unicompartmental knee arthroplasty: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2022;30:852–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ebraheim NA, Ray JR, Wandtke ME, et al. Systematic review of periprosthetic tibia fracture after total knee arthroplasties. World J Orthop. 2015;6:649–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rand JA, Coventry MB. Stress fractures after total knee arthroplasty. J Bone Joint Surg Am. 1980;62:226–233. [PubMed] [Google Scholar]
- 13.Schreiner AJ, Schmidutz F, Ateschrang A, et al. Periprosthetic tibial fractures in total knee arthroplasty - an outcome analysis of a challenging and underreported surgical issue. BMC Musculoskelet Disord. 2018;19:323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Felix NA, Stuart MJ, Hanssen AD. Periprosthetic fractures of the tibia associated with total knee arthroplasty. Clin Orthop Rel Res. 1997;345:113–124. [PubMed] [Google Scholar]
- 15.Unified Classification system for Periprosthetic Fractures (UCPF). J Orthop Trauma. 2018;32(suppl 1):S141–S144. [DOI] [PubMed] [Google Scholar]
- 16.Agarwal S, Sharma RK, Jain JK. Periprosthetic fractures after total knee arthroplasty. J Orthop Surg (Hong Kong). 2014;22:24–29. [DOI] [PubMed] [Google Scholar]
- 17.Hamilton DF, Howie CR, Burnett R, et al. Dealing with the predicted increase in demand for revision total knee arthroplasty. Bone Joint J. 2015;97-B:723–728. [DOI] [PubMed] [Google Scholar]
- 18.Haller JM, Kubiak EN, Spiguel A, et al. Intramedullary nailing of tibial shaft fractures distal to total knee arthroplasty. J Orthop Trauma. 2014;28:e296–e300. [DOI] [PubMed] [Google Scholar]
- 19.Kim HJ, Park KC, Kim JW, et al. Successful outcome with minimally invasive plate osteosynthesis for periprosthetic tibial fracture after total knee arthroplasty. Orthop Traumatol Surg Res. 2017;103:263–268. [DOI] [PubMed] [Google Scholar]