ABSTRACT
Background
Limited health literacy is associated with significant morbidity and mortality in the general population but the relation of health literacy with long-term clinical outcomes among adults with chronic kidney disease (CKD) is less clear.
Methods
Prospective data from the Chronic Renal Insufficiency Cohort (CRIC) Study (n = 3715) were used. Health literacy was assessed with the Short Test of Functional Health Literacy in Adults (dichotomized as limited/adequate). Cox proportional hazards models were used to separately examine the relations of health literacy with CKD progression, cardiovascular event (any of the following: myocardial infarction, congestive heart failure, stroke or peripheral artery disease), and all-cause, cardiovascular and non-cardiovascular mortality. Poisson regression was used to assess the health literacy–hospitalization association. Models were sequentially adjusted: Model 1 adjusted for potential confounders (sociodemographic factors), while Model 2 additionally adjusted for potential mediators (clinical and lifestyle factors) of the associations of interest.
Results
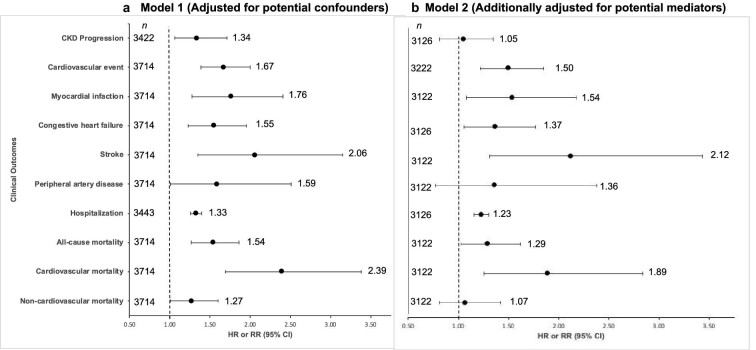
In confounder-adjusted models, participants with limited (vs adequate) health literacy [555 (15%)] had an increased risk of CKD progression [hazard ratio (HR) 1.34; 95% confidence interval (CI) 1.06–1.71], cardiovascular event (HR 1.67; 95% CI 1.39–2.00), hospitalization (rate ratio 1.33; 95% CI 1.26–1.40), and all-cause (HR 1.54; 95% CI 1.27–1.86), cardiovascular (HR 2.39; 95% CI 1.69–3.38) and non-cardiovascular (HR 1.27; 95% CI 1.01–1.60) mortality. Additional adjustments for potential mediators (Model 2) showed similar results except that the relations of health literacy with CKD progression and non-cardiovascular mortality were no longer statistically significant.
Conclusions
In the CRIC Study, adults with limited (vs adequate) health literacy had a higher risk for CKD progression, cardiovascular event, hospitalization and mortality—regardless of adjustment for potential confounders.
Keywords: chronic kidney disease, CVD, health literacy, hospitalization, mortality
KEY LEARNING POINTS.
What is already known about this subject?
The American Medical Association has previously defined health literacy as ‘the degree to which individuals have the capacity to obtain, process and understand basic health information needed to make appropriate health decisions.’
Limited health literacy is associated with lower use of disease prevention services, poorer chronic disease knowledge, worse medication adherence, and higher hospitalization and mortality rates in the general adult population.
Whether adults with chronic kidney disease (CKD) and limited health literacy are disproportionally burdened with a higher risk of adverse long-term outcomes than those with CKD and adequate health literacy is not clarified.
What this study adds?
Participants with limited health literacy showed a higher risk of CKD progression, any cardiovascular event, higher risk of hospitalization and a higher risk of mortality over approximately 4 years (as observed in confounder-adjusted models).
When examining each cardiovascular event component separately, we observed that limited health literacy was associated with a higher burden of congestive heart failure, stroke, myocardial infarction and peripheral artery disease.
What impact this may have on practice or policy?
Limited health literacy should be furthered considered as a potential risk factor for CKD progression, a cardiovascular event(s), mortality and hospitalization in adults with CKD.
There is a need for targeted efforts to address and promote health literacy among adults with CKD, including, for example, the use of language that facilitates effective communication between healthcare providers and patients.
INTRODUCTION
Health literacy, the `degree to which individuals have the capacity to obtain, process and understand basic health information needed to make appropriate health decisions' [1], has a pivotal role in the management of chronic kidney disease (CKD). It entails an individual's motivation to appraise and apply health-related information. Limited health literacy is highly prevalent in the USA, mainly among those with lower socioeconomic status and older age [1]. In the general population, limited health literacy has been associated with lower use of disease prevention services [2], poorer chronic disease knowledge [3], worse medication adherence [4], and higher hospitalization and mortality rates [5]. Limited health literacy may contribute to poor clinical outcomes through mechanisms that operate at both systematic and individual levels. For example, health literacy can influence one's capacity to obtain access to resources and navigate the healthcare system, as well as the efficacy and quality of communication between the healthcare provider and patient [6–8].
The significance of health literacy in populations living with CKD has been increasingly recognized, partly because health literacy is a potentially modifiable factor [5]. However, to date, health literacy remains largely understudied in the CKD population [9]. Research on the relationship of health literacy with clinical outcomes has primarily focused on the end-stage kidney disease (ESKD) population, with studies demonstrating that limited or low health literacy is associated with increased mortality [10], higher hospitalization rate [11] and missed dialysis treatments [11]. Moreover, among adults enrolled in the Chronic Renal Insufficiency Cohort (CRIC) Study, we previously demonstrated that limited health literacy is cross-sectionally associated with lower estimated glomerular filtration rate (eGFR), higher proteinuria, poorer blood pressure (BP) control and higher self-reported cardiovascular disease (CVD) [12].
To address critical gaps in the literature [5, 9], we analyzed data from the CRIC Study to evaluate the prospective relationships of health literacy with the long-term outcomes of CKD progression, cardiovascular events, hospitalization, and all-cause, cardiovascular and non-cardiovascular mortality. The growing burden of CKD represents a public health crisis, with about 15% of the US adult population affected by CKD [13]. Therefore, a better understanding of the role of potentially modifiable risk factors, such as health literacy, on adverse clinical outcomes is critical to inform clinical and public health strategies to improve CKD-related outcomes.
MATERIALS AND METHODS
Study population
The CRIC Study is an ongoing, prospective observational study designed to examine risk factors for the progression of CKD among racially diverse adults with CKD (as defined by an eGFR of 20–70 mL/min/1.73 m2). Participants are followed through annual in-person visits. Sampling design and methods have been previously described [14, 15]. The study protocol was approved by the Institutional Review Board at each participating site. All participants provided written informed consent. For the present analysis, we included non-Hispanic Whites and non-Hispanic Black CRIC participants who completed the health literacy questionnaire [Short Test of Functional Health Literacy in Adults (STOFHLA)]. Out of the 5499 CRIC Study participants, we excluded 801 participants who were of a race/ethnicity other than non-Hispanic White and non-Hispanic Black, and 983 participants who did not complete the STOFHLA. The final analytic sample of this study includes 3715 CRIC Study participants with self-reported race as non-Hispanic White or non-Hispanic Black and data on health literacy. Other racial/ethnic groups, particularly Hispanics, were not included in the current study due to the small sample size. Supplementary data, Table S1 depicts the baseline characteristics between participants included (n = 3715) and excluded (n = 983) from the study. In this study, the baseline visit was defined as year 5, i.e. the annual visit during which health literacy was assessed. Participants were followed up until the time of death, lost to follow-up due to withdrawal from the study or until the year 2018 when the data were locked for analyses.
Health literacy
To assess health literacy, we used the STOFHLA, a functional literacy assessment tool designed to measure an individual's ability to read and understand materials from healthcare settings [16]. The STOFHLA consists of two functional health reading comprehension passages with 36-items. Per the Cloze procedure, every fifth to seventh word was omitted in each passage. Interviewers asked participants to select the correct missing words. Participants had a maximum of 7 min for test completion. Total STOFHLA score (range: 0–36) is the number of correctly answered items. Based on previous studies [12, 16], participants who were not able to read were assigned a score of 0 and health literacy was categorized as limited (score = 0–22) or adequate (score ≥ 23). The STOFHLA has adequate reliability and validity to identify adults with limited health literacy regardless of race/ethnicity and age, with a previous study [16] reporting that Cronbach's alpha was 0.97 for the 36 items in the two prose passages.
Study outcomes
The primary outcomes of the present study were: (i) CKD progression, (ii) cardiovascular event, (iii) hospitalization, (iv) all-cause mortality, (v) cardiovascular mortality and (vi) non-cardiovascular mortality. CKD progression was defined as either a 50% decline from baseline eGFR or the development of ESKD. GFR was estimated annually using the CRIC estimating equation which uses serum creatinine and cystatin C levels, age, sex and race to predict measured GFR in the CRIC cohort [17]. Incident ESKD was defined as the initiation of chronic renal replacement therapy or kidney transplantation. To determine ESKD, CRIC Study personnel conducted semi-annual surveillance supplemented with the US Renal Data System. The cardiovascular event outcome was defined as the presence of myocardial infarction (MI), congestive heart failure (CHF), stroke or peripheral artery disease (PAD). Each component of the cardiovascular event outcome was examined separately as a secondary outcome. Study personnel queried participants every 6 months by telephone or in-person follow-up visits about hospitalizations, outpatient tests or interventions. Hospital billing codes were reviewed to identify any cardiovascular event. Two independent reviewers assessed hospital records to adjudicate events using standardized criteria [14]. Criteria for MI included a combination of chest pain, electrocardiography abnormalities and elevated cardiac biomarkers. As previously described [18], criteria for CHF events was adapted from the Framingham Heart Study [19] and included a combination of clinical symptoms, radiographic evidence of pulmonary congestion, physical examination of heart and lungs, and, when available, central venous hemodynamic monitoring data and echocardiographic imaging. Two neurologists adjudicated cerebrovascular accidents [14]. PAD procedures were ascertained based on the International Classification of Diseases, Ninth Revision, codes. Deaths were ascertained from reports by next of kin, death certificates, hospital records and linkage with the Social Security Death Master File. When a death event occurred during hospitalization and medical records were obtained, the death event was adjudicated by two physicians to determine whether it was related to a cardiovascular event (heart failure, MI, cerebrovascular, arrhythmia or other cardiovascular cause). Both all cause-mortality and non-cardiovascular mortality include unknown causes of death. For deaths that occurred out of the hospital, the CRIC Study built a machine learning algorithm using the National Death Index data to predict whether the death event was cardiovascular-related [20]. The SuperLearner algorithm utilizes the cross-validation approach twice, first when estimating the probability of cardiovascular mortality for individual models and second when combining multiple probabilities via ensemble. This algorithm avoids overfitting as much as possible. However, given that the number of participants in the training data was still relatively small, a certain degree of overfitting was unavoidable.
Statistical analysis
Descriptive statistics were computed for study covariates according to health literacy level. Chi-square tests and analysis of variance were used to detect statistically significant differences in categorical and continuous variables, respectively, across health literacy levels. Unadjusted event rates were calculated as the number of participants reaching the event divided by the total patient-year follow-up and were stratified by health literacy level. Complete case analysis was used. A series of Cox proportional hazard regression models were used to estimate hazard ratios (HR) and 95% confidence intervals (CIs) for the associations of health literacy with CKD progression, cardiovascular event(s) and mortality. Poisson regression was used to estimate rate ratios (RR) and 95% CIs for the association between health literacy and hospitalization rate. Adequate health literacy was defined as the reference group.
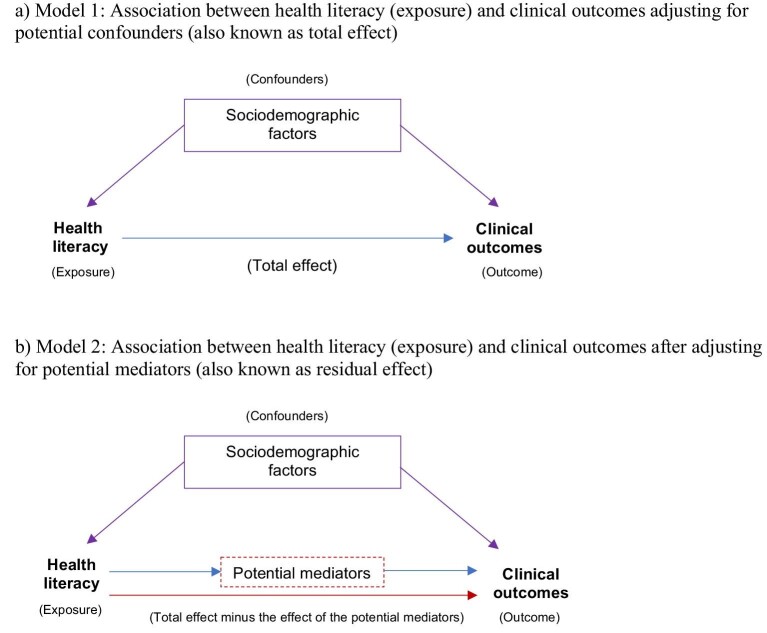
Models were sequentially adjusted for covariates measured at baseline. Covariates were chosen a priori for each outcome based on existing literature on the potential confounders and mediators of the associations of interest [10–12]. For all outcomes, Model 1 adjusted for sociodemographic factors (i.e. clinical center sex, race/ethnicity, education and annual household income), all of which are considered to be potential confounders of the association between health literacy and each clinical outcome (also known as total effect). Model 2 additionally adjusted for covariates that have been previously proposed to be potential mediators of the association between health literacy and each clinical outcome (also known as residual effect); these potential mediators were clinical factors/prior disease [i.e. systolic BP, diabetes, urine protein to creatinine ratio, and angiotensin-converting enzyme inhibitor (ACEi)/angiotensin II receptor blocker (ARB) medication use] and lifestyle factors [current smoking and body mass index (BMI)]. Model 2 of the CKD progression outcome was additionally adjusted for the following clinical covariates: prior contact with a nephrologist, baseline eGFR and hemoglobin A1C. Model 2 of both the cardiovascular event and mortality outcomes additionally adjusted for the following clinical covariates: baseline eGFR, hyperlipidemia, and aspirin and/or statin medication use. Model 2 of the hospitalization outcome additionally adjusted for the following clinical covariates: prior contact with a nephrologist, hemoglobin A1C, hyperlipidemia, and aspirin and/or statin medication use. Figure 1 depicts the assumed potential confounders and mediators of the association between health literacy and clinical outcomes in a simplified direct acyclic graph. In our secondary analysis, we evaluated the association between health literacy and each of the following cardiovascular events separately: MI, CHF, stroke and PAD. Finally, sensitivity analysis was conducted to examine the associations of health literacy with clinical outcomes without adjustment for education. For all analyses, SAS 9.4 (SAS Institute, Cary, NC, USA) was used and P < .05 was considered significant.
FIGURE 1:
Hypothesized association of health literacy with clinical outcomes, and potential confounders and mediators of this association (simplified direct acyclic graph). Model 1 was adjusted for potential confounders of the association between health literacy and clinical outcomes (also known as total effect). Model 2 additionally adjusted for potential mediators of the association between health literacy and clinical outcomes (also known as residual effect). The clinical outcomes examined in this study were CKD progression, cardiovascular event(s), hospitalizations and mortality. (a) The potential confounders of the association between health literacy and clinical outcomes include sociodemographic factors (i.e. clinical center, sex, race/ethnicity, education and annual household income). (b) The potential effect mediators of the association between health literacy and clinical outcomes include clinical factors/prior disease (i.e. systolic BP, diabetes, urine protein to creatinine ratio, ACEi/ARB medication use, prior contact with a nephrologist, baseline eGFR, hemoglobin A1C, as well as hyperlipidemia, and aspirin and/or statin medication use).
RESULTS
Baseline participant characteristics
Among the 3715 participants, 15% met our definition of limited health literacy (Table 1). Compared with adequate health literacy, participants with limited health literacy were more likely to be older, male and non-Hispanic Black, and had lower income and education. They were also more likely to have ever visited a nephrologist. Participants with limited health literacy (vs adequate) were significantly more likely to be current smokers and to have diabetes, CVD, MI, stroke, CHF and PAD, and higher systolic BP and hemoglobin A1C levels. Those with limited health literacy (vs adequate) had lower eGFR and higher urine protein to creatinine ratio.
Table 1.
Baseline characteristics of CRIC Study participants by health literacy level
| Health literacy | ||
|---|---|---|
| Characteristics | Adequate, n = 3160 (85.1%) | Limited, n = 555 (14.9%) |
| Demographic characteristics | ||
| Age, years | 62.4 ± 10.0 | 65.8 ± 8.3** |
| Male sex | 1721 (54.5%) | 352 (63.4%)** |
| Race | ||
| Non-Hispanic White | 1779 (56.3%) | 92 (16.6%)** |
| Non-Hispanic Black | 1381 (43.7%) | 463 (83.4%) |
| Annual household income ≤$20 000 | 627 (19.8%) | 268 (48.3%)** |
| Less than high school education | 236 (7.5%) | 232 (41.8%)** |
| Has health insurance | 3012 (96.9%) | 24 (96.0%) |
| Medical history | ||
| Ever visited a nephrologist (yes vs no) | 2325 (73.6%) | 446 (80.4%)** |
| Smoked >100 cigarettes | 1672 (52.9%) | 345 (62.2%)** |
| Diabetes | 1539 (48.7%) | 372 (67.0%)** |
| Cardiovascular disease | 1132 (35.8%) | 304 (54.8%)** |
| Myocardial infarction | 764 (24.2%) | 183 (33.0%)** |
| Stroke | 319 (10.1%) | 130 (23.4%)** |
| Congestive heart failure | 313 (9.9%) | 114 (20.5%)** |
| Peripheral artery disease | 218 (6.9%) | 67 (12.1%)** |
| Medication use | ||
| ACEi or ARB | 2097 (66.9%) | 360 (65.5%) |
| Statins | 1965 (62.7%) | 366 (66.5%) |
| Aspirin | 1574 (50.2%) | 309 (56.2%)* |
| Clinical characteristics | ||
| BMI, kg/m2 | 32.5 ± 7.8 | 32.3 ± 7.7 |
| Systolic BP, mmHg | 125.5 ± 19.4 | 129.5 ± 21.7** |
| Hemoglobin A1C % | 6.3 (1.4) | 6.7 (1.7)** |
| Calcium, mg/dL | 9.4 ± 0.5 | 9.4 ± 0.6 |
| Phosphate, mg/dL | 4.2 ± 1.2 | 4.5 ± 1.1 |
| Total parathyroid hormone, pg/mL | 90.1 ± 151.5 | 106.7 ± 95.2 |
| Kidney function measurements | ||
| eGFR (mL/min/1.73 m2) | 49.5 ± 15.6 | 46.0 ± 17.3** |
| Urine protein to creatinine ratio | 0.1 (0.1–0.5) | 0.3 (0.1–1.0)** |
Note: Values for categorical variables are given as count (percentage); values for continuous variables are given as mean ± standard deviation or median (IQR).
SD, standard deviation; ACEi, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blockers; BP, blood pressure; eGFR, estimated glomerular filtration rate.
P < .01, ** P < .001.
Event rates and associations of health literacy with clinical outcomes
CKD progression
During a median follow-up of 3.7 years [interquartile range (IQR) 2.5–8.3], there were 591 CKD progression events. The unadjusted CKD progression rate per 100 patient-years was significantly higher among participants with limited health literacy (6.7) versus adequate health literacy (3.6) (Supplementary data, Fig. S1). In Model 1 (i.e. confounder-adjusted model), adjusting for the sociodemographic factors, limited health literacy (vs adequate) was associated with an increased risk of CKD progression (HR 1.34; 95% CI 1.06–1.71). Upon additional adjustment for clinical factors (Model 2), the association between health literacy and CKD progression was no longer statistically significant (HR 1.05; 95% CI 0.81–1.35; Fig. 2).
FIGURE 2:
Associations of limited health literacy (vs adequate health literacy) with clinical outcomes: CKD progression, cardiovascular event, hospitalization and mortality, CRIC Study. (a) Model 1 (adjusted for potential confounders, also known as total effect): across all outcomes, Model 1 adjusted for the sociodemographic factors (i.e. clinical center, age, sex, race, education and annual household income). (b) Model 2 (adjusted for potential mediators, also known as residual effect): Model 2 of the CKD progression outcome additionally adjusted for clinical factors (i.e. systolic BP, diabetes, hemoglobin A1C, baseline eGFR, prior contact with a nephrologist, urine protein to creatinine ratio, and use of ACEi/ARB medication) and lifestyle factors (i.e. current smoking and BMI). Model 2 of the cardiovascular event and mortality outcomes additionally adjusted for systolic BP, diabetes, urine protein to creatinine ratio, baseline eGFR, hyperlipidemia, and use of ACEi/ARB, aspirin and/or statin medication. Model 2 of the hospitalization outcome additionally adjusted prior contact with a systolic BP, diabetes, urine protein to creatinine ratio, nephrologist, hemoglobin A1C, hyperlipidemia and use of ACEi/ARB, aspirin and/or statin medication. Cox proportional hazard regression models were used to estimate hazard ratios (HR) for the associations of healthy literacy with failure time outcomes (CKD progression, cardiovascular event and mortality). Poisson regression models were used to estimate rate ratios (RR) for the association between health literacy and hospitalization.
Cardiovascular event
Over a median follow-up of 4.1 years (IQR 2.7–8.1), a total of 831 participants experienced a cardiovascular event (i.e. MI, CHF, stroke or PAD). The unadjusted cardiovascular event rate per 100 patient-years was significantly higher among those with limited health literacy (10.7) versus adequate (3.8) (Supplementary data, Fig. S1). In Model 1, limited health literacy (vs adequate) was associated with an increased risk of a cardiovascular event (HR 1.67; 95% CI 1.39–2.00). This association of limited health literacy (vs adequate) with an increased risk of cardiovascular event persisted, albeit attenuated, in the adjusted Model 2 (HR 1.50; 95% CI 1.22–1.85). In secondary analyses of the individual components of the cardiovascular event outcome, we observed that limited health literacy was associated with a higher risk for MI (HR 1.54; 95% CI 1.08–2.18), CHF (HR 1.37; 95% CI 1.06–1.77) and stroke (HR 2.12; 95% CI 1.31–3.43); there was no association of health literacy with PAD (HR 1.36; 95% CI 0.77–2.38) in the fully adjusted Model 2; Fig. 2.
Hospitalization rate
Over a median follow-up of 4.2 years (IQR 3.1–8.2), there were 12 103 hospitalizations. The unadjusted hospitalization rate per 100 patient-years was about two times higher among individuals with limited health literacy (113.8) compared to adequate (60.1) (Supplementary data, Fig. S2). In Model 1, limited health literacy (vs adequate) was associated with a higher hospitalization rate (RR 1.33; 95% CI 1.26–1.40). Upon additional adjustment in Model 2, limited health literacy (vs adequate) remained significantly associated with a higher hospitalization rate (Model 2: RR 1.23; 95% CI 1.16–1.30; Fig. 2).
Mortality
During a median follow-up of 5.6 years (IQR 3.3–8.4), there were 776 deaths from all causes, including 221 deaths from cardiovascular-related causes and 286 from non-cardiovascular causes. Participants with limited health literacy (vs adequate) had significantly higher all-cause mortality rates (74.9 vs 30.5 per 1000 patient-years, P < .001). Similarly, participants with limited health literacy (vs adequate) had significantly higher cardiovascular-related mortality rates (2.8 vs 0.8 per 100 patient-years) and non-cardiovascular mortality (4.8 vs 2.3 per 100 patient-years) (Supplementary data, Fig. S1). The risk of all-cause mortality was higher among those with limited health literacy (vs adequate) in Model 1 (HR 1.54; 95% CI 1.27–1.86) and Model 2 (HR 1.29; 95% CI 1.03–1.62). Likewise, the risk of cardiovascular-related mortality was higher among those with limited health literacy in Model 1 (HR 2.39; 95% CI 1.69–3.38) and this association persisted after additional adjustments in Model 2 (HR 1.89; 95% CI 1.26–2.84). Finally, the risk of non-cardiovascular mortality was higher among those with limited health literacy (vs adequate) in Model 1 (HR 1.27; 95% CI 1.01–1.60) but the association was no longer significant when adjusting for potential mediators in the final model (Model 2; Fig. 2).
Sensitivity analysis
Finally, sensitivity analysis examining the association of limited health literacy with clinical outcomes without adjustment for education showed similar results to our main analysis (Supplementary data, Table S2). For instance, we observed that all the associations of health literacy with clinical outcomes were significant in Model 1 with and without adjustment for education. Further, the strength of the associations observed in the confounder-adjusted model without adjustment for education was similar to the strength of the association observed in the confounder-adjusted model with adjustment for education.
DISCUSSION
Among a large and diverse cohort of adults with CKD, we found that limited health literacy was prospectively associated with increased risk of CKD progression, a cardiovascular event, hospitalization and mortality (including all-cause, cardiovascular and non-cardiovascular) in confounder-adjusted models. The statistical significance and strength of these associations remained largely unchanged when additionally adjusting for potential mediators, with the exception of the relations of health literacy with CKD progression and non-cardiovascular mortality which were no longer statistically significant in the second model (a finding that is not surprising since the confounder-adjusted models were approaching non-statistical significance). Further, in secondary analyses, when examining each of the cardiovascular event components separately, we observed that limited health literacy was associated with a higher burden of MI, CHF, stroke and PAD in confounder-adjusted models (Model 1); the association between health literacy and PAD was not statistically significant when additionally adjusting for potential mediators (Model 2). Taken together, our findings extend previous evidence from the general population to suggest the role of limited health literacy as a potential risk factor for a cardiovascular event(s), mortality and hospitalization among adults with CKD.
To our knowledge, most of the evidence on the associations of health literacy with clinical outcomes in adults with CKD has been cross-sectional and largely focused on CVD risk factors. For example, in our cohort, we previously reported the cross-sectional association of limited health literacy with higher levels of systolic BP, low-density lipoprotein cholesterol, hemoglobin A1c and higher self-reported CVD prevalence [12]. Similarly, in a smaller sample of CKD dialysis patients, limited health literacy was cross-sectionally associated with both higher diastolic BP and mean arterial pressure [21]. Additionally, there is evidence in non-CKD populations demonstrating the associations of limited or low health literacy with a higher burden of CVD risk factors such as worse blood pressure control [22], poorer glycemic control [23], a greater buildup of plaques in carotid arteries [24] and higher CVD risk [24]. As such, our study extends previous evidence from both CKD and non-CKD populations to demonstrate that health literacy is prospectively related to a higher risk for a cardiovascular event in the CKD population (even after adjusting for a comprehensive array of sociodemographic, clinical, and lifestyle factors). Further, our findings contribute to addressing knowledge gaps identified by the American Heart Association [6] on whether health literacy is prospectively associated with the incidence of a cardiovascular event in populations living with chronic conditions.
Our findings on the relationship of health literacy with a higher risk for hospitalization and all-cause and cardiovascular mortality, regardless of adjustments, confirm previous studies showing that limited health literacy is associated with a higher hospitalization rate [6, 25–27], 30-day hospital readmission after MI [28], and all-cause mortality in hospital and community-based non-CKD cohorts [29]. Among the ESKD population, research has similarly shown that limited health literacy is associated with higher emergency department usage and ESKD hospitalization [11], missed dialysis treatments [11] and increased all-cause mortality [10]. Our finding on the higher hospitalization risk among adults with CKD and limited health literacy is of particular public health relevance given the well-established higher rates of hospitalization among adults with CKD [30, 31] and well-documented high economic costs of CKD-related hospitalizations [32, 33], compared with the general population.
In our study, there was no association between health literacy at baseline and CKD progression over time in the fully adjusted model (including sociodemographic, clinical and lifestyle factors). Such a null finding is consistent with a previous study [34] reporting that lower educational attainment, a variable that has been previously related to health literacy, is not associated with a higher risk of CKD progression (in fully adjusted models) among adults with moderate to severe CKD in the Study of Heart and Renal Protection (SHARP) [34]. While the potential reasons for our null finding are largely unknown, it is important to note that selection bias (e.g. our sample of participants with low educational attainment and high levels of risk factors) has been proposed as a potential explanation for the lack of association between health literacy and CKD progression. Other potential reasons for the lack of association between health literacy and CKD progression include that other types of health literacy (such as numeracy and nutrition) may have a more important role in CKD progression than functional health literacy (assessed in our study with the STOFHLA). Other potential explanations for the above null findings include that there was an overall high achievement of the CKD management guidelines in our cohort [35]—given that CRIC cohort participants were recruited from various well-recognized clinical centers. Finally, in the present study, there was no difference in health insurance coverage and ACEi or ARB medications across health literacy levels, and participants with limited health literacy were more likely to have visited a nephrologist than those with adequate health literacy.
Various mechanisms may help to explain the strong associations of health literacy with higher risk for a cardiovascular event, hospitalization and mortality in patients with CKD. For instance, patients with limited health literacy (vs adequate) may experience difficulty when trying to navigate the complex healthcare system, communicate with healthcare providers and maintain self-care regimens [7]—all of which can contribute to poor CKD management [36]. It has been previously shown that interventions to improve health literacy can promote increased access to health information, improve disease self-management skills, and enhance communication techniques between physicians and patients [37, 38]. Our study findings and evidence on health literacy interventions suggest that programs to address limited health literacy in CKD patients could be considered as strategies to improve clinical health outcomes in future studies.
This study has multiple strengths including that the study design was prospective and we had a relatively large sample of non-Hispanic White and Black participants. The CRIC Study has detailed characterizations of a wide range of carefully adjudicated and well-validated outcomes. Limitations of our study include that the STOFHLA only measured functional health literacy; thus, we did not examine other health literacy aspects such as conceptual knowledge on CKD and numeracy [39]. However, the reading comprehension portion of the STOFHLA that we used in our study has been previously demonstrated to have adequate reliability and validity and has been shown to be strongly correlated with other measures of overall health literacy such as the Rapid Estimate of Adult Literacy in Medicine (REALM) [16]. Additional study limitations are that medical history and medication use were self-reported and there may be residual confounding due to the observational nature of our study. Finally, we were not able to evaluate health literacy in all CRIC Study participants since the STOFHLA was included in the CRIC Study in year 5. As such, our findings may not be generalizable to all CRIC Study participants. Low health literacy is recognized as a distinct and stronger predictor of health outcomes than age, income, employment status, education level or race/ethnicity [40]. Moreover, it has been shown that higher educational attainment (i.e. years of education) does not necessarily equate to higher or adequate levels of health literacy [41], in part, because of the varying degree of quality of schooling and the health-related content of schooling across different educational settings. Therefore, in accordance with previous research [42], we conceptualized (a priori) education as a potential confounder of the association between health literacy and clinical health outcomes. Our post-hoc sensitivity analysis demonstrated that findings with and without adjustment for education were similar, which highlights the importance of not only examining years of education but also the quality of education within the context of health literacy. However, we recognize that education may also be conceptualized as an upstream factor that determines health literacy; thus, further research is needed to elucidate the causal pathways of the association amongst education, health literacy and health outcomes.
In summary, we found that patients with CKD and limited health literacy are disproportionally burdened by a higher risk for CKD progression, a cardiovascular event, hospitalization and mortality compared with patients with CKD and adequate health literacy—regardless of adjustment for potential confounders of these associations. Our findings underscore the need for targeted efforts to address limited health literacy among CKD patients. Future studies should consider whether interventions targeting the improvement of health literacy among patients with CKD are associated with improvement in clinical outcomes.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to express our special thanks to the CRIC participants for their commitment to this study.
APPENDIX
CRIC Study Investigators
Lawrence J. Appel, Harold I. Feldman, Alan S. Go, Jiang He, John W. Kusek, James P. Lash, Akinlolu Ojo,Mahboob Rahman and Raymond R. Townsend.
Contributor Information
Mayra L Estrella, Department of Epidemiology, Human Genetics and Environmental Sciences, The University of Texas Health Science Center at Houston (UTHealth) School of Public Health, Brownsville, TX, USA; Institute for Minority Health Research, University of Illinois at Chicago, Chicago, IL, USA.
Paula Allen-Meares, Institute for Minority Health Research, University of Illinois at Chicago, Chicago, IL, USA; Office of Health Literacy, University of Illinois at Chicago, Chicago, IL, USA.
Ana C Ricardo, Division of Nephrology, Department of Medicine, University of Illinois at Chicago, Chicago, IL, USA.
Michael J Fischer, Division of Nephrology, Department of Medicine, University of Illinois at Chicago, Chicago, IL, USA; Medicine/Nephrology, Jesse Brown VA Medical Center, Chicago, IL, USA; Center of Innovation for Complex Chronic Healthcare, Edward Hines Jr VA Hospital, Hines, IL, USA.
Elisa J Gordon, Division of Transplantation, Department of Surgery, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA.
Eunice Carmona-Powell, Division of Nephrology, Department of Medicine, University of Illinois at Chicago, Chicago, IL, USA.
James Sondheimer, Department of Medicine, Wayne State University, Detroit, MI, USA.
Jing Chen, Department of Medicine, Tulane University, New Orleans, LA, USA.
Edward Horwitz, Case Western Reserve University, School of Medicine, MetroHealth Medical Center, Cleveland, OH, USA.
Xue Wang, Department of Biostatistics, Epidemiology and Informatics, University of Pennsylvania Perelman School of Medicine, Philadelphia, PA, USA.
Jesse Y Hsu, Department of Biostatistics, Epidemiology and Informatics, University of Pennsylvania Perelman School of Medicine, Philadelphia, PA, USA.
James P Lash, Division of Nephrology, Department of Medicine, University of Illinois at Chicago, Chicago, IL, USA.
Claudia Lora, Department of Epidemiology, Human Genetics and Environmental Sciences, The University of Texas Health Science Center at Houston (UTHealth) School of Public Health, Brownsville, TX, USA.
the CRIC Study Investigators:
Lawrence J Appel, Jing Chen, Harold I Feldman, Alan S Go, Robert G Nelson, Mahboob Rahman, Panduranga S Rao, Vallabh O Shah, Raymond R Townsend, and Mark L Unruh
FUNDING
Funding for the CRIC Study was obtained under a cooperative agreement from National Institute of Diabetes and Digestive and Kidney Diseases (U01DK060990, U01DK060984, U01DK061022, U01DK061021, U01DK061028, U01DK060980, U01DK060963, U01DK060902 and U24DK060990). In addition, this work was supported in part by: the Perelman School of Medicine at the University of Pennsylvania Clinical and Translational Science Award NIH/NCATS UL1TR000003; Johns Hopkins University UL1 TR-000424, University of Maryland GCRC M01 RR-16500, Clinical and Translational Science Collaborative of Cleveland, UL1TR000439 from the National Center for Advancing Translational Sciences (NCATS) component of the National Institutes of Health and NIH roadmap for Medical Research, Michigan Institute for Clinical and Health Research (MICHR) UL1TR000433, University of Illinois at Chicago CTSA UL1RR029879, Tulane COBRE for Clinical and Translational Research in Cardiometabolic Diseases P20 GM109036, Kaiser Permanente NIH/NCRR UCSF-CTSI UL1 RR-024131, and Department of Internal Medicine, University of New Mexico School of Medicine Albuquerque, NM R01DK119199. Funding for M.L.E. was provided by NIA K01-AG075353 and by an NHBLI Research Supplement to Promote Diversity in Health-Related Research 75N92019D00012 to the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Chicago Field Center. P.A.-M. is funded by the NIMHD 5U54MD012523 Center For Health Equity Research (CHER). J.P.L. is funded by NIDDK K24 DK092290.
AUTHORS’ CONTRIBUTIONS
M.L.E., A.C.R., J.P.L. and C.L. conceived and designed the study. M.L.E. wrote the first draft of the manuscript. M.L.E., P.A.-M., A.C.R., J.P.L. and C.L. contributed to the writing of the manuscript and made critical revisions. All the authors reviewed and approved the final manuscript.
DATA AVAILABILITY STATEMENT
The data supporting the findings of this study are available in the NIDDK repository at https://repository.niddk.nih.gov/studies/cric/.
CONFLICT OF INTEREST STATEMENT
The authors have no financial relationships to disclose. The results presented in this paper have not been published previously in whole or part, except in abstract format.
REFERENCES
- 1. Institute of Medicine Health literacy: Past, present, and future: Workshop Summary. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- 2. Fang G, Bailey SC, Annis IEet al. Effects of estimated community-level health literacy on treatment initiation and preventive care among older adults with newly diagnosed diabetes. Patient Prefer Adherence 2020;14:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gazmararian JA, Williams M V, Peel Jet al. Health literacy and knowledge of chronic disease. Patient Educ Couns 2003;51:267–75. [DOI] [PubMed] [Google Scholar]
- 4. Miller TA. Health literacy and adherence to medical treatment in chronic and acute illness: a meta-analysis. Patient Educ Couns 2016;99:1079–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Berkman ND, Sheridan SL, Donahue KEet al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155:97. http://www.ncbi.nlm.nih.gov/pubmed/21768583 [DOI] [PubMed] [Google Scholar]
- 6. Magnani JW, Mujahid MS, Aronow HDet al. Health literacy and cardiovascular disease: fundamental relevance to primary and secondary prevention: a scientific statement from the American Heart Association. Circulation 2018;138:e48–74. http://www.ncbi.nlm.nih.gov/pubmed/29866648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lora CM, Gordon EJ, Sharp LKet al. Progression of CKD in Hispanics: potential roles of health literacy, acculturation, and social support. Am J Kidney Dis 2011;58:282–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kripalani S, Jacobson TA, Mugalla ICet al. Health literacy and the quality of physician-patient communication during hospitalization. J Hosp Med 2010;5:269–75. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3468649/?report=abstract [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Taylor DM, Fraser SDS, Bradley JAet al. A systematic review of the prevalence and associations of limited health literacy in CKD. Clin J Am Soc Nephrol 2017;12:1070–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cavanaugh KL, Wingard RL, Hakim RMet al. Low health literacy associates with increased mortality in ESRD. J Am Soc Nephrol 2010;21:1979–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Green JA, Mor MK, Shields AMet al. Associations of health literacy with dialysis adherence and health resource utilization in patients receiving maintenance hemodialysis. Am J Kidney Dis 2013;62:73–80. [DOI] [PubMed] [Google Scholar]
- 12. Ricardo AC, Yang W, Lora CMet al. Limited health literacy is associated with low glomerular filtration in the Chronic Renal Insufficiency Cohort (CRIC) study. Clin Nephrol 2014;81:30–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Chronic Kidney Disease in the United States, 2019. Atlanta, GA: Centers for Disease Control and Prevention. [Google Scholar]
- 14. Feldman HI, Appel LJ, Chertow GMet al. The Chronic Renal Insufficiency Cohort (CRIC) study: design and methods. J Am Soc Nephrol 2003;14:S148–53. [DOI] [PubMed] [Google Scholar]
- 15. Lash JP, Go AS, Appel LJet al. Chronic Renal Insufficiency Cohort (CRIC) study: baseline characteristics and associations with kidney function. Clin J Am Soc Nephrol 2009;4:1302–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Baker DW, Williams MV, Parker RMet al. Development of a brief test to measure functional health literacy. Patient Educ Couns 1999;38:33–42. [DOI] [PubMed] [Google Scholar]
- 17. Anderson AH, Yang W, Hsu CYet al. Estimating GFR among participants in the Chronic Renal Insufficiency Cohort (CRIC) study. Am J Kidney Dis 2012;60:250–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lash JP, Ricardo AC, Roy Jet al. Race/ethnicity and cardiovascular outcomes in adults with CKD: findings from the CRIC (Chronic Renal Insufficiency Cohort) and hispanic CRIC studies. Am J Kidney Dis 2016;68:545–53. https://pubmed.ncbi.nlm.nih.gov/27209443/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ho KKL, Anderson KM, Kannel WBet al. Survival after the onset of congestive heart failure in Framingham Heart Study subjects. Circulation 1993;88:107–15. https://pubmed.ncbi.nlm.nih.gov/8319323/ [DOI] [PubMed] [Google Scholar]
- 20. van der Laan M, Polley E, van der Laan, MJ, Hubbard, A. Super Learner in UC Berkeley Division of Biostatics Working Paper 2007. Available from: https://biostats.bepress.com/ucbbiostat/paper222 (6 October 2020, date last accessed). [Google Scholar]
- 21. Adeseun GA, Bonney CC, Rosas SE.. Health literacy associated with blood pressure but not other cardiovascular disease risk factors among dialysis patients. Am J Hypertens 2012;25:348–53. http://www.ncbi.nlm.nih.gov/pubmed/22237154 [DOI] [PubMed] [Google Scholar]
- 22. Du S, Zhou Y, Fu Cet al. Health literacy and health outcomes in hypertension: an integrative review. Int J Nurs Sci 2018;5:301–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Marciano L, Camerini AL, Schulz PJ.. The role of health literacy in diabetes knowledge, self-care, and glycemic control: a meta-analysis. J Gen Intern Med 2019;34:1007–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lindahl B, Norberg M, Johansson Het al. Health literacy is independently and inversely associated with carotid artery plaques and cardiovascular risk. Eur J Prev Cardiol 2020;27:209–15. [DOI] [PubMed] [Google Scholar]
- 25. Berkman ND, Sheridan SL, Donahue KEet al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155:97–107. [DOI] [PubMed] [Google Scholar]
- 26. Baker DW, Parker RM, Williams MVet al. Health literacy and the risk of hospital admission. J Gen Intern Med 1998;13:791–8. http://link.springer.com/10.1046/j.1525-1497.1998.00242.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Baker DW, Gazmararian JA, Williams MVet al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Public Health 2002;92:1278–83. http://ajph.aphapublications.org/doi/10.2105/AJPH.92.8.1278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bailey SC, Fang G, Annis IEet al. Health literacy and 30-day hospital readmission after acute myocardial infarction. BMJ Open 2015;5:e006975. http://bmjopen.bmj.com/cgi/doi/10.1136/bmjopen-2014-006975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Peterson PN, Shetterly SM, Clarke CLet al. Health literacy and outcomes among patients with heart failure. JAMA 2011;305:1695–1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Saran R, Robinson B, Abbott KCet al. US renal data system 2018 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis 2019;73:A7–8. https://pubmed.ncbi.nlm.nih.gov/30798791/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nitsch D, Nonyane BAS, Smeeth Let al. CKD and hospitalization in the elderly: a community-based cohort study in the United Kingdom. Am J Kidney Dis 2011;57:664–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Honeycutt AA, Segel JE, Zhuo Xet al. Medical costs of CKD in the Medicare population. J Am Soc Nephrol 2013;24:1478–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Smith DH, Gullion CM, Nichols Get al. Cost of medical care for chronic kidney disease and comorbidity among enrollees in a large HMO population. J Am Soc Nephrol 2004;15:1300–1306. [DOI] [PubMed] [Google Scholar]
- 34. Morton RL, Schlackow I, Staplin Net al. Impact of educational attainment on health outcomes in moderate to severe CKD. Am J Kidney Dis 2016; 67:31. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4685934/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ricardo AC, Roy JA, Tao Ket al. Influence of nephrologist care on management and outcomes in adults with chronic kidney disease. J Gen Intern Med 2016;31:22–9. http://link.springer.com/10.1007/s11606-015-3452-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Devraj R, Gordon EJ.. Health literacy and kidney disease: toward a new line of research. Am J Kidney Dis 2009;53:884–9. http://www.ncbi.nlm.nih.gov/pubmed/19324481 [DOI] [PubMed] [Google Scholar]
- 37. Berkman, ND, Stacey Sheridan ML, Katrina Donahue MEet al. Evidence report/technology assessment health literacy interventions and outcomes: an updated systematic review; 2011. Available from: www.ahrq.gov (2 August 2020, date last accessed). [PMC free article] [PubMed] [Google Scholar]
- 38. Allen-Meares P, Lowry B, Estrella MLet al. Health literacy barriers in the health care system: barriers and opportunities for the profession. Health Soc Work 2020;45:62–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rolison JJ, Wood S, Hanoch Yet al. Subjective numeracy scale as a tool for assessing statistical numeracy in older adult populations. Gerontology 2013;59:283–8. http://proxy.cc.uic.edu/login?url=https://search.proquest.com/docview/1508426850?accountid=14552 [DOI] [PubMed] [Google Scholar]
- 40. Health Literacy: Report of the Council on Scientific Affairs . Ad hoc committee on health literacy for the council on scientific affairs, American Medical Association. JAMA 1999;281:552–7. http://www.ncbi.nlm.nih.gov/pubmed/10022112 [PubMed] [Google Scholar]
- 41. Kickbusch IS. Health literacy: addressing the health and education divide. Health Promot Int 2001;16:289–97. https://academic.oup.com/heapro/article/16/3/289/653857 [DOI] [PubMed] [Google Scholar]
- 42. Berkman ND, Donahue K, Halpern Det al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155:97–107. www.annals.org [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data supporting the findings of this study are available in the NIDDK repository at https://repository.niddk.nih.gov/studies/cric/.