This systematic review and meta-analysis evaluates the association between daily alcohol intake and risk of all-cause mortality.
Key Points
Question
What is the association between mean daily alcohol intake and all-cause mortality?
Findings
This systematic review and meta-analysis of 107 cohort studies involving more than 4.8 million participants found no significant reductions in risk of all-cause mortality for drinkers who drank less than 25 g of ethanol per day (about 2 Canadian standard drinks compared with lifetime nondrinkers) after adjustment for key study characteristics such as median age and sex of study cohorts. There was a significantly increased risk of all-cause mortality among female drinkers who drank 25 or more grams per day and among male drinkers who drank 45 or more grams per day.
Meaning
Low-volume alcohol drinking was not associated with protection against death from all causes.
Abstract
Importance
A previous meta-analysis of the association between alcohol use and all-cause mortality found no statistically significant reductions in mortality risk at low levels of consumption compared with lifetime nondrinkers. However, the risk estimates may have been affected by the number and quality of studies then available, especially those for women and younger cohorts.
Objective
To investigate the association between alcohol use and all-cause mortality, and how sources of bias may change results.
Data Sources
A systematic search of PubMed and Web of Science was performed to identify studies published between January 1980 and July 2021.
Study Selection
Cohort studies were identified by systematic review to facilitate comparisons of studies with and without some degree of controls for biases affecting distinctions between abstainers and drinkers. The review identified 107 studies of alcohol use and all-cause mortality published from 1980 to July 2021.
Data Extraction and Synthesis
Mixed linear regression models were used to model relative risks, first pooled for all studies and then stratified by cohort median age (<56 vs ≥56 years) and sex (male vs female). Data were analyzed from September 2021 to August 2022.
Main Outcomes and Measures
Relative risk estimates for the association between mean daily alcohol intake and all-cause mortality.
Results
There were 724 risk estimates of all-cause mortality due to alcohol intake from the 107 cohort studies (4 838 825 participants and 425 564 deaths available) for the analysis. In models adjusting for potential confounding effects of sampling variation, former drinker bias, and other prespecified study-level quality criteria, the meta-analysis of all 107 included studies found no significantly reduced risk of all-cause mortality among occasional (>0 to <1.3 g of ethanol per day; relative risk [RR], 0.96; 95% CI, 0.86-1.06; P = .41) or low-volume drinkers (1.3-24.0 g per day; RR, 0.93; P = .07) compared with lifetime nondrinkers. In the fully adjusted model, there was a nonsignificantly increased risk of all-cause mortality among drinkers who drank 25 to 44 g per day (RR, 1.05; P = .28) and significantly increased risk for drinkers who drank 45 to 64 and 65 or more grams per day (RR, 1.19 and 1.35; P < .001). There were significantly larger risks of mortality among female drinkers compared with female lifetime nondrinkers (RR, 1.22; P = .03).
Conclusions and Relevance
In this updated systematic review and meta-analysis, daily low or moderate alcohol intake was not significantly associated with all-cause mortality risk, while increased risk was evident at higher consumption levels, starting at lower levels for women than men.
Introduction
The proposition that low-dose alcohol use protects against all-cause mortality in general populations continues to be controversial.1 Observational studies tend to show that people classified as “moderate drinkers” have longer life expectancy and are less likely to die from heart disease than those classified as abstainers.2 Systematic reviews and meta-analyses of this literature3 confirm J-shaped risk curves (protective associations at low doses with increasing risk at higher doses). However, mounting evidence suggests these associations might be due to systematic biases that affect many studies. For example, light and moderate drinkers are systematically healthier than current abstainers on a range of health indicators unlikely to be associated with alcohol use eg, dental hygiene, exercise routines, diet, weight, income4; lifetime abstainers may be systematically biased toward poorer health5; studies fail to control for biases in the abstainer reference group, in particular failing to remove “sick quitters” or former drinkers, many of whom cut down or stop for health reasons2; and most studies have nonrepresentative samples leading to an overrepresentation of older White men. Adjustment of cohort samples to make them more representative has been shown to eliminate apparent protective associations.6 Mendelian randomization studies that control for the confounding effects of sociodemographic and environmental factors find no evidence of cardioprotection.7
We published 2 previous systematic reviews and meta-analyses that investigated these hypotheses. The first of these focused on all-cause mortality,8 finding negligible reductions in mortality risk with low-volume alcohol use when study-level controls were introduced for potential bias and confounding, such as the widespread practice of misclassifying former drinkers and/or current occasional drinkers as abstainers (ie, not restricting reference groups to lifetime abstainers).8 Our alcohol and coronary heart disease (CHD) mortality meta-analysis of 45 cohort studies9 found that CHD mortality risk differed widely by age ranges and sex of study populations. In particular, young cohorts followed up to old age did not show significant cardio-protection for low-volume use. Cardio-protection was only apparent among older cohorts that are more exposed to lifetime selection biases (ie, increasing numbers of “sick-quitters” in the abstainer reference groups and the disproportionate elimination of drinkers from the study sample who had died or were unwell).
The present study updates our earlier systematic review and meta-analysis for all-cause mortality and alcohol use,8 including studies published up to July 2021 (ie, 6.5 years of additional publications). The study also investigated the risk of all-cause mortality for alcohol consumption according to (1) median ages of the study populations (younger than 56 years or 56 years and older), replicating the methods of Zhao et al9; (2) the sex distribution of the study populations, and (3) studies of cohorts recruited before a median age of 51 years of age and followed up in health records until a median age of at least 60 years (ie, with stricter rules to further minimize lifetime selection biases). Because younger cohorts followed up to an age at which they may experience heart disease are less likely to be affected by lifetime selection biases,9 we hypothesized that such studies would be less likely to show reduced mortality risks for low-volume drinkers. Finally, we reran the analyses using occasional drinkers (<1 drink per week) as the reference, for whom physiological health benefits are unlikely. Occasional drinkers are a more appropriate reference group, given evidence demonstrating that lifetime abstainers may be biased toward ill health.10
Methods
The present study updates the systematic reviews and meta-analyses described above8 by including studies published up to July 2021 to investigate whether the risk differed for subgroups. The study protocol was preregistered on the Open Science Framework.11 Inclusion criteria, search strategy, study selection, data extraction, and statistical analytical methods of the study are summarized in later sections (see eAppendix in Supplement 1 for more details).
The systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline.12 The review sought cohort studies of all-cause mortality and alcohol consumption. We identified all potentially relevant articles published up to July 31, 2021, regardless of language, by searching PubMed and Web of Science, through reference list cross-checking of previous meta-analyses (eFigure 1 in Supplement 1). There were 87 studies identified by Stockwell et al.8 After inclusion of 20 new studies meeting inclusion criteria, there were a total of 107 cohort studies (eTable 1 in Supplement 1).13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32
Three coders (J. Z., F. A., and J. C.) reviewed all eligible studies to extract and code data independently from all studies fulfilling the inclusion criteria. Data extracted included (1) outcome, all-cause mortality; (2) measures of alcohol consumption; (3) study characteristics, including cohort ages at recruitment and follow-up; (4) types of misclassification error of alcohol consumers and abstainers; (5) controlled variables in individual studies. Alcoholic drinks were converted into grams per day according to country-specific definitions if not otherwise defined.33,34
Statistical Analysis
We also assessed publication bias, heterogeneity, and confounding of covariates that might potentially affect the association of interest using several statistical approaches.35,36,37,38,39,40,41 Relative risk (RR), including hazard ratios or rate ratios, were converted to natural log-transformed formats to deal with skewness. Publication bias was assessed through visual inspection of the funnel plot of log-RR of all-cause mortality due to alcohol consumption against the inverse standard error of log-RR42 and Egger’s linear regression method.36 We also plotted forest graphs of log-RR of all-cause mortality for any level of drinking to assess heterogeneity among studies.42 The between-study heterogeneity of RRs were assessed using Cochran Q37 and the I2 statistic.38 If heterogeneity was detected, mixed-effects models were used to obtain the summarized RR estimates. Mixed-effects regression analyses were performed in which drinking groups and control variables were treated as fixed-effects with a random study effect because of significant heterogeneity.43
All analyses were weighted by the inverse of the estimated variance of the natural log relative risk. Variance was estimated from reported standard errors, confidence intervals, or number of deaths. The weights for each individual study were created using the inverse variance weight scheme and used in mixed regression analysis to get maximum precision for the main results of the meta-analysis.42 In comparison with lifetime abstainers, the study estimated the mean RR of all-cause mortality for former drinkers (ie, now completely abstaining), current occasional (<9.1 g per week), low-volume (1.3-24.0 g per day), medium-volume (25.0-44.0 g per day), high-volume (45.0-64.0 g) and highest-volume drinkers (≥65.0 grams per day). The analyses adjusted for the potential confounding effects of study characteristics including the median age and sex distribution of study samples, drinker biases, country where a study was conducted, follow-up years and presence or absence of confounders. Analyses were also repeated using occasional drinkers as the reference group. We used t tests to calculate P values, and significance was set at .05. All statistical analyses were performed using SAS version 9.4 (SAS Institute) and the SAS MIXED procedure was used to model the log-transformed RR.44 Data were analyzed from September 2021 to August 2022.
Results
Characteristics of Included Studies
There were 724 estimates of the risk relationship between level of alcohol consumption and all-cause mortality from 107 unique studies13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131, including 4 838 825 participants and 425 564 deaths available for the analysis. Table 1 describes the sample characteristics of the metadata. Of 39 studies13,15,18,21,23,24,25,26,29,31,45,46,47,49,50,52,53,54,57,58,59,62,64,70,80,81,85,87,91,94,96,100,104,107,118,124,125,127,130reporting RR estimates for men and women separately, 3314,17,48,51,61,63,66,68,69,72,76,79,83,84,86,88,90,92,93,97,98,101,103,105,109,110,111,113,114,115,119,120,128 were for males only, 816,65,73,99,102,108,112,123 for females only, and 3013,19,20,21,22,26,27,28,29,30,32,55,56,67,71,74,75,77,78,82,84,89,95,106,116,117,121,122,126,129 for both sexes. Twenty-one studies13,17,19,21,22,26,27,45,46,47,48,49,50,51,52,53,54,55,56,57,58 (220 risk estimates) were free from abstainer bias (ie, had a reference group of strictly defined lifetime abstainers). There were 50 studies14,15,16,18,20,23,24,25,29,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99 (265 risk estimates) with both former and occasional drinker bias; 28 studies28,30,31,32,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,130 (177 risk estimates) with only former drinker bias; and 8 studies123,124,125,126,127,128,129,131 (62 risk estimates) with only occasional drinker bias.
Table 1. The Sample Characteristics of the Metadata on All-Cause Mortality and Alcohol Consumption From 1980 to 2022.
| Covariates | All-cause mortality studies (n = 107) | Mean RR (95% CI)b | P value | |
|---|---|---|---|---|
| Studies, No. (%) | No. of RRs (%)a | |||
| Publication year | ||||
| 1980-2004 | 51 (47.66) | 310 (42.82) | 1.08 (1.03-1.14) | .26 |
| 2005-2014 | 36 (33.64) | 220 (30.39) | 1.07 (1.00-1.13) | .44 |
| 2015-2021c | 20 (18.69) | 194 (26.80) | 1.03 (0.96-1.10) | NA |
| Median age, yd | ||||
| 19-55 | 67 (59.29) | 438 (60.50) | 1.10 (1.05-1.14) | .02 |
| 56-78c | 46 (40.71) | 286 (39.50) | 1.01 (0.96-1.07) | NA |
| Sex | ||||
| Men only | 73 (48.03) | 343 (47.38) | 1.05 (1.00-1.11) | .47 |
| Women only | 48 (31.58) | 226 (31.22) | 1.11 (1.05-1.17) | .08 |
| Men and womenc | 31 (20.39) | 155 (21.41) | 1.02 (0.94-1.10) | NA |
| Countries | ||||
| North and Central America | 41 (37.96) | 287 (39.64) | 1.05 (1.00-1.11) | .58 |
| Europe and Australia | 53 (49.07) | 343 (47.38) | 1.07 (1.02-1.12) | .79 |
| Asiac | 14 (12.96) | 94 (12.98) | 1.08 (0.98-1.18) | NA |
| Follow-up years | ||||
| 03.70-10.50c | 45 (42.06) | 266 (36.74) | 0.98 (0.92-1.03) | NA |
| 11.00-41.00 | 62 (57.94) | 458 (63.26) | 1.12 (1.07-1.16) | <.001 |
| Baseline conditionse | ||||
| Exclusion/control | 49 (45.37) | 342 (47.24) | 1.12 (1.07-1.17) | .004 |
| No exclusion/control | 59 (54.63) | 382 (52.76) | 1.01 (0.97-1.06) | |
| Alcohol use measure | ||||
| Quantity-frequency | 30 (28.04) | 222 (30.66) | 1.18 (1.12-1.25) | <.001 |
| Othersc | 77 (71.96) | 502 (69.34) | 1.01 (0.97-1.05) | NA |
| Abstainer biases | ||||
| Both former and occasional | 50 (46.73) | 265 (36.60) | 0.98 (0.92-1.04) | <.001 |
| Former drinker bias only | 28 (26.17) | 177 (24.45) | 1.05 (0.98-1.12) | .005 |
| Occasional bias only | 8 (7.48) | 62 (8.56) | 1.01 (0.89-1.13) | .009 |
| Neither biasc,f | 21 (19.63) | 220 (30.39) | 1.19 (1.12-1.25) | NA |
| Control for smokingg | ||||
| No | 18 (16.51) | 135 (18.65) | 1.09 (1.01-1.18) | .43 |
| Yesc | 91 (83.49) | 589 (81.35) | 1.06 (1.02-1.10) | NA |
| Control for SES | ||||
| No | 39 (36.11) | 245 (33.84) | 1.16 (1.10-1.22) | <.001 |
| Yesc | 69 (63.89) | 479 (66.16) | 1.01 (0.97-1.06) | NA |
| Control for race | ||||
| No | 79 (73.83) | 530 (73.20) | 1.07 (1.02-1.11) | .85 |
| Yesc | 28 (26.17) | 194 (26.80) | 1.06 (0.99-1.13) | NA |
| Control for diet | ||||
| No | 90 (84.11) | 570 (78.73) | 1.06 (1.02-1.10) | .84 |
| Yesc | 17 (15.89) | 154 (21.27) | 1.07 (0.99-1.15) | NA |
| Control for exercise | ||||
| No | 63 (58.88) | 431 (59.53) | 1.04 (1.00-1.09) | .13 |
| Yesc | 44 (41.12) | 293 (40.47) | 1.10 (1.04-1.15) | NA |
| Control for BMIh | ||||
| No | 48 (44.04) | 294 (40.61) | 1.09 (1.03-1.14) | .28 |
| Yesc | 61 (55.96) | 430 (59.39) | 1.05 (1.00-1.09) | NA |
Abbreviations: BMI, body mass index; NA, not applicable; RR, relative risk; SES, socioeconomic status.
Number of relative risk estimates for any drinking from the included studies.
Unadjusted mean relative risk (RR) and 95% confidence interval (CI) due to any drinking from the included studies.
Reference category.
Median age at study enrollment.
Control for heart disease and/or other illnesses.
Lifetime abstention was strictly defined as 0 consumption or never drank 1 drink and did not include studies with any level of occasional lifetime or past year drinking (eg, less than 12 drinks or “rarely” or “hardly ever” drinking).
Smoking confounding effect was adjusted for in multivariable regression analysis in original studies.
Body mass index is calculated as weight in kilograms divided by height in meters squared.
Unadjusted mean RR estimates for most study subgroups categorized by methods/sample characteristics showed markedly or significantly higher RRs for alcohol consumers as a group vs abstainers. Exceptions were for studies with less than 10 years of follow-up and those with some form of abstainer bias (Table 1). Bivariable analyses showed that mortality risks for alcohol consumers varied considerably according to other study characteristics, such as quality of the alcohol consumption measure, whether unhealthy individuals were excluded at baseline, and whether socioeconomic status was controlled for (Table 1).
No evidence of publication bias was detected either by inspection of symmetry in the funnel plot of log-RR estimates and their inverse standard errors (eFigure 2 in Supplement 1) or by Egger linear regression analysis (eTable 2 in Supplement 1, all P > .05 for each study group). Significant heterogeneity was observed across studies for all drinking categories confirmed by both the Q statistic (Q723 = 5314.80; P < .001) and I2 estimates (all >85.87%). (See eFigure 3 in Supplement 1 for forest plot of unadjusted risk estimates of mortality risks for the 20 newly identified studies).
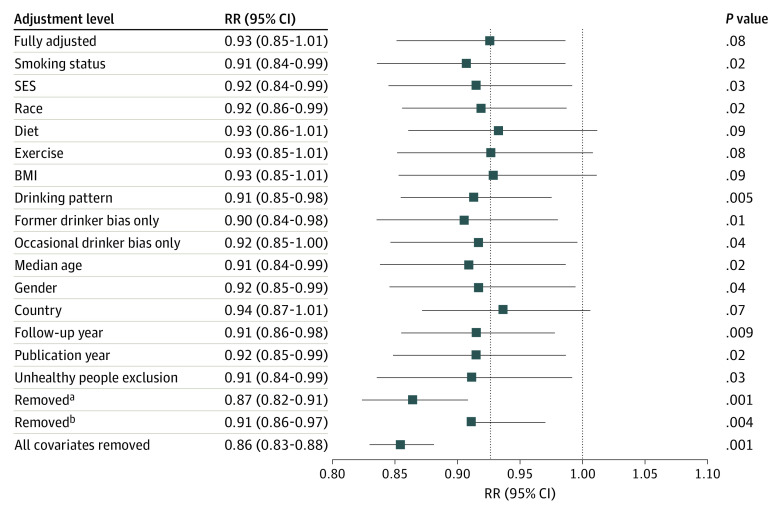
All-Cause Mortality Risk for Drinkers From Meta-analysis of Pooled Studies
Pooled unadjusted estimates (724 observations) showed significantly higher risk for former drinkers (RR, 1.22; 95% CI, 1.11-1.33; P = .001) and significantly lower risk for low-volume drinkers (RR, 0.85; 95% CI, 0.81-0.88; P = .001) compared with abstainers as defined in the included studies (Table 2; eFigure 4 in Supplement 1). In the fully adjusted model, mortality RR estimates increased for all drinking categories, becoming nonsignificant for low-volume drinkers (RR, 0.93; 95% CI, 0.85-1.01; P = .07), occasional drinkers (>0 to <1.3 g of ethanol per day; RR, 0.96; 95% CI, 0.86-1.06; P = .41), and drinkers who drank 25 to 44 g per day (RR, 1.05; 95% CI, 0.96-1.14; P = .28). There was a significantly increased risk among drinkers who drank 45 to 64 g per day (RR, 1.19; 95% CI, 1.07-1.32; P < .001) and 65 or more grams (RR, 1.35; 95% CI, 1.23-1.47; P < .001). The Figure shows the changes in RR estimates for low-volume drinkers when removing each covariate from the fully adjusted model. In most cases, removing study-level covariates tended to yield lower risk estimates from alcohol use.
Table 2. Mean Relative Risk Estimates of All-Cause Mortality Due to Alcohol Consumption Up to 2022 According to 107 Studies With 724 Relative Risk Estimates.
| Drinking categories | Studies, No./risk estimates, No. | Unadjusteda | Partially adjustedb | Fully adjustedc | ||||
|---|---|---|---|---|---|---|---|---|
| RR (95% CI) | P value | RR (95% CI) | P value | RR (95% CI) | P value | |||
| Reference group = lifetime nondrinker | ||||||||
| Abstainer | 107/191 | 1 [Reference] | 1 [Reference] | 1 [Reference] | ||||
| Any drinker vs abstainer | 107/724 | 1.06 (0.90-1.25) | .42 | 1.03 (0.89-1.19) | .65 | 1.11 (0.96-1.28) | .12 | |
| Former drinker vs abstainer | 28/56 | 1.22 (1.11-1.33) | <.001 | 1.17 (1.08-1.26) | <.001 | 1.26 (1.12-1.42) | .0001 | |
| Active drinker vs abstainer, g/d | 107/668 | 0.97 (0.94-1.00) | .02 | 0.93 (0.90-0.96) | <.001 | 1.02 (0.93-1.13) | .61 | |
| Occasional (<1.30) | 24/57 | 0.92 (0.84-1.01) | .08 | 0.89 (0.83-0.95) | <.001 | 0.96 (0.86-1.06) | .41 | |
| Low-volume (1.30 to <25) | 99/306 | 0.85 (0.81-0.88) | <.001 | 0.86 (0.83-0.88) | <.001 | 0.93 (0.85-1.01) | .08 | |
| Medium volume (25 to <45) | 80/146 | 1.02 (0.96-1.08) | .55 | 0.97 (0.92-1.02) | .21 | 1.05 (0.96-1.14) | .28 | |
| High volume (45 to <65) | 52/76 | 1.07 (0.99-1.16) | .09 | 1.11 (1.03-1.21) | .009 | 1.19 (1.07-1.32) | .001 | |
| Higher volume (≥65) | 45/83 | 1.35 (1.26-1.46) | <.001 | 1.24 (1.16-1.32) | <.001 | 1.35 (1.23-1.47) | .0001 | |
| Reference group = occasional drinker | ||||||||
| Abstainer | 1.09 (0.99-1.19) | .07 | 1.12 (1.05-1.20) | <.001 | 1.04 (0.94-1.16) | .45 | ||
| Any drinker vs occasional drinker | 107/724 | 1.15 (0.95-1.39) | .14 | 1.16 (0.99-1.36) | .08 | 1.16 (0.97-1.38) | .11 | |
| Former drinker vs abstainer | 28/56 | 1.33 (1.18-1.50) | <.001 | 1.31 (1.19-1.46) | <.001 | 1.31 (1.13-1.52) | .0007 | |
| Active drinker vs abstainer, g/d | 107/668 | 1.05 (0.96-1.16) | .29 | 1.04 (0.97-1.13) | .25 | 1.06 (0.92-1.23) | .41 | |
| Occasional (<1.30) | 24/57 | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | ||
| Low-volume (1.30 to <25) | 99/306 | 0.92 (0.84-1.02) | .12 | 0.97 (0.90-1.04) | .36 | 0.97 (0.85-1.11) | .65 | |
| Medium volume (25 to <45) | 80/146 | 1.11 (0.99-1.24) | .07 | 1.09 (1.00-1.19) | .047 | 1.09 (0.96-1.25) | .19 | |
| High volume (45 to <65) | 52/76 | 1.16 (1.03-1.31) | .02 | 1.25 (1.12-1.39) | <.001 | 1.24 (1.07-1.44) | .004 | |
| Higher volume (≥65) | 45/83 | 1.47 (1.30-1.65) | <.001 | 1.39 (1.27-1.53) | <.001 | 1.41 (1.23-1.61) | .0001 | |
Abbreviations: NA, not applicable; RR, relative risk.
Natural log of the RR estimated using the rate ratio or hazard ratio without weighting and adjusting for between-study variation or covariates.
Weighted estimates adjusted for between-study variation.
Weighted estimates adjusted for between-study variation, abstainer biases, median age, sex, country in which a study was conducted, study publication year, follow-up years of study samples, drinking pattern, and whether studies controlled for heart problem, social status, race, diet, exercise, body mass index, and smoking status.
Figure. Relative Risk (RR) of All-Cause Mortality Due to Low-Volume Alcohol Consumption (1.3-24.0 g Ethanol per Day) With and Without Adjustment for Potential Confounding by Each Covariate or Set of Covariates.
BMI indicates body mass index; SES, socioeconomic status.
aVariables smoking status, SES, drinking pattern, former drinker bias only, occasional drinker bias, median age, and gender were removed.
bVariables race, diet, exercise, BMI, country, follow-up year, publication year, and unhealthy people exclusion were removed.
Table 2 presents the RR estimates when occasional drinkers were the reference group. In fully adjusted models, higher though nonsignificant mortality risks were observed for both abstainers and medium-volume drinkers (RR, 1.04; 95% CI, 0.94-1.16; P = .44 and RR, 1.09; 95% CI, 0.96-1.25; P = .19, respectively). There were significantly elevated risks for both high and higher volume drinkers (RR, 1.24; 95% CI, 1.07-1.44; P = .004 and RR, 1.41; 95% CI, 1.23-1.61; .P = 001, respectively).
All-Cause Mortality Risk on the Basis of Median Age of Study Cohorts at Baseline
As hypothesized, there was a significant interaction between cohort age and mortality risk (P = .02; F601 = 2.93) and so RR estimates for drinkers were estimated in analyses stratified by median age of the study populations at enrollment (Table 3). In unadjusted and partially adjusted analyses, older cohorts displayed larger reductions in mortality risk associated with low-volume consumption than younger cohorts. However, in fully adjusted analyses with multiple covariates included for study characteristics, these differences disappeared. Younger cohorts also displayed greater mortality risks than older cohorts at higher consumption levels. Among studies in which participants were recruited at age 50 years or younger and followed up to age 60 years (ie, there was likely reduced risk of lifetime selection bias) higher RR estimates were observed for all drinking groups vs lifetime abstainers. These differences were significant in all drinking groups except low-volume drinkers (eTable 3 in Supplement 1).
Table 3. Mean RR Estimates of All-Cause Mortality Due to Alcohol Consumption by Median Age at Enrollment of Studies (<56 or ≥56 y) Up to 2022.
| Drinking categories by median age at enrollment in included studies | Studies, No./risk estimates, No. | Unadjusteda | Partially adjustedb | Fully adjustedc | |||
|---|---|---|---|---|---|---|---|
| RR (95% CI) | P value | RR (95% CI) | P value | RR (95% CI) | P value | ||
| Median age, younger than 56 y | |||||||
| Abstainer | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Any drinker vs abstainer | 67/436 | 1.08 (0.91-1.28) | .32 | 1.06 (0.93-1.22) | .30 | 1.13 (0.98-1.30) | .07 |
| Former drinker vs abstainer | 12/27 | 1.26 (1.11-1.42) | <.001 | 1.16 (1.06-1.26) | .001 | 1.23 (1.08-1.39) | .001 |
| Active drinker vs abstainer, g/d | 67/411 | 1.00 (0.96-1.03) | .93 | 0.96 (0.92-1.00) | .04 | 1.05 (0.97-1.13) | .26 |
| Occasional (<1.30) | 14/31 | 0.89 (0.80-1.01) | .06 | 0.96 (0.90-1.03) | .22 | 1.02 (0.94-1.11) | .62 |
| Low-volume (1.30 to <25) | 61/202 | 0.88 (0.84-0.93) | <.001 | 0.88 (0.84-0.91) | <.001 | 0.93 (0.86-1.01) | .10 |
| Medium volume (25 to <45) | 49/91 | 1.10 (1.03-1.18) | .005 | 1.00 (0.93-1.06) | .91 | 1.06 (0.96-1.16) | .25 |
| High volume (45 to <65) | 25/34 | 1.03 (0.92-1.15) | .60 | 1.16 (1.05-1.29) | .004 | 1.24 (1.10-1.40) | <.001 |
| Higher volume (≥65) | 28/53 | 1.39 (1.27-1.53) | <.001 | 1.29 (1.19-1.41) | <.001 | 1.38 (1.23-1.55) | <.001 |
| Median age ≥56 y | |||||||
| Abstainer | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Any drinker vs abstainer | 46/281 | 1.02 (0.85-1.22) | .79 | 0.99 (0.84-1.18) | .94 | 1.09 (0.94-1.27) | .19 |
| Former drinker vs abstainer | 16/29 | 1.18 (1.04-1.34) | .01 | 1.17 (1.06-1.29) | .002 | 1.27 (1.09-1.48) | .002 |
| Active drinker vs abstainer, g/d | 46/257 | 0.92 (0.88-0.97) | .001 | 0.91 (0.87-0.95) | <.001 | 1.02 (0.91-1.15) | .75 |
| Occasional (<1.30) | 12/26 | 0.95 (0.83-1.10) | .51 | 0.83 (0.77-0.90) | <.001 | 0.91 (0.82-1.01) | .09 |
| Low-volume (1.30 to <25) | 44/104 | 0.79 (0.74-0.84) | <.001 | 0.84 (0.81-0.87) | <.001 | 0.93 (0.85-1.02) | .11 |
| Medium volume (25 to <45) | 36/55 | 0.89 (0.81-0.98) | .02 | 0.95 (0.88-1.02) | .14 | 1.04 (0.95-1.14) | .37 |
| High volume (45 to <65) | 28/42 | 1.10 (0.99-1.23) | .08 | 1.05 (0.95-1.16) | .39 | 1.15 (1.02-1.30) | .02 |
| Higher volume (≥65) | 18/30 | 1.29 (1.13-1.47) | <.001 | 1.20 (1.10-1.31) | <.001 | 1.32 (1.18-1.47) | <.001 |
Abbreviations: NA, not applicable; RR, relative risk.
Natural log of the RR estimated using the rate ratio or hazard ratio without weighting and adjusting for between-study variation or covariates.
Weighted estimates adjusted for between-study variation.
Weighted estimates adjusted for between-study variation, abstainer biases, sex, country in which a study was conducted, study publication year, follow-up years, drinking pattern, and whether studies controlled for heart problem, social status, race, diet, exercise, body mass index, and smoking status.
All-Cause Mortality Risk for Drinkers by Sex
Across all levels of alcohol consumption, female drinkers had a higher RR of all-cause mortality than males (P for interaction = .001). As can be seen in Table 4, all female drinkers had a significantly increased mortality risk compared with female lifetime nondrinkers (RR, 1.22; 95% CI, 1.02-1.46; P = .03). Compared with lifetime abstainers, there was significantly increased risk of all-cause mortality among male drinkers who drank 45 to 64 g per day (RR, 1.15; 95% CI, 1.03-1.28; P = .01) and drank 65 or more (RR, 1.34; 95% CI, 1.23-1.47; P < .001), and among female drinkers who drank 25 to 44 g per day (RR, 1.21; 95% CI, 1.08-1.36; P < .01), 45 to 64 g (RR, 1.34; 95% CI, 1.11-1.63; P < .01) and 65 or more grams (RR, 1.61; 95% CI, 1.44-1.80; P = .001).
Table 4. Mean RRs of All-Cause Mortality Due to Alcohol Consumption by Sex (Men or Women) Up to 2022.
| Drinking categories by median age | Studies, No./risk estimates, No. | Unadjusteda | Partially adjustedb | Fully adjustedc | ||||
|---|---|---|---|---|---|---|---|---|
| RR (95% CI) | P value | RR (95% CI) | P value | RR (95% CI) | P value | |||
| Men | ||||||||
| Abstainer | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | |
| Any drinker vs abstainer | 73/343 | 1.05 (0.88-1.24 | .52 | 1.05 (0.89-1.22) | .49 | 1.12 (0.95-1.34) | .14 | |
| Former drinker vs abstainer | 20/24 | 1.24 (1.08-1.42) | <.001 | 1.29 (1.20-1.39) | <.001 | 1.39 (1.21-1.58) | <.001 | |
| Active drinker vs abstainer, g/d | 73/319 | 0.97 (0.93-1.01) | .09 | 0.96 (0.92-1.00) | .05 | 1.05 (0.96-1.15) | .27 | |
| Occasional (<1.30) | 13/15 | 0.95 (0.80-1.13) | .58 | 0.93 (0.85-1.01) | .07 | 1.00 (0.91-1.09) | .97 | |
| Low-volume (1.30 to <25) | 66/141 | 0.84 (0.80-0.89) | <.001 | 0.87 (0.84-0.91) | <.001 | 0.94 (0.88-1.01) | .07 | |
| Medium volume (25 to <45) | 54/70 | 0.97 (0.89-1.05) | .43 | 0.94 (0.90-0.98) | .008 | 1.01 (0.93-1.10) | .81 | |
| High volume (45 to <65) | 37/41 | 1.01 (0.91-1.12) | .87 | 1.07 (1.01-1.12) | .01 | 1.15 (1.03-1.28) | .01 | |
| Higher volume (≥65) | 36/52 | 1.35 (1.23-1.48) | <.001 | 1.25 (1.16-1.32) | <.001 | 1.34 (1.23-1.47) | <.001 | |
| Women | ||||||||
| Abstainer | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | |
| Any drinker vs abstainer | 48/226 | 1.12 (0.88-1.44) | .28 | 1.03 (0.85-1.26) | .69 | 1.22 (1.02-1.46) | .04 | |
| Former drinker vs abstainer | 16/22 | 1.16 (0.98-1.37) | .08 | 1.09 (1.03-1.14) | .001 | 1.27 (1.13-1.43) | <.001 | |
| Active drinker vs abstainer, g/d | 47/204 | 0.99 (0.93-1.05) | .64 | 0.88 (0.84-0.92) | <.001 | 1.03 (0.92-1.15) | .65 | |
| Occasional (<1.30) | 15/25 | 0.87 (0.74-1.01) | .08 | 0.83 (0.78-0.88) | <.001 | 0.99 (0.87-1.11) | .82 | |
| Low-volume (1.30 to <25) | 45/106 | 0.87 (0.81-0.94) | <.001 | 0.84 (0.80-0.89) | <.001 | 0.99 (0.90-1.10) | .90 | |
| Medium volume (25 to <45) | 37/42 | 1.16 (1.03-1.31) | .01 | 1.03 (0.96-1.11) | .44 | 1.21 (1.08-1.36) | .001 | |
| High volume (45 to <65) | 17/19 | 1.12 (0.94-1.34) | .21 | 1.13 (0.95-1.35) | .15 | 1.34 (1.11-1.63) | .003 | |
| Higher volume (≥65) | 11/12 | 1.77 (1.41-2.21) | <.001 | 1.37 (1.28-1.47) | <.001 | 1.61 (1.44-1.80) | <.001 | |
Abbreviations: NA, not applicable; RR, relative risk.
Natural log of the RR estimated using the rate ratio or hazard ratio without weighting and adjusting for between-study variation or covariates.
Weighted estimates adjusted for between-study variation.
Weighted estimates adjusted for between-study variation, abstainer biases, median age, country in which a study was conducted, study publication year, follow-up years, drinking pattern, and whether studies controlled for heart problem, social status, race, diet, exercise, body mass index, and smoking status.
Discussion
In fully adjusted, prespecified models that accounted for effects of sampling, between-study variation, and potential confounding from former drinker bias and other study-level covariates, our meta-analysis of 107 studies found (1) no significant protective associations of occasional or low-volume drinking (moderate drinking) with all-cause mortality; and (2) an increased risk of all-cause mortality for drinkers who drank 25 g or more and a significantly increased risk when drinking 45 g or more per day.
Several meta-analytic strategies were used to explore the role of abstainer reference group biases caused by drinker misclassification errors and also the potential confounding effects of other study-level quality covariates in studies.2 Drinker misclassification errors were common. Of 107 studies identified, 86 included former drinkers and/or occasional drinkers in the abstainer reference group, and only 21 were free of both these abstainer biases. The importance of controlling for former drinker bias/misclassification is highlighted once more in our results which are consistent with prior studies showing that former drinkers have significantly elevated mortality risks compared with lifetime abstainers.
In addition to presenting our fully adjusted models, a strength of the study was the examination of the differences in relative risks according to unadjusted and partially adjusted models, including the effect of removing individual covariates from the fully adjusted model. We found evidence that abstainer biases and other study characteristics changed the shape of the risk relationship between mortality and rising alcohol consumption, and that most study-level controls increased the observed risks from alcohol, or attenuated protective associations at low levels of consumption such that they were no longer significant. The reduced RR estimates for occasional or moderate drinkers observed without adjustment may be due to the misclassification of former and occasional drinkers into the reference group, a possibility which is more likely to have occurred in studies of older cohorts which use current abstainers as the reference group. This study also demonstrates the degree to which observed associations between consumption and mortality are highly dependent on the modeling strategy used and the degree to which efforts are made to minimize confounding and other threats to validity.
It also examined risk estimates when using occasional drinkers rather than lifetime abstainers as the reference group. The occasional drinker reference group avoids the issue of former drinker misclassification that can affect the abstainer reference group, and may reduce confounding to the extent that occasional drinkers are more like low-volume drinkers than are lifetime abstainers.2,8,132 In the unadjusted and partially adjusted analyses, using occasional drinkers as the reference group resulted in nonsignificant protective associations and lower point estimates for low-volume drinkers compared with significant protective associations and higher point estimates when using lifetime nondrinkers as the reference group. In the fully adjusted models, there were nonsignificant protective associations for low-volume drinkers whether using lifetime abstainers or occasional drinkers as the reference group, though this was only a RR of 0.97 for the latter.
Across all studies, there were few differences in risk for studies when stratified by median age of enrollment above or below age 56 years in the fully adjusted analyses. However, in the subset of studies who enrolled participants aged 50 years or younger who were followed for at least 10 years, occasional drinkers and medium-volume drinkers had significantly increased risk of mortality and substantially higher risk estimates for high- and higher-volume consumption compared with results from all studies. This is consistent with our previous meta-analysis for CHD,9 in which younger cohorts followed up to older age did not show a significantly beneficial association of low-volume consumption, while older cohorts, with more opportunity for lifetime selection bias, showed marked, significant protective associations.
Our study also found sex differences in the risk of all-cause mortality. A larger risk of all-cause mortality for women than men was observed when drinking 25 or more grams per day, including a significant increase in risk for medium-level consumption for women that was not observed for men. However, mortality risk for mean consumption up to 25 g per day were very similar for both sexes.
Limitations
A number of limitations need to be acknowledged. A major limitation involves imperfect measurement of alcohol consumption in most included studies, and the fact that consumption in many studies was assessed at only 1 point in time. Self-reported alcohol consumption is underreported in most epidemiological studies133,134 and even the classification of drinkers as lifetime abstainers can be unreliable, with several studies in developed countries finding that the majority of self-reported lifetime abstainers are in fact former drinkers.135,136 If this is the case, the risks of various levels of alcohol consumption relative to presumed lifetime abstainers are underestimates. Merely removing former drinkers from analyses may bias studies in favor of drinkers, since former drinkers may be unhealthy, and should rightly be reallocated to drinking groups according to their history. However, this has only been explored in very few studies. Our study found that mortality risk differed significantly by cohort age and sex. It might be that the risk is also higher for other subgroups, such as people living with HIV,137 a possibility future research should investigate.
The number of available studies in some stratified analyses was small, so there may be limited power to control for potential study level confounders. However, the required number of estimates per variable for linear regression can be much smaller than in logistic regression, and a minimum of at least 2 estimates per variable is recommended for linear regression analysis,138 suggesting the sample sizes were adequate in all models presented. It has been demonstrated that a pattern of binge (ie, heavy episodic) drinking removes the appearance of reduced health risks even when mean daily volume is low.139 Too few studies adequately controlled for this variable to investigate its association with different outcomes across studies. Additionally, our findings only apply to the net effect of alcohol at different doses on all-cause mortality, and different risk associations likely apply for specific disease categories. The biases identified here likely apply to estimates of risk for alcohol and all diseases. It is likely that correcting for these biases will raise risk estimates for many types of outcome compared with most existing estimates.
Conclusions
This updated meta-analysis did not find significantly reduced risk of all-cause mortality associated with low-volume alcohol consumption after adjusting for potential confounding effects of influential study characteristics. Future longitudinal studies in this field should attempt to minimize lifetime selection biases by not including former and occasional drinkers in the reference group, and by using younger cohorts (ie, age distributions that are more representative of drinkers in the general population) at baseline.
eAppendix. Methodology of Meta-analysis on All-Cause Mortality and Alcohol Consumption
eReferences
eFigure 1. Flowchart of Systematic Search Process for Studies of Alcohol Consumption and Risk of All-Cause Mortality
eTable 1. Newly Included 20 Studies (194 Risk Estimates) of All-Cause Mortality and Consumption in 2015 to 2022
eFigure 2. Funnel Plot of Log-Relative Risk (In(RR)) of All-Cause Mortality Due to Alcohol Consumption Against Inverse of Standard Error of In(RR)
eFigure 3. Relative Risk (95% CI) of All-Cause Mortality Due to Any Alcohol Consumption Without Any Adjustment for Characteristics of New Studies Published between 2015 and 2022
eFigure 4. Unadjusted, Partially Adjusted, and Fully Adjusted Relative Risk (RR) of All-Cause Mortality for Drinkers (vs Nondrinkers), 1980 to 2022
eTable 2. Statistical Analysis of Unadjusted Mean Relative Risk (RR) of All-Cause Mortality for Different Categories of Drinkers for Testing Publication Bias and Heterogeneity of RR Estimates From Included Studies
eTable 3. Mean Relative Risk (RR) Estimates of All-Cause Mortality Due to Alcohol Consumption up to 2022 for Subgroups (Cohorts Recruited 50 Years of Age or Younger and Followed up to 60 Years of Age)
Data Sharing Statement
References
- 1.Hawkins BR, McCambridge J. Partners or opponents? Alcohol INDUSTRY STRATEGY AND THE 2016 REVISION of the U.K. LOW-RISK DRINKING GUIDELINES. J Stud Alcohol Drugs. 2021;82(1):84-92. doi: 10.15288/jsad.2021.82.84 [DOI] [PubMed] [Google Scholar]
- 2.Fillmore KM, Kerr WC, Stockwell T, Chikritzhs T, Bostrom A. Moderate alcohol use and reduced mortality risk: systematic error in prospective studies. Addict Res Theory. 2006;14(2):101-132. doi: 10.1080/16066350500497983 [DOI] [PubMed] [Google Scholar]
- 3.Roerecke M, Rehm J. The cardioprotective association of average alcohol consumption and ischaemic heart disease: a systematic review and meta-analysis. Addiction. 2012;107(7):1246-1260. doi: 10.1111/j.1360-0443.2012.03780.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Naimi TS, Brown DW, Brewer RD, et al. Cardiovascular risk factors and confounders among nondrinking and moderate-drinking U.S. adults. Am J Prev Med. 2005;28(4):369-373. doi: 10.1016/j.amepre.2005.01.011 [DOI] [PubMed] [Google Scholar]
- 5.Ng Fat L, Cable N, Shelton N. Worsening of health and a cessation or reduction in alcohol consumption to special occasion drinking across three decades of the life course. Alcohol Clin Exp Res. 2015;39(1):166-174. doi: 10.1111/acer.12596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stamatakis E, Owen KB, Shepherd L, Drayton B, Hamer M, Bauman AE. Is cohort representativeness passé? Poststratified associations of lifestyle risk factors with mortality in the UK biobank. Epidemiology. 2021;32(2):179-188. doi: 10.1097/EDE.0000000000001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Biddinger KJ, Emdin CA, Haas ME, et al. Association of habitual alcohol intake with risk of cardiovascular disease. JAMA Netw Open. 2022;5(3):e223849. doi: 10.1001/jamanetworkopen.2022.3849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T. Do “moderate” drinkers have reduced mortality risk? A systematic review and meta-analysis of alcohol consumption and all-cause mortality. J Stud Alcohol Drugs. 2016;77(2):185-198. doi: 10.15288/jsad.2016.77.185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao J, Stockwell T, Roemer A, Naimi T, Chikritzhs T. Alcohol consumption and mortality from coronary heart disease: an updated meta-analysis of cohort studies. J Stud Alcohol Drugs. 2017;78(3):375-386. doi: 10.15288/jsad.2017.78.375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ng Fat L, Cable N, Marmot MG, Shelton N. Persistent long-standing illness and non-drinking over time, implications for the use of lifetime abstainers as a control group. J Epidemiol Community Health. 2014;68(1):71-77. doi: 10.1136/jech-2013-202576 [DOI] [PubMed] [Google Scholar]
- 11.Stockwell TR, Zhao J, Churchill S, et al. An updated systematic review and new meta analyses of studies on alcohol use and mortality risk that have reduced risk of lifetime selection biases. Open Science Framework. 2021. Accessed March 13, 2023. https://osf.io/tnhd3/
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG, Grp P; PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaprio J, Latvala A, Rose R.. Longitudinal patterns of alcohol use and mortality: a 40 year follow-up of the Finnish twin cohort. Eur Neuropsychopharm. 2019;29(Suppl 3):S804. doi: 10.1016/j.euroneuro.2017.08.043 [DOI] [Google Scholar]
- 14.Dai J, Mukamal KJ, Krasnow RE, Swan GE, Reed T. Higher usual alcohol consumption was associated with a lower 41-y mortality risk from coronary artery disease in men independent of genetic and common environmental factors: the prospective NHLBI Twin Study. Am J Clin Nutr. 2015;102(1):31-39. doi: 10.3945/ajcn.114.106435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bobak M, Malyutina S, Horvat P, et al. Alcohol, drinking pattern and all-cause, cardiovascular and alcohol-related mortality in Eastern Europe. Eur J Epidemiol. 2016;31(1):21-30. doi: 10.1007/s10654-015-0092-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Licaj I, Sandin S, Skeie G, Adami HO, Roswall N, Weiderpass E. Alcohol consumption over time and mortality in the Swedish Women’s Lifestyle and Health cohort. BMJ Open. 2016;6(11):e012862. doi: 10.1136/bmjopen-2016-012862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Almeida OP, McCaul K, Hankey GJ, Yeap BB, Golledge J, Flicker L. Excessive alcohol consumption increases mortality in later life: a genetic analysis of the health in men cohort study. Addict Biol. 2017;22(2):570-578. doi: 10.1111/adb.12340 [DOI] [PubMed] [Google Scholar]
- 18.Luksiene D, Tamosiunas A, Virviciute D, Radisauskas R.. The prognostic value of combined smoking and alcohol consumption habits for the estimation of cause-specific mortality in middle-age and elderly population: results from a long-term cohort study in Lithuania. Biomed Res Int. 2017:9654314. doi: 10.1155/2017/9654314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perreault K, Bauman A, Johnson N, Britton A, Rangul V, Stamatakis E. Does physical activity moderate the association between alcohol drinking and all-cause, cancer and cardiovascular diseases mortality? A pooled analysis of eight British population cohorts. Br J Sports Med. 2017;51(8):651-657. doi: 10.1136/bjsports-2016-096194 [DOI] [PubMed] [Google Scholar]
- 20.Sydén L, Landberg J. The contribution of alcohol use and other lifestyle factors to socioeconomic differences in all-cause mortality in a Swedish cohort. Drug Alcohol Rev. 2017;36(5):691-700. doi: 10.1111/dar.12472 [DOI] [PubMed] [Google Scholar]
- 21.Kunzmann AT, Coleman HG, Huang WY, Berndt SI. The association of lifetime alcohol use with mortality and cancer risk in older adults: a cohort study. PLoS Med. 2018;15(6):e1002585. doi: 10.1371/journal.pmed.1002585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ortolá R, García-Esquinas E, López-García E, León-Muñoz LM, Banegas JR, Rodríguez-Artalejo F. Alcohol consumption and all-cause mortality in older adults in Spain: an analysis accounting for the main methodological issues. Addiction. 2019;114(1):59-68. doi: 10.1111/add.14402 [DOI] [PubMed] [Google Scholar]
- 23.Saito E, Inoue M, Sawada N, et al. Impact of alcohol intake and drinking patterns on mortality from all causes and major causes of death in a Japanese population. J Epidemiol. 2018;28(3):140-148. doi: 10.2188/jea.JE20160200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Keyes KM, Calvo E, Ornstein KA, et al. Alcohol consumption in later life and mortality in the United States: results from 9 waves of the health and retirement study. Alcohol Clin Exp Res. 2019;43(8):1734-1746. doi: 10.1111/acer.14125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rosella LC, Kornas K, Huang A, Grant L, Bornbaum C, Henry D. Population risk and burden of health behavioral-related all-cause, premature, and amenable deaths in Ontario, Canada: Canadian Community Health Survey-linked mortality files. Ann Epidemiol. 2019;32:49-57.e3. doi: 10.1016/j.annepidem.2019.01.009 [DOI] [PubMed] [Google Scholar]
- 26.Daya NR, Rebholz CM, Appel LJ, Selvin E, Lazo M. Alcohol consumption and risk of hospitalizations and mortality in the atherosclerosis risk in communities study. Alcohol Clin Exp Res. 2020;44(8):1646-1657. doi: 10.1111/acer.14393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jankhotkaew J, Bundhamcharoen K, Suphanchaimat R, et al. Associations between alcohol consumption trajectory and deaths due to cancer, cardiovascular diseases and all-cause mortality: a 30-year follow-up cohort study in Thailand. BMJ Open. 2020;10(12):e038198. doi: 10.1136/bmjopen-2020-038198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van de Luitgaarden IAT, Schrieks IC, Kieneker LM, et al. Urinary ethyl glucuronide as measure of alcohol consumption and risk of cardiovascular disease: a population-based cohort study. J Am Heart Assoc. 2020;9(7):e014324. doi: 10.1161/JAHA.119.014324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Armas Rojas NB, Lacey B, Simadibrata DM, et al. Alcohol consumption and cause-specific mortality in Cuba: prospective study of 120 623 adults. EClinicalMedicine. 2021;33:100692. doi: 10.1016/j.eclinm.2020.100692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Di Castelnuovo A, Costanzo S, Bonaccio M, et al. Alcohol intake and total mortality in 142 960 individuals from the MORGAM Project: a population-based study. Addiction. 2022;117(2):312-325. doi: 10.1111/add.15593 [DOI] [PubMed] [Google Scholar]
- 31.Martínez-González MA, Barbería-Latasa M, Pérez de Rojas J, Domínguez Rodriguez LJ, Gea Sánchez A. Alcohol and early mortality (before 65 years) in the ‘Seguimiento Universidad de Navarra’ (SUN) cohort: does any level reduce mortality? Br J Nutr. 2022;127(9):1415-1425. doi: 10.1017/S0007114521002397 [DOI] [PubMed] [Google Scholar]
- 32.Zhang X, Liu Y, Li S, et al. Alcohol consumption and risk of cardiovascular disease, cancer and mortality: a prospective cohort study. Nutr J. 2021;20(1):13. doi: 10.1186/s12937-021-00671-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Turner C. How much alcohol is in a ‘standard drink’? An analysis of 125 studies. Br J Addict. 1990;85(9):1171-1175. doi: 10.1111/j.1360-0443.1990.tb03442.x [DOI] [PubMed] [Google Scholar]
- 34.International Alliance for Responsible Drinking . Drinking guidelines: general population. 2022. Accessed September 10, 2022. https://iard.org/science-resources/detail/drinking-guidelines-general-population/
- 35.Woodward M. Epidemiology Study design and data analysis. Chapman & Hall/CRC; 2000. [Google Scholar]
- 36.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629-634. doi: 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10(1):101-129. doi: 10.2307/3001666 [DOI] [Google Scholar]
- 38.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539-1558. doi: 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 39.Hosmer DW, Lemeshow S. Applied logistic regression. Wiley; 2000. doi: 10.1002/0471722146 [DOI] [Google Scholar]
- 40.Allison P. When can you safely ignore multicollinearity? 2012. Accessed September 10, 2022. https://statisticalhorizons.com/multicollinearity
- 41.Schreiber-Gregory DN. Multicollinearity: what is it, why should we care, and how can it be controlled? Paper presented at: The SAS Global Forum 2017 Conference; 2017; Orlando, Florida: SAS Institute Inc. [Google Scholar]
- 42.Woodward M. Epidemiology study design and data analysis. Chapman & Hall/CRC; 2000. [Google Scholar]
- 43.Normand SLT. Meta-analysis: formulating, evaluating, combining, and reporting. Stat Med. 1999;18(3):321-359. doi: [DOI] [PubMed] [Google Scholar]
- 44.SAS Institute . SAS/STAT 9.4 user’s guide. SAS Institute Inc; 2016. [Google Scholar]
- 45.Bergmann M, Rehm J, Klipstein-Grobusch K, et al. The association of pattern of lifetime alcohol use and cause of death in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Int J Epidemiol. 2013;42(6):1772-1790. doi: 10.1093/ije/dyt154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cullen KJ, Knuiman MW, Ward NJ. Alcohol and Mortality in Busselton, Western-Australia. Am J Epidemiol. 1993;137(2):242-248. doi: 10.1093/oxfordjournals.aje.a116665 [DOI] [PubMed] [Google Scholar]
- 47.Friesema IHM, Zwietering PJ, Veenstra MY, Knottnerus JA, Garretsen HFL, Lemmens PHHM. Alcohol intake and cardiovascular disease and mortality: the role of pre-existing disease. J Epidemiol Community Health. 2007;61(5):441-446. doi: 10.1136/jech.2006.050419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kono S, Ikeda M, Tokudome S, Nishizumi M, Kuratsune M. Alcohol and mortality: a cohort study of male Japanese physicians. Int J Epidemiol. 1986;15(4):527-532. doi: 10.1093/ije/15.4.527 [DOI] [PubMed] [Google Scholar]
- 49.Makela P, Paljarvi T, Poikolainen K. Heavy and nonheavy drinking occasions, all-cause and cardiovascular mortality and hospitalizations: a follow-up study in a population with a low consumption level. J Stud Alcohol. 2005;66(6):722-728. doi: 10.15288/jsa.2005.66.722 [DOI] [PubMed] [Google Scholar]
- 50.Nakaya N, Kurashima K, Yamaguchi J, et al. Alcohol consumption and mortality in Japan: The Miyagi Cohort Study. J Epidemiol. 2004;14:S18-S25. doi: 10.2188/jea.14.S18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pednekar MS, Sansone G, Gupta PC. Association of alcohol, alcohol and tobacco with mortality: findings from a prospective cohort study in Mumbai (Bombay), India. Alcohol. 2012;46(2):139-146. doi: 10.1016/j.alcohol.2011.08.006 [DOI] [PubMed] [Google Scholar]
- 52.Sadakane A, Gotoh T, Ishikawa S, et al. Amount and frequency of alcohol consumption and all-cause mortality in a Japanese population: the JMS cohort study. J Epidemiol. 2009;19(3):107-115. doi: 10.2188/jea.JE20081003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sempos CT, Rehm A, Wu TJ, Crespo CJ, Trevisan M. Average volume of alcohol consumption and all-cause mortality in African Americans: the NHEFS cohort. Alcohol Clin Exp Res. 2003;27(1):88-92. doi: 10.1111/j.1530-0277.2003.tb02726.x [DOI] [PubMed] [Google Scholar]
- 54.Sun WJ, Schooling CM, Chan WM, Ho KS, Lam TH, Leung GM. Moderate alcohol use, health status, and mortality in a prospective Chinese elderly cohort. Ann Epidemiol. 2009;19(6):396-403. doi: 10.1016/j.annepidem.2009.01.011 [DOI] [PubMed] [Google Scholar]
- 55.Thun MJ, Peto R, Lopez AD, et al. Alcohol consumption and mortality among middle-aged and elderly US adults. N Engl J Med. 1997;337(24):1705-1714. doi: 10.1056/NEJM199712113372401 [DOI] [PubMed] [Google Scholar]
- 56.Tsubono Y, Fukao A, Hisamichi S. Health practices and mortality in a rural Japanese population. Tohoku J Exp Med. 1993;171(4):339-348. doi: 10.1620/tjem.171.339 [DOI] [PubMed] [Google Scholar]
- 57.Zaridze D, Lewington S, Boroda A, et al. Alcohol and mortality in Russia: prospective observational study of 151 000 adults. Lancet. 2014;383(9927):1465-1473. doi: 10.1016/S0140-6736(13)62247-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rehm J, Greenfield TK, Rogers JD. Average volume of alcohol consumption, patterns of drinking, and all-cause mortality: results from the US national alcohol survey. Am J Epidemiol. 2001;153(1):64-71. doi: 10.1093/aje/153.1.64 [DOI] [PubMed] [Google Scholar]
- 59.Rehm J, Fichter MM, Elton M. Effects on mortality of alcohol-consumption, smoking, physical-activity, and close personal relationships. Addiction. 1993;88(1):101-112. doi: 10.1111/j.1360-0443.1993.tb02767.x [DOI] [PubMed] [Google Scholar]
- 60.Abramson JL, Williams SA, Krumholz HM, Vaccarino V. Moderate alcohol consumption and risk of heart failure among older persons. JAMA. 2001;285(15):1971-1977. doi: 10.1001/jama.285.15.1971 [DOI] [PubMed] [Google Scholar]
- 61.Boffetta P, Garfinkel L. Alcohol drinking and mortality among men enrolled in an American Cancer Society prospective study. Am J Epidemiol. 1990;132(4):797. doi: 10.1097/00001648-199009000-00003 [DOI] [PubMed] [Google Scholar]
- 62.Camacho TC, Kaplan GA, Cohen RD. Alcohol-consumption and mortality in Alameda County. J Chronic Dis. 1987;40(3):229-236. doi: 10.1016/0021-9681(87)90158-5 [DOI] [PubMed] [Google Scholar]
- 63.Delabry LO, Glynn RJ, Levenson MR, Hermos JA, Locastro JS, Vokonas PS. Alcohol-consumption and mortality in an american male-population: recovering the u-shaped curve—findings from the Normative Aging Study. J Stud Alcohol. 1992;53(1):25-32. doi: 10.15288/jsa.1992.53.25 [DOI] [PubMed] [Google Scholar]
- 64.Friedman LA, Kimball AW. Coronary heart-disease mortality and alcohol-consumption in Framingham. Am J Epidemiol. 1986;124(3):481-489. doi: 10.1093/oxfordjournals.aje.a114418 [DOI] [PubMed] [Google Scholar]
- 65.Garfinkel L, Boffetta P, Stellman SD. Alcohol and breast-cancer: a cohort study. Prev Med. 1988;17(6):686-693. doi: 10.1016/0091-7435(88)90086-2 [DOI] [PubMed] [Google Scholar]
- 66.Gordon T, Doyle JT. Drinking and mortality: the Albany Study. Am J Epidemiol. 1987;125(2):263-270. doi: 10.1093/oxfordjournals.aje.a114525 [DOI] [PubMed] [Google Scholar]
- 67.Gronbaek M, Becker U, Johansen D, et al. Type of alcohol consumed and mortality from all causes, coronary heart disease, and cancer. Ann Intern Med. 2000;133(6):411-419. doi: 10.7326/0003-4819-133-6-200009190-00008 [DOI] [PubMed] [Google Scholar]
- 68.Gun RT, Pratt N, Ryan P, Gordon I, Roder D. Tobacco and alcohol-related mortality in men: estimates from the Australian cohort of petroleum industry workers. Aust N Z J Public Health. 2006;30(4):318-324. doi: 10.1111/j.1467-842X.2006.tb00842.x [DOI] [PubMed] [Google Scholar]
- 69.Hart CL, Smith GD. Alcohol consumption and mortality and hospital admissions in men from the Midspan Collaborative cohort study. Addiction. 2008;103(12):1979-1986. doi: 10.1111/j.1360-0443.2008.02373.x [DOI] [PubMed] [Google Scholar]
- 70.Hoffmeister H, Schelp FP, Mensink GBM, Dietz E, Bohning D. The relationship between alcohol consumption, health indicators and mortality in the German population. Int J Epidemiol. 1999;28(6):1066-1072. doi: 10.1093/ije/28.6.1066 [DOI] [PubMed] [Google Scholar]
- 71.Holahan CJ, Schutte KK, Brennan PL, Holahan CK, Moos BS, Moos RH. Late-life alcohol consumption and 20-year mortality. Alcohol Clin Exp Res. 2010;34(11):1961-1971. doi: 10.1111/j.1530-0277.2010.01286.x [DOI] [PubMed] [Google Scholar]
- 72.Howie EK, Sui X, Lee DC, Hooker SP, Hebert JR, Blair SN. Alcohol consumption and risk of all-cause and cardiovascular disease mortality in men. J Aging Res. 2011;2011:805062. doi: 10.4061/2011/805062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Iversen L, Hannaford PC, Lee AJ, Elliott AM, Fielding S. Impact of lifestyle in middle-aged women on mortality: evidence from the Royal College of General Practitioners’ Oral Contraception Study. Br J Gen Pract. 2010;60(577):563-569. doi: 10.3399/bjgp10X515052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jakovljevic B, Stojanov V, Paunovic K, Belojevic G, Milic N. Alcohol consumption and mortality in Serbia: twenty-year follow-up study. Croat Med J. 2004;45(6):764-768. [PubMed] [Google Scholar]
- 75.Key TJ, Appleby PN, Spencer EA, Travis RC, Roddam AW, Allen NE. Mortality in British vegetarians: results from the European Prospective Investigation into Cancer and Nutrition (EPIC-Oxford). Am J Clin Nutr. 2009;89(5):S1613-S9. doi: 10.3945/ajcn.2009.26736L [DOI] [PubMed] [Google Scholar]
- 76.Kivela SL, Nissinen A, Punsar S, Puska P, Karvonen MJ. Changes in alcohol-consumption and mortality in aged Finnish men. Ann Med. 1989;21(3):245-246. doi: 10.3109/07853898909149945 [DOI] [PubMed] [Google Scholar]
- 77.Kvaavik E, Batty GD, Ursin G, Huxley R, Gale CR. Influence of individual and combined health behaviors on total and cause-specific mortality in men and women the United Kingdom Health and Lifestyle Survey. Arch Intern Med. 2010;170(8):711. doi: 10.1001/archinternmed.2010.76 [DOI] [PubMed] [Google Scholar]
- 78.Lantz PM, Golberstein E, House JS, Morenoff J. Socioeconomic and behavioral risk factors for mortality in a national 19-year prospective study of US adults. Soc Sci Med. 2010;70(10):1558-1566. doi: 10.1016/j.socscimed.2010.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Marmot MG, Rose G, Shipley MJ. Alcohol and mortality in British civil-servants. J Epidemiol Community Health. 1981;35(2):152. [Google Scholar]
- 80.Marugame T, Yamamoto S, Yoshimi I, Sobue T, Inoue M, Tsugane S. Patterns of alcohol drinking and all-cause mortality: results from a large-scale population-based cohort study in Japan. Am J Epidemiol. 2007;165(9):1039-1046. doi: 10.1093/aje/kwk112 [DOI] [PubMed] [Google Scholar]
- 81.Maskarinec G, Meng LX, Kolonel LN. Alcohol intake, body weight, and mortality in a multiethnic prospective cohort. Epidemiology. 1998;9(6):654-661. doi: 10.1097/00001648-199811000-00016 [DOI] [PubMed] [Google Scholar]
- 82.Mertens JR, Moos RH, Brennan PL. Alcohol consumption, life context, and coping predict mortality among late-middle-aged drinkers and former drinkers. Alcohol Clin Exp Res. 1996;20(2):313-319. doi: 10.1111/j.1530-0277.1996.tb01645.x [DOI] [PubMed] [Google Scholar]
- 83.Miller GJ, Beckles GLA, Maude GH, Carson DC. Alcohol-consumption: protection against coronary heart-disease and risks to health. Int J Epidemiol. 1990;19(4):923-930. doi: 10.1093/ije/19.4.923 [DOI] [PubMed] [Google Scholar]
- 84.Onat A, Hergenc G, Küçükdurmaz Z, et al. Moderate and heavy alcohol consumption among Turks: long-term impact on mortality and cardiometabolic risk. Türk Kardiyol Dern Arş. 2009;37(2):8. [PubMed] [Google Scholar]
- 85.Paganini-Hill A, Kawas CH, Corrada MM. Type of alcohol consumed, changes in intake over time and mortality: the Leisure World Cohort Study. Age Ageing. 2007;36(2):203-209. doi: 10.1093/ageing/afl184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Paunio M, Heinonen OP, Virtamo J, et al. HDL cholesterol and mortality in Finnish men with special reference to alcohol intake. Circulation. 1994;90(6):2909-2918. doi: 10.1161/01.CIR.90.6.2909 [DOI] [PubMed] [Google Scholar]
- 87.Pedersen JO, Heitmann BL, Schnohr P, Gronbaek M. The combined influence of leisure-time physical activity and weekly alcohol intake on fatal ischaemic heart disease and all-cause mortality. Eur Heart J. 2008;29(2):204-212. doi: 10.1093/eurheartj/ehm574 [DOI] [PubMed] [Google Scholar]
- 88.Romelsjo A, Allebeck P, Andreasson S, Leifman A. Alcohol, mortality and cardiovascular events in a 35 year follow-up of a nationwide representative cohort of 50,000 Swedish conscripts up to age 55. Alcohol Alcohol. 2012;47(3):322-327. doi: 10.1093/alcalc/ags021 [DOI] [PubMed] [Google Scholar]
- 89.Shaw BA, Agahi N. A prospective cohort study of health behavior profiles after age 50 and mortality risk. BMC Public Health. 2012;12:803. doi: 10.1186/1471-2458-12-803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Shuval K, Barlow CE, Chartier KG, Gabriel KP. Cardiorespiratory fitness, alcohol, and mortality in men: the Cooper Center Longitudinal Study. Am J Prev Med. 2012;42(5):460-467. doi: 10.1016/j.amepre.2012.01.012 [DOI] [PubMed] [Google Scholar]
- 91.Simons LA, McCallum J, Friedlander Y, Ortiz M, Simons J. Moderate alcohol intake is associated with survival in the elderly: the Dubbo Study. Med J Aust. 2000;173(3):121-124. doi: 10.5694/j.1326-5377.2000.tb125562.x [DOI] [PubMed] [Google Scholar]
- 92.Strandberg AY, Strandberg TE, Salomaa VV, Pitkala K, Miettinen TA. Alcohol consumption, 29-y total mortality, and quality of life in men in old age (1-3). Am J Clin Nutr. 2004;80(5):1366-1371. doi: 10.1093/ajcn/80.5.1366 [DOI] [PubMed] [Google Scholar]
- 93.Streppel MT, Ocke MC, Boshuizen HC, Kok FJ, Kromhout D. Long-term wine consumption is related to cardiovascular mortality and life expectancy independently of moderate alcohol intake: the Zutphen Study. J Epidemiol Community Health. 2009;63(7):534-540. doi: 10.1136/jech.2008.082198 [DOI] [PubMed] [Google Scholar]
- 94.Theobald H, Johansson SE, Bygren LO, Engfeldt P. The effects of alcohol consumption on mortality and morbidity: a 26-year follow-up study. J Stud Alcohol. 2001;62(6):783-789. doi: 10.15288/jsa.2001.62.783 [DOI] [PubMed] [Google Scholar]
- 95.Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):2599-2608. doi: 10.1056/NEJMoa025039 [DOI] [PubMed] [Google Scholar]
- 96.Wellmann J, Heidrich J, Berger K, Doring A, Heuschmann PU, Keil U. Changes in alcohol intake and risk of coronary heart disease and all-cause mortality in the MONICA/KORA-Augsburg cohort 1987-97. Eur J Cardiovasc Prev Rehabil. 2004;11(1):48-55. doi: 10.1097/01.hjr.0000118174.70522.20 [DOI] [PubMed] [Google Scholar]
- 97.Yang L, Zhou MG, Sherliker P, et al. Alcohol drinking and overall and cause-specific mortality in China: nationally representative prospective study of 220 000 men with 15 years of follow-up. Int J Epidemiol. 2012;41(4):1101-1113. doi: 10.1093/ije/dys075 [DOI] [PubMed] [Google Scholar]
- 98.Zureik M, Ducimetiere P. High alcohol-related premature mortality in France: concordant estimates from a prospective cohort study and national mortality statistics. Alcohol Clin Exp Res. 1996;20(3):428-433. doi: 10.1111/j.1530-0277.1996.tb01070.x [DOI] [PubMed] [Google Scholar]
- 99.Rundberg J, Nilsson PM, Samsioe G, Ojehagen A. Alcohol use and early mortality in Swedish middle-aged women: nine-year follow-up of the Women’s Health in Lund Area study. Scand J Public Health. 2014;42(4):344-348. doi: 10.1177/1403494814523343 [DOI] [PubMed] [Google Scholar]
- 100.Andreasson S, Brandt L. Mortality and morbidity related to alcohol. Alcohol Alcohol. 1997;32(2):173-178. doi: 10.1093/oxfordjournals.alcalc.a008251 [DOI] [PubMed] [Google Scholar]
- 101.Arndt V, Rothenbacher D, Krauledat R, Daniel U, Brenner H. Age, alcohol consumption, and all-cause mortality. Ann Epidemiol. 2004;14(10):750-753. doi: 10.1016/j.annepidem.2004.01.004 [DOI] [PubMed] [Google Scholar]
- 102.Behrens G, Leitzmann MF, Sandin S, et al. The association between alcohol consumption and mortality: the Swedish women’s lifestyle and health study. Eur J Epidemiol. 2011;26(2):81-90. doi: 10.1007/s10654-011-9545-x [DOI] [PubMed] [Google Scholar]
- 103.Brenner H, Arndt V, Rothenbacher D, Schuberth S, Fraisse E, Fliedner TM. The association between alcohol consumption and all-cause mortality in a cohort of male employees in the German construction industry. Int J Epidemiol. 1997;26(1):85-91. doi: 10.1093/ije/26.1.85 [DOI] [PubMed] [Google Scholar]
- 104.Britton A, Marmot M. Different measures of alcohol consumption and risk of coronary heart disease and all-cause mortality: 11-year follow-up of the Whitehall II Cohort Study. Addiction. 2004;99(1):109-116. doi: 10.1111/j.1360-0443.2004.00530.x [DOI] [PubMed] [Google Scholar]
- 105.Carmelli D, Swan GE, Page WF, Christian JC. World-War-II veteran male twins who are discordant for alcohol-consumption: 24-year mortality. Am J Public Health. 1995;85(1):99-101. doi: 10.2105/AJPH.85.1.99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Colditz GA, Branch LG, Lipnick RJ, et al. Moderate alcohol and decreased cardiovascular mortality in an elderly cohort. Am Heart J. 1985;109(4):886-889. doi: 10.1016/0002-8703(85)90654-4 [DOI] [PubMed] [Google Scholar]
- 107.Deev A, Shestov D, Abernathy J, Kapustina A, Muhina N, Irving S. Association of alcohol consumption to mortality in middle-aged US and Russian men and women. Ann Epidemiol. 1998;8(3):147-153. doi: 10.1016/S1047-2797(98)00004-0 [DOI] [PubMed] [Google Scholar]
- 108.Djousse L, Lee IM, Buring JE, Gaziano JM. Alcohol consumption and risk of cardiovascular disease and death in women potential mediating mechanisms. Circulation. 2009;120(3):237-244. doi: 10.1161/CIRCULATIONAHA.108.832360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to alcohol consumption: a prospective study among male British doctors. Int J Epidemiol. 2005;34(1):199-204. doi: 10.1093/ije/dyh369 [DOI] [PubMed] [Google Scholar]
- 110.Dyer AR, Stamler J, Paul O, et al. Alcohol, cardiovascular risk-factors and mortality: the Chicago experience. Circulation. 1981;64(3):20-27. [PubMed] [Google Scholar]
- 111.Emberson JR, Shaper AG, Wannamethee SG, Morris RW, Whincup PH. Alcohol intake in middle age and risk of cardiovascular disease and mortality: accounting for intake variation over time. Am J Epidemiol. 2005;161(9):856-863. doi: 10.1093/aje/kwi111 [DOI] [PubMed] [Google Scholar]
- 112.Fuchs CS, Stampfer MJ, Colditz GA, et al. Alcohol-consumption and mortality among women. N Engl J Med. 1995;332(19):1245-1250. doi: 10.1056/NEJM199505113321901 [DOI] [PubMed] [Google Scholar]
- 113.Goldberg RJ, Burchfiel CM, Reed DM, Wergowske G, Chiu D. A prospective-study of the health-effects of alcohol-consumption in middle-aged and elderly men: the Honolulu-heart-program. Circulation. 1994;89(2):651-659. doi: 10.1161/01.CIR.89.2.651 [DOI] [PubMed] [Google Scholar]
- 114.Leino EV, Romelsjo A, Shoemaker C, et al. Alcohol consumption and mortality. II. Studies of male populations. Addiction. 1998;93(2):205-218. doi: 10.1046/j.1360-0443.1998.9322055.x [DOI] [PubMed] [Google Scholar]
- 115.Malyutina S, Bobak M, Kurilovitch S, et al. Relation between heavy and binge drinking and all-cause and cardiovascular mortality in Novosibirsk, Russia: a prospective cohort study. Lancet. 2002;360(9344):1448-1454. doi: 10.1016/S0140-6736(02)11470-X [DOI] [PubMed] [Google Scholar]
- 116.San Jose B, van de Mheen H, van Oers JA, Mackenbach JP, Garretsen HF. The U-shaped curve: various health measures and alcohol drinking patterns. J Stud Alcohol. 1999;60(6):725-731. doi: 10.15288/jsa.1999.60.725 [DOI] [PubMed] [Google Scholar]
- 117.Scherr PA, Lacroix AZ, Wallace RB, et al. Light to moderate alcohol-consumption and mortality in the elderly. J Am Geriatr Soc. 1992;40(7):651-657. doi: 10.1111/j.1532-5415.1992.tb01954.x [DOI] [PubMed] [Google Scholar]
- 118.Serdula MK, Koong SL, Williamson DF, et al. Alcohol intake and subsequent mortality: findings from the NHANES I Follow-up Study. J Stud Alcohol. 1995;56(2):233-239. doi: 10.15288/jsa.1995.56.233 [DOI] [PubMed] [Google Scholar]
- 119.Suhonen O, Aromaa A, Reunanen A, Knekt P. Alcohol-consumption and sudden coronary death in middle-aged Finnish men. Acta Med Scand. 1987;221(4):335-341. doi: 10.1111/j.0954-6820.1987.tb03353.x [DOI] [PubMed] [Google Scholar]
- 120.Thorpe RJ Jr, Wilson-Frederick SM, Bowie JV, et al. Health behaviors and all-cause mortality in African American men. Am J Men Health. 2013;7(4)(suppl):8S-18S. doi: 10.1177/1557988313487552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Soedamah-Muthu SS, De Neve M, Shelton NJ, Tielemans SMAJ, Stamatakis E. Joint associations of alcohol consumption and physical activity with all-cause and cardiovascular mortality. Am J Cardiol. 2013;112(3):380-386. doi: 10.1016/j.amjcard.2013.03.040 [DOI] [PubMed] [Google Scholar]
- 122.Klatsky AL, Friedman GD, Siegelaub AB. Alcohol and mortality: a 10-Year Kaiser-Permanente experience. Ann Intern Med. 1981;95(2):139-145. doi: 10.7326/0003-4819-95-2-139 [DOI] [PubMed] [Google Scholar]
- 123.Freiberg MS, Chang YF, Kraemer KL, Robinson JG, Adams-Campbell LL, Kuller LL. Alcohol consumption, hypertension, and total mortality among women. Am J Hypertens. 2009;22(11):1212-1218. doi: 10.1038/ajh.2009.172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Liao YL, McGee DL, Cao GC, Cooper RS. Alcohol intake and mortality: findings from the National Health Interview Surveys (1988 and 1990). Am J Epidemiol. 2000;151(7):651-659. doi: 10.1093/oxfordjournals.aje.a010259 [DOI] [PubMed] [Google Scholar]
- 125.Lin YS, Kikuchi S, Tamakoshi A, et al. Alcohol consumption and mortality among middle-aged and elderly Japanese men and women. Ann Epidemiol. 2005;15(8):590-597. doi: 10.1016/j.annepidem.2004.10.010 [DOI] [PubMed] [Google Scholar]
- 126.Maraldi C, Volpato S, Kritchevsky SB, et al. Impact of inflammation on the relationship among alcohol consumption, mortality, and cardiac events: the health, aging, and body composition study. Arch Intern Med. 2006;166(14):1490-1497. doi: 10.1001/archinte.166.14.1490 [DOI] [PubMed] [Google Scholar]
- 127.Rostron B. Alcohol consumption and mortality risks in the USA. Alcohol Alcohol. 2012;47(3):334-339. doi: 10.1093/alcalc/agr171 [DOI] [PubMed] [Google Scholar]
- 128.Yuan JM, Ross RK, Gao YT, Henderson BE, Yu MC. Follow up study of moderate alcohol intake and mortality among middle aged men in Shanghai, China. BMJ. 1997;314(7073):18-23. doi: 10.1136/bmj.314.7073.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Klatsky AL, Armstrong MA, Friedman GD. Risk of cardiovascular mortality in alcohol drinkers, ex-drinkers and nondrinkers. Am J Cardiol. 1990;66(17):1237-1242. doi: 10.1016/0002-9149(90)91107-H [DOI] [PubMed] [Google Scholar]
- 130.Berberian KM, Vanduijn CM, Hoes AW, Valkenburg HA, Hofman A. Alcohol and mortality: results from the Epoz Follow-up-Study. Eur J Epidemiol. 1994;10(5):587-593. doi: 10.1007/BF01719577 [DOI] [PubMed] [Google Scholar]
- 131.Baglietto L, English DR, Hopper JL, Powles J, Giles GG. Average volume of alcohol consumed, type of beverage, drinking pattern and the risk of death from all causes. Alcohol Alcohol. 2006;41(6):664-671. doi: 10.1093/alcalc/agl087 [DOI] [PubMed] [Google Scholar]
- 132.WHO . The global health observatory: Explore a world of health data. 2022. Accessed October 28, 2022. https://www.who.int/data/gho/indicator-metadata-registry/imr-details/460
- 133.Stockwell T, Zhao J, Sherk A, Rehm J, Shield K, Naimi T. Underestimation of alcohol consumption in cohort studies and implications for alcohol’s contribution to the global burden of disease. Addiction. 2018;113(12):2245-2249. doi: 10.1111/add.14392 [DOI] [PubMed] [Google Scholar]
- 134.Stockwell T, Zhao J, Macdonald S. Who under-reports their alcohol consumption in telephone surveys and by how much? An application of the ‘yesterday method’ in a national Canadian substance use survey. Addiction. 2014;109(10):1657-1666. doi: 10.1111/add.12609 [DOI] [PubMed] [Google Scholar]
- 135.Kerr WC, Fillmore KM, Bostrom A. Stability of alcohol consumption over time: evidence from three longitudinal surveys from the United States. J Stud Alcohol. 2002;63(3):325-333. doi: 10.15288/jsa.2002.63.325 [DOI] [PubMed] [Google Scholar]
- 136.Shaper AG, Wannamethee G, Walker M. Alcohol and mortality in British men: explaining the U-shaped curve. Lancet. 1988;2(8623):1267-1273. doi: 10.1016/S0140-6736(88)92890-5 [DOI] [PubMed] [Google Scholar]
- 137.Justice AC, McGinnis KA, Tate JP, et al. Risk of mortality and physiologic injury evident with lower alcohol exposure among HIV infected compared with uninfected men. Drug Alcohol Depend. 2016;161:95-103. doi: 10.1016/j.drugalcdep.2016.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Austin PC, Steyerberg EW. The number of subjects per variable required in linear regression analyses. J Clin Epidemiol. 2015;68(6):627-636. doi: 10.1016/j.jclinepi.2014.12.014 [DOI] [PubMed] [Google Scholar]
- 139.Roerecke M, Rehm J. Irregular heavy drinking occasions and risk of ischemic heart disease: a systematic review and meta-analysis. Am J Epidemiol. 2010;171(6):633-644. doi: 10.1093/aje/kwp451 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Methodology of Meta-analysis on All-Cause Mortality and Alcohol Consumption
eReferences
eFigure 1. Flowchart of Systematic Search Process for Studies of Alcohol Consumption and Risk of All-Cause Mortality
eTable 1. Newly Included 20 Studies (194 Risk Estimates) of All-Cause Mortality and Consumption in 2015 to 2022
eFigure 2. Funnel Plot of Log-Relative Risk (In(RR)) of All-Cause Mortality Due to Alcohol Consumption Against Inverse of Standard Error of In(RR)
eFigure 3. Relative Risk (95% CI) of All-Cause Mortality Due to Any Alcohol Consumption Without Any Adjustment for Characteristics of New Studies Published between 2015 and 2022
eFigure 4. Unadjusted, Partially Adjusted, and Fully Adjusted Relative Risk (RR) of All-Cause Mortality for Drinkers (vs Nondrinkers), 1980 to 2022
eTable 2. Statistical Analysis of Unadjusted Mean Relative Risk (RR) of All-Cause Mortality for Different Categories of Drinkers for Testing Publication Bias and Heterogeneity of RR Estimates From Included Studies
eTable 3. Mean Relative Risk (RR) Estimates of All-Cause Mortality Due to Alcohol Consumption up to 2022 for Subgroups (Cohorts Recruited 50 Years of Age or Younger and Followed up to 60 Years of Age)
Data Sharing Statement