Abstract
Background
Sleep problems mark an important part of the research into the physical health and mental well-being of modern societies. Although there are many studies on restless sleep, they are dominated by approaches that either focus on health-related issues or social factors (such as socioeconomic status). In this report, we address both types of determinants. This study replicates the analysis for the UK that was carried out by Arber et al. (Gender and socio-economic patterning of self-reported sleep problems in Britain. Soc Sci Med 2009;68:281–9). However, this replication, based on European Social Survey data, covers 20 European countries.
Methods
Data are taken from the European Social Survey Round 7 from 2014 (N = 32 704). A multilevel logistic regression was used to assess the impact of sociodemographic, socioeconomic and health-related issues on reported restless sleeping.
Results
The results show that the influence of socioeconomic status has a secondary effect on sleep problems, health-related problems and depression. In addition, the study shows that individual-level, rather than country-level, factors have a major impact on restless sleep.
Conclusions
We have replicated all the findings of Arber et al. (Gender and socio-economic patterning of self-reported sleep problems in Britain. Soc Sci Med 2009;68:281–9) and confirmed the secondary nature of socioeconomic status factors to health and depression based on 20 European countries.
Introduction
Sleep problems are a serious sociomedical issue because up to 67% of adults worldwide report sleep disturbances at least once every night.1 More importantly, these problems translate into (and in some cases are a consequence of) both physical and mental well-being2,3 and a wide range of negative health complaints.4,5 The COVID-19 pandemic has exacerbated this situation, as confirmed by numerous studies.6–9
Given the momentousness of the consequences of sleep problems on mental health and well-being, which translate into general quality of life, researchers have used various data to describe and explain the diverse phenomena accompanying different degrees of sleep disorders. Some have used specialized (sub)national data,10–12 while others have utilized cross-national sources.13–15
Referring to the latter studies, we aim to apply an extended replication of Arber et al.’s16 analysis, which was based solely on data from one country (the UK); however, our studies do so on cross-national pan-European data by utilizing the European Social Survey results from Round 7/2014. We focus on exploring differences in reporting sleep problems in European countries by considering the sociodemographic and socioeconomic patterns of restless sleeping. Unlike studies that concentrate on a particular age category, gender or occupational group,13,17,18 our approach covers all individuals aged 16–74. Furthermore, although some researchers have focused on the impact of socioeconomic status on sleep problems (e.g. reference 15) we check whether the effect of socioeconomic status is moderated by sociodemographic factors and health-related issues (i.e. smoking, alcohol consumption, depression symptoms, self-related health and the occurrence of chronic illnesses). Although our analyses replicated all previous results presented by reference 16, we additionally demonstrated that respondents’ determinants of restless sleep have not changed over the years and are stable across European countries.
Methods
European Social Survey, wave 7 (2014)
The current article analyses the European Social Survey data wave 7/2014 (focused on health issues). Interviews were conducted face to face with 40 185 individuals aged 15 years and older living in private households within country borders, irrespective of nationality, citizenship, language or legal status. The ESS Round 7 data were taken from the ESS Data Portal https://ess-search.nsd.no/ and covered 21 European countries (including Israel). We excluded 2051 respondents from Estonia because the income question used in the country questionnaire did not follow the ESS requirements [note that income is one of the indicators of socioeconomic status (SES, hereafter) in our analysis]. Additionally, because we replicated the study by reference 16, we restricted our analyses to the population aged 16–74. In total, we worked on data covering 20 countries and 34 156 individuals before we finally excluded cases with missing data on any dependent and explanatory variables (see section Missing data).
Measures
Please consult Supplementary Appendix A to compare the measures implemented by reference 16 and those we obtained from the ESS data; note that whenever possible, we defined dependent and explanatory variables in the same way as in the 2009 study.
Sleep problems—dependent variable
Sleep problems were measured in the ESS as a part of the Center for Epidemiological Studies Depression Scale (CES-D), which was introduced and designed for inclusion in surveys in the 1970s to measure the frequency of depressive symptoms in the general population.19 The ESS project implemented a shortened version of CES-D based on six items; one of the items measured problems with sleeping, and we extracted this item for defining the dependent variable. The interviewers asked how much of the time during the past week the respondent’s sleep was restless. The response options were as follows: (i) None or almost none of the time; (ii) Some of the time; (iii) Most of the time; (iv) All or almost all of the time; and (v) Do not know. We analyzed a dichotomous variable of respondents reporting restless sleeping on ‘Most of the time’ or ‘All or almost all of the time’ as an indicator of frequently experienced sleep difficulties. We excluded those who indicated ‘Do not know’ because the option is an item-nonresponse case (for the information about missing data, see section Missing data).
Sociodemographic characteristics
We included four sociodemographic variables: sex, age groups (16–24, 25–34, 35–44, 45–54, 55–64, 65–74), marital status (Married/cohabiting, Never married, Widowed, Divorced/separated) and the number of children. As a subsample for analysis including respondents from 16 to 74 years old, we defined children as those up to 15 years old. The variable number of children had the following values: none, 1, 2 and 3 or more.
Socioeconomic characteristics
We included three out of four variables of socioeconomic status (SES) implemented in the analyses by Arber et al.,16 that is, level of education, employment status and household (HH) income (ESS does not contain data on housing tenure, and we could not incorporate this into the analysis.).
Because the ESS is a cross-national comparative survey, its measures are designed to be comparable across different nations, regardless of the country’s circumstances. For example, the level of education is measured by implementing the International Standard Classification of Education (ES-ISCED), and HH income is measured by considering differences in the net values of HH’s income. We created the variable level of education with values as follows: (i) ISCED IV-VI, (ii) ISCED III, (iii) ISCED II and (iv) ISCED I, and we created HH income by recoding 10 deciles (response options correspond to the deciles of HH’s income distribution in each country, separately) into 5 quintiles (to have the same number of income categories as Arber et al.16) Moreover, because the variable measuring household income had the highest item-nonresponse rates among all ESS items (totaling as high as 40.7% in Hungary), we decided not to exclude respondents who refused to answer or indicated they ‘Do not know’ what their HH income is, including them as an additional category of HH income in the analyses. Finally, employment status was coded in the ESS by asking respondents about their main activity during the past 7 days and was recoded as follows: (i) Full-time employed, (ii) Unemployed and (iii) Economically inactive.
Measures of other variables
Smoking was measured by asking the respondents which of the descriptions best described their smoking behaviors, with five response options: (i) I smoke daily, (ii) I smoke but not every day, (iii) I do not smoke now, but I used to, (iv) I have only smoked a few times and (v) I have never smoked. We categorized these options as Never smoked [by merging (iv) and (v)], Ex-smoker (iii) and Current smoker [merging (i) and (ii)].
Alcohol consumption was obtained from the question on how often a respondent had a drink containing alcohol in the past year, with seven response options that we merged and labeled as follows: Never, Monthly (‘Less than once a month’ or ‘Once a month’), Two to four times a month (‘Two to three times a month’ or ‘Once a week’), Two to three times a week (‘Several times a week’) and Four or more times a week (‘Every day’).
We derived data about depression symptoms from the shortened version of the 6-item CES-D scale (see section 1.2.1). Because we extracted one of the items (restless sleeping) when defining the dependent variable, for the rest of the five questions measuring depression symptoms [how much of the time during the past week respondents felt: (i) depressed; (ii) that everything they did was an effort; (iii) lonely; (iv) sad; and (v) could not get going], we receded original response options to have the dichotomous scores 0 or 1 (‘Most of the time’ or ‘All or most of the time’). We summed the score for each respondent and defined three levels of depression symptoms: none, medium (one symptom reported) and high (two or more symptoms reported).
Self-rated health was measured by asking the respondents how their health was in general. We recoded five response options into three categories: Very good, Good and Poor. The latter category merged three original response options from the ESS questionnaire (Fair, Bad and Very bad).
Finally, the number of chronic illnesses was measured by asking which of the health problems (the interviewers presented a list of 11 issues) the respondents had or had experienced in the past 12 months. We summed the number of chronic illnesses indicated for each respondent and recoded them as follows: none, 1, 2 and 3 or more.
Missing data
Note that in each of the questions we described, the interviewer could indicate whether the respondent provided a ‘Do not know’ answer or refused to answer (both options were not explicitly offered to the respondents). For each variable, we treated both options as missing values, with the exception of HH income, as previously mentioned. It is worth noting that the dependent variable and all explanatory variables reached a maximum of 1.5% of missing responses for employment status; hence, we decided to use complete case analysis. We excluded 1452 cases with missing values for any of the variables.
Analytical approach
Our dependent variable (hereafter ) had two outcomes such that is a probability of reporting restless sleeping by respondent in country , and is a probability of not reporting restless sleeping. Note that the cumulative probability of each possible outcome was equal to 1. We used a logit link function, where the logit coefficient is the log of the odds of the event as opposed to .
Our final multilevel mixed model for respondents nested within countries is as follows: where is the grand intercept and for represents the coefficients for all explanatory variables.
We start with the null model (which excludes all explanatory variables from the regression), allowing us to estimate the variance components (i.e. intraclass correlation coefficient, hereafter ICC) attributed to the country level. Note that the level-1 residual variance in the logistic regression was scaled to 1.0 and could not be tested for statistical significance. Nevertheless, the variance of the logistic distribution with a scale factor of 1.0 was approximately equal to 3.29, or more precisely (see reference 20) and the ICC attributed to the countries could be expressed as follows: .
All analyses were performed in the R Project for Statistical Computing21 with the packages for data analyses and visualization listed in Supplementary Appendix.
Results
Table 1 demonstrates the estimated proportion of the population aged 16–74 reporting restless sleeping in European countries, here broken down into females and males. The highest fraction of the population having sleep problems, reaching at least 20%, can be observed in Portugal (22.1%), France (21.6%), Belgium (20.3%), and the UK (20.2%). In comparison, the countries with the lowest fractions are Finland (10.5%), Austria (11.0%) and Ireland (11.0%), respectively. In all analyzed countries, more women than men reported restless sleeping ‘Most of the time’ or ‘Almost all of the time’ during the week. The highest differences between gender categories, reaching at least 10 percentage points, were in Belgium (26% of females, compared with 14.3% of males) and Spain (23.5% of females, compared with 12.9% of males), while the lowest was in Austria (11.8% females and 10.3% males, respectively). For each country, we verified whether the proportions of the respondents declaring sleep problems were equal in two gender categories (see P-values in table 1), and the results confirmed that the differences were statistically significant for 19 out of 20 countries (except for Austria).
Table 1.
Characteristics of the ESS-2017 data and fraction of respondents reporting restless sleeping (age 16–74) by gender and country
| Country | Sample size | Subsample size (age 16–74) | Total (%) | Men (%) | Women (%) | P-value |
|---|---|---|---|---|---|---|
| Austria | 1795 | 1617 | 11.0 | 10.3 | 11.8 | n.s. |
| Belgium | 1769 | 1602 | 20.3 | 14.3 | 26.0 | *** |
| Czechia | 2148 | 2047 | 16.5 | 13.6 | 19.4 | *** |
| Denmark | 1502 | 1357 | 16.6 | 14.2 | 18.9 | *** |
| Finland | 2087 | 1838 | 10.5 | 8.4 | 12.6 | *** |
| France | 1917 | 1694 | 21.6 | 16.6 | 26.3 | *** |
| Germany | 3045 | 2718 | 19.1 | 14.7 | 23.5 | *** |
| Hungary | 1698 | 1530 | 18.4 | 15.9 | 20.6 | *** |
| Ireland | 2390 | 2158 | 11.0 | 7.9 | 14.1 | *** |
| Israel | 2562 | 2244 | 14.5 | 11.2 | 17.7 | *** |
| Lithuania | 2250 | 2035 | 12.8 | 8.8 | 16.3 | *** |
| Netherlands | 1919 | 1711 | 14.0 | 10.7 | 17.1 | *** |
| Norway | 1436 | 1324 | 12.3 | 10.0 | 14.9 | *** |
| Poland | 1615 | 1469 | 15.6 | 11.4 | 19.6 | *** |
| Portugal | 1265 | 1068 | 22.1 | 17.8 | 26.0 | *** |
| Slovenia | 1224 | 1104 | 14.5 | 10.2 | 18.8 | *** |
| Spain | 1925 | 1707 | 18.2 | 12.9 | 23.5 | *** |
| Sweden | 1791 | 1574 | 13.3 | 8.8 | 18.0 | *** |
| Switzerland | 1532 | 1406 | 14.3 | 11.0 | 17.5 | *** |
| UK | 2264 | 1953 | 20.2 | 15.3 | 24.8 | *** |
Note: n.s., non-significance.
P < 0.001 in two-tail test for verifying equal proportions of reporting restless sleeping by male and female respondents.
To account for the hierarchical structure of the ESS data (with respondents nested within countries), we ran a series of multilevel logistic regressions to assess the impact of the respondents’ SES status, sociodemographic characteristics and health-related issues on reporting restless sleeping. We summarize the results of the multilevel regression models in table 2.
Table 2.
Multilevel logistic regression results
| Explanatory variables | Null model |
Model 1 |
Model 2 |
Model 3 |
Model 4 |
Model 5 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | SE | OR | SE | OR | SE | OR | SE | OR | SE | OR | SE | |
| Intercept | 0.19*** | 0.008 | 0.11*** | 0.007 | 0.08*** | 0.006 | 0.05*** | 0.004 | 0.05*** | 0.005 | 0.03*** | 0.003 |
| Female vs. Male | 1.79** | 0.055 | 1.78*** | 0.055 | 1.69*** | 0.054 | 1.70*** | 0.056 | 1.53*** | 0.055 | ||
| Age: 25–34 vs. 16–24 | 1.11 | 0.063 | 1.18** | 0.070 | 1.52*** | 0.099 | 1.41*** | 0.092 | 1.23** | 0.087 | ||
| Age: 35–44 vs. 16–24 | 1.16** | 0.066 | 1.27*** | 0.083 | 1.67*** | 0.117 | 1.54*** | 0.108 | 1.29** | 0.098 | ||
| Age: 45–54 vs. 16–24 | 1.33*** | 0.072 | 1.52*** | 0.100 | 1.91*** | 0.134 | 1.76*** | 0.125 | 1.30*** | 0.101 | ||
| Age: 55–64 vs. 16–24 | 1.55*** | 0.085 | 1.88*** | 0.132 | 1.99*** | 0.145 | 1.86*** | 0.137 | 1.34*** | 0.109 | ||
| Age: 65–74 vs. 16–24 | 1.47*** | 0.085 | 1.78*** | 0.134 | 1.50*** | 0.116 | 1.47*** | 0.116 | 1.16 | 0.101 | ||
| Single vs. Married | 1.27*** | 0.058 | 1.15** | 0.054 | 1.12* | 0.053 | 1.06 | 0.055 | ||||
| Widowed vs. Married | 1.27** | 0.095 | 1.09 | 0.083 | 1.06 | 0.081 | 0.76** | 0.066 | ||||
| Divorced/separated vs. Married | 1.46*** | 0.074 | 1.29*** | 0.068 | 1.21*** | 0.064 | 1.07 | 0.063 | ||||
| Children: 1 vs. None | 1.22*** | 0.055 | 1.20*** | 0.055 | 1.17*** | 0.053 | 1.22*** | 0.061 | ||||
| Children: 2 vs. None | 1.08 | 0.060 | 1.06 | 0.059 | 1.04 | 0.059 | 1.07 | 0.066 | ||||
| Children: 3 or more vs. None | 1.20* | 0.090 | 1.07 | 0.082 | 1.03 | 0.079 | 1.06 | 0.089 | ||||
| Income: 1st vs. 5th quintile | 1.58*** | 0.095 | 1.45*** | 0.089 | 1.03 | 0.069 | ||||||
| Income: 2nd vs. 5th quintile | 1.28*** | 0.073 | 1.22*** | 0.070 | 0.96 | 0.060 | ||||||
| Income: 3rd vs. 5th quintile | 1.24*** | 0.070 | 1.20** | 0.068 | 1.06 | 0.064 | ||||||
| Income: 4th vs. 5th quintile | 1.07 | 0.061 | 1.06 | 0.060 | 0.96 | 0.058 | ||||||
| Income: DK/REF vs. 5th quintile | 1.04 | 0.064 | 1.02 | 0.063 | 0.95 | 0.064 | ||||||
| Unemployed vs. Paid work | 1.54*** | 0.103 | 1.48*** | 0.099 | 1.25** | 0.093 | ||||||
| Economically inactive vs. Paid work | 1.48*** | 0.059 | 1.48*** | 0.059 | 1.20*** | 0.052 | ||||||
| ISCED III vs. (IV–VI) | 1.35*** | 0.054 | 1.28*** | 0.051 | 1.20*** | 0.052 | ||||||
| ISCED II vs. (IV–VI) | 1.51*** | 0.070 | 1.39*** | 0.066 | 1.19** | 0.062 | ||||||
| ISCED I vs. (IV–VI) | 1.66*** | 0.094 | 1.52*** | 0.088 | 1.34*** | 0.086 | ||||||
| Ex-smoker vs. Never smoked | 1.27*** | 0.052 | 1.12** | 0.050 | ||||||||
| Currently smoker vs. Never smoked | 1.58*** | 0.059 | 1.26*** | 0.051 | ||||||||
| Drinking alcohol: Monthly vs. No | 0.96 | 0.044 | 1.06 | 0.054 | ||||||||
| Drinking alcohol: 2–4 times a month vs. No | 0.74*** | 0.034 | 0.94 | 0.047 | ||||||||
| Drinking alcohol: 2–3 times a week vs. No | 0.78*** | 0.042 | 0.98 | 0.058 | ||||||||
| Drinking alcohol: 4 or more times a week vs. No | 0.82** | 0.055 | 1.00 | 0.073 | ||||||||
| Health: Good vs. Very good | 1.18** | 0.060 | ||||||||||
| Health: Poor vs. Very good | 1.92*** | 0.106 | ||||||||||
| Chronic illnesses: 1 vs. None | 1.38*** | 0.078 | ||||||||||
| Chronic illnesses: 2 vs. None | 1.68*** | 0.098 | ||||||||||
| Chronic illnesses: 3 or more vs. None | 2.44*** | 0.132 | ||||||||||
| Depression: Medium vs. No | 3.30*** | 0.140 | ||||||||||
| Depression: High vs. No | 9.00*** | 0.480 | ||||||||||
| ICC | 0.007 | 0.006 | 0.006 | 0.003 | 0.004 | 0.005 | ||||||
| Observations | 32 704 | 32 704 | 32 704 | 32 704 | 32 704 | 32 704 | ||||||
| Marginal R2/Conditional R2 | 0.000/0.007 | 0.032/0.038 | 0.039/0.044 | 0.067/0.070 | 0.079/0.083 | 0.238/0.242 | ||||||
| AIC | 24 574.054 | 24 137.677 | 24 077.972 | 23 663.808 | 23 499.906 | 20 428.518 | ||||||
| Log-likelihood | −12 285.027 | −12 060.838 | −12 024.986 | −11 807.904 | −11 719.953 | −10 177.259 | ||||||
P < 0.05.
P < 0.01.
P < 0.001; two-tail test.
We started with the null model and analysis of the ICC coefficient, which we found to be less than 0.01. The latter means that a small share of the total variation (less than 1%) in the outcome variable was associated with countries, that is, only a weak relationship existed among the reporting of restless sleeping for two respondents from the same country. Thus, we followed the recommendation by reference 22 to not include any level-2 variables to explain between-country variation in the intercepts (average scores of the outcome variable) if there was little or no variation in the outcomes between countries.
The order of variables entered into the regression models was the same as in reference 16, reflecting the authors’ a priori judgment of the primary causal ordering between variables. Age and gender were the primary variables included in Model 1, followed by the inclusion of two other sociodemographics in Model 2, that is, marital status and number of children. The primary direction of causation assumed that SES would affect smoking, alcohol consumption worries, health and depression; therefore, three SES characteristics (income, employment status and education) were included in Model 3. Smoking and alcohol consumption were assumed to be causal to health status and were included in Model 4, with the health variables and depression included in Model 5.
The overall predictive power of the sequence of the models can be assessed by comparing the changes of marginal , AIC and log-likelihood ratios. Although age and gender had little predictive power (Model 1), marital status and number of children (Model 2) did not increase the predictive power. The predictive power of SES variables increased from 0.039 to 0.067. The addition of smoking and alcohol consumption (in Model 4) increased to 0.079; however, the health variables included in Model 5 significantly increased the explained variance, as indicated by reaching 0.238.
The results of our analyses (Model 5) confirmed that females have significantly higher odds of reporting restless sleeping than males. Compared with the younger respondents (16–24 years old), all other age categories reported higher odds of sleeping problems. However, the differences between the youngest and oldest became negligible when Model 5 accounted for health issues. Widowed respondents indicated fewer sleeping problems than married respondents and those in a steady partnership, and those with one child had more sleep problems than respondents without children. Being unemployed or economically inactive increased sleep problems, while highly educated respondents reported restless sleeping significantly less often. For income, the significant impact (Model 3) disappeared when accounting for health issues (Models 4 and 5). Additionally, smoking increased the odds of reporting sleeping problems, while alcohol consumption did not. Nevertheless, the most significant impact on sleeping problems can be attributed to a health condition (there were strong associations of sleep problems with self-reported health and number of chronic illnesses) and depression, which had the most significant impact on restless sleeping (cf. reference 23).
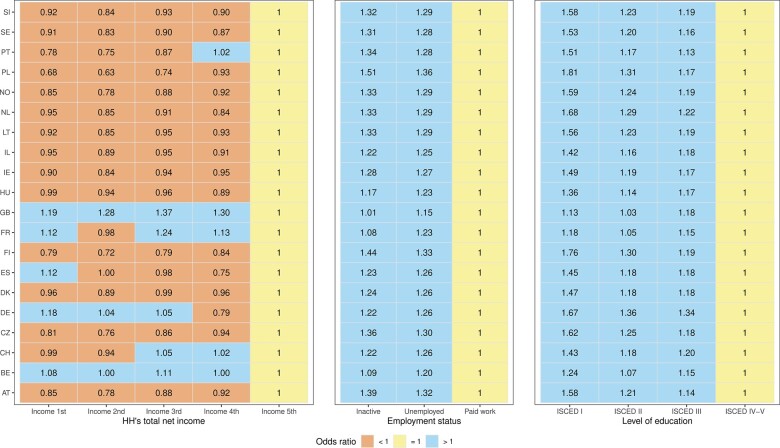
Besides the multilevel logistic regressions presented in table 2, we also ran separate models with random slopes to check whether the strength and direction of the impact of SES variables on the odds of reporting restless sleeping analyzed in table 2 were similar in all countries. Because our sample had 20 countries, we could not include random components of between-country variation in slopes for all three variables in one analysis step. Thus, for each SES variable, we independently modified our assumed multilevel mixed Model 5 by allowing one selected beta coefficient for three SES variables to vary between countries. The latter means that we analyzed whether the countries differed in terms of the impact of each SES variable on the outcome score, assuming all other associations are fixed. As shown in figure 1, the cross-country variation in random slopes for the three SES variables was negligible for employment status and education level, except for the impact of HH’s total net income, which was not the same in all countries.
Figure 1.
Cross-country variation in random slopes for SES variables.
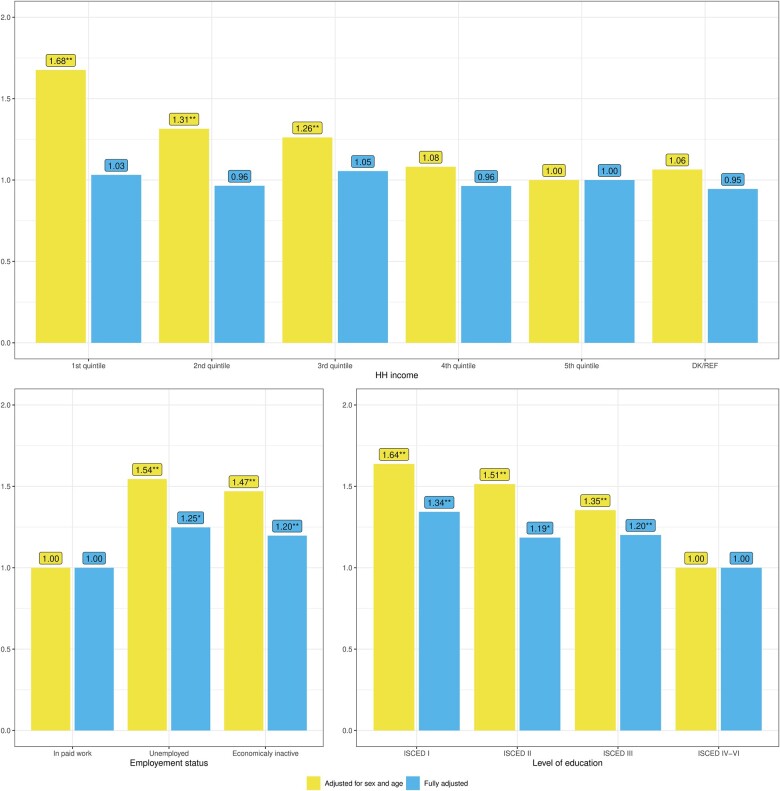
Finally, we also examined whether the impact of the three SES variables on reporting restless sleep would become weaker when we included variables describing respondents’ health. In other words, we aimed to check whether the impact of (i) income, (ii) employment status and (iii) level of education remained statistically significant after adjusting for the sociodemographic variables, smoking, worries and health variables. The assumption was that the effect of SES variables would disappear or become weaker after adjustment, which means that SES had a spurious effect on restless sleep. Figure 2 demonstrates the odds ratios of sleep problems for each SES variable following the adjustment for sex and age, here contrasted with the ‘fully adjusted’ Model 5 we presented in table 2, which adjusts for all variables we included in the analyses.
Figure 2.
Odds ratios of reporting restless sleeping by three socioeconomic status variables: (1) Adjusted for sex and age; (2) Fully adjusted for sex, age (10-year age groups), marital status, number of children, income, employment status, education, smoking, subjective health, number of chronic illnesses and depression.
The results of the analysis demonstrate that the impact of SES on reporting restless sleeping for models adjusted only for sex and age was higher than the impact we observed in the fully adjusted model. This observation was particularly evident concerning the household total net income because a significant effect disappeared when we accounted for sociodemographic and health-related issues. However, including health-related variables also weakened the impact of two other SES characteristics in our analysis, even if the odds of reporting restless sleeping between the employment and education categories remained significant in the fully adjusted model.
Discussion
The current study, an extended replication of the UK investigation by reference 16, has shown that socioeconomic status has only an apparent impact on sleep problems. According to the analyses we presented for 20 European countries, what determines sleep quality are primarily health issues and depression. These factors have been recognized in the literature on restless sleep, but the vast majority of the analyses have dealt either with individual health components24–26 or, as in the case of the Arber et al. study,16 a single country.27–29
Our replication also showed that sleep problems are influenced mainly by the individual characteristics of people, not by national factors (which is particularly important from the perspective of approaches seeking macro indicators to explain poor sleep quality/insomnia). Thus, although many insomnia studies pay attention to cross-cultural differences and the variables associated with them,30–32 our analyses demonstrated that the variance at the national level is negligible. This means that it is individual factors and not national conditions that explain the observed variability in sleep quality. It is worth adding at this point that the ESS pays special attention to the quality of questionnaire translations, which is crucial in terms of understanding by respondents what ‘restless’ sleep is (cf. reference 33).
Moreover, the link between poor sleep and mental health (especially depression) has been the subject of many previous studies.23 Some point to the impact of depression on sleep disorders,34 while others point to an inverse relationship.35 Our article is not concerned with determining the direction of this relationship, although based on the studies cited, we recognize its relevance to ‘prevention of depression in non-depressed individuals with insomnia symptoms’.23
Although females are more likely to experience restless sleep than males, which corresponds to the results of previous studies,15,36 the cross-country differences require further in-depth analysis. So, too, does the family situation, especially in the context of changing forms of socalled “family life,” with a particular focus on cohabitation or more independent forms of being together in same-sex relationships.37,38 Because the inclusion of individual variables in our models has shown that socioeconomic status has a secondary effect on sleep quality vis-á-vis self-rated health and depression, it is reasonable to use these results in a study of other countries. This is important because previous explorations of poor sleep have focused either on the predominance of socioeconomic (e.g., 39) or health-related factors (e.g., 40).
The findings contain limitations that can be addressed by future research. Above all, there seems to be a need for research that, based on a standardized methodology, can clarify the differences in sleeping problems between countries. Among other reasons, the differences between, for example, the UK (20.2%) and Ireland (11%), Austria (11%) and Germany (19.1%) cannot be conclusively explained based on the analyses carried out. This is true, as well, for the difference between the impact of cigarette smoking and alcohol consumption on sleeping problems. Nevertheless, there is a need for further verification of the hypothesis that the influence of socioeconomic determinants on sleep quality is secondary to health issues.
Contributor Information
Mariusz Baranowski, Faculty of Sociology, Adam Mickiewicz University, Poznań, Poland.
Piotr Jabkowski, Faculty of Sociology, Adam Mickiewicz University, Poznań, Poland.
Funding
This work was supported by grants awarded by the National Science Centre, Poland (grant numbers 2018/31/B/HS6/00403 and 2021/05/X/HS6/00067).
Conflicts of interest: None declared.
Key points.
Females more often experience sleep problems in European countries.
Gender differences were previously analyzed through the prism of socioeconomic status.
We demonstrated the significant impact of health-related issues and depression.
The patterns of restless sleeping are similar across European countries.
Data availability
Supplementary materials and replication codes are available via this link https://osf.io/apq84/.
References
- 1. Philips Global Sleep Survey. The global pursuit of better sleep health 2019. Available at: https://www.usa.philips.com/c-dam/b2c/master/experience/smartsleep/world-sleep-day/2019/2019-philips-world-sleep-day-survey-results.download.pdf (5 December 2022, date last accessed).
- 2. Dai H, Mei Z, An A, et al. Associations of sleep problems with health-risk behaviors and psychological well-being among Canadian adults. Sleep Health 2020;6:657–61. [DOI] [PubMed] [Google Scholar]
- 3. Smith CE, Lee S.. Identifying diverse forms of (un)healthy sleep: sleep profiles differentiate adults' psychological and physical well-being. Soc Sci Med 2022;292:114603. [DOI] [PubMed] [Google Scholar]
- 4. Kloss JD, Perlis ML, Zamzow JA, et al. Sleep, sleep disturbance, and fertility in women. Sleep Med Rev 2015;22:78–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tan H-L, Kheirandish-Gozal L, Gozal D.. Sleep, sleep disorders, and immune function. In: Fishbein A, Sheldon SH, editors. Allergy and Sleep: Basic Principles and Clinical Practice. Cham: Springer International Publishing, 2019: 3–15. [Google Scholar]
- 6. Altena E, Baglioni C, Espie CA, et al. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J Sleep Res 2020;29:e13052. [DOI] [PubMed] [Google Scholar]
- 7. Jahrami H, BaHammam AS, Bragazzi NL, et al. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med 2021;17:299–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Merikanto I, Kortesoja L, Benedict C, et al. Evening-types show highest increase of sleep and mental health problems during the COVID-19 pandemic—multinational study on 19 267 adults. Sleep 2021;45:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sørengaard TA, Saksvik-Lehouillier I.. Associations between burnout symptoms and sleep among workers during the COVID-19 pandemic. Sleep Med 2022;90:199–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dregan A, Armstrong D.. Age, cohort and period effects in the prevalence of sleep disturbances among older people: the impact of economic downturn. Soc Sci Med 2009;69:1432–8. [DOI] [PubMed] [Google Scholar]
- 11. Miller MB, Metrik J, Borsari B, Jackson KM.. Longitudinal associations between sleep, intrusive thoughts, and alcohol problems among veterans. Alcohol Clin Exp Res 2019;43:2438–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Palimaru AI, Dong L, Brown RA, et al. Mental health, family functioning, and sleep in cultural context among American Indian/Alaska Native urban youth: a mixed methods analysis. Soc Sci Med 2022;292:114582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dregan A, Armstrong D.. Cross-country variation in sleep disturbance among working and older age groups: an analysis based on the European Social Survey. Int Psychogeriatr 2011;23:1413–20. [DOI] [PubMed] [Google Scholar]
- 14. Meadows R, Brunton-Smith I, Ellis J.. Are sleep quality judgments comparable across individuals, places, and spaces? An interdisciplinary analysis of data from 207,608 individuals across 68 countries. Sleep Health 2022;8:380–6. [DOI] [PubMed] [Google Scholar]
- 15. van de Straat V, Bracke P.. How well does Europe sleep? A cross-national study of sleep problems in European older adults. Int J Public Health 2015;60:643–50. [DOI] [PubMed] [Google Scholar]
- 16. Arber S, Bote M, Meadows R.. Gender and socio-economic patterning of self-reported sleep problems in Britain. Soc Sci Med 2009;68:281–9. [DOI] [PubMed] [Google Scholar]
- 17. Amschler DH, McKenzie JF.. Perceived sleepiness, sleep habits and sleep concerns of public school teachers, administrators and other personnel. Am J Health Educ 2010;41:102–9. [Google Scholar]
- 18. Maume DJ, Hewitt B, Ruppanner L.. Gender equality and restless sleep among partnered Europeans. J Marriage Fam 2018;80:1040–58. [Google Scholar]
- 19. Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psycholog Measur 1977;1:385–401. [Google Scholar]
- 20. Hox JJ, Moerbeek M, Van de Schoot R.. Multilevel Analysis: Techniques and Applications. New York: Routledge; 2010. [Google Scholar]
- 21. R Core Team. R: A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing; 2021. [Google Scholar]
- 22. Heck RH, Thomas SL, Tabata LN.. Multilevel and Longitudinal Modeling with IBM SPSS. Routledge; 2013. [Google Scholar]
- 23. Li L, Wu C, Gan Y, et al. Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry 2016;16:375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Assari S, Sonnega A, Pepin R, Leggett A.. Residual effects of restless sleep over depressive symptoms on chronic medical conditions: race by gender differences. J Racial Ethn Health Disparities 2017;4:59–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tan X, Ruppanner L, Hewitt B, Maume D.. Restless sleep and emotional wellbeing among European full-time dual-earner couples: gendered impacts of children and workplace demands. Contemp Soc Sci 2022;17:396–411. [Google Scholar]
- 26. Wakefield JRH, Bowe M, Kellezi B, et al. Longitudinal associations between family identification, loneliness, depression, and sleep quality. Br J Health Psychol 2020;25:1–16. [DOI] [PubMed] [Google Scholar]
- 27. Blunden S, Yiallourou S, Fatima Y, Australasian Sleep Association Indigenous Sleep Health Working Party. Sleep health and its implications in First Nation Australians: a systematic review. Lancet Reg Health – West Pac 2022;21:100386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Etindele Sosso FA, Kreidlmayer M, Pearson D, Bendaoud I.. Towards a socioeconomic model of sleep health among the Canadian population: a systematic review of the relationship between age, income, employment, education, social class, socioeconomic status and sleep disparities. Eur J Investig Health Psychol Educ 2022;12:1143–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Peristera P, Nyberg A, Magnusson Hanson LL, et al. How consistently does sleep quality improve at retirement? Prospective analyses with group-based trajectory models. J Sleep Res 2022;31:e13474. [DOI] [PubMed] [Google Scholar]
- 30. Jeon M, Dimitriou D, Halstead EJ.. A systematic review on cross-cultural comparative studies of sleep in young populations: the roles of cultural factors. Int J Environ Res Public Health 2021;18:2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bakour C, Nieto FJ, Petersen DJ.. Chapter 2 - Sleep in human and cultural evolution. In: Nieto FJ, Petersen DJ, editors. Foundations of Sleep Health. London: Academic Press; 2022: 13–36. [Google Scholar]
- 32. Grandner MA, Patel NP, Jean-Louis G, et al. Sleep-related behaviors and beliefs associated with race/ethnicity in women. J Natl Med Assoc 2013;105:4–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Robbins R, Quan SF, Barger LK, et al. Self-reported sleep duration and timing: a methodological review of event definitions, context, and timeframe of related questions. Sleep Epidemiol 2021;1:100016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Riemann D, Voderholzer U.. Primary insomnia: a risk factor to develop depression? J Affect Disord 2003;76:255–9. [DOI] [PubMed] [Google Scholar]
- 35. Ohayon MM, Roth T.. Place of chronic insomnia in the course of depressive and anxiety disorders. J Psychiatr Res 2003;37:9–15. [DOI] [PubMed] [Google Scholar]
- 36. Lallukka T, Sares-Jäske L, Kronholm E, Sääksjärvi K, Lundqvist A, Partonen T, et al. Sociodemographic and socioeconomic differences in sleep duration and insomnia-related symptoms in Finnish adults. BMC Public Health 2012;12(1):565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Byrne EM, Timmerman A, Wray NR, Agerbo E.. Sleep disorders and risk of incident depression: a population case–control study. Twin Res Hum Genet 2019;22:140–6. [DOI] [PubMed] [Google Scholar]
- 38. Patterson CJ, Potter EC.. Sexual orientation and sleep difficulties: a review of research. Sleep Health 2019;5:227–35. [DOI] [PubMed] [Google Scholar]
- 39. Seo WH, Kwon JH, Eun S-H, et al. Effect of socio-economic status on sleep. J Paediatr Child Health 2017;53:592–7. [DOI] [PubMed] [Google Scholar]
- 40. Sidani S, Guruge S, Illanko K.. The experiences and determinants of sleep problems of immigrant and Canadian-born older adults-analysis of Canadian longitudinal study on aging baseline data. Can J Nurs Res 2022;54:168–76. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Supplementary materials and replication codes are available via this link https://osf.io/apq84/.