Abstract
Introduction
All national orthopaedic societies advocate the use of patient reported outcome measures (PROMs), but clear guidance on their use is limited. We utilised a collaborative methodology to perform a national audit aiming to assess the perceived variability in PROMs practice in orthopaedic surgery in the United Kingdom.
Methods
A multicentre collaborative audit of practice was performed extracting PROMs data on 21 commonly performed orthopaedic procedures. For each procedure, data were collected for frequency of PROM collection, type of PROM chosen, administration intervals, method and reason for collection. Compliance with national society recommendations was undertaken.
Results
Sixty-three trusts enrolled to participate in the study with a completion rate of 60% (38 trusts). The most frequently reported PROMs were those associated with best practice tariffs (83.3% and 80.6% for hip and knee replacements, respectively). Outside incentivised programmes we observed a higher rate of variation in PROMs practice which failed to meet our audit standard. Across all procedures evaluated, 69% (221/318) of respondents to the study used paper as the primary method of PROM collection.
Conclusions
This is the first national audit of PROMs collection in orthopaedics. The integration of PROMs within best practice tariff platforms positively influences the frequency and standardisation of collection. Outside this initiative, PROMS collection is infrequent and highly varied despite the presence of several registries. Because PROMs collection is a recommendation across all procedures using implantable devices, the success of this will depend on the adequacy of funding, resource delivery and the presence of clearer recommendations.
Keywords: Patient outcome assessments, Patient-reported outcome, Patient-relevant outcome, Orthopaedic surgery
Introduction
Patient-reported outcome measures (PROMs) aim to quantify aspects of a patient’s health and quality-of-life from their perspective.1 PROMs have become an accepted metric in orthopaedic practice and although traditionally used in research, PROMs collection has become widespread in an effort to quantify the patient-focused outcome of orthopaedic care.2 Furthermore, PROMs feedback has been shown to improve patient–clinician communication, which helps decision-making, detection of problems and provision of advice.3,4
Since 2009, the National PROMs programme has been routinely collecting both generic quality-of-life and joint-specific outcome measures from National Health Service (NHS) patients before and after hip and knee replacement surgery in England.5
A 10% reduction in tariff is attributed with a less than 50% completion rate or if providers are identified as outliers in comparison with the national average.6 However, the routine collection of PROMs outside these initiatives has struggled to progress and little is known about what happens at a local provider level.7
In 2019, eight members of The National PROMs Network across the UK agreed to share their organisations’ current PROMs practice.8 The National PROMs Network is a network of individuals (consultant orthopaedic surgeons, trainees, allied health professionals, researchers and administrators) who work together to share experiences and best practice in collecting and using PROMs. The Network found considerable variation in the PROMs used, their collection methods and their administration intervals. This variability in PROMs use extends to the academic literature where systematic reviews have identified a wide choice and usage of PROMs, particularly in the field of shoulder and elbow surgery.9,10
The importance of PROMs has recently been renewed following the publication of the Cumberlege ‘First Do No Harm’ report in 2020.11 Guidance from the report is explicit in recommending long-term PROMs follow-up for all cases associated with the use of medical devices. Responses to this report from the British Orthopaedic Association and the National Joint Registry (NJR)11,12 echo the importance of increasing the utilisation of PROMs. The Medicines and Healthcare products Regulatory Agency must also now engage with patient-reported outcomes and the government is committed to ensuring the continued usage of PROMs in clinical practice.13 With renewed interest in routine PROMs practice we aimed to develop a national overview of PROMs administration in orthopaedics by assessing the PROMs used in common procedures, their frequency of use and their administration technique. We also aimed to assess the variability in departmental strategy for PROMs collection and compliance with specialty society recommendations.
Methods
We searched for PROMs guidance available from each subspeciality orthopaedic society and used these recommendations to inform our audit gold standard of practice. We performed a national multicentre observation of practice audit involving 38 hospitals within the United Kingdom (UK). Study data were collected and managed using REDCap electronic data capture tools hosted at Royal Devon University Healthcare NHS Foundation Trust.14 The study is referred to as Evaluating the Measures in Patient Reported Outcomes, Values and Experiences (EMPROVE) for the remainder of the article.
To address the main aims of the study, a data collection tool was developed by a panel of consultant surgeons and administrators with affiliation to The National PROMs Network.8 The team included three PROMs administrative managers and five consultant orthopaedic surgeons. Guided by an initial search of PROMs guidance and working knowledge of The National PROMs Network, 21 orthopaedic conditions were chosen from 6 subspecialties, which included shoulder and elbow, hand and wrist, hip, knee, foot and ankle, and spinal surgery. For each condition, data were collected for frequency of PROM collection, type of PROM chosen, administration intervals, method of collection (eg paper format versus electronic format) and reason for collection. These data were compared directly with our audit standard (Tables 1–5). The results were analysed descriptively by a single researcher (AHM).
Table 1 .
Summary of PROM guidance and results of the EMPROVE study for hip and knee procedures
| Operation | PROMs advised | Time frame | Source | % collect PROMs? | What PROM collected? | Time frame collected | Method of collection |
|---|---|---|---|---|---|---|---|
| Hip | |||||||
| Hip arthroplasty | OHS, EQ-5D, EQ-VAS | Preoperative and 6 months postoperative | BOA/NPP | 83.3 (30/36) | OHS (24), HHS (2), iHOT (1), VAS (8), EQ-5D (19) | 100% preoperative and 63.3% (19/30) at 6 months | Paper 70% (21/30) |
| Revision hip arthroplasty | OHS, EQ-5D, EQ-VAS | Preoperative and 6 months postoperative | NPP/NJR | 61.1 (22/36) | OHS (19), EQ-5D (13), HHS (1), UCLA (1), VAS (6), START-MSK (1) | 100% (22) preoperative and 63.6% (14/22) at 6 months | Paper 68.2% (15/22) |
| Knee | |||||||
| Knee arthroplasty | OKS, EQ-5D, EQ-VAS | Preoperative and 6 months postoperative | BOA/NPP | 80.6 (29/36) | OKS (24), EQ-5D (19), VAS (8), Lysholm (1), KOOS (1) | 100% preoperative and 62.1% (18/29) at 6 months | Paper 69% (20/29) |
| Revision knee arthroplasty | |||||||
| OKS, EQ-5D, EQ-VAS | Preoperative and 6 months postoperative | NPP/NJR | 61.1 (22) | OKS (10), KOOS (1), EQ-5D (14), AWBT (1), START-MSK (1), VAS (5), UCLA (1) | 100% (22) preoperative and 59.1% (13) at 6 months | Paper 68.2% (15/22) | |
| ACL repair | KOOS, IKDC, TAS, EQ-5D | Not specified | BASK/BOSTAA/NLR | 28.6 (10/35) | EQ-5D (8), OKL (1), Lysholm (11), IKDC (5), KOOS (6), OKS (2) | 80% (8/10) preoperative and 80% at 12 months | Paper 70% (7/10) |
ACL = anterior cruciate ligament; AWBT = Aberdeen Weight Bearing Test; BASK = British Association for Surgery of the Knee; BOA = British Orthopaedic Association; BOSTAA = British Orthopaedic Sports Trauma and Arthroscopy Association; EQ-5D = EuroQol-Five Dimension Questionnaire; EQ-VAS = EuroQol-Visual Analogue Scale; HHS = Harris Hip Score; iHOT = internation Hip Outcome Tool; IKDC = International Knee Documentation Committee; KOOS = Knee injury and Osteoarthritis Outcome Score; NJR = National Joint Registry; NLR = National Ligament Registry; NPP = National PROMs Programme; OHS = Oxford Hip Score; OKL = Oswestry Knee Ligament; OKS = Oxford Knee Score; PROM = patient reported outcome measure; START-MSK = Keele STarT Tool; TAS = Tegner Activity Score; UCLA = University of California, Los Angeles Activity Scale; VAS = visual analogue scale
Table 5 .
Summary of PROM guidance and results of the EMPROVE study for spinal procedures
| Operation | PROMs advised | Time frame | Source | % collect PROMs? | What PROM collected? | Time frame collected | Method of collection |
|---|---|---|---|---|---|---|---|
| Spinal surgery | |||||||
| Anterior cervical decompression and fusion | EQ-5D, VAS neck and arm pain, NDI, MDI | Preoperative, 6 weeks postoperative, 6 months and 12 months | BASS | 37.1 (13/35) |
NDI (12), MDI (4), VAS (9), EQ-5D (9) | 100% (13) preoperative, 92.3% (12/13) at 6 weeks, 100% at 6 months, 76.9% (10/13) at 12 months | Paper 30.8% (4/13), web-based 30.8% (4/13) |
| Primary lumbar decompressor/discectomy | EQ-5D, VAS for back and leg pain, ODI | Preoperative, 6 weeks postoperative, 6 months, 12 months and 24 months | BOA/BASS | 37.1 (13/35) |
ODI (13), VAS (9), EQ-5D (13) | 100% preoperative, 92.3% (12/13) at 6 weeks, 100% at 6 months, 76.9% (10/13) at 12 months | Paper 38.5% (5/13), web-based 30.8% (4/13) |
BASS = British Association of Spinal Surgeons; BOA = British Orthopaedic Association; EQ-5D = EuroQol-Five Dimension Questionnaire; MDI = Myelopathy Disability Index; NDI = Neck Disability Index; ODI = Oswestry Disability Index; PROM = patient-reported outcome measure; VAS = visual analogue scale
Table 2 .
Summary of PROM guidance and results of the EMPROVE study for shoulder and elbow procedures
| Operation | PROMs advised | Time frame | Source | % collect PROMs? | What PROM collected? | Time frame collected | Method of collection |
|---|---|---|---|---|---|---|---|
| Shoulder and elbow | |||||||
| Excision arthroplasty of ACJ | OSS, SPADI, EQ-5D, DASH | Preoperative and at 12 months | BESS | 33 (12/36) | OSS (9), qDASH (3), DASH (1), SANE (1), EQ-5D (4) | 100% preoperative and 66 7% (8/12) at 12 months | Paper 75% (9/12) |
| Rotator cuff repair | OSS, SPADI, EQ-5D | Preoperative and at 12 months | BESS | 44 4 (16/36) | ASES (2), VAS (3), CMS (2), OSS (10), SANE (1), EQ-5D (5) qDASH (3) | 100% preoperative and 80% (12/15) at 12 months | Paper 80% (12/15) |
| Shoulder arthroplasty | DASH, CS, OSS, EQ-5D | Preoperative and at 6 months | BESS | 75 (27/36) | OSS (18), ASES (1), SANE (1), VAS-P (4). CMS (1). DASH (2), EQ-5D (9) | 100% preoperative and 50% (13/26) at 6 months | Paper 70.4% (19/27) |
| Shoulder instability | OSIS, EQ-5D | Preoperative and 12 months | BESS | 50 (18/36) | OSIS (11), ASES (1), SANE (1), VAS (1), OSS (5), EQ-5D (6), SPONSA (1) | 100% preoperative and 76 5% (13/17) at 12 months | Paper 72 2% (13/18) |
| Elbow replacement | OES, EQ-5D, DASH | Preoperative and at 6 months | BESS | 40 (14/35) | OES (9), SPONSA (1), VAS (2), MEPI (2), qDASH (3), EQ-5D (4) | 100% preoperative and 76.9% (10/13) at 12 months | Paper 71 4% (10/14) |
ACJ = acromioclavicular joint; ASES = American Shoulder and Elbow Score; BESS = British Elbow and Shoulder Society; CMS = Constant--Murley Shoulder score; DASH = Disability of the Arm, Shoulder and Hand; EQ-5D = EuroQol-Five Dimension Questionnaire; MEPI = Mayo Elbow Performance Index; OES = Oxford Elbow Score; OSIS = Oxford Shoulder Instability Score; OSS = Oxford Shoulder Score; PROM = patient-reported outcome measure; qDASH = The Quick Disabilities of the Arm, Shoulder, and Hand questionnaire; SANE = Single Assessment Numerical Evaluation; SPADI = Shoulder Pain and Disability Index; SPONSA = Stanmore Percentage of Normal Shoulder Assessment; VAS-P = visual analogue scale for pain
Table 3 .
Summary of PROM guidance and results of the EMPROVE study for hand and wrist procedures
| Operation | PROMs advised | Time frame | Source | % collect PROMs? | What PROM collected? | Time frame collected | Method of collection |
|---|---|---|---|---|---|---|---|
| Hand and wrist | |||||||
| Trigger finger release | Not given (UKHR not accessible) | Not given (UKHR not accessible) | Not given (UKHR not accessible) | 17.6 (6/34) | PEM (3), qDASH (3), PRWE (1), VAS (1), EQ-5D (1) | 100% (6/6) preoperative, 33.3% at 6 weeks, 50% at 6 months, 50% at 12 months | Paper 83.3% (5/6) |
| Duptryen's | Not given (UKHR not accessible) | Not given (UKHR not accessible) | Not given (UKHR not accessible) | 24.2 (8/33) | qDASH (3), EQ-5D (3), PEM (4), URAM (3), PRWE (1) | 87.5% (7/8) preoperative, 37.5% (3/8) at 6 weeks, 62.5% at 6 months, 50% at 12 months | Paper 75% (6/8) |
| Basilar thumb OA | Not given (UKHR not accessible) | Not given (UKHR not accessible) | Not given (UKHR not accessible) | 3.3 (1/30) | PEM (2), EQ-5D (1), VAS (1), PRWE (1), qDASH (1) | 100% (4/4) preoperative, 25% at 6 weeks, 75% at 6 months, 50% at 12 months | Paper 75% |
| Carpal tunnel surgery | PEM Levine |
Not given (UKHR not accessible) | BOA/UKHR | 23.5 (8/34) | PEM (4), qDASH (3). BCTQ (4), EQ-5D (3), PRWE (1) | 100% preoperative, 37.5% at 6 weeks, 50% at 6 months, 62.5% at 12 months | Paper 75% (6/8), web-based 25% |
BCTQ = Boston Carpal Tunnel Questionnaire; EQ-5D = EuroQol-Five Dimension Questionnaire; PEM = patient evaluation measure; PROM = patient-reported outcome measure; qDASH = The Quick Disabilities of the Arm, Shoulder, and Hand questionnaire; UKHR = United Kingdom Hand Registry; URAM = the Unité Rhumatologique des Affections de la Main (URAM) scale; VAS = visual analogue scale
Table 4 .
Summary of PROM guidance and results of the EMPROVE study for foot and ankle procedures
| Operation | PROMs advised | Time frame | Source | % collect PROMs? | What PROM collected? | Time frame collected | Method of collection |
|---|---|---|---|---|---|---|---|
| Foot and ankle | |||||||
| Great toe surgery | MOXFQ, EQ-5D | Preoperative and 12 months postoperative | BOA | 30.6 (11/36) | MOXFQ (9), VAS (3), EQ-5D (5), HMIS (1), START-MSK (1) | 100% (11) preoperative, 54.5% (6/11) at 12 months | Paper 72.7% (8/11) |
| Ankle fusion | MOXFQ, FFI, EQ-5D, SF-36 | Preoperative and 12 months postoperative | BOFAS | 47.2 (17/36) | MOXFQ (14), VAS (5), EQ-5D (10), OAS (1), AO FAS (2), START-MSK (1) | 100% (17/17) preoperative, 64.7% (11/17) at 6 months, 70.6% (12/17) at 12 months | Paper 82.4% (14/17) |
| Midfoot dusion | MOXFQ, FFI, EQ- 5D, SF-36 | Preoperative and 12 months postoperative | BOFAS | 27.8 (10/36) | MOXFQ (9), VAS (2), EQ-5D (4), FAOS (1) | 100% (10/10) preoperative, 60% (6/10) at 12 months | Paper 70% (7/10) |
| Ankle replacement | MOXFQ, EQ-5D | Preoperative and 6 months | NJR | 47.2 (17/36) | MOXFQ (14), VAS (5), EQ-5D (10), OAS (1), AO FAS (2), START-MSK (1) | 100% (17/17) preoperative, 64.7% (11/17) at 6 months, 70.6% (12/17) at 12 months | Paper 82.4% (14/17) |
| Lesser Toe surgery | Not specified | Not specified | None | 22.2 (8/36) | MOXFQ (6), VAS (1), EQ-5D (4), FAOS (1), START-MSK (1) | 100% (8/8) preoperative, 37.5% (3/8) at 6 months, 50% at 12 months | Paper 62.5% (5/8) |
AOFAS = American Orthopaedic Foot and Ankle Score; BOA = British Orthopaedic Association; BOFAS = British Orthopaedic Foot and Ankle Society; EQ-5D = EuroQol-Five Dimension questionnaire; FAOS = Foot and Ankle Outcome Score; FFI = Foot Function Index; HMIS = Hallux Metatarsophalangeal Interphalangeal Scale, MOXFQ = The Manchester Oxford Foot Questionnaire; NJR = National Joint Registry; OAS = Oxford Ankle Foot Questionnaire; PROM = patient-reported outcome measure; SF-36 = Short Form 36; START MSK = Keele Start MSK Tool; VAS = visual analogue scale
Results
Overview of results
Sixty-three trusts in the UK enrolled in the study. Following a period of 3 months’ data collection, 38 hospitals across 9 regions completed the study questionnaire (Figure 1). Some 65.8% (25/38) of responses were completed by registrars with the support of the supervising consultant at the participating site. Of the respondents, only eight (21.1%) hospitals have a designated PROMs manager or administrator. When asked who was responsible for collecting PROMs, 18 hospitals (62.1%) felt that it was left to the consultants to collection their own PROMs. Sixty-nine per cent (221/318) of respondents to questions concerning the method of PROM collection across all conditions used a paper format. Tables 1–5 give a summary of the national guidance15–22 for all 21 orthopaedic conditions subdivided by specialty with the results of the EMPROVE study. Where PROMs guidance was readily available, there was greatest compliance with that outlined by the commissioning care pathways for shoulder replacement surgery and hip and knee replacement surgery. PROMs collection for all hand and wrist conditions, foot and ankle conditions, and spinal conditions failed to meet the audit standard where this was available.
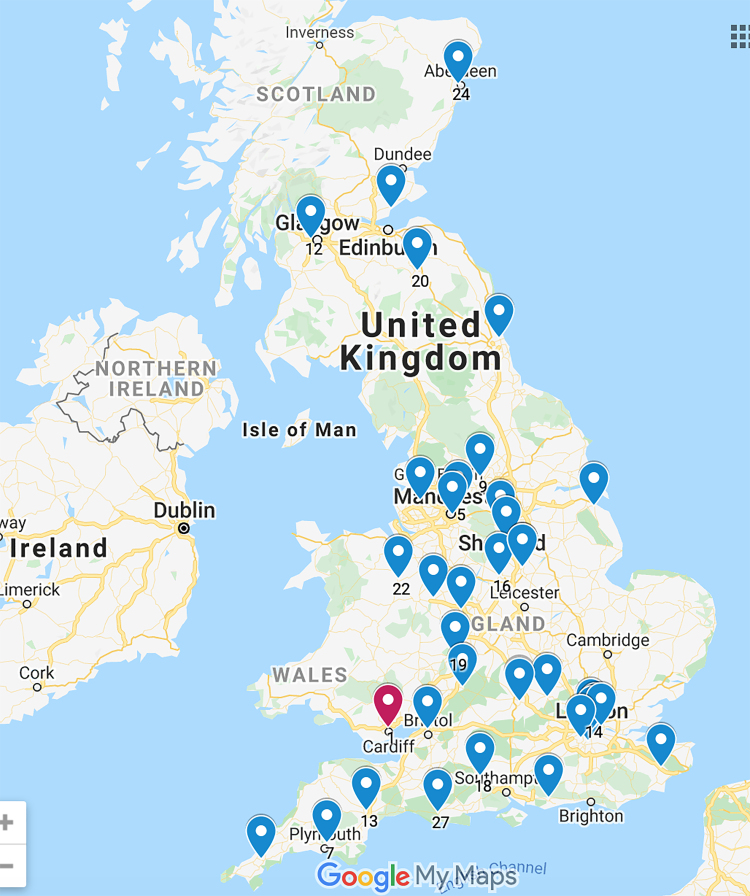
Figure 1 .
Map of United Kingdom showing dispersion of the 38 Trusts that enrolled and participated in the study
The national PROMs programme effect
The reporting of PROMs was most frequent and standardised among the group of conditions incentivised by the national PROMs programme. Table 1 outlines the results for hip and knee arthroplasty. Thirty hospitals (30/36, 83.3%) collect PROMs for patients undergoing primary hip replacement procedures. All hospitals collected pre-intervention hip PROMs; however, only 19 (63.3%) collected or accessed outcomes 6 months post-procedure. The Oxford Hip Score was used as the disease-specific PROM by 24 hospitals (24/30, 80.0%) and EQ-5D™ generic quality-of-life PROM was used in 19 hospitals (19/30, 63.3%). For patients undergoing primary knee arthroplasty, 29 hospitals (29/36, 80.6%) collected PROMs. All respondents collected pre-intervention PROMs and similarly 18 (62.1%) has access to a 6-month post-procedure outcome. The Oxford Knee Score was the most frequently collected condition-specific PROM (24/29, 82.8%).
The wider scope of PROMs practice
Outside procedures that attract best practice tariffs, PROMs collection was much more variable. We found good uptake of PROMs use for patients undergoing shoulder replacement surgery with 75.0% (27/36) of respondents indicating that this was the case. This was consistent with good societal PROMs recommendations from the British Elbow and Shoulder Society (BESS). The postoperative administration of PROMs was highly variable, with 50.0% (13/26) occurring at 6 months and 76.9% (20/26) occurring at 12 months despite BESS recommending only 12 months PROM collection. Such PROMs were mainly collected for individual patient monitoring (19/27, 70.4%). Although most centres (18/26, 69.2%) used the Oxford Shoulder Score, respondents also used the American Shoulder and Elbow Score, Constant–Murley Shoulder Score, Adleir Score, Single Assessment Numerical Evaluation, the Stanmore Percentage of Normal Shoulder Assessment, the Disability of the Arm, Shoulder and Hand score and the shortened version of the Disability of the Arm, Shoulder and Hand score (QuickDASH).
Despite the presence of the British Orthopaedic Foot and Ankle Registry, the UK National Hand Registry and the National Ligament Registry, we observed a poor uptake of PROMs collection in these subspecialty areas. Only 47.2% (17/36) of centres collect routine PROMs for ankle arthritis procedures. Within hand surgery, only 23.5% (8/34) of hospitals routinely collected data for carpal tunnel decompression. There was also greater variety in the type of PROM collected and the time intervals at which they were measured. This variability in PROM usage was most evident for patients with knee ligament injuries requiring reconstruction, where despite a poor uptake in centres collecting PROMs (10/35, 28.6%), seven condition-specific PROMs were recorded. We acknowledge the poor uptake of registries for these procedures (6/17, 35.3%) following ankle fusion procedures, carpal tunnel decompression (2/8, 25.0%) and ligament reconstruction procedures (5/10, 50.0%), and greater compliance with these may decreased the observation of several different PROMs being implemented in practice for a single condition.
Discussion
This is the first national review of PROMs in clinical practice within orthopaedics in the UK. The acquisition of PROMs linked to best practice tariffs led to increased frequency and improved standardisation of collection, and unification of the PROM used. Compliance with national society recommendations is most evident for PROMs linked to the national PROMs programme, with a compliance rate of 83.3% and 80.6% for hip and knee arthroplasty, respectively. Data from the national PROMs programme suggest an even higher frequency of PROMs collection of over 90%.15
PROMs data collection outside PROMs programmes and registry-incentivised schemes is lacking and poorly standardised. On review of national society guidelines we identified poor guidance on PROMs choice and collection. There is also poor uptake within the unincentivised national registries. We therefore advocate stronger and clearer national society PROMs recommendations, emphasising the importance of using registries where available. We propose that these recommendations should be based on a rigorous synthesis of the evidence rather than expert consensus using measurement tools such as Consensus-based Standards for the Selection of health Measurement Instruments. There are also international societies, such as the International Consortium for Health Outcomes Measurement, that aim to provide an international standardisation of outcome sets, including PROMs, at a condition-specific level, but whose recognition within the UK orthopaedic community is limited.16 They have produced standard sets for hip, knee osteoarthritis, hand and wrist conditions, and lower back pain. However, there is disparity between these outcome sets and those recommended by UK societies. Their recommendations are also highly resource intensive and therefore challenging to implement in practice.
Greenhalgh and colleagues3 found that where no incentives were attached to using PROMs, clinicians were less compliant with their use because they felt PROMs did not support the care of patients. Healthcare providers were found to be more likely to take steps to improve patient care in response to the feedback and public reporting of PROMs if they perceived that these data were credible, timely and identified problems. In 2013, a review by Varagunam et al17 determined that the national PROMs programme failed to alter the performance of poorly performing providers, and this was thought to be due to inadequate provision of feedback to providers/clinicians/patients. Our results suggest that this lack of feedback to providers is an ongoing problem with only 63.3% and 62.1% of respondents reporting 6-month postoperative PROMs data for hip and knee arthroplasty, respectively. We advocate the encouragement of local feedback of PROMs data to enable these programmes to encourage positive change in outlier institutions, in line with the recent Department of Health recommendations report.18
The majority of PROM questionnaires are sent to patients as a paper copy. It has been alluded to previously that such PROMs collection is burdensome on trusts in terms of cost and timeliness.19 The recent PROMs programme consultation reports advocate for greater digitisation of PROMs, which may allow more flexibility in their usage.20 This may, in turn, enable their incorporation into Hospital Episode Statistics21 and the NJR,22 providing greater transparency in outcomes for care providers, clinicians and patients. However, this will require not only standardisation, but also the sharing of data, and an economically viable platform is needed to achieve this. Previous concerns over electronic PROMs collection have centred on the ability to capture all sections of the population, particularly the middle-aged, elderly and ethnic/culturally diverse demographic in whom concerns over data privacy and computer literacy still exist.23 It is likely that some patients will still need paper PROMs. Here, the semi-automated digital approach using barcoded/QR-coded paper PROMs may help with administration time and accuracy, and ease of scanning when a digital PROMs solution is available. Greater digitisation may also allow for easier incorporation of different language PROMs, which will improve inclusion.
This study aims to depict a national snap-shot of current PROMs practice in the UK; however, we recognise its limitation. Only 60.3% (38/63) of sites completed full data sets. Although this does not represent a numerical majority of hospitals across the UK, we believe these units are likely to represent those collecting PROMs and were enthusiastic to take part. As such, the true performance of PROMs collection in the UK is probably much worse than we have portrayed. We observed respondent fatigue with a higher proportion of respondents completing tick box questions and a lower proportion completing questions aiming to list the type of PROM collected and their administration intervals. Of the 38 sites that responded, 8 were members of The National PROMs Network and potentially represent selection bias.
This audit focused solely on PROMs following surgical interventions in musculoskeletal (MSK) conditions. In practice, PROMs are also collected by physiotherapists to follow the effectiveness of non-surgical interventions. Given the current NHS focus on a system-wide approach to treating MSK conditions, PROMs should follow the patient journey from primary care to secondary care. This is one of the main priorities of the BEST MSK Health collaborative24 which aims to consolidate data collection to measure the quality of MSK healthcare delivery. As such, it would have been useful to identify current PROM trends in non-surgically treated MSK conditions.
Conclusion
The collection of patient-reported outcomes is integral to the delivery of better, safer patient care. This study has found that strategies used to incentivise clinicians and providers to collect PROMs, greater funding for administrative management of the data, and precise national society guidance are models of practice that improved PROMs use in orthopaedics. Outside these initiatives, PROMs utilisation remains highly variable and poorly standardised. Despite the presence of several unincentivised registries designed to aide PROMs collection, uptake is poor. To achieve the aspirations of national societies and healthcare regulators, clearer recommendations, clinician education, appropriate funding and provision of staffing resources are required.
Acknowledgements
The authors wish to thank South West Orthopaedic Research Division (SWORD), Anji Kingman, Cormac Kelly and Kanthan Theivendran. This publication is dedicated to Rebecca Lafferty.
References
- 1.Valderas JM, Alonso J. Patient reported outcome measures: a model-based classification system for research and clinical practice. Qual Life Res 2008; 17: 1125–1135. [DOI] [PubMed] [Google Scholar]
- 2.Evans JP, Smith A, Gibbons Cet al. The national institutes of health patient-reported outcomes measurement information system (PROMIS): a view from the UK. Patient Relat Outcome Meas 2018; 9: 345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Greenhalgh J, Dalkin S, Gooding Ket al. Functionality and feedback: a realist synthesis of the collation, interpretation and utilisation of patient-reported outcome measures data to improve patient care. Heal Serv Deliv Res 2017; 5: 1–280. [PubMed] [Google Scholar]
- 4.Gibbons C, Porter I, Goncalves-Bradley Det al. Routine provision of feedback from patient-reported outcome measurements to healthcare providers and patients in clinical practice. Cochrane Database Syst Rev 2021; 10: 257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patient Reported Outcome Measures (PROMs) - NHS Digital. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/patient-reported-outcome-measures-proms (cited March 2023).
- 6.NHS England Consultation Report on 2021/22 National Tariff Payment System. https://mtrconsult.com/news/consultation-202122-national-tariff-payment-system-now-open-england (cited March 2023).
- 7.Kyte D, Cockwell P, Lencioni M, et al. Reflections on the national patient-reported outcome measures (PROMs) programme: where do we go from here? J R Soc Med 2016; 109: 441–445. (cited March 2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National PROMs Network. https://promsnetwork.co.uk/ (cited September 2021).
- 9.Evans JP, Smith CD, Fine NF, et al. Clinical rating systems in elbow research—a systematic review exploring trends and distributions of use. J Shoulder Elb Surg 2018; 27: e98–e106. [DOI] [PubMed] [Google Scholar]
- 10.Ashton ML, Savage-Elliott I, Granruth C, O’Brien MJ. What Are We measuring? A systematic review of outcome measurements used in shoulder surgery. Arthrosc Sport Med Rehabil 2020; 2: e429–e434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Julia C. First Do No Harm The report of the Independent Medicines and Medical Devices Safety Review. Published online 2020. www.gov.uk/official-documents (cited March 2023).
- 12.NJR Statement on the publication of The Cumberlege Report. https://www.njrcentre.org.uk/njrcentre/News-and-Events/Cumberlege-Report-NJR-Statement (cited October 2021).
- 13.Smith H. Government response to the Report of the Independent Medicines and Medical Devices Safety Review. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1005847/IMMDS_Review_-_Government_response_-_220721.pdf (cited March 2023).
- 14.Harris P, Taylor R, Thielke Ret al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42: 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Finalised Patient Reported Outcome Measures (PROMs) in England for Hip and Knee Replacement Procedures (April 2019 to March 2020) - NHS Digital. https://digital.nhs.uk/data-and-information/publications/statistical/patient-reported-outcome-measures-proms/finalised-hip-and-knee-replacement-april-2019—march-2020 (cited March 2023).
- 16.Resources – ICHOM Connect. https://connect.ichom.org/resources/ (cited March 2023).
- 17.Varagunam M, Hutchings A, Neuburger J, Black N. Impact on hospital performance of introducing routine patient reported outcome measures in surgery. J Health Serv Res Policy 2014; 19: 77–84. [DOI] [PubMed] [Google Scholar]
- 18.Patient Reported Outcome Measures (PROMs) in England A Methodology for Identifying Potential Outliers. Published online 2011. https://www.gov.uk/government/publications/patient-reported-outcome-measures-proms-in-england-a-methodology-for-identifying-potential-outliers (cited March 2023).
- 19.Malhotra K, Buraimoh O, Thornton Jet al. Electronic capture of patient-reported and clinician-reported outcome measures in an elective orthopaedic setting: a retrospective cohort analysis. BMJ Open 2016; 6: e011975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Patient Reported Outcome Measures (PROMs) Programme Consultation Report. https://www.england.nhs.uk/wp-content/uploads/2017/10/proms-consultation-report.pdf (cited March 2023).
- 21.Hospital Episode Statistics (HES) - NHS Digital. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics (cited March 2023).
- 22.National Joint Registry. https://www.njrcentre.org.uk/ (cited March 2023).
- 23.Roberts N, Bradley B, Williams D. Use of SMS and tablet computer improves the electronic collection of elective orthopaedic patient reported outcome measures. Ann R Coll Surg Engl 2014; 96: 348–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The future of MSK and the Best MSK health Collaborative #BestMSKhealth. https://future.nhs.uk/ECDC/view?objectId=152147 (cited March 2023).