Abstract
Recent years have witnessed the emergence of several viruses and other pathogens. Some of these infectious diseases have spread globally, resulting in pandemics. Although biosensors of various types have been utilized for virus detection, their limited sensitivity remains an issue. Therefore, the development of better diagnostic tools that facilitate the more efficient detection of viruses and other pathogens has become important. Nanotechnology has been recognized as a powerful tool for the detection of viruses, and it is expected to change the landscape of virus detection and analysis. Recently, nanomaterials have gained enormous attention for their value in improving biosensor performance owing to their high surface-to-volume ratio and quantum size effects. This article reviews the impact of nanotechnology on the design, development, and performance of sensors for the detection of viruses. Special attention has been paid to nanoscale materials, various types of nanobiosensors, the internet of medical things, and artificial intelligence-based viral diagnostic techniques.
Keywords: Nanotechnology, Nanomaterials, Artificial intelligence, Nanobiosensors, Viral diagnostics
Introduction
The emergence of new pathogens and the rapid spread of infectious diseases have become a recurring phenomenon and a growing concern across the world [1, 2]. For example, coronavirus disease (COVID-19), a viral infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has led to the loss of millions of human lives and has decelerated the global economy. The COVID-19 pandemic has also taught us the value of fast and precise on-site pathogen detection and its importance in preventing the spread of infection.
Among the many technological tools available for virus detection, nanomaterials and nanotechnology-assisted biosensors have proven to have advantages owing to their mobility, specificity, and ease of operation by non-experts. Nanotechnology, which is defined as “the science and engineering involved in the design, synthesis, characterization, and application of materials and devices whose smallest functional organization in at least one dimension is on the nanometer scale” [3], has become a powerful platform for the development of various types of nanomaterials and nanoscale devices. These nanomaterials are suitable for the development of highly efficient nanoscale biosensors with enhanced performance and efficacy. In addition, they possess a high surface-to-volume ratio and quantum size effects, offering new possibilities for the detection of various biomolecules and extended limits of detection [4].
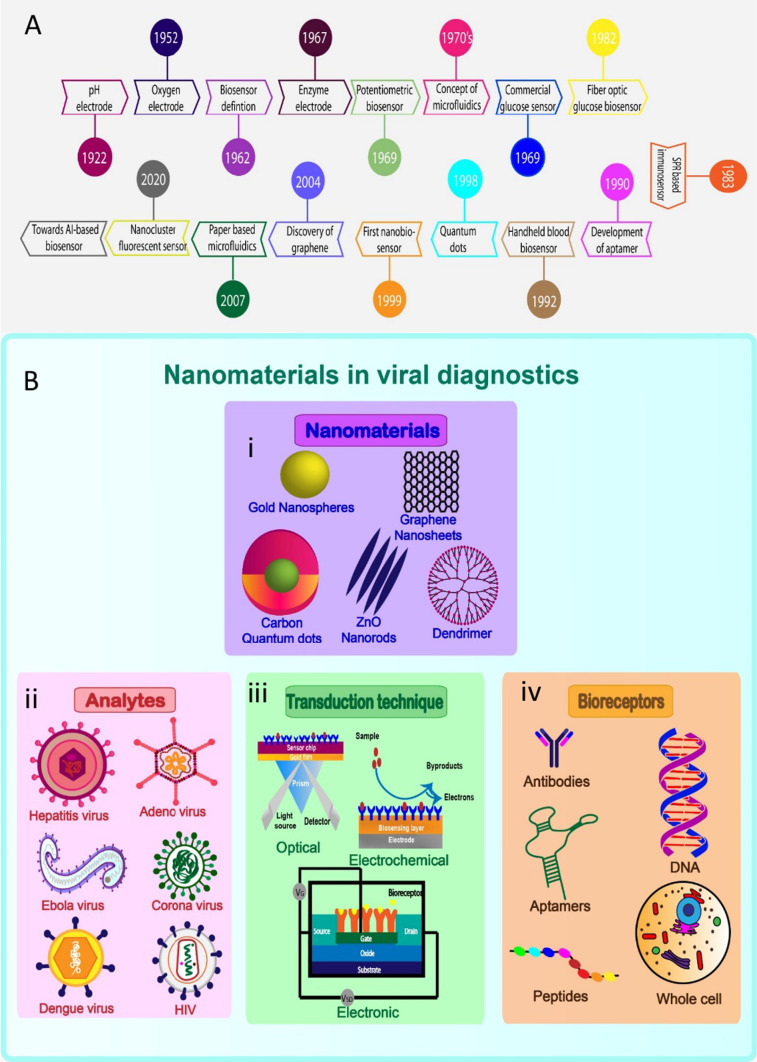
Numerous types of nanomaterials, including quantum dots (QDs) and graphene, gold, and silver nanoparticles, have recently been used in the development of sensors [5–7]. Biosensors designed based on nanoscale materials are often called nanobiosensors. These nanotechnology-based biosensors can be broadly classified into four types, namely, the electrochemical [8–11], optical [12–14], thermal [15], and piezoelectric types [16]. Fluorescent nanocluster biosensors, electrochemical nanobiosensors, and microfluidic nanomaterials have all enabled further improvements in detection sensitivity and specificity. Microfluidics, nanotechnology, and biosensors are currently being combined for a wide range of applications [17]. The evolution of nanobiosensors is depicted schematically in Fig. 1A. Although biosensors are being used to detect viruses, several issues remain to be addressed, particularly with respect to their limit of detection and sensitivity. In the recent years, the internet of medical things (IoMT), and artificial intelligence (AI)-based diagnostic techniques play a major role to enable human intervention-free detection of pathogens. It is envisioned that the integration of computer-based technologies, such as IoMT and AI, with conventional diagnostic technologies wound bring out a rapid, precise and user-friendly way of detection systems, which will revolutionize the effectiveness of the biosensors.
Fig. 1.
History and the state of the art of Nanobiosensor development: A Timeline of the (bio/nano) sensor development from 1920 to 2020. B Schematic representation of various forms of nanomaterials, analytes, transduction techniques and the bioreceptors applied for the development of viral diagnostics
Since existing reviews mainly focused on the conventional way of virus detection, the present review cover both conventional and AI-based approaches of virus detection from the nanoscale perspective. With this perspective, this article reviews the impact of nanotechnology on the conventional and AI-based biosensing approaches for the detection of viruses. It discusses the different types of nanomaterials suitable for use in biosensors as well as their key properties, and it highlights the design, development, and application of nanobiosensors in viral diagnostics. Finally, it provides insights into the impact of IoMT and AI on the detection of viruses.
Nanomaterials in biosensors
Nanomaterials are often used as a transducer that is an integral part of biosensor development and performance. Carbon-based materials such as carbon nanotubes (CNT); graphene; graphene oxide (GO); reduced graphene oxide (rGO) [18]; metallic nanoparticles such as platinum, gold, and silver [18–22]; and metal oxide nanoparticles such as indium tin oxide, titanium dioxide, and QDs [23, 24] have been used in diagnostics to enhance electrode surfaces and substrate functionalities [25]. A schematic representation of nanostructures for viral diagnostics is shown in Fig. 1B.
Gold nanomaterials are important in the field of detection because of their unique electrical and catalytic activity, high biocompatibility, and excellent electron transfer properties [26–28]. Gold nanorods (GNRs) [29], nanoporous gold, gold nanoflowers, gold nanospikes [30], bimetallic gold formations, and gold nanowires are a few forms of gold used for the detection of viruses. GNPs are prepared using a variety of methods, including laser irradiation, chemical reduction, biosynthesis, electrochemical synthesis, and seed growth [31]. GNRs-based sensors have advantages over GNPs, such as a better analytical response, simplicity, higher sensitivity, low sample quantity, label-free, and a lower limit of detection [32]. Nanoporous gold is preferred because its three-dimensional structure provides a high surface area-to-volume ratio, and also due to its robustness, ease of handling, and easily tunable pores. In addition, silver nanoparticles (AgNPs), with their high extinction coefficient and large interfacial surface area that increase electrocatalytic efficiency, are used directly for electrochemical detection [33–35]. Silver nanotriangles (AgNTs) have a stronger plasmonic effect than GNPs, can be fabricated using a simple and inexpensive process, and can be used across large areas [36]. Zinc oxide (ZnO) nanostructures provide faster responses, greater sensitivity, and better electron transfer properties [37].
Graphene, a carbon-based substance with a dense honeycomb crystal structure, has a huge surface area, good mechanical strength, and outstanding electrical conductivity. Thus, it favours electrochemical responses when deposited on an electrode. GO undergoes rapid agglomeration, while rGO can be stored without agglomeration. The oxygen-containing functional groups in rGO are useful for functionalization during the preparation of composites. Graphene QDs (GQDs) possess several favourable characteristics, such as high electron transport and mass diffusion of the analyte, electrocatalyst properties, biocompatibility, and reduced toxicity [38, 39]. CNF possesses a small number of defects, large aspect ratio, low density, high specific modulus, and high electrical conductivity.
Nanocomposites are suitable materials for electrochemical transducer systems owing to their synergistic properties [40]. The elements present in nano-composites maintain their individual features while also imparting novel properties through their combinations [41–44]. The use of different nanostructured materials in the right combination increases the efficiency and sensitivity of detection [45] while significantly reducing non-specific binding towards the analyte. After combination with CNFs, GNPs can get embedded within the sites of defect in the CNFs, increasing the sensitivity and electrochemical activity of the electrode [46, 47]. In yet another nanocomposite formed by the combination of QDs and GNP, the fluorescent properties of QDs were enhanced by the surface plasmon effect of GNPs. Nanomaterials are also well-suited for use as drug delivery systems, potentially paving the way for a new generation of theranostics [48].
Types of nanobiosensors
Nanobiosensors can be classified into different types, including electrochemical nanobiosensors, optical nanobiosensors, microfluidic nanobiosensors, and nanopore-based nanobiosensors. Each type of nanobiosensor has its own distinct working principle. The different types of nanobiosensors are briefly discussed below:
Electrochemical nanobiosensors
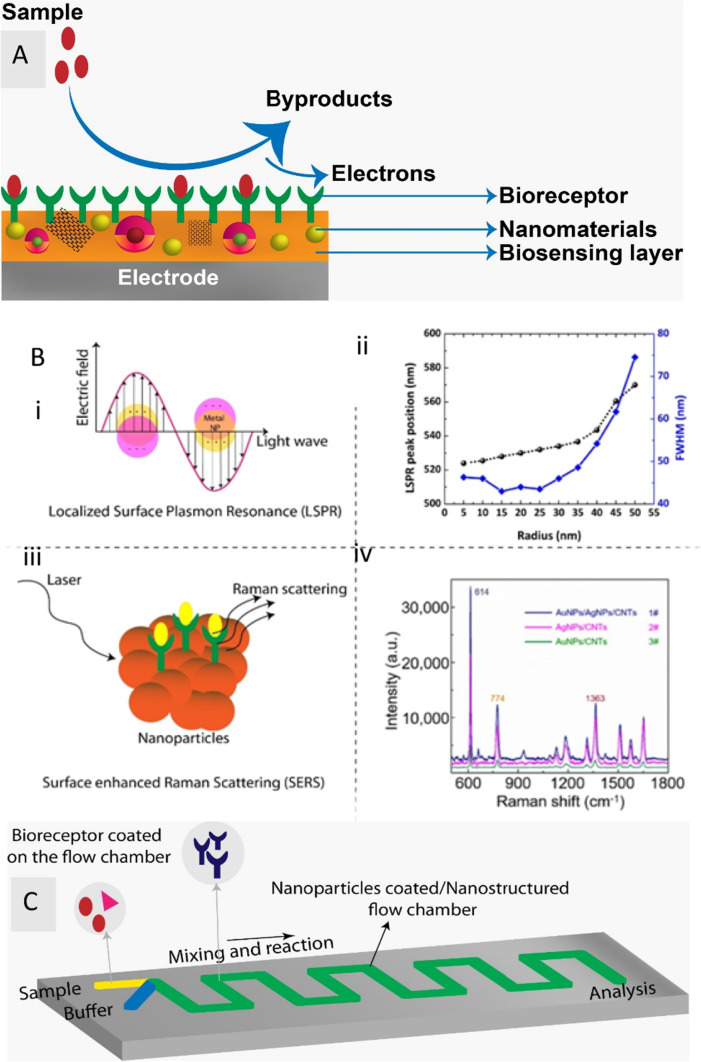
Electrochemical sensors require a receptor that can bind to the sample, and an electrode that converts the reaction into a measurable electrical signal (current, voltage, or impedance). The electrode acts as a transducer and as solid support for biomolecule immobilization and electron movement [49]. A high signal-to-noise ratio, ease of use, cost-effectiveness, compactness, high sensitivity, real-time monitoring, rapid reaction, and miniaturization potential are a few of the benefits offered by electrochemical sensing [50–52]. Amperometric [21, 53], potentiometric, impedimetric [54–56], and conductometric sensors are the four types of electrochemical sensors. A variety of biomolecules, including aptamers, proteins, DNA, microorganisms, and toxins, can be detected using these biosensors. The components of electrochemical-based nanobiosensors are shown in Fig. 2A.
Fig. 2.
Simple illustrations of Electrochemical, optical and microfluidic nanobiosensors: A Schematic illustrates the components of Electrochemical-based nanobiosensor. Here biosensing layer (electrode) is either made using nanomaterials or it is deposited onto it. When the sample interacts with the bioreceptor, by-products and electrons are formed, which is further used for detection. B Optical based nanobiosensor: (i) Schematic of the principle of LSPR, (ii) The radius of the nanoparticle is plotted against the LSPR peak resonance wavelength (black spheres) and full width half maximum (blue cubes).
Adapted from Farooq et al. [172] under Creative commons Attribution 4.0. (iii) Principle of Surface enhanced Raman scattring (iv) Raman spectra of rhodamine 6 G molecule collected on various film substrates such as Au/AgNP/crossed CNT film (#1), AgNP/crossed CNT film (#2), AuNP/crossed CNT film (#3) Adapted from Wei et al. [173] under Creative commons Attribution 4.0. C Illustration of Microfluidic based nanobiosensor. The sample is passed through one inlet and the buffer through the other and then it undergoes mixing and the reaction. It is either fabricated with a nanostructured flow chamber or coated with nanoparticles. Additionally, the flow chamber is coated with bioreceptors. Target-containing samples react with the bioreceptor when they are added, and the reaction products are then analysed in the outlet chamber
Most electrochemical reactions occur near the electrode’s surface, and the electrodes themselves play a significant role in the operation of electrochemical biosensors. The function of the materials utilized to construct the electrode as well as their surface modification and size have a significant impact on their sensing ability [57]. Nanomaterials can be used as carriers for biomolecules to detect targets with high sensitivity because of their high specific surface area. Meanwhile, when nanomaterials are used to modify electrode surfaces, their good conductivity greatly accelerates electron transfer [58]. As a result, platinum, gold, and carbon have attracted serious attention for their use in electrode fabrication given their high conductivity, inertness, biocompatibility, and large surface area.
Optical nanobiosensors
An optical biosensor generally exploits the optical field’s interaction with a bioreceptor. There are two modes of optical sensing: direct and indirect detection [59]. The indirect detection mode uses optically labelled probes, such as luminescent or fluorescent tags [60], which produce the optical signal. The direct detection mode uses LSPR [61, 62], surface-enhanced raman scattering (SERS) [63, 64], a fiber optic mode, or UV absorption techniques. In this mode, the signal is directly generated by the analyte’s interaction with the optical transducer, eliminating the need for an optically labelled probe. The principle of optical detection enables the development of simple and inexpensive analytical devices with numerous applications in portable nanobiosensor systems that can be efficiently used in remote areas and developing countries [65]. LSPR [66, 67] and SERS [42, 68, 69] have been the most commonly used approaches in optical biosensors and are explained in Fig. 2B. Metal nanoparticles, such as GNPs and AgNPs, possess distinct plasmonic properties that depend on the shape, size, and nature of nanoparticle dispersion on the substrate.
Microfluidic nanobiosensors
Microfluidics is defined as the “study of flows that are simple or complex, mono or multiphasic, and are circulating in artificial microsystems” [70]. Based on their flow properties, microfluidic biosensors can be classified into various different kinds, including continuous-flow [71], droplet-based [72, 73], digital [74, 75], and paper-based microfluidic nanobiosensors [76, 77]. The small volume of analytes and reagents required, high-throughput nature, portability, real-time detection, low cost, increased specificity and sensitivity, lower energy consumption, and parallel analysis of multiple analytes on one platform are all potential benefits of biosensors that incorporate microfluidics [71]. These sensors can also be integrated with electrochemical and optical transduction systems. Sample preparation, mixing, analysis, and signal readout can be accomplished on a single microfluidic device [78]. A simple microfluidic nanobiosensor is depicted in Fig. 2C. Materials such as glass, silicon, and polymers like polymethylmethacrylate and polydimethylsiloxane are commonly used for the fabrication of these device substrates. The use of nanobiosensors and microfluidic systems to create robust analytical tools represents a significant step forward in the development of self-testing methods that could positively impact healthcare in both developing and developed nations [79].
Nanopore-based nanobiosensors
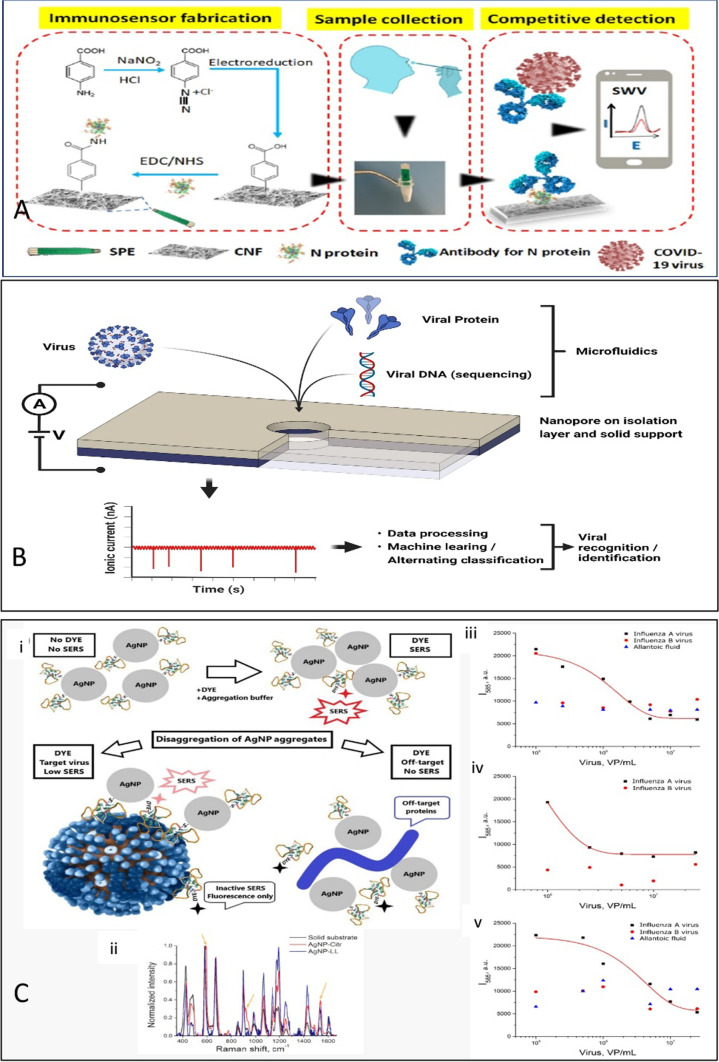
The nanopore detection of viruses is another rapidly evolving field. While numerous studies have described the application of biological nanopores for viral analyses, the emphasis here is mainly on virus identification via the nanopore-based sequencing of nucleic acids. Nanopores act as biosensors for a whole viral particle, but can also be used to detect and differentiate among distinct viruses in a label-free manner with portable low-cost devices (Fig. 3; for a recent comprehensive review, see Akhtarian et al. [80]). In fact, the use of solid-state nanopores appears to be increasingly successful in the detection of viral particles and diagnosis of viral diseases.
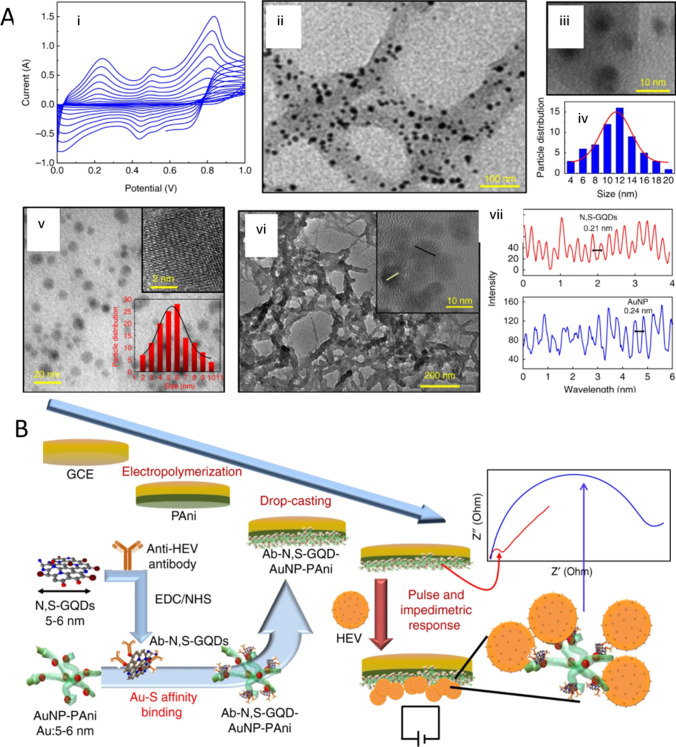
Fig. 3.
A Characterizations of polyaniline deposition, N,S-GQDs and Au-PAni preparation and N,S-GQDs@AuNP-PAni nanocomposites: (i) cyclic voltammograms of electropolymerized PAni film on the GCE electrode, (ii) TEM image of AuNP-PAni nanocomposites, (iii) high magnification of AuNP on the PAni chain, (iv) size distribution of the AuNPs inside the AuNP-PAni nanocomposites, (v) TEM image of N,S-GQDs (inset: HRTEM image of an isolated N,S-GQD and the size distribution), (vi) TEM image of N,S-GQDs@AuNP-PAni nanocomposites (inset: HRTEM of a small area), and (vii) fringe patterns of N,S-GQDs and AuNP from the HRTEM image of N,S-GQDs@AuNP-PAni nanocomposites. B Schematic diagram of the Ab-N,S-GQDs@AuNP-PAni nanocomposite-loaded sensor electrode and its electric pulse-induced impedimetric sensing of HEV (Creative Commons Attribution 4.0). Reprinted from [90] with permission from Nature Communications
Application of nanobiosensors in viral diagnostics
Nanobiosensors have tremendous potential in revolutionizing the landscape of diagnostic methods of viral infections. The key applications of different nanobiosensor-based approaches are stated below.
Electrochemical nanobiosensors in viral diagnostics
Recently, a variety of electrochemical nanobiosensors have been developed for viral detection [81–84]. Screen-printed electrodes (SPE) allow for the production of disposable sensors while also eliminating the disadvantages of traditional electrochemical sensors, such as electrode fouling and the memory effect [52]. Bialobrzeska et al. [85] compared the ability of screen-printed gold electrodes (SPGE) to detect the respiratory syncytial virus with that of reusable glassy carbon disc electrodes (GCDE). In SPGE, the distribution of gold on the electrodes was achieved through 4-aminothiophenol and glutaraldehyde linkers. The detection limit of the SPGE was measured using electrochemical impedance spectroscopy and was found to be three orders of magnitude lower than that of the GCDE. The sensitivity of SPGE was 3.15 × 10–5 pfu/mL, whereas the GCDE had a sensitivity of 2.36 × 10–6 pfu/mL. The higher sensitivity of SPGE was a result of the increased density of respiratory syncytial antibody coverage on the electrode surface, which was achieved through modification.
A novel electrochemical sensor was developed by Layqah et al. [50] electrodepositing GNPs on a disposable 8-channel carbon electrode array for the multiplexed detection of the Middle East Respiratory syndrome coronavirus (MERS-CoV). In this study, recombinant spike protein S1 was used as a biomarker for the detection of MERS CoV. The carbon electrode array enables multiplexed detection of different coronaviruses. The electrochemical measurements were recorded using square wave voltammetry using ferrocyanide/ferricyanide as a probe. This method was successfully applied to spiked nasal samples, and found to be highly selective, a single-step process, sensitive and accurate in detection. Furthermore, the increased number of electrodes in the chip allows for high-throughput screening, which reduces the overall cost and duration of the test.
A nanoporous gold platform for hepatitis B virus (HBV) detection was developed by Ahangar and Mehrgardi [86]. The porosity of the nanoporous gold was around 70 nm, with a standard deviation of roughly 8.9%, and its detection limit was 5 cycles/10–14 mol. Similarly, Rahmati et al. [87] developed a porous 3D N–C@NiCo2O4 nanowire that was used for detecting the hepatitis C virus (HCV) in conjunction with an HCV core antigen aptamer, yielding a detection limit of 0.16 fg/mL. Because of the porous structure, the active surface area of the nanosystem was increased, and the hydrothermal method was used to synthesize nanowires based on the morphology of sea urchins.
Nanocomposites, especially carbon-based materials combined with nanoparticles, are excellent materials for the fabrication of electrodes for electrochemical detection. Gold electrodes covered with a GO polymer composite can be used as sensors for the detection of dengue virus using electrochemical impedance spectroscopy, as reported by Navakul et al. [88]. In this study, the gold electrodes had a detection limit of 0.12 pfu/mL, and the charge transfer resistance had a linear correlation with virus concentrations ranging from 1 to 2 × 103 pfu/mL DENV. Another nanocomposite was developed by Palomar et al. [89] using multi-walled carbon nanotubes (MWCNT) and a GNP nanocomposite deposited on the gold electrode surface for the detection of dengue virus. The redox peak current intensities were in direct proportion with the electron exchange. Ferri/ferrocyanide (Fe (II/III)) was used as a signal reporter. After the electrodeposition of GNPs, the cathodic current increased from 5.1 × 10–5 A to 8.7 × 10–5 A. When antibodies were immobilised, the redox peak current of Fe (II/III) decreased from 8.7 × 10–5 A to 3.1 × 10–5 A. The electrochemically active area of the glass electrode (GE) increased by nearly 30-fold after the incorporation of MWCNT (GE/MWCNT), and it was 10-times higher in GE/MWCNTs/GNP than in GE/MWCNTs. The orientation of the immobilised antibodies affected their activity, but the three-dimensional structure of the porous network of MWCNTs and GNPs facilitated the antibody–toxin reaction. As a result, very minor changes in concentration could be recorded and a very low limit of detection was achieved.
A glassy carbon electrode (GCE) surface composed of nitrogen and sulphur co-doped GQDs and gold-embedded polyaniline nanowires with a pulse-triggered electrochemical sensor was developed for the detection of Hepatitis E virus (HEV) [90]. This nanocomposite was created using the interfacial polymerization and self-assembly processes, and it could enhance electrochemical activity and conjugate antibodies with edge carboxylic groups. The preparation of the nanocomposite-loaded electrode and the mechanism of HEV detection are depicted schematically in Fig. 4A. Similarly, Ghanbari et al. [91] developed an electrochemical aptasensor based on GQDs coated onto a GCE for HCV detection. These GQDs allowed better aptamer absorption on the electrode surface, providing a lower detection limit of 3.3 pg/mL.
Fig. 4.
A Schematic representing the Cotton-Tipped Electrochemical Immunosensor for COVID-19. Reprinted from [94] with permission from American Chemical Society. B Schematic sketch of nanopore biosensing of viruses and viral components. Viral components like proteins can be determined by use of nanopores by applying additional recognition elements like aptamers, viral nucleic acids by (mainly biological) nanopores. Whole virus particles can be identified by similar size nanopores and characteristic signal pattern. Sample concentration and pre-treatment can be integrated into microfluidic units. Electrical signals generated by passing nanopores are processed and can be analyzed by data analysis and statistics software tools for analysing high dimensional data and distinct virus particles (shape, size, rigidity) can be identified. C (i) Schematic representation of SERS based aptamer-functionalized AgNP for influenza virus A detection. (ii) SERS spectra of BODIPY FL dye onto substrate, aggregates of AgNP-citrate and AgNP-LL (iii–v) Concentration dependencies of SERS signal intensity of BODIPY FL for different experimental setups. Allantoic fluid was diluted to the same concentration as influenza A virus (Creative Commons Attribution License). Reprinted from [99] with permission from MDPI
Al-Douri et al. [92] proposed another nanocomposite combination, an aluminium nanoparticle-doped ZnO nanostructure, for the detection of dengue serotype 2. The nanocomposite was embedded in a p-silicon wafer, into which a silver interdigitated electrode (IDE) was integrated. Consequently, the limit of quantification reached 51.53 μA nM−1, with a sensitivity of 55.54 μA nM−1 cm−2. Another technique involved employing diazonium as a mediator to immobilise the AgNPs that had been functionalized with antibodies on the graphite pencil electrode. The increase in the faradic current with AgNP oxidation was proportional to the NS1 concentration. The proposed method had a detection limit of 0.5 ng/mL [93]. The use of a needle-like quaternary alloy Cu2CdSnS4 (CCTS) nanostructure deposited on a silicon dioxide (SiO2) substrate to detect dengue DNA serotype-2 in real time was described by Odeh et al. [21]. Spin coating and annealing were used to deposit the CCTS nanostructures on the substrate. As a result, a detection sensitivity of 24.2 μA nM−1 cm−2 and a quantification limit of 56.3 nM were achieved. Eissa et al. [94] established a new type of electrochemical immunosensor with cotton-tipped electrodes, as shown in Fig. 4B. By covering the SPE with absorbing cotton padding, sample collection and detection could be achieved on a single platform. After the CNF and antigens had been deposited on the SPCE, the tapering edge of the electrode was tethered with a bit of cotton fibre to obtain the cotton-tipped electrode. A portable potentiostat connected to a smartphone could be used for electrochemical detection and signal output. To consolidate, a list of nanomaterials employed in recently developed electrochemical nano sensors for virus detection is provided in Table 1.
Table 1.
Electrochemical detection of various viruses using nanomaterials
| Nanomaterial | Nanomaterial size | Analyte | Biorecognition element | Samples | Linear range | Limit of detection | Detection range | Label type | References |
|---|---|---|---|---|---|---|---|---|---|
| GNP | – | Respiratory Syncytial Virus | Anti-RSV antibodies | Virus containing samples | 1.0 × 10–1.0 × 107 pfu/mL | 1.10 × 103 pfu/mL | 0–1.0 × 107 pfu/mL | Label free | [85] |
| Array of carbon electrodes modified with GNP | 50 nm | MERS-CoV | MERS-CoV recombinant spike protein | Spiked nasal sample | 0.001–100 ng/mL | 1.0 pg/mL | 0.001–10,000 ng/mL | Label free | [50] |
| Nanoporous gold platform | – | Hepatitis B virus | Capture DNA | Human serum plasma | 0.4–10 nmol | 10 pmol | – | Label | [86] |
| GO reinforced polymer | 500 ± 250 nm | Dengue virus | DNA oligomers | Virus containing sample | 1–2 × 103 pfu/mL | 0.12 pfu/mL | 0–2000 pfu/mL | Label free | [88] |
| CNF-GNP | CNF-101 nm, GNP-10.1 nm | SARS-CoV-2 | Aptamer specific to SARS-CoV-2 RBD domain | Human saliva samples | 0.01–64 nM | 7 pM | – | Label free | [163] |
| GQD and gold-embedded polyaniline nanowires | GQD-5–6 nm, GNP-6–14 nm, Polyaniline nanowires-50–70 nm | Hepatitis E virus | Anti-HEV antibody | HEV like particles, human serum and fecal specimens of HEV-infected monkey | 1 fg/mL to 100 pg/mL, 102–107 RNA copies/mL | 0.8 fg/mL, 96.7 RNA copies/mL | – | Label free | [90] |
| GQD | – | Hepatitis C virus | Aptamer specific to HCV | Human serum samples | 10–70 pg/mL and 70–400 pg/mL | 3.3 pg/mL | – | Label free | [91] |
| AgNP | 45–60 nm | Dengue NS1 | Dengue NS1 antibody | NS1 spiked human serum samples | 3–300 ng/mL | 0.5 ng/mL | – | Label | [93] |
| Aluminium NP doped zinc oxide nanostructures | Aluminium NP-70 nm | Dengue serotype 2 | DNA probe | Complementary DNA probe | – | 16.9 nM | – | Label free | [92] |
| Needle-like Cu2CdSnS4 alloy nanostructure | – | Dengue serotype-2 | Dengue-specific DNA probe | – | – | 17 nM | 100 fM to 10 nM | Label free | [21] |
| 3D N–C@NiCo2O4 NWs | – | Hepatitis C virus | Hepatitis C virus core antigen (HCV) aptamer | Biological samples | 0.5 fg/mL to 0.12 pg/mL | 0.16 fg/mL | – | – | [87] |
| Cotton tipped electrode | – | SARS-CoV-2 N protein | SARS-CoV-2 Nucleocapsid Antigen | Nasopharyngeal swabs | 1–1000 ng/mL | 0.8 pg/mL | – | Label free | [94] |
GNR Gold nanorods, DNA Deoxyribonucleic acid, GNP Gold nanoparticles, RSV Respiratory syncytial virus, MERS Middle east respiratory syndrome coronavirus, GO Graphene oxide, CNF Carbon nanofiber, SARS-CoV Severe acute respiratory syndrome coronavirus, RBD Receptor binding domain, QD Quantum dots, HEV Hepatitis E virus, HCV Hepatitis C virus, AgNP Silver nanoparticles, NS1 Non-structural protein 1, ssDNA Single stranded DNA, HIV Human immunodeficiency virus, NP Nanoparticles
Optical nanobiosensors in viral diagnostics
The chemical stability, versatility, and unique optical propertiaes of GNPs, including LSPR, enable improved optical biosensing. Fu et al. [63] developed a lateral flow assay (LFA) combined with SERS for HIV detection using GNPs conjugated with malachite green isothiocyanate. This colour-based POC diagnostic device could detect concentrations as low as 0.24 pg/mL using a Raman instrument reader. Various nanomaterials such as GNPs, silver nanostructures, and rGO-polyamidoamine (PAMAM) dendrimers have been used in optical sensing for dengue virus detection. Yrad et al. [95] developed a portable strip-based assay using dextrin-capped GNPs for the easier detection of dengue-1 RNA within 20 min. The probes used in this study included a GNP-labelled DNA reporter probe, a dengue-1 specific DNA capture probe (test line), and a complementary DNA probe (control line). Human serum samples were used for sensor validation, and the detection limit was found to be 1.2 × 104 pfu/mL. Subsequently, dengue virus type-2 E protein was detected using SPR by depositing an rGO/PAMAM dendrimer on the substrate. This method provided a sensitivity, dissociation constant, and lower limit of detection of 0.25762 pM, 0.1496 pM, and 0.08 pM, respectively [96].
A chemiluminescent aptasensor that uses magnetic separation and surface-modified GNPs to detect concentrations as low as 0.05 ng/mL has been proposed [97]. Gold, iron oxide, and SiO2 NPs were combined to create a nanocomposite that was used to immobilize an HBsAg-specific aptamer for rapid magnetic separation, as well as double functionalized GNPs for signal enhancement. Chen et al. [98] improved the sensor by combining SERS with a three-dimensional nano-popcorn plasmonic substrate containing a gold layer. During the interaction of the DNA aptamer with the influenza A virus subtype H1N1, the Raman peak intensity decreased as the Cy3-labeled aptamer was released from the substrate. Consequently, the mapping image changed colour from bright yellow to dark orange with an increase in virus concentration. For specific recognition of the Influenza A virus, a SERS-based aptasensor with colloidal AgNPs was developed by Gribanyov et al. [99]. The SERS signal increased as the virus interacted with the aptamer. This aptasensor had a dynamic range of 2 × 105–2 × 106 VP/mL and a limit of detection of 2 × 105 VP/mL. A detailed schematic diagram of the SERS-based influenza A virus detection system is shown in Fig. 4C.
An LFA technique was developed by Liu et al. [100] for detecting influenza virus H3 using GNP-coated polystyrene latex microspheres (PLM). Monoclonal antibodies have been used as linkers between GNPs and PLM to prevent non-specific binding because both the particles are negatively charged. Antibodies are more readily conjugated on the surface of GNPs due to their large surface area, and latex microspheres are tunable. When both these agents are used in an appropriate ratio of 16:1 (GNP:PS), the sensitivity increases. This method was used to yield a qualitative detection limit of 1/16 hemagglutination units (HAU) and a quantitative detection limit of about 0.016 HAU. The detection limit of the bare 10-nm GNP-based LFA was 4 HAU, while that of GNP-PS was 1/16 HAU. Hence, it was 64 times more sensitive than the bare 10-nm GNP LFA. A magnetic/plasmonic-assisted fluoroimmunoassay was developed using magnetic-derivatized molybdenum trioxide QDs, which have plasmonic properties. Graphitic carbon nitride QDs were used as the detection probe because of their high fluorescence properties. This technique was tested in clinical samples, and it detected concentrations as low as 45 pfu/mL. Moreover, it had a sensitivity of around 0.25 pg/mL and 0.9 pg/mL in deionized water and human serum containing influenza virus [101]. A GNP–magnetic NP hybrid nanocomposite with CdSeS QDs was prepared by Takemura et al. [102]. The hybrid nanocomposite was used to separate the virus from impurities using a magnetic field induced by the LSPR phenomenon. This phenomenon is significant because it can enhance or quench the fluorescence of QDs, and the intensity of the fluorescence is proportional to the distance between GNPs and QDs. Similarly, GNPs were combined with fluorescent inorganic CdZnSeS/ZnSeS QDs for the development of an LSPR-based nanobiosensor [103]. When the target virus was present, the antibody and antigen created a steric hindrance due to dual antibody anchoring sites in the peptide sequence. This restricted LSPR, resulting in quenching, which was proportional to the concentration of the influenza virus.
Murine norovirus was detected using an optical transduction-based colorimetric method and an ultrasensitive nanozyme aptasensor, which had a detection limit of 3 viruses per assay, equivalent to 30 viruses/mL [104]. In this method, an enzyme that mimics the catalytic activity of GNPs with aptamers was used to convert a colourless substrate into a coloured product. Nanozyme activity was recovered due to the high-affinity AG3 aptamer in the presence of norovirus, causing aptamer desorption. This exposed the catalytic sites on the surface of GNPs, allowing tetramethylbenzidine (TMB) oxidation and the generation of a blue product. The Kd value between the AG3 aptamer and the GNPs was 1.85 × 10–8 M, indicating that this aptamer had a higher binding affinity to murine norovirus. A colourimetric aptasensor was also developed for the detection of human papillomavirus (HPV) using GNPs and an RNA aptamer with a hairpin structure against the HPV16 L1 protein. Even in the presence of ppb levels of protein, if salt was added, the GNP and aptamer aggregated. HPV16 L1 protein levels as low as 9.6 ng/mL could be detected [105].
Rodriguez-Moncayo et al. [106] developed a high-throughput, semi-automatic microfluidic device based on antibodies that react against four SARS-CoV-2 proteins: the spike protein, S1 subunit, receptor binding domain, and nucleocapsid protein. With a sensitivity of 95% and specificity of 91%, the device could analyse dozens of samples in parallel at a minimum volume of ~ 6 μL per serum sample. This advancement paved the way for more low-cost and large-scale screening. A single-step colourimetric nanobiosensor in which GNPs interacted with SARS-CoV-2 in nasal and throat swabs was developed by Ventura et al. [107]. In this device, GNPs functionalized with antibodies targeting three surface proteins present in SARS-CoV-2 (spike, envelope, and membrane) at a ratio of 1:1:1 underwent a red shift in the presence of virus particles. To consolidate, the list of nanomaterials employed in the recent development of optical sensors for viral detection is provided in Table 2.
Table 2.
Optical detection of various viruses using nanomaterials
| Nanomaterial | Nanomaterial size | Analyte | Biorecognition element | Method employed | Samples | Linear range | Limit of detection | Detection range | Label type | References |
|---|---|---|---|---|---|---|---|---|---|---|
| GNP | 30–40 nm | HIV-1 | DNA Oligonucleotides | SERS based LFA assay | HIV-1 DNA in buffer samples | 8–64 ng/mL | 0.24 pg/mL | 0–64 ng/mL | Label | [63] |
| GNP | 10 nm | Dengue-1 RNA | DENV probe | LFA | Human sera | 0.01–0.06 µM | 1.2 × 104pfu/mL | – | Label | [95] |
| Au@Fe3O4@SiO2 NP | – | HBV | HBsAg-specific aptamer | Chemiluminescence | Human serum samples | 1–225 ng/mL | 0.05 ng/mL | – | Label | [97] |
| Au/polyethylene naphthalate nano-popcorn substrate | 64 nm | Influenza virus A | Influenza virus A specific aptamer | SERS | Clinical samples | – | 97 pfu/mL | 10–10000 pfu/mL | Label | [98] |
| GNP | 20 nm | Human papillomavirus | RNA aptamer against HPV16 L1 protein | Colorimetric | Clinical samples and vaccine samples | 9.6–201.6 ng/mL | 9.6 ng/mL | – | Label | [105] |
| AgNP | 4, 10 nm | Influenza virus | Aptamer specific to influenza virus | SERS | Samples containing virus | – | 2 × 105 VP/mL | – | Label | [99] |
| GNP coated polystyrene latex | 10 nm, 208 nm | Influenza virus H3 subtype | Anti-influenza virus mAb1 | LFA | Virus containing samples diluted in buffer | 1/32–32 HAU | 0.016 HAU | – | Label | [100] |
| CdZnSeS/ZnSeS QD and GNP | 5 ± 0.5 nm and 28.4 ± 1.5 nm | Influenza virus | Anti-HA antibody (Ab) against influenza virus | LSPR | Serum media | 10−14–10−9 g/mL | 65.1 fg/mL | – | – | [103] |
| rGO-PAMAM Dendrimer | – | Dengue Virus Type 2 E-Protein | Antibodies specific to DENV E-proteins is | SPR | Recombinant dengue virus type 2 E-proteins | – | 0.08 pM | 0.08–0.5 pM | Label free | [96] |
| GNP and magnetic NP hybrid nanocomposite with CdSeS QD | GNP-14.8 nm, Magnetic NP-40 nm, | Norovirus | Anti-norovirus genogroup II antibody | LSPR-magnetoimmu-nofluorescence | Clinical samples of feces containing norovirus | – | 0.48 pg/mL | 1 pg/mL to 5 ng/mL | – | [102] |
| Plasmonic molybdenum trioxide QD and graphitic carbon nitride QD | 3–9 nm | Influenza virus | Antibody against influenza A virus | LSPR-magnetoimmuno-fluorescence | Clinically isolated influenza virus A/Yokohama (110/2009) (H3N2) | – | 45 pfu/mL | 45–25,000 pfu/mL | – | [101] |
GNP Gold nanoparticles, HIV Human immunodeficiency virus, DNA Deoxyribonucleic acid, SERS Surface enhanced Raman scattering, LFA Lateral flow assay, GaN Gallium nitride, Au Gold, Ag Silver, SiO2 Silicon dioxide, Hbs Hepatitis B, DENV Dengue virus, SARS-CoV-2 Severe acute respiratory syndrome corona virus-2, LSPR Localised surface plasmon resonance, NS1 Non-structural protein 1, RNA Ribonucleic acid, HPV Human papilloma virus, AgNP Silver nanoparticles, QD Quantum dots, SPR Surface plasmon resonance, rGO Reduced graphene oxide, PAMAM Polyamidoamine, NP Nanoparticles, RBD Receptor binding domain, HAU Hemagglutination unit
Microfluidic nanobiosensors in viral diagnostics
Lum et al. [108] created an electrochemical impedance-based aptasensor integrated with a microfluidic chip to detect the H5N1 avian influenza virus. The microfluidic chip was covered with gold-coated interdigitated microelectrodes, and a detection limit of 0.0128 HAU was achieved. For the detection of norovirus [109], Chand and Neethirajan utilized a microfluidic chip integrated with a graphene-GNP composite deposited on an SPCE. This nanocomposite of graphene-GNP provided a better substrate for immobilization and enabled excellent electron transfer at the interface. The interaction between norovirus and the ferrocene-labelled aptamer resulted in a reduced electrochemical signal when the nanocomposite was coated onto the, resulting in a norovirus detection range of 100 pM to 3.5 nM.
Another group of researchers [110] described the application of optical transduction techniques for semi-quantitative analysis in order to detect the p24 antigen using a fully integrated multicolour immunosensor. This system simultaneously combined two-step reactions in a single microfluidic chip to achieve the horseradish peroxidase (HRP)-linked immunoassay and GNR-based multicolour assay. This sensor had a qualitative visual detection limit of 0.5 ng/mL, as well as high sensitivity and low serum protein interference. Other researchers used carbon dots with fluorescent labels that have a high quantum yield and low toxicity. Chunduri et al. [24] developed a microfluidic carbon dot sandwich immunoassay with a detection range of 20–1000 pg/mL, providing a 100-fold increase in detection over traditional colorimetric assays. This technique could be multiplexed to detect other pathogens, such as those causing tuberculosis and hepatitis. A POC device with a broad linear range and high specificity, selectivity, and sensitivity was created by Kaminska et al. [64] by combining SERS and microfluidics for the detection of the hepatitis virus. In their study, antibodies (anti-HBsAg) covalently linked to fuchsin (Raman reporter)-labelled gold nanoflowers served as the biosensing element, and the substrate was made up of Au–Ag-coated gallium nitride (GaN). The detection limit for HBsAg antigens could be increased to 0.625 IU/mL. In addition, the presence of antibodies against the SARS-CoV-2 spike protein was detected in diluted human plasma using an opto-microfluidic sensing platform based on LSPR developed by Funari et al. [30]. The electrodeposition technique was used to fabricate a substrate with gold nanospikes. The local refractive index shifts in the gold nanospikes caused by biomolecule binding events cause a redshift proportional to the target antibody concentration.
Suthanthiraraj et al. [22] exploited the silver nanostructure-based LSPR effect to detect dengue NS1 antigens in whole blood samples. These nanostructures were formed through the thermal annealing of thin silver films onto a silicon substrate at 200 °C for 1 h. Silver nanostructures were chosen for this study because of their intrinsic ability to produce huge wavelength shifts and the wide differences in the real part of the dielectric constant within the visible range. The sensor substrate was coupled with a blood plasma separation platform to create a lab-on-chip device for quick detection, providing a sensitivity of 9 nm/(g/mL). In another study, the human angiotensin-converting enzyme 2 protein was used as a biorecognition element in an LSPR-based sensor with AgNT [36]. It was tested against the SARS-CoV-2 spike RBD protein and CoV NL63 virus and could detect concentrations as low as 0.83 pM and 391 pfu/mL, respectively. The list of nanomaterials employed in the recent development of microfluidic technique-based virus detection is illustrated in Table 3.
Table 3.
Microfluidic based detection of various viruses using nanomaterials
| Nanomaterial | Nanomaterial size | Analyte | Biorecognition element | Method employed | Samples | Linear range | Limit of detection | Detection range | Label type | References |
|---|---|---|---|---|---|---|---|---|---|---|
| Graphene-GNP composite | GNP-16 nm | Norovirus | Norovirus viral capsid-specific aptamer | Electrochemical | Spiked blood samples | – | 100 pM | 100 pM to 3.5 nM | Label free | [109] |
| Gold nanoflowers/Au–Ag coated GaN | 20–40 nm/90 nm | Hepatitis B virus | Anti-HBs Ag | SERS | Human blood plasma | 0.0125–60 IU/mL | 0.01 IU/mL | 0–625 IU/mL | Label | [64] |
| Gold spikes | – | SARS-CoV-2 | Anti-SARS-CoV-2 spike protein antibodies | LSPR | Plasma samples | – | 0.08 ng/mL | 0.1–10000 ng/mL | Label free | [30] |
| Silver nanostructures | 20–80 nm | Dengue NS1 | Anti-NS1 antibody | LSPR | Whole blood spiked with NS1 antigen | – | 0.06 µg/mL | 0–50 µg/mL | Label free | [22] |
| Silver nanotriangle | Side length-152 ± 3 nm height-60 ± 1 nm | SARS-CoV-2 | Human angiotensin-converting enzyme 2 protein | LSPR | SARS-CoV-2 spike RBD protein and CoV NL63 virus | 2.03 pM to 9420 pM | 0.83 pM, 391 pfu/mL | 1 pM to 104 pM | Label free | [36] |
GNP Gold nanoparticles, SERS Surface enhanced Raman scattering, Au Gold, Ag Silver, Hbs Hepatitis B, SARS-CoV-2 Severe acute respiratory syndrome corona virus-2, LSPR Localised surface plasmon resonance, NS1 Non-structural protein 1
Nanopore-based biosensors in viral diagnostics
Mc Mullen and colleagues [111] described the primarily voltage-independent passing of a stiff filamentous virus (880 nm long and 6.6 nm wide) through a solid-state membrane. The Filoviridae Marburg and Ebola viruses fulfil these requirements. While the current was not the driving force, the electric field helped align the virus to the nanopore. Similarly, the translocation of a rigid rod-shaped virus, a tobacco mosaic virus, through a solid-state nanopore was described in a paper by Wu et al. [112]. This study reported methods to determine the rigidity of (bio)material in general using solid-state nanopores. In a recent paper, data analysis was applied in combination with solid state nanopore analysis [113]. The authors highlighted the potential of solid-state nanopores in viral diagnostics through the detection and quantification of whole virus particles.
In addition to whole viruses, viral biomarkers have also been examined, and single-molecule detection of the nucleocapsid protein 7 (NCp7) from the HIV-1 virus has been performed using synthetic nanopores, specific aptamer–protein interactions, and the resistive-pulse technique [114]. Surface modification with solid-state nanopores has been applied to selectively detect viruses by exploiting the specific molecular interactions between recognition probes on the surface and target particles. This strategy has been adopted for selective single-virus identification [115]. Hemagglutinin antibody-mimicking oligopeptides with a weak affinity to influenza A virus have been utilized for functionalizing the pore wall surface, thus enabling specific virus–nanopore interactions. Such viral ligand binding led to an alteration in viral translocation dynamics in the nanochannel. Such a modification approach allowed the flexible introduction of specific interactions, and thus, the recognition and differentiation of distinct viruses and bacteria too. Along these lines, Taniguchi et al. [116] found that, by using nanopores in combination with artificial intelligence, coronaviruses of similar size could be identified. This could allow discrimination among coronaviruses such as HCoV-229E, SARS-CoV, MERS-CoV, and SARS-CoV-2. Moreover, this technique enabled the successful detection of SARS-CoV-2 in saliva. Together, solid-state virus immunosensing techniques hold promise in providing versatile, flexible, and cost-effective diagnostic tools in the future, particularly in combination with sophisticated data analysis, microfluidics, and chemical ingenuity.
Internet of medical things and artificial intelligence in viral biosensors
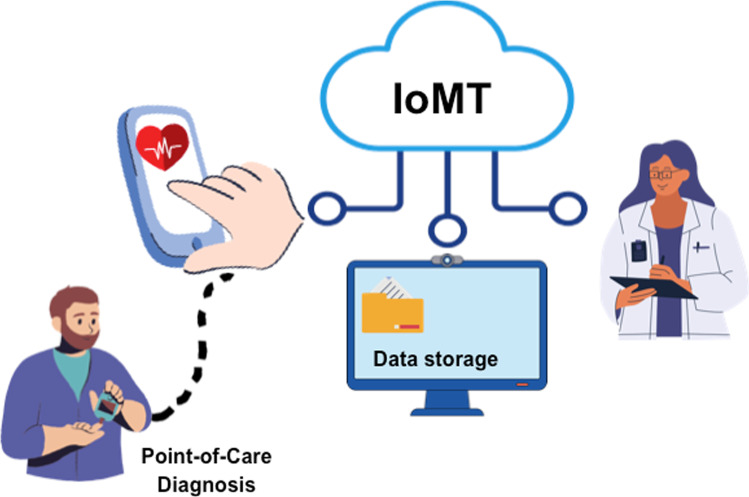
The Internet of Things (IoT) is a rapidly evolving interdisciplinary domain that integrates computer hardware, software, other electronic devices, and physical objects, both living and non-living, across a network. Numerous IoT-enabled services are being experimented with in healthcare, connecting patients to healthcare units remotely [117]. This IoT network, known as the Internet of Medical Things (IoMT), is a rapidly evolving area in which patients and doctors are communicating with each other through a series of medical devices with wireless connectivity [118]. A rapid and accurate screening of health conditions represents a key step in order to identify the sign of symptoms of an infection disease although its effect did not come forward. However, the real-time identification of viral infections is difficult and expensive to manage within traditional healthcare settings due to their high response time, the need for qualified personnel, as well as the cost per analysis. In view of this consideration, the healthcare industry is striving toward extending the accuracy, reliability, and productivity of biosensor-based POC devices. These diagnostic tools integrated with IoMT capacities can help in the screening, providing effective medical treatment, and most importantly, offers control over epidemic outbreaks [119, 120].
Smartphones have a wide range of applications for biosensors due to their popularity, portability, versatility and wireless communication technology that allows the connection to cloud data storage systems and IoT networks for collecting and sharing medical analysis data [121] Fig. 5. Moreover, smartphone-based biosensors are attractive to researchers because they can easily enable both qualitative and quantitative analysis of the sample in real time using a smartphone application that can perform the measurement of colorimetric, fluorescent, reflection-based, current, and turbidity signals [122, 123]. They are able to control the recognition process, receive recognition data through various interfaces such as Bluetooth, camera, audio jack, and micro-USB port, and display recognition results [124, 125]. Therefore, these features make smartphone-based devices ideal for developing diagnostics for virus detection that can be performed outside of the clinical laboratories.
Fig. 5.
Scheme of Internet of Medical Things combined with smartphone-based platforms for POC diagnostic applications
An OFF–ON biosensors for detection of H1N1 based on the interaction of QD-aptamer beacons with three-dimensional light guides photonic crystal was proposed from Nuree Lee et al. [126]. High sensitivity with LOD of 138 pg and high mL−1 and selectivity over other species of influenza A virus and biomolecules was obtained. The target virus was detected with a low-cost and portable home-made setup coupled with smartphone.
Recently, paper-based biosensors coupled to smartphones as transducers for rapid virus detection have gained much attention as a useful tool for rapid, easy, affordable, and accurate POC. Teengam et al. [127] developed paper-based analytical device for the early diagnosis of HCV using a highly specific pyrrolidinyl peptide nucleic acid (acpcPNA) probe. The acpcPNA was covalently immobilized onto oxidized cellulose paper via reductive alkylation between the aldehyde and amine groups. The detection occurred by monitoring the fluorescence signal response of a fluorescent dye that selectively binds the single-strand region of the DNA target over the PNA probe using a smartphone camera. The obtained LOD was 5 pmol−1.
An interesting miniaturized paper-based smartphone immunosensor for differential diagnosis of wild-type pseudorabies virus (PRV) infection versus vaccination immunization was proposed by Yong Tang et al. Latex beads were used to label PRV, and the test line (T-line) was coated with PRV gE monoclonal antibody (PRV gE-mAb). The smartphone was used to measure the transmitted light intensity from the T-line achieving excellent sensitivity and selectivity [128].
Although smartphones perform the same data collection, processing and decision tasks like a computer, they have some limitations. First, functionality of each smartphone app is independent of the other apps. In addition, more attention should be given to data security because the smartphones hold personal information.
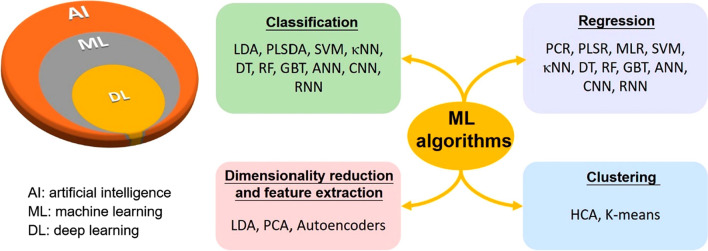
In some biosensors, a large quantity of data is rapidly generated as output. The analysis of these data requires additional processing by an experienced user, making the process error prone. Moreover, manual data processing is time-consuming, greatly reducing the efficiency of the biosensor. In the past years, numerous chemometric methods such as principal component analysis or regression (PCA or PCR), linear discriminant analysis (LDA), multiple linear regression (MLR), partial least-squares discriminant analysis or regression (PLSDA or PLSR), hierarchical clustering analysis (HCA), and their combination were applied in the field of biosensor technology in order to improve the quality and accuracy of clinical information. In the last decade, an increasing number of studies in the field of AI and ML have indicated the growing interest and scope of its use in this area for their ability to interrogate appropriate nonlinear dependencies for complex biological samples, offering unparalleled opportunities to address pressing biosensors challenges. ML algorithms for processing data are emerging, such as κ-nearest neighbour (κNN), support vector machine (SVM), Naïve Bayes (NB), decision tree (DT), gradient-boosted trees (GBT), random forest (RF), feedforward artificial neural network (Feedforward ANN), recurrent neural network (RNN) and convolutional neural network (CNN) are investigated to create the intelligent biosensors that can be easily integrated into the IoMT (Fig. 6) [129–132]. AI-integrated biosensors combine hybrid techniques of wireless biosensing technology and advanced ML algorithms, holding great promise for realizing continuous health monitoring and cloud-connected POC diagnostics [133]. They can be of great importance in the prediction of infectious diseases in which early interventions can be lifesaving (Table 4). They can bridge the gap between data acquisition and analysis and achieve enhanced diagnostic and therapeutic accuracy [134]. Despite the limited number of commercial applications, continuous remote sensing using wearable such as glucose monitoring devices, oximeters, temperature sensors, and heart and respiratory rate monitors connected to an AI-based central computing device is revolutionizing patient care. In addition, ML can be a possible solution to overcome the challenges and obstacles faced by biosensor testing in complex samples [135]. Most biosensors were developed for target detection using body fluids such as blood or urine samples. Recently, the application of additional biological matrices such as nasopharyngeal swab, oral secretions and body sweat has increased significantly because the tests are non-invasive, safe, pain-free, and easily operable. However, many physiological and pathological factors can influence the composition of these body samples production, including age, drug use, hormonal conditions, psychological stature, and physical recreation. ML can support biosensors by increasing their reliability, accuracy (objective identification), specificity (pattern recognition) and sensitivity (single molecule detect).
Fig. 6.
Relationship between AI, ML, and DL, and various ML algorithms applied to Biosensors. CNN Convolutional neural network; DT decision tree; Feedforward ANN Feedforward artificial neural network; GBT Gradient-boosted trees; HCA Hierarchical clustering analysis; κNN κ-nearest neighbour; LDA Linear discriminant analysis; MLR Multiple linear regression; NB Naive Bayes; PCA or PCR Principal component analysis or regression; PLSDA or PLSR Partial least-squares discriminant analysis or regression; RF Random forest; RNN Recurrent neural network; SVM Support vector machine. Reprinted with permission from [129]. Copyright {2020} American Chemical Society
Table 4.
List of some AI-biosensors for viral diseases detection
| Device | Detection principle | Target | Limit of detection | Time (min) | References |
|---|---|---|---|---|---|
| Dengue fever | |||||
| NAAT | QUASR multiplexed RT-LAMP assay | RNA | 108–103 pfu/mL | < 40 min | [164] |
| IoT PCR | PCR | cDNA | – | 34 min | [165] |
| Influenza A | |||||
| Fluorescent probe based POC | Fluorescence and light guiding | H1N1 | 138 pg/mL | 40 min | [126] |
| Genosensor | Electrochemical | Hemagglutinin gene | 0.002 ng/6 μL | 30 min | [166] |
| Human immunodeficiency virus | |||||
| EGOFET | Electrochemical | HIV-1 p24 capsid protein | 1 fM | – | [167] |
| Coronavirus-2 | |||||
| Supersandwich-type biosensor | Electrochemical | SARS-CoV-2 RNA | 200 copies/mL | – | [168] |
| Liquid crystal film | Thermotropic Liquid | RNA-CoV2 | fM | 20 min | [169] |
| Sensors | Localized Surface Plasmon Resonance | SARS-CoV-2 virus particle | 125.28 vp/mL | ||
| Others | |||||
| Plasmon resonance probes | Dark-field microscope | Enterovirus A71 | 3 copies/μL | [132] | |
| Immunochromatographic strip | LFA | EBOV-GP1−649 | 200 ng/mL | 15 min | [170] |
| Impedimetric micro-immunosensor | Electrochemical | ZIKV protein | 10 pM | 40 min | [171] |
cDNA Complementary deoxyribonucleic acid, NAAT Nucleic acid amplification tests, QUASR Quenching of unincorporated amplification signal reporters, EGOFET Electrolyte-gated organic field-effect transistor, ELISA Enzyme-linked immunosorbent assay, LAMP Loop-mediated isothermal amplification, LFA Lateral flow assay, LFD Lateral flow dipstick, MCFA Microchannel capillary flow assay, RNA Ribonucleic acid, RPA Recombinase polymerase amplification, RT-LAMP Reverse transcription loop-mediated isothermal amplification, SARS Severe acute respiratory syndrome
During the COVID-19 pandemic, the IoMT, applications of AI and ML in POCs have drastically grown [136]. Due to the contagious nature of the virus governments-imposed lockdowns on cities to prevent the virus from spreading. Unfortunately, acquiring medical supplies made it necessary to come out of isolation, which compromised the effectiveness of quarantine efforts. Better outcomes for controlling the spread of infection and offering adequate healthcare to patients without putting others at risk, it was POCs use to monitor patient health at home and IoMT creation to share information with doctors and hospitals [136–138]. Biosensors have been incorporated into simple miniaturized analytical devices that enable SARSCoV-2 diagnosis, monitoring, and management with various analytical approaches [139–141].
A portable smartphone-based quantum barcode serological assay device for real-time surveillance of patients infected with SARS-CoV-2 was developed by Chan et al. Instantaneous results to inform patients, physicians, and public health agencies was obtained by appropriate app [142]. A liquid crystal-based diagnostic kit and a smartphone-based application to enable automatic detection of SARS-CoV-2 ssRNA was realized. The analytical tool was applied for reliable self-test at femtomolar concentrations of single-stranded ribonucleic acid (ssRNA) SARS-CoV-2 [143].
A Nanozyme linked immunochromatographic sensor integrated with optical devices for the detection of SARS-CoV-2 nucleocapsid protein has been developed. Immunoreaction and enzyme-catalyzed substrate colour reaction were carried out on the chromatographic strip in a device, of which the light signal was read by a photometer through a biosensor channel, and the data was synchronously transmitted via the Bluetooth to the app in-stored smartphone for reporting the result. A LOD of 0.026 ng/mL was achieved [144].
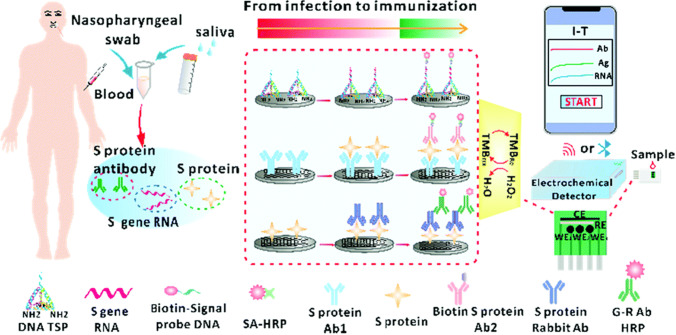
Multiplexing analysis has attracted researcher attention for clinical diagnosis because a number of diseases require analyse complex biological networks instead of analysing a single marker. Therefore, biosensors for multi-target analyses might facilitate infection screening and improve the rates of earlier detection and attendant improved prognosis were developed. Dou et al. designed a biosensor for co-detection of SARS-CoV-2 viral RNA, antigen, and antibody in combination with a smartphone. The online monitoring of SARS-CoV-2 virus-infected patients from infection to immunization was accomplished (Fig. 7) [145].
Fig. 7.
Scheme of electrochemical co-detection procedure for S gene RNA, S protein and S protein antibody of SARS-CoV-2 by sandwich approach. The biosensor is composed of three testing parts, each of which consists of a carbon working electrode (WE), a Ag/AgCl reference electrode (RE), and a carbon counter electrode (CE). Selective binding of different concentrations of SARS-CoV-2 biomarkers to surface-linked capture probes should produce the current change when the specific biomarker was present. The harvested current information was transmitted to the smartphone via wireless connections. The special APP was used for data analysis. Reprinted Chem. Commun., 2022, 58, 6108 [145]
The multiassay was applied in saliva samples for the detection of SARS-CoV-2. To increase the biosensors sensitivity, a paper-based immunoassay using magnetic beads to support the immune chain and 96-well wax-printed paper plate for colour background smartphone viewing in conjunction with the free-charge app was developed; a LOD of 0.1 μg/mL was obtained [146].
A multiplexed, colorimetric detection method was established for the detection of pathogens in wastewater samples to provide early warning of disease outbreaks. The developed method integrates on-chip nucleic acid extraction, two-step isothermal amplification, and colorimetric detection on a 3D-printed microfluidic chip. Colorimetric signals during nucleic acid amplification were recorded in real time and analysed by a programmed smartphone. The device exhibited potential for rapid spatiotemporal epidemiologic data collection regarding the environmental dynamics, transmission, and persistence of infectious diseases [147].
AI and ML biosensors are applied for detecting hidden disease signatures and for the management of COVID-19 [67, 140, 148–155]. It is known that early symptoms of SARS-CoV-2 infection overlap with other common conditions such as common cold and Influenza, making early screening and diagnosis are crucial goals for health practitioners. The parameters of the full blood counts can be analysed to distinguish the viral type at an earlier stage. Abhirup Banerjee et al. [150] successfully applied ML, artificial neural network and a simple statistical test to identify SARS-CoV-2 positive patients from full blood counts without knowledge of symptoms or history of the individuals. Moreover, AI is transforming medical practice and precision medicine in intensive care unit Safe, effective, efficient, and ethical clinical management of COVID-19 patients [151].
Despite efforts to identify proper new smart biosensors for intelligent healthcare based on the synergic integration of the IoMT, ML and AI for rapid and efficient selective SARS-CoV-2 diagnosis, research remains in its nascent stage. There is a clear need to increase highly sensitive non-invasive home-based diagnostic tools that mitigate testing and monitoring problems. By combining such devices with the IoMT and AI, a smart platform that provides timely patient care protocols could be developed and could help governmental organizations suitably allocate the apparatus and other necessities for viral disease management. This approach could help save numerous lives, provide economic benefits, and develop a plan for better managing the future risks caused by infectious diseases, conferring benefits across all levels of society.
Challenges and future perspectives
It is expected that commercially viable diagnostic tools based on nanomaterials that efficiently and cost-effectively perform multiplexed detection will become available in the foreseeable future. The miniaturisation of nanochip technology is going to be the future trend in diagnostics. The long-term outlook for nanobiosensors in disease diagnosis could result in high-volume sales and rapid adoption. However, there are some challenges associated with using biosensors today, such as the transformation of nanobiosensors from prototypes into commercial products. This is because field-scale trials are necessary to gauge and evaluate the effectiveness of nanobiosensors in practical settings, and user awareness of nanobiosensors is also crucial. End users may face real-time problems due to the integration and interrelationships of the numerous technologies involved in nano-diagnostics. They may expect minimally invasive procedures for sample collection and/or avoidance of liquid biopsy. In order to accomplish this, a nanoneedle could be used, and these are slowly advancing towards clinical adoption [156]. Simple nano patches that can be applied to the skin’s superficial surface could be developed as advanced tools for detection and diagnosis based on interstitial fluids exudated through skin pores. Additionally, the nanobiosensors developed ought to be biodegradable to prevent any environmental harm [157, 158]. Overall, the integration of wearable biosensors [159] and IoMT [160] along with nanotechnology could have a significant impact on healthcare in the future.
Currently, a few companies, including Roche, Nippon, Robert Bosch, and IBM, appear to be working towards the fabrication of nanobiosensors. Reports on commercial nanobiosensors are limited. Although there are some reports of commercial nanobiosensors being used in medical diagnostics and applications, there are still some limitations beginning with the high cost of fabrication, the requirement of automated testing, rapid result evaluation, and field trial validation, which forces the miniaturization of prototypes into the industry for production. Additionally, there is no market to compensate for and cover all of these costs. That could partly explain the dearth of commercial nanobiosensors. However, obtaining novel nanomaterials from leftover biomass could provide a more affordable option [161]. The versatility of nanobiosensors is another issue that requires more attention. More portable nanobiosensors may become commercially viable if a variety of nanomaterials for biosensing assays are developed [162]. In the future, nanotechnologies could represent a promising solution for molecular diagnostics, enabling POC diagnosis, and also for theranostics and the development of personalized medicine.
Conclusion
Nanotechnology has played a key role in the development of sensors for biomedical applications. Advances in nanomaterial synthesis and nanofabrication techniques have facilitated the development of innovative nanobiosensors for viral diagnostics. Integrative approaches for nanomaterial-based biosensors are vital, as traditional viral detection methods are time-consuming and expensive. Despite the range of their applications, nanobiosensors possess their own limitations, such as challenges in fabrication, sample preparation, substrate formation, bioreceptor immobilization, and appropriate substrate functionalization. These challenges must be overcome because they directly affect the sensitivity, reproducibility, detection limit, and selectivity of the nanobiosensors. The proper optimization of these parameters along with automation can significantly impact the development of highly sensitive nanobiosensors. This is an exciting time to be involved in the development of nanobiosensors, which should be designed in such a way that they are disposable and self-contained, allow remote sensing, and act as part of fully autonomous systems with interconnected sample processing and analysis in resource-constrained environments. Despite the great challenges, there are great expectations ahead.
Acknowledgements
This work was supported by, Sichuan Provincial Science and Technology Foundation (22NZZH0031), Medical Scientific Research Project of Chengdu City, China (2021043), Natural Science Foundation of Sichuan Province, China (2022NSFSC1510), ICTS “NANBIOSIS”, in particular by the Drug Formulation Unit (U10) of the CIBER in Bioengineering, Biomaterials and Nanomedicine (CIBER-BBN) at the University of the Basque Country (UPV/EHU) in Vitoria-Gasteiz, and National Research Foundation of Korea (2018K1A4A3A01064257 and F2018K1A4A3A01064257), Baden-Wuerttemberg Ministry of Economy, Labor and Housing, Germany (AsphyxDx project: 35–4223.10/17). The authors would like to thank all the reviewers and editorial members who participated in the review.
Abbreviations
- 3D
Three-dimensional
- Ab
Antibody
- Ag
Silver
- AgNPs
Silver nanoparticles
- AgNTs
Silver nanotriangles
- AI
Artificial intelligence
- Au
Gold
- CCTS
Cu2CdSnS4
- cDNA
Complementary deoxyribonucleic acid
- CNF
Carbon nanofiber
- CNT
Carbon nanotubes
- COVID-19
Coronavirus disease
- DENV
Dengue virus
- DNA
Deoxyribonucleic acid
- EGOFET
Electrolyte-gated organic field-effect transistor
- ELISA
Enzyme-linked immunosorbent assay
- GaN
Gallium nitride
- GCDE
Glassy carbon disc electrodes
- GCE
Glassy carbon electrode
- GE
Glass electrode
- GNP
Gold nanoparticle
- GNR
Gold nanorod
- GO
Graphene oxide
- H1N1
Influenza A
- HAU
Hemagglutination unit
- Hbs
Hepatitis B
- HBV
Hepatitis B virus
- HCV
Hepatitis C virus
- HEV
Hepatitis E virus
- HIV
Human immunodeficiency virus
- HPV
Human papilloma virus
- HRP
Horseradish peroxidase
- IDE
Interdigitated electrode
- IoMT
Internet of medical things
- IoT
Internet of things
- LAMP
Loop-mediated isothermal amplification
- LFA
Lateral flow assay
- LFD
Lateral flow dipstick
- LSPR
Localised surface plasmon resonance
- MCFA
Microchannel capillary flow assay
- MERS
Middle East respiratory syndrome coronavirus
- MERS-CoV
Middle East respiratory syndrome coronavirus
- ML
Machine learning
- MWCNT
Multi-walled carbon nanotubes
- NAAT
Nucleic acid amplification tests
- NCp7
Nucleocapsid protein 7
- NP
Nanoparticles
- NS1
Non-structural protein 1
- PAMAM
Polyamidoamine
- PLM
Polystyrene latex microspheres
- POC
Point-of-care
- PRV
Pseudorabies virus
- QD
Quantum dots
- QUASR
Quenching of unincorporated amplification signal reporters
- RBD
Receptor binding domain
- rGO
Reduced graphene oxide
- RNA
Ribonucleic acid
- RPA
Recombinase polymerase amplification
- RSV
Respiratory syncytial virus
- RT-LAMP
Reverse transcription loop-mediated isothermal amplification
- SARS
Severe acute respiratory syndrome
- SARS-CoV
Severe acute respiratory syndrome coronavirus
- SARS-CoV-2
Severe acute respiratory syndrome corona virus-2
- SERS
Surface-enhanced Raman scattering
- SiO2
Silicon dioxide
- SPE
Screen-printed electrodes
- SPGE
Screen-printed gold electrodes
- SPR
Surface plasmon resonance
- ssDNA
Single-stranded DNA
- TMB
Tetramethylbenzidine
- ZnO
Zinc oxide
Author contributions
MR, AJ, LC, HPD and GM drafted the manuscript, SK, LL and HTS prepared the tables, AH and HK prepared the figures, JLP, HK, MR and ZS revised the manuscript. All authors read and approved the final manuscript.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abinaya Jaisankar and Lijia Cheng are co-first authors, who contributed equally to this work
Contributor Information
Murugan Ramalingam, Email: rmurug2000@gmail.com.
Zheng Shi, Email: shizheng@cdu.edu.cn.
Giovanna Marrazza, Email: giovanna.marrazza@unifi.it.
References
- 1.Sebastian S, Nathalie S, Shattuck EC, Hawley DM, Ancel ML, Bolnick DI. Infectious diseases and social distancing in nature. Science. 2021;371:eabc8881. doi: 10.1126/science.abc8881. [DOI] [PubMed] [Google Scholar]
- 2.Buckee C, Noor A, Sattenspiel L. Thinking clearly about social aspects of infectious disease transmission. Nature. 2021;595:205–213. doi: 10.1038/s41586-021-03694-x. [DOI] [PubMed] [Google Scholar]
- 3.Silva GA. Introduction to nanotechnology and its applications to medicine. Surg Neurol. 2004;61:216–220. doi: 10.1016/j.surneu.2003.09.036. [DOI] [PubMed] [Google Scholar]
- 4.Sharifi M, Hasan A, Haghighat S, Taghizadeh A, Attar F, Bloukh SH, Edis Z, Xue M, Khan S, Falahati M. Rapid diagnostics of coronavirus disease 2019 in early stages using nanobiosensors: challenges and opportunities. Talanta. 2021;223:121704. doi: 10.1016/j.talanta.2020.121704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Naresh V, Lee N. A review on biosensors and recent development of nanostructured materials-enabled biosensors. Sensors. 2021;21:1109. doi: 10.3390/s21041109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nayak V, Singh KR, Verma R, Pandey MD, Singh J, Pratap Singh R. Recent advancements of biogenic iron nanoparticles in cancer theranostics. Mater Lett. 2022;313:131769. doi: 10.1016/J.MATLET.2022.131769. [DOI] [Google Scholar]
- 7.Singh KR, Solanki PR, Malhotra BD, Pandey AC, Singh RP. Introduction to nanomaterials: an overview toward broad-spectrum applications, nanomaterials in bionanotechnology. Boca Raton, FL, USA: CRC Press; 2021. 10.1201/9781003139744-1.
- 8.Lin WP, Wang WJ, Lee CH, Jan FJ, Wang GJ. A two-in-one immunoassay biosensor for the simultaneous detection of Odontoglossum ringspot virus and Cymbidium mosaic virus. Sensors Actuators B Chem. 2022;350:130875. doi: 10.1016/j.snb.2021.130875. [DOI] [Google Scholar]
- 9.Wu Z, Wen W, Luo F, Chen F, Xiong Y, Zhang X, Wang S. Single-particle electrochemical biosensor with DNA walker amplification for ultrasensitive HIV-DNA counting. Anal Chem. 2021;93:4506–4512. doi: 10.1021/acs.analchem.0c04861. [DOI] [PubMed] [Google Scholar]
- 10.Ashur I, Alter J, Werbner M, Ogungbile A, Dessau M, Gal-Tanamy M, Vernick S. Rapid electrochemical immunodetection of SARS-CoV-2 using a pseudo-typed vesicular stomatitis virus model. Talanta. 2022;239:123147. doi: 10.1016/j.talanta.2021.123147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang Y, Li P, Hou M, Chen L, Wang J, Yang H, Feng W. An electrochemical biosensor based on ARGET ATRP with DSN-assisted target recycling for sensitive detection of tobacco mosaic virus RNA. Bioelectrochemistry. 2022;144:108037. doi: 10.1016/j.bioelechem.2021.108037. [DOI] [PubMed] [Google Scholar]
- 12.Park G, Kim H-O, Lim J-W, Park C, Yeom M, Song D, Haam S. Rapid detection of influenza A (H1N1) virus by conductive polymer-based nanoparticle via optical response to virus-specific binding. Nano Res. 2022;15:2254–2262. doi: 10.1007/s12274-021-3772-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rabiee N, Fatahi Y, Ahmadi S, Abbariki N, Ojaghi A, Rabiee M, Radmanesh F, Dinarvand R, Bagherzadeh M, Mostafavi E, Ashrafizadeh M, Makvandi P, Lima EC, Saeb MR. Bioactive hybrid metal-organic framework (MOF)-based nanosensors for optical detection of recombinant SARS-CoV-2 spike antigen. Sci Total Environ. 2022;825:153902. doi: 10.1016/j.scitotenv.2022.153902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hadi MU, Khurshid M. SARS-CoV-2 detection using optical fiber based sensor method. Sensors. 2022;22:751. doi: 10.3390/s22030751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun Z, Liu H, Wang X. Thermal self-regulatory intelligent biosensor based on carbon-nanotubes-decorated phase-change microcapsules for enhancement of glucose detection. Biosens Bioelectron. 2022;195:113586. doi: 10.1016/j.bios.2021.113586. [DOI] [PubMed] [Google Scholar]
- 16.Zhang J, He F. Mycobacterium tuberculosis piezoelectric sensor based on AuNPs-mediated enzyme assisted signal amplification. Talanta. 2022;236:122902. doi: 10.1016/j.talanta.2021.122902. [DOI] [PubMed] [Google Scholar]
- 17.Hasan A, Nurunnabi M, Morshed M, Paul A, Polini A, Kuila T, Al Hariri M, Lee Y, Jaffa AA. Recent advances in application of biosensors in tissue engineering. Biomed Res Int. 2014;2014:307519. doi: 10.1155/2014/307519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Y, Bai X, Wen W, Zhang X, Wang S. Ultrasensitive electrochemical biosensor for HIV gene detection based on graphene stabilized gold nanoclusters with exonuclease amplification. ACS Appl Mater Interfaces. 2015;7:18872–18879. doi: 10.1021/acsami.5b05857. [DOI] [PubMed] [Google Scholar]
- 19.Guo Y, Chen J, Chen G. A label-free electrochemical biosensor for detection of HIV related gene based on interaction between DNA and protein sensors actuators. B Chem. 2013;184:113–117. doi: 10.1016/j.snb.2013.04.046. [DOI] [Google Scholar]
- 20.Abdullah J, Izuan J, Rashid A, Rashid A, Yusof A, Hashim U, Hajian R. A novel disposable biosensor based on SiNWs/AuNPs modified-screen printed electrode for dengue virus DNA oligomer detection. IEEE Sens J. 2015 doi: 10.1109/JSEN.2015.2417911. [DOI] [Google Scholar]
- 21.Odeh AA, Al-Douri Y, Voon CH, Mat Ayub R, Gopinath SCB, Odeh RA, Ameri M, Bouhemadou A. A needle-like Cu2CdSnS4 alloy nanostructure-based integrated electrochemical biosensor for detecting the DNA of dengue serotype 2. Microchim Acta. 2017;184:2211–2218. doi: 10.1007/s00604-017-2249-5. [DOI] [Google Scholar]
- 22.Prashanth P, Suthanthiraraj A, Sen AK. Biosensors and Bioelectronics Localized surface plasmon resonance ( LSPR ) biosensor based on thermally annealed silver nanostructures with on-chip blood-plasma separation for the detection of dengue non-structural protein NS1 antigen. Biosens Bioelectron. 2019;132:38–46. doi: 10.1016/j.bios.2019.02.036. [DOI] [PubMed] [Google Scholar]
- 23.Wang S, Ip A, Xu F, Giguel F, S.M. Sensors, undefined and, undefined 2010, Development of a microfluidic system for measuring HIV-1 viral load, Spiedigitallibrary.Org. (n.d.). https://www.spiedigitallibrary.org/conference-proceedings-of-spie/7666/76661H/Development-of-a-microfluidic-system-for-measuring-HIV-1-viral/10.1117/12.853132.short. Accessed May 26, 2021. [DOI] [PMC free article] [PubMed]
- 24.Chunduri LAA, Kumar M, Sandeep H, Eswarappa P, Aditya B, Jikun K. Development of carbon dot based microplate and microfluidic chip immunoassay for rapid and sensitive detection of HIV-1 p24 antigen. Microfluid Nanofluidics. 2016;20:1–10. doi: 10.1007/s10404-016-1825-z. [DOI] [Google Scholar]
- 25.Cho IH, Kim DH, Park S. Electrochemical biosensors: perspective on functional nanomaterials for on-site analysis. Biomater Res. 2020;24:1–2. doi: 10.1186/s40824-019-0181-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yi J, Xianyu Y. Gold nanomaterials-implemented wearable sensors for healthcare applications. Adv Funct Mater. 2022 doi: 10.1002/adfm.202113012. [DOI] [Google Scholar]
- 27.Petrucci R, Bortolami M, Di Matteo P, Curulli A. Gold nanomaterials-based electrochemical sensors and biosensors for phenolic antioxidants detection: recent advances. Nanomaterials. 2022;12:959. doi: 10.3390/nano12060959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sharifi M, Hosseinali SH, Hossein Alizadeh R, Hasan A, Attar F, Salihi A, Shekha MS, Amen KM, Aziz FM, Saboury AA, Akhtari K, Taghizadeh A, Hooshmand N, El-Sayed MA, Falahati M. Plasmonic and chiroplasmonic nanobiosensors based on gold nanoparticles. Talanta. 2020;212:120782. doi: 10.1016/j.talanta.2020.120782. [DOI] [PubMed] [Google Scholar]
- 29.Shakoori Z, Salimian S, Kharrazi S, Adabi M, Saber R. Electrochemical DNA biosensor based on gold nanorods for detecting hepatitis B virus. Anal Bioanal Chem. 2015;407:455–461. doi: 10.1007/s00216-014-8303-9. [DOI] [PubMed] [Google Scholar]
- 30.Funari R, Chu KY, Shen AQ. Detection of antibodies against SARS-CoV-2 spike protein by gold nanospikes in an opto-microfluidic chip. Biosens Bioelectron. 2020;169:112578. doi: 10.1016/j.bios.2020.112578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xiao T, Huang J, Wang D, Meng T, Yang X. Au and Au-Based nanomaterials: synthesis and recent progress in electrochemical sensor applications. Talanta. 2019 doi: 10.1016/j.talanta.2019.120210. [DOI] [PubMed] [Google Scholar]
- 32.Wasowicz M, Viswanathan S, Dvornyk A, Grzelak K, Kłudkiewicz B, Radecka H. Comparison of electrochemical immunosensors based on gold nano materials and immunoblot techniques for detection of histidine-tagged proteins in culture medium. Biosens Bioelectron. 2008;24:284–289. doi: 10.1016/j.bios.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 33.Ibrahim N, Jamaluddin ND, Tan LL, Yusof NYM. A review on the development of gold and silver nanoparticles-based biosensor as a detection strategy of emerging and pathogenic RNA virus. Sensors. 2021;21:5114. doi: 10.3390/s21155114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xing Y, Feng XZ, Zhang L, Hou J, Han GC, Chen Z. Open access full text article a sensitive and selective electrochemical biosensor for the determination of beta-amyloid oligomer by inhibiting the peptide-triggered in situ assembly of silver nanoparticles. Int J Nanomed. 2017;12:3171–3179. doi: 10.2147/IJN.S132776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yu CX, Xiong F, Liu LL. Electrochemical biosensors with silver nanoparticles as signal labels. Int J Electrochem Sci. 2020;15:3869–3890. doi: 10.20964/2020.05.53. [DOI] [Google Scholar]
- 36.Yang Y, Murray J, Haverstick J, Tripp RA, Zhao Y. Sensors and actuators: B. Chemical silver nanotriangle array based LSPR sensor for rapid coronavirus detection. Sens Actuators B Chem. 2022;359:131604. doi: 10.1016/j.snb.2022.131604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Que M, Lin C, Sun J, Chen L, Sun X, Sun Y. Progress in zno nanosensors. Sensors. 2021;21:1–22. doi: 10.3390/s21165502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ghaffarkhah A, Hosseini E, Kamkar M, Sehat AA, Dordanihaghighi S, Allahbakhsh A, van der Kuur C, Arjmand M. Synthesis, applications, and prospects of graphene quantum dots: a comprehensive review. Small. 2022;18:2102683. doi: 10.1002/smll.202102683. [DOI] [PubMed] [Google Scholar]
- 39.Tabish TA, Hayat H, Abbas A, Narayan RJ. Graphene quantum dot–based electrochemical biosensing for early cancer detection. Curr Opin Electrochem. 2021;30:100786. doi: 10.1016/j.coelec.2021.100786. [DOI] [Google Scholar]
- 40.Shrivastava S, Jadon N, Jain R. Next-generation polymer nanocomposite-based electrochemical sensors and biosensors: a review, TrAC. Trends Anal Chem. 2016;82:55–67. doi: 10.1016/J.TRAC.2016.04.005. [DOI] [Google Scholar]
- 41.Eskandarinezhad S, Irshad Ahmad W, Nourollahileilan M, Khosla A, Ahmad T. Review—metal and metal oxide nanoparticles/nanocomposites as electrochemical biosensors for cancer detection. J Electrochem Soc. 2022 doi: 10.1149/1945-7111/ac6076. [DOI] [Google Scholar]
- 42.Kim G, Kim J, Kim SM, Kato T, Yoon J, Noh S, Park EY, Park C, Lee T, Choi J-W. Fabrication of MERS-nanovesicle biosensor composed of multi-functional DNA aptamer/graphene-MoS2 nanocomposite based on electrochemical and surface-enhanced Raman spectroscopy. Sensors Actuators B Chem. 2022;352:131060. doi: 10.1016/j.snb.2021.131060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wei S, Xiao H, Gu M, Chen Z, Cao L. Ultrasensitive label-free electrochemical immunosensor based on core-shell Au@PtNPs functionalized rGO-TEPA/PB nanocomposite for HBsAg detection. J Electroanal Chem. 2021;890:115216. doi: 10.1016/j.jelechem.2021.115216. [DOI] [Google Scholar]
- 44.Amouzadeh Tabrizi M, Nazari L, Acedo P. A photo-electrochemical aptasensor for the determination of severe acute respiratory syndrome coronavirus 2 receptor-binding domain by using graphitic carbon nitride-cadmium sulfide quantum dots nanocomposite. Sensors Actuators B Chem. 2021;345:130377. doi: 10.1016/j.snb.2021.130377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nguyen BTT, Koh G, Hui SL, Chua AJS, Ng MML, Toh CS. Membrane-based electrochemical nanobiosensor for the detection of virus. Anal Chem. 2009;81:7226–7234. doi: 10.1021/ac900761a. [DOI] [PubMed] [Google Scholar]
- 46.Wang Z, Wu S, Wang J, Yu A, Wei G. Carbon nanofiber-based functional nanomaterials for sensor applications. Nanomaterials. 2019;9:1045. doi: 10.3390/nano9071045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Guo L, Wan K, Liu B, Wang Y, Wei G. Recent advance in the fabrication of carbon nanofiber-based composite materials for wearable devices. Nanotechnology. 2021;32:442001. doi: 10.1088/1361-6528/ac18d5. [DOI] [PubMed] [Google Scholar]
- 48.Chen A, Chatterjee S. Nanomaterials based electrochemical sensors for biomedical applications. Chem Soc Rev. 2013;42:5425–5438. doi: 10.1039/c3cs35518g. [DOI] [PubMed] [Google Scholar]
- 49.Harper A, Anderson MR. Electrochemical glucose sensors-developments using electrostatic assembly and carbon nanotubes for biosensor construction. Sensors. 1962;10:8248–8274. doi: 10.3390/s100908248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Layqah LA, Eissa S. An electrochemical immunosensor for the corona virus associated with the Middle East respiratory syndrome using an array of gold nanoparticle-modified carbon electrodes. Microchim Acta. 2019;186:1–10. doi: 10.1007/S00604-019-3345-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lai HC, Chin SF, Pang SC, Sia M, Sum H, Perera D. Carbon nanoparticles based electrochemical biosensor strip for detection of Japanese encephalitis. Virus. 2017;2017:1–8. [Google Scholar]
- 52.Dai L, Hai B, Van Hieu N, Vinh H. Electrochemical detection of short HIV sequences on chitosan/Fe3O4 nanoparticle based screen printed electrodes. Mater Sci Eng C. 2011;31:477–485. doi: 10.1016/j.msec.2010.11.007. [DOI] [Google Scholar]
- 53.Dong S, Zhao R, Zhu J, Lu X, Li Y, Qiu S, Jia L, Jiao X, Song S, Fan C, Hao RZ, Bin Song H. Electrochemical DNA biosensor based on a tetrahedral nanostructure probe for the detection of avian influenza A (H7N9) virus. ACS Appl Mater Interfaces. 2015;7:8834–8842. doi: 10.1021/acsami.5b01438. [DOI] [PubMed] [Google Scholar]
- 54.Gong Q, Wang Y, Yang H. A sensitive impedimetric DNA biosensor for the determination of the HIV gene based on graphene-Nafion composite film. Biosens Bioelectron. 2017;89:565–569. doi: 10.1016/j.bios.2016.02.045. [DOI] [PubMed] [Google Scholar]
- 55.Cecchetto J, Carvalho F, Santos A, undefined 2015, An impedimetric biosensor to test neat serum for dengue diagnosis, Elsevier. (n.d.). https://www.sciencedirect.com/science/article/pii/S0925400515002427. Accessed May 26, 2021.
- 56.Lin D, Tang T, Harrison DJ, Lee WE, Jemere AB. A regenerating ultrasensitive electrochemical impedance im-munosensor for the detection of adenovirus. Biosens Bioelectron. 2015;68:129–134. doi: 10.1016/j.bios.2014.12.032. [DOI] [PubMed] [Google Scholar]
- 57.Lee J, Oh B, Choi J. Biosensors and bioelectronics electrochemical sensor based on direct electron transfer of HIV-1 virus at Au nanoparticle modified ITO electrode. Biosens Bioelectron. 2013;49:531–535. doi: 10.1016/j.bios.2013.06.010. [DOI] [PubMed] [Google Scholar]
- 58.Mohsin DH, Saleh M, Fataneh M. Design of aptamer - based sensing platform using gold nanoparticles functionalized reduced graphene oxide for ultrasensitive detection of hepatitis B virus. Chem Pap. 2020;75:279–295. doi: 10.1007/s11696-020-01292-1. [DOI] [Google Scholar]
- 59.Rodriguez-lorenzo L, Fabris L, Alvarez-puebla RA. Analytica chimica acta multiplex optical sensing with surface-enhanced Raman scattering: a critical review. Anal Chim Acta. 2012;745:10–23. doi: 10.1016/j.aca.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 60.Pang S, Rong Y, Wang Z, Xiao J, Wang R. A fluorescent aptasensor for H5N1 influenza virus detection based-on the core–shell nanoparticles metal-enhanced fluorescence (MEF) Biosens Bioelectron. 2015 doi: 10.1016/j.bios.2014.10.052. [DOI] [PubMed] [Google Scholar]
- 61.Diao Y, Tang W, Ding M, Li S, Cheng X, Mo W, Yan F, Ma X, Yan H. Highly sensitive surface plasmon resonance biosensor for the detection of HIV-related DNA based on dynamic and structural DNA nanodevices. Biosens Bioelectron. 2018 doi: 10.1016/j.bios.2017.08.042. [DOI] [PubMed] [Google Scholar]
- 62.Sharma PK, Kumar JS, Singh VV, Biswas U, Sarkar SS, Alam SI, Dash PK, Boopathi M, Ganesan K, Jain R. Surface plasmon resonance sensing of Ebola virus: a biological threat. Anal Bioanal Chem. 2020;412:4101–4112. doi: 10.1007/s00216-020-02641-5. [DOI] [PubMed] [Google Scholar]
- 63.Fu X, Cheng Z, Yu J, Choo P, Chen L, Choo J. A SERS-based lateral flow assay biosensor for highly sensitive detection of HIV-1 DNA. Biosens Bioelectron. 2015;78:530–537. doi: 10.1016/j.bios.2015.11.099. [DOI] [PubMed] [Google Scholar]
- 64.Kamińska A, Witkowska E, Winkler K, Dzięcielewski I, Weyher JL, Waluk J. Detection of hepatitis B virus antigen from human blood: SERS im-munoassay in a microfluidic system. Biosens Bioelectron. 2014;66:461–467. doi: 10.1016/j.bios.2014.10.082. [DOI] [PubMed] [Google Scholar]
- 65.Damborský P, Švitel J, Katrlík J. Optical biosensors. Essays Biochem. 2016;60:91–100. doi: 10.1042/EBC20150010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zheng Y, Bian S, Sun J, Wen L, Rong G, Sawan M. Label-free LSPR-vertical microcavity biosensor for on-site SARS-CoV-2 detection. Biosensors. 2022;12:151. doi: 10.3390/bios12030151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Liang J, Zhang W, Qin Y, Li Y, Liu GL, Hu W. Applying machine learning with localized surface Plasmon resonance sensors to detect SARS-CoV-2 particles. Biosensors. 2022;12:173. doi: 10.3390/bios12030173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chen H, Park S-K, Joung Y, Kang T, Lee M-K, Choo J. SERS-based dual-mode DNA aptasensors for rapid classification of SARS-CoV-2 and influenza A/H1N1 infection. Sens Actuators B Chem. 2022;355:131324. doi: 10.1016/j.snb.2021.131324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhang Y, Xue C, Li P, Cui S, Cui D, Jin H. Metal-organic framework engineered corn-like SERS active Ag@Carbon with controllable spacing distance for tracking trace amount of organic compounds. J Hazard Mater. 2022;424:127686. doi: 10.1016/j.jhazmat.2021.127686. [DOI] [PubMed] [Google Scholar]
- 70.Moghadam AJ. Thermal characteristics of time - periodic electroosmotic flow in a circular microchannel. Heat Mass Transfer. 2015 doi: 10.1007/s00231-015-1513-7. [DOI] [Google Scholar]
- 71.Luka G, Ahmadi A, Najjaran H, Alocilja E, Derosa M, Wolthers K, Malki A, Aziz H, Althani A, Hoorfar M, Star A, Ligler FS. Microfluidics integrated biosensors: a leading technology towards lab-on-a-chip and sensing applications. Mdpi Com. 2015 doi: 10.3390/s151229783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dak MA, Ebrahimi P, Swaminathan A, Duarte-Guevara V, Bashir C, Alam R. Droplet-based biosensing for lab-on-a-chip, open microfluidics platforms. Biosensors. 2016;6:14. doi: 10.3390/bios6020014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hosokawa M, Nishikawa Y, Hyun Yoon D, Mori T, Hoshino Y, Hirose T, Sekiguchi T, Shoji S, Takeyama H. Droplet-based microfluidics for high-throughput screening of a metagenomic library for isolation of microbial enzymes Electrogenerated Chemiluminescence of donor-acceptor molecules with thermally activated delayed fluorescence view project droplet-based microfluidics for high-throughput screening of a metagenomic library for isolation of microbial enzymes. Allergol Immunopathol (Madr) 2015 doi: 10.1016/j.bios.2014.08.059. [DOI] [Google Scholar]
- 74.Samiei M, Luka E, Najjaran GS, Hoorfar H. Integration of biosensors into digital microfluidics: impact of hydrophilic surface of biosensors on droplet manipulation. Biosens Bioelectron. 2016 doi: 10.1016/j.bios.2016.03.035. [DOI] [PubMed] [Google Scholar]
- 75.Narahari T, Dahmer J, Sklavounos A, Kim T, Satkauskas M, Clotea I, Ho M, Lamanna J, Dixon C, Rackus DG, da Silva SJR, Pena L, Pardee K, Wheeler AR. Portable sample processing for molecular assays: application to Zika virus diagnostics. Lab Chip. 2022;22:1748–1763. doi: 10.1039/D1LC01068A. [DOI] [PubMed] [Google Scholar]
- 76.Liu B, Du D, Yu X-Y, Hua X, Lin Y. Chemical mixture methodology view project designing of novel nanobiosensor for detection of pathogenic bacteria from milk view project paper-based electrochemical biosensors: from test strips to paper-based microfluidics. Wiley Online Libr. 2014;26:1214–1223. doi: 10.1002/elan.201400036. [DOI] [Google Scholar]
- 77.Zhao C, Thuo MM, Liu X. A microfluidic paper-based electrochemical biosensor array for multiplexed detection of metabolic biomarkers. Sci Technol Adv Mater. 2013 doi: 10.1088/1468-6996/14/5/054402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhao Y, Hu X, Hu S, Peng Y. Applications of fiber-optic biochemical sensor in microfluidic chips: a review. Biosens Bioelectron. 2020;166:112447. doi: 10.1016/j.bios.2020.112447. [DOI] [PubMed] [Google Scholar]
- 79.Song Y, Lin B, Tian T, Xu X, Wang W, Ruan Q, Guo J, Zhu Z, Yang C. Recent progress in microfluidics-based biosensing. Anal Chem. 2019;91:388–404. doi: 10.1021/acs.analchem.8b05007. [DOI] [PubMed] [Google Scholar]
- 80.Akhtarian S, Miri S, Doostmohammadi A, Brar SK, Rezai P. Nanopore sensors for viral particle quantification: current progress and future prospects. Bioengineered. 2021;12:9189–9215. doi: 10.1080/21655979.2021.1995991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Roberts A, Mahari S, Shahdeo D, Gandhi S. Analytica chimica acta label-free detection of SARS-CoV-2 spike S1 antigen triggered by electroactive gold nanoparticles on antibody coated fluorine-doped tin oxide (FTO) electrode. Anal Chim Acta. 2021;1188:339207. doi: 10.1016/j.aca.2021.339207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Shahdeo D, Roberts A, Archana GJ, Sagar N, Mahari S, Nagamani K, Gandhi S. Biosensors and bioelectronics label free detection of SARS CoV-2 receptor binding domain ( RBD ) protein by fabrication of gold nanorods deposited on electrochemical immunosensor (GDEI) Biosens Bioelectron. 2022;212:114406. doi: 10.1016/j.bios.2022.114406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Roberts GS, Mahari S. Signal enhancing gold nanorods (GNR) and antibody modified electrochemical nanosensor for ultrasensitive detection of Japanese Encephalitis Virus (JEV) secretory Non-Structural 1 (NS1) biomarker. J Electroanal Chem. 2022;919:116563. doi: 10.1016/j.jelechem.2022.116563. [DOI] [Google Scholar]
- 84.Prakashan D, Shrikrishna NS, Gandhi KNS. Gold nanoparticle conjugate - based lateral flow immunoassay (LFIA) for rapid detection of RBD antigen of SARS-CoV-2 in clinical samples using a smartphone-based application. J Med Virol. 2022;2:1–12. doi: 10.1002/jmv.28416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Białobrzeska W, Firganek D, Czerkies M, Lipniacki T, Skwarecka M, Dziąbowska K, Cebula Z, Malinowska N, Bigus D, Bięga E, Pyrć K, Pala K, Żołędowska S, Nidzworski D. Electrochemical immunosensors based on screen-printed gold and glassy carbon electrodes: comparison of performance for respiratory syncytial virus detection. Biosensors. 2020;10:175. doi: 10.3390/bios10110175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ahangar LE, Mehrgardi MA. Amplified detection of hepatitis B virus using an electrochemical DNA biosensor on a nanoporous gold platform. Bioelectrochemistry. 2017;117:83–88. doi: 10.1016/j.bioelechem.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 87.Rahmati H, Roushani Z, Hosseini M. Three-dimensional NiCo2O4 nanowires encapsulated in nitrogen-doped carbon networks as a high-performance aptamer stabilizer for impedimetric ultrasensitive. Surf Interfaces. 2021 doi: 10.1016/j.surfin.2020.100813. [DOI] [Google Scholar]
- 88.Navakul K, Warakulwit C, Thai Yenchitsomanus P, Panya A, Lieberzeit PA, Sangma C. A novel method for dengue virus detection and antibody screening using a graphene-polymer based electrochemical biosensor. Nanomed Nanotechnol Biol Med. 2017;13:549–557. doi: 10.1016/j.nano.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 89.Palomar Q, Xu X, Gondran C, Holzinger M, Cosnier S, Zhang Z. A novel method for dengue virus detection and antibody screening using a graphene-polymer based electrochemical biosensor. Mikrochim Acta. 2017;187(6):363. doi: 10.1007/s00604-020-04339-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chowdhury AD, Takemura K, Li TC, Suzuki T, Park EY. Electrical pulse-induced electrochemical biosensor for hepatitis E virus detection. Nat Commun. 2019;10:4–7. doi: 10.1038/s41467-019-11644-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ghanbari K, Roushani M, Azadbakht A. Ultra-sensitive aptasensor based on a GQD nanocomposite for detection of hepatitis C virus core antigen. Anal Biochem. 2017;534:64–69. doi: 10.1016/j.ab.2017.07.016. [DOI] [PubMed] [Google Scholar]
- 92.Al-Douri Y, Gherab K, Batoo KM, Raslan EH. Detecting the DNA of dengue serotype 2 using aluminium nanoparticle doped zinc oxide nanostructure: Synthesis, analysis and characterization. J Mater Res Technol. 2020;9:5515–5523. doi: 10.1016/j.jmrt.2020.03.076. [DOI] [Google Scholar]
- 93.Awan M, Rauf S, Abbas A, Hasnain M, Yang C, Ahmad S, Amin N, Hayat A. A sandwich electrochemical immunosensor based on antibody functionalized-silver nanoparticles ( Ab-Ag NPs ) for the detection of dengue biomarker protein NS1. J Mol Liq. 2020;317:114014. doi: 10.1016/j.molliq.2020.114014. [DOI] [Google Scholar]
- 94.Eissa S, Zourob M. Development of a low-cost cotton-tipped electrochemical immunosensor for the detection of SARS-CoV-2. Anal Chem. 2021;93:1826–1833. doi: 10.1021/acs.analchem.0c04719. [DOI] [PubMed] [Google Scholar]
- 95.Yrad FM, Castañares JM, Alocilja EC. Visual detection of dengue-1 RNA using gold nanoparticle-based lateral flow biosensor. Diagnostics. 2019;9:74. doi: 10.3390/diagnostics9030074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Omar NAS, Fen YW, Abdullah J, Mustapha Kamil Y, Daniyal WMEMM, Sadrolhosseini AR, Mahdi MA. Sensitive detection of dengue virus type 2 E-proteins signals using self-assembled monolayers/reduced graphene oxide-PAMAM dendrimer thin film-spr optical sensor. Sci Rep. 2020;10:1–15. doi: 10.1038/s41598-020-59388-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Xi Z, Gong Q, Wang C, Zheng B. Highly sensitive chemiluminescent aptasensor for detecting HBV infection based on rapid magnetic separation and double-functionalized gold nanoparticles. Sci Rep. 2018;8:1–7. doi: 10.1038/s41598-018-27792-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Chen H, Park SG, Choi N, Il Moon J, Dang H, Das A, Lee S, Kim DG, Chen L, Choo J. SERS imaging-based aptasensor for ultrasensitive and reproducible detection of influenza virus A. Biosens Bioelectron. 2020;167:112496. doi: 10.1016/j.bios.2020.112496. [DOI] [PubMed] [Google Scholar]
- 99.Gribanyov D, Zhdanov G, Olenin A, Lisichkin G, Gambaryan A, Kukushkin V, Zavyalova E. Sers-based colloidal aptasensors for quantitative determination of influenza virus. Int J Mol Sci. 2021;22:1–13. doi: 10.3390/ijms22041842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Liu X, Yang J, Li Q, Wang Y, Wang Y, Li G, Shi J, Ding P. A strip test for the optical determination of influenza virus H3 subtype using gold nanoparticle coated polystyrene latex microspheres. Microchim Acta. 2020;187:1–7. doi: 10.1007/s00604-020-04255-1. [DOI] [PubMed] [Google Scholar]
- 101.Achadu OJ, Takemura K, Memdi I, Park EY. Sensors and actuators B: chemical plasmonic/magnetic molybdenum trioxide and graphitic carbon nitride quantum dots-based fluoroimmunosensing system for in fluenza virus. Sens Actuators B Chem. 2020;321:128494. doi: 10.1016/j.snb.2020.128494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Takemura K, Lee J, Suzuki T, Hara T, Abe F, Park EY. Sensors and actuators B : chemical ultrasensitive detection of norovirus using a magneto fluoroimmunoassay based on synergic properties of gold/magnetic nanoparticle hybrid nanocomposites and quantum dots. Sens Actuators B Chem. 2019;296:126672. doi: 10.1016/j.snb.2019.126672. [DOI] [Google Scholar]
- 103.Nasrin F, Chowdhury AD, Takemura K, Kozaki I, Honda H, Adegoke O, Park EY. Fluorometric virus detection platform using quantum dots-gold nanocomposites optimizing the linker length variation. Anal Chim Acta. 2020;1109:148–157. doi: 10.1016/j.aca.2020.02.039. [DOI] [PubMed] [Google Scholar]
- 104.Weerathunge P, Ramanathan R, Torok VA, Hodgson K, Xu Y, Goodacre R, Behera BK, Bansal V. Ultrasensitive colorimetric detection of murine norovirus using NanoZyme aptasensor. Anal Chem. 2019;91:3270–3276. doi: 10.1021/acs.analchem.8b03300. [DOI] [PubMed] [Google Scholar]
- 105.Zhu L, Zhao Y, Yao S, Xu M, Yin L, Zhai X, Teng X. A colorimetric aptasensor for the simple and rapid detection of human papillomavirus type 16 L1 proteins. Analyst. 2021;146:2712–2717. doi: 10.1039/d1an00251a. [DOI] [PubMed] [Google Scholar]
- 106.Garcia-Cordero JL, Rodriguez-Moncayo R, Cedillo-Alcantar DF, Guevara-Pantoja PE, Chavez-Pineda OG, Hernandez-Ortiz JA, Amador-Hernandez JU, Rojas-Velasco G, Sanchez-Muñoz F, Manzur-Sandoval D, Patino-Lopez LD, May-Arrioja DA, Posadas-Sanchez R, Vargas-Alarcon G. Lab on a chip devices and applications at the micro-and nanoscale A high-throughput multiplexed microfluidic device for COVID-19 serology assays lab on a chip A high-throughput multiplexed microfluidic device for COVID-19 serology assays †. Pubs Rsc Org. 2021;21:93. doi: 10.1039/d0lc01068e. [DOI] [PubMed] [Google Scholar]
- 107.Della Ventura B, Cennamo M, Minopoli A, Campanile R, Censi SB, Terracciano D, Portella G, Velotta R. Colorimetric test for fast detection of SARS-COV-2 in nasal and throat swabs. ACS Sens. 2020;5:3043–3048. doi: 10.1021/acssensors.0c01742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lum J, Wang R, Hargis B, Tung S, Bottje W, Lu H, Li Y. An impedance aptasensor with microfluidic chips for specific detection of H5N1 avian influenza virus. Sensors (Switzerland) 2015;15:18565–18578. doi: 10.3390/s150818565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Chand R, Neethirajan S. Microfluidic platform integrated with graphene-gold nano-composite aptasensor for one-step detection of norovirus. Biosens Bioelectron. 2017;98:47–53. doi: 10.1016/j.bios.2017.06.026. [DOI] [PubMed] [Google Scholar]
- 110.Liu D, Zhang Y, Zhu M, Yu Z, Song Y, Zhou S, Yang C. Micro fluidic-integrated multicolor immunosensor for visual detection of HIV-1 p24 antigen with the naked eye. Anal Chem. 2020;92:11826–11833. doi: 10.1021/acs.analchem.0c02091. [DOI] [PubMed] [Google Scholar]
- 111.McMullen A, de Haan HW, Tang JX, Stein D. Stiff filamentous virus translocations through solid-state nanopores. Nat Commun. 2014;5:4171. doi: 10.1038/ncomms5171. [DOI] [PubMed] [Google Scholar]
- 112.Wu H, Chen Y, Zhou Q, Wang R, Xia B, Ma D, Luo K, Liu Q. Translocation of rigid rod-shaped virus through various solid-state nanopores. Anal Chem. 2016;88:2502–2510. doi: 10.1021/acs.analchem.5b04905. [DOI] [PubMed] [Google Scholar]
- 113.Arima A, Tsutsui M, Washio T, Baba Y, Kawai T. Solid-state nanopore platform integrated with machine learning for digital diagnosis of virus infection. Anal Chem. 2021;93:215–227. doi: 10.1021/acs.analchem.0c04353. [DOI] [PubMed] [Google Scholar]
- 114.Niedzwiecki DJ, Iyer R, Borer PN, Movileanu L. Sampling a biomarker of the human immunodeficiency virus across a synthetic nanopore. ACS Nano. 2013;7:3341–3350. doi: 10.1021/nn400125c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Arima A, Harlisa IH, Yoshida T, Tsutsui M, Tanaka M, Yokota K, Tonomura W, Yasuda J, Taniguchi M, Washio T, Okochi M, Kawai T. Identifying single viruses using biorecognition solid-state nanopores. J Am Chem Soc. 2018;140:16834–16841. doi: 10.1021/jacs.8b10854. [DOI] [PubMed] [Google Scholar]
- 116.Taniguchi M, Minami S, Ono C, Hamajima R, Morimura A, Hamaguchi S, Akeda Y, Kanai Y, Kobayashi T, Kamitani W, Terada Y, Suzuki K, Hatori N, Yamagishi Y, Washizu N, Takei H, Sakamoto O, Naono N, Tatematsu K, Washio T, Matsuura Y, Tomono K. Combining machine learning and nanopore construction creates an artificial intelligence nanopore for coronavirus detection. Nat Commun. 2021;12:3726. doi: 10.1038/s41467-021-24001-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Famá F, Faria JN, Portugal D. An IoT-based interoperable architecture for wireless biomonitoring of patients with sensor patches. Internet Things. 2022;19:100547. doi: 10.1016/j.iot.2022.100547. [DOI] [Google Scholar]
- 118.Rejeb A, Rejeb K, Treiblmaier H, Appolloni A, Alghamdi S, Alhasawi Y, Iranmanesh M. Internet of things the (IoT) in healthcare: taking stock and moving forward. Internet Things. 2023;22:100721. doi: 10.1016/j.iot.2023.100721. [DOI] [Google Scholar]
- 119.Sood SK, Rawat KS, Kumar D. Analytical mapping of information and communication technology in emerging infectious diseases using CiteSpace. Telemat Inform. 2022;69:101796. doi: 10.1016/j.tele.2022.101796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Jain S, Nehra M, Kumar R, Dilbaghi N, Hu T, Kumar S, Kaushik A, Li C. Internet of medical things (IoMT)-integrated biosensors for point-of-care testing of infectious diseases. Biosens Bioelectron. 2021;179:113074. doi: 10.1016/j.bios.2021.113074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Beduk T, Beduk D, Hasan MR, Guler Celik E, Kosel J, Narang J, Salama KN. Smartphone-based multiplexed biosensing tools for health monitoring. Biosensors. 2022;12:583. doi: 10.3390/bios12080583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Salimiyan Rizi K. The smartphone biosensors for point-of-care detection of human infectious diseases: overview and perspectives—a systematic review. Curr Opin Electrochem. 2022;32:100925. doi: 10.1016/j.coelec.2021.100925. [DOI] [Google Scholar]
- 123.Qian S, Cui Y, Cai Z, Li L. Applications of smartphone-based colorimetric biosensors. Biosens Bioelectron X. 2022;11:100173. doi: 10.1016/j.biosx.2022.100173. [DOI] [Google Scholar]
- 124.Ding X, Mauk MG, Yin K, Kadimisetty K. Interfacing pathogen detection with smartphones for point-of-care applications. Anal Chem. 2018;91:655–672. doi: 10.1021/acs.analchem.8b04973.Interfacing. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Shrivastava S, Trung TQ. Recent progress, challenges, and prospects of fully integrated mobile and wearable point-of-care testing systems for self-testing. Chem Soc Rev. 2020;49:1812–1866. doi: 10.1039/c9cs00319c. [DOI] [PubMed] [Google Scholar]
- 126.Lee N, Wang C, Park J. User-friendly point-of-care detection of influenza A (H1N1) virus using light guide in three-dimensional photonic crystal. RSC Adv. 2018;8:22991–22997. doi: 10.1039/C8RA02596G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Teengam P, Nisab N, Chuaypen N, Tangkijvanich P, Vilaivan T. Fluorescent paper-based DNA sensor using pyrrolidinyl peptide nucleic acids for hepatitis C virus detection. Biosens Bioelectron. 2021;189:113381. doi: 10.1016/j.bios.2021.113381. [DOI] [PubMed] [Google Scholar]
- 128.Huang L, Xiao W, Xu T, Chen H, Jin Z, Zhang Z, Song Q, Tang Y. Sensors and actuators: B. Chemical miniaturized paper-based smartphone biosensor for differential diagnosis of wild-type pseudorabies virus infection versus vaccination immunization. Sens Actuators B Chem. 2021;327:128893. doi: 10.1016/j.snb.2020.128893. [DOI] [Google Scholar]
- 129.Cui F, Yue Y, Zhang Y, Zhang Z, Zhou HS. Advancing biosensors with machine learning. ACS Sens. 2020;5:3346–3364. doi: 10.1021/acssensors.0c01424. [DOI] [PubMed] [Google Scholar]
- 130.Abdeldayem OM, Dabbish AM, Habashy MM, Mostafa MK, Elhefnawy M, Amin L, Al-Sakkari EG, Ragab A, Rene ER. Viral outbreaks detection and surveillance using wastewater-based epidemiology, viral air sampling, and machine learning techniques: A comprehensive review and outlook. Sci Total Environ. 2022;803:149834. doi: 10.1016/j.scitotenv.2021.149834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Sagdic K, Eş I, Sitti M, Inci F. Smart materials: rational design in biosystems via artificial intelligence. Trends Biotechnol. 2022 doi: 10.1016/j.tibtech.2022.01.005. [DOI] [PubMed] [Google Scholar]
- 132.Yuan J, Shen J, Chen M, Lou Z, Zhang S, Song Z, Li W, Zhou X. Artificial intelligence-assisted enumeration of ultra-small viruses with dual dark-field plasmon resonance probes. Biosens Bioelectron. 2022;199:113893. doi: 10.1016/j.bios.2021.113893. [DOI] [PubMed] [Google Scholar]
- 133.Wang W, Chen K, Ma X, Guo J. Artificial intelligence reinforced upconversion nanoparticle-based lateral flow assay via transfer learning. Fundam Res. 2022 doi: 10.1016/j.fmre.2022.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Jin X, Liu C, Xu T, Su L, Zhang X. Artificial intelligence biosensors: challenges and prospects. Biosens Bioelectron. 2020;165:112412. doi: 10.1016/j.bios.2020.112412. [DOI] [PubMed] [Google Scholar]
- 135.Cardoso AG, Viltres H, Ortega GA, Phung V, Grewal R, Mozaffari H, Ahmed SR, Rajabzadeh AR, Srinivasan S. Electrochemical sensing of analytes in saliva: challenges, progress, and perspectives. TrAC Trends Anal Chem. 2023;160:116965. doi: 10.1016/j.trac.2023.116965. [DOI] [Google Scholar]
- 136.Paladhi AG, Manohar MV, Pal K, Vallinayagam S, Saravana A, Packirisamy B, Aafrin V, Nandhini RS, Eghonghon K. Novel electrochemical biosensor key significance of smart intelligence (IoMT & IoHT) of COVID-19 virus control management. Process Biochem. 2022;122:105–109. doi: 10.1016/j.procbio.2022.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Mohammed H, Al-khafaji R, Adnan R. Adopting effective hierarchal IoMTs computing with K-efficient clustering to control and forecast COVID-19 cases. Comput Electr Eng. 2022;104:108472. doi: 10.1016/j.compeleceng.2022.108472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ali Y, Ullah H. Survey paper A survey on harnessing the applications of mobile computing in healthcare during the COVID-19 pandemic: challenges and solutions. Comput Netw. 2023;224:109605. doi: 10.1016/j.comnet.2023.109605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Abubakar Sadique M, Yadav S, Ranjan P, Akram Khan M, Kumar A, Khan R. Rapid detection of SARS-CoV-2 using graphene-based IoT integrated advanced electrochemical biosensor. Mater Lett. 2021;305:130824. doi: 10.1016/j.matlet.2021.130824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Lukas H, Xu C, Yu Y, Gao W. Emerging telemedicine tools for remote COVID-19 diagnosis, monitoring, and management. ACS Nano. 2020;14:16180–16193. doi: 10.1021/acsnano.0c08494. [DOI] [PubMed] [Google Scholar]
- 141.Gowri A, Ashwin Kumar N, Suresh Anand BS. Recent advances in nanomaterials based biosensors for point of care (PoC) diagnosis of Covid-19—a minireview. TrAC Trends Anal Chem. 2021;137:116205. doi: 10.1016/j.trac.2021.116205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Zhang Y, Malekjahani A, Udugama BN, Kadhiresan P, Chen H, Osborne M, Franz M, Kucera M, Plenderleith S, Yip L, Bader GD, Tran V, Gubbay JB, Mcgeer A, Mubareka S, Chan WCW. Surveilling and tracking COVID-19 patients using a portable quantum dot smartphone device. Nano Lett. 2021 doi: 10.1021/acs.nanolett.1c01280. [DOI] [PubMed] [Google Scholar]
- 143.Xu Y, Rather AM, Song S, Fang J-C, Dupont RL, Kara UI, Chang Y, Paulson JA, Qin R, Bao X, Wang X. Ultrasensitive and selective detection of SARS-CoV-2 using thermotropic liquid crystals and image-based machine learning. Cell Rep Phys Sci. 2020;1:100276. doi: 10.1016/j.xcrp.2020.100276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Liang C, Liu B, Li J, Lu J, Zhang E, Deng Q, Zhang L, Chen R, Fu Y, Li C, Li T. Sensors and actuators: B. Chemical A nanoenzyme linked immunochromatographic sensor for rapid and quantitative detection of SARS-CoV-2 nucleocapsid protein in human blood. Sens Actuators B Chem. 2021;349:130718. doi: 10.1016/j.snb.2021.130718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Dou Y, Su J, Chen S, Li T, Wang L, Ding X, Song S, Fan C. A smartphone-based three-in-one biosensor for co-detection of SARS-CoV-2 viral RNA, antigen and antibody. Chem Commun. 2022;58:6108–6111. doi: 10.1039/D2CC01297A. [DOI] [PubMed] [Google Scholar]
- 146.Fabiani L, Mazzaracchio V, Moscone D, Fillo S, De Santis R, Monte A, Amatore D, Lista F, Arduini F. Biosensors and Bioelectronics Paper-based immunoassay based on 96-well wax-printed paper plate combined with magnetic beads and colorimetric smartphone-assisted measure for reliable detection of SARS-CoV-2 in saliva. Biosens Bioelectron. 2022;200:113909. doi: 10.1016/j.bios.2021.113909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Yin K, Ding X, Xu Z, Li Z, Wang X, Zhao H, Otis C, Li B, Liu C. Sensors and actuators: B. Chemical multiplexed colorimetric detection of SARS-CoV-2 and other pathogens in wastewater on a 3D printed integrated microfluidic chip. Sens Actuators B Chem. 2021;344:130242. doi: 10.1016/j.snb.2021.130242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Hemamalini V, Anand L, Nachiyappan S, Geeitha S, Ramana Motupalli V, Kumar R, Ahilan A, Rajesh M. Integrating bio medical sensors in detecting hidden signatures of COVID-19 with artificial intelligence. Measurement. 2022;194:111054. doi: 10.1016/j.measurement.2022.111054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Kaushik AK, Dhau JS, Gohel H, Mishra YK, Kateb B, Kim N-Y, Goswami DY. Electrochemical SARS-CoV-2 sensing at point-of-care and artificial intelligence for intelligent COVID-19 management. ACS Appl Bio Mater. 2020;3:7306–7325. doi: 10.1021/acsabm.0c01004. [DOI] [PubMed] [Google Scholar]
- 150.Banerjee A, Ray S, Vorselaars B, Kitson J, Mamalakis M, Weeks S, Baker M, Mackenzie LS. Use of machine learning and artificial intelligence to predict SARS-CoV-2 infection from full blood counts in a population. Int Immunopharmacol. 2020;86:106705. doi: 10.1016/j.intimp.2020.106705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Jansson M, Rubio J, Gavaldà R, Rello J. Artificial Intelligence for clinical decision support in critical care, required and accelerated by COVID-19. Anaesth Crit Care Pain Med. 2020;39:691–693. doi: 10.1016/j.accpm.2020.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Yadav AK, Verma D, Kumar A, Kumar P, Solanki PR. The perspectives of biomarker-based electrochemical immunosensors, artificial intelligence and the internet of medical things toward COVID-19 diagnosis and management. Mater Today Chem. 2021;20:100443. doi: 10.1016/j.mtchem.2021.100443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Thapa S, Singh KRB, Verma R, Singh J. State-of-the-art smart and intelligent nanobiosensors for SARS-CoV-2 diagnosis. Biosensors. 2022;12(8):1–27. doi: 10.3390/bios12080637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Hashmi A, Nayak V, Rb K, Jain B, Baid M, Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID-19. The COVID-19 resource centre is hosted on Elsevier Connect, the company’ s public news and information website. Elsevier hereby grants permission to make all its COVID-19-related research that is available on the COVID-19 resource centre—including this research content—immediately available in PubMed Central and other publicly funded repositories, such as the WHO COVID database with rights for unrestricted research re-use and analyses in any form or by any means with acknowledgement of the original source. These permissions are granted for free by Elsevier for as long as the COVID-19 resource centre remains active. Potentialities of graphene and its allied derivatives to combat against SARS-CoV-2 infection, 2020.
- 155.Singh KRB, Rathee S, Nagpure G, Singh J, Pratap R. Smart and emerging nanomaterials-based biosensor for SARS-CoV-2 detection. Mater Lett. 2022;307:131092. doi: 10.1016/j.matlet.2021.131092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Elnathan R, Tay A, Voelcker NH, Chiappini C. The start-ups taking nanoneedles into the clinic. Nat Nanotechnol. 2022 doi: 10.1038/s41565-022-01158-5. [DOI] [PubMed] [Google Scholar]
- 157.Yasri S, Wiwanitkit V. Sustainable materials and COVID-19 detection biosensor: a brief review. Sensors Int. 2022;3:100171. doi: 10.1016/j.sintl.2022.100171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Kanwar VS, Sharma A, Rinku M, Kanwar AL, Srivastav DKS. An overview for biomedical waste management during pandemic like COVID-19. Int J Environ Sci Technol. 2022 doi: 10.1007/s13762-022-04287-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Yang Q, Rosati G, Abarintos V, Aroca MA, Osma JF, Merkoçi A. Wearable and fully printed microfluidic nanosensor for sweat rate, conductivity, and copper detection with healthcare applications. Biosens Bioelectron. 2022;202:114005. doi: 10.1016/j.bios.2022.114005. [DOI] [PubMed] [Google Scholar]
- 160.Verma D, Singh KRB, Yadav AK, Nayak V, Singh J, Solanki PR, Singh RP. Internet of things (IoT) in nano-integrated wearable biosensor devices for healthcare applications. Biosens Bioelectron X. 2022;11:100153. doi: 10.1016/j.biosx.2022.100153. [DOI] [Google Scholar]
- 161.Wong CDS, Yeoh JX, Wu T, Manickam S, Pang CH. Biomass to nanoparticles: recent advances in the process and processing towards sustainability. Chem Eng Process Process Intensif. 2022;175:108908. doi: 10.1016/j.cep.2022.108908. [DOI] [Google Scholar]
- 162.Thakur M, Wang B, Verma ML. Development and applications of nanobiosensors for sustainable agricultural and food industries: Recent developments, challenges and perspectives. Environ Technol Innov. 2022;26:102371. doi: 10.1016/J.ETI.2022.102371. [DOI] [Google Scholar]
- 163.Amouzadeh Tabrizi M, Acedo P. An electrochemical impedance spectroscopy-based aptasensor for the determination of SARS-CoV-2-RBD using a carbon nanofiber & gold nanocomposite modified screen-printed electrode. Biosensors. 2022 doi: 10.3390/bios12030142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Priye A, Bird SW, Light YK, Ball CS, Negrete OA, Meagher RJ. A smartphone-based diagnostic platform for rapid detection of Zika, chikungunya, and dengue viruses. Sci Rep. 2017;7:44778. doi: 10.1038/srep44778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Zhu H, Podesva P, Liu X, Zhang H, Teply T, Xu Y, Chang H, Qian A, Lei Y, Li Y, Niculescu A, Iliescu C, Neuzil P. IoT PCR for pandemic disease detection and its spread monitoring. Sens Actuators B Chem. 2020;303:127098. doi: 10.1016/j.snb.2019.127098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Dalal A, Gill PS, Narang J, Prasad M, Mohan H. Genosensor for rapid, sensitive, specific point-of-care detection of H1N1 influenza (swine flu) Process Biochem. 2020;98:262–268. doi: 10.1016/j.procbio.2020.09.016. [DOI] [Google Scholar]
- 167.Sailapu SK, Macchia E, Merino-Jimenez I, Esquivel JP, Sarcina L, Scamarcio G, Minteer SD, Torsi L, Sabaté N. Standalone operation of an EGOFET for ultra-sensitive detection of HIV. Biosens Bioelectron. 2020;156:112103. doi: 10.1016/j.bios.2020.112103. [DOI] [PubMed] [Google Scholar]
- 168.Zhao H, Liu F, Xie W, Zhou TC, OuYang J, Jin L, Li H, Zhao CY, Zhang L, Wei J, Zhang YP, Li CP. Ultrasensitive supersandwich-type electrochemical sensor for SARS-CoV-2 from the infected COVID-19 patients using a smartphone. Sens Actuators B Chem. 2021;327:128899. doi: 10.1016/j.snb.2020.128899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Pandit S, Banerjee T, Srivastava I, Nie S, Pan D. Machine learning-assisted array-based biomolecular sensing using surface-functionalized carbon dots. ACS Sens. 2019;4:2730–2737. doi: 10.1021/acssensors.9b01227. [DOI] [PubMed] [Google Scholar]
- 170.Brangel P, Sobarzo A, Parolo C, Miller BS, Howes PD, Gelkop S, Lutwama JJ, Dye JM, McKendry RA, Lobel L, Stevens MM. A serological point-of-care test for the detection of IgG antibodies against ebola virus in human survivors. ACS Nano. 2018;12:63–73. doi: 10.1021/acsnano.7b07021. [DOI] [PubMed] [Google Scholar]
- 171.Kaushik A, Yndart A, Kumar S, Jayant RD, Vashist A, Brown AN, Li C-Z, Nair M. A sensitive electrochemical immunosensor for label-free detection of Zika-virus protein. Sci Rep. 2018;8:9700. doi: 10.1038/s41598-018-28035-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Farooq S, Wali F, Zezell DM, De Araujo RE. Optimizing and quantifying gold nanospheres based on lspr label-free biosensor for dengue diagnosis. Polymers. 2022;14(8):1592. doi: 10.3390/polym14081592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Wei H, Peng Z, Yang C, Tian Y, Sun L, Wang G, Liu M. Three-dimensional Au/Ag nanoparticle/crossed carbon nanotube SERS substrate for the detection of mixed toxic molecules. Nanomater (Basel, Switzerland). 2021;11:2026. doi: 10.3390/nano11082026. [DOI] [PMC free article] [PubMed] [Google Scholar]