Abstract
Objective:
To investigate the association between children’s health-related quality of life (HRQoL) and childhood attention-deficit/hyperactivity disorder (ADHD).
Method:
Databases were systematically searched for peer-reviewed literature published between 2010 and 2022. Two reviewers independently screened and assessed the quality of included studies. Meta-analysis was conducted for studies that used the Pediatric Quality of Life Inventory (PedsQL).
Results:
Twenty-three studies were included, with most rated as “good” quality. Meta-analysis found “very large” effect in both parent- (Hedges’ g −1.67, 95% CI [−2.57, −0.78]) and child-reported (Hedges’ g −1.28, 95% CI [−2.01, −0.56]) HRQoL for children with ADHD compared to children without ADHD. No difference between parent- and child-reported HRQoL in children with and without ADHD was found. However, parent-reported HRQoL was lower than child-reported HRQoL among children with ADHD.
Conclusion:
ADHD was associated with substantially poorer children’s HRQoL. Among children with ADHD, parents rated their children’s HRQoL lower than the children themselves.
Keywords: HRQoL, ADHD, children and adolescents
Introduction
Childhood-onset attention-deficit/hyperactivity disorder (ADHD) is the most prevalent neurodevelopmental disorder globally (Asherson et al., 2016; Franke et al., 2018). ADHD is characterized by levels of inattention, impulsivity, and hyperactivity that are developmentally inappropriate and contribute to impairment in daily life (American Psychology Association, 2013; Costa Dias et al., 2013). The overall prevalence of ADHD in children was reported as 7.2% worldwide (Thomas et al., 2015). On average, children tend to be diagnosed with ADHD around the age of 7 in the US (Visser et al., 2014).
A robust body of evidence suggests that children with ADHD are at increased risk for other co-occurring conditions, including depression, anxiety, and substance use disorders (Asherson et al., 2016; Costa Dias et al., 2013). Additionally, ADHD is associated with lower educational or occupational achievement, reduced social functioning (Costa Dias et al., 2013; Franke et al., 2018), and increased risk of mortality driven by unnatural causes such as accidents (Dalsgaard et al., 2015), criminality (Dalsgaard et al., 2013), and suicidal behavior (Ljung et al., 2014). Evidence also suggests that children and adolescents with ADHD face significant stigmatization (Lebowitz, 2016) and increased victimization and bullying (Singh et al., 2010). On the other hand, there are ADHD-associated strengths related to children’s personality functions, such as high focus and energy, creativity, empathy, and agreeableness (Mahdi et al., 2017).
In recent years, the concept of quality of life (QoL) has become increasingly incorporated into health status evaluation as health-related quality of life (HRQoL) (D. Coghill et al., 2009; Danckaerts et al., 2010). While HRQoL and QoL have been used interchangeably (Karimi & Brazier, 2016), there are often confusions or misinterpretations on these terms (D. Coghill et al., 2009; Karimi & Brazier, 2016). In brief, QoL is a broad concept which measures someone’s perception of their life in terms of culture and value systems as well as about their standards, expectations, goals, and concerns (WHOQOL Group, 1995). On the other hand, the focus of HRQoL is on more the impacts of a disease or a health condition, and it does not measure some QoL aspects that are irrelevant to a health condition such as cultural and political attributes (Ferrans et al., 2005). As the most commonly accepted definition (Dey et al., 2012), HRQoL as a health status measure incorporates the holistic definition of health (World Health Organization, 2022) and provides insight into self-perceived wellbeing—that is, whether a patient “feels” healthy—and thus contributes to understanding the burden of a condition in terms of physical, psychological, and social functioning beyond simply symptomology (Celebre et al., 2021; D. Coghill et al., 2009; Dey et al., 2012).
HRQoL is, therefore, an important outcome measure and a meaningful opportunity to understand the impact of a condition on an individual’s life (Danckaerts et al., 2010; Dolan, 2000; Romero et al., 2013). Enhancing understanding of how conditions such as ADHD influence HRQoL can also provide directional insights for patient-centered service planning and supports to optimize outcomes for individuals (Danckaerts et al., 2010; Dolan, 2000; Romero et al., 2013; Sharpe et al., 2016).
When measuring overall functioning of children with ADHD, there are inconsistencies between HRQoL measurement tools as to how the domains are defined and what is included in each (D. Coghill et al., 2009; Danckaerts et al., 2010). Therefore, it can be difficult to corroborate and compare results from different HRQoL measurement tools. Both child self-reporting and parent-proxy reports have been used to measure HRQoL in children with ADHD, exhibiting a moderate agreement between these two raters (Bastiaansen et al., 2004). De Los Reyes et al. (2015) suggested that representation of a construct being measured in a child through parent- or teacher-reports should not be expected to be free from errors. Although parent-proxy reports may differ from children’s self-reported HRQoL in subjective experience and perception, they contribute to understanding HRQoL by providing complementary information (Bastiaansen et al., 2004; Danckaerts et al., 2010; Dey et al., 2012; Lee et al., 2016). Discrepancies between raters can be used to reveal key information regarding a child’s behavior in different contexts such as home or school, predicting poor outcomes on children, and identifying treatment outcome patterns (De Los Reyes, 2011). There is currently no agreed-upon “gold standard” for measuring children’s HRQoL, which makes it difficult to establish the validity of HRQoL tools (Danckaerts et al., 2010), particularly across a range of child age and cognitive abilities.
There are several previous systematic reviews exploring the impact of ADHD on children’s HRQoL (D. Coghill, 2010; Danckaerts et al., 2010; Galloway & Newman, 2017; Wehmeier et al., 2010) and two meta-analyses (Klassen, 2005; Lee et al., 2016). Specifically, these reviews found that ADHD significantly reduces children’s HRQoL, particularly from a parent’s perspective. Medication was associated with higher HRQoL in the short term (D. Coghill, 2010), while more significant social and emotional impairment was associated with lower HRQoL (Wehmeier et al., 2010). The impact of ADHD varies across domains of HRQoL, with a stronger association found for psychosocial than physical domains (Klassen, 2005; Lee et al., 2016). Some studies found disagreement between raters, with parent-proxy raters assigning lower HRQoL scores than children themselves (Danckaerts et al., 2010; Galloway & Newman, 2017), but Lee et al. (2016) found no difference between raters.
These reviews included literature published over 7 to 10 years ago. Given the growing research in this area over the past 10 years, an updated systematic review is needed to understand what is known more recently about the impact of ADHD on children and adolescents’ HRQoL. This knowledge will assist population health clinicians and policy-makers to effectively design interventions that can help improve children’s health and wellbeing among those living with ADHD. Therefore, we conducted a systematic review and a meta-analysis to synthesize the evidence on the relationship between childhood ADHD and children’s HRQoL, as well as the discrepancy of children’s HRQoL between parent- and child-reported HRQoL. We hypothesized that there is a negative association between childhood ADHD and children’s HRQoL.
Methods
The systematic review adhered to and was reported based on the PRISMA 2020 guidelines (Page et al., 2021) and was registered in PROSPERO, ID number CRD42017071889 (Wanni Arachchige Dona et al., 2022).
Identification of Studies
The following databases were systematically searched for literature published in English: MEDLINE, The Cochrane Library, EconLit, Embase, PsycINFO, CINAHL, DARE/NHSEED/HTA. As we aim to explore contemporary literature in the field of ADHD and children’s HRQoL, the search was limited to publications between 1st January 2010 and 15th July 2022. The search terms included various terms for children, ADHD, and HRQoL (see Appendix 1).
Inclusion and Exclusion Criteria
Peer-reviewed studies were included if they: (1) focused on children and adolescents (between 0 and 18 years old), (2) included children with a formal diagnosis (that requires symptoms and impairment).Those with high symptoms for whom impairment was not formally assessed, we included studies that examined HRQoL in children (i) who met criteria for a diagnosis of ADHD which was diagnosed by any approach (e.g., previously diagnosed, diagnostic interview or above threshold on rating scales) or (ii) had high levels of ADHD symptoms rated using a validated rating scale, and (3) had a comparison group of children without ADHD. No restriction on HRQoL measures was applied. We considered all HRQoL measures, including ADHD-specific or generic measures, for example, Pediatric Quality of Life Inventory (PedsQL), EuroQoL-5D-Youth (EQ-5D-Y), and the Inventory of Quality of Life in Children and Adolescents (ILK). Studies were excluded if they did not meet the above criteria, or if they were: (1) not published in English, (2) published before 2010, (3) literature reviews, (4) qualitative studies, (5) grey literature, or (6) on non-human subjects.
Study Selection and Data Extraction
All studies identified in the initial search underwent title and abstract screening by two reviewers (NB and SWAD) independently using Covidence (Veritas Health Innovation, 2020). Any disagreement between the reviewers resulted in the paper being retained for full-text screening. The remaining papers underwent full-text screening by the two reviewers (NB and SWAD) independently. Inter-rater reliability for the agreement between the two raters was tested using Cohen’s Kappa, resulting in a strong level of agreement (McHugh, 2012) at 0.81 and 0.87 Kappa value for title and abstract screening and full-text screening, respectively. Disagreements were discussed between the three reviewers (NB, SWAD, and HL) until a consensus was reached. One reviewer (NB) extracted data using MS Excel, which was then checked for accuracy by the other two reviewers (HL and SWAD), with an almost perfect level of agreement at 1.00 Kappa value for inter-rater reliability (McHugh, 2012). The data extracted included: the study population, the HRQoL instrument, whether the children’s HRQoL was self-reported or parent-reported, overall study results, and HRQoL scores (mean, SD), effect sizes, and p values where possible. The data were narratively synthesized by identifying common themes across studies following the guidelines by Braun and Clarke (2006).
Quality Assessment
Quality assessment was conducted independently by two reviewers (NB and SWAD) on the included studies using the National Heart, Lung, and Blood Institute (NHLBI, 2014) quality assessment checklists for cohort, cross-sectional, and case-control studies. Any discrepancies were discussed and resolved between the three reviewers (NB, SWAD, and HL). As per previous literature using the same checklists (Gundmi et al., 2018; Sabeena et al., 2017), a “yes” option for each of the criteria was given a score of one, and the overall quality of studies was rated as “good,” “fair,” and “poor” when the overall score was ≥6, 4 to 5, and <4, respectively. Cohort, cross-sectional, and randomized controlled trials could receive a maximum score of 14, while the maximum score for case-control studies is 12. NHLBI allows to evaluate internal validity of studies by assessing the potential for bias where a “good” study represents the least risk of bias. The tool consists of 12 to 14 items assessing sources of bias such as patient selection, study power, and confounding (NHLBI, 2014). NHLBI has been widely used in previous literature reviews (Akpan et al., 2020; Gupta et al., 2017; Haighton et al., 2019; Ismaiel et al., 2021; Pires, 2022; Torres et al., 2020). Inter-rater reliability was conducted for the agreement between raters for each question of the assessment tools.
Meta-Analysis (Quantitative Analysis)
Of studies that used the same HRQoL measures, most commonly used HRQoL measure (PedsQL) was included in meta-analysis to minimize errors in interpretation. Meta-analysis was conducted using MetaXL software version 5.3 on Excel (Epi Gear, 2022). An aggregated level of the meta-analysis was conducted to calculate the pooled effect sizes (standardized mean difference) using a more robust inverse variance heterogeneity (IVhet) model. The IVhet model retains a correct coverage probability and a lower observed variance than the random effect model estimates despite heterogeneity (Doi et al., 2015). Hedges’ g score was calculated to estimate the standardized mean difference (effect size). Multiple models (n = 4) were separately run using table parameters differently to compare: (1) parent-reported HRQoL between children with and without ADHD, (2) child-reported HRQoL between children with and without ADHD, (3) parent- and child-reported HRQoL for children with ADHD, and (4) parent- and child-reported HRQoL for the children without ADHD. For the above first and second analysis, a negative Hedges g indicated that children with ADHD have a lower HRQoL than children without ADHD, and a positive value indicates the opposite. For the above third and fourth analysis, a negative Hedges g indicated that parent-reported HRQoL was lower than child-reported. The effect size is interpreted as huge, very large, large, medium, small, and very small if (absolute value) Hedges’ g is at least 2.0, 1.2, 0.8, 0.5, 0.2, and 0.01, respectively (Sawilowsky, 2009). When 95% confidence intervals for the mean overlap between two groups, it is considered a non-significant difference.
Cochrane Q test and I2 test were conducted to assess homogeneity. I2 test was conducted to assess the percentage of true variation of included studies, and the Q-test to assess the variation in effect sizes in studies. A p-value less than .05 was regarded as statistically significant. I2 at least 25%, 50%, and 75% are considered low, moderate, and high heterogeneity, respectively (Higgins & Thompson, 2002). Publication bias was assessed using the Luis Furuya-Kanamori (LFK) index, which is related to the Doi plot (Furuya-Kanamori et al., 2018). An LFK index less than 1 shows no asymmetry, an index from 1 to 2 indicates a minor asymmetry, and an index of more than 2 suggests a major asymmetry (Furuya-Kanamori et al., 2018).
Results
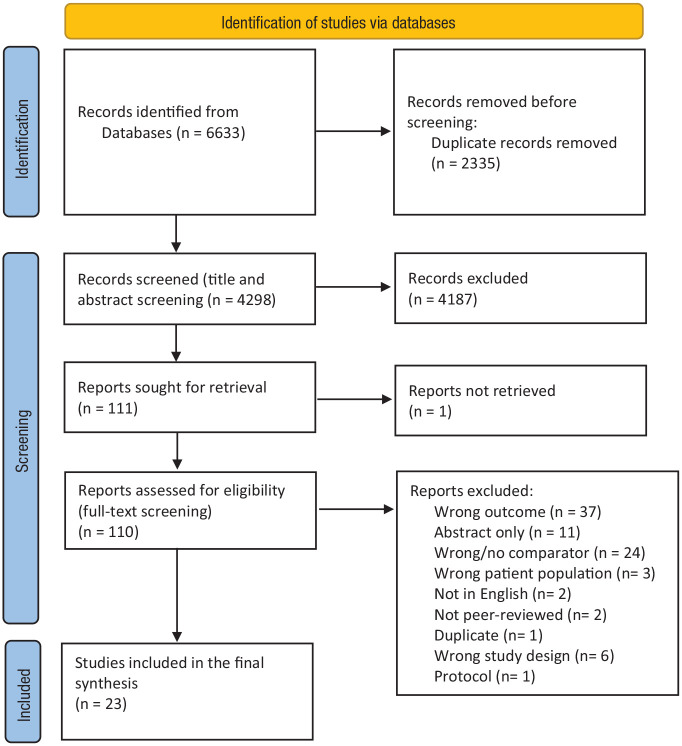
After duplicates were removed, 4,298 records were included in the title and abstract screening. Following this, 110 records underwent full-text screening, of which 23 were included for final synthesis (Figure 1). Table 1 presents the key characteristics of included studies, along with the quality assessment outcomes.
Figure 1.
PRISMA diagram.
Source. Adopted from: Page et al. (2021).
Table 1.
Summary of Studies and Main Outcomes.
| No. | Reference | Design | Country | HRQoL instrument | Sample (n); age | Outcomes in children with ADHD compared to children without ADHD | Quality of the study |
|---|---|---|---|---|---|---|---|
| Parent-reported | |||||||
| 1 | Bai et al. (2017) | Cross-sectional | Netherlands | CHQ-PF28 | ADHD n = 51; HC n = 4,539; 4–11-year-olds | Significant small effect on physical; physical score 59.93 (5.13) vs. 58.53 (4.28) for ADHD vs. control group*; large and significantly lower psychosocial scores; psychosocial score 46.57 (6.21) vs. 53.86 (5.87) for ADHD vs. control group | Good |
| 2 | Darweesh et al. (2021) | Cross-sectional | Egypt | PedsQL | ADHD n = 42; HC n = 42; 6–12-year-olds | Significant reduction in overall and individual domains; total score 125.76 (17.54) vs. 195.22 (3.81) for ADHD vs. control group; a correlation between subjective sleep problems/objective sleep parameters and PedsQL scores | Good |
| 3 | Green et al. (2016) | Cross-sectional | Australia | PedsQL | ADHD n = 164; HC n = 198; 6–10-year-olds | Significantly lower total and individual domain scores; total score 63.3 (13.7) vs. 81.7 (12.9) for ADHD vs. control group; ASD symptoms correlated with reduced HRQoL | Good |
| 4 | Grünwald and Schlarb (2017) | Cross-sectional | Germany | KINDL | ADHD n = 72; HC n = 79; 6–13-year-olds | Significantly lower HRQoL in children with all subtypes of ADHD; total score 69.39 (8.72) vs. 79 for ADHD-C vs. control group; reduced HRQoL in children with co-occurring sleep disorders than those without comorbidities | Good |
| 5 | Jamali et al. (2021) | Cross-sectional | Iran | POQL | ADHD/ODD n = 40; HC n = 80; 3–7-year-olds | Significantly higher dmft total scores; significantly poorer oral HRQoL; total score 0.096 (0.02) vs. 0.165 (0.01) for ADHD/ODD vs. control group | Good |
| 6 | Larsen et al. (2021) | Secondary analysis of RCT | Denmark | CHQ-PF28 | ADHD n = 164 (pre and post); 3–7-year-olds | Lower total and psychosocial scores; score for psychosocial domain 38.07 (10.72) vs. 52.10 (7.90) for ADHD vs. control group | Good |
| 7 | Telman et al. (2017) | Cross-sectional | Netherlands | KIDSCREEN-27 | ADHD-C n = 62; ADHD-I n = 64; HC n = 42; 6–21-year-olds (mean age 11.7) | Lower HRQoL scores across all domains, except for the school functioning; physical score 54.87 (11.12) vs. 57.77 (11.48) for ADHD-C vs. control group | Good |
| 8 | Maden and Gamlı (2022) | Cross-sectional | Turkey | The Turkish version of the ECOHIS (T-ECOHIS) | ADHD n = 76; HC n = 71; 6–13-year-olds | Significantly higher impact score, indicating poorer OHRQoL in children with ADHD than those without ADHD | Fair |
| Child self-reported | |||||||
| 9 | Dewey and Volkovinskaia (2018) | Cross-sectional | Canada | KIDSCREEN-52; PRQ | ADHD n = 9; HC n = 16; DCD n = 9; ADHD + DCD n = 10; 11–18-year-olds | No significant difference in total HRQoL scores; 201.78 (25.62) vs. 212.69 (17.21) for ADHD vs. control group; significantly lower scores in mood and emotions and school domains in children with DCD + ADHD; high victimization correlated with reduced HRQoL | Good |
| 10 | Peasgood et al. (2016) | Cross-sectional | UK | CHU-9D; EQ-5D-Y/EQ-VAS | ADHD n = 476; HC n = 196 (SYC) + 4,234 (USoc); 6–18-year-olds | Significantly lower HRQoL across all domains, including happiness with life and family; 80.16 (20.61) vs. 86.93 (14.71) for ADHD vs. control group in EQ-VAS; significantly poorer outcomes in schoolwork, sleep problems, daily routine, feeling annoyed, and joining in activities | Good |
| 11 | Schwörer et al. (2020) | Cross-sectional | Germany | ILK | ADHD with drug treatment n = 58; ADHD without drug treatment n = 42; HC n = 100; 6–12-year-olds | Significantly poorer total HRQoL in children with ADHD without drug treatment than healthy controls, including school and family domains; lower social HRQoL in children with ADHD and executive function problems than healthy control; total score 4.10 (1.04) vs. 4.60 (0.68) for ADHD vs. control group | Good |
| 12 | Zambrano-Sánchez et al. (2012) | Prospective cohort | Mexico | AUQUEI | ADHD n = 120; HC n = 96; 7–12-year-olds | Significantly lower HRQoL scores; significantly lower scores in domains of family life and social relationships, and functions performance*; total score 45.2 vs. 54.3 for ADHD vs. control group | Good |
| Combination of both parent- and child-reported | |||||||
| 13 | Becker et al. (2011) | Cross-sectional | Ireland | KINDL | ADHD n = 721 (pre and post); 6–17-year-olds | Significantly parent-reported lower scores on domains; total score 63.1 (13.3) vs. 66.6 (12.6) for parent vs. child rating | Good |
| 14 | Bussing et al. (2010) | Case-control | US | CIS; CHQ-PF28; YQOL | ADHD n = 169; HC n = 163; 6–17-year-olds | Significantly reduced parent-reported psychosocial scores; non-significant reduction in physical score; lower child-reported HRQoL; CIS score 51 vs. 32 for parents vs. child rating | Fair |
| 15 | D. Coghill and Hodgkins (2016) | Cross-sectional | Scotland | PedsQL; CHIP-CE | ADHD n = 213; HC n = 117; 6–16-year-olds | Reduced parent and child reported HRQoL; lower HRQoL with increased age, lower SES, and ADHD symptom severity; total score 62.1 (16.5) vs. 72.1 (15.5) for parents vs. child rating | Good |
| 16 | Göker et al. (2011) | Cross-sectional | Turkey | CQLS; Rosenburg Self Esteem Scale | ADHD n = 50; HC n = 30; 7–15-year-olds | Significantly lower parent-reported total and individual domain scores; no significant difference in child-reported HRQoL between children with and without ADHD, except school domain; significantly lower HRQoL in children with ADHD and low self-esteem than healthy control with low self-esteem; total score 56.7 (15.6) vs. 75.1 (15.8) for parents vs. child rating | Good |
| 17 | Jafari et al. (2011) | Cross-sectional | Iran | PedsQL | ADHD n = 72; HC n = 140; 8–18-year-olds | Significantly lower parent and child-reported total and individual scores (except parent-reported social domain); higher child scores than parents in children with and without ADHD; total score 57.06 (14.67) vs. 62.39 (17.20) for parents vs. child rating | Good |
| 18 | Kandemir et al. (2014) | Cross-sectional | Turkey | PedsQL | ADHD n = 76; HC n = 59; 7–16-year-olds | Significantly lower parent and child-reported total and psychosocial scores; total score 69.06 (14.32) vs. 72.13 (15.02) for parents vs. child rating | Good |
| 19 | Limbers et al. (2011) | Cross-sectional | US | PedsQL; PedsQL Family | ADHD n = 196; HC n = 876; 5–18-year-olds | Significantly lower parent and child-reported total and individual domain scores, particularly child-reported school and parent-reported psychosocial score; total score 69.88 (15.91) vs. 73.91 (17.19) for parents vs. child rating | Good |
| 20 | Marques et al. (2013) | Cross-sectional | Brazil | PedsQL | ADHD n = 45; HC n = 43; 8–12-year-olds | Significantly lower parent-reported total and individual domain scores; child-reported lower scores in all domains, but statistically significant lower scores in total, psychosocial, school, and social functioning; total score 67.10 (2.21) vs. 69.15 (2.37) for parents vs. child rating | Good |
| 21 | Thaulow and Jozefiak (2012) | Cross-sectional | Norway | ILK; C-GAS | ADHD n = 62; Anxiety/depression n = 49; HC n = 65; 8–15.5-year-olds | Significantly lower parent and child-reported HRQoL; significantly higher HRQoL in children with ADHD than children with anxiety or depression disorders; higher child-reported HRQoL than parent-reported scores in children with ADHD; total score 73.6 (14.9) vs. 62.5 (13.8) for parent vs. child rating | Fair |
| 22 | Velő et al. (2021) | Cross-sectional | Hungary | ILK | ADHD n = 79; HC n = 54; 6–18-year-olds | A significant negative weak correlation between peer relationships and child-reported HRQoL only in children with ADHD; a significant negative moderate correlation between peer relationships and parent-reported HRQoL in both children with ADHD and healthy control; total score 28.12 (5.40) vs. 29.17 (3.85) for parents vs. child rating | Good |
| 23 | Yürümez and Kılıç (2016) | Cross-sectional | Turkey | PedsQL | ADHD n = 46; HC n = 31; 7–13-year-olds | Significantly higher frequency of sleep problems; lower parent and child-reported HRQoL scores, even after correcting for having/not having sleep problems; total score 65.2 (15.1) vs. 68.8 (16) for parents vs. child rating | Fair |
Note. ADHD = Attention deficit hyperactivity disorder; HC = Healthy Control (Children without ADHD); HRQoL = Health-related Quality of life; ASD = autism spectrum disorder; AUQUEI = Auto Questionnaire Qualité de Vie-Enfant-Imagé; C-GAS = Children’s Global Assessment Scale; CHIP-CE = Child Health & Illness Profile-Child Edition; CHQ-PF28 = Child Health Questionnaire Parent Form28; CHU-9D = Child Health Utility 9D; CIS = Columbia Impairment Scale; CQLS = Children’s Quality of Life Scale; DCD = Developmental Coordination Disorder; dmft = decayed missing filled teeth; EQ-5D-Y = EuroQoL-5D-Youth; ILK = the Inventory of Quality of Life in Children and Adolescents; KINDL = a generic instrument to measure the quality of life in children; LIS = Impairment scale developed for Lifetime Impairment Survey; ODD = Oppositional Defiant Disorder; PedsQL = the Pediatric Quality of Life Inventory; POQL = Pediatric Oral Health-related Quality of Life; PRQ = Peer Relations Questionnaire; RCT = Randomized Control Trial; SES = Socioeconomic Status; SYC = South Yorkshire Cohort; USoc = Understanding Society: The UK’s Household Longitudinal Survey; YQOL = Youth Quality of Life questionnaire.
Study Characteristics
There were a broad range of different HRQoL instruments used in included studies such as the Child Health Questionnaire (CHQ) (n = 3), the Inventory of Quality of Life in Children and Adolescents (ILK) (n = 3), KINDL (n = 2), and the KIDSCREEN instrument (n = 2). The most commonly used HRQoL instrument was PedsQL (n = 8) (Table 1).
Among 23 included studies, most were cross-sectional (n = 20), with one cohort study, one case-control study, and one secondary analysis of a randomized controlled trial. Ten studies were from Europe, seven from the Middle East-North Africa region, five from the Americas, and one from Australia (Table 1). Half of the studies (n = 11) used both parent- and child-reported HRQoL measures, four studies used only child-reported, and eight relied solely on parent-reported HRQoL measures. Studies included children who were clinically diagnosed for ADHD (n = 18), or reported symptoms (presence of at least three main diagnostic criteria of the Diagnostic and Statistical Manual of Mental Disorders [DSM]) by their parents (n = 1) or categorized using various tools (e.g., DSM, parent questionnaires, and school report) by researchers (n = 4). Of 18 studies that included children with clinical diagnosis, the DSM-IV or V was the most common approach (n = 13 studies) to clinical diagnosis of ADHD. The quality of the majority of the studies (n = 19, 83%) was rated as “good.” Only four studies were rated as “fair,” and none were of “poor” quality (Appendix 2.1). Inter-rater reliability for the agreement between two raters was in a range of strong (0.80) to almost perfect (1.00) (Appendix 2.2).
Impact of ADHD on Children’s HRQoL
Narrative Synthesis
Self-Reported HRQoL of Children With ADHD Compared to Children Without ADHD
Child-reported overall HRQoL was found to be lower in children with ADHD than children without ADHD in all included studies, except one (Dewey & Volkovinskaia, 2018).
In regards to the association between ADHD and HRQoL domains, studies using the same child-reported HRQoL measure (i.e., PedsQL) (n = 6) found significantly lower HRQoL scores in the school and psychosocial domains (including social, emotional, and school domains) among children with ADHD compared to children without ADHD (D. Coghill & Hodgkins, 2016; Jafari et al., 2011; Kandemir et al., 2014; Limbers et al., 2011; Marques et al., 2013; Yürümez & Kılıç, 2016). Studies using other instruments also found consistently lower domain HRQoL scores in related domains (e.g., family life and social relationship) among children with ADHD than children without ADHD (Bussing et al., 2010; D. Coghill & Hodgkins, 2016; Dewey & Volkovinskaia, 2018; Göker et al., 2011; Peasgood et al., 2016; Schwörer et al., 2020; Thaulow & Jozefiak, 2012; Velő et al., 2021; Zambrano-Sánchez et al., 2012).
There are mixed findings in relation to the association between ADHD and physical domains of HRQoL. Five studies indicated that children with ADHD did not report any significant difference in the physical domain compared to children without ADHD (Bussing et al., 2010; Dewey & Volkovinskaia, 2018; Göker et al., 2011; Kandemir et al., 2014; Marques et al., 2013) while eight studies found significantly lower scores in physical domains in children with ADHD than children without ADHD (Becker et al., 2011; D. Coghill & Hodgkins, 2016; Jafari et al., 2011; Limbers et al., 2011; Peasgood et al., 2016; Thaulow & Jozefiak, 2012; Velő et al., 2021; Yürümez & Kılıç, 2016).
Among children with ADHD, children with ADHD treatment had higher HRQoL than those without treatment but even with medication treatment, children with ADHD still had lower HRQoL in the family domain than those without ADHD (Schwörer et al., 2020).
Parent-Reported HRQoL of Children With ADHD Compared to Children Without ADHD
A total of 19 studies used parent-proxy HRQoL measures. Similar to child-reported HRQoL, parents of children with ADHD consistently rated their child’s HRQoL lower than children without ADHD in all included studies (see Table 1). The association between ADHD and lower parent-reported HRQoL domain scores were also reported in the emotional, school, and psychosocial HRQoL domains (measured by the PedsQL) (Darweesh et al., 2021; Kandemir et al., 2014; Larsen et al., 2021; Limbers et al., 2011; Marques et al., 2013; Telman et al., 2017) and in achievement and risk avoidance (assessed using the Child Health & Illness Profile-Child Edition [CHIP-CE]) (D. Coghill & Hodgkins, 2016) in children with ADHD compared to children without ADHD.
Again, parent-proxy reports of HRQoL yielded inconsistent results for the physical domains of HRQoL among children with ADHD. The majority of studies (n = 12) found a significant reduction in physical HRQoL among children with ADHD than children without ADHD (Becker et al., 2011; D. Coghill & Hodgkins, 2016; Darweesh et al., 2021; Göker et al., 2011; Green et al., 2016; Grünwald & Schlarb, 2017; Jafari et al., 2011; Limbers et al., 2011; Telman et al., 2017; Thaulow & Jozefiak, 2012; Yürümez & Kılıç, 2016). However, Bai et al. (2017) found that parents reported a higher physical HRQoL on the Child Health Questionnaire (CHQ) for children with ADHD than for children without ADHD, and the authors gave the highly active nature of the condition as a possible reason. Other studies (n = 4) found no significant difference in parent-reported physical HRQoL in children with ADHD compared to children without ADHD (Bussing et al., 2010; Kandemir et al., 2014; Larsen et al., 2021; Marques et al., 2013).
Jamali et al. (2021), who examined the oral HRQoL among children with ADHD compared to children without ADHD, found significantly more decayed, missing, or filled teeth among children with ADHD than children without ADHD, and significantly lower scores across all domains of oral HRQoL (Jamali et al., 2021). Similarly, Maden and Gamlı (2022) reported poorer oral HRQoL in children with ADHD than those without ADHD.
Agreement Between Child- and Parent-Reported HRQoL
There were mixed findings on the agreement between parent- and child-reported HRQoL across studies. Marques et al. (2013) found a greater agreement between parent- and child-reported HRQoL among those with ADHD compared to children without ADHD across all domains except school functioning. D. Coghill and Hodgkins (2016) reported a significant correlation between parent and child ratings for PedsQL and CHIP-CE measures with low to moderate strength among all children. On the other hand, other studies found that children with ADHD rated their HRQoL higher than parent ratings (Göker et al., 2011; Jafari et al., 2011; Thaulow & Jozefiak, 2012).
Quantitative Analysis (Meta-Analysis) Findings
To minimize the difficulties resulting from pooling data and interpreting results of various HRQoL measures, studies that used the same HRQoL measure (i.e., PedsQL) reporting results in a consistent way were included in the meta-analysis (n = 8). Eight studies used a parent-reported measure and six used both parent and child-reported HRQoL measures using PedsQL. When the HRQoL of the children with ADHD was compared with more than one group, only comparison data from the group of children without ADHD were used.
Overall HRQoL
The pooled effect (the standardized mean difference) of ADHD on parent-reported children’s overall HRQoL for children with ADHD compared to children without ADHD was “very large” (Hedges’ g −1.67, 95% CI [−2.57, −0.78]). Similarly, the effect of ADHD on child-reported children’s HRQoL was also “very large” (Hedges’ g −1.28, 95% CI [−2.01, −0.56]) for children with ADHD compared to children without ADHD (see Appendix 3 for forest plots). The negative Hedges’ g values indicated that children with ADHD had a worse overall HRQoL than children without ADHD from both parent’s and children’s perspectives. There was no significant difference between parent-reported and child-reported HRQoL (i.e., there is an overlap between the 95% confidence interval of parent-reported [−2.57, −0.78] and child-reported children’s overall HRQoL [−2.01, −0.56]) when analyzing children with and without ADHD together.
However, for the subgroup of children with ADHD, there was a statistically significant difference between parent and child ratings, with parent ratings of their children’s HRQoL lower than the children’s ratings of their own HRQoL (Hedges g −0.49, 95% CI [−0.68, −0.31]) (Appendix 4). For the subgroup of children without ADHD, there was no significant difference between parent and child ratings (Hedges’ g 0.005, 95% CI [−1.08, 1.09]) (Appendix 5).
Individual Domains of Children’s HRQoL
We found a “medium” (Hedges’ g −0.79, 95% CI [−1.14, −0.45]) to “large” (Hedges’ g −0.88, 95% CI [−1.48, −0.29]) impact of ADHD on the physical domain in child- and parent-reported, respectively. A “very large” impact on psychosocial domain was found in both parent- (Hedges’ g −1.96, 95% CI [−3.24, −0.68]) and child-reported (Hedges’ g −1.42, 95% [CI −2.53, −0.32]) scorings (see Appendices 3.2 and 3.3). The impact of ADHD on the school domain was “very large” (Hedges’ g −1.29 and −1.79 for child- and parent-reported).
There was no significant difference between parent- and child-reported HRQoL for all individual domains across all children (Appendix 3). However, in the subgroup of children with ADHD, the difference between parent and child ratings of HRQoL was statistically significant for the physical (Hedges’ g −0.23, 95% CI [−0.37, −0.08]), psychosocial (Hedges’ g −0.50, 95% CI [−0.89, −0.11]), and emotional (Hedges’ g −0.52, 95% CI [−0.79, −0.25]) domains, but not for the other sub-domains of the psychosocial domain (i.e., school and social domains).
Heterogeneity and Publication Bias
Heterogeneity in effect sizes of difference between children with and without ADHD was significant for overall HRQoL from both parent (Q 245.47, p < .05) and child perspectives (Q 96.11, p < .05). The I2 test indicated a high heterogeneity at 97 and 95 for both parent and child ratings (I2 > 75%) (Appendix 6). The Luis Furuya-Kanamori (LFK) index indicated a major asymmetry for parent-reported overall, and psychosocial domains and a minor asymmetry for physical domain due to publication bias. Similarly, the LFK index for child-reported emotional, social, and school domains showed a major asymmetry and a minor asymmetry for overall and physical domains due to publication bias (Appendix 6).
Discussion
HRQoL is increasingly valued as a key element to understanding the impact of health problems on children, particularly with mental health issues (D. Coghill et al., 2009; Danckaerts et al., 2010) and is increasingly considered to be crucial to measure as a treatment outcome (Adamo et al., 2015). Given that previous reviews included literature published more than 7 to 10 years ago and the growing research in this area, this systematic review has synthesized contemporary literature (i.e., published since 2010) relating to the impact of ADHD on children’s HRQoL to better understand the impact of the condition. Consistent with previous reviews (D. Coghill, 2010; Danckaerts et al., 2010; Galloway & Newman, 2017; Klassen, 2005; Lee et al., 2016; Wehmeier et al., 2010), we found that both the children themselves and their parents reported poorer HRQoL in children with ADHD compared to children without ADHD. There was no difference between child and parent ratings of children’s HRQoL when HRQoL data from all children (with and without ADHD) were considered together. However, for the subgroup of children with ADHD, parents rated their child’s HRQoL lower than the children themselves.
The large number of studies that included child self-reported HRQoL measures suggests a positive growth in the use of individual self-perception instruments as a measure of child’s HRQoL. This is consistent with previous systematic reviews in this area which have found that child self-reporting is not interchangeable to parent-proxy ratings of child’s HRQoL (Danckaerts et al., 2010; Galloway & Newman, 2017). The differences in the agreement between parent- and child ratings of HRQoL in the included studies indicate the importance of including both proxy- and self-reported measures of HRQoL in research (D. Coghill et al., 2009; Dey et al., 2012; Jonsson et al., 2017). This is the approach used in half of included studies (11/23) in our review, which is much higher than the proportion of studies including both proxy-and self-rating HRQoL measures in previous reviews, for example, 4/16 in D. Coghill (2010) and 4/20 in Danckaerts et al. (2010).
There are possible explanations for the differences in parent and child rating. For example, Klassen et al. (2006) mentioned that ADHD symptoms and the associated impulsive cognitive style could influence how a child may complete a HRQoL questionnaire, highlighting the conceptual challenges of measuring HRQoL among children with ADHD. Waters et al. (2003) stated that the difference could be due to various health, social, and educational factors, such as parents with health issues or low sociodemographic status. De Los Reyes and Kazdin (2005) developed a theoretical framework on raters’ discrepancies in clinical research and provided attributions and perspectives as factors for child-parent discrepancies. For example, they proposed that as per parents, children’s disposition (i.e., being aggressive) contributes to their problems (e.g., aggressive behavior, hyperactivity, depression), while children often see the context or environment (i.e., protecting themselves from peers) as attributions to their problems, resulting in differences in ratings.
HRQoL is by definition self-evaluative, making self-reported instruments crucial in researching HRQoL outcomes (Varni & Burwinkle, 2006). There are, however, benefits and insights to be gained from proxy reports (Varni et al., 2007). In particular, when a child is too young, cognitively impaired, or severely ill, parent proxy reports are a reliable and valid option (Varni et al., 2007). Moreover, parents’ perception is crucial in health service utilization as they make decisions on child’s health in seeking care and treatment (Cremeens et al., 2006). Seeking treatments should be promoted as there are short-term and long-term positive effects of treatments on HRQoL in children with ADHD (D. Coghill, 2010).
Despite some differences between self-reported and parent proxy-report, the studies included in this review consistently demonstrated that regardless of self- or parent-proxy reporting, children and adolescents with ADHD experience a poorer overall HRQoL, particularly in the psychosocial domains, compared to children without ADHD. These findings align with previous reviews (Danckaerts et al., 2010; Jonsson et al., 2017; Lee et al., 2016; Orm & Fjermestad, 2021; Wehmeier et al., 2010). Larsen et al. (2022) found that children with ADHD are prone to frequent and severe functional somatic symptoms (e.g., stomach pain, tiredness, and headache), resulting in poor HRQoL with more emotional and behavioral difficulties than those without ADHD. Riley et al. (2006) reported that children’s HRQoL can be deteriorated because of ADHD symptoms, co-occurring health conditions (e.g., autism spectrum disorder), issues with peers, conduct and co-ordination as well as family issues such as parental sickness and behaviors (e.g., depressions/stress, maternal smoking) and family composition (e.g., divorced, living separately). Understanding these contributing factors to poor HRQoL is important to evaluate and improve treatment options for ADHD in children.
Our meta-analysis confirmed the large impact of ADHD on children and adolescents from both parents’ and children’s perspectives. Findings on the agreement in parent-reported and child-reported overall and individual domains of children’s HRQoL are consistent with the previous meta-analysis on HRQoL in children and adolescents with ADHD (Lee et al., 2016). Consistent with Lee et al. (2016)’s study, we found a “very large” impact of ADHD on psychosocial domain, with a “very large” impact on the school, emotional and social sub-domains. This evidence is consistent with literature exploring the impact of ADHD on academic performance (Arnold et al., 2020; Taanila et al., 2014) and highlights a need to provide adequate educational and behavioral support for children with ADHD at school. Population health interventions for ADHD also need to incorporate educational support services in addition to the pharmacological and behavioral interventions.
Consistent with previous reviews, we found that ADHD impacted more on the psychosocial domains than physical domains of HRQoL. However, slightly different to Lee et al. (2016)’s meta-analysis who found a moderate impact on physical domain, our meta-analysis found a “medium” and a “large” impact of ADHD on the physical domain respectively in child- and parent-reported HRQoL. It should be noted that our review and meta-analysis included more recent studies (from 2010 onward) while Lee et al. (2016)’s included studies prior to 2014, with only three studies common in both meta-analyses. Consistent with Lee et al. (2016), substantial heterogeneity was also found across studies which could be due to differences in study design and study participants. For example, four out of eight studies included in the meta-analysis included children with co-occurring conditions (e.g., ODD) which could have impacted these children’s HRQoL above and beyond ADHD itself (D. Coghill & Hodgkins, 2016; Limbers et al., 2011; Marques et al., 2013; Yürümez & Kılıç, 2016).
We extended the previous meta-analysis by exploring the agreement of self and proxy HRQoL reporting in the subgroup of children with ADHD. We found a significant difference between parent and child reporting on overall HRQoL as well as in the physical and emotional QoL domains, but no differences in the school and social domains. Consistent with Lee et al. (2016), this finding shows the importance of assessing children’s and adolescent’s HRQoL with ADHD using both parent proxy- and child self-reporting.
Strengths of this study include the broad search of the contemporary literature on the impact of ADHD on children’s HRQoL. Some limitations are noted. First, studies published in languages other than English, prior to 2010 and grey literature were not considered, and the review may have missed some literature due to this exclusion. Second, given that the studies included in the meta-analysis did not provide segregated PedsQL scoring for individual age groups or gender, subgroup analysis by age or gender could not be conducted. Given that age was associated with all domains of HRQoL as shown in Lee et al. (2016), further research should explore the age or gender effect on HRQoL among children with ADHD.
Findings about the large impact of ADHD on children’s HRQoL in our review and meta-analysis highlight a need for effective treatment (e.g., pharmacological [D. R. Coghill et al., 2017]) and behavioral treatment) and adequate support for these children. Children and adolescents with ADHD also experience poorer functional outcomes, which has been well-documented in previous literature as well as being an established diagnostic criterion for ADHD diagnosis (Cândido et al., 2021; Garner et al., 2013; Weiss, 2015). Furthermore, an ADHD diagnosis can increase the likelihood of experiencing victimization and bullying for a child, possibly due to the social stigma associated with ADHD (Lebowitz, 2016; Singh et al., 2010). It is, therefore, important to acknowledge the broader impact of ADHD on children and adolescent’s daily functionality so that sufficient support could be provided for children with ADHD. Given the school domain is severely impacted by ADHD, as evidenced in our meta-analysis, educational support for children with ADHD is essential.
Improving children’s HRQoL is increasingly identified as a key goal of ADHD treatment alongside clinical treatment outcomes and improvement in functional outcomes (Danckaerts et al., 2010), thus, routine inclusion of a generic HRQoL measure in health interventions for children with ADHD is encouraged. Future research should also incorporate both parent and child perspectives in HRQoL measures as both appear to be important in understanding the broad impact of ADHD on the child’s everyday life functioning/wellbeing.
Conclusion
This systematic review and meta-analysis found that children with ADHD had significantly poorer HRQoL than children without ADHD from both parents’ and children’s perspectives. The impact of ADHD on children’s HRQoL appeared to be “very large” for both parent- and child-reported HRQoL. There were no significant differences in parent-reported and child-reported HRQoL across all children. However, for the children with ADHD, there was a statistically significant difference between parent and child reporting on overall HRQoL, physical and psychosocial domains.
These findings highlight the need for effective ADHD treatment and for increased efforts to make ADHD treatment accessible for families. Strategies to treat or support children with ADHD should consider the child’s wellbeing rather than only the condition itself. Future studies exploring HRQoL in children with ADHD may consider including both parent- and child-reported HRQoL measures.
Supplemental Material
Supplemental material, sj-docx-1-jad-10.1177_10870547231155438 for The Impact of Childhood Attention-Deficit/Hyperactivity Disorder (ADHD) on Children’s Health-Related Quality of Life: A Systematic Review and Meta-Analysis by Sithara Wanni Arachchige Dona, Nalini Badloe, Emma Sciberras, Lisa Gold, David Coghill and Ha N. D. Le in Journal of Attention Disorders
Author Biographies
Sithara Wanni Arachchige Dona, MBBS, MPH, MHHSM, is an associate research fellow at Deakin Health Economics, Deakin University.
Nalini Badloe, BS, MHP, is a graduate of Deakin University.
Emma Sciberras, PhD, is a senior clinical psychologist and an associate professor at Deakin University.
Lisa Gold, PhD, is a professor in the economics of maternal and child health at Deakin Health Economics, Deakin University.
David Coghill, BSc, MBChB, MD, is the Chair of Developmental Mental Health at the University of Melbourne and a professor of child and adolescent psychiatry at the Royal Children's Hospital.
Ha N.D. Le, BScEcon, MHEcon, PhD, is a senior research fellow at Deakin Health Economics, Deakin University.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Author Ha N. D. Le received funding from Institute of Health Transformation/School of Health and Social Development (IHT/HSD) Cat 1 Seed Funding and Deakin Dean health postdoctoral fellowship.
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs: Sithara Wanni Arachchige Dona  https://orcid.org/0000-0002-3631-930X
https://orcid.org/0000-0002-3631-930X
Emma Sciberras  https://orcid.org/0000-0003-2812-303X
https://orcid.org/0000-0003-2812-303X
References
- Adamo N., Seth S., Coghill D. (2015). Pharmacological treatment of attention-deficit/hyperactivity disorder: Assessing outcomes. Expert Review of Clinical Pharmacology, 8(4), 383–397. 10.1586/17512433.2015.1050379 [DOI] [PubMed] [Google Scholar]
- Akpan M. R., Isemin N. U., Udoh A. E., Ashiru-Oredope D. (2020). Implementation of antimicrobial stewardship programmes in African countries: A systematic literature review. Journal of Global Antimicrobial Resistance, 22, 317–324. 10.1016/j.jgar.2020.03.009 [DOI] [PubMed] [Google Scholar]
- American Psychology Association. (2013). Diagnostic and statistical manual of mental disorders. [Google Scholar]
- Arnold L. E., Hodgkins P., Kahle J., Madhoo M., Kewley G. (2020). Long-term outcomes of ADHD: Academic achievement and performance. Journal of Attention Disorders, 24(1), 73–85. [DOI] [PubMed] [Google Scholar]
- Asherson P., Buitelaar J., Faraone S. V., Rohde L. A. (2016). Adult attention-deficit hyperactivity disorder: Key conceptual issues. The Lancet Psychiatry, 3(6), 568–578. 10.1016/S2215-0366(16)30032-3 [DOI] [PubMed] [Google Scholar]
- Bai G., Herten M. H., Landgraf J. M., Korfage I. J., Raat H. (2017). Childhood chronic conditions and health-related quality of life: Findings from a large population-based study. PLoS One, 12(6), e0178539. 10.1371/journal.pone.0178539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastiaansen D., Koot H. M., Ferdinand R. F., Verhulst F. C. (2004). Quality of life in children with psychiatric disorders: Self-, parent, and clinician report. Journal of the American Academy of Child and Adolescent Psychiatry, 43(2), 221–230. 10.1097/00004583-200402000-00019 [DOI] [PubMed] [Google Scholar]
- Becker A., Roessner V., Breuer D., Döpfner M., Rothenberger A. (2011). Relationship between quality of life and psychopathological profile: Data from an observational study in children with ADHD. European Child & Adolescent Psychiatry, 20(Suppl 2), S267–S275. 10.1007/s00787-011-0204-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V., Clarke V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. [Google Scholar]
- Bussing R., Mason D. M., Bell L., Porter P., Garvan C. (2010). Adolescent outcomes of childhood attention-deficit/hyperactivity disorder in a diverse community sample. Journal of the American Academy of Child and Adolescent Psychiatry, 49(6), 595–605. 10.1016/j.jaac.2010.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cândido R. C. F., Menezes de, Padua C. A., Golder S., Junqueira D. R. (2021). Immediate-release methylphenidate for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database of Systematic Reviews, 2021(1), CD013011. 10.1002/14651858.CD013011.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celebre A., Stewart S. L., Theall L., Lapshina N. (2021). An examination of correlates of quality of life in children and youth with mental health issues. Frontiers in Psychiatry, 12, 709516. 10.3389/fpsyt.2021.709516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coghill D. (2010). The impact of medications on quality of life in attention-deficit hyperactivity disorder: A systematic review. CNS Drugs, 24(10), 843–866. [DOI] [PubMed] [Google Scholar]
- Coghill D., Danckaerts M., Sonuga-Barke E., Sergeant J. (2009). Practitioner review: Quality of life in child mental health – Conceptual challenges and practical choices. Journal of Child Psychology & Psychiatry, 50(5), 544–561. 10.1111/j.1469-7610.2009.02008.x [DOI] [PubMed] [Google Scholar]
- Coghill D., Hodgkins P. (2016). Health-related quality of life of children with attention-deficit/hyperactivity disorder versus children with diabetes and healthy controls. European Child & Adolescent Psychiatry, 25(3), 261–271. 10.1007/s00787-015-0728-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coghill D. R., Banaschewski T., Soutullo C., Cottingham M. G., Zuddas A. (2017). Systematic review of quality of life and functional outcomes in randomized placebo-controlled studies of medications for attention-deficit/hyperactivity disorder. European Child & Adolescent Psychiatry, 26(11), 1283–1307. 10.1007/s00787-017-0986-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa Dias T. G., Kieling C., Graeff-Martins A. S., Moriyama T. S., Rohde L. A., Polanczyk G. V. (2013). Developments and challenges in the diagnosis and treatment of ADHD. Revista Brasileira de Psiquiatria, 35(Suppl 1), S40–S50. 10.1590/1516-4446-2013-S103 [DOI] [PubMed] [Google Scholar]
- Cremeens J., Eiser C., Blades M. (2006). Characteristics of health-related self-report measures for children aged three to eight years: A review of the literature. Quality of Life Research, 15(4), 739–754. [DOI] [PubMed] [Google Scholar]
- Dalsgaard S., Mortensen P. B., Frydenberg M., Thomsen P. H. (2013). Long-term criminal outcome of children with attention deficit hyperactivity disorder. Criminal Behaviour and Mental Health, 23(2), 86–98. [DOI] [PubMed] [Google Scholar]
- Dalsgaard S., Østergaard S. D., Leckman J. F., Mortensen P. B., Pedersen M. G. (2015). Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: A nationwide cohort study. Lancet, 385(9983), 2190–2196. [DOI] [PubMed] [Google Scholar]
- Danckaerts M., Sonuga-Barke E. J., Banaschewski T., Buitelaar J., Döpfner M., Hollis C., Santosh P., Rothenberger A., Sergeant J., Steinhausen H. C., Taylor E., Zuddas A., Coghill D. (2010). The quality of life of children with attention deficit/hyperactivity disorder: A systematic review. European Child & Adolescent Psychiatry, 19(2), 83–105. 10.1007/s00787-009-0046-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darweesh A. E. M., El Beh K. A., Hashem M. M., Nagy N. E. (2021). Shorter rapid eye movement sleep duration in children with attention-deficit /hyperactivity disorder: The impact on quality of life. Sleep Medicine, 87, 77–84. 10.1016/j.sleep.2021.07.034 [DOI] [PubMed] [Google Scholar]
- De Los Reyes A. (2011). Introduction to the special section: More than measurement error: Discovering meaning behind informant discrepancies in clinical assessments of children and adolescents. Journal of Clinical Child & Adolescent Psychology, 40(1), 1–9. 10.1080/15374416.2011.533405 [DOI] [PubMed] [Google Scholar]
- De Los Reyes A., Augenstein T. M., Wang M., Thomas S. A., Drabick D. A. G., Burgers D. E., Rabinowitz J. (2015). The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological Bulletin, 141(4), 858–900. 10.1037/a0038498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A., Kazdin A. E. (2005). Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin, 131(4), 483–509. [DOI] [PubMed] [Google Scholar]
- Dewey D., Volkovinskaia A. (2018). Health-related quality of life and peer relationships in adolescents with developmental coordination disorder and attention-deficit-hyperactivity disorder. Developmental Medicine and Child Neurology, 60(7), 711–717. 10.1111/dmcn.13753 [DOI] [PubMed] [Google Scholar]
- Dey M., Landolt M. A., Mohler-Kuo M. (2012). Health-related quality of life among children with mental disorders: A systematic review. Quality of Life Research, 21(10), 1797–1814. https://ezproxy.deakin.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&AuthType=sso&db=edsjsr&AN=edsjsr.41812135&authtype=sso&custid=deakin&site=eds-live&scope=site [DOI] [PubMed] [Google Scholar]
- Doi S. A., Barendregt J. J., Khan S., Thalib L., Williams G. M. (2015). Advances in the meta-analysis of heterogeneous clinical trials I: The inverse variance heterogeneity model. Contemporary Clinical Trials, 45, 130–138. [DOI] [PubMed] [Google Scholar]
- Dolan P. (2000). The measurement of health-related quality of life for use in resource allocation decisions in health care. In Culyer A. J., Newhouse J. P. (Eds.), Handbook of health economics (vol.1, pp. 1723–1760). Elsevier. [Google Scholar]
- Epi Gear. (2022). MetaXL Version 5.3. http://epigear.com/index_files/metaxl.html
- Ferrans C. E., Zerwic J. J., Wilbur J. E., Larson J. L. (2005). Conceptual model of health-related quality of life. Journal of Nursing Scholarship, 37(4), 336–342. [DOI] [PubMed] [Google Scholar]
- Franke B., Michelini G., Asherson P., Banaschewski T., Bilbow A., Buitelaar J. K., Cormand B., Faraone S. V., Ginsberg Y., Haavik J., Kuntsi J., Larsson H., Lesch K.-P., Ramos-Quiroga J. A., Réthelyi J. M., Ribases M., Reif A. (2018). Live fast, die young? A review on the developmental trajectories of ADHD across the lifespan. European Neuropsychopharmacology, 28(10), 1059–1088. 10.1016/j.euroneuro.2018.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuya-Kanamori L., Barendregt J. J., Doi S. A. R. (2018). A new improved graphical and quantitative method for detecting bias in meta-analysis. International Journal of Evidence-Based Healthcare, 16(4), 195–203. [DOI] [PubMed] [Google Scholar]
- Galloway H., Newman E. (2017). Is there a difference between child self-ratings and parent proxy-ratings of the quality of life of children with a diagnosis of attention-deficit hyperactivity disorder (ADHD)? A systematic review of the literature. ADHD Attention Deficit and Hyperactivity Disorders, 9(1), 11–29. 10.1007/s12402-016-0210-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner A. A., OʼConnor B. C., Narad M. E., Tamm L., Simon J., Epstein J. N. (2013). The relationship between ADHD symptom dimensions, clinical correlates, and functional impairments. Journal of Developmental and Behavioral Pediatrics: JDBP, 34(7), 469–477. 10.1097/DBP.0b013e3182a39890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Göker Z., Aktepe E., Kandil S. (2011). Self-esteem and quality of life in children and adolescents with attention deficit hyperactivity disorder. Yeni Symposium, 49, 209–216. [Google Scholar]
- Green J. L., Sciberras E., Anderson V., Efron D., Rinehart N. (2016). Association between autism symptoms and functioning in children with ADHD. Archives of Disease in Childhood, 101(10), 922–928. 10.1136/archdischild-2015-310257 [DOI] [PubMed] [Google Scholar]
- Grünwald J., Schlarb A. A. (2017). Relationship between subtypes and symptoms of ADHD, insomnia, and nightmares in connection with quality of life in children. Neuropsychiatric Disease and Treatment, 13, 2341–2350. 10.2147/ndt.S118076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gundmi S., Maiya A. G., Bhat A. K., Ravishankar N., Hande M. H., Rajagopal K. V. (2018). Hand dysfunction in type 2 diabetes mellitus: Systematic review with meta-analysis. Annals of Physical and Rehabilitation Medicine, 61(2), 99–104. [DOI] [PubMed] [Google Scholar]
- Gupta A., Huettner D. P., Dukewich M. (2017). Comparative effectiveness review of cooled versus pulsed radiofrequency ablation for the treatment of knee osteoarthritis: A systematic review. Pain Physician, 20(3), 155–171. [PubMed] [Google Scholar]
- Haighton L., Roberts A., Jonaitis T., Lynch B. (2019). Evaluation of aspartame cancer epidemiology studies based on quality appraisal criteria. Regulatory Toxicology and Pharmacology, 103, 352–362. 10.1016/j.yrtph.2019.01.033 [DOI] [PubMed] [Google Scholar]
- Higgins J. P. T., Thompson S. G. (2002). Quantifying heterogeneity in a meta-analysis. Statistics in Medicine, 21(11), 1539–1558. [DOI] [PubMed] [Google Scholar]
- Ismaiel A., Leucuta D.-C., Popa S.-L., Dumitrascu D. L. (2021). Serum visfatin levels in nonalcoholic fatty liver disease and liver fibrosis: Systematic review and meta-analysis. Journal of Clinical Medicine, 10(14), 3029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jafari P., Ghanizadeh A., Akhondzadeh S., Mohammadi M. R. (2011). Health-related quality of life of Iranian children with attention deficit/hyperactivity disorder. Quality of Life Research, 20(1), 31–36. 10.1007/s11136-010-9722-5 [DOI] [PubMed] [Google Scholar]
- Jamali Z., Ghaffari P., Aminabadi N. A., Norouzi S., Shirazi S. (2021). Oral health status and oral health-related quality of life in children with attention-deficit hyperactivity disorder and oppositional defiant disorder. Special Care in Dentistry, 41(2), 178–186. 10.1111/scd.12563 [DOI] [PubMed] [Google Scholar]
- Jonsson U., Alaie I., Löfgren Wilteus A., Zander E., Marschik P. B., Coghill D., Bölte S. (2017). Annual research review: Quality of life and childhood mental and behavioural disorders – A critical review of the research. Journal of Child Psychology and Psychiatry, 58(4), 439–469. 10.1111/jcpp.12645 [DOI] [PubMed] [Google Scholar]
- Kandemir H., Kilic B., Ekinci S., Yuce M. (2014). An evaluation of the quality of life of children with attention-deficit/hyperactivity disorder (ADHD) and their families. Anatolian Journal of Psychiatry, 15, 265–271. 10.5455/apd.46202 [DOI] [Google Scholar]
- Karimi M., Brazier J. (2016). Health, health-related quality of life, and quality of life: What is the difference? PharmacoEconomics, 34(7), 645–649. [DOI] [PubMed] [Google Scholar]
- Klassen A. F. (2005). Quality of life of children with attention deficit hyperactivity disorder. Expert Review of Pharmacoeconomics & Outcomes Research, 5(1), 95–103. [DOI] [PubMed] [Google Scholar]
- Klassen A. F., Miller A., Fine S. (2006). Agreement between parent and child report of quality of life in children with attention-deficit/hyperactivity disorder. Child Care Health and Development, 32(4), 397–406. 10.1111/j.1365-2214.2006.00609.x [DOI] [PubMed] [Google Scholar]
- Larsen L. B., Daley D., Lange A.-M., Sonuga-Barke E., Thomsen P. H., Jensen J. S., Rask C. U. (2022). Functional somatic symptoms in preschool attention-deficit/hyperactivity disorder: A secondary analysis of data from a randomized controlled trial of parent training. European Child & Adolescent Psychiatry. Advance online publication. 10.1007/s00787-022-02025-3 [DOI] [PubMed]
- Larsen L. B., Daley D., Lange A. M., Sonuga-Barke E., Thomsen P. H., Rask C. U. (2021). Effect of parent training on health-related quality of life in preschool children with attention-deficit/hyperactivity disorder: A secondary analysis of data from a randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 60(6), 734–744.e3. 10.1016/j.jaac.2020.04.014 [DOI] [PubMed] [Google Scholar]
- Lebowitz M. S. (2016). Stigmatization of ADHD: A developmental review. Journal of Attention Disorders, 20(3), 199–205. 10.1177/1087054712475211 [DOI] [PubMed] [Google Scholar]
- Lee Y.-C., Yang H.-J., Chen V. C. H., Lee W.-T., Teng M.-J., Lin C.-H., Gossop M. (2016). Meta-analysis of quality of life in children and adolescents with ADHD: By both parent proxy-report and child self-report using PedsQL™. Research in Developmental Disabilities, 51–52, 160–172. 10.1016/j.ridd.2015.11.009 [DOI] [PubMed] [Google Scholar]
- Limbers C. A., Ripperger-Suhler J., Boutton K., Ransom D., Varni J. W. (2011). A comparative analysis of health-related quality of life and family impact between children with ADHD treated in a general pediatric clinic and a psychiatric clinic utilizing the PedsQL. Journal of Attention Disorders, 15(5), 392–402. 10.1177/1087054709356191 [DOI] [PubMed] [Google Scholar]
- Ljung T., Chen Q., Lichtenstein P., Larsson H. (2014). Common etiological factors of attention-deficit/hyperactivity disorder and suicidal behavior: A population-based study in Sweden. JAMA Psychiatry, 71(8), 958–964. [DOI] [PubMed] [Google Scholar]
- Maden E. A., Gamlı İ. S. (2022). Oral Health and oral health-related quality of life in children with attention deficit hyperactivity disorder. The Journal of Pediatric Research, 9(2), 116–125. [Google Scholar]
- Mahdi S., Viljoen M., Massuti R., Selb M., Almodayfer O., Karande S., de Vries P. J., Rohde L., Bölte S. (2017). An international qualitative study of ability and disability in ADHD using the WHO-ICF framework. European Child & Adolescent Psychiatry, 26(10), 1219–1231. 10.1007/s00787-017-0983-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques J. C., Oliveira J. A., Goulardins J. B., Nascimento R. O., Lima A. M., Casella E. B. (2013). Comparison of child self-reports and parent proxy-reports on quality of life of children with attention deficit hyperactivity disorder. Health and Quality of Life Outcomes, 11, 186. 10.1186/1477-7525-11-186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh M. L. (2012). Interrater reliability: The kappa statistic. Biochemical Medicine, 22(3), 276–282. [PMC free article] [PubMed] [Google Scholar]
- National Heart, Lung, and Blood Institute (NHLBI). (2014). Study quality assessment tools. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- Orm S., Fjermestad K. (2021). A scoping review of psychosocial adjustment in siblings of children with attention-deficit/hyperactivity disorder. Advances in Neurodevelopmental Disorders, 5(4), 381–395. 10.1007/s41252-021-00222-w [DOI] [Google Scholar]
- Page M. J., McKenzie J. E., Bossuyt P. M., Boutron I., Hoffmann T. C., Mulrow C. D., Shamseer L., Tetzlaff J. M., Akl E. A., Brennan S. E., Chou R. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page M. J., Moher D., Bossuyt P. M., Boutron I., Hoffmann T. C., Mulrow C. D., Shamseer L., Tetzlaff J. M., Akl E. A., Brennan S. E., Chou R., Glanville J., Grimshaw J. M., Hróbjartsson A., Lalu M. M., Li T., Loder E. W., Mayo-Wilson E., McDonald S., . . . McKenzie J. E. (2021). PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ, 372, n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peasgood T., Bhardwaj A., Biggs K., Brazier J. E., Coghill D., Cooper C. L., Daley D., De Silva C., Harpin V., Hodgkins P., Nadkarni A., Setyawan J., Sonuga-Barke E. J. (2016). The impact of ADHD on the health and well-being of ADHD children and their siblings. European Child & Adolescent Psychiatry, 25(11), 1217–1231. 10.1007/s00787-016-0841-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pires C. (2022). Global predictors of COVID-19 vaccine hesitancy: A systematic review. Vaccines, 10(8), 1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley A. W., Spiel G., Coghill D., Döpfner M., Falissard B., Lorenzo M. J., Preuss U., Ralston S. J.; ADORE Study Group. (2006). Factors related to health-related quality of life (HRQoL) among children with ADHD in Europe at entry into treatment [corrected] [published erratum appears in Eur Child Adolesc Psychiatry 2009 Mar;18(3):194-6]. European Child & Adolescent Psychiatry, 15, i38–i45. https://ezproxy.deakin.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=mdc&AN=EPTOC106114349&site=eds-live&scope=site [DOI] [PubMed] [Google Scholar]
- Romero M., Vivas-Consuelo D., Alvis-Guzman N. (2013). Is Health Related Quality of Life (HRQoL) a valid indicator for health systems evaluation? SpringerPlus, 2(1), 664. 10.1186/2193-1801-2-664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabeena S., Bhat P. V., Kamath V., Bhat S. H. K., Nair S. N, R., Chandrabharani K., Arunkumar G. (2017). Community-based prevalence of genital human papilloma virus (HPV) infection: A systematic review and meta-analysis. Asian Pacific Journal of Cancer Prevention: APJCP, 18(1), 145–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawilowsky S. S. (2009). New effect size rules of thumb. Journal of Modern Applied Statistical Methods, 8(2), 597–599. [Google Scholar]
- Schwörer M. C., Reinelt T., Petermann F., Petermann U. (2020). Influence of executive functions on the self-reported health-related quality of life of children with ADHD. Quality of Life Research, 29(5), 1183–1192. 10.1007/s11136-019-02394-4 [DOI] [PubMed] [Google Scholar]
- Sharpe H., Patalay P., Fink E., Vostanis P., Deighton J., Wolpert M. (2016). Exploring the relationship between quality of life and mental health problems in children: Implications for measurement and practice. European Child & Adolescent Psychiatry, 25(6), 659–667. 10.1007/s00787-015-0774-5 [DOI] [PubMed] [Google Scholar]
- Singh I., Kendall T., Taylor C., Mears A., Hollis C., Batty M., Keenan S. (2010). Young people’s experience of ADHD and stimulant medication: A qualitative study for the NICE guideline. Child and Adolescent Mental Health, 15(4), 186–192. 10.1111/j.1475-3588.2010.00565.x [DOI] [PubMed] [Google Scholar]
- Taanila A., Ebeling H., Tiihala M., Kaakinen M., Moilanen I., Hurtig T., Yliherva A. (2014). Association between childhood specific learning difficulties and school performance in adolescents with and without ADHD symptoms: A 16-year follow-up. Journal of Attention Disorders, 18(1), 61–72. [DOI] [PubMed] [Google Scholar]
- Telman L. G. E., van Steensel F. J. A., Maric M., Bögels S. M. (2017). Are anxiety disorders in children and adolescents less impairing than ADHD and autism spectrum disorders? Associations with child quality of life and parental stress and psychopathology. Child Psychiatry and Human Development, 48(6), 891–902. 10.1007/s10578-017-0712-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thaulow C. M., Jozefiak T. (2012). A comparison between child psychiatric outpatients with AD/HD and anxiety/depression. Nordic Journal of Psychiatry, 66(6), 396–402. 10.3109/08039488.2012.660546 [DOI] [PubMed] [Google Scholar]
- Thomas R., Sanders S., Doust J., Beller E., Glasziou P. (2015). Prevalence of attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Pediatrics, 135(4), e994–e1001. [DOI] [PubMed] [Google Scholar]
- Torres D., Lopes J., Magno M. B., Cople Maia L., Normando D., Leão P. B. (2020). Effects of rapid maxillary expansion on temporomandibular joints. The Angle Orthodontist, 90(3), 442–456. 10.2319/080619-517.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varni J. W., Burwinkle T. M. (2006). The PedsQL as a patient-reported outcome in children and adolescents with attention-deficit/hyperactivity disorder: A population-based study. Health and Quality of Life Outcomes, 4, 26. 10.1186/1477-7525-4-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varni J. W., Limbers C. A., Burwinkle T. M. (2007). Parent proxy-report of their children’s health-related quality of life: An analysis of 13,878 parents’ reliability and validity across age subgroups using the PedsQL 4.0 Generic Core Scales. Health and Quality of Life Outcomes, 5, 2. 10.1186/1477-7525-5-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velő S., Keresztény Ferenczi-Dallos G, Pump L, Móra K, Balázs J. (2021). The association between prosocial behaviour and peer relationships with comorbid externalizing disorders and quality of life in treatment-naïve children and adolescents with attention deficit hyperactivity disorder. Brain Sciences, 11(4), 475. 10.3390/brainsci11040475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veritas Health Innovation. (2020). Covidence systematic review software. [Google Scholar]
- Visser S. N., Danielson M. L., Bitsko R. H., Holbrook J. R., Kogan M. D., Ghandour R. M., Perou R., Blumberg S. J. (2014). Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003-2011. Journal of the American Academy of Child and Adolescent Psychiatry, 53(1), 34–46.e2. 10.1016/j.jaac.2013.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wanni Arachchige Dona S., Badloe N., Sciberras E., Gold L., Coghill D., Le H. (2022) The impact of childhood attention-deficit/hyperactivity disorder (ADHD) on children's health-related quality of life: A systematic review and meta-analysis. PROSPERO 2017 CRD42017071889 Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42017071889 [DOI] [PMC free article] [PubMed]
- Waters E., Stewart-Brown S., Fitzpatrick R. (2003). Agreement between adolescent self-report and parent reports of health and well-being: Results of an epidemiological study. Child Care Health and Development, 29, 501–509. [DOI] [PubMed] [Google Scholar]
- Wehmeier P. M., Schacht A., Barkley R. A. (2010). Social and emotional impairment in children and adolescents with ADHD and the impact on quality of life. Journal of Adolescent Health, 46(3), 209–217. 10.1016/j.jadohealth.2009.09.009 [DOI] [PubMed] [Google Scholar]
- Weiss M. (2015). Functional impairment in ADHD. In Adler L. A., Spencer T. J., Wilens T. E. (Eds.), Attention-deficit hyperactivity disorder in adults and children (pp. 42–52). Cambridge University Press. [Google Scholar]
- WHOQOL Group. (1995). The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. Social Science & Medicine, 41(10), 1403–1409. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2022). Constitution. https://www.who.int/about/governance/constitution
- Yürümez E., Kılıç B. G. (2016). Relationship between sleep problems and quality of life in children with ADHD. Journal of Attention Disorders, 20(1), 34–40. 10.1177/1087054713479666 [DOI] [PubMed] [Google Scholar]
- Zambrano-Sánchez E., Martínez-Cortés J. A., Río-Carlos Y. D., Dehesa-Moreno M., Poblano A. (2012). Low quality of life scores in school children with attention deficit-hyperactivity disorder related to anxiety. Archives of Neuropsychiatry, 70(3), 180–184. 10.1590/s0004-282x2012000300005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jad-10.1177_10870547231155438 for The Impact of Childhood Attention-Deficit/Hyperactivity Disorder (ADHD) on Children’s Health-Related Quality of Life: A Systematic Review and Meta-Analysis by Sithara Wanni Arachchige Dona, Nalini Badloe, Emma Sciberras, Lisa Gold, David Coghill and Ha N. D. Le in Journal of Attention Disorders