Abstract
Background/purpose
Digital impressions using intraoral scanners have recently gained popularity. The aim of the present study was to evaluate the fit of full-arch screw-retained cobalt-chromium frameworks fabricated via two different digital impression methods.
Materials and methods
An edentulous resin master model with four dental implants was fabricated. Forty cobalt-chromium superstructures were fabricated and evaluated according to four groups. In Group 1, the superstructures were evaluated using an intraoral scanner to generate digital impressions. Group 2 relied on the help of an auxiliary geometric appliance in generation of digital impressions via intraoral scanner. The traditional method of splinted open-tray conventional impressions was designated for Group 3. Finally, the control group (Group 4) relied on scanning of the master model directly with a laboratory scanner. Vertical marginal discrepancy was evaluated, and data obtained were statistically analyzed.
Results
The highest mean vertical marginal gap value (80.86 ± 50.06 μm) was observed for Group 1 and statistically higher than Group 2, 3, and 4 (P < 0.05). The lowest mean vertical marginal gap value (41.98 ± 26.33 μm) was measured from Group 4 and statistically similar to Group 2 and 3 (P > 0.05).
Conclusion
It has been suggested that the use of auxiliary geometric appliances yields increased scanning accuracy. Frameworks fabricated using the traditional splinted open-tray technique were more reliable compared to those frameworks from digital impressions.
Keywords: Digital dentistry, Digital impression, Fit, Framework, Implant, Intraoral scanner
Introduction
Accurately transferring the 3-dimensional (3-D) position of implants is one of the most important steps in the fabrication of implant-supported prosthesis.1,2 Conventional implant impressions obtained by using elastomeric materials have long been the gold standard, although they involve numerous clinical and laboratory steps that can cause errors in the overall fabrication process.
As digital dentistry continues to evolve, the use of intraoral scanners (IOS) has become more prevalent in both the laboratory setting as well as chair-side. These scanners have the potential to replace conventional dental impressions with digital scans.3, 4, 5, 6 Application of IOS provides a series of advantages including: more patient-friendly and hygienic, time-efficient, simplicity of clinical procedures, elimination of secondary transfer of the impression tray from the clinic to the laboratory and real-time evaluation of the clinical situation.4,5
Several studies have reported the accuracy of IOS are clinically acceptable for the fabrication of single crowns and short-span implant-supported restorations.7, 8, 9, 10 However, in the fabrication of the long-span implant-supported restorations, the use of IOS involves many difficulties and subsequently, errors in the digital technique affecting the fit of restoration.11 Important considerations when speaking of accuracy are trueness and precision. Trueness dictates how close a measurement is to the actual dimension of the object being scanned, while precision refers to the consistency of scan measurements.12
Stitching of successive images is essential for accurate scanning results. The stitching process includes dimensional differences that are directly related to both the scanning scope and the inter-implant distance occur.13, 14, 15 Homogeneity, due to limited reference points and landmarks among the implants in fully edentulous arches, often causes difficulty in predictable scanning of the soft tissue.16,17 Some studies have been carried out in search to overcome this problem from various perspectives. This includes a study evaluating whether the inclusion of the palate during the stitching process of the scan body position, influenced the accuracy of digital implant scans when four implants were used in a completely edentulous maxilla.18 As hypothesized, scanning data from the palate did not result in statistically higher accuracy. In another study by Kim and coworkers have found that an artificial landmark used in the long edentulous area improves trueness and precision of the intraoral scanners.19 The effectiveness of using auxiliary geometric devices attached onto implant scan bodies via flowable composite has recently come of interest in research as it has the ability to increase three dimensional spatial recognition of soft tissues.20 Regardless of the intraoral scanner tested, higher accuracy was obtained when an auxiliary geometric device was used. The difficulty in predictable scanning of the soft tissue between implants in edentulous arches remains a major problem and requires further studies.
Passive fit between implant frameworks and underlying structures is critical for long-term mechanical and biological success. Minimizing misfit to prevent complications in implant-supported prostheses is the generally accepted goal. However, a consensus on an acceptable inconsistency threshold has not been reached.21 Due to each clinical and laboratory step, from impression to prosthesis delivery, being a potential source of error in clinical practice, absolute passive fit is often difficult to achieve.22
Numerous methods have been suggested to evaluate the passivity of the framework.23 The one-screw test, also known as “Sheffield” test, has been applied for many years in daily routine and has been proven efficient for long-span prostheses. According to the test, only the most distal screw is tightened to the framework and vertical marginal discrepancy (VMD) of the other connections is evaluated.
In addition to the impression technique, fabrication of the framework is another important step in providing passive fit. The computer-aided design/computer-aided manufacturing (CAD/CAM) method has resulted in significant improvements in marginal adaptation of frameworks compared to traditional laboratory procedures.24 In literature, it was reported that mechanical properties of metals fabricated by using additive manufacturing techniques are comparable to those that are milled and exceeds those that are manufactured through conventional casting routes. Moreover, additive manufacturing such as selective laser melting (SLM) provides dental prosthetic restorations more efficiently and less expansively without compromising their quality.25 The purpose of the present study was to evaluate the fit of full-arch screw-retained cobalt-chromium (Co–Cr) frameworks fabricated via two different digital impression methods. The null hypothesis of this study was that there are no significant differences between the accuracy of intraoral scans obtained with or without an auxiliary geometric appliance (AGA).
Material and methods
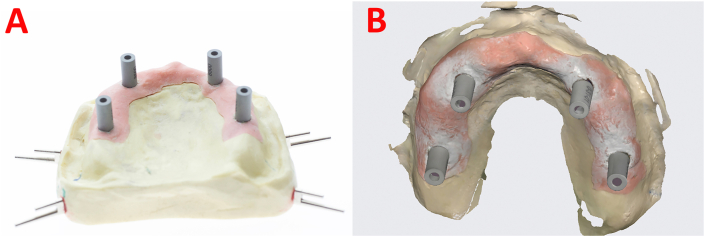
An epoxy resin master model simulating an edentulous maxilla with four parallel dental implants (Medentika GmbH, Hugelsheim, Germany) in the maxillary canine (#13 and #23) and first molar positions (#16 and #26) bilaterally, with a soft tissue replica was fabricated (Fig. 1). Titanium multiunit abutments (Medentika GmbH) were tightened to the implants with 25 Ncm torque. Forty Co–Cr superstructures were fabricated according to the groups evaluated (n = 10).
Figure 1.
Master model and digital impression. (A) The epoxy resin master model with four implants. (B) Full-arch digital impression of the maxilla with scan bodies in Group 1.
The groups were created as follows
Group 1: digital impression with an intraoral scanner.
Group 2: digital impression with the aid of an auxiliary geometric appliance.
Group 3: splinted open-tray conventional impression.
Group 4 (control group): scanning of the master model directly with a laboratory scanner.
For digital impression (Group 1), surface scanning of the master model was made with an intraoral scanner (Medit i500, Medit, Seoul, Korea). After, scan bodies (SBs) (Medentika GmbH) were torqued onto the abutments with 5 Ncm. The scanning strategy was zig-zag technique. The operator started from the buccal surface of the model and advanced precisely from the first SB of the posterior maxilla to the occlusal and then palatal side. The operator then returned to the occlusal and then buccal side, moving slowly forward. All scans were captured in the same environmental conditions (in a room with constant temperature (22 °C), controlled humidity (45%) and ambient light, without interference from external light sources) by the same operator. For Group 2, the data from digital measurements were primarily used to produce an AGA. The purpose of this appliance was to eliminate the commonly occurring error in the stitching process of long edentulous areas and to ensure that the scanning continues as if there were teeth in that area.
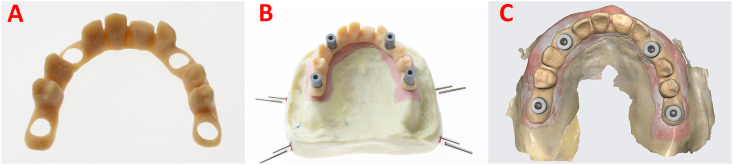
The AGA was designed and fabricated with orally useable resin by using a 3-D printer (Fig. 2). The appliance was positioned by matching its circular holes with the corresponding scannable impression copings to prevent movement during scanning, it was then fixed with light-polymerizing resin (Filtek Ultimate, 3 M Espe, Germany) onto the SBs. Scanning was performed as described previously. After the second complete-arch scans were completed by using a reverse engineering software (Geomagic Studio, 3D System, Rock Hill, SC, USA), the AGA was removed from the digital image. This left behind as much surface area as possible of the SBs, the remainder of the mesh was erased. These copings served as the reference position for constructing the definitive digital complete arch image. Using the reverse engineering software, a virtual partition of the digital scan was achieved.
Figure 2.
Workflow in Group 2. (A) Auxiliary geometric appliance. (B) The epoxy resin master model with four implants and auxiliary geometric appliance. (C) Full-arch digital impression of the maxilla with scan bodies and auxiliary geometric appliance.
For Group 3, open-tray multiunit impression copings were screwed onto the abutments and splinted using autopolymerizing acrylic resin. Impressions were taken using a custom tray with a vinyl impression material (Elite HD+, Zhermack SpA, Rovigo, Italy). Type IV scannable dental stone was mixed in a vacuum mixer and poured. Definitive conventional stone models were created. These were then scanned after the SBs were tightened on the analogs with a laboratory scanner (Dentsply Sirona inEos X5, Charlotte, NC, USA).
For the control group (Group 4), the master model was powdered with a homogeneous layer of scannable dust and SBs were tightened onto the abutments. Scanning was performed with a laboratory scanner (Dentsply Sirona inEos X5). All digital data (STL) acquired from the groups were used for the fabrication of Co–Cr superstructures.
For each data point, a screw-retained 12-unit superstructure was designed using a software program (Exocad DentalCAD, Darmstadt, Germany) with 20 μm (μm) allotted for cement space. Superstructures were fabricated using the SLM method (Eos CobaltChrome P2; EOS GmbH, Munich, Germany). For fabrication of the SLM specimens, 35 μm-thick metal powder layers were repeatedly applied until the designed framework was constructed. All superstructures were devested by airborne-particle abrasion with 50 μm aluminum oxide powder and tungsten carbide burs at low speed, then steam-cleaned and dried.
For VMD evaluation, each superstructure was fixed on the master model by one screw on the terminal abutment, #26. Images were captured of each implant-superstructure interface area (#26, #23, #13, #16). VMD evaluation was also performed with one screw in the other terminal abutment, #16. These areas were digitally photographed under stereomicroscope (SZ61/SZ51; Olympus Corp, Tokyo, Japan) at 45x magnification using a microscope camera (CMEX-10 Pro; Euromex, Arnhem, The Netherlands). VMD values were measured at eight measurement points for each abutment by using an image-analyzing software program.
Obtained data were statistically analyzed by using a software program (SPSS version 25, IBM Corp, Armonk, NY, USA). Data normality was confirmed with the Levene normality test (P < 0.05). A one-way ANOVA was conducted to investigate the influence of two variables (evaluation site and impression technique) on the VMD values and Scheffe post-hoc test was used for pairwise comparisons. Statistical significance was accepted at the P < 0.05 level.
Results
As a result of the reliability analysis between parallel tests, the reliability coefficient was found to be high (rxx = 0.939). The highest mean vertical marginal gap (VMG) value (80.86 ± 50.06 μm) was observed for Group 1 and statistically higher than Group 2, 3, and 4 (P < 0.05). The lowest mean VMG value (41.98 ± 26.33 μm) was measured from Group 4 and statistically similar to Group 2 and 3 (P > 0.05) (Table 1).
Table 1.
Vertical marginal gap values for each group. Identical letters in each column (vertically) indicated no statistically significant differences (P > 0.05), while non-identical letters in each column indicated statistically significant differences (P < 0.05).
| Impression techniques | Vertical marginal gap values Mean ± standard deviation (μm) |
|---|---|
| Group 1: Digital Impression using intraoral scanner | 80.86 ± 50.1 a |
| Group 2: Digital Impression using intraoral scanner with AGA | 53.15 ± 50.06 ᵇ |
| Group 3: Conventional Impression + laboratory scanner | 52.22 ± 32.16 ᵇ |
| Group 4: Control (Laboratory scanner) | 41.98 ± 26.33 ᵇ |
μm: microns.
In the measurements where the single screw was on the abutment #26, the lowest mean VMG value was measured (14.7 ± 5.12 μm) and no significant difference was found between the groups for this abutment (P > 0.05). While the lowest mean VMG values for the abutments #23, #13 and #16 were measured in Group 4, no statistical difference was found between Group 2 and Group 3 (P > 0.05). The largest mean VMG values were measured for the abutments #23, #13 and #16 in Group 1 and were significantly higher than Group 2, Group 3, and Group 4 (P < 0.05) (Table 2).
Table 2.
Single-screw test results of frameworks (Mean ± standard deviation) (n = 10). Identical (lower case) letters in each column (vertically) indicated no statistically significant differences (P > 0.05), while non-identical letters in each column indicated statistically significant differences (P < 0.05). Identical (upper case) letters in each row (horizontally) indicated no statistically significant differences (P > 0.05), while non-identical letters in each row indicated statistically significant differences (P < 0.05).
| Vertical marginal gap measured in implant areas (μm) |
|||||
|---|---|---|---|---|---|
| Impression techniques | Screwed abutment # | 26 | 23 | 13 | 16 |
| Group 1 | 26 | 15.2 ± 6.05 a, A | 76.5 ± 28.47 c, B | 102.8 ± 32.88 e, C | 117.6 ± 35.23 g, D |
| Group 2 | 26 | 16.7 ± 8.24 a, E | 41.2 ± 11 b, F | 61.8 ± 13.46 d, G | 92.4 ± 7.30 f, H |
| Group 3 | 26 | 14.7 ± 5.12 a, I | 36 ± 15.55 b, J | 68.8 ± 12.09 d, K | 92.6 ± 14.86 f, L |
| Group 4 | 26 | 15 ± 9.01 a, M | 24.5 ± 9.02 b, N | 56.1 ± 14.69 d, P | 78 ± 10.53 f, R |
μm: microns.
When the single screw was on the abutment #16, the lowest mean VMG value was measured on the abutment #16 (14.2 ± 6.39 μm), the largest mean VMG value was measured on the abutment #26 (123.6 ± 40.1 μm). The mean VMG values measured for the abutments #23, #13, #16 for Group 2, 3 and 4 were statistically similar (P > 0.05) (Table 3). In all groups the mean VMG values increased further away the terminal abutment (P < 0.05).
Table 3.
Single-screw test results of frameworks (Mean ± standart deviation) (n = 10). Identical (lower case) letters in each column (vertically) indicated no statistically significant differences (P > 0.05), while non-identical letters in each column indicated statistically significant differences (P < 0.05). Identical (upper case) letters in each row (horizontally) indicated no statistically significant differences (P > 0.05), while non-identical letters in each row indicated statistically significant differences (P < 0.05).
| Vertical marginal gap measured in implant areas (μm) |
|||||
|---|---|---|---|---|---|
| Impression techniques | Screwed abutment # | 16 | 13 | 23 | 26 |
| Group 1 | 16 | 17.2 ± 6.19 a, A | 81.6 ± 35.4 c, B | 112.4 ± 37.97 e, C | 123.6 ± 40.1 g, D |
| Group 2 | 16 | 16.9 ± 8.39 a, E | 42.5 ± 10.2 b, F | 62.4 ± 17.43 d, G | 91.3 ± 13.41 f, H |
| Group 3 | 16 | 14.2 ± 6.39 a, I | 34.1 ± 14.09 b, J | 67.5 ± 12.98 d, K | 89.9 ± 15.98 f, L |
| Group 4 | 16 | 15 ± 8.64 a, M | 24.9 ± 11.3 b, N | 49.7 ± 10.9 d, P | 72.7 ± 14.71 f, R |
μm: microns.
Discussion
This study aimed to analyze the effects of the use of an AGA on the accuracy of intraoral scans. Based on the results, the null hypothesis that there are no significant differences between the accuracy of intraoral scans obtained with or without an AGA was rejected. Also, when the accuracy of frameworks obtained by digital impression methods or conventional impression methods were compared, the VMG values of the frameworks obtained by the digital impressions were significantly higher than the other methods. This result is consistent with the findings of Iturrate et al.,3 that the use of an AGA increases the impression precision and accuracy when making digital impressions from four implants placed in the edentulous maxilla. The presence of long and homogeneous surfaces between implants, especially in edentulous patients, negatively affects the digital impression accuracy. Creating a continuous reference point with the use of auxiliary geometric appliance increases the scanning sensitivity, therefore improving stitching accuracy during scanning.
Miyoshi et al.,17 made digital impressions of six implants placed in a maxillary complete edentulous arch with four different intraoral scanners. Using the splinted open-tray technique for the control group, inconsistency and width of scanned area appeared to be directly correlated, especially in the digital impression group. As width of the scanned area increased so too did inconsistency. This finding allowed Miyoshi et al.,17 to determine in the case of digital impressions of an implant, restorations with a maximum of three units should be made. Gimenez-Gonzalez et al.,26 who investigated full-arch digital impressions of fully edentulous maxilla with six implants scanned by four operators, reported similarly that the trueness of scanned data deteriorated when the scan distance was longer.
Due to their pivotal role in prosthesis fabrication, incorrect impressions may cause an ill-fitting prosthesis, ultimately leading to mechanical complications. The clinically acceptable passive fit threshold is one of the most frequently discussed topics, as there is no clear gold standard. It has been suggested that a recommended maximum passive fit value, to prevent long-term complications such as loss of retention, screw loosening, fracture of the framework and chipping of porcelain, be defined and agreed upon.27 The generally accepted goal is to minimize misfit in an attempt to prevent complications in implant-retained prostheses. However, it is practically impossible to achieve absolute passive fit. Some studies have reported maximum acceptable errors of between 95 μm and 150 μm. Andriessen et al.,28 claimed that the maximum amount of lateral movement of an implant in the bone is 50 μm and the mismatch threshold value between two implants should be 2 × 50 μm = 100 μm. In the present study, the VMA values measured in all groups and at all baseline levels were less than 150 μm and were within clinically acceptable limits. In addition, the difference in VMA values between adjacent abutments is less than 100 μm.
There are different approaches to evaluate the precision of impression methods. Traditional methods mainly rely on manual technique and the evaluation of two-dimensional measurements obtained from the prosthesis-abutment junction cross-section necessary to reveal the geometric configuration between prosthesis and abutment in the marginal region. Silicone replica technique can be used as an alternative to this cross-sectional evaluation. Current digital methods also make it possible to perform three-dimensional analyzes with the use of scanning devices. Another method is to create a virtual copy of the measured models and compare them with a highly accurate reference dataset (master model). Three-dimensional discrepancies between two surface data can be analyzed by superimposition using appropriate software. Often, these software programs use best fit algorithms for registration and subsequent comparison of three-dimensional datasets. However, using the best fit algorithm produces positive and negative deviations between the reference object and test objects, which may cause the results to cancel each other out and not represent the true deviation.29
In the present study, a procedure similar to the clinical scenario was performed to evaluate the measurement accuracy. A cobalt-chromium framework was produced using the SLM method. This method has been used frequently in metal framework production recently and has been shown to be among high precision production techniques.30 While there may be errors caused by factors affecting the sensitivity of the method, the fit of the produced multi-unit frameworks is comparable with the literature and is within clinical limits.31 An in vitro study by Akcin E. et al., evaluated the marginal and internal fit of implant-supported cement retained 3-,4- and 5-unit Co–Cr metal frameworks produced via different methods including lost wax, CAD/CAM milling, and SLM. As a result of the study, the lowest marginal gap values were observed in the 3-unit and 4-unit frameworks fabricated with the SLM technique, while the lowest marginal gap values were observed in the 5-unit frameworks in the lost wax method.32
Within the limitations of this in-vitro study, it has been suggested that the use of auxiliary geometric appliances has the ability to increase scanning accuracy of edentulous arches with multiple implants. When fabricating these frameworks, the conventional splinted open-tray impression technique proved to be more accurate when compared to digital impression.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgments
This work was not supported by any organizations.
References
- 1.Turkyilmaz I., Unsal G.S. Full-mouth rehabilitation of an elderly patient with Sjogren's syndrome by using implant-supported fixed dental prostheses including CAD/CAM frameworks. J Dent Sci. 2019;14:428–429. doi: 10.1016/j.jds.2019.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bandiaky O.N., Le Bars P., Gaudin A., et al. Comparative assessment of complete-coverage, fixed tooth-supported prostheses fabricated from digital scans or conventional impressions: a systematic review and meta-analysis. J Prosthet Dent. 2022;127:71–79. doi: 10.1016/j.prosdent.2020.09.017. [DOI] [PubMed] [Google Scholar]
- 3.Iturrate M., Eguiraun H., Solaberrieta E. Accuracy of digital impressions for implant-supported complete-arch prosthesis, using an auxiliary geometry part-An in vitro study. Clin Oral Implants Res. 2019;30:1250–1258. doi: 10.1111/clr.13549. [DOI] [PubMed] [Google Scholar]
- 4.Asutay H.C., Turkyilmaz I., Benli M., Martinez J.L. Transforming smiles using an intraoral scanner and face scan application on smartphone. J Dent Sci. 2022;17:1413–1414. doi: 10.1016/j.jds.2022.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Uluc I.G., Guncu M.B., Aktas G., Turkyilmaz I. Comparison of marginal and internal fit of 5-unit zirconia fixed dental prostheses fabricated with CAD/CAM technology using direct and indirect digital scans. J Dent Sci. 2022;17:63–69. doi: 10.1016/j.jds.2021.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turkyilmaz I., Wilkins G.N., Varvara G. Tooth preparation, digital design and milling process considerations for CAD/CAM crowns: understanding the transition from analog to digital workflow. J Dent Sci. 2021;16:1312–1314. doi: 10.1016/j.jds.2021.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhivago P., Turkyilmaz I. A comprehensive digital approach to enhance smiles using an intraoral optical scanner and advanced 3-D sculpting software. J Dent Sci. 2021;16:784–785. doi: 10.1016/j.jds.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asar N.V., Yun S., Schwartz S., Turkyilmaz I. Analysis of the relationship between the surface topography of prepared tooth surfaces and data quality of digital impressions from an intraoral scanner. J Dent Sci. 2022;17:545–550. doi: 10.1016/j.jds.2021.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marghalani A., Weber H.P., Finkelman M., Kudara Y., El Rafie K., Papaspyridakos P. Digital versus conventional implant impressions for partially edentulous arches: an evaluation of accuracy. J Prosthet Dent. 2018;119:574–579. doi: 10.1016/j.prosdent.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 10.Schmidt A., Wostmann B., Schlenz M.A. Accuracy of digital implant impressions in clinical studies: a systematic review. Clin Oral Implants Res. 2022;33:573–585. doi: 10.1111/clr.13951. [DOI] [PubMed] [Google Scholar]
- 11.Rutkunas V., Gedrimiene A., Akulauskas M., Fehmer V., Sailer I., Jegelevicius D. In vitro and in vivo accuracy of full-arch digital implant impressions. Clin Oral Implants Res. 2021;32:1444–1454. doi: 10.1111/clr.13844. [DOI] [PubMed] [Google Scholar]
- 12.Turkyilmaz I., Lakhia S., Tarrida L.G., Varvara G. Guest commentary: the battle of file formats from intraoral optical scanners. Int J Prosthodont (IJP) 2020;33:369–371. doi: 10.11607/ijp.2020.4.gc. [DOI] [PubMed] [Google Scholar]
- 13.Marques S., Ribeiro P., Falcao C., et al. Digital impressions in implant dentistry: a literature review. Int J Environ Res Publ Health. 2021;18:1020. doi: 10.3390/ijerph18031020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Knechtle N., Wiedemeier D., Mehl A., Ender A. Accuracy of digital complete-arch, multi-implant scans made in the edentulous jaw with gingival movement simulation: an in vitro study. J Prosthet Dent. 2022;128:468–478. doi: 10.1016/j.prosdent.2020.12.037. [DOI] [PubMed] [Google Scholar]
- 15.Kim K.R., Seo K.Y., Kim S. Conventional open-tray impression versus intraoral digital scan for implant-level complete-arch impression. J Prosthet Dent. 2019;122:543–549. doi: 10.1016/j.prosdent.2018.10.018. [DOI] [PubMed] [Google Scholar]
- 16.Patzelt S.B., Vonau S., Stampf S., Att W. Assessing the feasibility and accuracy of digitizing edentulous jaws. J Am Dent Assoc. 2013;144:914–920. doi: 10.14219/jada.archive.2013.0209. [DOI] [PubMed] [Google Scholar]
- 17.Miyoshi K., Tanaka S., Yokoyama S., Sanda M., Baba K. Effects of different types of intraoral scanners and scanning ranges on the precision of digital implant impressions in edentulous maxilla: an in vitro study. Clin Oral Implants Res. 2020;31:74–83. doi: 10.1111/clr.13548. [DOI] [PubMed] [Google Scholar]
- 18.Mizumoto R.M., Alp G., Ozcan M., Yilmaz B. The effect of scanning the palate and scan body position on the accuracy of complete-arch implant scans. Clin Implant Dent Relat Res. 2019;21:987–994. doi: 10.1111/cid.12821. [DOI] [PubMed] [Google Scholar]
- 19.Kim J.E., Amelya A., Shin Y., Shim J.S. Accuracy of intraoral digital impressions using an artificial landmark. J Prosthet Dent. 2017;117:755–761. doi: 10.1016/j.prosdent.2016.09.016. [DOI] [PubMed] [Google Scholar]
- 20.Iturrate M., Eguiraun H., Etxaniz O., Solaberrieta E. Accuracy analysis of complete-arch digital scans in edentulous arches when using an auxiliary geometric device. J Prosthet Dent. 2019;121:447–454. doi: 10.1016/j.prosdent.2018.09.017. [DOI] [PubMed] [Google Scholar]
- 21.Tahmaseb A., De Clerck R., Aartman I., Wismeijer D. Digital protocol for reference-based guided surgery and immediate loading: a prospective clinical study. Int J Oral Maxillofac Implants. 2012;27:1258–1270. [PubMed] [Google Scholar]
- 22.Figueras-Alvarez O., Canto-Naves O., Real-Voltas F., Roig M. Protocol for the clinical assessment of passive fit for multiple implant-supported prostheses: a dental technique. J Prosthet Dent. 2021;126:727–730. doi: 10.1016/j.prosdent.2020.10.001. [DOI] [PubMed] [Google Scholar]
- 23.Abduo J., Bennani V., Waddell N., Lyons K., Swain M. Assessing the fit of implant fixed prostheses: a critical review. Int J Oral Maxillofac Implants. 2010;25:506–515. [PubMed] [Google Scholar]
- 24.Turkyilmaz I., Asar N.V. Eighteen-month outcomes of titanium frameworks using computer-aided design and computer-aided manufacturing method. Implant Dent. 2017;26:480–484. doi: 10.1097/ID.0000000000000582. [DOI] [PubMed] [Google Scholar]
- 25.Revilla Leon M., Klemm I.M., Garcia-Arranz J., Ozcan M. 3D metal printing - additive manufacturing technologies for frameworks of implant-borne fixed dental prosthesis. Eur J Prosthodont Restor Dent. 2017;25:143–147. doi: 10.1922/EJPRD_RevillaLeon05. [DOI] [PubMed] [Google Scholar]
- 26.Gimenez-Gonzalez B., Hassan B., Ozcan M., Pradies G. An in vitro study of factors influencing the performance of digital intraoral impressions operating on active wavefront sampling technology with multiple implants in the edentulous maxilla. J Prosthodont. 2017;26:650–655. doi: 10.1111/jopr.12457. [DOI] [PubMed] [Google Scholar]
- 27.Mericske-Stern R., Worni A. Optimal number of oral implants for fixed reconstructions: a review of the literature. Eur J Oral Implant. 2014;7(Suppl 2):S133–S153. [PubMed] [Google Scholar]
- 28.Andriessen F.S., Rijkens D.R., van der Meer W.J., Wismeijer D.W. Applicability and accuracy of an intraoral scanner for scanning multiple implants in edentulous mandibles: a pilot study. J Prosthet Dent. 2014;111:186–194. doi: 10.1016/j.prosdent.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 29.Amin S., Weber H.P., Finkelman M., et al. Digital vs. conventional full-arch implant impressions: a comparative study. Clin Oral Implants Res. 2017;28:1360–1367. doi: 10.1111/clr.12994. [DOI] [PubMed] [Google Scholar]
- 30.Barbin T., Veloso D.V., Del Rio Silva L., et al. 3D metal printing in dentistry: an in vitro biomechanical comparative study of two additive manufacturing technologies for full-arch implant-supported prostheses. J Mech Behav Biomed Mater. 2020;108 doi: 10.1016/j.jmbbm.2020.103821. [DOI] [PubMed] [Google Scholar]
- 31.Yap C.Y., Chua K., Dong Z., et al. Review of selective laser melting: materials and applications. Appl Phys Rev. 2015;2 [Google Scholar]
- 32.Akcin E.T., Guncu M.B., Aktas G., Aslan Y. Effect of manufacturing techniques on the marginal and internal fit of cobalt-chromium implant-supported multiunit frameworks. J Prosthet Dent. 2018;120:715–720. doi: 10.1016/j.prosdent.2018.02.012. [DOI] [PubMed] [Google Scholar]