Abstract
Background
The aim of this study was to evaluate the effect of a virtual reality video on preoperative anxiety, hemodynamic parameters, and patient satisfaction in patients undergoing septorhinoplasty.
Methods
This was a prospective, observational cohort trial. Forty patients between the ages of 18...65 who were scheduled for elective septorhinoplasty, with an American Society of Anesthesiologists (ASA) physical status I...II were included in the study. Patients experienced a 15-minute virtual reality (VR) video via a phone using a VR device. A three-dimensional, 360.. video depicted the beauty of nature and was accompanied by meditation music. Patients... oxygen saturation values, heart rate, and blood pressure were monitored and recorded. Using the State-Trait Anxiety Inventory scale, anxiety scores and hemodynamic parameters were compared before and after VR application.
Results
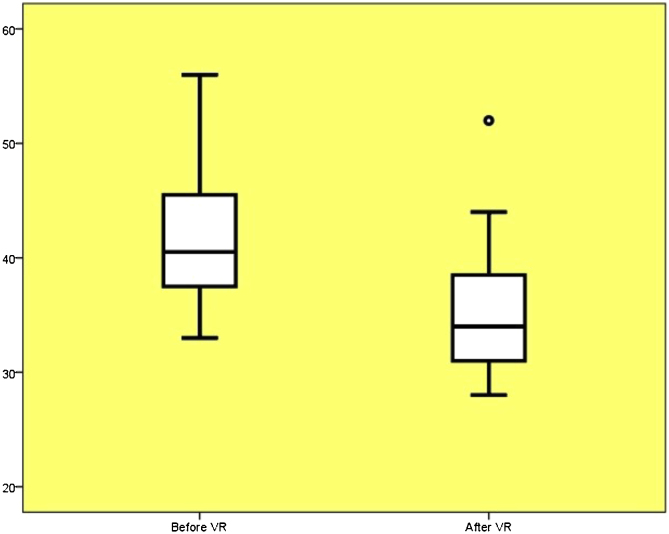
Median anxiety scores decreased significantly from 40.5 to 34 (p.ß<.ß0.001). VR also had positive effects on hemodynamic parameters.
Conclusions
VR reduces preoperative anxiety and has positive effects on hemodynamic parameters in patients undergoing septorhinoplasty. We anticipate that VR will be increasingly used as a non-pharmacological preoperative approach in the future.
Keywords: Virtual reality, Anxiety, Premedication, Nasal surgery procedures
Introduction
Preoperative anxiety is a condition observed in approximately 80% of patients and occurs in response to surgical stress.1, 2 It usually starts 2 days before the operation and increases until the day of the procedure.3 This unpleasant situation affects a patient...s comfort and well-being, leading to physiological and psychological changes such as tachycardia and hypertension and ultimately endangering the patient...s health.4 In addition, patients feel increased pain and require more analgesics postoperatively5, 6; thus, preoperative anxiety prolongs the duration of anesthesia and decreases the quality of postoperative recovery. Controlling preoperative anxiety reduces the length of hospital stay, healthcare-related costs, and postoperative complications.7
Current methods used to reduce patients... anxiety in the preoperative period primarily focus on pharmacological interventions such as benzodiazepines or antihistaminic drugs.8 However, with the use of these pharmacological agents, patients face risks such as addiction, anaphylaxis, end-organ damage, polypharmacy, and development of tolerance.9 In recent years, Virtual Reality (VR) applications have become an increasingly popular alternative approach to manage preoperative anxiety.10
VR is a computer technology that provides the feeling of being immersed in a simulated three-dimensional (3D) world where the user may interact with the virtual environment.11 Clinical studies have shown that VR technology is effective in reducing pain perception and anxiety. It has also been proposed as an effective non-pharmacological alternative for reducing acute procedural pain and providing anxiety relief.12, 13
We aimed to evaluate the effect of VR as a non-pharmacological premedication met74hod on preoperative anxiety, hemodynamic parameters, and patient satisfaction in patients undergoing septorhinoplasty. Results from our study are expected to contribute to the growing support for the use of VR applications as an alternative method to reduce preoperative anxiety.
Methods
After obtaining approval from the Local Research Ethics Committee (reference number: 2020...19/17, ClinicalTrials.gov identifier: NCT04598217) and patients... written informed consent, a prospective, single-center study was conducted in Zonguldak B..lent Ecevit University Medicine Faculty Hospital with patients undergoing elective septorhinoplasty.
Patients between the ages of 18...65 years, who were scheduled for elective septorhinoplasty, with an American Society of Anesthesiologists (ASA) physical status I...II were included in the study. Exclusion criteria included congestive heart failure, adrenal insufficiency, chronic alcohol and substance addiction, Glasgow Coma Score <15, cerebrovascular disease, psychiatric-cognitive dysfunction, claustrophobia, use of sedative and narcotic drugs, blindness, and deafness. A total of 40 patients were included in the study.
On the day of the operation, the VR procedure was explained to the patients while they waited for surgery in the preoperative area. The demographic data of the patients were recorded. Then, patients... oxygen saturation values, heart rate, and blood pressure were monitored and recorded. The State Anxiety Inventory (STAI-S) test, which is accepted as the standard test for anxiety measurement, was provided to the patients to determine preoperative anxiety levels. The STAI-S scale consists of 20 statements and uses a 4-point scale, as follows: 1- Not at all, 2- Somewhat, 3- Moderately so, and 4- Very much so. Scores vary between and 20...80 with high scores associated with higher anxiety levels. Patients were asked to read each statement and then indicate how they were feeling at that moment by marking the appropriate parentheses on the right side of each statement. Patients were asked not to spend much time on each statement. It was explained that there was no right or wrong answer and that they would be asked to fill out a form of the same anxiety scale after the VR procedure.
Thereafter, patients were informed that a video would be shown to provide a visual and auditory experience for 15 minutes. Patients were fitted with a Samsung Gear VR headset (Samsung Electronics, Suwon, South Korea) equipped with a Samsung Note 7 Edge smartphone. The VR device displayed a video with a mobile application (Guided meditation VR, a virtual reality relaxation application) over Oculus (Fig. 1). The patients adopted the position they were most comfortable with, and the VR device was placed on the patients... faces at the most appropriate angle. Patients were questioned in terms of comfort. After obtaining verbal consent, patients were left in silence in their rooms. After the video ended, the VR headset was removed from the patients... faces. During the follow-up, patients... blood pressure, oxygen saturation, and heart rate values were recorded at 5, 10, and 15 minutes.
Figure 1.
A patient using virtual reality.
Patients completed the STAI-S scale a second time. Additionally, they were asked about their satisfaction with the procedure (very satisfied, satisfied, undecided, unsatisfied), complications (headache, dizziness, nausea), and whether they would want this VR application again in case of a future surgery. Then, the patients were transferred to the operating room without loss of time.
Statistical analysis
The approximate sample size was calculated before the study using the Power Analysis & Sample Size-11 software (NCSS statistical software, Kaysville, Utah, USA). The sample size was calculated on the basis of a previous study (Group 1: 19.ß...ß1.7, Group 2: 15.ß...ß1.3, effect size: 0.88).14 Accordingly, in the sample size analysis performed with reference to 99% confidence interval and 80% power, the minimum number of patients required was calculated to be 35. Considering a 10...15% attrition rate, the required sample size was determined to be 40. The SPSS 22 program (IBM Corporation, Armonk, NY, USA) was used to analyze the data. The Kolmogorov-Smirnov test was used as a normal distribution test. Paired t-test, t-test, and the repeated measures analysis of variance (RANOVA) test were used to analyze the data that had a normal distribution. Mann-Whitney U and Wilcoxon tests were used to analyze data that did not have a normal distribution. In cases of significance, posthoc single comparisons were performed by Bonferroni test. A p.ß<.ß0.05 was considered statistically significant as the level of significance in the assessment. Cohens... d was used in effect size analysis of measurements before and after VR. Cohen...s d value was accepted as d.ß....ß1 very large effect, 0.8.ß=.ßlarge effect, 0.5.ß=.ßmedium effect, and 0.2.ß=.ßsmall effect.
Results
Forty patients who underwent septorhinoplasty were included in the study. The demographic data of the patients are summarized in Table 1.
Table 1.
Demographic data.
| X.ß...ßSD | |
|---|---|
| Age (years) | 32.68.ß...ß8.74 |
| BMI (kg.ßm-2) | 23.85.ß...ß4.44 |
| n (%) | |
| Sex (male/female) | 16(40) / 24(60) |
| Study in university (no/yes) | 21(52.5) / 19(47.5) |
| Marital status married/single | 21(52.5) / 19(47.5) |
| Smoking yes/no | 18(45.0) / 22(55.0) |
| Total | 40 (100.0) |
X.ß...ßSD, Mean.ß...ßstandard deviation, n, (%).
Considering the change in anxiety levels of patients before and after VR application, it was found that there was a significant decrease in STAI scores, and the effect of VR application on preoperative anxiety was large (p.ß<.ß0.001, Cohen...s d: 1.28). The distribution of STAI scores before and after the VR application is shown in Figure 2. Anxiety scores decreased significantly regardless of gender, age, education level, and smoking status (Table 2).
Figure 2.
Distribution of State Anxiety Inventory scores before and after virtual reality.
Table 2.
Anxiety scores before and after virtual reality.
| Before VR |
After VR |
Change | p | Cohen...s d | |||
|---|---|---|---|---|---|---|---|
| X.ß...ßSD | Median (range) | X.ß...ßSD | Median (range) | ||||
| STAI scores | 41.9.ß...ß5.7 | 40.5 (23) | 35.1.ß...ß4.8 | 34.0 (24) | <0.001 | 1.28 | |
| Sex | |||||||
| Male | 39.5.ß...ß3.7 | 39.5 (15) | 33.3.ß...ß2.3 | 33.0 (9) | -6.25 | <0.001 | 2.01 |
| Female | 43.5.ß...ß6.30 | 43.5 (22) | 36.3.ß...ß5.7 | 37.0 (24) | -7.20 | <0.001 | 1.19 |
| p | 0.029 | 0.052 | |||||
| Studies in University | |||||||
| No | 41.8.ß...ß5.5 | 40.0 (23) | 35.9.ß...ß5.9 | 35.0 (22) | -5.95 | <0.001 | 1.03 |
| Yes | 42.0.ß...ß6.0 | 41.0 (18) | 34.2.ß...ß3.9 | 33.0 (12) | -7.78 | <0.001 | 1.54 |
| p | 0.916 | 0.376 | |||||
| Marital status | |||||||
| Married | 41.5.ß...ß6.2 | 40.0 (23) | 35.4.ß...ß5.5 | 34.0 (22) | -6.42 | <0.001 | 1.04 |
| Single | 42.3.ß...ß5.1 | 41.0 (17) | 35.1.ß...ß4.1 | 35.0 (13) | -7.26 | <0.001 | 1.55 |
| p | 0.665 | 0.981 | |||||
| Smoking | |||||||
| Yes | 41.9.ß...ß5.9 | 41.5 (23) | 35.4.ß...ß5.6 | 34.5 (22) | -6.50 | <0.001 | 1.13 |
| No | 41.9.ß...ß5.6 | 40.0 (18) | 34.8.ß...ß4.2 | 33.5 (13) | -7.09 | <0.001 | 1.43 |
| p | 0.996 | 0.712 | |||||
| Aged (years) | |||||||
| 18-29 | 41.0.ß...ß5.1 | 40.0 (18) | 34.6.ß...ß4.4 | 33.0 (13) | -6.46 | <0.001 | 1.34 |
| ...30 | 42.4.ß...ß6.0 | 43.0 (23) | 35.4.ß...ß5.1 | 35.0 (22) | -7.04 | <0.001 | 1.25 |
| p | 0.456 | 0.603 | |||||
VR, Virtual Reality; X.ß...ßSD, Mean.ß...ßstandard deviation, p.ß<.ß0.05.
The average values of heart rate, systolic blood pressure, diastolic blood pressure, mean blood pressure, and oxygen saturation before, and at 5, 10, and 15 minutes during VR application are shown in Table 3.
Table 3.
Changes in hemodynamic parameters and saturation before, and 5, 10, and 15.ßminutes during virtual reality.
| Before VR | 5 minutes | 10 minutes | 15.ßminutes | p | Partial eta square | |
|---|---|---|---|---|---|---|
| HR | 86.8.ß...ß14.0a,b,c | 81.0.ß...ß13.4a | 79.8.ß...ß12.1b | 78.6.ß...ß11.9c | <0.001 | 0.512 |
| SBP | 126.7.ß...ß18.3a,b,c | 121.9.ß...ß15.0a | 119.0.ß...ß14.9b | 117.2.ß...ß14.6c | <0.001 | 0.588 |
| DBP | 79.9.ß...ß12.5 | 77.9.ß...ß11.4 | 76.4.ß...ß11.5 | 76.2.ß...ß10.8 | 0.001 | 0.354 |
| MBP | 95.3.ß...ß13.0a,b,c | 92.4.ß...ß11.7a | 90.4.ß...ß11.5b | 89.4.ß...ß11.3c | <0.001 | 0.422 |
| SpO2 | 98.7.ß...ß0.6 | 98.5.ß...ß0.8 | 98.6.ß...ß0.6 | 98.6.ß...ß0.6 | 0.531 |
HR, Heart Rate;SBP, Systolic Blood Pressure; DBP, Diastolic Blood Pressure; MBP, Mean Blood Pressure; SpO2, Oxygen Saturation.
a, b, cRepresent the binary groups that make up the difference in post hoc analysis (p.ß<.ß0.05).
The satisfaction of the patients and their wishes to repeat the experience in a hypothetical future surgical procedure are shown in Table 4. Only one patient described having mild dizziness that did not hinder the completion of the procedure. No other complications were reported.
Table 4.
Satisfaction of patients and their wishes to repeat the experience in a hypothetical future surgical procedure.
| Would you like to experience virtual reality again if you undergo a surgery in the future? | n/% |
|---|---|
| Yes | 36/90 |
| No | 4/10 |
| Satisfaction | |
| Very satisfied | 21/52.5 |
| Satisfied | 15/37.5 |
| Undecided | 4/10 |
| Not satisfied | 0/0 |
Discussion
In this prospective study, we demonstrated that VR application before surgery reduced patients... anxiety prior to undergoing septorhinoplasty. A significant decrease in the heart rate and mean arterial pressure compared to that before the VR application was observed. Most patients were satisfied with the application and stated that they would like to have the same experience if they undergo a surgery again.
Distraction is a strategy to direct attention away from the stressor and toward other thoughts and behaviors that are not related to the stressor.15 These strategies have been shown to be effective during medical procedures.16 VR is an exposure tool that uses 3D computer technology to mislead an individual...s senses and allow them to feel physically as if they are in the virtual environment. Realistic virtual environments are created in which users can interact with VR systems that allow the integration of real-time computer images, sounds, and other sensory inputs,17 allowing the user to experience the environment actively in 360...18, 19 Immersive VR directly focuses on the patient's individual perception of stressful stimuli and reduces negative experiences through distraction.18 Instead of looking at a handheld or table-mounted computer screen, the computer screens are mounted on the face. The user wears a VR headset with miniature computer screens close to the patients' eyes. A successful virtual experience should allow a user to feel physically inside the virtual environment. This feeling can be achieved by excluding external stimuli and only hearing and seeing the stimuli generated by the computer. The equipment used is inexpensive, non-invasive, easily available, and transportable, and may be used by anyone. When used for premedication, VR does not require extra labor as a patient can make self-adjustments; most patients experience almost no side effects.
Many anxiety scales have been developed to assess anxiety. We used the STAI scale, which was self-reported. This scale measures the presence and severity of current anxiety symptoms and contains two subscales. 1) The State Anxiety Scale (S-Anxiety), which evaluates current anxiety levels by asking participants about their current feelings and uses elements of the autonomic nervous system that measure subjective anxiety, such as tension, irritability, anxiety, and activation/arousal feelings. 2) The Trait Anxiety Scale (T-Anxiety), which indicates the relatively constant anxiety levels that do not arise according to a specific situation or time. The dependence of an individual on anxiety experience was evaluated.20 State anxiety is an indicator of an individual...s feelings of tension and restlessness due to a stressful situation. Preoperative anxiety caused by doubts and fears is an unpleasant reaction experienced by a patient that is specific to the situation. Therefore, we preferred the State Anxiety Scale for evaluating preoperatine anxiety. Studies on adaptation of the scale to Turkish society, validity, and reliability have been conducted.21, 22
In our study, the STAI median value, which was 40.5 before VR, decreased to 34 after VR application. Ganry et al.8 conducted a study on controlling preoperative anxiety using VR in ambulatory surgeries in patients undergoing maxillofacial and plastic surgery. This study aimed to reduce preoperative anxiety levels by offering natural scenes presented in a VR system to 20 patients undergoing skin cancer surgery. They concluded that anxiety scores and salivary cortisol levels were significantly reduced by viewing nature scenes on the VR system. A meta-analysis involving 813 patients concluded that preoperative anxiety scores were lower in the VR group than in the control group (SMD.ß=.ß...0.64, 95% CI ...1.08 to ...0.20, p.ß=.ß0.004). In a subgroup analysis, preoperative anxiety scores were lower in the VR group than in the control group in pediatric patients (SMD.ß=.ß...0.71, 95% CI ...1.14 to ...0.27, p.ß=.ß0.002), whereas a significant difference was not observed between the two groups in adult patients (p.ß=.ß0.226). The results of this meta-analysis indicated that VR could decrease preoperative anxiety, especially in pediatric patients.23
Music is anoher non-pharmacological method for reducing preoperative anxiety. Music depresses the sympathetic system activated by anxiety and thus provides a relaxing effect in patients.24 Music significantly decreased STAI scores in a study investigating the effect of music on preoperative anxiety.25 We predict that VR has a similar positive effect on anxiety levels since it provides patients with auditory experience as well as visual experiences.
In order to reduce the anxiety of the patients in the preoperative period, pharmacological interventions are preferred primarily.8 However, these interventions may have undesirable side effects such as respiratory complications, addiction, anaphylaxis, end-organ damage, polypharmacy, and development of tolerance.9, 26 In a study conducted on patients undergoing urological surgery under spinal anesthesia, pharmacological interventions were compared with VR. It was stated that VR is better in terms of patient-anesthesiologists... satisfaction and reduced respiratory side effects as compared to a pharmacological agent.26
It is known that preoperative anxiety affects postoperative pain, the need for anesthesia and analgesia, and even increases morbidity and mortality in some types of surgery. Preoperative anxiety also directly affects the patient...s clinical symptoms by disrupting hemodynamic parameters. In contrast, controlled preoperative anxiety reduces the length of hospital stay, healthcare-related costs, and postoperative complications. Pandya et al.,27 for example, indicated that VR application decreased the use of intravenous opioids and sedatives and reduced procedure-related pain without increasing the procedural duration compared to the control group. Thus, it is directly effective in the intraoperative-postoperative period of the patient.7
Preoperative anxiety also has negative effects on hemodynamic parameters. In the presence of anxiety, stress hormone levels increase; as a result of rising catecholamine levels, arterial blood pressure and heart rate increase and arrhythmia can develop.28, 29 For the ideal induction of anesthesia and anesthesia, the hemodynamic parameters should be stabilized as much as possible by controlling anxiety.30 We found that the application of VR before surgery had positive effects on the hemodynamic parameters of the patients. The heart rate and mean arterial pressure of the patients decreased significantly after VR. Thus, patients became more suitable for anesthesia post VR application.
Chan et al.10 used preoperative VR to reduce anxiety in women undergoing gynecological surgery. The results of the study showed that the VR experience significantly reduced preoperative anxiety and was readily accepted by patients. It was stated that approximately 82% of the patients rated the VR experience as excellent or good. Similarly, the satisfaction rate of patients in our study was very high. While 90% of the patients were very satisfied or satisfied with the application, 36 of 40 patients stated that they would like to experience VR again during future surgical procedures. In addition, only one of our patients experienced mild dizziness when the application ended, but this complaint was not serious enough to terminate the application.
There are some limitations to this prospective study. Our study was based on the patients-reported scale. Objective physiological measurements, such as determining salivary cortisol concentration, were not performed, and the effects of VR on the postoperative period were not investigated. Another limitation is that the Trait Anxiety Scale was not evaluated.
Conclusion
In conclusion, VR reduces preoperative anxiety and has positive effects on hemodynamics in patients undergoing septorhinoplasty. This inexpensive, noninvasive, easy-to-use application has high patient satisfaction, and we believe that it will be increasingly used as a non-pharmacological premedication method in the future.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Erkilic E., Kesimci E., Soykut C., et al. Factors associated with preoperative anxiety levels of Turkish surgical patients: From a single center in Ankara. Patient Prefer Adherence. 2017;11:291–296. doi: 10.2147/PPA.S127342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bahrami N., Soleymani M., Arjinee Z., et al. Impact anxious patient care based upon the nursing process for elective surgery for women. J Nurs Iran. 2012;25:9–30. [Google Scholar]
- 3.Miller R.D. 4th ed. Churchill Livingstone; Philadelphia: 1994. Psychological preparation and preoperative medication in anesthesia. Miller...s Anesthesia; pp. 1015–1016. [Google Scholar]
- 4.Namazi M., Akbari S.A.A., Mojab F., et al. Aromatherapy with citrus aurantium oil and anxiety during the first stage of labor. Iran Red Crescent Med J. 2014;16 doi: 10.5812/ircmj.18371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ali A., Altun D., Oguz B.H., et al. The effect of preoperative anxiety on postoperative analgesia and anesthesia recovery in patients undergoing laparascopic cholecystectomy. J Anesth. 2014;28:222–227. doi: 10.1007/s00540-013-1712-7. [DOI] [PubMed] [Google Scholar]
- 6.Dehghan F., Jalali R., Bashiri H. The effect of virtual reality technology on preoperative anxiety in children: a Solomon four-group randomized clinical trial. Perioper Med. 2019;8:1–7. doi: 10.1186/s13741-019-0116-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Turksal E., Alper I., Sergin D., et al. The effects of preoperative anxiety on anesthetic recovery and postoperative pain in patients undergoing donor nephrectomy. Rev Bras Anestesiol. 2020;70:271–277. doi: 10.1016/j.bjane.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ganry L., Hersant B., Sidahmed-Mezi M., et al. Using virtual reality to control preoperative anxiety in ambulatory surgery patients: A pilot study in maxillofacial and plastic surgery. J Stomatol Oral Maxillofac Surg. 2018;119:257–261. doi: 10.1016/j.jormas.2017.12.010. [DOI] [PubMed] [Google Scholar]
- 9.Stevens Alan. Mary Pomerantz Advertising; Palm Beaches: 2013. Understanding addiction to benzos; pp. 4–16. [Google Scholar]
- 10.Chan J.J.I., Yeam C.T., Kee H.M., et al. The use of pre-operative virtual reality to reduce anxiety in women undergoing gynecological surgeries: a prospective cohort study. BMC Anesthesiol. 2020;20:1–8. doi: 10.1186/s12871-020-01177-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sz..kely G., Satava R.M. Virtual reality in medicine. Interview by Judy Jones. BMJ. 1999;319:1305. doi: 10.1136/bmj.319.7220.1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li A., Montano Z., Chen V.J., Gold J.I. Virtual reality and pain management: Current trends and future directions. Pain Manag. 2011;1:147–157. doi: 10.2217/pmt.10.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ryu J.H., Park J.W., Nahm F.S., et al. The effect of gamification through a virtual reality on preoperative anxiety in pediatric patients undergoing general anesthesia: A prospective, randomized, and controlled trial. J Clin Med. 2018;7:284. doi: 10.3390/jcm7090284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hendricks T.M., Gutierrez C.N., Stulak J.M., Dearani J.A., Miller J.D. The use of virtual reality to reduce preoperative anxiety in first-time sternotomy patients: a randomized controlled pilot trial. Mayo Clin Proc. 2020;95:1148–1157. doi: 10.1016/j.mayocp.2020.02.032. [DOI] [PubMed] [Google Scholar]
- 15.Hoffman H.G., Doctor I.N., Patterson D.R., et al. Virtual reality as an adjunctive pain control during burn wound care in adolescent patients. Pain. 2000;85:305–309. doi: 10.1016/s0304-3959(99)00275-4. [DOI] [PubMed] [Google Scholar]
- 16.Hoffman H.G., Garcia-Palacios A., Patterson D.R., et al. The effectiveness of virtual reality for dental pain control: a case study. Cyberpsychol Behav. 2001;4:527–535. doi: 10.1089/109493101750527088. [DOI] [PubMed] [Google Scholar]
- 17.Kim K., Kim C.H., Kim S.Y., et al. Virtual reality for obsessive-compulsive disorder: past and the future. Psychiatry Investig. 2009;6:115–121. doi: 10.4306/pi.2009.6.3.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoffman H.G. Virtual-reality therapy. Sci Am. 2004;291:58–65. doi: 10.1038/scientificamerican0804-58. [DOI] [PubMed] [Google Scholar]
- 19.Gregg L., Tarrier N. Virtual reality in mental health: a review. Soc Psychiatry Psychiatr Epidemiol. 2007;42:343–354. doi: 10.1007/s00127-007-0173-4. [DOI] [PubMed] [Google Scholar]
- 20.Julian L.J. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A) Arthritis Care Res (Hoboken). 2011;63:467–472. doi: 10.1002/acr.20561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21...ner N., Le Compte A. Bo..azi..i University Press; Istanbul: 1983. Handbook of State-Trait Anxiety Inventory. [Google Scholar]
- 22.Le Compte A., ..ner N. 1975. Durumluk-S..rekli Kayg.. Envanterinin T..rk..e...ye adaptasyon ve standardizasyonu ile ilgili bir ..al....ma [A study on the adaptation and standardization of the State-Trait Anxiety Inventory]. IX. Milli Psikiyatri ve N..rolojik Bilimler Kongresi ..al....malar.. pp. 457–462. [Google Scholar]
- 23.Koo C.H., Park J.W., Ryu J.H., et al. The effect of virtual reality on preoperative anxiety: a meta-analysis of randomized controlled trials. J Clin Med. 2020;9:3151. doi: 10.3390/jcm9103151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Palmer J.B., Lane D., Mayo D., et al. Effects of music therapy on anesthesia requirements and anxiety in women undergoing ambulatory breast surgery for cancer diagnosis and treatment: a randomized controlled trial. J Clin Oncol. 2015;33:3162–3168. doi: 10.1200/JCO.2014.59.6049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.U..ra.. G.A., Y..ld..r..m G., Y..ksel S., et al. The effect of different types of music on patients... preoperative anxiety: A randomized controlled trial. Complement Ther Clin Pract. 2018;31:158–163. doi: 10.1016/j.ctcp.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 26.Moon J.Y., Shin J., Chung J., et al. Virtual reality distraction during endoscopic urologic surgery under spinal anesthesia: a randomized controlled trial. J Clin Med. 2018;8:2. doi: 10.3390/jcm8010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pandya P.G., Kim T.E., Howard S.K., et al. Virtual reality distraction decreases routine intravenous sedation and procedure-related pain during preoperative adductor canal catheter insertion: a retrospective study. Korean J Anesthesiol. 2017;70:439–445. doi: 10.4097/kjae.2017.70.4.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maze M., Tranquilli W. Alpha-2 adrenoceptor agonists: Defining the role in clinicalanesthesia. Anesthesiology. 1991;74:581–605. [PubMed] [Google Scholar]
- 29.Aho M., Scheinin M., Lehtinen A.M., et al. Intramuscularly administered dexmedetomidine attenuates hemodynamic and stress hormone responses to gynecologic laparoscopy. Anesth Analg. 1992;75:932–939. [PubMed] [Google Scholar]
- 30.Eren G., Cukurova Z., Demir G., et al. Comparison of dexmedetomidine and three different doses of midazolam in preoperative sedation. J Anaesthesiol Clin Pharmacol. 2011;27:367–372. doi: 10.4103/0970-9185.83684. [DOI] [PMC free article] [PubMed] [Google Scholar]