Abstract
Purpose:
While identifying older adults at risk for falls is important, fall prediction models have had limited success, in part because of a poor understanding of which physical function measures to include. The purpose of this secondary analysis was to determine physical function measures that are associated with future falls in older adults.
Methods:
In a 12-month trial comparing Vitamin D3 supplementation versus placebo on neuromuscular function, 124 older adults completed physical function measures at baseline, including the Short Physical Performance Battery (SPPB), Timed Up and Go, tests of leg strength and power, standing balance on a force plate with firm and foam surfaces, and walking over an instrumented walkway. Falls were recorded with monthly diaries over 12 months and categorized as no falls vs. one or more falls. Univariate and multivariable logistic regression adjusting for demographics, treatment assignment, depression, and prescription medications were conducted to examine the association between each physical function measure and future falls. Models were additionally adjusted for fall history.
Results:
61 participants sustained one or more falls. In univariate analysis, white race, depression, fall history, SPPB, and postural stability on foam were significantly associated with future falls. In multivariable analysis, fall history (OR (95% CI): 3.20 (1.42–7.43)), SPPB (0.80 (0.62–1.01)), and postural stability on foam (3.01 (1.18, 8.45)) were each significantly associated with future falls. After adjusting for fall history, only postural stability on foam was significantly associated with falls.
Conclusions:
When developing fall prediction models, fall history, the SPPB, and postural stability when standing on foam should be considered.
Keywords: Physical function, Physical performance logistic regression, Postural stability, Gait, Model
Introduction
Falls are a prevalent concern among adults 65 years and older, with approximately one in four older adults falling per year.1 Falls can result in serious health consequences, including fractures, hospitalizations, and death.2 Moreover, falls are the leading cause of accidental death and injury in older adults.3 In addition to physical injuries, falls can result in fear of falling which may lead to activity curtailment and social isolation.4 This psychosocial impact may lead to further physiological decline and loss of independence.5 Therefore, preventing fall-related injuries in older adults is important to maintain functional independence and improve overall quality of life.
Due to the detrimental consequences of falls, many researchers have attempted to develop and validate fall prediction models and identify measures that best predict older adult fallers.6–9 Prediction models can identify older adults at higher risk for falls and lead to implementation of early fall prevention strategies. Previous studies using data from electronic health records or baseline cohort visits found that age, past history of falls, fear of falling, medications, and mobility impairment are associated with falls.6–8 However, the sensitivity, specificity, and discrimination of these prediction models range from 0.65 to 0.74.6,8,9 One challenge to developing fall prediction models is that, while there are a multitude of measures related to falls, it is unclear which measures or combination of measures are most associated with falls.
Decline in physical function, for instance, is one of the most important predictors of falls in older adults due to loss of proprioception, muscle strength, and vision that occur with aging.10,11 However, there are multiple methods to assess physical function that range from routine clinical assessments to instrument-based assessments. Clinical assessments, such as the Timed Up and Go (TUG),12 Short Physical Performance Battery (SPPB),13 or chair stands,14 are relatively simple to administer. However, they are prone to ceiling or floor effects and may not be sensitive enough to detect small yet clinically meaningful differences in mobility.15 Instrument-based assessments, such as force plates, pressure mats, or dynamometers, are more precise and can detect small changes in postural sway, gait, or strength, but they are expensive and require time to process and analyze. While previous fall prediction models often included a measure of physical function because of its association with falls,16 it is unclear which measures, whether clinical assessments, instrumented-based assessments, or a combination of the two, should be included. Moreover, previous studies predicting falls in older adults included self-reported or clinical assessments but did not include instrumented-based assessments.17,18 It’s unclear among a wide range of physical function measures which are more predictive of future falls. Determining which physical function measures, among clinical and instrumented-based, that are associated with falls may guide researchers in collecting and including appropriate measures in fall prediction models, and may result in improved accuracy.19
Improving upon current fall prediction models can further help researchers and clinicians assess for fall risk with the proper tools while saving time, expenses, and resources. Identifying older adults at risk for falls can also lead to fall prevention strategies to reduce the risk for sustaining future falls. Therefore, the purpose of this secondary analysis was to determine, among clinical and instrumented-based measures, which physical function and routinely collected clinical measures are associated with future falls in older adults.
Methods
Participants
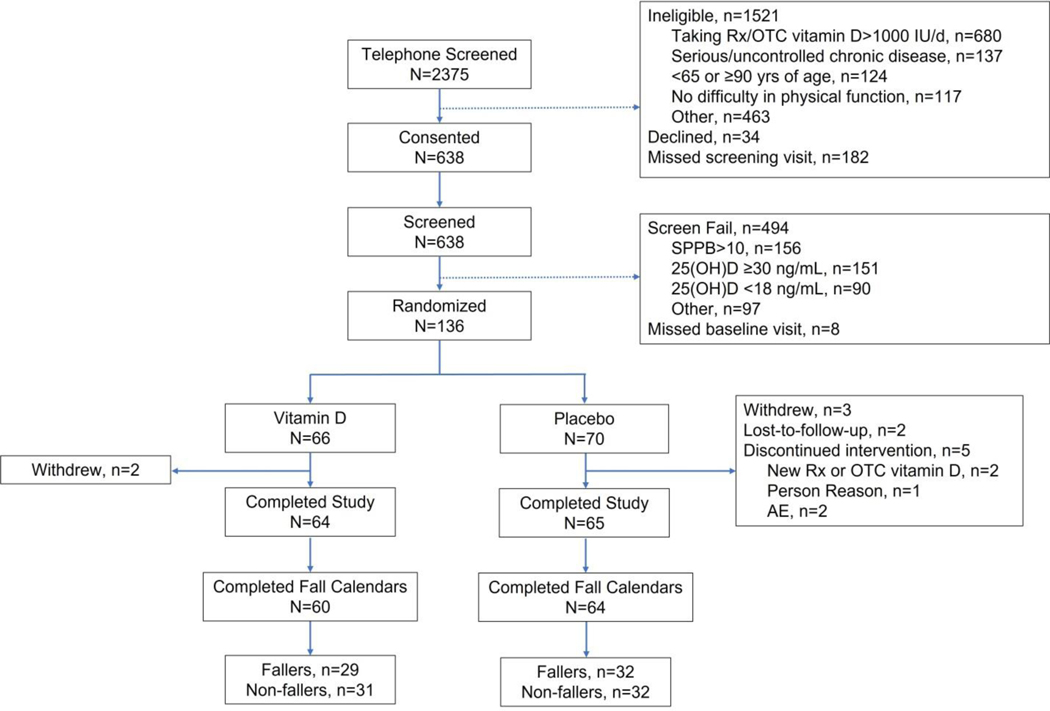
This is a secondary analysis of the Exploring Vitamin D’s Effects on Neuromuscular Endpoints (EVIDENCE; NCT02015611) study, a 12-month, double-blind randomized controlled trial comparing the effect of Vitamin D3 supplementation to placebo on neuromuscular function in older adults.20 Inclusion criteria were: 1) between ages 65 to 90 years, 2) SPPB score of 10 or less if chair stand score is three or less, or SPPB score less than 10 then if chair stand score is four, 3) Serum 25(OH)D concentration of 18 to <30 ng/mL, 4) not dependent on a walker, and 5) self-reported difficulty with physical function. Exclusion criteria included: 1) serious or uncontrolled chronic disease, 2) Montreal Cognitive Assessment score less than 18, 3) taking prescription vitamin D2 or >1000 IU/day of vitamin D3, 4) knee or hip surgery in the last six months, 5) body mass index over 40 kg/m2, and 6) eye surgery within the past month. One hundred and thirty-six participants met all entry criteria and were enrolled in the trial (Figure 1). All participants provided written informed consent to participate in the study according to the guidelines set forth by the Wake Forest University School of Medicine Institutional Review Board for Human Research.
Figure 1.
Consort diagram of participants who were included in the study.
Measurements
At baseline, participants completed questionnaires related to demographics, medical history, and medication history. Participants were asked how many times they had fallen over the past year and those who fell one or more times were considered to have a positive fall history. Weight and height were measured and body mass index (BMI; kg/m2) was calculated. Depression was assessed with the Center for Epidemiologic Studies Depression Scale (CES-D), a 20-item questionnaire scored from 0–60, with higher scores indicating greater depressive symptoms.21
Participants also completed several physical performance measures. For the Short Physical Performance Battery (SPPB), a measure of lower extremity performance, participants stand in side-by-side, semi-tandem, and tandem positions for ten seconds, walk four meters at usual pace, and rise from a chair five times as quickly as possible.22 Each of the three performance measures was assigned a score ranging from 0 (inability to perform the task) to 4 (the highest level of performance) and summed to create an SPPB score ranging from 0 to 12, with higher scores indicating greater lower extremity function. Participants also completed a modified physical performance battery, the expanded SPPB, to minimize ceiling effects of the SPPB.23 The expanded SPPB increased the holding time of the standing balance tasks to 30 seconds and added a single leg stand and a narrow 4-m walk test of balance. Expanded SPPB scores are continuous and range from 0 to 4, with higher scores indicative of better performance. Participants also completed one trial of the Timed Up and Go (TUG), a task that involves standing from a chair, walking three meters, turning around a cone, walking back to the chair, and sitting back down in the chair.12
Muscle power was assessed using the Nottingham Power Rig.24 Participants sat in a chair and pressed a foot lever attached to a flywheel as hard and fast as possible. Five trials were performed with each leg, and the ratio of the maximum leg power from the right or left leg to body weight was used for analysis. Muscle strength was assessed using an isokinetic dynamometer (Biodex). Participants sat with their hips and knees flexed at 90° and extended their knee to push as hard as possible against a resistance pad. Two trials were performed with four repetitions each. The maximum strength of the four repetitions from the second trial from participants’ dominate leg was used for analysis.
Participants also completed standing balance tasks on a force plate (AMTI, Watertown, MA). Participants completed ten 30-second trials standing barefoot with their feet abducted 10° and heels separated medio-laterally by 6 cm with eyes open (firm base) and five 30 second trials standing with eyes open on a 6.4 cm thick Airex foam pad (foam base). Participants were instructed to focus their eyes on a point on the wall in front of them and stand quietly throughout the test. Center of pressure data were extracted and average sway velocity, anteroposterior range, mediolateral range, and 95% confidence ellipse were calculated and averaged over the firm and foam trials.25,26 Greater center of pressure velocity, range, and confidence ellipse values indicate worse postural control. Gait velocity and other spatiotemporal parameters were assessed using a 4.88 meter long instrumented walkway (GAITRite, Clifton, NJ).27 Participants walked at their usual speed for four trials and at a fast speed for four trials. For their usual speed, participants were instructed to walk “at a pace that feels comfortable to you, as if you were walking to the mailbox or window shopping at the mall”, and for their fast speed, participants were instructed to walk “as quickly as you can without running, as if you were hurrying to get out of the rain”. Velocity, stride length, base of support, and percent stance phase were extracted and averaged over the four usual and fast trials.
Each month over 12 months, participants completed fall calendars, marking any falls that occurred on the calendar. Fall calendars are considered the gold standard to record falls.28 A fall was defined as any event in which the individual unintentionally came to rest on the ground or lower level. Monthly fall calendar completion was monitored through monthly phone calls and collected at four and 12-month visits. The total number of falls over the 12-month period was recorded.
Statistical Analysis
Categorical variables were reported as N (percent), and continuous variables were reported as mean (standard deviation). Unadjusted univariate analyses for each variable were assessed using logistic regression. Multivariable analyses were conducted for each of the clinical assessments and instrument-based assessments using logistic regression adjusted for age, sex, race, treatment assignment from the original trial, CES-D, and number of prescription medications. Multivariable models were further adjusted for a history of one or more falls over the past year. Multicollinearity was assessed for each multivariable model using variance inflation factors and was not deemed an issue for any of the models (values less than 10). Logistic regression output for each variable was reported as odds ratio (95% confidence interval), and p-value. We conducted complete case analysis because the amount of missing data was low and a missing completely at random pattern was reasonable.
P-values of less than 0.05 were considered significant for univariate analysis. A conservative threshold considering P-values of less than 0.1 as significant in multivariable analysis adjusted for covariates was used to detect possible associations of predictive variables for falls.
Analyses were conducted using R software (version 4.1.2). The following R packages were used in the analysis: tableone,29 naniar,30 and car. 31 Logistic regression models were developed with the base R function glm.
Results
Participants
A total of 129 participants completed the 12-month study; 124 had complete falls calendar data and were included in this analysis. Figure 1 depicts the consort diagram showing the number of participants who were screened, eligible and randomized into the study and those with complete falls calendar data at 12-month follow-up. Demographic information and descriptive characteristics at baseline are presented in Table 1. The mean age was 73.0 years, 49% were female, 68% were white, all were Non-Hispanic, and average BMI was 30.3 kg/m2. Of the 124 participants, 63 had no falls while 61 had one or more falls. Older adults who had one or more falls were more likely to be of white race, had greater depressive symptoms, used an assistive device, and had worse lower extremity function as measured by the SPPB (all p’s <0.05). Intervention assignment was balanced by no falls vs. one or more falls, and the main trial found no difference in change in the clinical or instrumented-based physical performance measures between the vitamin D and placebo groups.20
Table 1.
Demographic and descriptive characteristics of participants at baseline.
| Sample size | Overall (n=124) | No Falls (n=63) | One or More Falls (n=61) | |
|---|---|---|---|---|
| Age (years) | 124 | 73.02 (6.08) | 72.44 (6.26) | 73.62 (5.89) |
|
| ||||
| Sex | 124 | |||
| Male | 64 (51.6%) | 32 (50.8%) | 32 (52.5%) | |
| Female | 60 (48.4%) | 31 (49.2%) | 29 (47.5%) | |
|
| ||||
| Body Mass Index (kg/m2) | 124 | 30.26 (4.48) | 30.43 (4.67) | 30.08 (4.30) |
|
| ||||
| Race | 124 | |||
| White | 85 (68.5%) | 37 (58.7%) | 48 (78.7%) | |
| African American | 39 (31.5%) | 26 (41.3%) | 13 (21.3%) | |
|
| ||||
| Presence of Comorbidities | 124 | |||
| Stroke | 11 (8.9%) | 5 (7.9%) | 6 (9.8%) | |
| Diabetes | 30 (24.2%) | 12 (19.0%) | 18 (29.5%) | |
| Cardiovascular Disease | 9 (7.3%) | 4 (6.3%) | 5 (8.2%) | |
|
| ||||
| Number of Medications | 124 | 4.08 (2.82) | 3.60 (2.33) | 4.57 (3.20) |
|
| ||||
| CES-D Score | 124 | 7.59 (6.98) | 5.77 (5.97) | 9.46 (7.48) |
|
| ||||
| Positive Fall History | 124 | 66 (53.20) | 23 (36.50) | 43 (70.5) |
|
| ||||
| Assisted Device Usage | 124 | 22 (17.7%) | 9 (14.3%) | 13 (21.3%) |
|
| ||||
| SPPB Score (range 0–12) | 124 | 7.81 (1.82) | 8.21 (1.57) | 7.39 (1.97) |
|
| ||||
| Expanded SPPB Score (range 0–4) | 124 | 1.67 (0.45) | 1.73 (0.44) | 1.60 (0.47) |
|
| ||||
| Usual Gait Speed (m/s) | 121 | 0.77 (0.17) | 0.79 (0.16) | 0.75 (0.17) |
|
| ||||
| TUG (seconds) | 122 | 11.64 (2.65) | 11.23 (2.24) | 12.08 (2.99) |
|
| ||||
| Leg Strength (Nm) | 108 | 98.66 (28.21) | 100.95 (30.03) | 96.10 (26.09) |
|
| ||||
| Leg Power (watts/kg) | 123 | 1.44 (0.48) | 1.45 (0.50) | 1.43 (0.46) |
|
| ||||
| Stride Length Usual Speed (cm) | 121 | 118.18 (17.96) | 119.85 (17.07) | 116.42 (18.83) |
|
| ||||
| Base of Support Usual Speed (cm) | 121 | 10.63 (3.25) | 10.77 (3.25) | 10.48 (3.27) |
|
| ||||
| Stance Phase Usual Speed (% of gait cycle) | 121 | 65.20 (1.86) | 64.90 (1.56) | 65.52 (2.10) |
|
| ||||
| Stride Length Fast Speed (cm) | 121 | 140.69 (22.87) | 142.45 (22.23) | 138.83 (23.57) |
|
| ||||
| Base of Support Fast Speed (cm) | 121 | 10.52 (3.17) | 10.67 (3.30) | 10.36 (3.05) |
|
| ||||
| Stance Phase Fast Speed (% of gait cycle) | 121 | 62.30 (2.02) | 62.01 (1.72) | 62.61 (2.26) |
|
| ||||
| Sway Velocity Firm Base (cm/sec) | 117 | 0.84 (0.21) | 0.82 (0.18) | 0.87 (0.24) |
|
| ||||
| 95% Confidence Ellipse Firm Base (cm2) | 117 | 0.56 (0.41) | 0.50 (0.32) | 0.63 (0.49) |
|
| ||||
| Medial Lateral Range Firm Base (cm) | 117 | 0.75 (0.33) | 0.70 (0.29) | 0.80 (0.36) |
|
| ||||
| Anteroposterior Range Firm Base (cm) | 117 | 1.01 (0.32) | 0.96 (0.27) | 1.06 (0.37) |
|
| ||||
| Sway Velocity Foam Base (cm/sec) | 117 | 1.36 (0.39) | 1.31 (0.38) | 1.41 (0.40) |
|
| ||||
| 95% Confidence Ellipse Foam Base (cm2) | 117 | 1.98 (1.16) | 1.73 (0.92) | 2.25 (1.32) |
|
| ||||
| Medial Lateral Range Foam Base (cm) | 117 | 1.66 (0.52) | 1.55 (0.49) | 1.78 (0.53) |
|
| ||||
| Anteroposterior Range Foam Base (cm) | 117 | 1.79 (0.48) | 1.67 (0.39) | 1.91 (0.53) |
Note: Continuous data are presented as mean (SD), and discrete data are presented as n (%). Abbreviations: CES-D=Center for Epidemiological Studies Depression; SPPB=Short Physical Performance Battery; TUG=Timed Up and Go
Univariate Analysis
Table 2 presents measures from baseline that are associated with one or more falls in the unadjusted models. Older white adults were 2.6 times more likely to have one or more future falls than African Americans. For every one point higher CES-D score, there was a 9% higher odds of having one or more falls. For every one point higher SPPB score, there was 23% lower odds of sustaining one or more falls. Older adults with history of falls in the past year had a four-fold higher odds of having one or more falls. Postural sway when standing on foam was significantly associated with falls. For every square centimeter increment in 95% confidence ellipse area, there was a 53% higher odds of sustaining one or more falls. For every centimeter increment in medial lateral range, there was a two-fold higher odds; and for every centimeter increment in anteroposterior range, there was a three-fold higher odds of sustaining one or more falls.
Table 2.
Association between physical function measures and one or more falls over 12 months of follow-up.
| Unadjusted | Adjusted* | |||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% Confidence Interval | P-value | Odds Ratio | 95% Confidence Interval | P-value | |
| Age | 1.03 | (0.97, 1.10) | 0.28 | |||
| Male Sex | 1.07 | (0.53, 2.17) | 0.85 | |||
| White Race | 2.60 | (1.19, 5.86) | 0.02 | |||
| Intervention Assignment | 1.07 | (0.53, 2.17) | 0.85 | |||
| Number of Medications | 1.13 | (1.0, 1.30) | 0.06 | |||
| CES-D Score | 1.09 | (1.03, 1.16) | 0.005 | |||
| Positive Fall History | 4.16 | (1.99, 8.98) | <0.0001 | 3.20 | (1.42, 7.43) | 0.01 |
| Assisted Device Usage | 1.63 | (0.64, 4.26) | 0.31 | 0.85 | (0.28, 2.61) | 0.78 |
| SPPB Score | 0.77 | (0.62, 0.94) | 0.02 | 0.80 | (0.62, 1.02) | 0.07 |
| Expanded SPPB Score | 0.52 | (0.22, 1.18) | 0.12 | 0.69 | (0.25, 1.87) | 0.47 |
| Gait Speed (m/s) | 0.20 | (0.02, 1.73) | 0.15 | 0.25 | (0.02, 2.96) | 0.28 |
| TUG (seconds) | 1.14 | (0.99, 1.32) | 0.08 | 1.14 | (0.96, 1.37) | 0.16 |
| Leg Strength (Nm) | 1.0 | (0.98, 1.01) | 0.37 | 1.00 | (0.98, 1.02) | 0.88 |
| Leg Power (Watts/Kg) | 0.92 | (0.44, 1.93) | 0.83 | 0.90 | (0.34, 2.38) | 0.82 |
| Stride Length Usual Speed (cm) | 0.99 | (0.97, 1.01) | 0.30 | 0.99 | (0.97, 1.02) | 0.50 |
| Base of Support Usual Speed (cm) | 0.97 | (0.87, 1.09) | 0.63 | 0.97 | (0.86, 1.10) | 0.62 |
| Stance Phase Usual Speed (% of gait cycle) | 1.21 | (0.99, 1.51) | 0.07 | 1.21 | (0.96, 1.55) | 0.11 |
| Stride Length Fast Speed (cm) | 0.99 | (0.98, 1.01) | 0.38 | 1.0 | (0.98, 1.02) | 0.73 |
| Base of Support Fast Speed (cm) | 0.97 | (0.86, 1.09) | 0.59 | 0.97 | (0.85, 1.09) | 0.59 |
| Stance Phase Fast Speed (% of gait cycle) | 1.17 | (0.97, 1.41) | 0.11 | 1.12 | (0.91, 1.39) | 0.28 |
| 95% Confidence Ellipse Firm Base (cm2) | 2.11 | (0.86, 5.72) | 0.12 | 1.92 | (0.71, 5.71) | 0.22 |
| Sway Velocity Firm Base (cm/sec) | 2.95 | (0.52, 20.23) | 0.24 | 2.41 | (0.31, 23.23) | 0.42 |
| Medial Lateral Range Firm Base (cm) | 2.63 | (0.84, 8.80) | 0.10 | 2.18 | (0.62, 8.15) | 0.23 |
| Anteroposterior Range Firm Base (cm) | 2.67 | (0.84, 9.29) | 0.11 | 2.60 | (0.71, 10.38) | 0.16 |
| 95% Confidence Ellipse Foam Base (cm2) | 1.53 | (1.09, 2.25) | 0.02 | 1.48 | (1.01, 2.28) | 0.06 |
| Sway Velocity Foam Base (cm/sec) | 1.96 | (0.77, 5.22) | 0.17 | 1.71 | (0.55, 5.47) | 0.36 |
| Medial Lateral | 2.45 | (1.18, 5.40) | 0.02 | 2.13 | (0.94, 5.07) | 0.07 |
| Range Foam Base (cm) | ||||||
| Anteroposterior Range Foam Base (cm) | 3.24 | (1.42, 8.12) | 0.008 | 3.01 | (1.18, 8.45) | 0.03 |
Models adjusted for age, sex, race, intervention assignment, number of medications, and depression. Abbreviations: CES-D=Center for Epidemiological Studies Depression; SPPB=Short Physical Performance Battery; TUG=Timed Up and Go
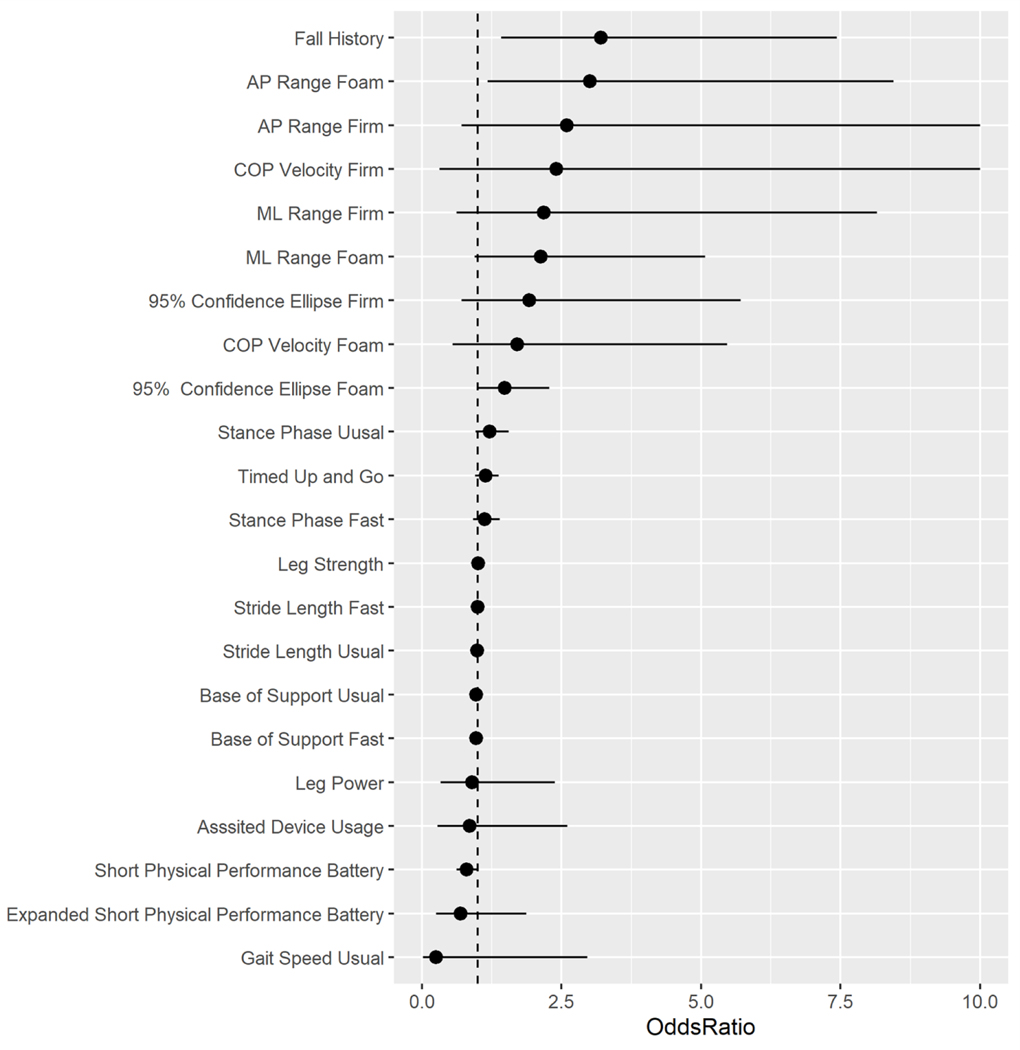
Multivariable Analysis
Table 2 also presents measures from baseline that were associated with one or more falls, when controlling for age, sex, race, intervention group, number of medications, and depression. For every one point higher SPPB score, there was a 20% lower odds of having one or more falls. Older adults who had one or more falls in the past year were three times more likely to have one or more future falls. Postural sway when standing on foam was significantly associated with falls. For every square centimeter increment in 95% confidence ellipse area, there was a 50% higher odds of sustaining one or more falls. For every centimeter increment in mediolateral range, there was a two-fold higher odds; and for every centimeter increment in anteroposterior range there was a three-fold higher odds of sustaining one or more falls. All adjusted measures and their odds ratio are depicted in Figure 2.
Figure 2.
Association between baseline physical function measures and one or more falls over 12 months of follow-up. Odds ratios (95% confidence intervals). Abbreviations: AP=anteroposterior; ML=medio-lateral; COP=center of pressure
When including fall history in addition to demographics, medications and depression in the multivariable models, anteroposterior range when standing on foam was the only physical function measure significantly associated with one or more falls (OR: 2.50; CI: 0.94, 7.22; p=0.08).
Discussion
The purpose of this secondary analysis was to determine, among a battery of demographic, clinical, and physical function measures, which ones were associated with falls over 12 months of follow-up in older adults. In unadjusted analyses, race, depression, fall history, SPPB, and postural instability when standing on foam were significantly associated with falls. When adjusted for age, sex, race, intervention group, number of medications, and depression as covariates, key predictors of fall history, SPPB, and postural instability when standing on foam were significantly associated with falls. However, when multivariable models with physical function measures were further adjusted for fall history, only postural instability when standing on foam was significantly associated with falls.
Our results are similar to previous studies that found race and depression to be associated with falls in older adults.32–34 The National Health and Aging Trends Study found that Non-Hispanic white, older adults had a greater likelihood of falling than African American older adults after adjusting for health and environmental factors.32 We found similar results with Non-Hispanic white older adults having a greater odds of falling than African Americans. Our results are also similar to other studies that found older adults with depression have a greater risk of falls.33,34 Past studies reported that older adults with depression also have increased fear of falling, which can lead to activity curtailment, physiological deconditioning, and thus a greater risk of future falls.33,34 In addition, antidepressant medications can lead to falls, and older adults with depression often have comorbidities that are related to greater fall risk.35
After controlling for confounding variables, fall history was most significantly associated with falls. These results align with past studies that found fall history to be one of the strongest predictors of future falls and health declines. 6,36,37 Moreover, after further controlling for fall history, we found that only center of pressure range in the anteroposterior direction while standing on foam base was significantly associated with future falls. This highlights the importance of fall history data for identifying older adults at risk for future falls, but additional assessments to examine modifiable risk factors should follow.38 The SPPB was also associated with future falls, which is similar to findings from previous studies.39,40 The SPPB measures static balance, dynamic balance, and gait speed, which are indicators of the physiological systems needed to maintain postural control to prevent a fall. While one study did not find the SPPB to predict future falls in older adults,41 this study included well-functioning older adults, while our study included lower functioning older adults. It is possible that the SPPB may be a better tool at predicting future falls for older adults with poorer physical function. The expanded SPPB, on the other hand, was not associated with falls in our sample. Because the older adults in the study were of lower physical function (SPPB below 10), the expanded SPPB, which includes longer and more challenging balance and walking tasks, may not add additional value. Postural sway center of pressure metrics including mediolateral range, anteroposterior range, and 95% ellipse area when standing on foam were associated with falls after controlling for confounders. When proprioception is challenged, older adults with less postural control are more likely to lose their balance and fall. When standing on a firm base, these center of pressure measures were not associated with falls in our study. Standing on a firm base may not be not a challenging enough task for older adults. Previous studies have also demonstrated that poor postural control is related to falls in older adults when proprioception is challenged among a variety of force plate measures alone.42,43 Our results further demonstrate the importance of including postural control measures even after adjusting for age, sex, depression, number of medications, and fall history. Fall prediction models may benefit from including a postural stability measure specifically when proprioception is challenged.
After controlling for confounding variables, several measures of physical function were not associated with one or more future falls in our study. While our gait measures were comparable to previous studies with low functioning older adults,44,45 none of the gait measures at usual or fast speeds derived from an instrumented walkway were significantly associated with one or more future falls. Previous prospective studies found that stride length, double support phase, and gait variability were associated with future falls.46,47 It is possible that our sample size was too small to detect significant associations, as these previous studies included larger sample sizes. Another 12-month prospective study in older adults with a similar sample size to ours did not find significant associations with gait variables derived from an instrumented walkway and future falls.45 We also found that leg strength and leg power were not significantly associated with one or more future falls. Previous studies have reported mixed results. In the Osteoporotic Fractures in Men Study, lower leg power in older men was associated with greater fall risk injury.48,49 Another study, though, did not find differences in leg strength between fallers and non-fallers over a year, while balance and gait measures were significantly different.50 Because the SPPB includes a sit-to-stand task that also measures leg strength, the SPPB may be enough capture leg strength.
This study has many strengths, including using monthly fall calendars which is the gold standard to record falls. The prospective study design also allowed us to determine baseline physical function measures that were associated with falls over 12 months. This study was also balanced with approximately 50% male and female participants, and over 30% of the participants were of African American race. However, there are also limitations to consider. This study had a small sample size, and the older adults included where those with lower physical function. These results may not be generalizable to older adults of higher physical function or those at a low risk for falls. Future studies should determine whether physical function measures differ in predicting falls for those at low and high fall risk. Because of the small sample size and distribution of some categorical variables, we did not have enough power to develop a meaningful prediction model; however, we were able to assess variables in unadjusted and adjusted analyses to evaluate potential variables that can be considered in future prediction models. Future studies with larger sample sizes should further determine if instrumented-based assessments provide prognostic value for predicting falls compared to clinical assessments alone.
When developing future fall prediction models, researchers should consider collecting and including fall history, the SPPB, and postural sway measures from a force plate when standing on foam. Static and dynamic balance tasks appear to be associated with future falls and may be better measures of physical function to include in prediction models compared to other measures. If resources limit performing the SPPB or accessing postural sway with a force plate, fall history alone is useful to identify future older adult fallers. Including these measures in future fall prediction models may improve the accuracy of those models. An important first step in falls prevention is identifying those at risk for falls, and having robust prediction models will help to identify older adults who may benefit from fall prevention interventions.
Highlights.
We identified physical function measures in older adults associated with future falls
Fall history, Short Physical Performance Battery, and postural instability were associated with future falls
When adjusting for fall history, postural instability on foam was associated with future falls
Fall prediction models may consider including these measures to predict future falls
Acknowledgements
This work was supported by grants from the National Institutes of Health (R01 AG042411, T32 AG033534, F32 AG077940, P30 AG021332, K25 AG068253).
Footnotes
Credit author statement
Conceptualization: KLH and DKH
Methodology: JLS, KLH, DKH
Formal Analysis: JLS
Writing – original - draft: KLH
Writing – review & edit: KLH, JLS, RN, APM, JAT, DKH
Supervision: DKH
Funding acquisition: DKH, JAT, APM
Declaration of Competing Interest
All authors have no conflicts of interest.
References
- 1.Bergen G, Stevens MR, Burns ER. Falls and Fall Injuries Among Adults Aged ≥65 Years - United States, 2014. MMWR Morb Mortal Wkly Rep. Sep 23 2016;65(37):993–998. doi: 10.15585/mmwr.mm6537a2 [DOI] [PubMed] [Google Scholar]
- 2.Haddad YK, Shakya I, Moreland BL, Kakara R, Bergen G. Injury Diagnosis and Affected Body Part for Nonfatal Fall-Related Injuries in Community-Dwelling Older Adults Treated in Emergency Departments. J Aging Health. Dec 2020;32(10):1433–1442. doi: 10.1177/0898264320932045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. Sep 2006;35 Suppl 2:ii37–ii41. doi: 10.1093/ageing/afl084 [DOI] [PubMed] [Google Scholar]
- 4.Painter JA, Allison L, Dhingra P, Daughtery J, Cogdill K, Trujillo LG. Fear of falling and its relationship with anxiety, depression, and activity engagement among community-dwelling older adults. Am J Occup Ther. Mar-Apr 2012;66(2):169–76. doi: 10.5014/ajot.2012.002535 [DOI] [PubMed] [Google Scholar]
- 5.Kempen GI, van Haastregt JC, McKee KJ, Delbaere K, Zijlstra GA. Socio-demographic, health-related and psychosocial correlates of fear of falling and avoidance of activity in community-living older persons who avoid activity due to fear of falling. BMC Public Health. Jun 2 2009;9:170. doi: 10.1186/1471-2458-9-170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dormosh N, Schut MC, Heymans MW, van der Velde N, Abu-Hanna A. Development and Internal Validation of a Risk Prediction Model for Falls Among Older People Using Primary Care Electronic Health Records. The Journals of Gerontology: Series A. 2021;doi: 10.1093/gerona/glab311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gade GV, Jørgensen MG, Ryg J, Masud T, Jakobsen LH, Andersen S. Development of a multivariable prognostic PREdiction model for 1-year risk of FALLing in a cohort of community-dwelling older adults aged 75 years and above (PREFALL). BMC Geriatrics. 2021/06/30 2021;21(1):402. doi: 10.1186/s12877-021-02346-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oshiro CES, Frankland TB, Rosales AG, et al. Fall Ascertainment and Development of a Risk Prediction Model Using Electronic Medical Records. Journal of the American Geriatrics Society. 2019;67(7):1417–1422. doi: 10.1111/jgs.15872 [DOI] [PubMed] [Google Scholar]
- 9.van de Loo B, Seppala LJ, van der Velde N, et al. Development of the ADFICE_IT Models for Predicting Falls and Recurrent Falls in Community-Dwelling Older Adults: Pooled Analyses of European Cohorts With Special Attention to Medication. The Journals of Gerontology: Series A. 2022;77(7):1446–1454. doi: 10.1093/gerona/glac080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: A review of the literature. Maturitas. 2013/05/01/ 2013;75(1):51–61. doi: 10.1016/j.maturitas.2013.02.009 [DOI] [PubMed] [Google Scholar]
- 11.Peterka RJ. Sensory integration for human balance control. Handbook of clinical neurology. 2018;159:27–42. [DOI] [PubMed] [Google Scholar]
- 12.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. Feb 1991;39(2):142–8. doi: 10.1111/j.1532-5415.1991.tb01616.x [DOI] [PubMed] [Google Scholar]
- 13.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. Journal of gerontology. 1994;49(2):M85–M94. [DOI] [PubMed] [Google Scholar]
- 14.Alcazar J, Losa-Reyna J, Rodriguez-Lopez C, et al. The sit-to-stand muscle power test: An easy, inexpensive and portable procedure to assess muscle power in older people. Exp Gerontol. Oct 2 2018;112:38–43. doi: 10.1016/j.exger.2018.08.006 [DOI] [PubMed] [Google Scholar]
- 15.Omaña H, Bezaire K, Brady K, et al. Functional Reach Test, Single-Leg Stance Test, and Tinetti Performance-Oriented Mobility Assessment for the Prediction of Falls in Older Adults: A Systematic Review. Phys Ther. Oct 1 2021;101(10)doi: 10.1093/ptj/pzab173 [DOI] [PubMed] [Google Scholar]
- 16.Gadkaree SK, Sun DQ, Huang J, Varadhan R, Agrawal Y. Comparison of Simple Versus Performance-Based Fall Prediction Models: Data From the National Health and Aging Trends Study. Gerontology and Geriatric Medicine. 2015/01/01 2015;1:2333721415584850. doi: 10.1177/2333721415584850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gafner SC, Allet L, Hilfiker R, Bastiaenen CHG. Reliability and diagnostic accuracy of commonly used performance tests relative to fall history in older persons: a systematic review. Clinical interventions in aging. 2021;16:1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lusardi MM, Fritz S, Middleton A, et al. Determining risk of falls in community dwelling older adults: a systematic review and meta-analysis using posttest probability. Journal of geriatric physical therapy (2001). 2017;40(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.da Costa BR, Rutjes AWS, Mendy A, Freund-Heritage R, Vieira ER. Can falls risk prediction tools correctly identify fall-prone elderly rehabilitation inpatients? A systematic review and meta-analysis. PloS one. 2012;7(7):e41061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Houston DK MA, Neiberg RH, Demons JL, Campos CL, Delbono O, Kritchevsky SB, Tooze JA. The effect of vitamin D supplementation on lower extremity power, strength and physical performance in older adults: a randomized controlled trial. J Frailty Aging. 2020;9(Suppl 1):S28. [Google Scholar]
- 21.Sheehan TJ, Fifield J, Reisine S, Tennen H. The measurement structure of the Center for Epidemiologic Studies Depression scale. Journal of personality assessment. 1995;64(3):507–521. [DOI] [PubMed] [Google Scholar]
- 22.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. Mar 1994;49(2):M85–94. doi: 10.1093/geronj/49.2.m85 [DOI] [PubMed] [Google Scholar]
- 23.Simonsick EM, Newman AB, Nevitt MC, et al. Measuring higher level physical function in well-functioning older adults: expanding familiar approaches in the Health ABC study. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2001;56(10):M644–M649. [DOI] [PubMed] [Google Scholar]
- 24.Bassey EJ, Short AH. A new method for measuring power output in a single leg extension: feasibility, reliability and validity. Eur J Appl Physiol Occup Physiol. 1990;60(5):385–90. doi: 10.1007/bf00713504 [DOI] [PubMed] [Google Scholar]
- 25.Lafond D, Corriveau H, Hébert R, Prince F. Intrasession reliability of center of pressure measures of postural steadiness in healthy elderly people11No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the authors(s) or upon any organization with which the author(s) is/are associated. Archives of Physical Medicine and Rehabilitation. 2004/06/01/ 2004;85(6):896–901. doi: 10.1016/j.apmr.2003.08.089 [DOI] [PubMed] [Google Scholar]
- 26.Raymakers JA, Samson MM, Verhaar HJJ. The assessment of body sway and the choice of the stability parameter(s). Gait & Posture. 2005/01/01/ 2005;21(1):48–58. doi: 10.1016/j.gaitpost.2003.11.006 [DOI] [PubMed] [Google Scholar]
- 27.Webster KE, Wittwer JE, Feller JA. Validity of the GAITRite® walkway system for the measurement of averaged and individual step parameters of gait. Gait & posture. 2005;22(4):317–321. [DOI] [PubMed] [Google Scholar]
- 28.Hannan MT, Gagnon MM, Aneja J, et al. Optimizing the Tracking of Falls in Studies of Older Participants: Comparison of Quarterly Telephone Recall With Monthly Falls Calendars in the MOBILIZE Boston Study. American Journal of Epidemiology. 2010;171(9):1031–1036. doi: 10.1093/aje/kwq024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yoshida K, Bohn J, Yoshida MK. Package ‘tableone’. R Foundation for Statistical Computing, Vienna, Austria: (30 November 2016). 2020; [Google Scholar]
- 30.Tierney NJ, Cook DH. Expanding tidy data principles to facilitate missing data exploration, visualization and assessment of imputations. arXiv preprint arXiv:180902264. 2018; [Google Scholar]
- 31.Fox J, Weisberg S, Adler D, et al. Package ‘car’. Vienna: R Foundation for Statistical Computing. 2012. [Google Scholar]
- 32.Sun DQ, Huang J, Varadhan R, Agrawal Y. Race and fall risk: data from the National Health and Aging Trends Study (NHATS). Age Ageing. Jan 2016;45(1):120–7. doi: 10.1093/ageing/afv173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Choi NG, Gell NM, DiNitto DM, Marti CN, Kunik ME. Depression and activity-limiting fall worry among older adults: longitudinal reciprocal relationships. Int Psychogeriatr. Apr 2020;32(4):495–504. doi: 10.1017/s1041610219000838 [DOI] [PubMed] [Google Scholar]
- 34.Yao Q, Jin W, Li Y. Associations between fear of falling and activity restriction and late life depression in the elderly population: Findings from the Irish longitudinal study on ageing (TILDA). J Psychosom Res. Jul 2021;146:110506. doi: 10.1016/j.jpsychores.2021.110506 [DOI] [PubMed] [Google Scholar]
- 35.Iaboni A, Flint AJ. The Complex Interplay of Depression and Falls in Older Adults: A Clinical Review. The American Journal of Geriatric Psychiatry. 2013/05/01/ 2013;21(5):484–492. doi: 10.1016/j.jagp.2013.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Laird RD, Studenski S, Perera S, Wallace D. Fall history is an independent predictor of adverse health outcomes and utilization in the elderly. Am J Manag Care. Dec 2001;7(12):1133–8. [PubMed] [Google Scholar]
- 37.Makino K, Lee S, Bae S, et al. Simplified Decision-Tree Algorithm to Predict Falls for Community-Dwelling Older Adults. J Clin Med. Nov 5 2021;10(21)doi: 10.3390/jcm10215184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Montero-Odasso M, van der Velde N, Martin FC, et al. World guidelines for falls prevention and management for older adults: a global initiative. Age and Ageing. 2022;51(9)doi: 10.1093/ageing/afac205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lauretani F, Ticinesi A, Gionti L, et al. Short-Physical Performance Battery (SPPB) score is associated with falls in older outpatients. Aging Clin Exp Res. Oct 2019;31(10):1435–1442. doi: 10.1007/s40520-018-1082-y [DOI] [PubMed] [Google Scholar]
- 40.Welch SA, Ward RE, Beauchamp MK, Leveille SG, Travison T, Bean JF. The Short Physical Performance Battery (SPPB): A Quick and Useful Tool for Fall Risk Stratification Among Older Primary Care Patients. Journal of the American Medical Directors Association. 2021/08/01/ 2021;22(8):1646–1651. doi: 10.1016/j.jamda.2020.09.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pettersson B, Nordin E, Ramnemark A, Lundin-Olsson L. Neither Timed Up and Go test nor Short Physical Performance Battery predict future falls among independent adults aged ≥75 years living in the community. J Frailty Sarcopenia Falls. Jun 2020;5(2):24–30. doi: 10.22540/jfsf-05-024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Anson E, Studenski S, Sparto PJ, Agrawal Y. Community-dwelling adults with a history of falling report lower perceived postural stability during a foam eyes closed test than non-fallers. Experimental Brain Research. 2019/03/01 2019;237(3):769–776. doi: 10.1007/s00221-018-5458-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Piirtola M, Era P. Force Platform Measurements as Predictors of Falls among Older People – A Review. Gerontology. 2006;52(1):1–16. doi: 10.1159/000089820 [DOI] [PubMed] [Google Scholar]
- 44.Hollman JH, McDade EM, Petersen RC. Normative spatiotemporal gait parameters in older adults. Gait & Posture. 2011/05/01/ 2011;34(1):111–118. doi: 10.1016/j.gaitpost.2011.03.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Paterson K, Hill K, Lythgo N. Stride dynamics, gait variability and prospective falls risk in active community dwelling older women. Gait & Posture. 2011/02/01/ 2011;33(2):251–255. doi: 10.1016/j.gaitpost.2010.11.014 [DOI] [PubMed] [Google Scholar]
- 46.Callisaya ML, Blizzard L, Schmidt MD, et al. Gait, gait variability and the risk of multiple incident falls in older people: a population-based study. Age and Ageing. 2011;40(4):481–487. doi: 10.1093/ageing/afr055 [DOI] [PubMed] [Google Scholar]
- 47.Verghese J, Holtzer R, Lipton RB, Wang C. Quantitative Gait Markers and Incident Fall Risk in Older Adults. The Journals of Gerontology: Series A. 2009;64A(8):896–901. doi: 10.1093/gerona/glp033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chan BKS, Marshall LM, Winters KM, Faulkner KA, Schwartz AV, Orwoll ES. Incident Fall Risk and Physical Activity and Physical Performance among Older Men: The Osteoporotic Fractures in Men Study. American Journal of Epidemiology. 2006;165(6):696–703. doi: 10.1093/aje/kwk050 [DOI] [PubMed] [Google Scholar]
- 49.Winger ME, Caserotti P, Cauley JA, et al. Lower Leg Power and Grip Strength Are Associated With Increased Fall Injury Risk in Older Men: The Osteoporotic Fractures in Men Study. The Journals of Gerontology: Series A. 2022;doi: 10.1093/gerona/glac122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bird M-L, Pittaway JK, Cuisick I, Rattray M, Ahuja KD. Age-related changes in physical fall risk factors: results from a 3 year follow-up of community dwelling older adults in Tasmania, Australia. International journal of environmental research and public health. 2013;10(11):5989–5997. [DOI] [PMC free article] [PubMed] [Google Scholar]