Abstract
Non-syndromic cleft lip with or without cleft palate (NSCL/P) is the most common developmental defect that significantly affects the morphology and function of the stomatognathic system in children. The etiology of these birth defects is multifactorial, and single nucleotide polymorphisms (SNPs) in IRF6 and FGF1 have been associated with NSCL/P. This study aimed to evaluate whether SNPs in IRF6, namely rs2013162, rs642961, rs2235373, and rs34010 in FGF1, are associated with NSCL/P occurrence in the Polish population. The study included 627 participants: 209 children with NSCL/P and 418 healthy controls. DNA was isolated from saliva in the study group and from umbilical cord blood in controls. Genotyping of polymorphisms was performed using quantitative PCR. There was no statistically significant association of IRF6 gene variants with NSCL/P occurrence, although for rs2013162, AA genotype, odds ratio (OR) = 1.16 and for AC genotype, OR = 0.83; for rs642961, AA genotype, OR = 0.84 and for AG genotype, OR = 1.41; and for rs2235373, AA genotype, OR = 0.79 and for AG, OR = 0.85. In the instance of rs34010 polymorphism in FGF1, the presence of the AA genotype was statistically significant in reducing the risk of NSCL/P (OR = 0.31, p = 0.001). Genetic variation in FGF1 is an important risk marker of NSCL/P in the Polish population, which cannot be stated for the polymorphisms in the IRF6 gene.
Keywords: birth defect, cleft lip, cleft palate, genetic variation, single nucleotide polymorphism, IRF6, FGF1
1. Introduction
Annually, more than 8 million children are born worldwide with various birth defects, 17% of which affect the facial part of the skull [1]. Orofacial clefts (OFCs) are the most common congenital anomaly affecting the facial part of the skull and the second most common birth defect in newborn children overall (after phimosis). The most common ORFs are non-syndromic cleft lip with or without cleft palate (NSCL/P), which occur with an average prevalence of 1 in 700 live births [2], and affect 135,000 newborns worldwide [3]. The prevalence of NSCL/P varies among ethnic groups and depends on the geographic origin. Infants with congenital malformations are born significantly more often in parts of South America and Asia, while the fewest are born in Israel, South Africa, and Southern Europe [4]. The cleft palate only (CPO) phenotype occurs less frequently, with a worldwide average of 1–25 in 10,000 children [5]. A higher incidence of isolated cleft palate is reported in Canada and Northern Europe, and significantly lower in parts of Latin America and South Africa [4].
The medical care of children with NSCL/P requires a comprehensive approach. The defect impairs many aspects of daily life, including eating, speech, and due to facial appearance, social interaction with peers [6]. The etiology of ORFs is quite complex, involving both genetic and environmental factors [7]. Many studies indicate that the genetic component has a very strong influence on the development of facial birth defects. The risk of NSCL/P is three times higher in siblings than in the general population and is 25–45% for monozygotic twins compared to 3–6% for heterozygotic twins. Moreover, the risk of birth defects for first-degree relatives is estimated at 4%; for second-degree relatives, 0.67%; and for third-degree relatives, 0.3% [8]. However, the lack of complete coincidence of the occurrence of NSCL/P in monozygotic twins shows that environmental factors also play important roles in the etiology of clefts [9].
Although the last few decades have seen tremendous progress in understanding the genetic basis of syndromic birth defects [10], the identification of specific genetic variants involved in the onset of NSCL/P has progressed at a slower pace, primarily due to the presence of a significant environmental component [2]. Numerous studies have shown that several genes are related to craniofacial deformities [11,12,13,14].
In recent years, advances in research techniques have accelerated the identification of genes and their polymorphisms correlating with NSCL/P occurrence through the use of genome-wide association studies (GWAS) and whole genome sequencing. Numerous studies have shown that a gene whose polymorphisms may be associated with NSCL/P is the IRF6 gene, mutations of which are responsible for van der Woude syndrome (VWS) [12,15,16]. Loss-of-function mutations in the IRF6 gene are responsible for approximately 70% of VWS syndrome cases (VWS1, MIM#119300) [17]. Multiple studies have indicated that polymorphisms of the IRF6 gene could be an important factor in the etiology of non-syndromic malformations [18,19,20]. Genes coding for fibroblast growth factors and their receptors, for instance, FGF1, are considered excellent candidate genes. Their proteins play important roles in craniofacial growth and their polymorphisms may influence the abnormal development of palatal and connective tissue structures [21].
The purpose of the present study was to replicate the association between four single nucleotide polymorphisms (SNPs; rs2013162, rs642961, rs2235375, and rs34010) in the IRF6 and the FGF1 gene and NSCL/P in Polish children. Therefore, we compared the frequencies of the four SNPs between children with and without NSCL/P.
2. Materials and methods
2.1. Study population
We studied unselected children with NSCL/P and healthy controls. The study included patients being treated for orthodontic conditions at the Pomeranian Medical University in Szczecin or the Wroclaw Medical University Department of Dentofacial Orthopeadics and Orthodontics.
In the NSCL/P group (n = 209), clinical diagnostics of existing congenital defects and differential diagnostics for monogenic syndromes related to NSCL/P were based on medical and anamnesis history followed by clinical examination. The type of cleft was assessed according to the World Health Organization classification – International Statistical Classification of Diseases and Related Health Problems – ICD 10; Congenital malformations, deformations, and chromosomal abnormalities section (Q35–Q37) [22].
In the control group, 418 unsanctioned children (average age: 14.0 + 10.2 years) were recruited and their genetic material was stored in the Szczecin Department of Genetics and Pathology’s biobank. Patients with NSCL/P and the control group were matched on age and geography. A total of 180 children were enrolled from Szczecin and 238 were enrolled from Wroclaw.
2.2. Sample preparation
In the group of children with NSCL/P, 2 ml of saliva samples were collected from each subject using Oragene collection kits (DNA Genotek Inc., Canada). Subjects were asked not to consume any solid food for 30 min before the collection of the biological material. Samples were stored in a dry place, protected from light, at room temperature. DNA was isolated using automatic Chemagen sets. The DNA extracted from the samples was stored in a freezer at −20°C. In the control group, DNA from the umbilical cord blood was extracted using the standard method described by Lahiri and Schnabel [23].
2.3. Genotyping
Genotyping of rs2013162, rs642961, rs2235373, and rs34010 was performed using the real-time PCR-based TaqMan technique with LightCycler 480 II (Roche Diagnostics). The mixture (5 µl total) consisted of 2.5 µl of LightCycler 480 Probes Master Mix (Roche Diagnostics), 0.0625 µl of each SNP TaqMan Genotyping Assay × 40 (Applied Biosystems), 1 µl of DNA (25 ng/µl), and 1.4375 µl of deionized water (Roche Diagnostics). On each plate, four negative controls without DNA were included to monitor potential contamination. Primers used for the detection of gene polymorphisms were as follows:
rs2013162 forward: CACCTGCGAGCTTGTGTATC; reverse: CCATCATCCCCACTCACCAT,
rs642961 forward: GCTTTGGATTGTTAATCTTACCCAAAGG; reverse: CTTCCCACCTCCAGGACAGGCAGATG,
rs2235373 forward: AAGTAAGTGAGACTTTATCTTTC; reverse: TCCCTGGTGACTCATGGGCT, and
rs34010 forward: GGCCTCTACCCACTAGATGCCAGTAG; reverse: CTGCTTTCATTATCAACCTGCACAGG.
2.4. Statistical analysis
A logistic regression test used for nonlinear analysis was used for statistical analysis to describe the effect of independent variables on the dichotomous dependent variable. The odds ratio (OR) with a 95% confidence interval (95% CI) was calculated to estimate the risk of a craniofacial cleft defect. The most common genotype was used as a reference. For each genetic variation, the risk carried by the occurrence of the given genotypes on the occurrence of the birth defect was evaluated with respect to the control group. The significance of individual logistic regression coefficients was evaluated using Wald’s test. The OFC risk was assessed for each genotype. The significance of particular logistic regression rates was assessed using Wald’s test. Statistica 10.0 (StatSoft, Tulsa OK, USA) and R 3.0.2 (The R Foundation for Statistical Computing) were used for statistical analysis. P-values of less than 0.05 were considered significant.
Biobank materials obtained from umbilical cord blood were used as the control group, and deposited in the Department of Genetics and Pathomorphology of Pomeranian Medical University in Szczecin. In the control group, individuals were selected based on their age and region of birth.
Ethical approval: The Bioethics Committee of Pomeranian Medical University in Szczecin approved the research protocol as complying with GCP – Good Clinical Practice (KB-0012/77/10). Oncology biobank project approved by PAM Ethics Committee (BN-001/174/05 dated 11. 10. 2005). Informed consent was obtained from all patients or their legal guardians before participating in the study.
3. Results
The study group consisted of 209 individuals with NSCL/P (age range, 4–30 years; mean age, 17.4 ± 13.6 years). The control group consisted of 418 subjects matched for age and birthplace. Relatives in the ascending line up to the second generation in both groups were Polish. The NSCL/P group consisted of 91 women (43.5%) and 118 men (56.5%). In 113 cases (54.1%), unilateral cleft of the lip and the hard palate was observed; in 45 cases (21.5%), – bilateral cleft of the lip and hard palate; in 32 cases (15.3%), CPO; and in 19 cases (9.1%), isolated cleft lip. The characteristics of the NSCL/P patients are presented in Table 1.
Table 1.
Characteristics of patients with NSCL/P [24]
| No. and proportion of individuals | ||
|---|---|---|
| Sex | Female | 91 (43.5%) |
| Male | 118 (56.5%) | |
| Cleft type | Unilateral cleft of the lip and the hard palate | 113 (54.1%) |
| Bilateral cleft of the lip and the hard palate | 45 (21.5%) | |
| CPO | 32 (15.3%) | |
| Isolated cleft lip | 19 (9.1%) |
Table 2 summarizes the results obtained for the IRF6 gene. Statistical analysis showed that the rs2013162 polymorphism did not significantly predict the risk of the cleft defect (p = 0.455). The OR for genotypes AA and AC were, respectively, 1.16 (0.66–2.07) with a significance level of p = 0.604 and 0.83 (0.56–1.25) with a significance level of p = 0.382. A similarly statistically insignificant result was obtained for the rs642961 polymorphism (p = 0.189). In this case, the OR was 0.84 (0.34–2.08) for the AA genotype, with a significance level of p = 0.709, and 1.41 (0.95–2.07) for the AG genotype, with a significance level of p = 0.085. Also, the analysis of the rs2235373 polymorphism showed no significant (p = 0.716) change in the risk of the OR of congenital craniofacial malformations with OR = 0.79 (0.24–2.68), p = 0.71 (for the AA variant) and OR = 0.85 (0.55–1.31), p = 0.453 (for the AG variant). On the other hand, the presence of the rs34010 polymorphism statistically significant affects the risk of developing a cleft defect (p < 0.001, Table 3). A reduced risk (OR = 0.31 (0.18–0.54)) is carried out by the presence of the AA genotype ( p < 0.001) and the AC genotype, but in this case this was not confirmed by statistical significance (p = 0.219).
Table 2.
NSCL/P risk and polymorphisms in the IRF6 gene (namely, rs2013162, rs642961, rs2235373)
| Genotype | OR (95% CI) | P (Wald’s test) | P (LR-test) |
|---|---|---|---|
| rs2013162 ref. = CC | 0.455 | ||
| AA | 1.16 (0.66–2.07) | 0.604 | |
| AC | 0.83 (0.56–1.25) | 0.382 | |
| rs642961 ref. = GG | 0.189 | ||
| AA | 0.84 (0.34–2.08) | 0.709 | |
| AG | 1.41 (0.95–2.07) | 0.085 | |
| rs2235373 ref. = GG | 0.716 | ||
| AA | 0.79 (0.24–2.68) | 0.71 | |
| AG | 0.85 (0.55–1.31) | 0.453 |
Table 3.
NSCL/P risk and rs34010 polymorphism in the FGF1 gene
| Genotype | OR (95% CI) | P (Wald’s test) | P (LR-test) |
|---|---|---|---|
| rs34010 ref. = CC | <0.001 | ||
| AA | 0.31 (0.18–0.54) | <0.001 | |
| AC | 0.77 (0.51–1.17) | 0.219 |
The distribution of genotypes for rs34010 is shown in Figure 1. The presented result of the fluorescence analysis of the sample was performed using a LightCycler 480II. The blue color represents the AC allele (stained with VIC dye); the green color, if present, would represent the AA allele (stained with FAM dye); and the red color represents both alleles.
Figure 1.
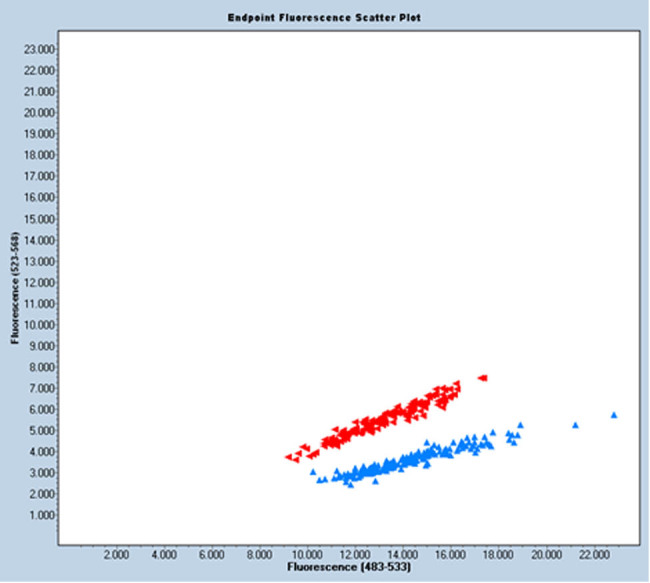
Graphical distribution of genotypes for rs34010.
4. Discussion
In the present study, we found an association between the presence of SNP rs34010 within FGF1 and the risk of NSCL/P in a Polish population. The same results were obtained in a study conducted on Latvian, Lithuanian, and Estonian populations. It was shown that the occurrence of a rarer allele of the rs34010 polymorphism in the FGF1 gene is associated with a reduced incidence of the cleft defect. A particularly strong association with a decreased risk (OR = 0.689; 95% CI, 0.559–0.849; p = 4.56 × 10−4) was found for the protective rs250092/rs34010 GT haplotype, within the aforementioned gene [25].
The FGF gene family signaling pathway is responsible for the regulation and proper execution of many developmental processes as early as embryogenesis. It plays an important role in the formation of head structures, particularly the craniofacial region and palate development. Conducted studies in the FGF gene family have shown an overrepresentation of missense mutations in patients with cleft palates compared with healthy individuals. It has been shown that a group of missense and nonsense mutations (M369I, E467K, R609X, D138N, R84S, V329I, D73H de novo, S59F, K172) can account for up to 5% of NSCL/P cases. Taken together with the results for IRF6 −12%, FOXE1, GLI2, MSX2, SKI, and SPRY2 −6%, and MSX1 −2% [11,12,26], these genes may account for more than 25% of NSCL/P and represent a significant predictor of facial clefts [27]. The missense and nonsense FGFR1 mutations indicate problems with reduced penetrance when identifying mutations in ORFs. The R609X mutation was found in a father and his daughter. The M369I mutation correlates with the cleft phenotype in the family, but there were family members without a birth defect with this mutation, who may be examples of reduced penetrance. Some apparently nonpenetrating individuals in ORF families show other phenotypic features, such as discontinuity of the orbicularis oris muscle [28,29].
Human FGFs control a wide range of biological functions, and their biological activity is mediated by seven major FGF receptor tyrosine kinases encoded by four genes (FGFR1-4). In the presence of heparan sulfate proteoglycans, two FGFs bind to two FGFRs, inducing receptor dimerization and allowing intracellular tyrosine kinase domains to phosphorylate and activate [30]. As a result of impaired FGF signaling, craniofacial syndromes, craniofacial dysplasia, and Kallmann syndrome may result. The S252W and P253R mutations in the FGFR2 gene are responsible for almost all cases of Apert syndrome. The cleft type is associated with the S252W mutation in 59% of patients, with the P253R mutation in 17% of patients. Cleft palate is present in 44% of Apert syndrome cases [31,32,33]. Autosomal-dominant Kallmann syndrome, whose main features are anosmia and hypogonadism, is caused by loss-of-function mutations in FGFR1, and 5–10% of these patients have cleft [34,35,36].
In this study, we found no association between the presence of IRF6 gene SNPs and the occurrence of NSCL/P. Interferon regulatory factor (IRF6) plays an important role during embryonic development. This factor is responsible for immune system function and wound healing [37]. Unlike the other interferon regulatory factors, IRF6 is also crucial during fetal cranial growth and the development of ectodermal structures [38]. Lack of IRF6 expression may implicate birth defects such as VWS and popliteal pterygium syndrome [39]. These defects are characterized by the presence of a cleft palate and abnormalities of the teeth (20–40%) and skin and mucous membranes [40].
For the rs2013162 SNP located in the IRF6 gene in the present study, ORs were 1.16 for the AA genotype and 0.83 for the AC genotype, but these results were not statistically significant. Similarly, a statistically insignificant result was obtained by Huang et al. subjecting a Chinese population [41]. But these results are significantly different from those conducted previously on Italian, American, and Belgian populations [42,43,44], in which a strong association between the occurrence of rs2013162 polymorphism and the occurrence of isolated cleft facial defects was demonstrated, and by Park et al. [45] on the Chinese population. Also in each of the above-mentioned studies, in the haplotype analysis, it was noted that the C allele was present in all individuals affected by cleft lip or palate.
The literature data suggest a correlation of rs642961 with the occurrence of craniofacial cleft defects. The results of the studies present a contradictory view. The first study was conducted on the Brazilian population, but the researchers chose a small size of the control group, which, with MAF A = 0.017 (characterizes this variation), may not be a representative result for the entire population. In their study, 228 cleft patients and 126 healthy subjects were examined [46]. Another publication in which the results indicate that there is no association between rs642961 and the occurrence of isolated facial cleft defects is based on a study of a Honduran population [19]. However, other publications describe examples of positive correlations with the occurrence of cleft defects. A paper describing a Brazilian population presents a correlation between the polymorphisms and the occurrence of cleft, although only in a group of individuals with isolated cleft palate [47]. Researchers from China, in addition to finding a relationship between this genetic variation and the occurrence of congenital cleft defects, demonstrated that rs642961 can alter the expression of the IRF6 gene in vivo. They have surgically removed a small section of the lip skin with tissue adjacent to the region of the cleft lip present. They have indicated that the genotypes of this polymorphism are in correlation with different expression levels of IRF6 gene receptors [48]. Interestingly, studies conducted on a Polish group of patients show the result of a positive correlation with the occurrence of isolated facial cleft defects, which is statistically significant. The reported OR coefficient was 1.63, with a significance level of p = 0.05 [49]. Also, a high OR coefficient (1.79) at the retained level of significance is reported in the results of their work by Birnbaum et al. whose study was based on the examination of genetic material collected from 460 subjects with isolated cleft lips with or without cleft palate and from 952 control subjects, representatives of the Caucasian population [50].
An interesting finding was made by Murdoch et al., who examined the absence of tooth buds and palate type in association with a given genotype. As a result, it has been found that the first palatal folds on the right side were larger than on the left side in the group of individuals with the rs642961 polymorphism, although p = 0.06, indicating the need for further research. No correlation was found concerning hypodontia [51].
In the present study, the results obtained for the IRF6 rs2235373 gene polymorphism were not found to be statistically significant. In the literature, evidence showing a sevenfold increased predisposition to congenital malformations correlated with the co-occurrence of haplotypes: GC rs2235373-rs2235371 (V274I) and AAG rs599021-rs2235373-rs595918 can be found [45]. A study including a Norwegian population (377 patients with isolated cleft lip with or without cleft palate, 196 patients with isolated cleft palate, and 763 healthy subjects) showed a reduced risk (OR = 0.38, p < 0.001) of isolated cleft lip with or without cleft palate in the presence of the rs2235371 (V274I) genotype, also located in the IRF6 gene. However, no association between the aforementioned polymorphism and the presence of an isolated cleft palate was demonstrated [52].
Studies in the Han population have shown that the risk of having a child with an isolated cleft lip with or without a cleft palate is increased for mothers who were taking medication or were exposed to passive smoking during the first trimester of pregnancy. Folic acid supplementation at the recommended dose had a protective effect on fetal development. The concomitant presence of the TT genotype of the rs2235373 polymorphism and a history of previous miscarriage increase the risk of an isolated cleft defect more than sixfold (OR = 6.7) [53]. Studies demonstrate the interaction of IRF6 and TGFA gene polymorphisms and an increased risk of the craniofacial cleft with their simultaneous presence [54].
In the Polish population, Mostowska et al. analyzed 18 polymorphisms of FOXE1, IRF6, MSX1, PAX9, TBX10, FGF10, FGFR1, TGFa, TGFb3, and SUMO1, and chromosomal region 8q24 in a group of 175 children with NSCL/P and a matched control group. A strongly significant association with NSCL/P risk was observed for rs642961 in IRF6 (OR [AG + AA vs GG] = 1.635, 95% CI 1.153–2.319, p = 0.005) [49]. Mostowska et al. also examined variants located in chromosomal regions 1p22.1, 10q25.3, 17q22, and 20q12 in a group of 206 individuals with NSCL/P and a matched control group of 446 individuals. As a result, rs227731 (located on 17q22) increased the risk of NSCL/P in the analysis in the dominant model (OR = 1.732, 95% CI 0.184–2.253, p = 0.0044). The lack of convergence of results in the Mostowska et al. [55] study may reflect differences in the geographic origin of cases compared with our study.
Reports to date on the predisposition of genetic variations to isolated cleft defects are usually based on single studies and are not in accordance with different research centers. Often, these studies are based on populations that are ethnically distinct from the Polish ones. Furthermore, there are no studies that clearly state that the predisposition for isolated cleft defects is based on a single gene. It is difficult to find papers that unambiguously point in the direction of research aimed at creating a probabilistic model of the etiology of ORFs that could be established [56].
4.1. Limitations
There has been extensive research on the etiology of NSCL/P but the results have been inconsistent. A study based on the association between SNPs and the presence of different phenotypes may have limited power to detect relevant complex inheritance patterns (e.g., synergistic involvement of different polymorphisms or interactions between environmental factors). In fact, ORs tend to be low or moderate when we examine the association between single genes and the risk of a complex trait that is likely to be regulated by a large number of genes. As a result, phenotypes result from a combination of genes and environmental factors. The residual genetic risk of nonsyndromic craniofacial clefts must therefore be explained by gene–environment interactions.
At this point, it is also worth noting that the conducted case–control studies are less adept at showing a causal relationship than cohort studies. They are also more prone to bias. The same hypothesis could also be studied in population-based cohort studies. Case–control studies do not require a long follow-up period and are easier to conduct. This design is especially useful for rare diseases but not for rare causes.
5. Conclusions
This is the first study to investigate the association between IRF6 and FGF1 genotypes and NSCL/P in the Polish population. Our findings suggest that rs34010 in the FGF1 gene is associated with a decreased risk of NSCL/P, while rs2013162, rs642961, and rs2235373 in the IRF6 gene require further study due to lack of statistical significance. This study contributes to our understanding of genetic factors related to NSCL/P; however, further investigation in a larger population is warranted.
Footnotes
Funding information: This research was supported by the National Science Centre, grant number 2169/B/P01/2011/40.
Author contributions: Conceptualization, A.Z., and A.J.; methodology, A.Z. and A.J.; software, S.G.; validation, K.W., and A.J.; formal analysis, A.Z.; investigation, A.Z.; B.K., and A.Z.-B. resources, A.Z., K.W., and B.K., A.Z.-B.; data curation, A.Z.; writing – original draft preparation, A.Z.; writing – review and editing, A.Z., K.G., J.J.-O., and J.L.C-G.; visualization, S.G. and A.Z.; supervision, K.W., A.J., and J.L.; project administration, A.Z., K.W., A.J., and J.L.; funding acquisition, K.W. and J.L. All authors have read and agreed to the published version of the manuscript.
Conflict of interest: The authors declare no conflict of interest.
Data availability statement: All data are available from the corresponding author upon request.
References
- [1].Baird PA, Anderson TW, Newcombe HB, Lowry RB. Genetic disorders in children and young adults: A population study. Am J Hum Genet. 1988 May;42(5):677–93. [PMC free article] [PubMed]
- [2].Dixon MJ, Marazita ML, Beaty TH, Murray JC. Cleft lip and palate: Understanding genetic and environmental influences. Nat Rev Genet. 2011 Mar;12(3):167–78. 10.1038/nrg2933. [DOI] [PMC free article] [PubMed]
- [3].Yuan Q, Blanton SH, Hecht JT. Genetic causes of nonsyndromic cleft lip with or without cleft palate. Adv Otorhinolaryngol. 2011;70:107–13. 10.1159/000322486. [DOI] [PubMed]
- [4].Mossey PA, Little J, Munger RG, Dixon MJ, Shaw WC. Cleft lip and palate. Lancet. 2009 Nov 21;374(9703):1773–85. 10.1016/S0140-6736(09)60695-4. [DOI] [PubMed]
- [5].Burg ML, Chai Y, Yao CA, 3rd Magee W, Figueiredo JC. Epidemiology, etiology, and treatment of isolated cleft palate. Front Physiol. 2016 Mar 1;7:67. 10.3389/fphys.2016.00067. [DOI] [PMC free article] [PubMed]
- [6].Wehby GL, Cassell CH. The impact of orofacial clefts on quality of life and healthcare use and costs. Oral Dis. 2010 Jan;16(1):3–10. 10.1111/j.1601-0825.2009.01588.x. [DOI] [PMC free article] [PubMed]
- [7].Vieira AR, McHenry TG, Daack-Hirsch S, Murray JC, Marazita ML. Candidate gene/loci studies in cleft lip/palate and dental anomalies finds novel susceptibility genes for clefts. Genet Med. 2008 Sep;10(9):668–74. 10.1097/gim.0b013e3181833793. [DOI] [PMC free article] [PubMed]
- [8].Drewa G. Genetyka medyczna. Podręcznik dla studentów. Wrocław. Poland: Edra Urban & Partner; 2011. p. 301.
- [9].Gorlin RJ, Jr Cohen MM, Hennekam RCM. Syndromes of the head and neck. New York: Oxford University Press; 2001. p. 236.
- [10].Marazita ML. The evolution of human genetic studies of cleft lip and cleft palate. Annu Rev Genomics Hum Genet. 2012;13:263–83. 10.1146/annurev-genom-090711-163729. [DOI] [PMC free article] [PubMed]
- [11].Jezewski PA, Vieira AR, Nishimura C, Ludwig B, Johnson M, O’Brien SE, et al. Complete sequencing shows a role for MSX1 in non-syndromic cleft lip and palate. J Med Genet. 2003 Jun;40(6):399–407. 10.1136/jmg.40.6.399. [DOI] [PMC free article] [PubMed]
- [12].Zucchero TM, Cooper ME, Maher BS, Daack-Hirsch S, Nepomuceno B, Ribeiro L, et al. Interferon regulatory factor 6 (IRF6) gene variants and the risk of isolated cleft lip or palate. N Engl J Med. 2004 Aug 19;351(8):769–80. 10.1056/NEJMoa032909. [DOI] [PubMed]
- [13].Chiquet BT, Lidral AC, Stal S, Mulliken JB, Moreno LM, Arcos-Burgos M, et al. CRISPLD2: A novel NSCLP candidate gene. Hum Mol Genet. 2007 Sep 15;16(18):2241–8. 10.1093/hmg/ddm176. [DOI] [PMC free article] [PubMed]
- [14].Zawiślak A, Woźniak K, Jakubowska A, Lubiński J, Kawala B, Znamirowska-Bajowska A. Polymorphic variants in VAX1 gene (rs7078160) and BMP4 gene (rs762642) and the risk of non-syndromic orofacial clefts in the Polish population. Dev Period Med. 2014;18(1):16–22. [PubMed]
- [15].Kerameddin S, Namipashaki A, Ebrahimi S, Ansari-Pour N. IRF6 Is a marker of severity in nonsyndromic cleft lip/palate. J Dent Res. 2015 Sep;94(9 Suppl):226S–32SS. 10.1177/0022034515581013. [DOI] [PubMed]
- [16].Ray D, Venkataraghavan S, Zhang W, Leslie EJ, Hetmanski JB, Weinberg SM, et al. Pleiotropy method reveals genetic overlap between orofacial clefts at multiple novel loci from GWAS of multi-ethnic trios. PLoS Genet. 2021 Jul 9;17(7):e1009584. 10.1371/journal.pgen.1009584. [DOI] [PMC free article] [PubMed]
- [17].Burdick AB. Genetic epidemiology and control of genetic expression in van der Woude syndrome. J Craniofacial Genet Dev Biol Suppl. 1986;2:99–105. [PubMed]
- [18].Butali A, Mossey PA, Adeyemo WL, Eshete MA, Gaines LA, Even D, et al. Novel IRF6 mutations in families with Van Der Woude syndrome and popliteal pterygium syndrome from sub-Saharan Africa. Mol Genet Genomic Med. 2014 May;2(3):254–60. 10.1002/mgg3.66. [DOI] [PMC free article] [PubMed]
- [19].Larrabee YC, Birkeland AC, Kent DT, Flores C, Su GH, Lee JH, et al. Association of common variants, not rare mutations, in IRF6 with nonsyndromic clefts in a Honduran population. Laryngoscope. 2011 Aug;121(8):1756–9. 10.1002/lary.21870. [DOI] [PubMed]
- [20].Wu-Chou YH, Lo LJ, Chen KT, Chang CS, Chen YR. A combined targeted mutation analysis of IRF6 gene would be useful in the first screening of oral facial clefts. BMC Med Genet. 2013 Mar 20;14:37. 10.1186/1471-2350-14-37. [DOI] [PMC free article] [PubMed]
- [21].Rafiqdoost Z, Rafiqdoost A, Rafiqdoost H, Hashemi M, Khayatzadeh J, Eskandari-Nasab E. Investigation of FGF1 and FGFR gene polymorphisms in a group of Iranian patients with nonsyndromic cleft lip with or without cleft palate. Int J Pediatr Otorhinolaryngol. 2014 May;78(5):731–6. 10.1016/j.ijporl.2014.01.024. [DOI] [PubMed]
- [22].WHO. International Statistical Classification of Diseases and Related Health Problems 10th Revision, 2019. Available at https://icd.who.int/browse10/2019/en [accessed 28 January 2021].
- [23].Lahiri DK, Schnabel B. DNA isolation by a rapid method from human blood samples: Effects of MgCl2, EDTA, storage time, and temperature on DNA yield and quality. Biochem Genet. 1993 Aug;31(7-8):321–8. 10.1007/BF02401826. [DOI] [PubMed]
- [24].Zawiślak A, Woźniak K, Agirre X, Gupta S, Kawala B, Znamirowska-Bajowska A, et al. Association of ABCA4 gene polymorphisms with cleft lip with or without cleft palate in the Polish population. Int J Env Res Public Health. 2021 Oct 31;18(21):11483. 10.3390/ijerph182111483. [DOI] [PMC free article] [PubMed]
- [25].Nikopensius T, Kempa I, Ambrozaitytė L, Jagomägi T, Saag M, Matulevičienė A, et al. Variation in FGF1, FOXE1, and TIMP2 genes is associated with nonsyndromic cleft lip with or without cleft palate. Birth Defects Res A Clin Mol Teratol. 2011 Apr;91(4):218–25. 10.1002/bdra.20791. [DOI] [PubMed]
- [26].Vieira AR, Avila JR, Daack-Hirsch S, Dragan E, Félix TM, Rahimov F, et al. Medical sequencing of candidate genes for nonsyndromic cleft lip and palate. PLoS Genet. 2005 Dec;1(6):e64. 10.1371/journal.pgen.0010064. [DOI] [PMC free article] [PubMed]
- [27].Wang H, Zhang T, Wu T, Hetmanski JB, Ruczinski I, Schwender H, , et al. The FGF and FGFR gene family and risk of cleft lip with or without cleft palate. Cleft Palate Craniofacial J. 2013 Jan;50(1):96–103. 10.1597/11-132. [DOI] [PMC free article] [PubMed]
- [28].Weinberg SM, Neiswanger K, Martin RA, Mooney MP, Kane AA, Wenger SL, et al. The Pittsburgh oral-facial cleft study: Expanding the cleft phenotype: Background and justification. Cleft Palate Craniofacial J. 2006 Jan;43(1):7–20. 10.1597/04-122r1.1. [DOI] [PubMed]
- [29].Riley BM, Mansilla MA, Ma J, Daack-Hirsch S, Maher BS, Raffensperger LM, et al. Impaired FGF signaling contributes to cleft lip and palate. Proc Natl Acad Sci U S A. 2007 Mar 13;104(11):4512–7. 10.1073/pnas.0607956104. [DOI] [PMC free article] [PubMed]
- [30].Mohammadi M, Olsen SK, Ibrahimi OA. Structural basis for fibroblast growth factor receptor activation. Cytokine Growth Factor Rev. 2005 Apr;16(2):107–37. 10.1016/j.cytogfr.2005.01.008. [DOI] [PubMed]
- [31].Slaney SF, Oldridge M, Hurst JA, Moriss-Kay GM, Hall CM, Poole MD, et al. Differential effects of FGFR2 mutations on syndactyly and cleft palate in Apert syndrome. Am J Hum Genet. 1996 May;58(5):923–32. [PMC free article] [PubMed]
- [32].Park WJ, Theda C, Maestri NE, Meyers GA, Fryburg JS, Dufresne C, et al. Analysis of phenotypic features and FGFR2 mutations in Apert syndrome. Am J Hum Genet. 1995 Aug;57(2):321–8. [PMC free article] [PubMed]
- [33].Kreiborg S, Jr Cohen MM. The oral manifestations of Apert syndrome. J Craniofacial Genet Dev Biol. 1992 Jan-Mar;12(1):41–8. [PubMed]
- [34].Dodé C, Levilliers J, Dupont JM, De Paepe A, Le DûN, Soussi-Yanicostas N, et al. Loss-of-function mutations in FGFR1 cause autosomal dominant Kallmann syndrome. Nat Genet. 2003 Apr;33(4):463–5. 10.1038/ng1122. [DOI] [PubMed]
- [35].Dodé C, Hardelin JP. Kallmann syndrome: Fibroblast growth factor signaling insufficiency? J Mol Med. 2004 Nov;82(11):725–34. 10.1007/s00109-004-0571-y. [DOI] [PubMed]
- [36].Kim HG, Herrick SR, Lemyre E, Kishikawa S, Salisz JA, Seminara S, et al. Hypogonadotropic hypogonadism and cleft lip and palate caused by a balanced translocation producing haploinsufficiency for FGFR1. J Med Genet. 2005 Aug;42(8):666–72. 10.1136/jmg.2004.026989. [DOI] [PMC free article] [PubMed]
- [37].Savitsky D, Tamura T, Yanai H, Taniguchi T. Regulation of immunity and oncogenesis by the IRF transcription factor family. Cancer Immunol Immunother. 2010 Apr;59(4):489–510. 10.1007/s00262-009-0804-6. [DOI] [PMC free article] [PubMed]
- [38].Richardson RJ, Dixon J, Malhotra S, Hardman MJ, Knowles L, Boot-Handford RP, et al. Irf6 is a key determinant of the keratinocyte proliferation-differentiation switch. Nat Genet. 2006 Nov;38(11):1329–34. 10.1038/ng1894. [DOI] [PubMed]
- [39].Gritli-Linde A. The etiopathogenesis of cleft lip and cleft palate: Usefulness and caveats of mouse models. Curr Top Dev Biol. 2008;84:37–138. 10.1016/S0070-2153(08)00602-9. [DOI] [PubMed]
- [40].Kondo S, Schutte BC, Richardson RJ, Bjork BC, Knight AS, Watanabe Y, et al. Mutations in IRF6 cause Van der Woude and popliteal pterygium syndromes. Nat Genet. 2002 Oct;32(2):285–9. 10.1038/ng985. [DOI] [PMC free article] [PubMed]
- [41].Huang Y, Wu J, Ma J, Beaty TH, Sull JW, Zhu L, et al. Association between IRF6 SNPs and oral clefts in West China. J Dent Res. 2009 Aug;88(8):715–8. 10.1177/0022034509341040. [DOI] [PMC free article] [PubMed]
- [42].Blanton SH, Cortez A, Stal S, Mulliken JB, Finnell RH, Hecht JT. Variation in IRF6 contributes to nonsyndromic cleft lip and palate. Am J Med Genet A. 2005 Sep 1;137A(3):259–62. 10.1002/ajmg.a.30887. [DOI] [PubMed]
- [43].Ghassibé M, Bayet B, Revencu N, Verellen-Dumoulin C, Gillerot Y, Vanwijck R, et al. Interferon regulatory factor-6: A gene predisposing to isolated cleft lip with or without cleft palate in the Belgian population. Eur J Hum Genet. 2005 Nov;13(11):1239–42. 10.1038/sj.ejhg.5201486. [DOI] [PubMed]
- [44].Scapoli L, Palmieri A, Martinelli M, Pezzetti F, Carinci P, Tognon M, et al. Strong evidence of linkage disequilibrium between polymorphisms at the IRF6 locus and nonsyndromic cleft lip with or without cleft palate, in an Italian population. Am J Hum Genet. 2005 Jan;76(1):180–3. 10.1086/427344. [DOI] [PMC free article] [PubMed]
- [45].Park JW, McIntosh I, Hetmanski JB, Jabs EW, Vander Kolk CA, Wu-Chou YH, et al. Association between IRF6 and nonsyndromic cleft lip with or without cleft palate in four populations. Genet Med. 2007 Apr;9(4):219–27. 10.1097/gim.0b013e3180423cca. [DOI] [PMC free article] [PubMed]
- [46].Paranaíba LM, Bufalino A, Martelli-Júnior H, de Barros LM, Graner E, Coletta RD. Lack of association between IRF6 polymorphisms (rs2235371 and rs642961) and non-syndromic cleft lip and/or palate in a Brazilian population. Oral Dis. 2010 Mar;16(2):193–7. 10.1111/j.1601-0825.2009.01627.x. [DOI] [PubMed]
- [47].Brito LA, Bassi CF, Masotti C, Malcher C, Rocha KM, Schlesinger D, et al. IRF6 is a risk factor for nonsyndromic cleft lip in the Brazilian population. Am J Med Genet A. 2012 Sep;158A(9):2170–5. 10.1002/ajmg.a.35526. [DOI] [PubMed]
- [48].Pan Y, Ma J, Zhang W, Du Y, Niu Y, Wang M, et al. IRF6 polymorphisms are associated with nonsyndromic orofacial clefts in a Chinese Han population. Am J Med Genet A. 2010 Oct;152A(10):2505–11. 10.1002/ajmg.a.33624. [DOI] [PubMed]
- [49].Mostowska A, Hozyasz KK, Wojcicki P, Biedziak B, Paradowska P, Jagodzinski PP. Association between genetic variants of reported candidate genes or regions and risk of cleft lip with or without cleft palate in the polish population. Birth Defects Res A Clin Mol Teratol. 2010 Jul;88(7):538–45. 10.1002/bdra.20687. [DOI] [PubMed]
- [50].Birnbaum S, Ludwig KU, Reutter H, Herms S, de Assis NA, Diaz-Lacava A, et al. IRF6 gene variants in central European patients with non-syndromic cleft lip with or without cleft palate. Eur J Oral Sci. 2009 Dec;117(6):766–9. 10.1111/j.1600-0722.2009.00680.x. [DOI] [PubMed]
- [51].Murdoch AM, Patir A, Seymen F, Vieira AR. Studies of palatine rugae and interferon regulatory factor 6 variations in a group of families with sporadic hypodontia. J Oral Sci. 2009 Dec;51(4):521–6. 10.2334/josnusd.51.521. [DOI] [PubMed]
- [52].Jugessur A, Rahimov F, Lie RT, Wilcox AJ, Gjessing HK, Nilsen RM, et al. Genetic variants in IRF6 and the risk of facial clefts: Single-marker and haplotype-based analyses in a population-based case-control study of facial clefts in Norway. Genet Epidemiol. 2008 Jul;32(5):413–24. 10.1002/gepi.20314. [DOI] [PMC free article] [PubMed]
- [53].Jia ZL, Li Y, Li L, Wu J, Zhu LY, Yang C, et al. Association among IRF6 polymorphism, environmental factors, and nonsyndromic orofacial clefts in Western China. DNA Cell Biol. 2009 May;28(5):249–57. 10.1089/dna.2008.0837. [DOI] [PubMed]
- [54].Sull JW, Liang KY, Hetmanski JB, Wu T, Fallin MD, Ingersoll RG, et al. Evidence that TGFA influences risk to cleft lip with/without cleft palate through unconventional genetic mechanisms. Hum Genet. 2009 Sep;126(3):385–94. 10.1007/s00439-009-0680-3. [DOI] [PMC free article] [PubMed]
- [55].Mostowska A, Hozyasz KK, Wojcicka K, Biedziak B, Jagodzinski PP. Polymorphic variants at 10q25.3 and 17q22 loci and the risk of non-syndromic cleft lip and palate in the Polish population. Birth Defects Res A Clin Mol Teratol. 2012 Jan;94(1):42–6. 10.1002/bdra.22862. [DOI] [PubMed]
- [56].Candotto V, Oberti L, Gabrione F, Greco G, Rossi D, Romano M et al. Current concepts on cleft lip and palate etiology. J Biol Regul Homeost Agents. 2019 May-Jun;33(3 Suppl. 1):145–51. [PubMed]


