Abstract
Background
In epidemics of highly infectious diseases, such as Ebola Virus Disease (EVD) or SARS, healthcare workers (HCW) are at much greater risk of infection than the general population, due to their contact with patients’ contaminated body fluids. Contact precautions by means of personal protective equipment (PPE) can reduce the risk. It is unclear which type of PPE protects best, what is the best way to remove PPE, and how to make sure HCWs use PPE as instructed.
Objectives
To evaluate which type or component of full-body PPE and which method of donning or removing (doffing) PPE have the least risk of self-contamination or infection for HCWs, and which training methods most increase compliance with PPE protocols.
Search methods
We searched MEDLINE (PubMed up to 8 January 2016), Cochrane Central Register of Trials (CENTRAL up to 20 January 2016), EMBASE (embase.com up to 8 January 2016), CINAHL (EBSCOhost up to 20 January 2016), and OSH-Update up to 8 January 2016. We also screened reference lists of included trials and relevant reviews, and contacted NGOs and manufacturers of PPE.
Selection criteria
We included all eligible controlled studies that compared the effect of types or components of PPE in HCWs exposed to highly infectious diseases with serious consequences, such as EVD and SARS, on the risk of infection, contamination, or noncompliance with protocols. This included studies that simulated contamination with fluorescent markers or a non-pathogenic virus.
We also included studies that compared the effect of various ways of donning or removing PPE, and the effects of various types of training in PPE use on the same outcomes.
Data collection and analysis
Two authors independently selected studies, extracted data and assessed risk of bias in included trials. We intended to perform meta-analyses but we did not find sufficiently similar studies to combine their results.
Main results
We included nine studies with 1200 participants evaluating ten interventions. Of these, eight trials simulated the exposure with a fluorescent marker or virus or bacteria containing fluids. Five studies evaluated different types of PPE against each other but two did not report sufficient data. Another two studies compared different types of donning and doffing and three studies evaluated the effect of different types of training.
None of the included studies reported a standardised classification of the protective properties against viral penetration of the PPE, and only one reported the brand of PPE used. None of the studies were conducted with HCWs exposed to EVD but in one study participants were exposed to SARS.
Different types of PPE versus each other
In simulation studies, contamination rates varied from 25% to 100% of participants for all types of PPE. In one study, PPE made of more breathable material did not lead to a statistically significantly different number of spots with contamination but did have greater user satisfaction (Mean Difference (MD) −0.46 (95% Confidence Interval (CI) −0.84 to −0.08, range 1 to 5, very low quality evidence). In another study, gowns protected better than aprons. In yet another study, the use of a powered air-purifying respirator protected better than a now outdated form of PPE. There were no studies on goggles versus face shields, on long-versus short-sleeved gloves, or on the use of taping PPE parts together.
Different methods of donning and doffing procedures versus each other
Two cross-over simulation studies (one RCT, one CCT) compared different methods for donning and doffing against each other. Double gloving led to less contamination compared to single gloving (Relative Risk (RR) 0.36; 95% CI 0.16 to 0.78, very low quality evidence) in one simulation study, but not to more noncompliance with guidance (RR 1.08; 95% CI 0.70 to 1.67, very low quality evidence). Following CDC recommendations for doffing led to less contamination in another study (very low quality evidence). There were no studies on the use of disinfectants while doffing.
Different types of training versus each other
In one study, the use of additional computer simulation led to less errors in doffing (MD −1.2, 95% CI −1.6 to −0.7) and in another study additional spoken instruction led to less errors (MD −0.9, 95% CI −1.4 to −0.4). One retrospective cohort study assessed the effect of active training - defined as face-to-face instruction - versus passive training - defined as folders or videos - on noncompliance with PPE use and on noncompliance with doffing guidance. Active training did not considerably reduce noncompliance in PPE use (Odds Ratio (OR) 0.63; 95% CI 0.31 to 1.30) but reduced noncompliance with doffing procedures (OR 0.45; 95% CI 0.21 to 0.98, very low quality evidence). There were no studies on how to retain the results of training in the long term or on resource use.
The quality of the evidence was very low for all comparisons because of high risk of bias in studies, indirectness of evidence, and small numbers of participants. This means that it is likely that the true effect can be substantially different from the one reported here.
Authors’ conclusions
We found very low quality evidence that more breathable types of PPE may not lead to more contamination, but may have greater user satisfaction. We also found very low quality evidence that double gloving and CDC doffing guidance appear to decrease the risk of contamination and that more active training in PPE use may reduce PPE and doffing errors more than passive training. However, the data all come from single studies with high risk of bias and we are uncertain about the estimates of effects.
We need simulation studies conducted with several dozens of participants, preferably using a non-pathogenic virus, to find out which type and combination of PPE protects best, and what is the best way to remove PPE. We also need randomised controlled studies of the effects of one type of training versus another to find out which training works best in the long term. HCWs exposed to highly infectious diseases should have their use of PPE registered and should be prospectively followed for their risk of infection.
Keywords: Body Fluids; Health Personnel; Personal Protective Equipment; Gloves, Protective; Hemorrhagic Fever; Ebola [transmission]; Infectious Disease Transmission; Patient-to-Professional [prevention & control]; Respiratory Protective Devices; Severe Acute Respiratory Syndrome [transmission]; Surgical Attire
PLAIN LANGUAGE SUMMARY
Clothes and equipment for healthcare staff to prevent Ebola and other highly infective diseases
Healthcare staff are at much greater risk of infections such as Ebola Virus Disease or SARS than people in general. One way of preventing infection is to use personal protective equipment, such as protective clothing, gloves, masks, and goggles to prevent contamination of the worker. It is unclear which type of equipment protects best and how it can best be removed after use. It is also unclear what is the best way to train workers to comply with guidance for this equipment.
Studies found
We found six studies with 295 participants in which workers’ protective clothing was sprayed with a fluorescent marker or a harmless virus to simulate what happens in hospitals. Four of these compared different types of protective clothing. Two studies compared different ways of putting clothing on and taking it off. Three studies with 905 participants compared the effect of active training on the use of protective equipment to passive training. All studies had a high risk of bias.
Various types of clothing compared
In spite of protective clothing, the marker was found on the skin of 25% to 100% of workers. In one study, more breathable clothing did not lead to more contamination than non-breathable clothing, but users were more satisfied. Gowns led to less contamination than aprons in another study. Two studies did not report enough data to enable conclusions. This evidence was of very low quality.
Various types of removal of clothing compared
In one study, two pairs of gloves led to less contamination than only one pair of gloves. The outer gloves were immediately removed after the task was finished. In another study, following CDC guidance for apron or gown removal led to less contamination. This evidence was also of very low quality.
Active training
Active training, including computer simulation and spoken instructions, led to less errors with guidance on which protection to use and how to remove it among healthcare staff compared to passive training.
Quality of the evidence
We judged the quality of the evidence to be very low because of limitations in the studies, indirectness and small numbers of participants.
What do we still need to find out?
There were no studies on the effects of goggles, face shields, long-sleeved gloves or taping on the risk of contamination. We need simulation studies with several dozens of participants, preferably using exposure to a harmless virus, to find out which type and combination is most protective. The best way to remove protective clothing after use is also unclear. We need studies that use chance to assign workers to different types of training to find out which training works best. Healthcare staff exposed to highly infectious diseases should have their protective equipment registered and be followed for their risk of infection. We urge WHO and NGOs to organise more studies.
SUMMARY OF FINDINGS
Summary of findings for the main comparison. Comparison 1: One type of PPE versus another – PAPR versus E-RCP attire
| PAPR versus E-RCP Attire for preventing contact with contaminated body fluids in healthcare staff | ||||||
|
Patient or population: healthcare staff volunteers Settings: simulation study Intervention: PPE with Powered Air Purifying Respirator (PAPR) Attire Control: Enhanced respiratory and contact precautions (E-RCP) attire according to 2005 CDC recommendation | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| E-RCP attire | PAPR Attire | |||||
|
Any contamination fluorescent marker Follow-up: post intervention |
960 per 1000 |
259 per 1000 (163 to 413) |
RR 0.27 (0.17 to 0.43) |
50 (1 cross-over RCT) |
⊕⊕⊝⊝ very low 1,2,3 |
Analyses presented in this table are unadjusted for the paired nature of the cross-over design but similar to the results that the authors presented while taking the cross-over into account |
| Compliance with guidance - Noncompliance with donning guidance Follow-up: post intervention |
40 per 1000 |
300 per 1000 (72 to 1000) |
RR 7.5 (1.81 to 31.1) |
50 (1 cross-over RCT) |
⊕⊕⊝⊝ very low 1,2,3 |
|
| Compliance with guidance - Noncompliance with doffing guidance Follow-up: post intervention |
240 per 1000 |
120 per 1000 (48 to 295) |
RR 0.5 (0.2 to 1.23) |
50 (1 cross-over RCT) |
⊕⊕⊝⊝ very low 1,2,3 |
|
| Infection with EVD | See comment | See comment | Not estimable | 0 (0 studies) |
See comment | No studies evaluated the effect of the interventions on infection rates. |
The basis for the assumed risk is the control group risk. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
CI: Confidence interval; RR: Risk ratio;
GRADE Working Group grades of evidence
High quality: Further research is very unlikely to change our confidence in the estimate of effect.
Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality: We are very uncertain about the estimate.
Simulation study, downgraded for indirectness
One cross-over study with 50 participants, downgraded for imprecision
HIgh risk of bias, downgraded for study limitations
Summary of findings 2. Comparison 1: One type of PPE versus another – Three types of PPE attire
| Three types of PPE attire compared by number of contaminated spots | |||||
|
Patient or population: healthcare worker volunteers Settings: simulation study Intervention: more protective attire, not permeable not breathable (A) Comparison: less protective attire: permeable but breathable (B); fairly permeable, not breathable (D) | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | ||||
| Less protective type of PPE (B or D) | Most protective type of PPE attire (A) | ||||
|
Number of contaminated spots - Neck fluorescent marker Follow-up: post intervention |
The mean number of contaminated spots i n control grou p B was 0.12 spots | The mean number of contaminated spots in the intervention group was 0.7 higher (0.26 lower to 1.66 higher) |
50 (1 study) |
⊕⊝⊝⊝ very low 1,2,3 |
|
|
Number of contaminated spots - Foot fluorescent marker Follow-up: post intervention |
The mean number of contaminated spots in the control group B was 2.86 spots | The mean number of contaminated spots in the intervention group was 0.96 lower (2.35 lower to 0.43 higher) |
50 (1 study) |
⊕⊝⊝⊝ very low 1,2,3 |
|
|
Number of contaminated spots - Palm fluorescent marker Follow-up: post intervention |
The mean number of contaminated spots in the control group B was 17.83 | The mean number of contaminated spots in the intervention group was 7.72 lower (15.65 lower to 0.21 higher) |
50 (1 study) |
⊕⊝⊝⊝ very low 1,2,3 |
|
|
Number of contaminated spots - Foot fluorescent marker Follow-up: post intervention |
The mean number of contaminated spots in the control group D was 4.96 | The mean number of contaminated spots in the intervention group was 4.1 lower (6.94 to 1.26 lower) |
50 (1 study) |
⊕⊝⊝⊝ very low 1,2,3 |
|
|
Number of contaminated spots - Palm fluorescent marker Follow-up: post intervention |
The mean number of contaminated spots in the control group D was 20.49 | The mean number of contaminated spots in the intervention group was 12.76 lower (21.62 to 3.9 lower) |
50 (1 study) |
⊕⊝⊝⊝ very low 1,2,3 |
|
| Infection with EVD | See comment | See comment | 0 (0 studies) |
See comment | No studies evaluated the effect of the interventions on infection rates. |
| Compliance with guidance | See comment | See comment | 0 (0 studies) |
See comment | No studies evaluated the effect of the interventions on compliance with guidance. |
The basis for the assumed risk is the control group risk. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group.
CI: Confidence interval;
GRADE Working Group grades of evidence
High quality: Further research is very unlikely to change our confidence in the estimate of effect.
Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality: We are very uncertain about the estimate.
Simulation study, downgraded for indirectness
One study 100 participants, 25 participants per arm, downgraded for imprecision
Unclear risk of bias in the study, downgraded one level
Summary of findings 3. Comparison 1: One type of PPE versus another – Gowns versus aprons
| Gowns versus aprons for preventing highly infectious diseases due to contact with contaminated body fluids in healthcare staff | |||||
|
Patient or population: healthcare worker volunteers Settings: simulation study Intervention: gowns versus aprons | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | ||||
| Aprons | Gowns | ||||
|
Contamination with marker; individual type of doffing Follow-up: post intervention |
The mean contamination with marker in the control groups was 16.98 small spots | The mean contamination with marker in the intervention groups was 10.28 lower (14.77 to 5.79 lower) | 50 (1 study) |
⊕⊝⊝⊝ very low 1,2,3 |
Cross-over study; the analyses were unadjusted for the paired nature of the data but similar to the analysis of the authors who took this into account |
|
Contamination with marker; CDC recommended doffing Follow-up: post intervention |
The mean contamination with marker in the control groups was 1.88 small spots | The mean contamination with marker in the intervention groups was 0.62 lower (1.75 lower to 0.51 higher) | 50 (1 study) |
⊕⊝⊝⊝ very low 1,2,3 |
|
| Infection with EVD | See comment | See comment | 0 (0 studies) |
See comment | No studies evaluated the effect of the interventions on infection rates. |
| Compliance with guidance | See comment | See comment | 0 (0 studies) |
See comment | No studies evaluated the effect of the interventions on compliance with guidance. |
The basis for the assumed risk is the control group risk. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group.
CI: Confidence interval;
GRADE Working Group grades of evidence
High quality: Further research is very unlikely to change our confidence in the estimate of effect.
Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality: We are very uncertain about the estimate.
Randomisation method unclear, downgraded one level
Simulation study, downgraded for indirectness
Single cross-over study with 50 participants, downgraded for imprecision
Summary of findings 4. Comparison 2: One procedure for donning/doffing versus another – Doffing with double gloves compared to doffing with single gloves
| Doffing with double gloves compared to doffing with single gloves for preventing contact with contaminated body fluids in healthcare staff | ||||||
|
Patient or population: healthcare staff volunteers Settings: Simulation study Intervention: Doffing with double gloves Comparison: Doffing with single gloves | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Doffing with single gloves | Doffing with dubble gloves | |||||
|
Contamination: virus detected - All body parts Follow-up: post intervention |
778 per 1000 | 280 per 1000 (124 to 607) |
RR 0.36 (0.16 to 0.78) |
18 (1 cross-over study) |
⊕⊝⊝⊝ very low 1,2 |
Non-randomised cross-over study; the analyses were unadjusted for the paired nature of the data but the results are similar to those analysed taking into account the paired nature of the data |
| Compliance with guidance - Noncompliance: any error Follow-up: post intervention |
667 per 1000 | 720 per 1000 (467 to 1000) |
RR 1.08 (0.7 to 1.67) |
18 (1 cross-over study) |
⊕⊝⊝⊝ very low 1,2 |
|
| Infection with EVD | See comment | See comment | Not estimable | 0 (0 studies) |
See comment | No studies evaluated the effect of the interventions on infection rates. |
The basis for the assumed risk is the control group risk. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
CI: Confidence interval; RR: Risk ratio;
GRADE Working Group grades of evidence
High quality: Further research is very unlikely to change our confidence in the estimate of effect.
Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality: We are very uncertain about the estimate.
Similation study, downgraded one level
One cross over study with 18 participants, downgraded for imprecision
Summary of findings 5. Comparison 2: One procedure for donning/doffing versus another – CDC method versus individual doffing
| CDC method versus individual doffing for preventing contact with contaminated body fluids in healthcare staff | ||||||
|
Patient or population: healthcare staff volunteers Settings: simulation study Intervention: CDC method in doffing Control: Individual method of doffing | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Individual doffing method | CDC recommended doffing method | |||||
|
Contamination with fluor marker when using gowns Follow-up: post intervention |
The mean contamination with fluor marker in the control group was 6.7 small spots | The mean contamination with fluor marker in the intervention group was 5.44 lower (7.43 to 3.45 lower) |
50 (1 study) |
⊕⊝⊝⊝ very low 1,2,3 |
Cross-over study; the analyses were unadjusted for the paired nature of the data but similar to the analysis of the authors who took this into account | |
|
Contamination with fluor marker when using aprons Follow-up: post intervention |
The mean contamination with fluor marker in the control group was 16.98 small spots | The mean contamination with fluor marker in the intervention group was 15.1 lower (19.28 to 10.92 lower) |
50 (1 study) |
⊕⊝⊝⊝ very low 1,2,3 |
||
| Infection with EVD | See comment | See comment | 0 (0 studies) |
See comment | No studies evaluated the effect of the interventions on infection rates. | |
| Compliance with guidance | See comment | See comment | 0 (0 studies) |
See comment | No studies evaluated the effect of the interventions on compliance with guidance. | |
The basis for the assumed risk is the control group risk. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group.
CI: Confidence interval;
GRADE Working Group grades of evidence
High quality: Further research is very unlikely to change our confidence in the estimate of effect.
Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality:We are very uncertain about the estimate.
Randomisation procedure unclear, downgraded one level
Simulation study, downgraded for indirectness
One cross-over study with 50 participants
BACKGROUND
Description of the condition
Over 59 million people are employed in the healthcare sector worldwide (WHO 2006). Some of these healthcare workers (HCWs) are at risk of developing life-threatening infectious diseases due to contact with patients’ blood or body fluids such as mucus or vomit. The risk of infection and its consequences vary, but the 2013 to 2015 Ebola Virus Disease (EVD) epidemic put healthcare workers at high risk of a disease with a very high fatality rate in the epidemic areas (Ebola 2014). Not only nurses and doctors are at risk, but also staff engaged in transportation, cleaning and burial of patients. Healthcare workers can also be at risk when seeing patients arriving from the epidemic areas (Forrester 2014). Due to the high risk of infection and the high fatality rate, hundreds of HCWs died in the epidemic areas (Kilmarx 2014). According to the most recent statistics from October 2015, there were 1049 registered cases of HCWs infected with 535 deaths (WHO 2015). Just a decade earlier, healthcare workers lost their lives due to the Severe Acute Respiratory Syndrome (SARS) epidemic (CDC 2003). Even though the transmission routes are different, EVD and SARS are both highly infectious and they can have fatal consequences and especially affect healthcare workers.
Healthcare workers can get infected through various routes of transmission, depending on the pathogen. Infection can occur through splashes and droplets of contaminated body fluids on non-intact skin, or via needle-stick injuries through intact skin. Infection can also occur when splashes or droplets of contaminated body fluids land on the mucous membranes in the eyes, mouth or nose, or when the same mucous membranes come into contact with contaminated skin, such as when rubbing the eyes with a hand carrying pathogens after shaking hands with a patient. For EVD, this is the main route of transmission, even though there is doubt about the transmission of virus particles through aerosols, or while performing patient care. For SARS, the highest risk of infection was due to inhalation of aerosols, but the disease was also transmitted through droplet infection. Another risk of HCW infection is that infected HCWs will infect patients or that they will act as a vector for the transfer of the disease between patients.
Here, we focus on highly infectious diseases which means that contamination with a small amount of infectious material can already lead to clinical disease. We also focus on those infections that have serious consequences such as a high case fatality rate because this has implications for the motivation of HCWs to protect oneself.
Description of the intervention
Exposure can be best controlled by organisational measures that minimise the exposure to contaminated body fluids or infected patients. One part of this comprehensive prevention strategy is that HCWs use proper personal protective equipment. The most important preventive measure is the proper organization of the hospital or health care unit to avoid unnecessary contact. Once this has been implemented, the main strategy for reducing physical exposure to highly infectious diseases is through personal protective equipment (PPE). Coveralls, gowns, hoods, masks, eye shields, and respirators, among others, are used to prevent skin and mucous membranes from becoming contaminated.
Personal protective equipment will only be effective if the equipment can form a barrier between the HCW and the exposure to contaminated body fluids. Therefore, standards have been developed that, once complied with, assure that PPE is of sufficient quality to protect against biohazards (Mäkelä 2014; NIOSH 2014). Even though the biohazard symbol (Figure 1) is widely used to indicate the presence of biohazards, it is not a label for protective clothing. For biohazards, these standards are based on laboratory tests that evaluate to what extent the fabric and the seams of protective clothing are leak-tight, that is, they are impermeable for liquids, viruses, or both at certain pressure levels. The standards in Europe and the US are different. Personal protective equipment should contain a label that specifically indicates the standards against which it has been tested.
Figure 1. International symbol indicating biohazards.
In Europe, there is standard EN 14126 for clothing, specifically coveralls that protect workers against biological hazards from microorganisms. Clothing compliant with the standard EN 14126 is classified with the same six clothing types as chemical protective clothing. Type one provides the most protection by complete encapsulation. Type three clothing protects against pressurised liquid splashes, but is also very leak-tight, which makes it heavy to work in. Type four provides protection against non-pressurised liquid splashes, and is more breathable. There is no requirement for the type of clothing, whether it be a coverall or a gown. In addition, the clothing material should be classified according to the ISO 16604 test against viral penetration. Again, materials can pass the test at six levels. Class six is the most protective, and indicates that the test bacteriophage particles do not pass through the fabric at a hydrostatic pressure of 20 kPa (2.9 psi), but for Class one, the fabric is protective only at a pressure of 0 kPa. There is a separate standard for surgical gowns, EN 13795, which is designed to protect the patient.
In the US, there is standard ANSI/AAMI PB70 2012 for surgical and isolation gowns to protect both patients and healthcare workers from becoming infected. The standard specifies four levels of protection, with the highest, level four, being tested for viral protection at a pressure of 2 psi. Level one is tested for water resistance, with less than 4.5 grams of water allowed to be absorbed during the test. There is also US standard NFPA 1999 for protective coveralls, which was specifically developed to address a range of different clothing items worn by emergency medical service first responders, and also applies to medical first receivers. NFPA 1999 lists many performance requirements for garments used by emergency medical personnel, including (but not limited to) viral penetration resistance, tensile strength, liquid integrity, and seam strength.
Thus, the qualities of garments certified by different standards are not fully comparable. Nonetheless they all aim to ensure that garments are of a quality that prohibits water and blood-like fluids with virus particles, applied under a specified amount of pressure, to pass through. In addition, some standards have requirements that the whole garment, including the seams, must be non-permeable to liquids (NFPA 1999).
For gowns to be used with EVD, WHO 2014 currently recommends EN 13795 high performance surgical gowns or ANSI/AAMI PB70 2012 level three (option one), level four (option two), or equivalent. As the first option for coveralls, WHO currently recommends protection equivalent to EN 14126, with clothing material that provides Class three protection against blood at 0.5 kPa, based on ISO 16603 (ISO 2004a), and Class two against viruses at a pressure of 1.75 kPa, based on ISO 16604 (ISO 2004).
Both in the EU and in the US, it is mandatory for employers to protect their workers against blood-borne pathogens and other infections at work (EU 2010; OSHA 2012).
Clothing that is manufactured according to the standards mentioned above is impermeable to body fluids and viruses and will technically prevent skin contamination. However, this review does not deal with the technical physical standards of equipment, but rather if its use in practice will prevent contamination and infection.
There are several guidelines available for choosing proper PPE (Australian NHMRC 2010; CDC 2014; ECDC 2014; WHO 2014). Even though all guidelines propose using similar protective clothing, there are also noticeable differences. In 2014, guidelines differed widely. For example, WHO 2014 proposed double gloving only when carrying out strenuous tasks, or when in contact with body fluids whereas the other guidelines proposed always using double gloves. ECDC 2014 proposed taping gloves, boot covers and goggles onto the coveralls to prevent leaving any openings but the other guidelines did not recommend this. By March 2015, most guidelines had been updated and are now more in line with each other. However, differences still exist. WHO 2014 does not recommend taping, but ECDC 2014 does.
Overprotection can be a problem. Some propose using three layers of gloves, because according to their experience, this is best practice (Lowe 2014). However, it may make work more difficult, and eventually lead to an increased rather than a decreased risk of infection, especially during doffing (i.e. removing the PPE). For example, the combined use of several respirators probably does not lead to more protection, but considerably increases the burden on the worker (Roberge 2008; Roberge 2008a).
In spite of using proper PPE, probably the biggest risk of infection is associated with self-contamination by HCWs inappropriately removing the PPE (Fischer 2014). Some types of PPE make donning and doffing more difficult, thereby increasing the risk of contamination (Zamora 2006). The highest risk time of doffing is usually managed by an assistant, who guides the worker through the process while watching for breaches, and spraying chlorine as each item is removed. There is evidence that when doffing PPE, the use of a double pair of gloves decreases the risk of contamination (Casanova 2012). How contamination of PPE occurs has also been clearly illustrated with a simulation study about cleaning up vomit (Makison 2014). The results of such simulation studies should increase HCWs’ confidence in executing the donning and doffing procedures correctly, and thus can also be an incentive for their uptake and compliance with the guidelines. Therefore, specific guidance has been developed for donning and doffing PPE (CDC 2014; WHO 2014).
Compliance with guidance on correct PPE use in health care is historically poor. HCWs sometimes distrust infection control, and using PPE is stressful (Zelnick 2013). For respiratory protection such as masks and respirators, compliance has been reported to be around 50% on many occasions (Nichol 2008). Due to lack of proper fitting and incorrect use, real field conditions almost never match laboratory standards (Coia 2013; Howie 2005). Also, reports of hand hygiene show that there is still large room for improvement and guidelines recommend education and training in combination with other implementation measures (WHO 2009). From reports of HCWs, it is clear that most appropriate PPE is not user-friendly in tropical conditions. It prevents heat loss through sweating because it is not made of breathable material. A common reason for a breach in the barrier of the PPE is the worker sweating and then instinctively wiping their face (Cherry 2006). Staff are being trained on arrival to the epidemic or treatment site by repeatedly practicing donning and doffing PPE and running through drills of what they should do if the protocol is breached while in the “red zone” (i.e. the Ebola patient area, also called hot zone).
In this review, we only concentrated on PPE for highly infectious diseases that have serious consequences for health, such as EVD. We excluded other highly infectious, but less serious viral infections, such as norovirus, as we expected the effect of PPE to be different. We included SARS as it was highly infectious to HCWs, sometimes fatal, and had similar recommendations on PPE use and training as EVD.
We did not specifically study the effects of hand hygiene or of respiratory protection. Hand hygiene is also crucial in preventing skin contamination, but this has already been covered in another review (Gould 2010). The protective effect of different types of respiratory protection, and effects of interventions to increase their uptake are covered in two other reviews (Jefferson 2011; Sakunkoo 2012).
How the intervention might work
First, HCWs, their supervisors, or occupational health professionals should choose the proper type of PPE, as indicated in the guidance described above. Then, a HCW needs to know how to don and doff PPE according to the guidelines provided. Next, a HCW needs to comply with established procedures for correctly using, donning and doffing PPE. Education and training is used to increase compliance. The emphasis in teaching correct use of PPE is on doing everything slowly and carefully to minimise the risk of making a mistake. Often an assistant or buddy, sometimes coupled with a mirror, is used while donning PPE, while a hygienist supervises doffing.
Compliance can be increased by personal supervision and instruction, checklists, audits of performance, by providing feedback, and by allowing sufficient time for donning and doffing. Education and training on uptake and compliance with PPE should have an effect in both the short term and the long term (Northington 2007; Ward 2011). Education and training can be seen as one method to increase compliance (Gershon 2009; Hon 2008). Compliance with PPE can also be improved by providing sufficient, comfortable, well-fitting, and more user- and patient-friendly PPE. Compliance with guidelines has been studied for hand hygiene. There is some evidence that multifaceted interventions and staff involvement are important, but altogether, there is little evidence that allows firm conclusions (Gould 2010).
Why it is important to do this review
There is still uncertainty about the optimal type, composition, amount, and way of using full-body PPE to prevent skin and mucous membrane contamination of HCWs, while treating patients infected with highly infectious diseases. This is also reflected in the different ways guidelines for PPE are implemented in Europe (De Iaco 2012), and acknowledged in current WHO guidelines (WHO 2014).
Since full-body protective suits have mainly evolved as a direct result of experiences gained from the recent outbreaks of deadly viruses, there are still many types available with varying types of components. The comparative effectiveness of one type against another is still unknown. Recent cases of HCWs becoming infected, despite wearing seemingly appropriate PPE when treating EVD patients, have raised the question of what really works and what does not when using a full-body protective suit. There are ongoing debates about types of PPE, with individuals from various nations and roles having different opinions. Factors to consider when choosing PPE for a healthcare facility may include: availability of supply, because large numbers of disposable suits will be used; standardisation of equipment, which will avoid mistakes; worker preferences (e.g. goggles steam up, which could be avoided by visors); and costs of making equipment affordable for low income countries.
We have learned from those who have faced the Ebola epidemic that breaches in PPE use are common. One possible explanation for this could be the lack of a common language between HCWs representing international aid organisations and local staff. Another explanation is the often poor literacy of local staff. This means that checklists are often unhelpful for training and implementation of PPE. Yet another problem with PPE is that HCWs walking around residential areas wearing what might be described as “astronaut suits” can be scary and may impact on community engagement and service avoidance.
HCWs working with Ebola patients and occupational health professionals still have uncertainty about which types of equipment to choose, the best procedures for doffing and how to deal with breaches of the barrier of the PPE, and with gross contamination.
Regarding the equipment, there is uncertainty if visors protect as well as goggles, especially when goggles are combined with a hood. It is not immediately obvious if the strap of the goggles should go over or under the hood. There is uncertainty if triple or quadruple gloves would be more protective than double gloves. Regarding suits, it is unclear if gowns are as protective as coveralls, and how breathable and impermeable for liquids or viruses they should be. Some argue that using more breathable material would decrease the risk of contamination (Kuklane 2015).
When it comes to donning and doffing procedures, there is uncertainty about the effect of integrity checks of gloves and other equipment, and if gloves should be changed when highly contaminated. With doffing especially, it is unclear if this should be done in pairs with a helper buddy removing part of the PPE, or if this can be done alone or in pairs. Another element of the doffing procedure that is uncertain is if spraying with a disinfectant chlorine spray is more protective than not using spray. It is not clear which disinfectant is the best anti-viral: chlorine solution or alcohol gel, and at which concentration.
The complexity of the drill and the procedures for updating skills, retraining, and responding to individual training needs after a potential or realised breach are also important.
OBJECTIVES
To summarise and critically appraise current evidence of the effectiveness of PPE for preventing nosocomial infection in healthcare staff exposed to body fluids contaminated with viral haemorrhagic fevers such as EVD, Lassa, Marburg, Congo-Crimean Haemorrhagic Fever, or comparable highly infectious diseases with serious consequences, such as SARS. In particular, we addressed questions identified from the West Africa EVD epidemic, that include the evaluation of the effect of:
one type or component of PPE as part of full-body protection PPE versus another on contamination and infection rates;
one procedure in donning and doffing full-body PPE versus another on contamination and infection rates; and
one intervention to improve compliance with guidelines for full-body PPE, including education and training, versus another on compliance, contamination and infection rates.
METHODS
Criteria for considering studies for this review
Types of studies
Since the circumstances for evaluation studies are difficult during epidemics, we anticipated including a broad range of study designs.
We included simulation studies of different full-body PPE types for donning and doffing procedures that use marker chemicals that make contamination visible. We included any study that compared different types of PPE or different procedures of donning and doffing, or different types of education and training.
We included field studies that compared outcomes between hospitals or treatment centres that used different types of PPE, different procedures, or different types of education and training. These studies were observational and retrospective, and measured infection rates and compliance rates. This included cohort studies, defined as studies that followed HCWs over time and compared the effect of PPE, procedures, or training on infection or compliance rates. This also included case-control studies that compared PPE, procedures, or training retrospectively between cases that had become infected and comparable controls that did not get infected. We also included randomised controlled trials that compared different types of PPE, procedures, or training.
We intended to also include uncontrolled audit reports or case reports of PPE failure for descriptive purposes, but we did not find any. If we find any such reports in future updates of this review, we will not use them for drawing conclusions, but only to compare with findings produced by the above study types.
Types of participants
For simulation studies, we included participants using PPE designed for EVD or comparable highly infectious diseases with serious consequences.
For field studies, we included studies conducted with HCWs and ancillary staff exposed to body fluids in the form of splashes, droplets or aerosols contaminated with particles of highly infectious diseases that have serious consequences for health such as EVD or SARS. We excluded studies conducted with laboratory staff because there preventive measures would be more detailed and easier to comply with.
Types of interventions
-
We included studies that evaluated the effectiveness of different types of whole-body protection, comparing different types, compositions, or amounts of the following:
- body protection such as gowns, coveralls or hazmat suits;
- eye and face protection such as glasses, goggles, face shields or visors, or masks or hoods that cover the entire head;
- hand protection: gloves; and
- foot protection: overshoes or boots.
We defined PPE as any of the above equipment designed or intended to protect healthcare staff from contamination with infected patients’ body fluids.
We especially sought to include studies that had compared the use of gowns with coveralls, different types of fabrics, such as less breathable fabrics with more breathable fabrics, goggles versus visors, various forms of hoods in combination with goggles, single versus multiple layers of gloves, and taping versus no taping of separate elements of PPE.
-
We included studies that evaluated the effectiveness of different procedures for donning and doffing of the PPE.
We especially sought to include studies that had compared a single person or two person procedure, procedures with and without spraying disinfectants, procedures for changing gloves or PPE after gross contamination or breach of barrier protection versus no change.
- We included any intervention to increase compliance with guidance for selection and proper use of PPE, including but not limited to:
- education,
- training,
- supervision during donning and doffing,
- information only such as posters, guideline leaflets, etc.,
- audit and feedback, or
- monetary or organisational incentives.
Types of outcome measures
Primary outcomes
We included all studies that had measured the effectiveness of interventions as:
contamination of skin or clothing, measured with any type of test material to visualise contamination (e.g. stains made visible with UV-light);
infection with EVD, another viral haemorraghic fever, or comparable highly infectious disease with serious consequences such as SARS; or
compliance with guidance on selection of type and use of PPE measured, for example, with an observation checklist.
Secondary outcomes
User-reported assessment of comfort and convenience
Costs or resource use
Time to don and doff the PPE
For future updates of this review we will also look for other outcomes that appear relevant to the questions being addressed.
Search methods for identification of studies
Electronic searches
We conducted a systematic literature search to identify all published and unpublished trials that could be considered eligible for inclusion in this review. We adapted the search strategy we developed for PubMed (see Appendix 1) for use in the other electronic databases. The literature search identified potential studies in all languages. We asked native speakers to assess the papers in Russian (AP) and in Chinese (CCC) for potential inclusion in the review.
We searched the following electronic databases from inception to present for identifying potential studies:
Cochrane Central Register of Controlled Trials (CENTRAL) (Wiley Online Library) until 20 January 2016;
MEDLINE (PubMed) (Appendix 1) until 8 January 2016;
EMBASE (embase.com) to 8 January 2016;
CINAHL (EBSCOhost) to 20 January 2016;
NIOSHTIC (OSH-UPDATE) to 8 January 2016;
NIOSHTIC-2 (OSH-UPDATE) to 8 January 2016;
HSELINE (OSH-UPDATE) to 8 January 2016;
CISDOC (OSH-UPDATE) to 8 January 2016;
We also conducted a search of ClinicalTrials.gov (www.ClinicalTrials.gov) and the WHO trials portal (www.who.int/ictrp/en/) which includes the Pan African Registry for potential studies on EVD. We searched all databases from their inception to the present and we did not impose a restriction on language of publication.
Searching other resources
We checked reference lists of all primary studies and reviewed articles for additional references. We contacted non-governmental organisations involved in medical relief operations in the high risk EVD areas to identify additional unpublished materials:
Médécins Sans Frontières (MSF)
Save the Children
We also used Twitter to ask for unpublished reports from people in the field. Evidence Aid helped in locating relevant organisations and asking them for unpublished reports.
We further contacted the following manufacturers of PPE to request unpublished studies:
DuPont
3M
Alpha Pro Tech
Data collection and analysis
Selection of studies
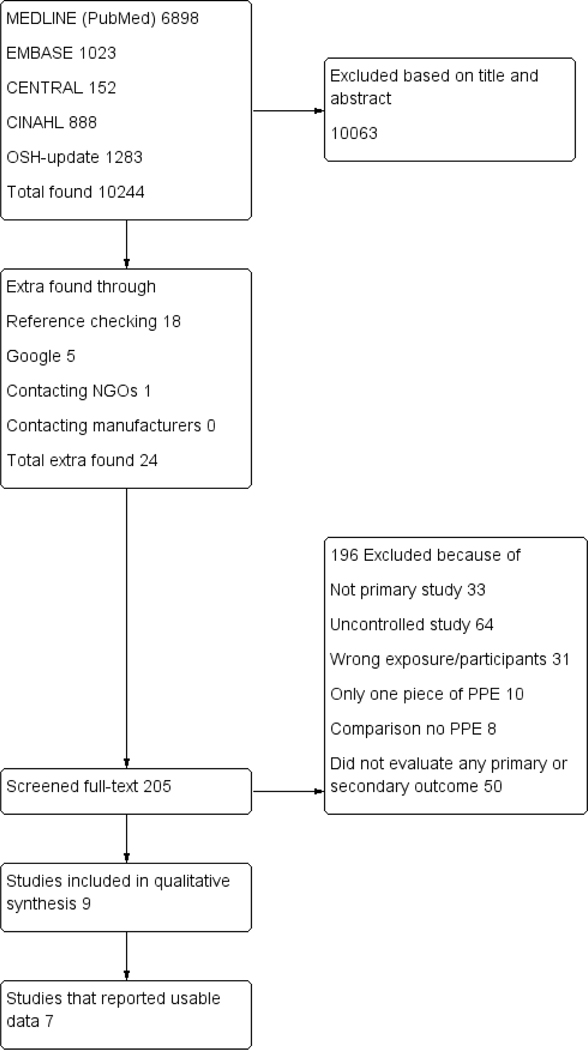
Pairs of two review authors (JV, CM, SI, JR, KN and RS) independently screened titles and abstracts of all the potential studies that we identified with our systematic search, to identify studies for inclusion. The same authors coded them as ‘retrieve’ (eligible or potentially eligible/unclear) or ‘do not retrieve’. We retrieved the full-text study reports/publication and pairs of two review authors (JV, CM, SI, JR, KN and RS) independently screened the full-text and identified studies for inclusion, and identified and recorded reasons for exclusion of the ineligible studies. We used the computer programme Covidence for the selection of references and full-text studies. We resolved any disagreement through discussion so there was no need to consult a third review author. We identified and excluded duplicates and collated multiple reports of the same study so that each study rather than each report is the unit of interest in the review. We recorded the selection process in sufficient detail and completed a PRISMA flow diagram (see Figure 2) and a ‘Characteristics of excluded studies’ table.
Figure 2. PRISMA study flow diagram.
Data extraction and management
We used a data collection form for study characteristics and outcome data which had been piloted on one included study. Two review authors (JV, CM, JR, SI, ME, KN, RS) independently extracted the following study characteristics from included studies:
Methods: study design, total duration of study, study location, study setting, withdrawals, and date of study.
Participants: N, mean age or age range, gender, severity of condition, diagnostic criteria if applicable, inclusion criteria, and exclusion criteria.
Interventions: description of intervention, comparison, duration, intensity, content of both intervention and control condition, and co-interventions.
Outcomes: description of primary and secondary outcomes specified and collected, and at which time points reported.
Notes: funding for trial, and notable conflicts of interest of trial authors, country where trial was conducted.
Pairs of two review authors (JV, CM, SI, JR, KN, ME, RS) independently extracted outcome data from included studies. We noted in the ‘Characteristics of included studies’ table if outcome data were not reported in a usable way. We resolved disagreements by consensus so there was no need to involve a third review author. One review author (JV) transferred the data into Review Manager (RevMan 2014). We double-checked that data were entered correctly by comparing the data presented in the systematic review with the study reports. A second review author (CM) spot-checked study characteristics for accuracy against the trial report.
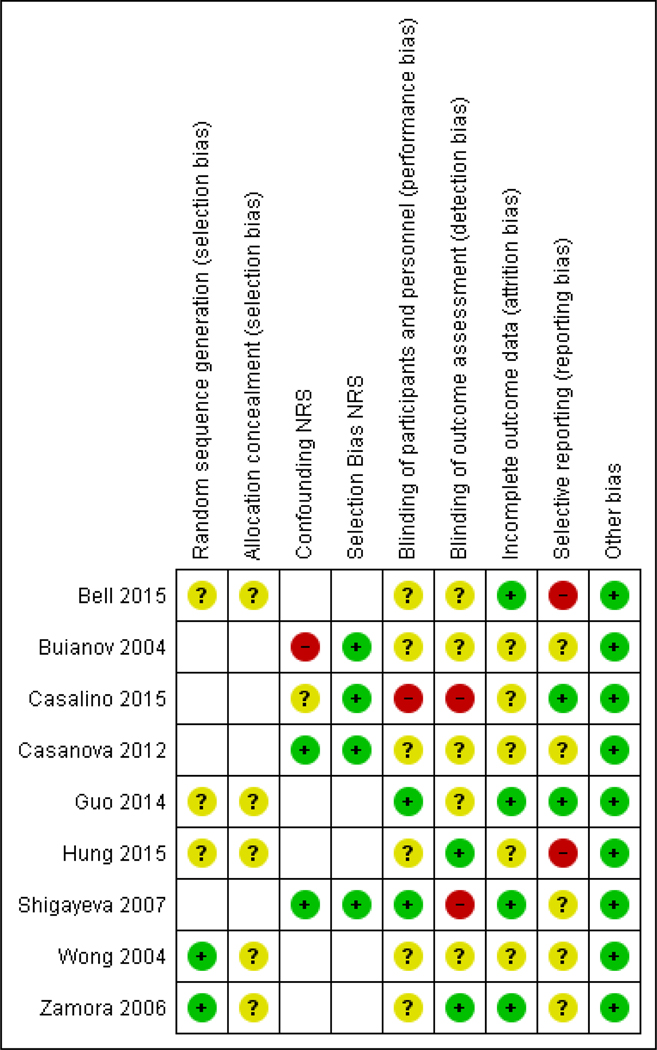
Assessment of risk of bias in included studies
Pairs of two review authors (JV, CM, SI, JR, KN, ME, RS) independently assessed risk of bias for each randomised study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved any disagreements by discussion so there was no need to involve another author. We assessed the risk of bias according to the following domains in all randomised controlled trials.
Random sequence generation,
Allocation concealment,
Blinding of participants and personnel,
Blinding of outcome assessment,
Incomplete outcome data,
Selective outcome reporting, and
Other bias
We rated each potential source of bias as high, low or unclear and provided a quote from the study report or author together with a justification for our judgment in the ‘Risk of bias’ table. We summarised the risk of bias judgements across different studies for each of the domains listed. For compliance, we considered blinding to PPE type significant for the outcome assessor only. Where information on risk of bias relates to unpublished data or correspondence with a trial author, we noted this in the ‘Risk of bias’ table.
We considered randomised studies to have a low overall risk of bias when we judged random sequence generation and blinded outcome assessment to have a low risk of bias and none of the other domains to have a high risk of bias.
We used domains three to seven listed above for all non-randomised studies. Instead of the domains one and two - random sequence generation and allocation concealment - we used the following items as suggested in the Cochrane Acrobat tool for the assessment of risk of bias in non-randomised intervention studies:
- Bias due to confounding. We made an overall assessment of risk of bias based on the following questions if the signalling question “Is confounding of the effect of intervention unlikely in this study?” was answered with no.
- Did the authors use an appropriate analysis method that adjusted for all the critically important confounding domains?
- Were confounding domains that were adjusted for measured validly and reliably by the variables available in this study? For this review question, we considered baseline differences between compared groups in the following factors significant: prior experience with PPE, healthcare qualification or education of HCWs, age and sex, ambient temperatures, and stressful activities.
- Bias due to selection of participants into the study. We made an overall assessment of this risk of bias based on the following questions if the signalling questions “Was selection into the study unrelated to intervention or unrelated to outcome?” and “Do start of follow-up and start of intervention coincide for most subjects?” were answered with no.
- Were adjustment techniques used that are likely to correct for the presence of selection biases?
- For case-control studies: Were the controls sampled from the population that gave rise to the cases, or using another method that avoids selection bias?
We considered the domains of confounding and selection of participants to yield high, low or unclear risk of bias. For a non-randomised study as a whole, we considered the study to have a low risk of bias if all domains received a judgment of low risk of bias comparable to an RCT. This means receiving a low risk of bias judgment on the two domains listed above as well as domains three to seven in the previous section.
When considering treatment effects, we took into account the risk of bias for the studies that contributed to that outcome.
Assesment of bias in conducting the systematic review
We conducted the review according to the published protocol and where there were deviations from it, we reported these in the ‘Differences between protocol and review’ section of the systematic review.
DIFFERENCES BETWEEN PROTOCOL AND REVIEW.
We changed the title from “Personal protective equipment for preventing highly infectious diseases due to contact with contaminated body fluids in health care staff” to “Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff” to avoid confusion with the term “contact precautions”.
We replaced the statement in the methods section: “We will also include audit reports or case reports of PPE failure in which there are no comparisons. We will not use these for drawing conclusions but only to compare with findings produced by the above study types. For audit reports, we will examine any reports of failed PPE or audits of health care staff being infected or contaminated” with “We intended to also include uncontrolled audit reports or case reports of PPE failure for descriptive purposes, but we did not find any. If we find any such reports in future updates of this review, we will not use them for drawing conclusions, but only to compare with findings produced by the above study types”.
We added the following definition of PPE in the methods section because it was lacking: “We defined PPE as any of the above equipment designed or intended to protect health care staff from contamination with body fluids”.
We added an extra outcome “Time to don and doff the PPE” because we stated in our protocol that we would add outcomes that we had not defined in advance and that we considered important.
We added a more detailed description of the specific resources that we searched in addition to the electronic databases, i.e. the specific non-governmental organisations (MSF and Save the Children), and specific manufacturers (DuPont, 3M, and Alpha Pro Tech). We could not foresee in advance which parties we would be contacting.
When using the GRADE considerations to assess the quality of the evidence, for non-randomised studies, we started at the ‘low-quality’ level, rather than the ‘moderate-quality’ level outlined in the protocol, as per the recommendations of the Cochrane Handbook.
Measures of treatment effect
We entered the outcome data for each study into the data tables in RevMan 2014 to calculate the treatment effects. We used risk ratios (RRs) for dichotomous outcomes, and mean differences (MDs) or standardised mean differences (SMDs) for continuous outcomes. When only effect estimates and their 95% confidence intervals or standard errors were reported in studies, we entered these data into RevMan 2014 using the generic inverse variance method. When authors used multivariate analyses, we used the most adjusted OR (Odds Ratios) or RRs. We ensured that higher scores for continuous outcomes had the same meaning for the particular outcome, explained the direction and reported where the directions were reversed, if this was necessary. If in future updates of this review we come across studies reporting results that we cannot enter in either way, we will describe them in the ‘Characteristics of included studies’ table, or we will enter the data into Additional tables. For cohort studies that compare an exposed to a non-exposed population we intended to report both the RR for the intervention versus the control at baseline and at follow-up for dichotomous outcomes to indicate the change brought about by the intervention but we did not find any such studies.
Unit of analysis issues
If in future updates of this review we come across studies that employ a cluster-randomised design and that report sufficient data to be included in the meta-analysis but do not make an allowance for the design effect, we will calculate the design effect based on a fairly large assumed intra-cluster correlation of 0.10. We based this assumption of 0.10 being a realistic estimate by analogy on studies about implementation research (Campbell 2001). We will follow the methods stated in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) for the calculations.
We intended to take the paired nature of the cross-over design in the included studies into account in our data analysis. However, the included studies did not present suffidient data to do so and the results presented here are based on the unpaired test that is implemented in RevMan 2014 which resulted in wider confidence intervals than with the use of a paired t-test.
Dealing with missing data
We contacted investigators in order to verify key study characteristics and obtain missing numerical outcome data where possible (e.g. when a study was identified as abstract only). If in future updates of this review we come across studies where this is not possible, and the missing data are thought to introduce serious bias, we will explore the impact of including such studies in the overall assessment of results by a sensitivity analysis.
Similarly, If in future updates of this review we come across studies where numerical outcome data are missing, such as SDs or correlation coefficients and they cannot be obtained from the authors, we will calculate them from other available statistics such as P values, according to the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Assessment of heterogeneity
We assessed the clinical homogeneity of the results of included studies based on similarity of population, intervention, outcome and follow-up. We considered populations as similar when they were HCWs directly engaged in patient treatment (nurses, doctors, paramedics) versus those who were not involved in patient therapy directly (cleaning and transport staff).
We considered interventions as similar when they fell into one of the intervention categories as stated in Types of interventions.
We considered any assessment of contamination of the skin or mucous membranes as similar enough to combine.
We considered the following follow-up times as similar: from immediately following a procedure up until the end of the work shift (short term), and any time after the incubation time (long-term).
We used the I2 statistic to measure heterogeneity among the trials in each analysis. Where we identified substantial heterogeneity, we reported it and explored possible causes by prespecified subgroup analysis. We regarded an I2 value above 50% as substantial heterogeneity.
We made a distinction between any kind of protection and protection that had been certified based on testing for biological hazards like CEN (European Committee for Standardization) or comparable standards.
Data synthesis
We pooled data from studies we judged to be clinically homogeneous using Review Manager 5.3 software (RevMan 2014). Where more than one study provided usable data in any single comparison, we performed a meta-analysis. We used a random-effects model when I2 was above 40%; otherwise we used a fixed-effect model. Where I2 was higher than 75% we did not pool results of studies in meta-analyses. We included a 95% confidence interval (CI) for all estimates.
If in future updates of this review, we come across studies with skewed data reported as medians and interquartile ranges, we will simply describe the data.
If in future updates of this review, we come across studies reporting multiple trial arms in a single trial, we will include only the relevant arms. If we need to combine two comparisons in the same meta-analysis, we will halve the control group to avoid double-counting.
Summary of findings table
We created a series of ‘Summary of findings’ tables to present the primary outcomes for Comparison 1 (One type of PPE versus another) and Comparison 2 (One procedure for donning/doffing versus another) only, as we felt these findings were the most useful to present as Summary of Findings tables. We used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of a body of evidence as it related to the studies that contributed data to the meta-analyses for the prespecified outcomes. We used methods and recommendations described in Section 8.5 and Chapter 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), using GRADEpro software (GRADEpro 2008). We justified all decisions to down-or upgrade the quality of studies using footnotes and we made comments to aid reader’s understanding of the review where necessary. For non-randomised studies, we started at the low-quality level and for randomised studies at a high-quality level. For future updates of this review, if the outcomes are measured in many different ways, we will prioritise the reporting of outcomes as follows: infection rates, contamination rates, compliance rates.
Subgroup analysis and investigation of heterogeneity
If future updates of this review find a sufficient number of studies, we will carry out the following subgroup analyses: high income versus low and middle income countries. We will also use our primary outcomes in subgroup analyses, and we will use the X2 test, as implemented in RevMan 2014, to test for subgroup interactions. At this time, we did not identify enough studies to allow for such a subgroup analysis.
Sensitivity analysis
If future updates of this review find a sufficient number of studies, we will perform sensitivity analyses defined a priori to assess the robustness of our conclusions. This involves including only studies we judge to have a low risk of bias. At this time we did not identify enough studies to allow such a sensitivity analysis. However, we did check if using a fixed-effect model instead of a random-effects model had an influence on our conclusions when heterogeneity was between 10% and 50%.
Reaching conclusions
We based our conclusions only on findings from the quantitative or narrative synthesis of included studies we judged to have the lowest risk of bias. Consequently, we used findings from non-randomised studies when we did not find evidence from randomised trials. We avoided making recommendations for practice based on more than just the evidence, such as values and available resources. Our implications for research suggest priorities for future research and outline what the remaining uncertainties are in the area.
RESULTS
Description of studies
Results of the search
Alltogether, we screened 10234 references (see Figure 2) in three separate batches. The first search was ran in February-April 2015, the second in October 2015 and the third in January 2016. We report the results of these searches here together. The search in PubMed yielded 6898 references. When we excluded references already identified in MEDLINE, EMBASE yielded 1023 references. In CENTRAL, the search yielded 152 references. From CINAHL, we retrieved 888 references and from OSH-update 1283. From these references, we selected 205 articles for full-text assessment. Through checking the references of included articles we found 18 additional articles, by using Google another five and through contacting NGOs one (Tomas 2015). Our contacts with the manufacturers did not yield any answers. Most of the studies that we did not locate with our electronic searches were studies of PPE use during the SARS epidemic that did not make reference to any type of PPE in the title or abstract. The same happened during the EBV epidemic where we could not locate Nyenswah 2015 because there was no reference to PPE. By using Google search, we found one additional article (Bell 2015) that wasn’t indexed in any of the databases that we searched. We did not locate Tomas 2015 with our search strategy because the authors did not use any words referring to infection, disease or decontamination. Therefore we checked if there would be any other studies that only used the word contamination in addition to PPE. We did not find any other additional studies that we missed with our search strategy.
Based on a request of one of the peer referees we also searched the African Index Medicus which yielded 24 references but no new studies to include. For the next update of the review we will search also this database.
This added up to 205 papers that we checked full-text for inclusion. Of these, we excluded 196. This resulted in nine included studies.
Included studies
Study Types
We located eight simulation studies of which six simulated exposure to contaminated body fluids and two studies simulated donning and doffing procedures.
Of these simulation studies five were randomised studies (three parallel group (Bell 2015; Hung 2015; Wong 2004) and two cross-over (Guo 2014; Zamora 2006)) and three were non-randomised controlled studies (one cross-over (Casanova 2012; and two parallel group (Buianov 2004; Casalino 2015)).
In addition, we found one retrospective cohort study that evaluated the effect of PPE training on SARS infection rates and noncompliance with the doffing protocol (Shigayeva 2007). In this study, the authors located all HCWs that had been exposed to SARS patients and assessed, by questionnaire, compliance with PPE guidelines and PPE doffing guidelines.
Participants
In the simulation studies, researchers included 266 intervention and 139 control participants, taking into account that four used a cross-over design and thus all participants were intervention participants. In the cohort study, there were 563 intervention and 232 control participants. Altogether there were 1031 participants.
The participants in all studies were healthcare workers with a mixture of occupations, but mainly physicians, nurses and respiratory technicians. There was one study that included medical students during their internships (Casalino 2015). There were no studies that included other healthcare staff such as persons working in emergency services or cleaning staff.
Countries
Two studies were performed in Canada, three in China and Hong Kong, two studies in the US, one in Russia and one was performed in three countries at the same time: France, Peru and Mexico (Casalino 2015). There were no studies that were carried out in countries dealing with an EVD epidemic.
Time period
All studies had been conducted after the year 2000, with four before and five after 2010.
Interventions and comparisons
The nine studies evaluated ten interventions. Five studies compared one type of PPE to another. Four studies compared two different ways of doffing. One study evaluated the effect of instruction and training.
Comparison 1: One type of PPE versus another
Five simulation studies compared different types of PPE outfits, but all in a different way. None of them were similar enough to be combined. None of the included studies used a standardized classification of the properties of the PPE that protect against viral penetration such as the EN 14126.
Buianov 2004 compared two different types of Powered Air-Purifying Respirator (PAPR) that were escpecially developed for this project in Russia to protect health care personel against Ebola and similar viruses. Buianov 2004 also compared the effect of different airflow rates that varied from 50 to 300 liters per minute. The intervention participants were rquired to carry out a step test that lasted for four hours. The authors did not describe the equipment they tested in sufficient detail to be able to judge their technical qualities.
Zamora 2006 compared the use of a PAPR in use at the study hospital with the PPE for Enhanced Respiratory and Contact Precautions (E-RCP)CDC recommended at the time of the study.
Wong 2004 compared four types of PPE according to their material properties. First, they tested the material according to the American Association of Textile Chemists and Colorists standards 22 and 127. We excluded the surgical gowns only category since it had no water repellency and insufficient viral barrier properties. Type A had good water repellency and water penetration resistance, but at the cost of poor air permeability. Type B had good water repellency and good air permeability, but poor water penetration resistance. Type C was the surgical gown with both poor water repellency and water penetration resistance. Type D, Barrierman ®, was made of Tyvek ® and had good water repellency, poor air permeability and fair water resistance.
Bell 2015 compared commercially available PPE compliant with CDC recommendations with locally available clothing, such as rain coats that were thought to be as protective as the commercially available ones.
Guo 2014 compared three types of PPE: disposable water resistant non-woven gown, reusable woven cotton gown, and disposable non-woven plastic apron. The second one was a cotton, water permeable, gown like a surgical gown. We left this arm out of the analysis because surgical gowns alone are not used for EVD. They tested the fabrics for water repellency and liquid penetration according to the American Association of Textile Chemists and Colorists standard 22. The gown and the apron received ratings of four and five respectively on a scale of zero to five for water repellency.
Contamination rates are not only determined by the type of PPE but also by the donning and doffing procedures. All studies had a priori determined donning and doffing procedures. It should be noted that these studies evaluated the totality of the type of PPE with the donning and doffing procedure. We have described the procedures in the ‘Characteristics of included studies’ table.
Comparison 2: One procedure for donning/doffing versus another
Two studies specifically evaluated different ways of donning and doffing.
Casanova 2012 compared the effect of wearing two pairs of gloves with wearing one pair of gloves on contamination rates. The study was classified under methods of doffing because the intention of the double gloving was to decrease the contamination during doffing. Doffing was done as per CDC recommendation, which describes how to do both single gloving and double gloving.
Guo 2014 compared the effect of doffing a gown or an apron according to an individual’s own views versus the procedure recommended by CDC in the US in 2007: The following instruction were given: “Gown front and sleeves are contaminated! Unfasten neck, then waist ties. Remove gown using a peeling motion; pull gown from each shoulder toward the same hand. Gown will turn inside out. Hold removed gown away from body, roll into a bundle and discard into waste or linen receptacle”.
Comparison 3: One intervention to improve compliance versus another
Three studies evaluated different training methods for donning and doffing procedures.
Casalino 2015 compared what they called reinforced training versus training that was not reinforced. The reinforcement consisted of an instructor saying out loud what the next step of donning and doffing was. They used the reinforcement with both basic PPE and enhanced PPE where the enhancement consisted of a full-body suit and hood instead of a impermeable apron without a hood.
Hung 2015 compared a conventional training session for donning and doffing procedures to a procedure in which the conventional session was complemented with a computer simulation later in time.
Shigayeva 2007 evaluated the effect of active and passive training versus no training on compliance rates. Active training was defined as training that involved any group or face-to-face interaction. Passive training was defined as watching a video or receiving written instructions. This allowed us to make an indirect comparison between the effect of active and passive training. We calculated the effect of active training compared to passive training by subtracting the OR for passive training from the OR for active training, as outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We calculated the variance of this indirect comparison by summing the variances of both direct comparisons. Then we calculated the SE by taking the square root of the combined variance. We used this as input for the generic inverse variance method in RevMan.
Outcomes
Infection rates
No studies evaluated the effect of the interventions on infection rates.
Contamination outcomes
Simulation studies simulated and measured contamination by using either a fluorescent marker that lit up with the use of a UV-lamp, a non-pathogenic bacteriophage MS2 virus, or ‘aerosol containing microbes’ to contaminate PPE, a manikin and its surroundings, or both.
Study authors developed the fluorescent markers in various, non-standardised ways as follows:
For exposure, Bell 2015 used a base mixture of 500 ml liquid detergent, 500 ml water and three fluorescent tablets (Fluorescent powder (GloGerm ®), liquid clothes detergent with bleach alternative (Tide ®) and dissolvable fluorescent tablets (Bright Dyes Orange Dye ®)). This was combined with oatmeal, chocolate powder and crushed cereal to simulate different body fluids. For measurement of contamination after doffing, the researchers assessed the participants with an LED black light panel (Chauvet ®) and took photographs. Participants were counted as contaminated or not contaminated.
For exposure Wong 2004 used 0.2 mg of fluorescein (25% diluted in 100 ml of water). After doffing, participants were assessed with an UV-scan and photographed. Researchers measured the number of stains that lit up.
For exposure, Guo 2014 used a fluorescent powder (GloGermCo, Moab, UT), developed for determining hand hygiene compliance. The GloGerm ® powder was mixed with light olive oil and water to resemble human aerosol as closely as possible. For measuring contamination, the authors used a UV scan in dim light and measured fluorescent patches as small and large patches.
For exposure, Zamora 2006 used 1 ml of a 25% solution in 100 ml of sterile water to spray on the torso and the face of the participants. Then ‘invisible’ Detection Paste ® 15 ml was applied to the forearms up to the elbows, and the palms of the hands. After doffing, an observer assessed contamination with an UV-lamp. An evaluator assessed and measured all areas of contamination.
Casanova 2012 used bacteriophage MS2 in the following way to detect contamination: PPE was contaminated with bacteriophage MS2 suspended in 0.01 mol/L phosphate-buffered saline. Sites of contamination were the front of the shoulder, right side of the N95 respirator, right front of the eye-protection, and the palm of the dominant hand. Each side was contaminated with 105 plaque forming units (PFU) in 5 drops of 5 μl each. After doffing, the researchers took swabs from the face and sampled the hands with the ‘glove juice-method’ and put the scrub shirt and pants in eluant liquid for sampling.
Buianov 2004 used an aerosol containing microbes with a concentration of 108 colony forming units (CFU)/m3. There were no further specifications of the aerosol and what it contained. We could not reach the authors for further clarification.
Compliance with guidance: Noncompliance rates with donning and doffing procedures
Five studies evaluated the effect on noncompliance.
Two contamination simulation studies (Casanova 2012; Zamora 2006) also measured the effect of different attire on noncompliance with the donning and doffing protocol because the researchers thought that a more complicated PPE composition would lead to more errors. Noncompliance was measured as the number of participants that did not follow the correct order of the protocol, omitted elements, or did not use the correct equipment.
Noncompliance in one training study (Shigayeva 2007) was measured as the number of violations against protocol as recorded from interviews. There were two different compliance outcomes. One was called consistent adherence and was calculated as the proportion of exposure episodes with full compliance with PPE. The other one was called unsafe doffing, measured if one or more of the elements of the doffing procedure were violated. We recalculated outcomes in such a way that they represented the frequency of noncompliance.
Hung 2015 measured compliance as a score on a 16-item checklist for donning and 20-item checklist for doffing. To get results comparable to the other studies we substracted the mean compliance values from the maximum score and used these as noncompliance values.
Casalino 2015 measured noncompliance as the number of errors per person for donning and for doffing and the number of persons with one or more errors as measured by the specialist trainer/instructor who also gave the spoken instructions in case of reinforcement. The authors also measured critical errors, which were those where there was contact between skin and potentially contaminated PPE, but we did not consider this a valid measure of contamination and disregarded this. We took measurement of the errors at the last training session as the effect of the intervention. We disregarded the error measurements at earlier training sessions.
Costs and economic outcomes
No studies reported on costs or other economic outcomes such as resource use.
Other relevant outcomes
Buianov 2004 measured heart rate and body temperature. We chose to report the results of this outcome as well, as we identified it as an additional outcome that appeared relevant to the questions being addressed.
Excluded studies
Description of case series or outbreak
One reason for excluding important studies was that the researchers only described a case-series of HCW cases’ use of PPE for EVD (Muyembe-Tamfum 1999), Marburg Haemorraghic Fever infection (MHF) (Borchert 2007; Colebunders 2004; Jeffs 2007; Kerstiens 1999), Congo Crimean Haemorraghic Fever (CCHF) (Gozel 2013) or for SARS (Christian 2004; Ho 2003; Ofner 2003; Ofner-Agostini 2006). None of these studies described the use of PPE by the cases in such detail that they could be replicated. In combination with the lack of a control condition, it is difficult to conclude how much PPE, or the lack thereof, contributed to the infection. The only different study of a series of cases during an outbreak was the study by Dunn 2015 that contained proper descriptions of PPE.
Description of PPE use only
We excluded studies if they only described how and what PPE was used without relation to an outcome (Lowe 2014; Marklund 2002; Minnich 2003).
One type of PPE only
Luo 2011 and Tomas 2015 evaluated only one type of PPE without a comparison in a simulation study.
No infection rates or compliance outcomes
Some studies measured only performance with PPE compared to no PPE use and not infection rates or compliance (Castle 2009; Coates 2000; Hendler 2000).
Comparison with no PPE only
We excluded studies that only compared PPE use with no PPE and not with alternative PPE use (Lu 2006; Schumacher 2010; Teleman 2004).
Studies that evaluated only one type of PPE and not part of full body PPE
Ogendo 2008 measured eye protection only. Bearman 2007 measured universal glove use only. Chughtai 2013, Lindsey 2012 and Lindsley 2014 measured masks or face shields only. Even though these studies yield valuable information, it is unclear how well the results also cover the use of these items as part of full-body protection and therefore we excluded these studies.
Participants not exposed to highly infectious diseases with serious consequences
Many studies evaluated PPE use for other diseases than EVD and related haemorraghic fevers, such as HIV or other nosocomial infections that were not considered highly infectious and/or having serious consequences and we excluded these studies (Malik 2006; Ransjo 1979; Sorensen 2008).
Training or simulation studies without a control group
There were a number of studies that evaluated training but that did not use a control group. This makes it difficult to draw inferences about the effect of one type of training compared to another (Abrahamson 2006; Beam 2014; Hon 2008; Northington 2007; Tomas 2015).
Inconsistent use of PPE during the SARS epidemic
After intensive discussion, we excluded 11 studies that measured the use of PPE (mask, gloves, gowns, goggles) during the SARS outbreak and related that to the risk of SARS infection. One line of thinking was that these studies did not fulfil the inclusion criteria because the comparison here was not clearly one type of PPE versus another type of PPE. Another line of thinking was that the studies compared different types of PPE composition and thus would fulfil the inclusion criteria. We finally decided to deal with these studies in the discussion section only (Ho 2004; Lau 2004; Le 2004; Liu 2009; Loeb 2004; Nishiura 2005; Park 2004; Pei 2006; Scales 2003; Seto 2003; Teleman 2004).
Risk of bias in included studies
See Figure 3 for an overview of our judgment of the risk of bias per study. Since the table contains the risk of bias assessments for both randomised and non-randomised studies, not all cells are applicable to both study types and those that aren’t applicable remain empty.
Figure 3. Risk of bias summary: review authors’ judgements about each risk of bias item for each included study.
Allocation
Allocation was random in five studies but only two of them stated what method they had used for generating the random sequence (Wong 2004; Zamora 2006). Consequently we assessed these two as having a low risk of bias. Allocation concealment was not reported in the included randomised studies and therefore we rated it as unclear.
Blinding
In the simulation studies, the participants could not be blinded for the type of attire they were wearing or the type of donning or doffing procedure they were following. It is unclear if they could have contaminated themselves more with attire that they thought was not good, or they did not like, and we rated the risk of bias as unclear for all these studies. For one study, Casalino 2015, we rated the risk of performance bias as high, because the instructors who provided the intervention were very much aware if instruction was given or not and they were the assessors at the same time.
For the non-randomised SARS study (Shigayeva 2007), we considered the risk of performance bias low because the study was retrospective and the participants did not know they were part of a study.
The risk of detection bias was unclear in most studies, as it not reported whether outcome assessors were blinded. We considered the risk to be high in one study (Casalino 2015) as providers of the intervention are also the assessors of compliance, and in a second study (Shigayeva 2007) because the intervention and the outcome were assessed with the same questionnaire at the same time. We judged the risk to be low in the remaining two studies because the authors stated that assessors were blind to group status (Hung 2015; Zamora 2006).
Incomplete outcome data
We judged the risk of attrition bias low in four studies (Bell 2015; Guo 2014; Shigayeva 2007; Zamora 2006) and unclear in five studies (Buianov 2004; Casalino 2015; Casanova 2012; Hung 2015; Wong 2004).
Selective reporting
Selective reporting was a risk of bias that was difficult to judge because none of the included studies had published a protocol. We judged Bell 2015 to be at risk of reporting bias because they did not report separate outcomes for high or normal exposure. We also judged Hung 2015 to have a high risk of reporting bias, as the authors did not fully report the results of the computer usability questionnaire. We judged two studies (Casalino 2015; Guo 2014) to have a low risk of reporting bias, as the authors appeared to have reported all relevant data.
Other potential sources of bias
We did not consider any other sources of bias.
Bias due to confounding (Non-randomised studies)
We judged there to be a low risk of bias due to confounding in two non-randomised studies (Casanova 2012; Shigayeva 2007), unclear risk in one non-randomised study (Casalino 2015), and a high risk in one non-randomised study (Buianov 2004).
Bias due to selection of participants into the study (Non-randomised studies)
We judged there to be a low risk of bias due to selection of participants into the study for all four non-randomised studies (Buianov 2004; Casalino 2015; Casanova 2012; Shigayeva 2007).
Overall Risk of Bias per study
We judged studies to have a low overall risk of bias if we judged them to have a low risk of bias in the following domains: both random allocation and allocation concealment, or both confounding and selection bias, and incomplete outcome data and selective reporting. We considered the blinding of participants and outcome assessors less important because the outcomes were objective or we could not imagine that participants would have an interest in a certain type of attire and outcome. This left us with no studies at low risk of bias but all at either unclear or high risk of bias.
Effects of interventions
See: Summary of findings for the main comparison Comparison 1: One type of PPE versus another – PAPR versus E-RCP attire; Summary of findings 2 Comparison 1: One type of PPE versus another – Three types of PPE attire; Summary of findings 3 Comparison 1: One type of PPE versus another – Gowns versus aprons; Summary of findings 4 Comparison 2: One procedure for donning/doffing versus another – Doffing with double gloves compared to doffing with single gloves; Summary of findings 5 Comparison 2: One procedure for donning/doffing versus another – CDC method versus individual doffing
PPE types
1. Comparison 1: One type of PPE versus another
1.1. Powered air-purifying respirator (PAPR) versus Enhanced respiratory and contact precautions (E-RCP)
1.1.1. Outcome: Contamination with fluorescent marker
Zamora 2006 found that the PAPR system in use in their hospital led to less contamination than using the E-RCP system (Relative Risk (RR) 0.27; 95% Confidence Interval (CI) 0.17 to 0.43, Analysis 1.1). Other ways of measuring contamination also led to less contamination with the PAPR system: contamination more than 1 cm (RR 0.21; 95% CI 0.12 to 0.36). The total contaminated area was also less with a Mean Difference (MD) of −81.10 cm2 (95% CI −96.07 to −66.13). This was mainly due to a lack of protection of the neck in the E-RCP system.
1.1.2. Outcomes: Compliance with guidance - Donning and doffing noncompliance
Noncompliance with donning guidelines occurred more with the PAPR system as this consists of more elements (RR 7.50; 95% CI 1.81 to 31.10; Analysis 1.4; Zamora 2006). Noncompliance with doffing guidelines was more frequent with the E-RCP system, but this was not statistically significant (RR 0.50; 95% CI 0.20 to 1.23; Analysis 1.5).
1.1.3. Outcomes: Donning and doffing time
The donning (MD = 259 seconds) and doffing time (MD = 337 seconds) were considerably longer with the PAPR system (Analysis 1.6; Analysis 1.7; Zamora 2006).
1.2. One type of PAPR versus another and different airflow rates
1.2.1. Outcome: Contamination with microbial aerosol
Buianov 2004 found that the suit that had the hood attached to the suit (СКБ-I) had a lower ‘contamination penetration rate’ than the suits that had separate hoods and coveralls with a percentage of 8.10−8 for the suit and 2.10−1 for the coveralls. However, we could not understand the meaning of the penetration rate and we decided that we would not use these results for our conclusions (their results are not shown in data tables).
1.2.2. Outcomes: Heart rate and body temperature
Buianov 2004 also found that beyond 250L/min airflow rates there was no contamination anymore. Body temperature and heart rates were also lower at these airflow rates.
1.3. Four types of PPE versus another
Wong 2004 compared four types of PPE according to their material properties. Type A had good water repellency and water penetration resistance but at the cost of poor air permeability. Type B had good water repellency and good air permeability but poor water penetration resistance. Type C was the surgical gown with both poor water repellency and water penetration resistance. Type D, Barrierman ®, was made of Tyvek ® and had good water repellency, poor air permeability, and fair water resistance.
1.2.1. Outcomes: Contamination, User-reported assessment of comfort and convenience - usability, donning and doffing times
There were no considerable differences in contamination (Analysis 2.1) between Type A and Type B for face, neck, trunk, foot, or hand, but Type B scored about 10% higher on usability with MD −0.46 (95% CI −0.84 to −0.08; Analysis 2.2); this was due especially to better breathability of the fabric. There were no considerable differences in donning and doffing times (Analysis 2.3; Analysis 2.4).
There were considerable differences in contamination of the foot (MD −4.1 spots; 95% CI −6.94 to −1.26) and the hand (MD −12.76 spots; 95% CI −21.62 to −3.9) between Type A and Type D (Analysis 2.5); donning (MD 33 seconds, Analysis 2.7) and doffing (MD 17 seconds, Analysis 2.8) times were also much worse for Type D. Usability was not rated considerably differently (MD 0.25; 95% CI −0.12 to 0.62, Analysis 2.6).
It was unclear how many participants had no contamination. On average, all types of PPE had some contamination.
1.4. Formal PPE versus locally available PPE
Bell 2015 compared contamination in four subjects with formal PPE with four subjects with locally available protective gear, such as raincoats. They found contamination in one participant in both study arms. The study was so small that it is difficult to draw conclusions (Analysis 3.1).
1.5. Gown versus apron
Guo 2014 compared a gown with an apron and found that the gown left less contamination than an apron, regardless of the way of doffing (Analysis 4.1; Analysis 4.2).
2. Comparison 2: One procedure for donning/doffing versus another
2.1. Double gloving versus single gloving
2.1. Outcomes: Contamination with MS2 virus and Compliance with guidance - compliance errors
Casanova 2012 found that contamination with the use of double gloves was less than with single gloves, if all contaminated sites were taken together (RR 0.36; 95% CI 0.16 to 0.78; Analysis 5.1). However, all participants had some level of contamination. Measured as the quantity of virus found, the hands were less contaminated after degloving when participants used double gloves but due to missing data this could not be tested (Analysis 5.2). There were no more errors in compliance with the donning or doffing protocol (RR 1.08; 95% CI 0.70 to 1.67; Analysis 5.3).
2.2. CDC’s recommended versus individual doffing
Guo 2014 found that the CDC’s recommended way of doffing a gown or an apron led to a different decrease in contamination than individually chosen doffing. When doffing the gown, there were 5.4 fewer smaller contamination patches (95% CI −7.4 to −3.4) and 5.2 fewer stains in the environment (95% CI −7.3 to −3.3), but no difference in small contamination patches on the hands, shoes or underwear. For doffing the apron, there were fewer smaller stains, stains on the hands, shoes, and environment, but more large stains and a similar number of stains on the underwear (Analysis 6.1; Analysis 6.2).
Comparison 3: One intervention to improve compliance versus another
Comparison 3a. Training and instruction for proper and complete PPE use
3a.1. Active training versus passive training
3a.1.1. Outcome: Compliance with guidance - Noncompliance with PPE guidance
Shigayeva 2007 defined consistent adherence as always wearing gloves, gown, mask, and eye-protection. We transformed this to inconsistent use as being non-compliant with the guidance. The study found that active training led to less noncompliance than no training (OR 0.37; 95% CI 0.2 to 0.58; Analysis 7.1). For passive training, they found a lower risk of noncompliance compared to no training (OR 0.58; 95% CI 0.33 to 1.00). For the indirect comparison, active versus passive training, the OR was 0.63 (95% CI 0.31 to 1.30).
Comparison 3b. Training and instruction for PPE donning and doffing
3b.1. Active versus passive instruction
3b.1.2. Outcome: Compliance with guidance - Noncompliance with doffing procedures
Shigayeva 2007 did not find a considerable effect of active (OR 0.70; 95% CI 0.45 to 1.11) or passive training (OR 1.56; 95% CI 0.83 to 2.94) compared to no training (Analysis 8.1), on the number of errors in compliance with the doffing protocol. For the indirect comparison, active versus passable training, the OR was 0.45 (95% CI 0.21 to 0.98).
3b.2. Additional spoken personal instructions versus no such instructions
4.1.1. Outcome: Compliance with guidance - Noncompliance
Casalino 2015 found that there were substantially less noncompliance (persons with one or more errors) after additional spoken instruction compared to no instructions with RR = 0.31 (95% CI 0.11 to 0.93) and also that the mean number of errors fell with on average almost one (MD −0.89 95% CI −1.36 to −0.41) in the group with spoken instructions (Analysis 9.1; Analysis 9.2).
3b.3. Additional computer simulation versus no additional computer simulation
3b.3.1. Outcome: Compliance with guidance - Noncompliance
Even though the number of errors was low already, Hung 2015 found that adding computer simulation reduced the number of errors with on average half an error for donning (MD = −0.52, 95% CI −0.90 to −0.14, Analysis 10.1) and with more then one error for doffing (MD = −1.16, 95% CI −1.63, −0.69) doffing (Analysis 10.2).
4. Subgroup and sensitivity analysis
We planned a subgroup analysis of high versus low and middle income countries. However, there were not enough studies for such a subgroup analysis to be meaningful.
We also planned a sensitivity analysis including only studies we judged to have a low risk of bias. As none of the included studies fulfilled this criterion, we could not perform this analysis.
5. Quality of the evidence
We judged if there was a reason to downgrade the quality of the evidence for each domain of GRADE. Since we judged all studies to have a high risk of bias, we downgraded all comparisons by one level. We considered simulation studies to be indirect evidence, and downgraded the evidence yielded by these studies by one level as well. In addition, when there was only one small study, we downgraded because of imprecision. All in all, the quality of the evidence was very low for all comparisons.
DISCUSSION
Summary of main results
We found no studies conducted among HCWs exposed to EVD. We found one study that was conducted among HCWs exposed to SARS. We found eight simulation studies that either simulated the exposure or the donning and doffing procedure.
There were five studies that compared various types of PPE to one another but we could not combine their results due to clinical differences and thus all conclusions are based on single studies. There is very low quality evidence that it seems possible to improve breathability of protective suits without increasing the risk of contamination. Improved breathability of protective suits also increases user satisfaction ratings. For doffing, there is low quality evidence that double gloving as part of full-body PPE possibly reduces the risk of contamination and reduces the viral load on the hands without increasing the frequency of noncompliance with the doffing protocol. Following CDC recommendations for doffing gowns and aprons compared to individually chosen ways seems to decrease the risk of contamination. In all simulation studies, contamination happened both in the intervention arm and in the control arm for most participants.
For training, there is very low quality evidence from one SARS-related study and two simulation studies that more active training in PPE use decreases noncompliance with donning and doffing guidance more than passive training. Active training comprised of, for example, spoken instruction and computer simulation. The effect of training on noncompliance with PPE guidance was not significant in one study.
We found no audit reports or other unpublished reports, even though we put considerable effort into asking PPE producers and NGOs involved in relief aid to provide them.
Overall completeness and applicability of evidence
We did not find evidence on a number of important comparisons for types of PPE: gowns versus coveralls, goggles versus visors, hoods in combination with goggles, or taping versus no taping. In the studies, there were no data on breach of PPE. Most studies provided sparse descriptions of the PPE they used, except for Zamora 2006. They gave a detailed description of the name and brand of each PPE item used, including details of the manufacturer. Five studies were over ten years old, and it is unclear if the attire used in those studies would still be obtainable today. This makes the evidence on absolute level of protection difficult to apply.
None of the studies used the ISO or EN classifications for chemical protection (ISO 2013) or for viral protection (ISO 2004; EN 14126). We believe that the standards are very helpful to determine the protective potential of PPE, and we don’t see a reason to doubt the technical protection that these materials provide when properly implemented. A working group led by Médecins Sans Frontières (MSF) has suggested that a new standard should be developed for the ability of fabric to prevent penetration with EVD (Sprecher 2015). To us, this does not seem like the first research priority, given the high level of contamination in the included studies while donning and doffing, even after instruction and training.
Even though doffing procedures are fairly easy to evaluate in simulation studies, we found only two studies that evaluated the effect of double gloving and CDC recommendations for gowns and aprons. Important questions that we could not answer were: single versus two-person procedures, with or without spraying of disinfectants, and what to do in a case of breach of barrier protection. It seems that it would not be difficult to perform simulation studies to find out how important these procedures are. For the evaluation of the use of disinfectants, bacteriophage MS2 could be a viable option for simulated exposure with the assumption that the disinfectant would work equally well for EVD and the MS2 virus. Using MS2 has the advantage of being able to quantify the contamination as the amount of virus that is found on the skin. For example Casanova 2012 found that the amount of virus on the hands after doffing ranged from 1.4 to 316 PFU (measured as MPN). According to Judson 2015 infectious doses of less than 10 PFU of EVD have been reported to cause viremia in non-human primates. This means that in spite of protection, in the Casanova 2012 study there was still a risk of infection.
Because studies seem feasible and because we searched exhaustively, there must be other reasons why there is so little evidence. One of these is probably the highly politicized context in which such a study has to be performed during an epidemic. For example, during the epidemic in 2014, we weren’t able to get in touch with WHO and the researchers of the systematic review commissioned by WHO did not want to communicate with us, presumably because of the political implications. During the Ebola epidemic, 28 HCWs who worked for MSF became infected and 14 of them died (MSF 2015).Two of those that have been infected were not locals, but international HCWs (French and Norwegian). There were a total of 250 international HCWs working during the Ebola epidemic which yields an infection risk of 0.8 %. As 26 out of 3000 national HCWs died their risk was also 0.8%. MSF assumes in their report that both international HCWs had an occupational infection and that all national HCWs were infected outside work. In their report, MSF also promises to provide more information. Even though we asked MSF several times for more explanation about their HCWs that became infected, we did not get a response. This stresses the need for a joint initiative, possibly coordinated by WHO to overcome the political pressures and to organise more studies.
While the included studies showed that more active training prevented errors, it is not clear how long the effects of training last. Northington 2007 showed that at six months after training, only 14% of participants were able to correctly don and doff PPE. It is unclear from the included studies, if fit-testing of masks is part of training. This is a prerequisite for proper functioning of respiratory protection.
There were no studies conducted in a low- and middle-income (LMI) country. Since most serious haemorrhagic fever epidemics occur in Africa, this is a serious disadvantage of the current evidence. Training on the correct way to use appropriate PPE is a challenge in these countries. We still hope that there are unpublished reports from the 2014 to 2015 Ebola epidemic that we can use for an update of this review.
From the SARS epidemic, it seems that the consistent use of PPE rather than the the type of PPE was most important (Appendix 6). At the start of the epidemic, SARS patients were not appropriately diagnosed, and the importance of PPE was not immediately clear. Personal protective equipment compliance was higher in the later stages, and infections occurred less frequently (Nishiura 2005). During the 1995 Ebola epidemic in Kiwit, a study also reported that once PPE and other control measures were used, there were very few HCW infections (Kerstiens 1999).
We set out to include and describe case studies in the hope that they would provide information on the effects of PPE. Only one (Dunn 2015) of the case studies we found provided systematic information on the use of PPE and therefore we weren’t able to draw any conclusions from these. This is a similar experience as Hersi 2015 had as they performed a systematic review of case studies and case series but had to conclude that they did not provide useful information. We reanalysed the case study by Dunn 2015 as a cohort of exposed HCWs. The relative risk of contracting Ebola infection for HCWs using gloves only versus those not using PPE was 0.16 (0.04 to 0.71) indicating that using gloves already provides a lot of protection. For using gloves or a gown or more compared to no PPE, the RR was 0.03 (0.00 to 0.57) (Verbeek 2016). This is very similar to the findings of the SARS studies mentioned above. It is also, to a certain extent, reassuring for those situations in low- and middle income countries that do not have sufficient PPE available (Levy 2015) that some PPE already decreases the risk of infection considerably.
Quality of the evidence
We rated the quality of the evidence as very low for all comparisons, mainly because all the included studies had a high risk of bias. The SARS study had a high risk of recall bias because participants had to recall their use of PPE after the epidemic occurred. Half of the simulation studies had a very small sample size and did not report their outcomes by intervention or control group.
One of the major problems was that most of the studies did not indicate if the PPE that they used complied with one or more of the international standards for protective clothing and whether they used viral barrier fabrics. The lack of attention to the designation of PPE as being protective for viruses is problematic also in practice.
The many different labels and standards in use to designate protection against contamination with viral diseases such as EBV make it almost impossible to make the right choice for a HCW in practice. The confusing language of infection control has also been reported for isolation practices in general. Therefore, Landers 2010 called for the adoption of internationally accepted and standardized category terms for isolation precautions. Others have tried to improve the standardisation by providing HCWs with a summary card of the various types of precautions that have to be taken and indicated that this increased the implementation of precautionary measures (Russell 2015).
Zamora 2006 used attire recommended by the CDC in 2005, but since then, the recommendation has been superseded by much more stringent protection.
In simulation studies, it is not clear how well the exposure represents real life exposure. Some studies used ‘high volume exposure to simulate splash’ (Bell 2015), whereas other studies only used a powdered fluorescent marker spread in the room (Beam 2011). It is also not clear how well the fluorescent marker can indicate that there is no viral contamination. Casanova 2008 showed that in spite of no fluorescent marker being detected, there could still be viral contamination with bacteriophage MS2. Therefore, in simulation studies, the objective should be to reach zero contamination.
Only one of the case studies that we collected (Dunn 2015) properly described the use of PPE. Better description would enable better analysis.
Potential biases in the review process
We excluded all studies that evaluated only one piece of PPE, such as goggles or masks. However, none of these excluded studies would have answered the questions that in our current review remained unanswered. From Casanova 2012, it became clear that using double gloves as part of full-body PPE is important, because it facilitates the removal of the other pieces of PPE without contaminating the hands. This shows that it is important to consider the effect of one piece of PPE as part of the full-body PPE. In addition, seldom is there only one clear transmission route. Even with SARS which, as a respiratory infection, was spread by droplets and aerosols, consistent use of other pieces of PPE besides respiratory protection was still important. Therefore, we don’t think that these strict inclusion criteria biased the results of our review.
We assumed that adherence to PPE use and training would work in a similar way between SARS, EVD and simulation studies. However, there is an important difference; at the start of the SARS epidemic, the causal virus and transmission were unclear and workers were probably not instructed well enough to protect themselves. On the other hand, it has been known for years that EVD is a highly contagious disease with a very high fatality rate. Thus, compliance and effectiveness of training concerning EVD might be higher than we concluded from the SARS study.
In the SARS studies that we excluded, there was high heterogeneity in the effects of consistently wearing PPE that we could not explain. The heterogeneity in effect is also underpinned by studies that did not find any SARS infections in spite of imperfect protection with PPE. This means that the effectiveness of PPE at best, is not fully understood.
Four of the simulation studies were cross-over studies where the authors analysed the data with tests that took into account the paired nature of the data: Zamora 2006 used the Mailand-Gart test, Guo 2014 used repeated measures, and Casanova 2012 the paired t-test. We could not use the results of these tests in our analyses in RevMan which resulted in wider confidence intervals than if a paired analysis had been used. There were insufficient data in the studies to properly adjust for the cross-over effect in our analyses. However, all results that were reported as being statistically significant were also statistically significant in our analyses. Therfore, we don’t think that this has biased our results.
For the simulation studies, the way exposure was simulated is an important element to consider. This varied highly between the studies. However, most studies used a worst case scenario, spraying fluorescent marker over large parts of the body. For future studies, it would be good to have consensus on how exposure can be best simulated.
For the included non-randomised studies, we assessed risk of bias with a hybrid version of the Cochrane risk of bias tool and the recently developed Acrobat tool. This might not have been the most optimal way to assess risk of bias. However, we believe that the limitations of the available studies are profound and a more rigorous bias assessment could not have lowered our confidence in the evidence.
Agreements and disagreements with other studies or reviews
We found two other reviews that have evaluated the effect of PPE for highly infectious diseases with serious consequences in HCWs: Hersi 2015 and Fischer 2015. Hersi 2015 was commissioned by WHO to underpin the PPE guidelines issued for HCWs exposed to EVD. The authors originally included only controlled studies of interventions to protect HCWs against EVD and similar hemorrhagic fever infections with infection rates as outcomes. During the review process the authors decided to also include case studies and case series but they were not able to draw conclusions from these studies because the PPE use was not well described. Fischer 2015 took a more pragmatic but unsystematic approach and included all articles pertaining to filovirus transmission and PPE and in addition articles that evaluated donning and doffing strategies. They conclude that there is a lack of evidence but that simulation studies could provide evidence for guidelines.
Heat stress and breathability is an important issue in PPE especially for Ebola. Kuklane 2015 argued that using other materials would substantially reduce the heat stress but these come at a tenfold higher price. Other researchers that have looked into this problem have found inconsistent results. Coca 2015 found that PPE on manikins led to a critical body core temperature of 38.4°C in one hour. On the other hand, Grélot 2015 found that HCWs caring for Ebola patients had only a 0.46°C rise in core body temperature after being at work for one hour. Of the 25 workers studied only four reached a core body temperature over 38.5°C.
An independent panel of experts that evaluated the Ebola response (Moon 2015) concluded, among many other things, that a coordinated research effort is needed to build a better global system for infectious disease outbreak and response. Their recommendation is that research funders should establish a worldwide research and development financing facility for outbreak-relevant drugs, vaccines, diagnostics, and non-pharmaceutical supplies (such as PPE). This is very much in line with what we experienced and found in this review.
Missair 2014 reviewed implications of EVD patient management for anaesthetists based on a literature review of all types of studies on EVD. This is why their inclusion criteria were very broad and non-specific. Finally the authors relied on PPE guidelines as provided by WHO and MSF to make recommendations with no evidence of their comparability. This makes their results difficult to compare to ours.
Moore 2005 reviewed all measures to prevent healthcare workers from SARS and other respiratory pathogens in a narrative format, from 168 publications. They concluded that a positive safety climate is the most important factor for adherence to universal precautions. They recommend using adequate PPE, but they do not define ‘adequate’. Their inclusion criteria were much broader and the results are difficult to compare with ours. The same research group formulated valuable advice about research gaps based on this review but focused only on respiratory protection (Yassi 2005). They corroborate the findings of Jefferson 2011, that N95 respirators may not be all that superior, citing the early containment of the SARS epidemic without these in Hanoi.
The Cochrane review by Jefferson 2008, updated in Jefferson 2011, evaluated the effect of physical interventions to interrupt the spread of respiratory viruses for all populations. Even though they only included studies on respiratory infections and any type of protection for any person at risk, 10 studies in their review are about SARS and protecting healthcare workers. The authors did not conduct a subgroup or additional analysis of these HCW studies. Because the infection risk for HCW is substantially different from the populations they protect, the Jefferson 2011 results are not applicable to HCWs.
AUTHORS’ CONCLUSIONS
Implications for practice
In addition to other infection control measures, consistent use of full-body PPE can diminish the risk of infection for HCWs. EN and ISO standards for chemical protective clothing and fabric permeability for viruses are helpful to determine which PPE should technically protect sufficiently against highly infectious diseases. However the risk of contamination depends on more than just these technical factors. In simulation studies, contamination happened in almost all intervention and control arms.
There is very low quality evidence, based on single exposure simulation studies, that more breathable fabric may still lead to similar levels of contamination protection as less breathable fabric, and is preferred by users. The lack of use of standards in the included studies prevents the extrapolation of results of studies comparing PPE types to PPE in current use. There were no studies, and thus no evidence, of the effectiveness of taping parts of PPE together, or the effects of goggles compared to visors.
For different procedures of donning and doffing, there is very low quality evidence based on a single study each that double gloves, as part of PPE and following CDC guidelines, may reduce the risk of contamination. There are no studies on the use of disinfectant during doffing.
For various training procedures there is very low quality evidence that more active training, including computer simulation or spoken instructions may reduce the risk of infection compared to passive training or to not giving such instructions or to simulation. There are no studies that have compared methods to retain PPE skills needed for proper donning and doffing in the long term.
The quality of the evidence is very low for all comparisons because of high risk of bias in studies, indirectness of evidence, and small numbers of participants. This means that we are uncertain about the estimates of effects, and it is therefore likely that the true effects may be substantially different from the ones reported in this review.
Implications for research
We call on WHO and NGOs in medical relief work to organise studies and to raise awareness for the lack of evidence for the effect of specific PPE. We also call upon them to develop a more transparent and uniform labeling of infection control measures and the protection level of PPE for HCWs. We believe that this is an important prerequisite for the universal implementation of infection control measures for HCWs.
Simulation studies are a feasible and relatively simple way to compare different types of PPE such as gowns versus coveralls, goggles versus visors, combinations of hoods and goggles, taping versus no taping, spraying disinfectant versus not spraying and various procedures after breach of PPE to find out which protects best against contamination. It is a prerequisite for a reliable answer that methods of simulation studies are standardised in terms of exposure and outcome measurement. Viral marker Bacteriophage MS2 seems to be the most sensitive marker and we would advocate to use this. Studies should have sufficient power. To be able to detect a RR of 0.5 with a control group rate of contamination of 0.7, assuming α = 0.05 and β = 0.80, a sample size of 62 would be needed.
To find out how PPE behaves under real exposure, we need prospective follow-up of HCWs involved in the treatment of patients with highly infectious diseases, with careful registration of PPE and risk of infection. Because different NGOs use different PPE guidance, cohorts of workers would be relatively simple to establish if there would be sufficient political will. Here, the effect sizes would be smaller and thus the sample size should be bigger than 60.
In addition, case-control studies comparing PPE use among infected HCWs and matched healthy controls, using rigorous collection of exposure data, can provide information about the effects of PPE on the risk of infection. The sample sizes should be much bigger than the current case studies because we would like to detect small but important differences in effect between various combinations of PPE such as gowns versus coveralls. There is a need for collaboration between organisations serving epidemic areas to carry out this important research within limited resources, and during the throes of an outbreak.
We also need more randomised controlled studies of the effects of one type of training versus another, to find out which training works best, especially at long-term follow-up of one year or more. Also here, the effect size seems to be quite large and thus a sample size of around 60 seems to provide adequate power.
ACKNOWLEDGEMENTS
We thank the Cochrane Editorial Unit for providing financial support to undertake this review. We thank Toby Lasserson, Hannah Ryan, Darrel Singh, Fiona Smaill, Mauriccio Ferri, Annalee Yassi, Nuala Livingstone and Julian Higgins for their comments on the text. We extend a special thank you to Consol Serra for her editorial work. We thank Vicki Pennick for copy editing the text. We thank Claire Allen from Evidence Aid for her help in trying to locate unpublished reports. We thank Alexey Pristupa for assessing the studies written in Russian.
SOURCES OF SUPPORT
Internal sources
-
Cochrane Collaboration, UK.
Bursary to Sharea Ijaz
-
Finnish Institute of Occupational Health, Finland.
Salary for Jos Verbeek, Christina Mischke, Jani Ruotsalainen, Erja Mäkelä and Kaisa Neuvonen
-
National Institute for Occupational Safety and Health, USA.
Salary for F Selcen Kilinc Balci
External sources
No sources of support supplied
CHARACTERISTICS OF STUDIES
Characteristics of included studies
| Methods | Randomized two parallel groups; simulation study | |
|---|---|---|
| Participants | N = 8, nurses (6), physicians 2; women 7/8 Intervention: 4 Control: 4 Volunteer healthcare providers, no further details provided Location: USA |
|
| Interventions |
Intervention: Commercially available PPE: neck-to-ankle coverall (type not reported), water impermeable surgical gown, knee length impermeable leggings, Stryker hood, double gloves with outer arm-length surgical gloves, N95 masks; meeting CDC recommendations; each participant was assisted in PPE donning by an experienced trainer. Control: Local readily available attire: two plastic gowns worn over the front and the back of the torso, rain-suit pants and hood, spark-shield as face-cover, ankle length shoe covers, double gloves with outer arm-length surgical gloves, N95 masks; meeting CDC recommendations; each participant was assisted in PPE donning by an experienced trainer. |
|
| Outcomes | Contamination: measured in ml of fluorescent agent with LED black light after doffing. Random order of two types of exposure: high volume or standard. High volume meant 100 ml of fluorescent agent splashed on the torso. Standard meant working on a manikin contaminated with fluorescent agent. Fluorescent liquid mimicked body fluids and consisted of fluorescent powder, clothes detergent, fluorescent tablets |
|
| Notes | No funding or conflict of interest reported Apparently tape was used to put attire together; this resulted in more difficult doffing but no figures reported; costs of locally available equipment was 36 US dollars, that of commercial material not reported |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “randomized to one of two PPE ensembles” |
| Allocation concealment (selection bias) | Unclear risk | not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | no incomplete outcome data |
| Selective reporting (reporting bias) | High risk | Contamination outcomes reported but no separate outcomes for high or normal exposure, however small sample and no statistical analysis by study authors |
| Other bias | Low risk | No indication |
| Methods | Controlled simulation study, not randomised; probably cross-over study | |
|---|---|---|
| Participants | N = 9 volunteers that carried out a 4-hour step test of average workload at a temperature of 20° C and 60% relative humidity, no further details provided. | |
| Interventions |
Intervention: Positive pressure suit (special biological suit, CKE-I) consisting of a rubber hood connected to a powered air-purifying respirator and a ‘dust-proof’ coverall in one piece with different rates of air supply: initially 250 L/min, then 50, 100, 150, 200, 250, 300 L/min. No information about the filtering piece. PPE was especially developed for highly infectious diseases such as Ebola, Marburg and Lassa fever intended for use by health care staff, such as doctors, nurses and orderlies Comparison: Two different types of positive pressure hoods (лИ3–4 and ПшБ-3) together with a coverall type Biotekhnolog-1. Procedure: Tests are carried out in a so-called Meltserovsky room (individual room with quarantine). The pressure suit or hood and coverall is put on before entering and checked whether it functions by attaching the connecting pipe to the air supply system. Then the worker enters the buffer zone (gateway with entrance and exit) and proceeds to the individual measurement room. After the step test in the individual room the worker goes to the buffer zone in order to treat the outside surface of the pressure suit. The worker attaches the suit to the connecting pipe of the air supply system and treats the suit with the help of aerosol disinfectant, usually 3–6% hydrogen peroxide (2–3 aerosol generators are situated at different heights). After the aerosol rests are pumped out of the buffer zone the worker leaves through the gateway, takes off the pressure suit and places it in the special containers for final disinfection. |
|
| Outcomes | Contamination exposure: Participants were exposed to a microbial aerosol with a concentration of 108 colony forming units(cfu)/m3. No further details on the spray aerosol provided. Contamination outcome measured aerosol particles on different parts of the body (neck, shoulder, forearm, chest, loin, thigh, shin) and the suit with “washouts” and triple agar prints. Only data from triple agar prints is presented since the “washouts” resulted in unreliable data (because the textile materials used in the pressure suit were impregnated with hydrophobic materials). Triple agar prints were taken from the outside surface of the pressure suit, inside surface of the pressure suit, clothes and skin areas at different parts of the body (neck, shoulder and forearm, chest, loin, thigh and shin). The outcome was both expressed as cfu/m3 and as penetration rate as a percentage of the outside that has leaked inside the PPE. It was unclear if these outcomes were expressed as an average across the participants and what the variation was. The authors conclude that "despite the significant concentration of microbial aerosol in the experimental room (107-105 cfu/m3) no microbial aerosol was measured on skin areas with air supply speeds of 250 L/min and higher". Additionally, the authors assessed skin temperature, heart rate, breath rate, and moisture loss |
|
| Notes | Article in Russian, data retrieved with help of a native speaker (AP) Article difficult to judge due to cultural differences in style and translation |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Confounding NRS | High risk | No confounders reported |
| Selection Bias NRS | Low risk | Selection of volunteers unrelated to intervention or to outcome. Start follow-up and intervention coincide for all participants. |
| Blinding of participants and personnel (performance bias) All outcomes |
Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes |
Unclear risk | Unclear if data reported for all nine participants |
| Selective reporting (reporting bias) | Unclear risk | All data announced in methods reported in results |
| Other bias | Low risk | No other biases assessed |
| Methods | Controlled before-after study of two training variants | |
| Participants | N = 120, 63% nursing students, 37% medical students Age 21.2 +/− 3.5 years, 35% male The authors did not present demographic data per group Location: Paris (France), Lima (Peru), and Guadalajara (Mexico), in December 2014 and January 2015 with no previous training in PPE use, with no special intention to be involved in Ebola care. |
|
| Interventions |
Intervention: There were two intervention groups that only differed in type of PPE used: 1. Basic PPE + reinforced training (N = 30); basic PPE consited of boots, goggles, surgical mask, surgical cap, impermeable apron (11 pieces of equipment) with 6 steps for donning and 13 steps for doffing. 2. Enhanced PPE + reinforced training (N = 30); enhanced PPE consisted of boots, full-body impermeable suit, hood with surgical cap and mask, double gloves, impermeable apron (9 pieces of equipment) with 6 steps for donning and 12 steps for doffing. Training for all participants consisted of 60 minutes of theoretical course including 10 minutes of donning instruction and 20 minutes of doffing instruction. In addition, there were three practical training sessions per two students who mutually assisted each other observed by a specialist trainer who intervened in case of non-compliance. The sessions were held with 3 days intervals. Compared to the control group the additional intervention was that the specialist trainer "repeated aloud each of the steps and technical skills or processes necessary" to comply with the standard during the practical training sessions. The sessions were also reviewed comprehensively. Control group: There were two control groups that differed in type of PPE used just as in the intervention groups: 1. Basic PPE + conventional training (N = 30), 2. Enhanced PPE + conventional training (N = 30). These groups received the same training as the intervention group but the specialist-trainer did not repeat aloud the necessary steps. |
|
| Outcomes |
Primary outcome: number of errors per person for donning and for doffing and the number of persons with one or more errors measured by the specialist trainer. The authors also measured critical errors, which were those where there was contact between skin and potentially contaminated PPE, but we did not consider this a valid measure of contamination and disregarded this. We took measurement of the errors at the last training session as the effect of the intervention. We disregarded the error measurements at earlier training sessions. Secondary outcomes: errors for doffing of the gown, full-body suit and boots; duration of donning and doffing in minutes at the last training session. |
|
| Notes | Country: France, Peru Mexico; no funding reported; no conflict of interest reported The first author, Enrique Casalino, answered some of our questions regarding the study, but we were unable to retrieve more information on the group allocation and therefore classified the study as non-randomised. |
|
| Risk of bias | ||
|---|---|---|
| Bias | Authors’ judgement | Support for judgement |
| Confounding NRS | Unclear risk | None of the confounders mentiond |
| Selection Bias NRS | Low risk | Students were randomly chosen and did not have any experience or intention to use the knowledge and skills. |
| Blinding of participants and personnel (performance bias) All outcomes |
High risk | Blinding not possible but students could be motivated to perform better because of knowing that they are in the intervention group and not as a result of the oral instructions. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Providers are also the assessors of the compliance. We asked authors for more information but did not get any information that increased our confidence in the outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes |
Unclear risk | Not reported if all data were available |
| Selective reporting (reporting bias) | Low risk | All outcomes in methods section reported; no protocol available |
| Other bias | Low risk | No other biases assessed |
| Methods | Controlled simulation study, non-randomised, first intervention then control condition for all participants | |
| Participants | N = 18 volunteer healthcare providers over 18 years of age; Exclusion criteria:pregnant, latex allergy, skin disorder, previous fit-testing for N95 respirator; 17/18 right handed, 18/18 previous experience with PPE Location: USA |
|
| Interventions |
Intervention: Two pairs of latex gloves; inner glove under the cuff of the gown sleeve, the outer glove, one size larger worn over the gown cuff; in addition, full PPE consisted of contact isolation gown, N95 respirator and eye protection Control: One pair of latex gloves in addition to similar full PPE as in intervention group Doffing was performed according to CDC instructions: gloves, goggles, gown, mask or respirator in case of single gloves; in case of double gloves, outer pair of gloves first and inner pair last |
|
| Outcomes | 1. Contamination of the hands, face, gloves and scrubs with bacteriophage MS2 virus;hands sampled with "glove juice method", face with a swab at the edge of the N95 respirator, shirt pants and gloves were immersed in beef extract. All eluants were assayed by ‘most probable number enrichment infectivity assay' (MPN). Detection level 0.15 log 10 MPN; Used paired t-test for the analysis of continuous data to take the cross-over into account 2. Noncompliance with doffing guidelines. Contamination with bacteriophage MS2 was put on front shoulder of the gown, right side of respirator, right front of eye protection and palm of dominant hand by simulated droplet contamination; before doffing participants had to perform neck and wrist pulses on manikin. |
|
| Notes | No funding or conflict of interest reported | |
| Risk of bias | ||
|---|---|---|
| Bias | Authors’ judgement | Support for judgement |
| Confounding NRS | Low risk | No apparent confounders for this type of study and outcome |
| Selection Bias NRS | Low risk | No apparent selection of participants into the study |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | no blinding, but performance bias not likely because participants would not have an interest with either intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Some data only in figures and not in tables |
| Other bias | Low risk | no other biases anticipated |
| Methods | Randomised multiple arm cross-over simulation study | |
| Participants | N = 50; Voluntary HCWs who gave informed consent; excluded were those who were allergic to the fluorescent marker; 34/50 female, 20/50 nurses, 10/50 doctors, 15/50 support staff, 5/50 allied health workers; age 32.9 ± 5.7 years average; working experience 10.9 ± 5.1 years Location: Hong Kong China |
|
| Interventions |
Intervention 1: N = 50 participants. Three types of protective clothing: 1. Disposable water resistant non-woven gown, 2. Reusable woven cotton gown, 3. Disposable non-woven plastic apron; and two different removal methods: individually determined or CDC recommended. Each of the 50 subjects was required to test the 3 different types of PPE followed by one of two different removal methods. Intervention 2: First the participant should doff according to their own views (individual method), then a CDC instruction video was shown and participants were asked to perform the donning/doffing method for gowns that was recommended by CDC in 2007: Gown front and sleeves are contaminated! Unfasten neck, then waist ties. Remove gown using a peeling motion; pull gown from each shoulder toward the same hand. Gown will turn inside out. Hold removed gown away from body, roll into a bundle and discard into waste or linen receptacle. Control: Cross-over N = 50 participants. Three types of protective clothing were compared against each other. |
|
| Outcomes | 1. small patches of fluorescence < 1 cm2. 2.large patches of fluorescence > 1 cm2. 3.patches on the hands 4.patches on the shoes 5. underwear patches 6. patches in the environment; a fluorescent powder (GloGermCo,Moab,UT) especially developed for determining hand hygiene compliance was used in this study. The Glo Germ powder was mixed with light olive oil and water to resemble human aerosol as closely as possible. The authors used repeated measures analysis to take into account the cross-over design of the study |
|
| Notes | Funding Hong Kong polytechnic University; no conflict of interest declared | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | interventions were offered "in random order"; authors asked for clarification |
| Allocation concealment (selection bias) | Unclear risk | not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding possible, but no performance bias expected as participants would not have an interest with any intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | no loss to follow-up |
| Selective reporting (reporting bias) | Low risk | all data reported |
| Other bias | Low risk | not detected |
| Methods | Randomised two parallel groups controlled trial of two training variants | |
| Participants | Intervention group: N = 25, Age 44% < 31 years, health care assistant 56%, nurse 44%, work experience < 6 years 44%, no gender reported Control group: N = 25, Age 28% < 31 years, health care assistant 56%, nurse 44%, work experience < 6 years 48%, no gender reported All HCWs of an outpatient department of a private hospital handling infectious pateints before admission; able to read English, basic computer skills. |
|
| Interventions | Intervention: All participants were asked to don and dof N95 respirator, face shield, cap, gown, gloves for "precautions against airborne danger". External observers rated the procedures for errors. All participants then attented a PPE-training consisting of a 15 minutes demonstration of donning and doffing by an "infection control link nurse". After one week the intervention group got the computer simulation programme and again after one week was assessed for compliance with the donning and doffing procedures. | |
| Control: the control group was assesssed for compliance with donning and doffing procedures one week after PPE training. The group did not get the computer simulation training. | ||
| Outcomes | Primary outcome: score on 16 item checklist for donning and 20 item checklist for doffing. Secondary outcome: IBM computer system usability questionnaire (CSUQ) consisting of 19 items with a 7-point Likert response scale. |
|
| Notes | Hong Kong China; Funding: Hong Komg Research Grant Council; no conflict of interest reported | |
| Risk of bias | ||
|---|---|---|
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The subjects were randomly assigned to the control and experimental group of the same size", page 53 |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes |
Unclear risk | Not possible to blind participants or providers |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Nurse assessing PPE compliance "was blinded about the research", page 53 |
| Incomplete outcome data (attrition bias) All outcomes |
Unclear risk | Not reported if all participants contributed data |
| Selective reporting (reporting bias) | High risk | Results of computer usability questionnaire not fully reported |
| Other bias | Low risk | No other biases assessed |
| Methods | Retrospective cohort study | |
| Participants | HCW who provided care or entered the room of a Toronto SARS patient who required intubation during the 24 hours before and 4 hours after intubation. Eligible N = 879, Analysed N = 795; age (median) = 41 years (range 21 to 67 years); employment in current occupation (median) = 12 years (range 0 to 43 years); 46% nurses, 14% physicians, 14% respiratory therapists, 10% imaging staff and 16% other; 1055 exposure episodes or shifts. Intervention Active training: N = 511 episodes (= 385 persons), Intervention Passive training: N = 236 episodes (= 178 persons), Comparison no active training: N = 308 episodes (= 323 persons). Location: Canada |
|
| Interventions |
Intervention 1: Active training: participants answered that they had received any individual or group face-to-face training sessions Intervention 2: Passive training: participants watched a video or got written information. Comparison: no training reported Other predictors of PPE studied in a multivariate GEE logistic regression analysis in addition to training for both outcomes: phase of epidemic, occupation, work experience, hospital type, location of care, number of times patienťs room entered, SARS diagnosis recognised, Apache II score of patient. |
|
| Outcomes | 1. Consistent adherences as proportion of exposure episodes. Participants were interviewed based on a questionnaire 0.2 to 10 months after the exposure. Interviewers asked about consistent use of PPE: masks, gowns, gloves and eye protection and possible predictors of their use, including training. Consistent adherence was defined as always wearing gloves, a gown, a mask, and eye protection. Consistent adherence was reported in 817/1055 (77%) exposure episodes. Eye protection was least with 13.5% consistent and no PPE in 23 episodes (2.2%). PPE use increased during epidemic from 34.6% at start to 97.4% in the end. 2. Doffing as proportion of exposure episodes (safe, at some risk, or at risk). Participants were asked about their sequence of doffing PPE. Safe was defined as the sequence of removing gown and gloves, hand hygiene, mask, goggles, or safety glasses, hand hygiene. At some risk was considered if hand hygiene was performed only once. At risk if no hand hygiene was performed or hands touched potentially contaminated face. Doffing description was available for 810/1055 (77%) of exposure episodes; 15.4% qualified as safe, 63% as at some risk, and 22% as at risk. |
|
| Notes | Units of analysis used in studies: exposure episodes not persons exposed, based on work schedules, patient assignments and health records. There were 65 intubations of SARS patients of which 7 were not recognised as such at the time of intubation. Funding Ontario Ministery of Health and Long term Care; no Conflict of Interest reported |
|
| Risk of bias | ||
|---|---|---|
| Bias | Authors’ judgement | Support for judgement |
| Confounding NRS | Low risk | Adjustment in multiple regression analysis for education, work experience, and presumably for age and sex |
| Selection Bias NRS | Low risk | Whole cohort assessed that was working during the epidemic. Exposure to SARS patients clearly defined |
| Blinding of participants and personnel (performance bias) All outcomes |
Low risk | Both the intervention and the outcome were assessed at the same time |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Both the intervention and the outcome were assessed with the same questionnaire at the same time |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | 90% HCW participated for adherence and for 77% of shifts more or less reliable info about doffing available |
| Selective reporting (reporting bias) | Unclear risk | Not clear which predictors of adherence or safe doffing were tested and negative |
| Other bias | Low risk | No indication of other bias |
| Methods | Randomised multiple-arm parallel group simulation study | |
| Participants | Nursing students volunteering; N =100 nursing students who had given written consent, 82% female, age 21 ± 1.2 years, 60% completed more than one study year, all had been taught PPE use, none had been involved with SARS patients | |
| Interventions | Ten different brands and types of PPE at the time of the study in use in Hong Kong hospitals; one type was a surgical gown and one the brand Barrierman, probably Tyvek by DuPont, the others were denoted as White A, White, Green, Y-HR-9, Yellow, Blue, Blue-9, B-NHK-9, B-HR-9. These were categorised into four categories: A: Good water repellency and penetration resistance but poor air permeability; B Good water repellency and air permeability but poor water penetration resistance; C: Surgical gown with poor water repellency and penetration resistance and fair air permeability; D Barrierman, with good water repellency, poor air permeability and fair water penetration resistance. Types A,B, C, and D were compared against each other |
|
| Outcomes | 1. Usability rated by the users as the mean of 5-point scales for: instructions, comfort, ease of donning and doffing, and satisfaction 2. Donning and doffing time/durations in minutes 3. Contamination after spraying fluorescent marker on the trunk and doffing of PPE, measured as mean number of contaminated spots that light up in UV-light |
|
| Notes | Hong Kong, China; Funded by Hong Kong Infection Control Nurses’ Association, Hong Kong Polytechnic University; no conflict of interest is reported in the article | |
| Risk of bias | ||
|---|---|---|
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Subjects were allocated a PPC using a random table page 91 |
| Allocation concealment (selection bias) | Unclear risk | Not reported and information asked from authors did not lead to a higher confidence in allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes |
Unclear risk | Not blinded; page 91 and discussion page 95 indicates that they knew what they were wearing, obviously, as PPC Type D was a one-piece construct, and they were asked to read manual for wearing. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes |
Unclear risk | Not reported if any data were missing |
| Selective reporting (reporting bias) | Unclear risk | Apparently all data reported |
| Other bias | Low risk | No indication of other bias |
| Methods | Randomised two-arm cross-over simulation study | |
| Participants | Clincians from Queen‘s Hospital, Kingston, ON, Canada volunteering to participate. N = 50; Powered Air Purifying Respirator (PAPR)-first N = 27, Age 34.3 ± 8.7 years, height 171.8 ± 8.1, weight 76.3 ± 16.7, Male 16/27, Anaesthesists 19/27, Prior PAPR training 15/27 E-RCP first N = 23, Age 36.8 ± 9.8, height 172.3 ± 7.6, Male 11/23, Anaesthesist 10/23, Prior PAPR training 18/23 Location: Canada |
|
| Interventions | Intervention: PPE with PAPR, consisting of Tyvek hood (3M), Bouffant hair cover, Spartan economy impact goggle, 3M air-mate breathing tube, 3M HEPA filter unit, N95 mask, 3 pair of gloves, Tyvek coverall with hood, 2 Tyvek boot covers, Astound impervious surgical gown. Doffing order: first gloves, turbo unit hose, hood, gown, second gloves, belt and battery, shoe covers, third gloves, wash hands, new gloves, coverall, second shoe covers, gloves, new gloves, goggles, hair cover, gloves, wash hands, new mask. Comparison: Enhanced respiratory and contact precautions (E-RCP) consisting of Bouffant hair cover, Spartan economy impact goggle, Face shield (Splash shield), N95 mask, 2 pairs of gloves, Astound impervious gown. Doffing order: outer gloves, gown, inner gloves, wash hands, new gloves, face shield, hair cover, goggles, mask, gloves, wash hands |
|
| Outcomes | 1. Number of participants with presence of contamination on base layer of clothes or skin. Contamination measured with fluorescein solution (5 ml in front of face shield and torso) plus invisible detection paste on forearms and palms of the hands; assessment after removing of outer layer by unblinded assessor with UV lamp; blinded evaluator then inspected all skin and clothes and measured area of contamination. Secondary outcomes were: contamination of inner layers of PAPR system, area size of contamination, number of donning/doffing violations; time required for donning and doffing. 2. Number of participants with donning or removal violation was defined as out of sequence removal, touching or tearing item of clothing, touching body part before hand washing. Used the Mainland-Gart test for the analysis of cross-over studies |
|
| Notes | Funding: Physicians‘ Services Incorporated Foundation and Clinical Teachers‘ Association of Queen‘s University; no Conflict of Interest declared | |
| Risk of bias | ||
|---|---|---|
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants randomised by coin tossing |
| Allocation concealment (selection bias) | Unclear risk | Once started, order was known, but unclear if subjects could still change groups and if there would be an interest to do so. |
| Blinding of participants and personnel (performance bias) All outcomes |
Unclear risk | Participants knew attire |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Evaluators blind for attire |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Apparently all data collected and usable |
| Selective reporting (reporting bias) | Unclear risk | Apparently all outcomes reported |
| Other bias | Low risk | No indication of other bias |
Characteristics of excluded studies
| Study | Reason for exclusion |
|---|---|
| Abrahamson 2006 | Uncontrolled study; one type of training only |
| Beam 2011 | No control group with an active intervention |
| Beam 2014 | Uncontrolled study; only one type of training in donning and doffing studied with video recordings |
| Bearman 2007 | Trial of universal gloving, not as part of full body PPE |
| Belkin 1991 | Commentary, not a primary study |
| Belkin 2000 | Commentary, not a primary study |
| Belkin 2005 | Description of standards and tests not a primary study |
| Borchert 2007 | Description of use of PPE in MHF outbreak, not a case control or cohort study |
| Buianov 1991 | Study compares two types of PPE for highly infectious diseases but does not measure contamination or infection as outcome, only physiological parameters (native speaker assessment AP) |
| Bunyan 2013 | Review not primary study |
| Casanova 2008 | Not a comparative study; only studied one method of doffing |
| Castle 2009 | Outcome only performance with PPE and not infection rate or adherence |
| Christian 2004 | Investigation of cluster of SARS infected HCW; not a case control or cohort study |
| Chughtai 2013 | Overview focusing on mask use only, not part of full body PPE |
| Clay 2015 | Simulation study; military HCWs; no control group |
| Coates 2000 | Outcome performance only not infection rates or adherence |
| Coca 2015 | Wrong type of participants, thermal manikin study |
| Colebunders 2004 | Description of MHF outbreak; not a case control or cohort study |
| Cooper 2005 | Simulation study, but of facial protection only, no full-body ppe involved |
| Dunn 2015 | Case study of spread of infection in one hospital; used in discussion section |
| Fischer 2015 | Not a primary study, literature review |
| Gozel 2013 | Description of use of PPE among HCW exposed to CCHF; not case-control or cohort study |
| Grelot 2015 | Measurement of thermal strain, no infection or contamination or compliance measured |
| Hendler 2000 | PPE versus no PPE; outcome performance only |
| Hersi 2015 | Not a primary study, rapid review |
| Hildwine 2006 | Annoucement of breathable virus resistant fabric; not a primary study |
| Ho 2003 | Descriptive study of SARS outbreak and HCWs use of PPE; not a case-control or cohort study |
| Ho 2004 | Compares consistent versus inconsistent use of PPE, not two different types |
| Hon 2008 | Evaluation of on-line PPE training; uncontrolled study, no comparison training |
| Hormbrey 1996 | Description of introduction of new clothing; no infection or adherence outcome |
| Jeffs 2007 | Description of control of MHF outbreak; not a case control or cohort study |
| Jinadatha 2015 | Wrong type of participants, investigation of disinfection on different PPE fabrics and components |
| Keane 1977 | Description of risk of HCW only; no evaluation of PPE safety |
| Kerstiens 1999 | Desription of Ebola outbreak; not case control or cohort study |
| Kim 2015 | No control group, HCWs infected with MERS CoV |
| Ko 2004 | Description of risk of EMT staff; no evaluation of PPE safety |
| Lai 2005 | Study of SARS IgG prevalence in HCWs who did not become sick, no PPE use measured |
| Lai 2011 | Simulation study of glove removal, no full-body PPE tested. |
| Lange 2005 | Letter to the editor; not primary study |
| Lau 2004 | Compares consistent versus inconsistent use of PPE, not two different types |
| Le 2004 | Compares consistent versus inconsistent use of PPE, not two different types |
| Lindsey 2012 | Test respiratory protection only; not part of full-body PPE |
| Lindsley 2014 | Tests respiratory protection only; not part of full-body PPE |
| Liu 2009 | Compares consistent versus inconsistent use of PPE, not two different types |
| Loeb 2004 | Compares consistent versus inconsistent use of PPE, not two different types |
| Low 2005 | A review of SARS and HCW; not a primary study |
| Lowe 2014 | Description of PPE use only; no adherence or infection outcomes |
| Lu 2006 | Comparison of viral load in patients infected outside and inside hospital; comparison is with no PPE |
| Luo 2011 | Simulation study of one Tyvek® (duPont) suit only, no comparison suit or no comparison doffing method |
| Ma 2004 | Retrospective case-control study about PPE for SARS, compares consistent versus inconsistent use not two types |
| Malik 2006 | Participants not exposed to highly infectious diseases |
| Marklund 2002 | Description of Ebola patient transportation; not an intervention study |
| Matanock 2014 | Description of risk of infection of HCW compared to general population; no evaluation of PPE |
| Mehtar 2015 | No control group, two IPC training courses |
| Minnich 2003 | Description of ambulance adaptation for transport of highly infected patients; not evaluation or intervention study |
| Mollura 2015 | Review; EVD within radiology wards and on imaging equipment |
| Moore 2005 | Review not intervention study |
| Morgan 2009 | Review of adverse effects of contact precautions |
| Muyembe-Tamfum 1999 | Description of Ebola outbreak; not case-control or cohort study |
| Nishiura 2005 | Compares consistent versus inconsistent use of PPE, not two different types |
| Northington 2007 | No comparison group; only one type of education with follow-up |
| Nyenswah 2015 | Case study of EVD cluster including HCWs, but insufficient information on PPE to draw any conclusions |
| Ofner 2003 | SARS case series only; no healthy controls; not case control or cohort study |
| Ofner-Agostini 2006 | SARS case series only; no healthy controls; not case control or cohort study |
| Ogendo 2008 | Eye protection only; not part of full-body PPE |
| Ong 2013 | No exposure to highly infectious diseases |
| Park 2004 | Compares consistent versus inconsistent use of PPE, not two different types |
| Pei 2006 | Compares consistent versus inconsistent use of PPE, not two different types |
| Ragazzoni 2015 | No control group, virtual reality simulation training study |
| Ransjo 1979 | No exposure to highly infectious diseases |
| Reynolds 2006 | Case control study evaluating SARS risk in HCWs in Vietnam but no inclusion of PPE use |
| Russell 2015 | No control group, no outcome, before/after summary card |
| Scales 2003 | Compares consistent versus inconsistent use of PPE, not two different types |
| Schumacher 2010 | Comparison is no PPE; outcome is performance time only |
| Seto 2003 | Compares consistent versus inconsistent use of PPE, not two different types |
| Shao 2015 | Not a primary study, Chinese review |
| Sorensen 2008 | No exposure to highly infectious diseases |
| Tartari 2015 | No control group, infection control readiness checklist (from 45 countries), no outcome |
| Teleman 2004 | Compares consistent versus inconsistent use of PPE, not two different types |
| Tomas 2015 | No comparison used only description of contamination in a simulation study. |
| Torres 2015 | Not a primary study, literature review |
| West 2014 | Not a primary study but a commentary |
| Yin 2004 | Case-control study of use of PPE for SARS, not comparing two different types of PPE |
| Zellmer 2015 | No control group, checklist for removing PPE |
| Zhou 2003 | Follow-up of HCWs exposed to SARS and their PPE and protection measures, not comparative study |
DATA AND ANALYSES
Comparison 1.
PAPR versus E-RCP Attire
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any contamination | 1 | Risk Ratio (M-H, Random, 95% CI) | Totals not selected | |
| 2 Contamination > 1 cm | 1 | Risk Ratio (M-H, Random, 95% CI) | Totals not selected | |
| 3 Contamination area | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Donning noncompliance | 1 | Risk Ratio (M-H, Random, 95% CI) | Totals not selected | |
| 5 Doffing noncompliance | 1 | Risk Ratio (M-H, Random, 95% CI) | Totals not selected | |
| 6 Donning time | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Doffing time | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Analysis 1.1.
Comparison 1 PAPR versus E-RCP Attire, Outcome 1 Any contamination.
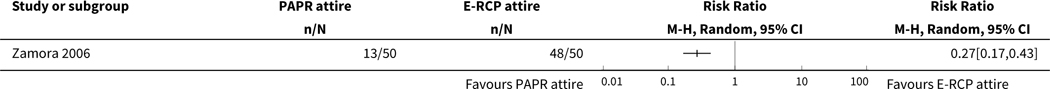
|
Analysis 1.2.
Comparison 1 PAPR versus E-RCP Attire, Outcome 2 Contamination > 1 cm.
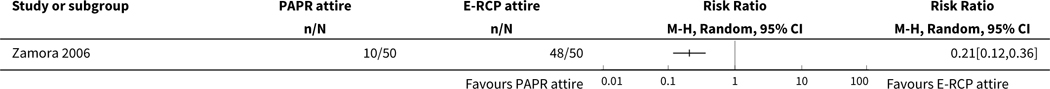
|
Analysis 1.3.
Comparison 1 PAPR versus E-RCP Attire, Outcome 3 Contamination area.
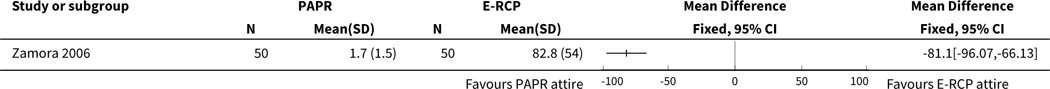
|
Analysis 1.4.
Comparison 1 PAPR versus E-RCP Attire, Outcome 4 Donning noncompliance.
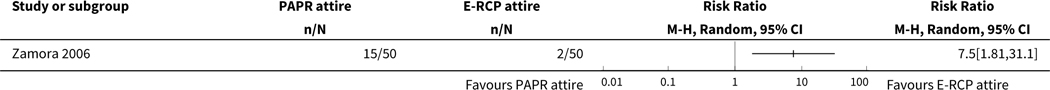
|
Analysis 1.5.
Comparison 1 PAPR versus E-RCP Attire, Outcome 5 Doffing noncompliance.
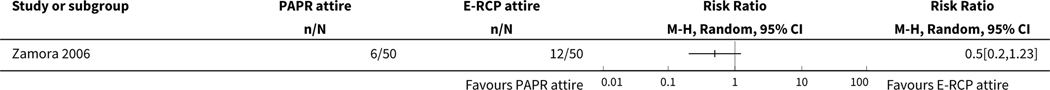
|
Analysis 1.6.
Comparison 1 PAPR versus E-RCP Attire, Outcome 6 Donning time.
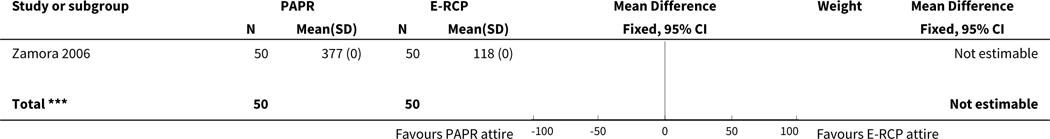
|
|
Analysis 1.7.
Comparison 1 PAPR versus E-RCP Attire, Outcome 7 Doffing time.
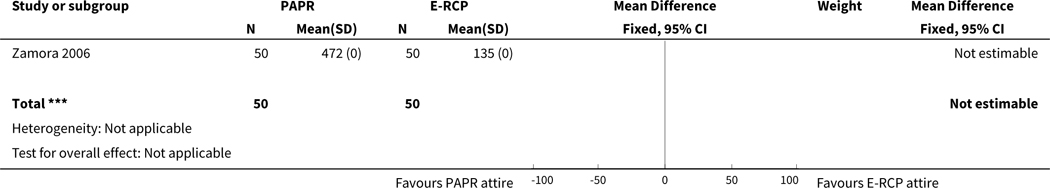
|
Comparison 2.
Four types of PPE attire compared
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 A vs B Contamination, mean number of spots | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Face type A vs type B | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Trunk type A vs type B | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Neck type A vs type B | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Foot type A vs type B | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 Palm type A vs type B | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 A vs B Usability score (1–5) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 A vs B Donning time | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 A vs B Doffing time | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 A vs D Contamination, mean number of spots | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Face type A vs type D | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Trunk type A vs type D | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Neck type A vs type D | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.4 Foot type A vs type D | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.5 Palm type A vs type D | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 A vs D Usability score (1–5) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7 A vs D Donning time | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8 A vs D Doffing time | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Analysis 2.1.
Comparison 2 Four types of PPE attire compared, Outcome 1 A vs B Contamination, mean number of spots.
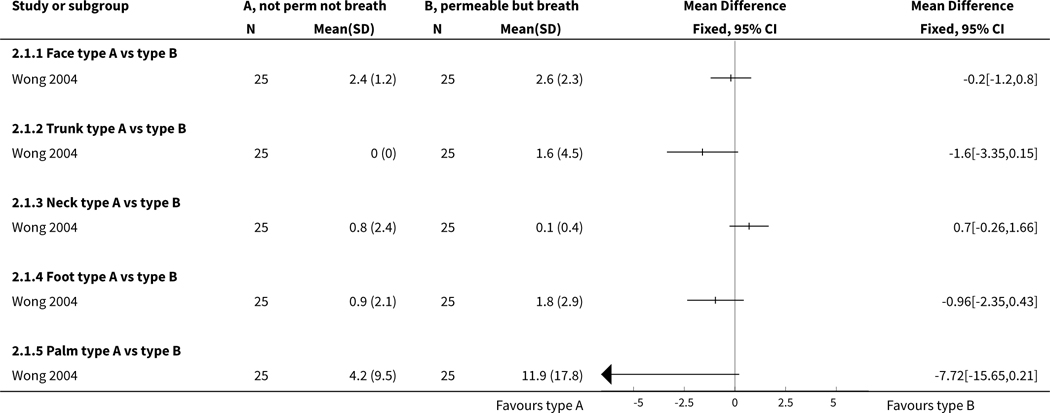
|
Analysis 2.2.
Comparison 2 Four types of PPE attire compared, Outcome 2 A vs B Usability score (1–5).
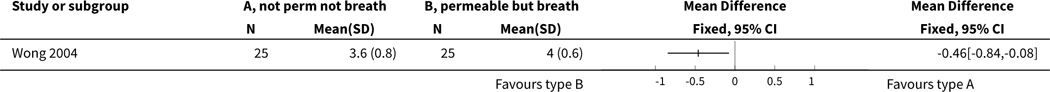
|
Analysis 2.3.
Comparison 2 Four types of PPE attire compared, Outcome 3 A vs B Donning time.
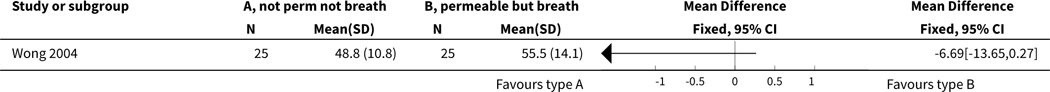
|
Analysis 2.4.
Comparison 2 Four types of PPE attire compared, Outcome 4 A vs B Doffing time.
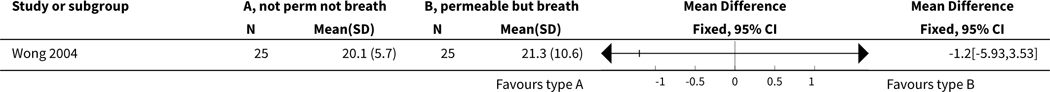
|
Analysis 2.5.
Comparison 2 Four types of PPE attire compared, Outcome 5 A vs D Contamination, mean number of spots.
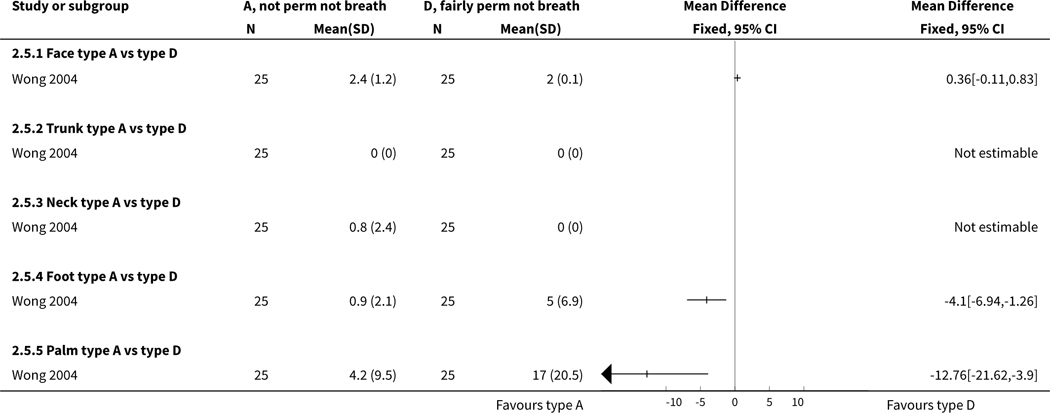
|
Analysis 2.6.
Comparison 2 Four types of PPE attire compared, Outcome 6 A vs D Usability score (1–5).
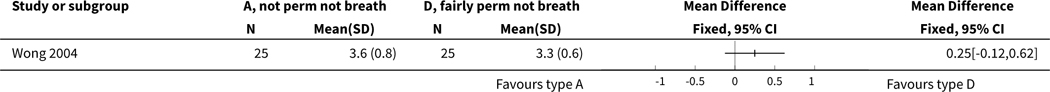
|
Analysis 2.7.
Comparison 2 Four types of PPE attire compared, Outcome 7 A vs D Donning time.
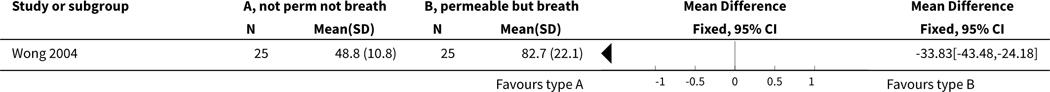
|
Analysis 2.8.
Comparison 2 Four types of PPE attire compared, Outcome 8 A vs D Doffing time.
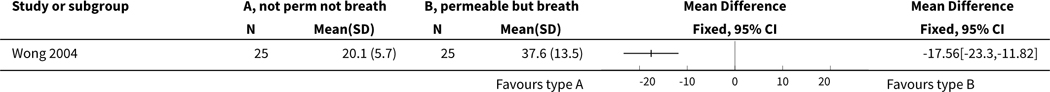
|
Comparison 3.
Formal versus local available attire
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Contamination | 1 | Risk Ratio (M-H, Fixed, 95% CI) | Totals not selected |
Analysis 3.1.
Comparison 3 Formal versus local available attire, Outcome 1 Contamination.
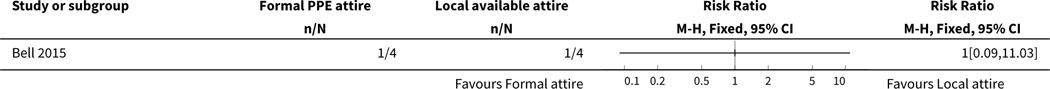
|
Comparison 4.
Gown versus apron
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Contamination with marker; individual doffing | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 small patches | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 large patches | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 hand | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 shoe | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 underwear | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.6 environment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Contamination with marker; CDC doffing | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 small patches | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 large patches | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 hand | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 shoe | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 underwear | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.6 environment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Analysis 4.1.
Comparison 4 Gown versus apron, Outcome 1 Contamination with marker; individual doffing.
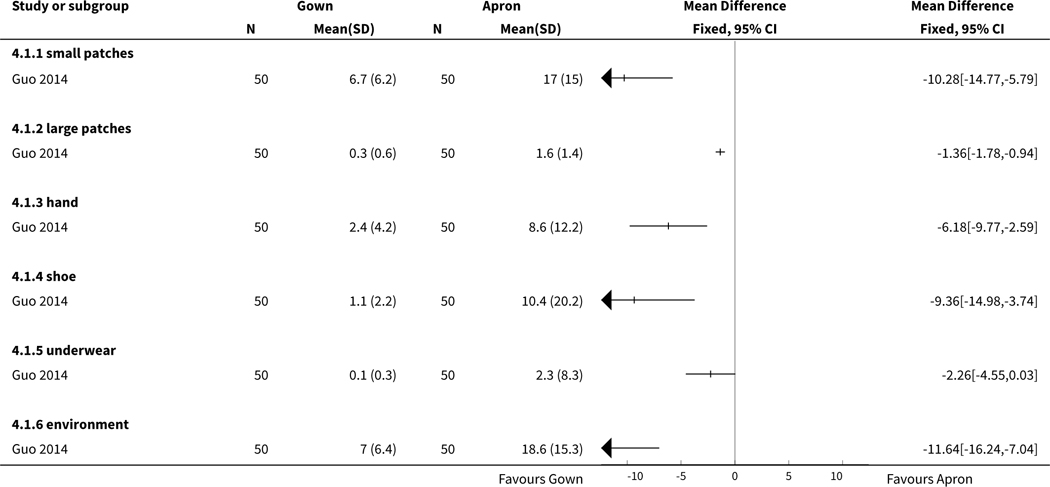
|
Analysis 4.2.
Comparison 4 Gown versus apron, Outcome 2 Contamination with marker; CDC doffing.
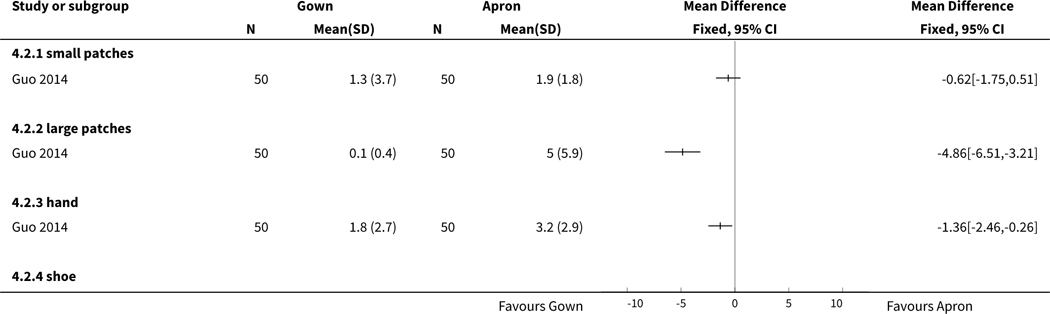
|
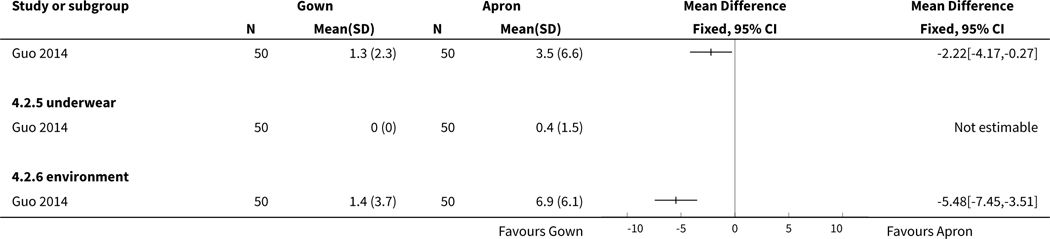
|
Comparison 5.
Doffing with double gloves vs doffing with single gloves
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Contamination: virus detected | 1 | Risk Ratio (M-H, Fixed, 95% CI) | Totals not selected | |
| 1.1 All body parts | 1 | Risk Ratio (M-H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Face | 1 | Risk Ratio (M-H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Shirt | 1 | Risk Ratio (M-H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Pants | 1 | Risk Ratio (M-H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Contamination: virus quantity | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Dominant hand | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Non-dominant hand | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Face | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Shirt | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 Pants | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Non-compliance: any error | 1 | Risk Ratio (M-H, Fixed, 95% CI) | Totals not selected |
Analysis 5.1.
Comparison 5 Doffing with double gloves vs doffing with single gloves, Outcome 1 Contamination: virus detected.
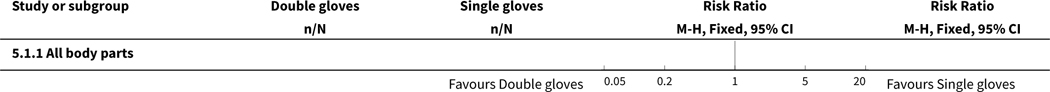
|
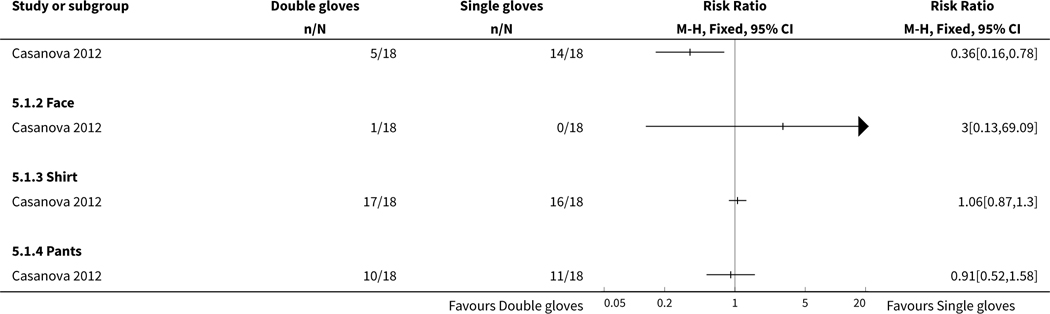
|
Analysis 5.2.
Comparison 5 Doffing with double gloves vs doffing with single gloves, Outcome 2 Contamination: virus quantity.
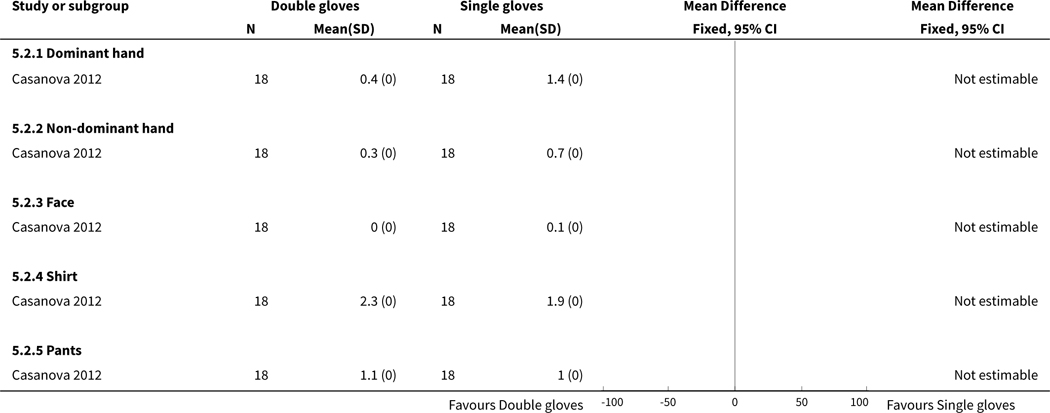
|
Analysis 5.3.
Comparison 5 Doffing with double gloves vs doffing with single gloves, Outcome 3 Non-compliance: any error.
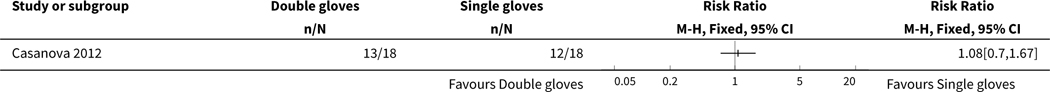
|
Comparison 6.
CDC versus individual doffing
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gown; Contamination with fluor marker | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 small patch | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 large patch | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 hand | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 shoe | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 underwear | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.6 environment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Apron; Contamination with fluor marker | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 small patch | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 large patch | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 hand | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 shoe | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 underwear | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.6 environment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Analysis 6.1.
Comparison 6 CDC versus individual doffing, Outcome 1 Gown; Contamination with fluor marker.
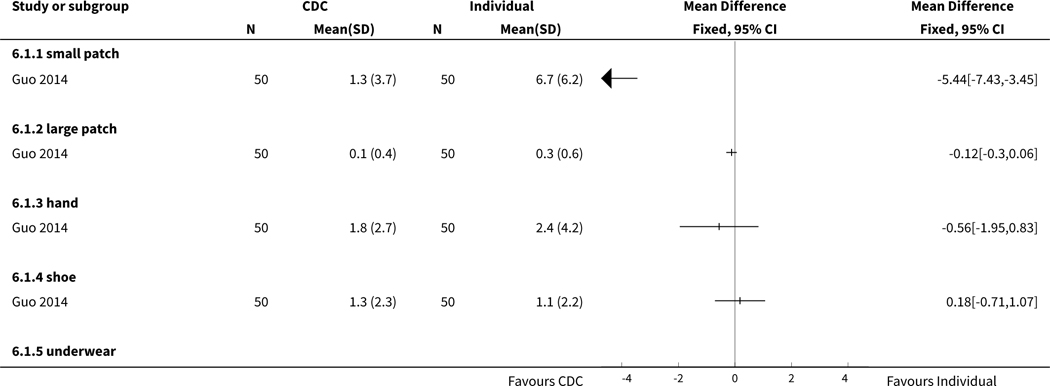
|
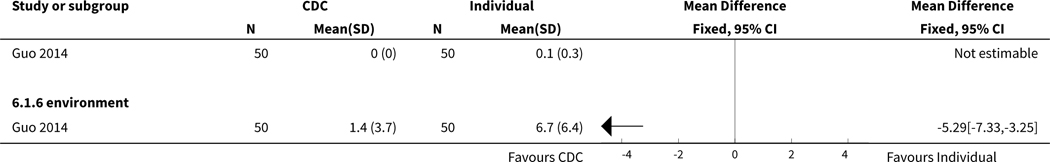
|
Analysis 6.2.
Comparison 6 CDC versus individual doffing, Outcome 2 Apron; Contamination with fluor marker.
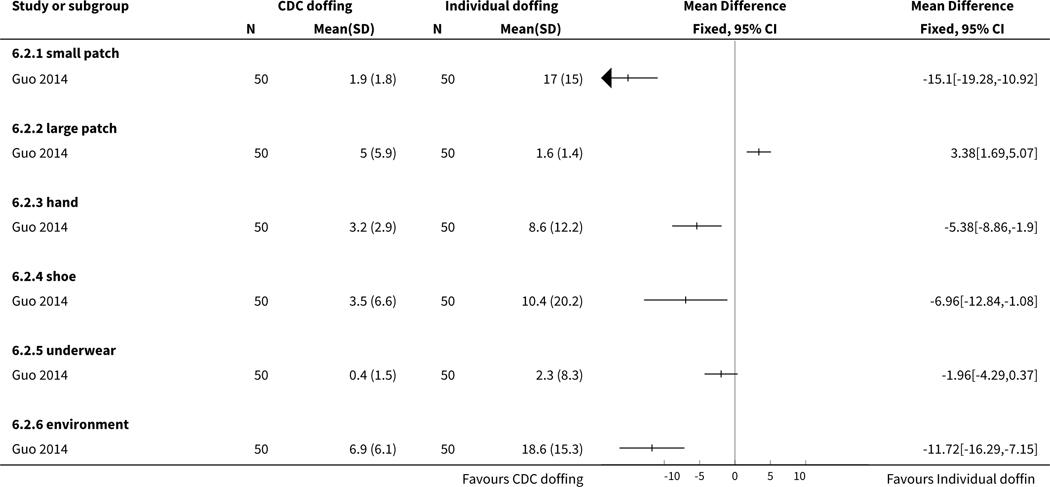
|
Comparison 7.
Active training in PPE use versus passive training
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Noncompliance with PPE | 1 | Odds Ratio (Fixed, 95% CI) | Totals not selected |
Analysis 7.1.
Comparison 7 Active training in PPE use versus passive training, Outcome 1 Noncompliance with PPE.
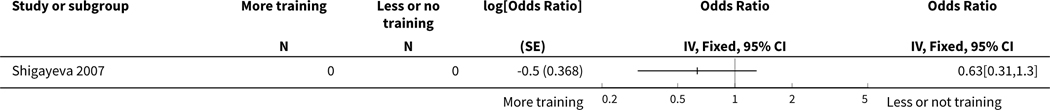
|
Comparison 8.
Active training in PPE doffing versus passive training
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Noncompliance doffing protocol | 1 | Odds Ratio (Fixed, 95% CI) | Totals not selected |
Analysis 8.1.
Comparison 8 Active training in PPE doffing versus passive training, Outcome 1 Noncompliance doffing protocol.
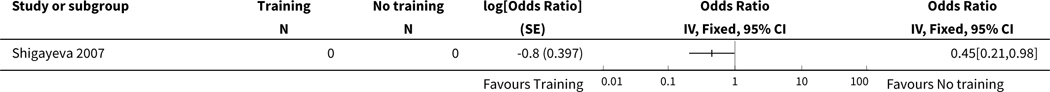
|
Comparison 9.
Donning and doffing with instructions versus without instructions
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Persons with one or more errors | 1 | 120 | Risk Ratio (M-H, Random, 95% CI) | 0.31 [0.11, 0.93] |
| 1.1 Basic PPE | 1 | 60 | Risk Ratio (M-H, Random, 95% CI) | 0.15 [0.04, 0.62] |
| 1.2 Enhanced PPE | 1 | 60 | Risk Ratio (M-H, Random, 95% CI) | 0.47 [0.22, 0.98] |
| 2 Mean errors | 1 | 120 | Mean Difference (IV, Random, 95% CI) | −0.89 [−1.36, −0.41] |
| 2.1 Basic PPE | 1 | 60 | Mean Difference (IV, Random, 95% CI) | −0.70 [−1.15, −0.25] |
| 2.2 Enhanced PPE | 1 | 60 | Mean Difference (IV, Random, 95% CI) | −1.2 [−1.87, −0.53] |
Analysis 9.1.
Comparison 9 Donning and doffing with instructions versus without instructions, Outcome 1 Persons with one or more errors.
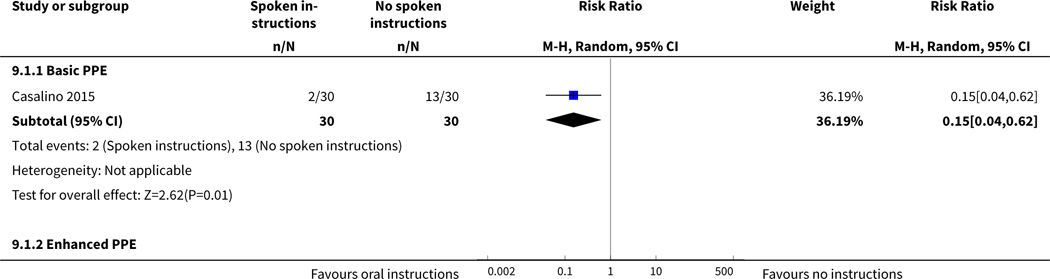
|
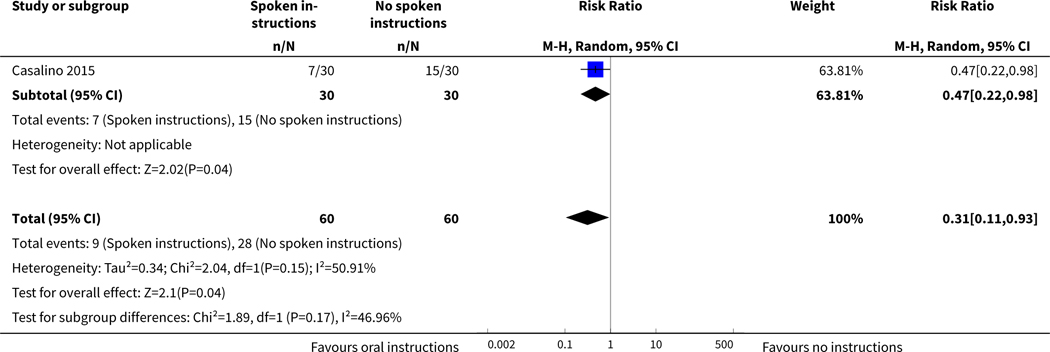
|
Analysis 9.2.
Comparison 9 Donning and doffing with instructions versus without instructions, Outcome 2 Mean errors.
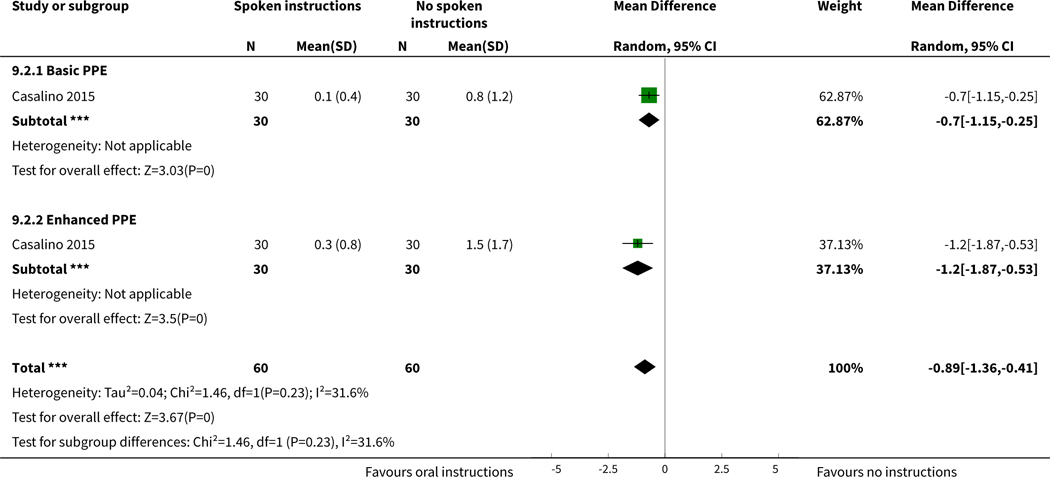
|
Comparison 10.
Computer simulation vs no simulation
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of errors while donning | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Number of errors while doffing | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Analysis 10.1.
Comparison 10 Computer simulation vs no simulation, Outcome 1 Number of errors while donning.
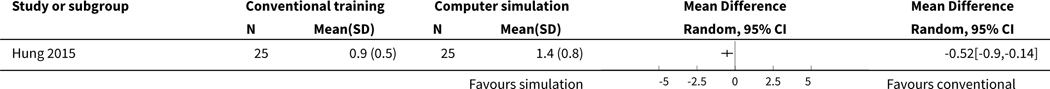
|
Analysis 10.2.
Comparison 10 Computer simulation vs no simulation, Outcome 2 Number of errors while doffing.
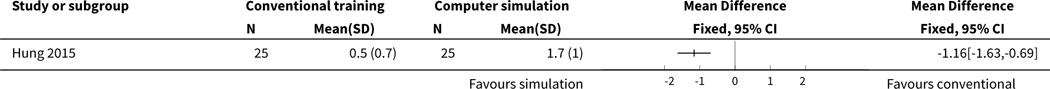
|
APPENDICES
Appendix 1. The basis for the assumed risk is the control group risk
#1
“Protective Clothing”[Mesh] OR gown*[tw] OR coverall*[tw] OR “protective layer”[tw] OR “protective layers”[tw] OR “surgical toga”[tw] OR apron*[tw] OR “smock”[tw] OR “smocks”[tw] OR “hazmat suit”[tw] OR (hazmat[tw] AND suit[tw]) OR “Gloves, Protective”[Mesh] OR “glove”[tw] OR “gloves”[tw] OR “Respiratory Protective Devices”[Mesh] OR “Masks”[Mesh] OR “mask”[tw] OR “masks”[tw] OR “air-purifying respirator”[tw] OR “PAPR”[tw] OR “enhanced respiratory and contact precautions” OR “E-RCP”[tw] OR “respiratory protection”[tw] OR “transparent panel”[tw] OR “surgical mask”[tw] OR “surgical masks”[tw] OR “filtering face piece”[tw] OR “filtering facepiece”[tw] OR “Eye Protective Devices”[Mesh] OR goggle*[tw] OR “visor”[tw] OR “facial protection equipment”[tw] OR “safety glass”[tw] OR “safety glasses”[tw] OR “safety spectacles”[tw] OR “personal protective equipment”[tw] OR “PPE”[tw] OR “protective equipment”[tw] OR overshoe*[tw] OR “shoe cover”[tw] OR “shoe covers”[tw] OR “rubber boot”[tw] OR “rubber boots”[tw] OR “head cover”[tw] OR “head covering”[tw] OR “face shield”[tw] OR “face shields”[tw] OR “surgical hood”[tw] OR “hood”[tw] OR “Equipment Contamination/prevention and control”[Mesh] OR “Infection Control”[Mesh] OR “infection control”[tiab] OR “gloving”[tw] OR “donning”[tw] OR “doffing”[tw]
#2
“Communicable Diseases”[Mesh] OR “infectious disease”[tiab] OR “infectious diseases”[tiab] OR “Disease Transmission, Infectious”[Mesh] OR “disease transmission”[tw] OR “Infectious Disease Transmission, Patient-to-Professional”[Mesh] OR “infection control precautions”[tw] OR “human-to-human transmission”[tw] OR “parenteral transmission”[tw] OR “Virus Diseases/prevention and control”[Mesh] OR “viral disease”[tw] OR “viral diseases”[tw] OR “Bacterial Infections/prevention and control”[Mesh] OR “bacterial infection”[tw] OR “filovirus”[tw] OR “Ebolavirus”[Mesh] OR “Hemorrhagic Fever, Ebola”[Mesh] OR “Ebola”[tw] OR “Marburg virus”[tw] OR “Lassa virus”[tw] OR “haemorrhagic fever”[tw] OR “HIV Infections/prevention and control”[Mesh] OR “HIV”[ti] OR “hiv infection”[tiab] OR “hiv transmission”[tw] OR “Influenza, Human/prevention and control”[Mesh] OR “SARS Virus”[Mesh] OR “Severe Acute Respiratory Syndrome Virus”[tw] OR “SARS”[tw] OR “MERS”[tw] OR “respiratory infection”[tw] OR “Influenza, Human/prevention and control”[Mesh] OR “influenza”[tiab] OR “Tuberculosis/prevention and control”[Mesh] OR “tuberculosis”[tiab] OR “Hepatitis A”[Mesh] OR “hepatitis a”[ti] OR “Hepatitis B/prevention and control”[Mesh] OR “hepatitis b”[ti] OR “Hepatitis C/transmission”[Mesh] OR “hepatitis c”[ti] OR “bioterrorism”[tw] OR “aerosol-generating procedure”[tw] OR “Cross Infection”[Mesh] OR “bacterial contamination”[tw] OR “microbial contamination”[tw] OR “self-contamination”[tw] OR “decontamination”[tw] OR “surface decontamination”[tw] OR “skin decontamination”[tw]
#3
“Health Personnel”[Mesh] OR “Personnel, Hospital”[Mesh] OR “health care worker”[tw] OR “health care workers”[tw] OR “health care personnel”[tw] OR “health personnel”[tw] OR “health-personnel”[tw] OR “health provider”[tw] OR “health providers”[tw] OR “health care provider”[tw] OR “health care providers”[tw] OR “medical staff”[tw] OR “medical personnel”[tw]OR “medical professional”[tw] OR “medical worker”[tw] OR “medical workers”[tw] OR “dental personnel”[tw] OR “dental staff”[tw] OR “Dentists”[Mesh] OR “dentist”[tw] OR “dentists”[tw] OR “dental assistant”[tw] OR “dental assistants”[tw] OR “Dental Assistants”[Mesh] OR “nursing staff”[tw] OR “Nurses”[Mesh] OR “nurse”[tw] OR “nurses”[tw] OR “nursing assistant”[tw] OR “nursing assistants”[tw] OR “Nurses’ Aides”[Mesh] OR “Nurse Midwives”[Mesh] OR “midwife”[tw] OR “midwives”[tw] OR “military-medical personnel”[tw] OR “Physicians”[Mesh] OR “physician”[tw] OR “physicians”[tw] OR “emergency medical services”[tw] OR “Emergency Medical Services”[MeSH] OR “transporting patients”[tw] OR “patient transport”[tw] OR “Ambulances”[Mesh] OR “Allied Health Personnel”[Mesh] OR paramedic[tw] OR paramedics[tw] OR paramedical personnel[tw] OR “Burial”[Mesh] OR burial staff OR cleaning workers[tw] OR cleaner work OR cleaner[tw] OR cleaners[tw]
#4
(#1 AND #2 AND #3)
Appendix 2. Embase search strategy
#7
#6 NOT [medline]/lim) (646)
#6
#5 AND [embase]/lim (2,227)
#5
#4 AND [humans]/lim (5,270)
#4
#1 AND #2 AND #3 (5,675)
#3
‘communicable disease’/de OR “infectious disease”:ab,ti OR ‘disease transmission’/de OR “disease transmission” OR “infection control precautions” OR “human-to-human transmission” OR “parenteral transmission” OR ‘virus infection’/de OR “viral disease”:ab,ti OR ‘bacterial infection’/de OR “bacterial infection”:ab,ti OR “filovirus” OR ‘ebola virus’/de OR ‘hemorrhagic fever ebola’/de OR “ebola” OR “marburg virus” OR “lassa virus” OR “haemorrhagic fever” OR ‘sars coronavirus’/de OR “Severe Acute Respiratory Syndrome Virus” OR “SARS” OR “MERS” OR “bioterrorism” OR ‘cross infection’/de OR “bacterial contamination” OR “microbial contamination” OR “self-contamination” OR “decontamination” OR “surface decontamination” OR “skin decontamination” (323,524)
#2
‘health care personnel’/de OR ‘hospital personnel’/de OR “health care worker” OR “health care workers” OR “health care personnel” OR “health personnel” OR “health-personnel” OR “health provider” OR “health providers” OR “health care provider” OR “health care providers” OR “medical staff” OR “medical personnel” OR “medical professional” OR “medical worker” OR “medical workers” OR “dental personnel” OR “dental staff” OR “dentist” OR “dentists” OR “dental assistant” OR “dental assistants” OR “nursing staff” OR ‘nurses’/de OR “nurse” OR “nurses” OR “nursing assistant” OR “nursing assistants” OR ‘nursing assistant’/de OR ‘nurse midwife’/de OR “midwife” OR “midwives” OR “military-medical personnel” OR ‘physician’/de OR “physician” OR “physicians” OR “emergency medical services” OR “transporting patients” OR “patient transport” OR ‘ambulance’/de OR ‘paramedical personnel’/de OR “paramedical personnel” OR paramedic OR paramedics OR ‘posthumous care’/de OR “burial staff” OR “cleaning workers” OR “cleaner work” OR cleaner OR cleaners (1,287,399)
#1
‘protective clothing’/de OR gown* OR coverall* OR “protective layer” OR “protective layers” OR “surgical toga” OR apron* OR smock OR smocks OR “hazmat suit” OR (hazmat AND suit) OR glove OR gloves OR ‘respiratory protective devices’/de OR ‘mask’/de OR mask OR “air-purifying respirator” OR “PAPR” OR “enhanced respiratory and contact precautions” OR “E-RCP” OR “respiratory protection” OR “transparent panel” OR “surgical mask” OR “surgical masks” OR “filtering face piece” OR “filtering facepiece” OR ‘eye protective device’/de OR goggle* OR visor OR “facial protection equipment” OR “safety glass” OR “safety glasses” OR “safety spectacles” OR “personal protective equipment” OR “PPE” OR “protective equipment” OR overshoe* OR “shoe cover” OR “shoe covers” OR “rubber boot” OR “rubber boots” OR “head cover” OR “head covering” OR “face shield” OR “face shields” OR “surgical hood” OR hood OR ‘medical device contamination’/de OR ‘infection control’/de OR ‘infection control’:ab,ti OR gloving OR donning OR doffing (160,118)
Appendix 3. Central search strategy
#1 MeSH descriptor: [Health Personnel] explode all trees (5912)
#2 MeSH descriptor: [Personnel, Hospital] explode all trees (797)
#3 MeSH descriptor: [Dentists] explode all trees (66)
#4 MeSH descriptor: [Dental Assistants] explode all trees (12)
#5 MeSH descriptor: [Nurses] explode all trees (1004)
#6 MeSH descriptor: [Nurses’ Aides] explode all trees (55)
#7 MeSH descriptor: [Nurse Midwives] explode all trees (99)
#8 MeSH descriptor: [Physicians] explode all trees (1293)
#9 MeSH descriptor: [Emergency Medical Services] explode all trees (3006)
#10 MeSH descriptor: [Ambulances] explode all trees (131)
#11 MeSH descriptor: [Allied Health Personnel] explode all trees (754)
#12 MeSH descriptor: [Burial] explode all trees (0)
#13
“health care worker” or “health care personnel” or “health personnel” or “health provider” or “health care provider” or “medical staff” or “medical personnel” or “medical professional” or “medical worker” or “dental personnel” or “dental staff” or “dentist” or “dental assistant” or “nursing staff” or “nurse” or “nursing assistant” or “midwife” or “midwives” or “military-medical personnel” or “physician” or “emergency medical services” or “transporting patients” or “patient transport” or “paramedic” or “paramedical personnel” (Word variations have been searched) (55128)
#14
#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 (57838)
#15 MeSH descriptor: [Communicable Diseases] explode all trees (113)
#16 MeSH descriptor: [Disease Transmission, Infectious] explode all trees (783)
#17 MeSH descriptor: [Infectious Disease Transmission, Patient-to-Professional] explode all trees (56)
#18 MeSH descriptor: [Virus Diseases] explode all trees and with qualifier(s):[Prevention & control - PC] (5886)
#19 MeSH descriptor: [Bacterial Infections] explode all trees and with qualifier(s):[Prevention & control - PC] (3740)
#20 MeSH descriptor: [Ebolavirus] explode all trees (2)
#21 MeSH descriptor: [Hemorrhagic Fever, Ebola] explode all trees (3)
#22 MeSH descriptor: [SARS Virus] explode all trees (13)
#23 MeSH descriptor: [Cross Infection] explode all trees (1360)
#24 “infectious disease”:ti,ab,kw (Word variations have been searched) (1692)
#25 “disease transmission” or “infection control precautions” or “human-to-human transmission” (Word variations have been searched) (942)
#26 “parenteral transmission” or “viral disease” or “bacterial infection” (Word variations have been searched) (5011)
#27 “filovirus” or “Ebola” or “Marburg virus” or “Lassa virus” or “haemorrhagic fever” (Word variations have been searched) (159)
#28 “Severe Acute Respiratory Syndrome Virus” or “SARS” or “MERS” (Word variations have been searched) (115)
#29 “respiratory infection” (Word variations have been searched) (1667)
#30 “bioterrorism” (Word variations have been searched) (33)
#31
“aerosol-generating procedure” or “bacterial contamination” or “microbial contamination” or “self-contamination” or “decontamination” or “surface decontamination” or “skin decontamination”
(Word variations have been searched) (883)
#32 #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 (18013)
#33 MeSH descriptor: [Protective Clothing] explode all trees (424)
#34 MeSH descriptor: [Gloves, Protective] explode all trees (179)
#35 MeSH descriptor: [Respiratory Protective Devices] explode all trees (44)
#36 MeSH descriptor: [Masks] explode all trees (1154)
#37 MeSH descriptor: [Eye Protective Devices] explode all trees (44)
#38 MeSH descriptor: [Equipment Contamination] explode all trees and with qualifier(s): [Prevention & control - PC] (178)
#39 MeSH descriptor: [Infection Control] explode all trees (1205)
#40 gown* or coverall* or “protective layer” or “surgical toga” or apron* or “smock” (Word variations have been searched) (188)
#41 “hazmat suit” or (hazmat and suit) (Word variations have been searched) (0)
#42
“glove” or “mask” or “air-purifying respirator” or “PAPR” or “enhanced respiratory and contact precautions” or “E-RCP” or “respiratory protection” or “transparent panel” or “surgical mask” or “filtering face piece” or goggle* or “visor” or “facial protection equipment” or “safety glass” or “safety glasses” or “safety spectacles” or “personal protective equipment” or “PPE” or “protective equipment” or overshoe* or “shoe cover” or “shoe covers” or “rubber boot” or “head cover” or “head covering” or “face shield” or “surgical hood” or “hood” (Word variations have been searched) (16557)
#43 “gloving” or “donning” or “doffing” (Word variations have been searched) (1460)
#44 “infection control”:ti,ab,kw (Word variations have been searched) (1050)
#45 #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 (19022)
#46 #14 and #32 and #45 (651)
#47 #46 in trials (152)
Appendix 4. CINAHL search strategy
S5 S4 MEDLINE records excluded (878)
S4 (S1 AND S2 AND S3) (2,584)
S3
(MH “Communicable Diseases”) OR (TI “infectious disease”) OR (AB “infectious disease”) OR (MH “Disease Transmission) OR TX “disease transmission” OR (MH “Disease Transmission, Patient-to-Professional”) OR TX “infection control precautions” OR TX “human-to-human transmission” OR TX “parenteral transmission” OR (MH “Virus Diseases/PC”) OR TX “viral disease” OR TX “viral diseases” OR TX “bacterial infection” OR (MH “Bacterial infection/PC”) OR TX “filovirus” OR TX “ebolavirus” OR (MH “Hemorrhagic Fever, Ebola”) OR TX “ebola” OR TX “marburg virus” OR TX “lassa virus” OR TX “haemorrhagic fever” OR (MH “SARS Virus”) OR TX “severe acute respiratory syndrome virus” OR TX “SARS” OR TX “MERS” OR TX “respiratory infection” OR TX “bioterrorism” OR TX “aerosol-generating procedure” OR (MH “Cross Infection”) OR TX “bacterial contamination” OR TX “microbial contamination” OR TX “self-contamination” OR TX “decontamination” OR TX “surface decontamination” OR TX “skin decontamination” (37,937)
S2
(MH Protective Clothing) OR TX gown* OR TX coverall* OR TX “protective layer” OR TX “protective layers” OR TX “surgical toga” OR TX apron* OR TX “smock” OR TX “smocks” OR TX “hazmat suit” OR TX (hazmat AND suit) OR (MH “gloves protective”) OR TX glove OR TX gloves OR (MH “Respiratory Protective Devices”) OR (MH “Masks”) OR TX mask OR TX masks OR TX “air-purifying respirator” OR TX “PAPR” OR TX “enhanced respiratory and contact precautions” OR TX “E-RCP” OR TX “respiratory protection” OR TX “transparent panel” OR TX “surgical mask” OR TX “surgical masks” OR TX “filtering face piece” OR TX “filtering facepiece” OR (MH “Eye Protective Devices”) OR TX goggle* OR TX “visor” OR TX “facial protection equipment” OR TX “safety glass” OR TX “safety glasses” OR TX “safety spectacles” OR TX “personal protective equipment” OR TX “PPE” OR TX “protective equipment” OR TX overshoe* OR TX “shoe cover” OR TX “shoe covers” OR TX “rubber boot” OR TX “rubber boots” OR TX “head cover” OR TX “head covering” OR TX “face shield” OR TX “face shields” OR TX “surgical hood” OR TX “hood” OR (MH “Equipment Contamination/PC”) OR (MH “Infection Control”) OR (TI “infection control”) OR (AB “infection control”) OR TX “gloving” OR TX “donning” OR TX “doffing” (28,554)
S1
(MH “Health Personnel”) OR TX health care workers OR TX health care personnel OR TX health personnel OR TX health-personnel OR TX health providers OR TX health care providers OR TX medical staff OR TX medical personnel OR TX medical professional OR TX medical workers OR TX dental personnel OR TX dental staff OR (MH “Dentists”) OR TX dentist OR TX dental assistant OR TX nursing staff OR (MH “Nurses”) OR TX nurse OR TX nursing assistant OR (MH “Allied Health Personnel” OR (MH “Midwives”) OR TX nurse midwife OR TX nurse midwives OR TX military-medical personnel OR (MH “Physicians”) OR TX physician OR TX emergency medical services OR (MH “Emergency Medical Services”) OR TX transporting patients OR TX patient transport OR (MH “Ambulance”) OR (MH “Allied Health Personnel”) OR TX paramedic OR TX paramedical personnel OR (MH “Burial”) OR TX burial staff OR TX cleaning worker OR TX cleaner work OR TX cleaner OR TX cleaners (498,394)
Appendix 5. OSH-update search strategy
| Step: | Hits: | Strategy: |
|---|---|---|
| #1 | 32657 | GW{protective clothing OR gown* OR coverall* OR protective layer* OR surgical toga* OR apron* OR smock* OR hazmat suit* OR (hazmat AND suit) OR glove* OR respiratory protective device* OR mask OR masks OR air purifying respirator* OR ‘PAPR’ OR ‘enhanced respiratory and contact precautions’ OR ‘E-RCP’ OR respiratory protection OR transparent panel* OR surgical mask* OR filtering face piece OR eye protective device* OR goggle* OR visor OR facial protective equipment OR safety glass* OR safety spectacles OR personal protective equipment OR ‘PPE’ OR protective equipment OR overshoe* OR shoe cover* OR rubber boot* OR head cover* OR face shield* OR surgical hood OR hood OR equipment contamination OR infection control OR gloving OR donning OR doffing} |
| #2 | 11286 | GW{communicable disease* OR infectious disease* OR disease transmission OR infection control precautions OR human-to-human transmission OR parenteral transmission OR viral disease* OR bacterial infection* OR filovirus OR Ebolavirus OR hemorrhagic fever OR Ebola OR Marburg virus OR Lassa virus OR SARS virus OR severe acute respiratory syndrome virus OR ‘SARS’ OR ‘MERS’ OR respiratory infection* OR bioterrorism OR aerosol-generating procedure OR cross infection* OR bacterial contamination OR microbial contamination OR self-contamination OR decontamination OR surface decontamination OR skin decontamination} |
| #3 | 32599 | GW{health personnel OR health care worker* OR health care personnel OR health personnel OR health-personnel OR health provider* OR health care provider* OR medical staff OR medical personnel OR medical professional OR medical worker* OR dental personnel OR dental staff OR dentist* OR dental assistant* OR nursing staff OR nurse* OR nursing assistant* OR nurses’ aides OR nurse midwife OR nurse midwives OR midwife OR midwives OR military-medical personnel OR physician* OR emergency medical services OR transporting patients OR patient transport OR ambulance* OR allied health personnel OR paramedic* OR paramedical personnel OR burial OR burial staff OR cleaning worker* OR cleaner work OR cleaner*} |
| #4 | 1250 | #1 AND #2 AND #3 |
| #5 | 742476 | DC{OUBIB OR OUCISD OR OUHSEL OR OUISST OR OUNIOC OR OUNIOS OR OURILO} |
| #6 | 1103 | #4 AND #5 |
Appendix 6. Effects of wearing PPE consistently on the risk of SARS infection
2. Wearing PPE consistently versus wearing PPE inconsistently
During and just after the SARS epidemic a number of of studies evaluated the impact of the use of PPE on SARS infection rates. Six of these studies were case-control studies and five were retrospective cohort studies. Since information in these studies was collected in the same retrospective way by questionnaires and/or interviews we combined the results of these studies.
There were two studies (Le 2004; Park 2004), one in a single hospital in Vietnam and the other in multiple hospitals in the US, that reported no cases in spite of sufficient exposure to SARS patients. The Vietnamese study claimed that this was because of the almost universal use of N95 masks later during the epidemic. The US study could not find an explanation because the use of PPE was not optimal in many cases. We could find no reasons to explain this result because these studies were rather similar to the other studies included. Also, in another hospital near the one in the Vietnamese study, SARS cases did occur among HCWs but this was more at the beginning of the epidemic and it was unclear how well PPE had been used (Reynolds 2006).
2.1. Consistent mask use versus inconsistent use
Six studies (Liu 2009; Loeb 2004; Nishiura 2005; Scales 2003; Seto 2003; Teleman 2004) could be combined in a meta-analysis that showed a beneficial effect of consistent mask use as part of PPE both in a fixed effect (OR 0.28, 95% CI 0.17 to 0.46, Analysis 9.1, I2 = 42%) and in a random effects meta-analysis model (OR 0.27, 95% CI 0.13 to 0.53).
2.2. Consistent gown/suit use versus inconsistent use
Four studies (Loeb 2004; Nishiura 2005; Pei 2006; Teleman 2004) could be combined and showed that consistent gown use had a preventive effect on SARS infection both in a fixed and random effects analysis (OR 0.22, 95% 0.10 to 0.50 Analysis 9.1, I2 = 53%). The data in Teleman 2004 were reported as OR 0.5, 95% CI 0.4 to 6.9 p = 0.6). However, this is an apparent mistake as the confidence interval does not fit with the OR nor with the p-value. We corrected this to OR 0.5, 95% CI 0.04 to 6.9 which makes the results consistent.
2.3. Consistent glove use versus inconsistent use
Also consistent glove use in six studies (Loeb 2004; Nishiura 2005; Pei 2006; Scales 2003; Seto 2003; Teleman 2004) led to a decrease in the risk of SARS infection both in fixed effects meta-analysis (OR 0.54 95% CI 0.33 to 0.89, Analysis 9.1, I2 = 0%) and in a random effects analysis (OR 0.53, 95% CI 0.28 to 1.01) but this was not statistically significant.
2.4. Consistent use of more than one PPE part versus inconsistent use
Ho 2004, Lau 2004, and Scales 2003 measured consistent use of more than one PPE part compared to no use at all. The combination of more than one PPE had a similar effect on SARS infection risk but this was not statistically significant, neither in the fixed effects analysis (OR 0.36, 95% CI 0.09 to 1.39, Analysis 9.1, I2 = 35%) nor in the random effects analysis (OR 0.37, 95% CI 0.07 to 1.98).
Footnotes
Disclaimer: The findings and conclusions in this Cochrane systematic review are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health. Mention of product names does not imply endorsement.
DECLARATIONS OF INTEREST
Jos Verbeek: None known.
Sharea Ijaz: None known.
Christina Mischke: None known.
Jani Ruotsalainen: None known.
F Selcen Kilinc Balci: None known.
Erja Mäkelä: None known.
Kaisa Neuvonen: None known.
Michael Edmond: I have given several lectures to non-profit professional associations (e.g. APIC) on topics related to infection control that in some instances provide an honorarium. None of these lectures were for industry.
Riitta Sauni: None known.
Raluca C Mihalache: None known.
REFERENCES
References to studies included in this review
- Bell 2015.Bell T, Smoot J, Patterson JE, Smalligan R, Jordan R. Ebola virus disease: The use of fluorescents as markers of contamination for personal protective equipment. ID Cases 2015;2:27–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buianov 2004.Buianov VV, Kolesnikov NV, Malyshev NA, Suprun IP. [Use of new individual protection substances in Mel’tser boxes]. Vestnik Rossiĭskoĭ Akademii Meditsinskikh Nauk 2004;1:30–5. [PubMed] [Google Scholar]
- Casalino 2015.Casalino E, Astocondor E, Sanchez JC, Diaz-Santana DE, Del Aquila C, Carrillo JP. Personal protective equipment for the Ebola virus disease: A comparison of 2 training programs. American Journal of Infection Control 2015;43(12):1281–7. [DOI] [PubMed] [Google Scholar]
- Casanova 2012.Casanova LM, Rutala WA, Weber DJ, Sobsey MD. Effect of single- versus double-gloving on virus transfer to health care workers’ skin and clothing during removal of personal protective equipment. American Journal of Infection Control 2012;40(4):369–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo 2014.Guo YP, Li Y, Wong PLH. Environment and body contamination: a comparison of two different removal methods in three types of personal protective clothing. American Journal of Infection Control 2014;42(4):e39–e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung 2015.Hung PP, Choi KS, Chiang VC. Using interactive computer simulation for teaching the proper use of personal protective equipment. CIN: Computers, Informatics, Nursing 2015;33 (2):49–57. [DOI] [PubMed] [Google Scholar]
- Shigayeva 2007.Shigayeva A, Green K, Raboud JM, Henry B, Simor AE, Vearncombe M, et al. Factors associated with critical-care healthcare workers’ adherence to recommended barrier precautions during the Toronto severe acute respiratory syndrome outbreak. Infection Control 2007;28(11):1275–83. [DOI] [PubMed] [Google Scholar]
- Wong 2004.Wong TK, Chung JW, Li Y, Chan WF, Ching PT, Lam CH, et al. Effective personal protective clothing for health care workers attending patients with severe acute respiratory syndrome. American Journal of Infection Control 2004;32(2):90–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamora 2006.Zamora JE, Murdoch J, Simchison B, Day AG. Contamination: a comparison of 2 personal protective systems. Canadian Medical Association Journal 2006;175(3):249–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
- Abrahamson 2006.Abrahamson SD, Canzian S, Brunet F. Using simulation for training and to change protocol during the outbreak of severe acute respiratory syndrome. Critical Care 2006;10(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beam 2011.Beam EL, Gibbs SG, Boulter KC, Beckerdite ME, Smith PW. A method for evaluating health care workers’ personal protective equipment technique. American Journal of Infection Control 2011;39(5):415–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beam 2014.Beam EL, Gibbs SG, Hewlett AL, Iwen PC, Nuss SL, Smith PW. Method for investigating nursing behaviors related to isolation care. American Journal of Infection Control 2014;42(11):1152–6. [DOI] [PubMed] [Google Scholar]
- Bearman 2007.Bearman GM, Marra AR, Sessler CN, Smith WR, Rosato A, Laplante JK, et al. A controlled trial of universal gloving versus contact precautions for preventing the transmission of multidrug-resistant organisms. American Journal of Infection Control 2007;35(10):650–5. [DOI] [PubMed] [Google Scholar]
- Belkin 1991.Belkin NL. The protectiveness of protective clothing. Infection Control and Hospital Epidemiology 1991;12(8):464–468. [PubMed] [Google Scholar]
- Belkin 2000.Belkin NL. Selecting protective apparel for the degree of exposure anticipated. Infection Control and Hospital Epidemiology 2000;21(7):436. [DOI] [PubMed] [Google Scholar]
- Belkin 2005.Belkin NL. “False faith in the surgeon’s gown” revisited. Bulletin of the American College of Surgeons 2005;90(4):19–23,56. [PubMed] [Google Scholar]
- Borchert 2007.Borchert M, Mulangu S, Lefevre P, Tshomba A, Libande ML, Kulidri A, et al. Use of protective gear and the occurrence of occupational Marburg hemorrhagic fever in health workers from Watsa health zone, Democratic Republic of the Congo. Journal of Infectious Diseases 2007;196 Suppl 2:S168–75. [DOI] [PubMed] [Google Scholar]
- Buianov 1991.Buianov VV, Elkin EN, Kolmykov VG, Kaplunov IuV, Malyshev NA, Kelli EI, et al. [Use of personal protective equipment by pathologists and legal physicians working with particularly dangerous infectious diseases]. Arkhiv Patologii 1991;53(3):59–61. [PubMed] [Google Scholar]
- Bunyan 2013.Bunyan D, Ritchie L, Jenkins D, Coia JE. Respiratory and facial protection: a critical review of recent literature. The Journal of Hospital Infection 2013;85(3):165–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova 2008.Casanova L, Alfano-Sobsey E, Rutala WA, Weber DJ, Sobsey M. Virus transfer from personal protective equipment to healthcare employees’ skin and clothing. Emerging Infectious Diseases 2008 2008;14(8):1291–3. [DOI: 10.3201/eid1408.080085] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castle 2009.Castle N, Owen R, Hann M, Clark S, Reeves D, Gurney I. Impact of chemical, biological, radiation, and nuclear personal protective equipment on the performance of low- and high-dexterity airway and vascular access skills. Resuscitation 2009;80(11):1290–5. [DOI] [PubMed] [Google Scholar]
- Christian 2004.Christian MD, Loutfy M, McDonald LC, Martinez KF, Ofner M, Wong T, et al. Possible SARS coronavirus transmission during cardiopulmonary resuscitation. Emerging Infectious Diseases 2004;10(2):287–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chughtai 2013.Chughtai AA, Seale H, MacIntyre CR. Availability, consistency and evidence-base of policies and guidelines on the use of mask and respirator to protect hospital health care workers: a global analysis. BMC Research Notes 2013;6(216):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clay 2015.Clay KA, O’Shea MK, Fletcher T, Moore AJ, Burns DS, Craig D, et al. Use of an ultraviolet tracer in simulation training for the clinical management of Ebola virus disease. The Journal of Hospital Infection 2015;91(3):275–7. [DOI] [PubMed] [Google Scholar]
- Coates 2000.Coates MJ, Jundi AS, James MR. Chemical protective clothing; a study into the ability of staff to perform lifesaving procedures. Journal of Accident and Emergency Medicine 2000;17(2):115–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coca 2015.Coca A, DiLeo T, Kim JH, Roberge R, Shaffer R. Baseline evaluation with a sweating thermal manikin of personal protective ensembles recommended for use in West Africa. Disaster medicine and public health preparedness 2015;9(5):536–42. [DOI] [PubMed] [Google Scholar]
- Colebunders 2004.Colebunders R, Sleurs H, Pirard P, Borchert M, Libande M, Mustin JP, et al. Organisation of health care during an outbreak of Marburg haemorrhagic fever in the Democratic Republic of Congo, 1999. Journal of Infection 2004;48(4):347–53. [DOI] [PubMed] [Google Scholar]
- Cooper 2005.Cooper DM, Charles D, Durnell AJ, Anderson JM, Kern T, Self T. Assessment of personal protective equipment used for facial mucocutaneous exposure protection in nonhuman primate areas. Lab Animal (NY) 2005;34(5):49–53. [DOI] [PubMed] [Google Scholar]
- Dunn 2015.Dunn AC, Walker TA, Redd J, Sugerman D, McFadden J, Singh T, et al. Nosocomial transmission of Ebola virus disease on pediatric and maternity wards: Bombali and Tonkolili, Sierra Leone, 2014. American Journal of Infection Control 2015;43: [Epub ahead of print]. [DOI: 10.1016/j.ajic.2015.09.016; [DOI] [PubMed] [Google Scholar]
- Fischer 2015.Fischer WA 2nd, Weber DJ, Wohl DA. Personal Protective Equipment: Protecting Health Care Providers in an Ebola Outbreak. Clinical Therapeutics 2015;37(11):2402–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gozel 2013.Gozel MG, Dokmetas I, Oztop AY, Engin A, Elaldi N, Bakir M. Recommended precaution procedures protect healthcare workers from Crimean-Congo hemorrhagic fever virus. International Journal of Infectious Diseases 2013;17(11):e1046–50. [DOI] [PubMed] [Google Scholar]
- Grélot 2015.Grélot L, Koulibaly F, Maugey N, Janvier F, Foissaud V, Aletti M, et al. Moderate thermal strain in healthcare workers wearing personal protective equipment during treatment and care activities in the context of the 2014 Ebola virus disease outbreak. Journal of Infectious Diseases 2015. Dec 9;212:[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Hendler 2000.Hendler I, Nahtomi O, Segal E, Perel A, Wiener M, Meyerovitch J. The effect of full protective gear on intubation performance by hospital medical personnel. Association of Military Surgeons of the United States 2000;165(4):272–4. [PubMed] [Google Scholar]
- Hersi 2015.Hersi M, Stevens A, Quach P, Hamel C, Thavorn K, Garritty C, et al. Effectiveness of personal protective equipment for healthcare workers caring for patients with filovirus disease: a rapid review. PloS one 2015;10(10):e0140290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildwine 2006.Hildwine F. Breathable PPE. New fabric blocks virus transmission. JEMS: a Journal of Emergency Medical Services 2006;31(9):100. [DOI] [PubMed] [Google Scholar]
- Ho 2003.Ho AS, Sung JJ, Chan-Yeung M. An outbreak of severe acute respiratory syndrome among hospital workers in a community hospital in Hong Kong. Annals of Internal Medicine 2003;139(7):564–7. [DOI] [PubMed] [Google Scholar]
- Ho 2004.Ho KY, Singh KS, Habib AG, Ong BK, Lim TK, Ooi EE, et al. Mild illness associated with severe acute respiratory syndrome coronavirus infection: lessons from a prospective seroepidemiologic study of health-care workers in a teaching hospital in Singapore. Journal of Infectious Diseases 2004;189(4):642–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hon 2008.Hon CY, Gamage B, Bryce EA, LoChang J, Yassi A, Maultsaid D, et al. Personal protective equipment in health care: can online infection control courses transfer knowledge and improve proper selection and use?. American Journal of Infection Control 2008;36(10):e33–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hormbrey 1996.Hormbrey PJ, Moore F, Skinner DV. Protective clothing in accident and emergency departments: cost versus risk benefit. Journal of Accident and Emergency Medicine 1996;13(1):70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffs 2007.Jeffs B, Roddy P, Weatherill D, de la Rosa O, Dorion C, Iscla M, et al. The Medecins Sans Frontieres intervention in the Marburg hemorrhagic fever epidemic, Uige, Angola, 2005. I. Lessons learned in the hospital. Journal of Infectious Diseases 2007;196 Suppl 2:S154–61. [DOI] [PubMed] [Google Scholar]
- Jinadatha 2015.Jinadatha C, Simmons S, Dale C, Ganachari-Mallappa N, Villamaria FC, Goulding N, et al. Disinfecting personal protective equipment with pulsed xenon ultraviolet as a risk mitigation strategy for health care workers. American Journal of Infection Control 2015;43(4):412–4. [DOI] [PubMed] [Google Scholar]
- Keane 1977.Keane E, Gilles HM. Lassa fever in Panguma Hospital, Sierra Leone, 1973–6. British Medical Journal 1977;1(6073):1399–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerstiens 1999.Kerstiens B, Matthys F. Interventions to control virus transmission during an outbreak of Ebola hemorrhagic fever: experience from Kikwit, Democratic Republic of the Congo, 1995. Journal of Infectious Diseases 1999;179(suppl. 1):s263–7. [DOI] [PubMed] [Google Scholar]
- Kim 2015.Kim SG. Healthcare workers infected with Middle East respiratory syndrome coronavirus and infection control. Journal of the Korean Medical Association 2015;58(7):647–54. [Google Scholar]
- Ko 2004.Ko PC, Chen WJ, Ma MH, Chiang WC, Su CP, Huang CH, et al. Emergency medical services utilization during an outbreak of severe acute respiratory syndrome (SARS) and the incidence of SARS-associated coronavirus infection among emergency medical technicians. Academic Emergency Medicine 2004;11(9):903–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai 2005.Lai TS, Keung Ng T, Seto WH, Yam L, Law KI, Chan J. Low prevalence of subclinical severe acute respiratory syndrome-associated coronavirus infection among hospital healthcare workers in Hong Kong. Scandinavian Journal of Infectious Diseases 2005;37(6/7):500/3. [DOI] [PubMed] [Google Scholar]
- Lai 2011.Lai J, Guo Y, Or P, Li Y. Comparison of hand contamination rates and environmental contamination levels between two different glove removal methods and distances. American Journal of Infection Control 2011;39(2):104–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange 2005.Lange JH. SARS, emerging diseases, healthcare workers and respirators. Journal of Hospital Infection 2005;60(3):293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau 2004.Lau JT, Fung KS, Wong TW, Kim JH, Wong E, Chung S, et al. SARS transmission among hospital workers in Hong Kong. Emerging Infectious Diseases 2004;10(2):280–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le 2004.Le DH, Bloom SA, Nguyen QH, Maloney SA, Le QM, Leitmeyer KC, et al. Lack of SARS transmission among public hospital workers, Vietnam. Emerging Infectious Diseases 2004;10(2):265–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsey 2012.Lindsley WG, King WP, Thewlis RE, Reynolds JS, Panday K, Cao G, et al. Dispersion and exposure to a cough-generated aerosol in a simulated medical examination room. Journal of Occupational and Environmental Hygiene 2012;9(12):681–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsley 2014.Lindsley WG, Noti JD, Blachere FM, Szalajda JV, Beezhold DH. Efficacy of face shields against cough aerosol droplets from a cough simulator. Journal of Occupational and Environmental Hygiene 2014;11(8):509–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu 2009.Liu W, Tang F, Fang LQ, de Vlas SJ, Ma HJ, Zhou JP, et al. Risk factors for SARS infection among hospital healthcare workers in Beijing: A case control study. Tropical Medicine and International Health 2009; Vol. 14, issue supplement 1:52–9. [Google Scholar]
- Loeb 2004.Loeb M, McGeer A, Henry B, Ofner M, Rose D, Hlywka T, et al. SARS among critical care nurses, Toronto. Tropical Medicine and International Health 2004;10(2):251–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low 2005.Low JG, Wilder-Smith A. Infectious respiratory illnesses and their impact on healthcare workers: a review. Annals of Academic Medicine Singapore 2005;34(1):105–10. [PubMed] [Google Scholar]
- Lowe 2014.Lowe JJ, Jelden KC, Schenarts PJ, Rupp LE, Hawes KJ, Tysor BM, et al. Considerations for safe EMS transport of patients infected with Ebola virus. Prehospital Emergency Care 2015;19(2):179–83. [DOI] [PubMed] [Google Scholar]
- Lu 2006.Lu YT, Chen PJ, Sheu CY, Liu CL. Viral load and outcome in SARS infection: the role of personal protective equipment in the emergency department. Journal of Emergency Medicine 2006;30(1):7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo 2011.Luo CH, Yang S, Wen CY, Syu MY, Lin KH, Chiu SH, et al. Fluorescent aerosol leakage quantification for protective clothing with an entropy-based image processor for industrial and medical workers. Journal of Aerosol Science 2011;42(7):491–6. [Google Scholar]
- Ma 2004.Ma HJ, Wang HW, Fang LQ, Jiang JF, Wei MT, Liu W, et al. [A case-control study on the risk factors of severe acute respiratory syndromes among health care workers]. Zhonghua Liu Xing Bing Xue Za Zhi 2004;25(9):741–4. [PubMed] [Google Scholar]
- Malik 2006.Malik MH, Handford E, Staniford E, Gambhir AK, Kay PR. Comfort assessment of personal protection systems during total joint arthroplasty using a novel multi-dimensional evaluation tool. Annals of the Royal College of Surgeons England 2006;88(5):465–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marklund 2002.Marklund LA. Transporting patients with lethal contagious infections. International Journal of Trauma Nursing 2002;8(2):51–3. [DOI] [PubMed] [Google Scholar]
- Matanock 2014.Matanock A, Arwady MA, Ayscue P, Forrester JD, Gaddis B, Hunter JC, et al. Ebola virus disease cases among health care workers not working in Ebola treatment units--Liberia, June-August, 2014. Morbidity and Mortality Weekly Report 2014;63(46):1077–81. [PMC free article] [PubMed] [Google Scholar]
- Mehtar 2015.Mehtar S, Hakizimana B, Infection Control Africa Network Education and Training Working Group. IPC training in Sierra Leone- ICAN’s role in fighting Ebola. Antimicrobial Resistance and Infection Control 16 June 2015;4(Suppl 1):12.25908966 [Google Scholar]
- Minnich 2003.Minnich G. A clean ride. Building EMS vehicles for easier cleaning & decontamination. JEMS : a journal of emergency medical services 2003;28(5):104–15. [PubMed] [Google Scholar]
- Mollura 2015.Mollura DJ, Palmore TN, Folio LR, Bluemke DA. Radiology preparedness in ebola virus disease: guidelines and challenges for disinfection of medical imaging equipment for the protection of staff and patients. Radiology 2015;275(2):538–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore 2005.Moore D, Gamage B, Bryce E, Copes R, Yassi A. Protecting health care workers from SARS and other respiratory pathogens: organizational and individual factors that affect adherence to infection control guidelines. American Journal of Infection Control 2005;33(2):114–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan 2009.Morgan DJ, Diekema DJ, Sepkowitz K, Perencevich EN. Adverse outcomes associated with contact precautions: a review of the literature. American Journal of Infection Control 2009;37(2):85–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muyembe-Tamfum 1999.Muyembe-Tamfum JJ, Kipasa M, Kiyungu C, Colebunders R. Ebola outbreak in Kikwit, Democratic Republic of the Congo: discovery and control measures. Journal of Infectious Diseases 1999;179(Suppl 1):S259–62. [DOI] [PubMed] [Google Scholar]
- Nishiura 2005.Nishiura H, Kuratsuji T, Quy T, Phi NC, Van Ban V, Ha LE, et al. Rapid awareness and transmission of severe acute respiratory syndrome in Hanoi French Hospital, Vietnam. American Journal of Tropical Medicine and Hygiene 2005;73(1):17–25. [PubMed] [Google Scholar]
- Northington 2007.Northington WE, Mahoney GM, Hahn ME, Suyama J, Hostler D. Training retention of level C personal protective equipment use by emergency medical services personnel. Academic Emergency Medicine 2007;14(10):846–9. [DOI] [PubMed] [Google Scholar]
- Nyenswah 2015.Nyenswah T, Fallah M, Sieh S, Kollie K, Badio M, Gray A, et al. Controlling the last known cluster of Ebola virus disease - Liberia, January-February 2015. MMWR Morbidity and Mortality Weekly Report 2015;64(18):500–4. [PMC free article] [PubMed] [Google Scholar]
- Ofner 2003.Ofner M, Lem M, Sarwal S, Vearncombe M, Simor A. Cluster of severe acute respiratory syndrome cases among protected health care workers -Toronto, April 2003. Canada Communicable Disease Report 2003;29(11):93–7. [PubMed] [Google Scholar]
- Ofner-Agostini 2006.Ofner-Agostini M, Gravel D, McDonald LC, Lem M, Sarwal S, McGeer A, et al. Cluster of cases of severe acute respiratory syndrome among Toronto healthcare workers after implementation of infection control precautions: A case series. Infection Control 2006;27(5):473–8. [DOI] [PubMed] [Google Scholar]
- Ogendo 2008.Ogendo SW, Awori MN, Omondi MA, Mulatya EM, Mugo PW. Risk of conjunctival contamination from blood splashes during surgery at the Kenyatta National Hospital, Nairobi. East African Medical Journal 2008;85(9):432–7. [DOI] [PubMed] [Google Scholar]
- Ong 2013.Ong MS, Magrabi F, Post J, Morris S, Westbrook J, Wobcke W, et al. Communication interventions to improve adherence to infection control precautions: a randomised crossover trial. BMC Infectious Diseases 2013;13:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park 2004.Park BJ, Peck AJ, Kuehnert MJ, Newbern C, Smelser C, Comer JA, et al. Lack of SARS transmission among healthcare workers, United States. Emerging Infectious Diseases 2004;10(2):244–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pei 2006.Pei LY, Gao ZC, Yang Z, Wei DG, Wang SX, Ji JM, et al. Investigation of the influencing factors on severe acute respiratory syndrome among health care workers. Journal of Peking University (Health Sciences) 2006;38(3):271–5. [PubMed] [Google Scholar]
- Ragazzoni 2015.Ragazzoni L, Ingrassia PL, Echeverri L, Maccapani F, Berryman L, Burkle FM, et al. Virtual reality simulation training for Ebola deployment. Disaster Medicine and Public Health Preparedness 2015;9(5):543–6. [DOI] [PubMed] [Google Scholar]
- Ransjo 1979.Ransjo U. Attempts to control clothes-borne infection in a burn unit, 3. An open-roofed plastic isolator or plastic aprons to prevent contact transfer of bacteria. Journal of Hygiene (London) 1979;82(3):385–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds 2006.Reynolds MG, Anh BH, Thu VH, Montgomery JM, Bausch DG, Shah JJ, et al. Factors associated with nosocomial SARS-CoV transmission among healthcare workers in Hanoi, Vietnam, 2003. BMC Public Health 2006;6:207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell 2015.Russell CD, Young I, Leung V, Morris K. Healthcare workers’ decision-making about transmission-based infection control precautions is improved by a guidance summary card. The Journal of Hospital Infection 2015;90(3):235–9. [DOI] [PubMed] [Google Scholar]
- Scales 2003.Scales DC, Green K, Chan AK, Poutanen SM, Foster D, Nowak K, et al. Illness in intensive care staff after brief exposure to severe acute respiratory syndrome. Emerging Infectious Diseases 2003;9(10):1205–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacher 2010.Schumacher J, Gray SA, Michel S, Alcock R, Brinker A. Respiratory protection during paediatric cardiopulmonary resuscitation. European Journal of Anaesthesiology 2011;28:150. [Google Scholar]
- Seto 2003.Seto WH, Tsang D, Yung RW, Ching TY, Ng TK, Ho M, et al. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS). Lancet 2003;361(9368):1519–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao 2015.Shao X-p, Zhou Q, Ju J-t, Xin H-g, Chen J, Wan C-l, et al. Evaluation of anti-Ebola training system in the PLA Medical Team to Liberia and some suggestion. Academic Journal Of Second Military Medical University 2015;36(8):822–7. [Google Scholar]
- Sorensen 2008.Sorensen P, Ejlertsen T, Aaen D, Poulsen K. Bacterial contamination of surgeons gloves during shunt insertion: a pilot study. British Journal of Neurosurgery 2008;22(5):675–7. [DOI] [PubMed] [Google Scholar]
- Tartari 2015.Tartari E, Allegranzi B, Ang B, Calleja N, Collignon P, Hopman J, et al. Preparedness of institutions around the world for managing patients with Ebola virus disease: an infection control readiness checklist. Antimicrobial Resistance and Infection Control 2015;4:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tartari E, Falzon Parascandalo A R, Borg MA. Ensuring healthcare workers’ safety in the management of Ebola virus disease: a novel competency assessment checklist for proper PPE use. Antimicrobial Resistance and Infection Control 2015;4:Suppl 1. [Google Scholar]
- Teleman 2004.Teleman MD, Boudville IC, Heng BH, Zhu D, Leo YS. Factors associated with transmission of severe acute respiratory syndrome among health-care workers in Singapore. Epidemiology and Infection 2004;132(5):797–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomas 2015.Tomas ME, Kundrapu S, Thota P, Sunkesula VC, Cadnum JL, Mana TS, et al. Contamination of health care personnel during removal of personal protective equipment. JAMA Internal Medicine 2015;175(12):1904–10. [DOI] [PubMed] [Google Scholar]
- Torres 2015.Torres M, Hansen KN, Jerrard D. Ebola: a review for emergency providers. Emergency Medicine Clinics of North America 2015;33(2):e1–18. [DOI] [PubMed] [Google Scholar]
- West 2014.West K. Ebola outbreak 2014. Why we don’t need moon suits. JEMS: a Journal of Emergency Medical Services 2014;39(11):28–30. [PubMed] [Google Scholar]
- Yin 2004.Yin WW, Gao LD, Lin WS, Gao LD, Lin WS, Du L, et al. [Effectiveness of personal protective measures in prevention of nosocomial transmission of severe acute respiratory syndrome]. Zhonghua Liu Xing Bing Xue Za Zhi 2004;25(1):18–22. [PubMed] [Google Scholar]
- Zellmer 2015.Zellmer C, Van Hoof S, Safdar N. Variation in health care worker removal of personal protective equipment. American Journal of Infection Control 2015;43(7):750–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou 2003.Zhou G, Qi Y, Li L. [Investigation report on the SARS infection rate of the second medical team of Peking University First Hospital]. Beijing Da Xue Xue Bao 2003;35 Suppl:59–61. [PubMed] [Google Scholar]
Additional references
- ANSI/AAMI PB70 2012.ANSI/AAMI. PB70: Liquid barrier performance and classification of protective apparel and drapes in health care facilities. Association for the Advancement of Medical Instrumentation; 2012. [Google Scholar]
- Australian NHMRC 2010.Australian National Health and Medical Research Council. Australian guidelines for the prevention and control of infection in healthcare. http://www.nhmrc.gov.au/book/html-australian-guidelines-prevention-and-control-infection-healthcare-2010. (accessed 8 December 2014).
- Campbell 2001.Campbell MK, Mollison J, Grimshaw JM. Cluster trials in implementation research: estimation of intracluster correlation coefficients and sample size. Statistics in Medicine 2001;20(3):391–9. [DOI] [PubMed] [Google Scholar]
- CDC 2003.Centers for Disease Control and Prevention (CDC). Outbreak of severe acute respiratory syndrome - worldwide, 2003. Morbidity and Mortality Weekly Report 2003;52(11):226–8. [PubMed] [Google Scholar]
- CDC 2014.Center for Disease Control. Guidance on personal protective equipment to be used by healthcare workers during management of patients with Ebola virus disease in U.S. Hospitals, including procedures for putting on (donning) and removing (doffing). http://www.cdc.gov/vhf/ebola/hcp/procedures-for-ppe.html (accessed 8 December 2014).
- Cherry 2006.Cherrie JW, Semple S, Christopher Y, Saleem A, Hughson GW, Philips A. How important is inadvertent ingestion of hazardous substances at work?. Annals of Occupational Hygiene 2006;50(7):693–704. [DOI] [PubMed] [Google Scholar]
- Coia 2013.Coia JE, Ritchie L, Adisesh A, Makison Booth C, Bradley C, Bunyan D, et al. Guidance on the use of respiratory and facial protection equipment. The Journal of Hospital Infection 2013;85(3):170–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covidence [Computer program].Veritas Health Innovation. Covidence Systematic Review Software. Melbourne, Australia: Veritas Health Innovation, 2016. [Google Scholar]
- De Iaco 2012.De Iaco G, Puro V, Fusco FM, Schilling S, Maltezou HC, Brouqui P, et al. European network for highly infectious diseases working group. Personal protective equipment management and policies: European network for highly infectious diseases data from 48 isolation facilities in 16 European countries. Infection Control and Hospital Epidemiology 2012;33(10):1008–16. [DOI] [PubMed] [Google Scholar]
- Ebola 2014.[no authors listed]. Ebola: protection of health workers on the front line. Lancet 2014; Vol. 384, issue 9942:470. [DOI] [PubMed] [Google Scholar]
- ECDC 2014.European Center for Disease Control. Tutorial on the safe use of personal protective equipment. http://www.ecdc.europa.eu/en/healthtopics/ebola_marburg_fevers/Pages/tutorial-ppe.aspx; http://www.ecdc.europa.eu/en/publications/_layouts/forms/Publication_DispForm.aspx?List=4f55ad51-4aed-4d32-b960-af70113dbb90&ID=1193 (accessed 8 December 2014, updated 15 March 2015). [Google Scholar]
- EN 13795.CEN (European Committee for Standardization). EN 13795–2 Surgical drapes, gowns, clean air suits used as medical devices for patients, clinical staff and equipment. CEN (European Committee for Standardization) 2005. [Google Scholar]
- EN 14126.CEN (European Committee for Standardization). CSN EN 14126 Protective clothing - Performance requirements and tests methods for protective clothing against infective agents. CEN (European Committee for Standardization) 2003. [Google Scholar]
- EU 2010.European Commission. Council Directive 2010/32/EU of 10 May 2010 implementing the Framework Agreement on prevention from sharp injuries in the hospital and healthcare sector concluded by HOSPEEM and EPSU. http://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX:32010L0032 (accessed 30 March 2015). [Google Scholar]
- Fischer 2014.Fischer WA 2nd, Hynes NA, Perl TM. Protecting health care workers from ebola: personal protective equipment is critical but is not enough. Annals of Internal Medicine 2014;161(10):753–4. [DOI] [PubMed] [Google Scholar]
- Forrester 2014.Forrester JD, Hunter JC, Pillai SK, Arwady MA, Ayscue P, Matanock A, et al. : Centers for Disease Control and Prevention (CDC). Cluster of Ebola cases among Liberian and U.S. health care workers in an Ebola treatment unit and adjacent hospital -Liberia, 2014. Morbidity and Mortality Weekly Report 2014; Vol. 63, issue 41:925–9. [PMC free article] [PubMed] [Google Scholar]
- Gershon 2009.Gershon RR, Vandelinde N, Magda LA, Pearson JM, Werner A, Prezant D. Evaluation of a pandemic preparedness training intervention of emergency medical services personnel. Prehospital and Disaster Medicine 2009;24(6):508–11. [DOI] [PubMed] [Google Scholar]
- Gould 2010.Gould DJ, Moralejo D, Drey N, Chudleigh JH. Interventions to improve hand hygiene compliance in patient care. Cochrane Database of Systematic Reviews 2010, Issue 9. [DOI: 10.1002/14651858.CD005186.pub3] [DOI] [PubMed]
- GRADEpro 2008 [Computer program].Brozek J, Oxman A, Schünemann H. GRADEpro. Version 3.2 for Windows. GRADE working group, 2008. [Google Scholar]
- Higgins 2011.Higgins JPT, Green S(editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org. Available from www.cochrane-handbook.org. [Google Scholar]
- Howie 2005.Howie RM. Respiratory protection use. Occupational Environmental Medicine 2005;62(6):423–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ISO 2004.International Organization for Standardization (ISO). Clothing for protection against contact with blood and body fluids -Determination of resistance of protective clothing materials to penetration by blood-borne pathogens -- Test method using Phi-X 174 bacteriophage ISO 166604:2004. International Organization for Standardization; 2004. [Google Scholar]
- ISO 2004a.International Organization for Standardization (ISO). Clothing for protection against contact with blood and body fluids -Determination of the resistance of protective clothing materials to penetration by blood and body fluids -- Test method using synthetic blood, ISO 16603:2004. International Organization for Standardization (ISO) 2004. [Google Scholar]
- ISO 2013.International Organization for Standardization (ISO). Protective clothing -- Protection against chemicals -- Determination of resistance of protective clothing materials to permeation by liquids and gases ISO 6529:2013. International Organization for Standardization (ISO) 2013. [Google Scholar]
- Jefferson 2008.Jefferson T, Foxlee R, Del Mar C, Dooley L, Ferroni E, Hewak B, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses: systematic review. BMJ 2008;12(7635):77–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefferson 2011.Jefferson T, Del Mar CB, Dooley L, Ferroni E, Al-Ansary LA, Bawazeer GA, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database of Systematic Reviews 2011, Issue 7. [DOI: 10.1002/14651858.CD006207.pub4;] [DOI] [PMC free article] [PubMed]
- Judson 2015.Judson S, Prescott J, Munster V. Understanding Ebola virus transmission. Viruses 2015;7(2):511–21. [DOI: 10.3390/v7020511;] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilmarx 2014.Kilmarx PH, Clarke KR, Dietz PM, Hamel MJ, Husain F, McFadden JD, et al. : Centers for Disease Control and Prevention (CDC). Ebola virus disease in health care workers - Sierra Leone, 2014. Morbidity and Mortality Weekly Report 2014;63(49):1168–71.] [PMC free article] [PubMed] [Google Scholar]
- Kuklane 2015.Kuklane K, Lundgren K, Gao C, Löndahl J, Hornyanszky ED, Östergren PO, et al. Ebola: Improving the design of protective clothing for emergency workers allows them to better cope with heat stress and help to contain the epidemic. Annals of Occupational Hygiene 2015;59(2):258–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landers 2010.Landers T, McWalters J, Behta M, Bufe G, Ross B, Vawdrey DK, et al. Terms used for isolation practices by nurses at an academic medical center. Journal of Advanced Nursing 2010;66(10):2309–19. [DOI: 10.1111/j.1365-2648.2010.05398.x;] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy 2015.Levy B, Rao CY, Miller L, Kennedy N, Adams M, Davis R, et al. Ebola infection control in Sierra Leonean health clinics: A large cross-agency cooperative project. American Journal of Infection Control 2015;43(7):752–5. [DOI: 10.1016/j.ajic.2015.03.011;] [DOI] [PubMed] [Google Scholar]
- Makison 2014.Makison Booth C. Vomiting Larry: a simulated vomiting system for assessing environmental contamination from projectile vomiting related to norovirus infection. Journal of Infection Prevention 2014;15(5):176–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Missair 2014.Missair A, Marino MJ, Vu CN, Gutierrez J, Missair A, Osman B, et al. Anesthetic Implications of Ebola Patient Management: A Review of the Literature and Policies Dec 30 2014;():. Anesthesia and Analgesia 2014;121(3):e-pub. [DOI] [PubMed] [Google Scholar]
- Moon 2015.Moon S, Sridhar D, Pate MA, Jha AK, Clinton C, Delaunay S, et al. Will Ebola change the game? Ten essential reforms before the next pandemic. The report of the Harvard-LSHTM independent panel on the global response to Ebola. Lancet 2015;386:2204–21. [DOI: 10.1016/S0140-6736(15)00946-0;] [DOI] [PMC free article] [PubMed] [Google Scholar]
- MSF 2015.MSF. Pushed to the Limit and Beyond, A year into the largest ever Ebola outbreak. https://www.doctorswithoutborders.org/sites/usa/files/msf143061.pdf (accessed 11 January 2016).
- Mäkelä 2014.Mäkelä E, Mäkinen H. Protective clothing against chemical and biological hazards. http://oshwiki.eu/wiki/Protective_clothing_against_chemical_and_biological_hazards#cite_note-EN14126-11 (accessed 12 November 2014).
- NFPA 1999.National Fire Protection Association. Standard on protective clothing for emergency medical operations. National Fire Protection Association; 2013. [Google Scholar]
- Nichol 2008.Nichol K, Bigelow P, O’Brien-Pallas L, McGeer A, Manno M, Holness DL. The individual, environmental, and organizational factors that influence nurses’ use of facial protection to prevent occupational transmission of communicable respiratory illness in acute care hospitals. American Journal of Infection Control 2008;36(7):481–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIOSH 2014.The National Institute for Occupational Safety and Health (NIOSH). Considerations for selecting protective clothing used in health care for protection against microorganisms in blood and body fluids. http://www.cdc.gov/niosh/npptl/topics/ProtectiveClothing/default.html (accessed 2 January 2015).
- OSHA 2012.Occupational Safety & Health Administration (OSHA). Bloodborne pathogens. 1910.1030(d)(3) Personal Protective Equipment https://www.osha.gov/law-regs.html (accessed 10 December 2014).
- RevMan 2014.The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014. [Google Scholar]
- Roberge 2008.Roberge RJ. Evaluation of the rationale for concurrent use of N95 filtering face piece respirators with loose-fitting powered air-purifying respirators during aerosol-generating medical procedures. American Journal of Infection Control 2008;36(2):135–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberge 2008a.Roberge RJ. Effect of surgical masks worn concurrently over N95 filtering face piece respirators: extended service life versus increased user burden. Journal of Public Health Management and Practice 2008;14(2):E19–26. [DOI] [PubMed] [Google Scholar]
- Sakunkoo 2012.Sakunkoo P, Laopaiboon M, Koh D. Behavioural interventions for promoting respiratory protection use in workers. Cochrane Database of Systematic Reviews 2012, Issue 10. [DOI: 10.1002/14651858.CD010157] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprecher 2015.Sprecher AG, Caluwaerts A, Draper M, Feldmann H, Frey CP, Funk RH, et al. Personal Protective Equipment for Filovirus Epidemics: A Call for Better Evidence. Journal of Infectious Diseases 2015;March 27:e-pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbeek 2016.Verbeek JHAM Mihalache RC. Letter to the editor. American Journal of Infection Control 2016;44:[accepted for publication]. [Google Scholar]
- Ward 2011.Ward DJ. The role of education in the prevention and control of infection: a review of the literature. Nurse Education Today 2011;31(1):9–17. [DOI] [PubMed] [Google Scholar]
- WHO 2006.World Health Organization (WHO). Health workers: a global profile. World Health Organization (WHO), Geneva: 2006. [Google Scholar]
- WHO 2009.World Health Organization. WHO guidelines on hand hygiene in health care: a summary. http://www.who.int/gpsc/5may/tools/who_guidelines-handhygiene_summary.pdf (accessed 8 December 2014).
- WHO 2014.World Health Organization. Protection against Ebola guidelines. http://apps.who.int/iris/bitstream/10665/137410/1/WHO_EVD_Guidance_PPE_14.1_eng.pdf (accessed 17 March 2015).
- WHO 2015.WHO regional office for Africa. Overview of Ebola virus disease epidemic in West Africa. WHO regional office for Africa Outbreak Bulletin 2015; Vol. 5, issue 5:2–3. [Google Scholar]
- Yassi 2005.Yassi A, Moore D, Fitzgerald JM, Bigelow P, Hon CY, Bryce E: BC Interdisciplinary Respiratory Protection Study Group. Research gaps in protecting healthcare workers from SARS and other respiratory pathogens: an interdisciplinary, multi-stakeholder, evidence-based approach. Journal of Occupational and Environmental Medicine 2005;47(1):41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zelnick 2013.Zelnick JR, Gibbs A, Loveday M, Padayatchi N, O’Donnell MR. Health-care workers’ perspectives on workplace safety, infection control, and drug-resistant tuberculosis in a high-burden HIV setting. Journal of Public Health Policy 2013;34(3):388–402. [DOI] [PMC free article] [PubMed] [Google Scholar]