Abstract
Aim
Evaluate the effect of the training program on knowledge and practice of breastfeeding women during coronavirus disease 2019 (COVID-19).
Methods
One-group pretest/post-test quasiexperimental research design was utilized to accomplish the aim of this study. The study was carried out at the primary health care units Ad Dar Al Baida 1, Ad Dar Al Baida 2, Al Aziziyah at Riyadh Province of Saudi Arabia. The study included a convenience sample of 100 breastfeeding women.
Tool
A structured interviewing questionnaire sheet was used for data collection that included three parts knowledge, reported practice, and demographic characteristics.
Results
More than one-quarter (30%) and (28%) of studied women had satisfactory knowledge-related causes, risk factor and signs, symptoms of COVID-19 at preintervention, while the majority 85% and 86% of them had satisfactory knowledge postintervention at p-value <.01**. In addition, less than one-fifth (17%) and (16%) of studied women had satisfactory knowledge about Breastfeeding guidelines during COVID-19 and care of breastfeeding women during COVID-19, compared with most of them (89%) and (92%) postintervention at p-value <.01**.
Conclusion
Based on our current study, it was concluded that the educational program effectively improves breastfeeding women's knowledge and practices. There was a highly statistically significant positive linear correlation between the breastfeeding women's knowledge and reported practices regarding COVID-19 infection before and after the implementation of the educational program at p < .0.
Keywords: breastfeeding, women, knowledge, practice, COVID-19, training program
Introduction
Severe acute respiratory syndrome coronavirus 2 is an RNA virus that causes coronavirus disease 2019 (COVID-19) (Park, 2020). In December 2019 the new coronavirus emerged in Wuhan, Central China, and quickly spread across the country to date more than 11 million people worldwide have been affected by COVID-19 (Dimopoulou et al., 2022). At this time, every continent on the planet has been affected. The COVID-19 epidemic is wreaking havoc on people's lives across the world. The epidemic needs immediate intervention, and when new knowledge becomes available, reliable standards for care are required (Pereira et al., 2020).
As the virus transmission occurs through respiratory droplets and mainly in close contact, among the proposed global health measures to reduce its spread are the implementation of lockdowns, confinement, and social distancing. Such measures have resulted in the separation of mothers and infants after birth, particularly in cases of suspected or confirmed COVID-19-positive mothers, preventing mother-baby close contact including breastfeeding. COVID-19-related policies (e.g., separation of the mother-infant) are expected to negatively impact maternal mental health outcomes (Pacheco et al., 2021).
The World Health Organization (WHO, 2021) declares breast milk as the ideal food for infants because is safe, clean and contains antibodies that help protect against many common childhood illnesses. Breast milk provides all the energy and nutrients that the infant needs for the first months of life, and it continues to provide up to half or more of a child's nutritional needs during the second half of the first year, and up to one-third during the second year of life. Given the immaturity of the immune system of newborns (Lubbe et al., 2020a, 2020b). Breastfeeding promotes mother's and child's health, as well as provides advantages to families, having a good social and economic benefit (Giuliani et al., 2020). The benefits of breastfeeding in conjunction with the relatively low prevalence of SARS-CoV-2 and mild illness in newborns and children support the practice of recommending direct breastfeeding as the preferred option during this pandemic (Bastug et al., 2020).
The main risk for infants of breastfeeding is close contact with the mother, who is likely to share infective airborne droplets. So, for women who prefer to breastfeed, precautions should be taken to limit viral spread to the baby (Govind et al., 2020). The benefits of breastfeeding outweigh the risks of virus transmission, so even women with suspected or proven COVID-19 infection are urged to continue breastfeeding (Lubbe et al., 2020a, 2020b). As an added precaution, mothers can wear masks and wash their hands with soap and water before contact with their babies. Breast milk can also be expressed via a breast pump or by hand expression if breastfeeding is not done directly from the breast (Verd et al., 2021).
Moreover, the technical language of the breastfeeding guidelines and discrepancies in the initially available literature on breastfeeding led to various misconceptions about breastfeeding during the pandemic. The lack of easy-to-understand, evidence-based, and accessible resources available on breastfeeding during COVID-19 suggested the crucial need to promote, protect, and support breastfeeding during COVID-19 through a knowledge mobilization project targeting Saudi mothers, the general public, and organizations providing direct and indirect care/services to mothers with young children, including vulnerable groups of Indigenous, refugee, and immigrant mothers (Hirani et al., 2021).
Review of Literature
Costantini et al. (2021) found that the majority of mothers were strongly committed to continuing breastfeeding during the pandemic. Also, Piankusol et al. (2021) stated that 93% continued breastfeeding because of the availability of health provider support during the lockdown. Moreover, many breastfeeding women who would benefit from breastfeeding counseling are unable to maintain regular touch with healthcare providers because of the COVID-19 pandemic. In addition, the technical nature of the breastfeeding recommendations and inconsistencies in the early literature on breastfeeding contributed to a number of misconceptions about nursing throughout the epidemic. The lack of easy-to-understand, evidence-based, and accessible resources available on breastfeeding during COVID-19 suggested the crucial need to promote, protect, and support breastfeeding during COVID-19 through an education program with pre/post-assessment and using different illustrative and teaching methods (Hirani et al., 2021). Moreover, Gebretsadik et al., 2022 implied that developing programs that enhance women's participation in education and decision-making could improve breast-feeding practice. Besides, providing lactating mothers with adequate and up-to-date breastfeeding information during the COVID-19 pandemic could be significant in improving breastfeeding practices. Therefore, this study aimed to evaluate the effect of training program on knowledge and practice of breast-feeding women during COVID-19.
Methods
Hypothesis
H1: Training program had a positive effect on knowledge and practice of breast-feeding women during COVID-19.
Research Design
One-group pretest/posttest quasi-experimental research design was utilized to accomplish the aim of this study. It is an empirical study that is used to estimate the effect of an intervention on its target population without random assignment (Cook & Wong, 2008).
Setting
The study was carried out at three primary health care (PHC) units Ad Dar Al Baida 1, Ad Dar Al Baida 2, Al Aziziyah at Riyadh Province of Saudi Arabia. The primary curative healthcare services through PHCs include controlling infectious diseases through immunization, child and maternity health, basic dental services, chronic disease management and follow-up, essential medications in addition to basic dental services, and health education
Participant
Participants were recruited using a convenience sampling technique at Ad Dar Al Baida 1 “20 women,” Ad Dar Al Baida 2 “40 women,” Al Aziziyah “40 women” at Riyadh Province in Saudi Arabia. A total of 100 breastfeeding women, from the previously mentioned setting, who accepted to participate in the study were recruited in the study.
Sample Size. The sample size was calculated based on the statistical power of 90%, level of confidence (1-Alpha Error): 95%, Alpha 0.05, Beta 0.1, determines the sample size, which is set at 90 breastfeeding women. Considering 15% sample attrition, the final sample size of 100 breastfeeding women distributed in three settings Ad Dar Al Baida 1 “20 women,” Ad Dar Al Baida 2 “40 women,” Al Aziziyah “40 women” at Riyadh Province of Saudi Arabia
Tools of Data Collection
Data for the current study were collected through a structured interviewing questionnaire sheet, which was developed by the researcher in the Arabic language after reviewing the literature reviews of Sakalidis et al. (2021). It consists of three parts as the following:
Part I: Concerned with the demographic profile of the studied mothers, included sociodemographic characteristics of the studied women such as age, employment, residence, educational level, marital status …. etc.
Part II: Concerned with breastfeeding women’ knowledge. It included 12 MCQ questions as concept of COVID-19, causes and risk factors of COVID-19, signs and symptoms of COVID-19, complication of COVID-19, ways of prevention COVID-19 infection, breastfeeding guidelines during COVID-19 and care of breastfeeding women during COVID-19 …. etc. Each answer scored with 1 score if correct and zero if incorrect. The total knowledge score was categorized as the following unsatisfactory (<70.0%), and satisfactory (≥ 70.0%). The reliability score of this tool was 0.819 “good.”
Part III: Concerned with mothers’ reported practice. It included 10 items about wash hands before and after touch the infant, avoid using pump shared by others, wear mask during breast feeding, clean shared surface in lactation room before and after use, clean and sanitize breast pumps and all infant feeding items … etc. Each answer scored with 1 score if done and zero if not done. The total practice score was categorized as the following unsatisfactory (<70.0%), and satisfactory (≥ 70.0%). The reliability score of this tool was 0.836 “good.”
Fieldwork. The researcher attended the PHC units, during the morning shift from 9.00 a.m. to 1.00 p.m. Data collection was extended over a period of 3 months period from the 1 of January 2022 to the end of March 2022 for pretest, educational program session implementation, and posttest. The researcher started by introducing herself to breastfeeding women and simply explaining the aim of the study. Data collection was carried out by interviewing with breastfeeding mother. Women were interviewed individually. Time consumed for each interview was 30 min.
Framework
Assessment Phase. The researcher explained the aim of the study and the components of the tools to the studied women. The researcher distributed a questionnaire to the studied women for assessing their knowledge and practices dependent on the previously designed questionnaire regarding COVID-19 infection and ways to prevent the spreading infection before implementation of the intervention. The educational program was prepared and designed according to the women’ needs according to pretest.
Intervention Phase. The researcher divided the studied women into five groups, each trained in four one-hour sessions in the form of lectures and seminars. The women were informed about the group to which they would be allocated via an invitation letter. They were also notified about the time and place of training. In the PHC conference hall, theoretical sessions were led by a researcher, over 10 continuous weeks on Saturday and Thursday. This one-hour session was held every week from 10 a.m. to 11 a.m. The Training Program. The training program for breastfeeding women was developed by the researcher after reviewing the literature to improve women’ knowledge regarding COVID-19 infection and ways to prevent the spreading infection.
The Training Program's Content
The first session focused on the concept of COVID-19, the causes and risk factors of COVID-19, and signs and symptoms of COVID-19. The second session focused on the complication of COVID-19, and prevention ways to prevent COVID-19 infection. The third session was concerned with care of COVID-19 patient, breastfeeding women during COVID-19 pandemic. The fourth session focused on instructions for breastfeeding women to prevent spreading infection.
Evaluation Phase. Reevaluation of breastfeed woman's knowledge and reported practices regarding COVID-19 infection after implementing the educational program and were compared with pretest levels.
Ethical Considerations
Ethical approval was provided by the Institutional Review Board of the Faculty of Nursing, with ID 287/21. As well as oral consent was obtained from each breastfeeding woman after the researcher informed them about the aim of the study. Moreover, women who agreed to participate in the study, informed that all data gathered during the study were confidential. Also, they have the right to withdraw from the study at any time. The questionnaire was filled in anonymously and the data were kept confidential and used for research purposes only.
Statistical Analysis
Data were organized, categorized, result were presented in tables. Data were analyzed using a compatible personal computer using the Statistical Package for the Social Sciences (SPSS Inc; version 21; IBM Corp., Armonk, NY, USA). The chi-square was used to compare scores preintervention and postintervention (Franke et al., 2012). The correlation coefficient is a numerical measure of some type of correlation, meaning a statistical relationship between two variables. The results were considered significant when the probability of error is less than 5% (p < .05) and highly significant when the probability of error is less than 0.1% (p < .001). The developed tool was tested for its reliability by using Cronbach's alpha test (Nayak & Hazra, 2011).
Results
According to the characteristics of breastfeeding women, the mean age of them was 37.40±5.66 years, more than two-thirds (70%) of them were unemployed and one-fifth (20%) of studied women were had preparatory education and able to read and write. Regarding marital status, most (95%) of the studied women were married. Also, the majority of studied women (86%) did not attend training courses about COVID-19, see more in Table 1.
Table 1.
Distribution of Studied Breastfeeding Mothers Related Their Characteristics (n = 100).
| Items | N | % |
|---|---|---|
| Age: | ||
| 20– < 30 | 18 | 18 |
| 30– < 40 | 40 | 40 |
| 40–50 Mean SD | 42 | 42 |
| 37.40±5.66 | ||
| Employment: | ||
| Employee | 30 | 30 |
| Unemployed | 70 | 70 |
| Educational level: | ||
| Not read and write | 8 | 8 |
| Read and write | 20 | 20 |
| Primary school | 16 | 16 |
| Preparatory school | 20 | 20 |
| Secondary school | 22 | 22 |
| Bachelor education | 14 | 14 |
| Marital status: | ||
| Married | 95 | 95 |
| Divorced | 3 | 3 |
| Widow | 2 | 2 |
| Training courses about coronavirus disease 2019 (COVID-19) | ||
| Yes | 14 | 14 |
| No | 86 | 86 |
| Family income | ||
| Sufficient | 90 | 90 |
| Insufficient | 10 | 10 |
Related knowledge of breast-feeding women, Table 2 reveals that more than one quarter (30%) and (28%) of studied women had satisfactory knowledge of related causes, risk factors and signs, symptoms of COVID-19 at preintervention, while the majority 85% and 86% of them had satisfactory knowledge postintervention at p value <.01**. In addition, less than one-fifth (17%) and (16%) of studied women had satisfactory knowledge about breastfeeding guidelines during COVID-19 and Care of breastfeeding women during COVID-19, compared with most of them (89%) and (92%) postintervention at p-value <.01**.
Table 2.
Distribution of Studied Breastfeeding Mothers Related Satisfactory Knowledge About coronavirus disease 2019 (COVID-19) pre and Post (n = 100).
| Domains | Pre | Post | Chi-square | p-value | ||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Concept of COVID-19 | 23 | 23 | 87 | 87 | 12.083 | <.01** |
| Causes and risk factors of COVID-19 | 30 | 30 | 85 | 85 | 13.044 | <.01** |
| Signs and symptoms of COVID-19 | 28 | 28 | 86 | 86 | 10.888 | <.01** |
| Complication of COVID-19 | 19 | 19 | 93 | 93 | 12.767 | <.01** |
| Ways of prevention COVID-19 infection | 22 | 22 | 90 | 90 | 11.029 | <.01** |
| Breastfeeding guidelines during COVID-19 | 17 | 17 | 89 | 89 | 15.321 | <.01** |
| Care of breastfeeding women during COVID-19 | 16 | 16 | 92 | 92 | 10.999 | <.01** |
Notes: **highly significant <.01, * significant <.05*.
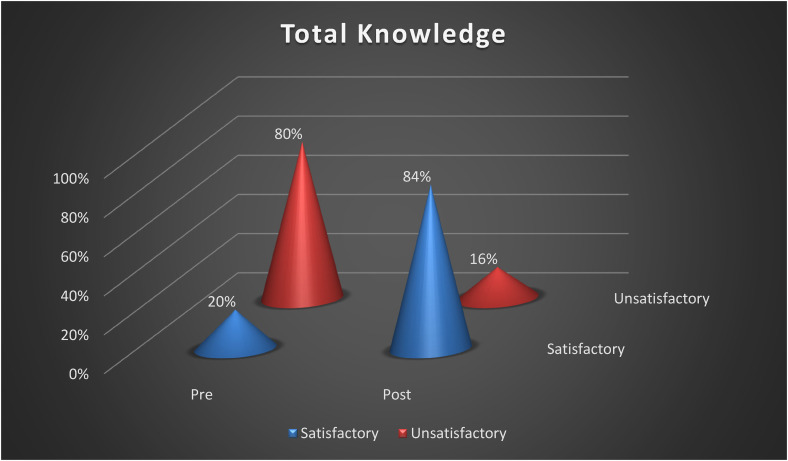
Figure 1 states that more than three-quarters (80%) of studied breastfeeding mothers had unsatisfactory knowledge, while the majority (84%) of them had satisfactory knowledge postintervention with chi-square test was 13.555 at p-value <.01**.
Figure 1.
Distribution of studied breastfeeding mothers related total knowledge about coronavirus disease 2019 (COVID-19) pre and post (n = 100). Note: Chi-square 13.555 p-value <.01**.
According to the practice of breastfeeding women, Table 3 reveals that more than one-third (43%) and (39%) of studied women had satisfactory practice related wash hands before and after touching the infant and avoiding using pump shared by others at preintervention, while the most 98% and 96% of them had satisfactory practice postintervention at p-value <.01**. In addition, less than one-fifth (18%) and (15%) of studied women had satisfactory practice about touching the front of the mask but untie it from behind and replace masks as soon as they become damp compared with most of them (90%) and (87%) at postintervention at p-value <.01**.
Table 3.
Distribution of Studied Breastfeeding Mothers Related Satisfactory Practice About coronavirus disease 2019 (COVID-19) pre and Post (n = 100).
| Domains | Pre | Post | Chi-square | p value | ||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Wash hands before and after touching the infant | 43 | 43 | 98 | 98 | 12.083 | <.01** |
| Avoid using pumps shared by others | 39 | 39 | 96 | 96 | 13.044 | <.01** |
| Wear mask during breastfeeding | 29 | 29 | 95 | 95 | 10.888 | <.01** |
| Clean shared surface in the lactation room before and after use | 25 | 25 | 96 | 96 | 12.767 | <.01** |
| Clean and sanitize breast pumps and all infant feeding items | 23 | 23 | 92 | 92 | 11.029 | <.01** |
| Sneeze or cough into a tissue, immediately dispose of it and use alcohol-based hand rub or wash hands again with soap and clean water | 20 | 20 | 89 | 89 | 15.321 | <.01** |
| Do not touch the front of the mask but untie it from behind | 18 | 18 | 90 | 90 | 10.999 | <.01** |
| Replace masks as soon as they become damp | 15 | 15 | 87 | 87 | 13.808 | <.01** |
Notes: **highly significant <.01, * significant <.05*.
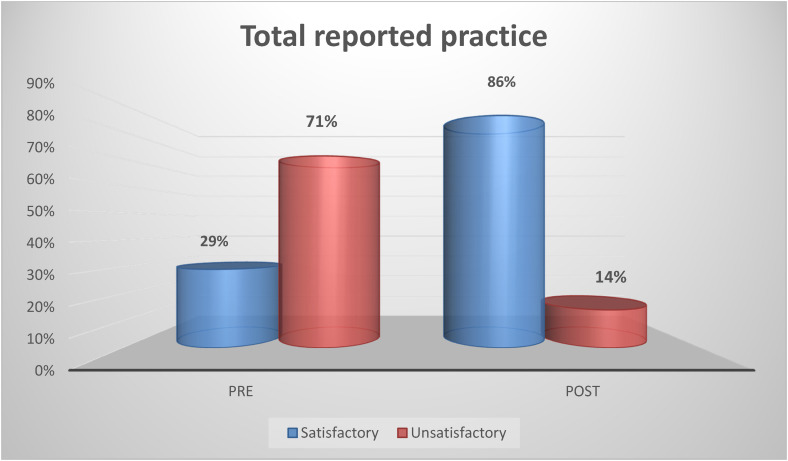
Figure 2 states that more than two-thirds (71%) of studied breastfeeding mothers had unsatisfactory reported practice, while the majority (86%) of them had satisfactory reported practice postintervention with chi-square test was 14.678 at p-value <.01**.
Figure 2.
Distribution of studied breastfeeding mothers related total practice about coronavirus disease 2019 (COVID-19) pre and post (n = 100). Note: Chi-square 14.678 p-value <.01**.
Regarding the correlation between mothers’ knowledge and their practice preintervention, Table 4 shows that there was a high significant correlation at p-value <.01**.
Table 4.
Correlation Between Studied Variable Preinterventions.
| Total knowledge pre | ||
|---|---|---|
| Total reported practice pre | r. p | 0.689 <.01** |
**highly significant <.01**
Regarding the correlation between mothers’ knowledge and their practice postintervention, Table 5 detects that there was a highly significant correlation at p-value <.01**.
Table 5.
Correlation Between Studied Variable Postinterventions.
| Total knowledge post | ||
|---|---|---|
| Total reported practice post |
r. p |
0.750 <.01** |
**highly significant <.01**
Discussion
COVID-19 is reported to have a different impact on women than on men due to women's often central role in caring for the family (Wenham et al., 2020). The COVID-19 pandemic has increased the vulnerability of mothers and young children due to lack of opportunity to have regular contact with healthcare professionals, inaccessibility to breastfeeding counseling facilities, growing myths and misconceptions around breastfeeding during the COVID-19 pandemic, loss of family income, and stress associated with an uncertain future. The impact of COVID-19 on mothers and young children is substantial (Zhu et al., 2020).
Successful execution of the Training Program requires proper guidance, counseling, and breastfeeding education for the mother. The following steps are based on established counseling principles for breastfeeding with necessary modifications applied to COVID-19 (Ng et al.,2020). So, this study aimed to investigate the effect of Training Program on Knowledge and Practice of BreastFeeding Women During COVID-19
In the present work, results prove a significant improvement in breastfeeding knowledge and practice during COVID-19 of the 100-breastfeeding women after a structured education program.
Our results revealed that more than two-thirds of studied breastfeeding mothers had unsatisfactory reported practice, while the majority of them had satisfactorily reported practice postintervention. Furthermore, more than three-quarters of studied breastfeeding mothers had unsatisfactory knowledge, while the majority of them had satisfactory knowledge postintervention. These results may attribute to using different effective teaching/illustrative methods such as slideshow, videos, photo, group discussion and we are preparing the education program dependent on mothers need which are assessed at preassessment test.
These results supported the study by El-Ghany et al., (2022) who founded that less than one-fifth of the total participants had a good level of knowledge score preintervention, compared with 87.50% postintervention with a highly statistically significant difference at t = 18.663, and p < 0.01. Also, agreement with the study by Gonçalves-Ferri et al., (2021) who presented that most of the studied mothers had satisfactory practice postintervention. Additionally, in the same line with the study conducted by Hirani et al. (2021) who reported that improved level of practice among studied mothers after educational program with p value <.01**. Likewise, Abuidhail et al., 2022 mentioned that mothers have misconceptions regarding some modes of transmission, especially through blood and breast milk and the need to increase awareness of breastfeeding mothers regarding preventive measures for COVID-19. Abdelglil et al., 2022 found that there were poor knowledge scores regarding WHO breastfeeding guideline during COVID-19 and recommended conducting an education program for improving knowledge and practice. Also, Brown and Shenker, 2021 found that it is important to reassure and educate breastfeeding mothers about the nature of the disease and the modes of transition. Moreover, Setyowati et al., 2022 detected that there was a difference in knowledge and attitudes among pregnant, postpartum, and lactating women in self-care and prevention regarding the spread of COVID-19 before and after health education via an android application. On other hand, disagreement with a study Adhikari et al., (2020) who detected that the majority of the studied mothers had satisfactory knowledge at preintervention-related causes and signs, symptoms of COVID-19.
Regarding the correlation between mothers’ knowledge and their practice, there was highly significant correlation at p value <.01**. This outcome was in same line with the study conducted by Aduloju et al., (2021) who founded that there was a positive and highly significant correlation between mothers’ knowledge and their practice at p-value <.01**. Also, Kunno et al., 2022 reported that there was correlation analysis performed that found a weak positive correlation between knowledge and practice scores (r = 0.210, p-value = .01). Similarly, Maina et al., 2022 stated that there was positive correlation between knowledge level and their practice level.
Implication for Practice: Further specialized continuous education campaigns are needed to correct misconceptions about practices of breastfeeding during COVID-19 pandemic. Continuous education, feedback, assessment/reassessment are recommended to keep the gained improvement. Also, assessing factors affecting practice of breastfeeding women during COVID-19 pandemic is necessary.
Conclusion
Based on our current study, it was concluded that more than two-thirds of studied breastfeeding mothers had unsatisfactory reported practice, while the majority of them had satisfactory reported practice postintervention. Furthermore, more than three-quarters of studied breastfeeding mothers had unsatisfactory knowledge, while the majority of them had satisfactory knowledge postintervention. Also, improving mothers’ knowledge had a positive effect on their practice level.
Acknowledgments
Great thanks to all mothers who participated in this study.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Ethical approval was provided by the Institutional Review Board of the Faculty of Nursing with ID 287/21.
Informed Consent: Oral consent was obtained from each breastfeeding woman after the researcher informed them about the aim of the study. Moreover, women who agreed to participate in the study were informed that all data gathered during the study were confidential.
ORCID iD: Abdelaziz Hendy https://orcid.org/0000-0003-2960-3465
References
- Abdelglil A. A., Mohamed H. I., Elfeshawy N. I. (2022). Assessment of nurse's knowledge and attitude regarding WHO breastfeeding guideline during COVID-19. Tanta Scientific Nursing Journal, 24(1), 339–359. https://tsnj.journals.ekb.eg/article_221608_a441bd04d135ba7c523895cb4681c097.pdf [Google Scholar]
- Abuidhail J., Tamim F., Abdelrahman R. Y., Al-Shalabi E. (2022). Knowledge and practices of breastfeeding mothers towards prevention of the emerging corona virus (COVID-19). Global Pediatrics, 2(1), 100024. 10.1016/j.gpeds.2022.100024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adhikari S. P., Pariyar J., Sapkota K., Gurung T. K., Adhikari S. R. (2020). Evaluation of knowledge, attitude, practice and hospital experience regarding COVID-19 among postpartum mothers at a tertiary care center: A cross-sectional study. Kathmandu University Medical Journal (KUMJ), 18(70), 10–14. PMID: 33605232. 10.3126/kumj.v18i2.32938 [DOI] [PubMed] [Google Scholar]
- Aduloju O. P., Okunola T. O., Adefisan A. S., Aduloju T. (2021). Knowledge, attitude and practice of preventive measures against coronavirus disease 2019 among pregnant women in a tertiary health facility in southwest Nigeria. Int J Clin Obstet Gynaecol, 5(3), 101–107. 10.33545/gynae.2021.v5.i3b.911 [DOI] [Google Scholar]
- Bastug A., Hanifehnezhad A., Tayman C., Ozkul A., Ozbay O., Kazancioglu S., Bodur H. (2020). Virolactia in an asymptomatic mother with COVID-19. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine, 15(8), 488–491. 10.1089/bfm.2020.0161 [DOI] [PubMed] [Google Scholar]
- Brown A., Shenker N. (2021). Experiences of breastfeeding during COVID-19: Lessons for future practical and emotional support. Maternal & Child Nutrition, 17(1), e13088. 10.1111/mcn.13088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook T. D., Wong V. C. (2008). Better quasi-experimental practice. The Sage handbook of social research methods, 134–164.
- Costantini C., Joyce A., Britez Y. (2021). Breastfeeding experiences during the COVID-19 lockdown in the United Kingdom: An exploratory study into maternal opinions and emotional states. Journal of Human Lactation: Official Journal of International Lactation Consultant Association, 37(4), 649–662. 10.1177/08903344211026565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimopoulou D., Triantafyllidou P., Daskalaki A., Syridou G., Papaevangelou V. (2022). Breastfeeding during the novel coronavirus (COVID-19) pandemic: Guidelines and challenges. The Journal of Maternal-Fetal & Neonatal Medicine : The Official Journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians, 35(19), 3776–3782. 10.1080/14767058.2020.1838481 [DOI] [PubMed] [Google Scholar]
- El-Ghany A., Mustafa G., Hassan L. A. A. (2022). Effect of precaution guidelines on breast feeding women during COVID-19 pandemic in Beni Suef city. Tanta Scientific Nursing Journal, 24(1), 31–53. 10.21608/tsnj.2022.217494 [DOI] [Google Scholar]
- Franke T. M., Ho T., Christie C. A. (2012). The chi-square test: Often used and more often misinterpreted. American Journal of Evaluation, 33(3), 448–458. 10.1177/1098214011426594 [DOI] [Google Scholar]
- Gebretsadik G. G., Tadesse Z., Mamo L., Adhanu A. K., Mulugeta A. (2022). Knowledge, attitude, and determinants of exclusive breastfeeding during COVID-19 pandemic among lactating mothers in Mekelle, Tigrai: A cross sectional study. BMC Pregnancy and Childbirth, 22(1), 850. 10.1186/s12884-022-05186-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giuliani C., Li Volsi P., Brun E., Chiambretti A., Giandalia A., Tonutti L., Di Bartolo P., Napoli A. (2020). Breastfeeding during the COVID-19 pandemic: Suggestions on behalf of woman study group of AMD. Diabetes Research and Clinical Practice, 165(3), 108239. 10.1016/j.diabres.2020.108239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonçalves-Ferri W. A., Pereira-Cellini F. M., Coca K., Aragon D. C., Nader P., Lyra J. C., de Oliveira Pinto R. M. (2021). The impact of coronavirus outbreak on breastfeeding guidelines among Brazilian hospitals and maternity services: A cross-sectional study. International Breastfeeding Journal, 16(1), 1–11. 10.1186/s13006-021-00377-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Govind A., Essien S., Karthikeyan A., Fakokunde A., Janga D., Yoong W., Nakhosteen A. (2020). Re: Novel coronavirus COVID-19 in late pregnancy: Outcomes of first nine cases in an inner-city London hospital. European Journal of Obstetrics and Gynecology and Reproductive Biology, 251(4), 272–274. 10.1016/j.ejogrb.2020.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirani S. A. A., Pearce M., Lanoway A. (2021). Knowledge mobilization tool to promote, protect, and support breastfeeding during COVID-19. Canadian Journal of Public Health = Revue Canadienne de Sante Publique, 112(4), 599–619. 10.17269/s41997-021-00532-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunno J., Yubonpunt P., Supawattanabodee B., Sumanasrethakul C., Wiriyasirivaj B. (2022). Knowledge, attitudes, and practices related to the COVID-19 pandemic among pregnant women in Bangkok, Thailand. BMC Pregnancy and Childbirth, 22(1), 1–11. 10.1186/s12884-022-04612-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubbe W., Botha E., Niela-Vilen H., Reimers P. (2020a). Breastfeeding during the COVID-19 pandemic - a literature review for clinical practice. International Breastfeeding Journal, 15(1), 82. 10.1186/s13006-020-00319-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubbe W., Botha E., Niela-Vilen H., Reimers P. (2020b). Breastfeeding during the COVID-19 pandemic–a literature review for clinical practice. International Breastfeeding Journal, 15(1), 1–9. 10.1186/s13006-020-00319-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maina R., Kimani R. W., Orwa J., Mutwiri B. D., Nyariki C. K., Shaibu S., Fleming V. (2022). Knowledge, attitudes, and preparedness for managing pregnant and postpartum women with COVID-19 among nurse-midwives in Kenya. SAGE Open Nursing, 8(1), 23779608221106445. 10.1177/23779608221106445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nayak B. K., Hazra A. (2011). How to choose the right statistical test? Indian Journal of Ophthalmology, 59(2), 85–86. 10.4103/0301-4738.77005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng Y., Low Y. F., Goh X. L., Fok D., Amin Z. (2020). Breastfeeding in COVID-19: A pragmatic approach. American Journal of Perinatology, 37(13), 1377–1384. 10.1055/s-0040-1716506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacheco F., Sobral M., Guiomar R., de la Torre-Luque A., Caparros-Gonzalez R. A., Ganho-Ávila A. (2021). Breastfeeding during COVID-19: A narrative review of the psychological impact on mothers. Behavioral Sciences, 11(3), 34. 10.3390/bs11030034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S. E. (2020). Epidemiology, virology, and clinical features of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; coronavirus disease-19). Pediatric Infection and Vaccine, 27(1), 1–10. 10.14776/piv.2020.27.e9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira A., Cruz-Melguizo S., Adrien M., Fuentes L., Marin E., Forti A., Perez-Medina T. (2020). Breastfeeding mothers with COVID-19 infection: A case series. International Breastfeeding Journal, 15(1), 69. 10.1186/s13006-020-00314-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piankusol C., Sirikul W., Ongprasert K., Siviroj P. (2021). Factors affecting breastfeeding practices under lockdown during the COVID-19 pandemic in Thailand: A cross-sectional survey. International Journal of Environmental Research and Public Health, 18(16), 8729. 10.3390/ijerph18168729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakalidis V. S., Rea A., Perrella S. L., McEachran J., Collis G., Miraudo J., Prosser S. A., Gibson L. Y., Silva D., Geddes D. T. (2021). Wellbeing of breastfeeding women in Australia and New Zealand during the COVID-19 pandemic: A cross-sectional study. Nutrients, 13(6), 1831. 10.3390/nu13061831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setyowati S., Afiyanti Y., Rachmawati I. N., Sari E. P. (2022). Improving knowledge and attitudes in pregnant, postpartum, and lactating women toward preventing COVID-19 transmission and self-care with health education packages using android applications. Open Access Macedonian Journal of Medical Sciences, 10(G), 625–632. 10.3889/oamjms.2022.8241 [DOI] [Google Scholar]
- Verd S., Ramakers J., Vinuela I., Martin-Delgado M. I., Prohens A., Díez R. (2021). Does breastfeeding protect children from COVID-19? An observational study from pediatric services in Majorca, Spain. International Breastfeeding Journal, 16(1), 1–6. 10.1186/s13006-021-00430-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenham C., Smith J., Morgan R. (2020). COVID-19: The gendered impacts of the outbreak. The Lancet, 395(10227), 846–848. https://doi.org/https:// https://doi.org/10.1016/S0140-6736(20)30526-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO.int. Breastfeeding and COVID-19.2020.Retrieved 6 August 2021, Available from: https://www.who.int/newsroom/commentaries/detail/breastfeeding-and-covid19
- Zhu H., Wang L., Fang C., Peng S., Zhang L., Chang G., Xia S. (2020). Clinical analysis of 10 neonates born to mothers with 2019- nCoV pneumonia. Translational Pediatrics, 9(1), 51–60. 10.21037/tp.2020.02.06 [DOI] [PMC free article] [PubMed] [Google Scholar]