Abstract
Background
Approximately 23% of patients develop hip pain after total hip arthroplasty (THA). In this systematic review, we aimed to identify risk factors associated with postoperative pain after THA to optimize preoperative surgical planning.
Methods
Six literature databases were searched for articles published from January 1995 to August 2020. Controlled trials and observational studies that reported measurements of postoperative pain with assessments of preoperative modifiable and non-modifiable risk factors were included. Three researchers performed a literature review independently.
Results
Fifty-four studies were included in the study for analysis. The most consistent association between worse pain outcomes and the female sex is poor preoperative pain or function, and more severe medical or psychiatric comorbidities. The correlation was less strong between worse pain outcomes and preoperative high body mass index value, low radiographic grade arthritis, and low socioeconomic status. A weak correlation was found between age and worse pain outcomes.
Conclusions
Preoperative risk factors that were consistently predictive of greater/server postoperative pain after THA were identified, despite the varying quality of studies that prohibited the arrival of concrete conclusions. Modifiable factors should be optimized preoperatively, whereas non-modifiable factors may be valuable to patient education, shared decision-making, and individualized pain management.
Keywords: Total hip arthroplasty, Systematic review, Pain, Risk factors
Introduction
Total hip arthroplasty (THA) is highly effective in alleviating pain, restoring function, and improving quality of life in patients with severe hip arthritis. However, approximately 23% of patients develop hip pain after THA [1–4]. Some may even experience no improvement or worse pain postoperatively [2]. Known causes of postoperative pain include loosening of implants, infection, periprosthetic fracture, and soft-tissue abnormalities [3]. However, many cases cannot be explained by radiographic or mechanical abnormalities.
Hip pain following THA is often exacerbated by using stairs, walking on uneven surfaces, sitting for extended periods of time, and standing from a seated position. Factors that may influence hip pain involve both modifiable and non-modifiable risk factors. Modifiable risk factors include body mass index (BMI), certain medical and psychological comorbidities, and select socioeconomic variables. Non-modifiable risk factors may cover age, sex, and race. Identification of these modifiable risk factors of increased postoperative pain is critical in guiding preoperative optimization. Understanding non-modifiable risk factors also has added value in determining surgical expectations, individualizing pain management, and guiding the informed decision-making process.
This systematic review aimed to determine preoperative risk factors that are associated with post-THA pain. Hernández et al. reviewed studies prior to 2013 for predictive factors in total knee and total hip replacements [5]. However, THA and TKA are fundamentally distinct surgeries with well-documented differences in outcomes [6]. To our knowledge, there has been no systematic evaluation of risk factors for postoperative pain specific to THA.
Methods
Search strategy
We developed a comprehensive search strategy according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines with the assistance of a trained librarian. A systematic search was conducted in the PubMed (Medline), Scopus, Web of Science, Cumulative Index of Nursing and Allied Health Literature Plus (EBSCO), Embase, and Cochrane databases by using title, abstract, keywords, and medical subject headings (MeSH). MeSH terms included arthroplasty, replacement, total hip, THA, follow-up, risk assessment, risk factors, reinforcing factors, predictors, pain, postoperative, chronic, long-term, and pain measurement. Title, abstract, and keyword search terms were "hip arthroplasty, THA, THR, hip replacement, OR total hip" AND "after, continue, post, recur, ongoing, chronic, persistent, OR long term" AND "pain" AND "risk, predict, factor, associated, correlate, effect, affect, OR influence". The search strategy was tailored to and optimized for each database.
Inclusion and exclusion criteria
Our review screened for prospective controlled trials, prospective and retrospective observational cohort studies, and case–control studies. The inclusion criteria were full-text articles published between January 1995 and August 2020 with postoperative pain outcomes in only adult THA cases for osteoarthritis with respect to preoperative risk factors. Studies of patients undergoing THA in combination with other large-joint replacement surgeries were included if data specific to THA were provided. The literature review was performed independently by three researchers. Search results were reviewed in order of title, abstract, then full text, and excluded if they did not meet all criteria. Additional relevant studies were identified through a manual search of the bibliographies of selected studies. All other studies that did not assess risk factors, pain, risk factors for pain, or specific THA data were excluded from this analysis.
Bias assessment
Criteria for bias are not well described for systematic reviews of observational studies. We performed a bias assessment for each article based on study design and characteristics. The bias assessment was based on (1) loss to follow-up of <20% before 1 year or <30% after 1 year; (2) consecutive patient selection; (3) multicenter recruitment; and (4) use of univariable or multivariable analysis to adjust for confounders. Studies were rated as high risk (meeting zero or one criterion), medium risk (meeting two criteria), or low risk (meeting three or more criteria). If it was unclear whether a study met a criterion, we assumed that it did not.
Data
Data extracted included study design, patient characteristics, preoperative risk factors, study duration, outcome measurements, postoperative pain outcomes, and criteria for bias assessment. Results for each factor were compared across the studies. Medical or psychological comorbidities, BMI, preoperative pain, and certain socioeconomic elements were considered modifiable factors; whereas, age, sex, and race were deemed as non-modifiable. A descriptive analysis was performed as the heterogeneity of outcome measures and study characteristics prohibited a meaningful meta-analysis.
Patient and public involvement
No patients were involved in determining the research question, outcome measures, or study design. There are no plans to involve patients in the dissemination of research findings.
Results
Study characteristics
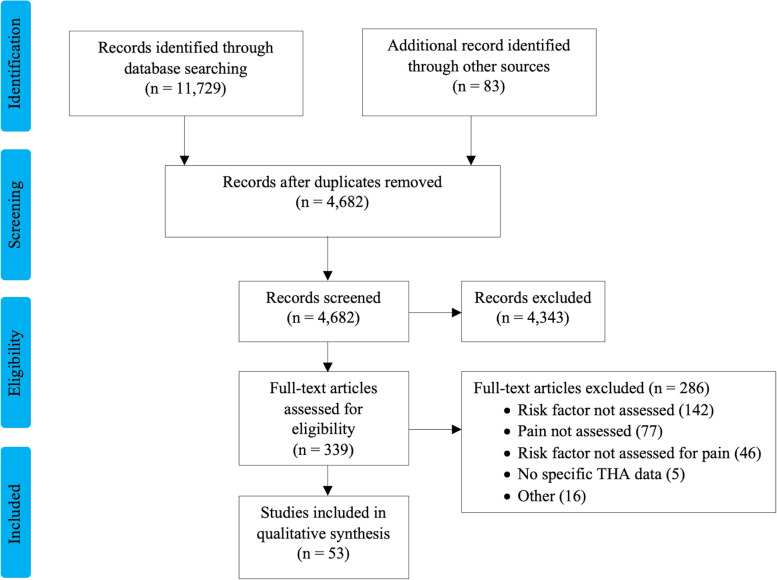
A total of 11,729 studies were identified, including duplicates. The full-text review was performed for 339 publications, and 54 studies satisfied our inclusion criteria (Fig. 1). Most studies were observational cohort studies. The sample size ranged from 54 to 37,393 patients, and follow-up ranged from 24 h to 12 years. Other than in the studies by Busato et al. [7] and Röder et al. [8], THAs were performed in 1993 or later. Commonly evaluated risk factors for postoperative pain were preoperative pain and function (20 studies), medical and psychological comorbidities (18 studies), BMI (13 studies), socioeconomic status and ethnicity (12 studies), sex (11 studies), and radiographic severity of osteoarthritis (4 studies). Functional outcomes were assessed using the Western Ontario and McMaster Universities Arthritis Index (WOMAC), Oxford Hip Score (OHS), Harris Hip Score (HHS), and Hip Disability and Osteoarthritis Outcome Score (HOOS).
Fig. 1.
Flow diagram of a systematic review of articles published from January 1995 to May 2018 about adults undergoing total hip arthroplasty. The databases searched were PubMed (Medline), Scopus, Web of Science, Cumulative Index of Nursing and Allied Health Literature Plus (EBSCO), Embase, and Cochrane
According to the bias criteria, 10 studies had a high risk of bias, 31 had a medium risk, and 13 had a low risk (Table 1). Most studies adjusted for confounders. However, because of the retrospective design of many studies, selection methods and follow-up rates often could not be assessed.
Table 1.
Risk of bias among 53 studies of adult THA
| First author | Year | Consecutive patient selection | Multicenter enrollment | Adequate follow-upa | Adjustment for confounders | Risk of bias |
|---|---|---|---|---|---|---|
| Prentice [9] | 2019 | Yes | Yes | Yes | Yes | Low |
| Goodman [10] | 2018 | Yes | No | Yes | Yes | Low |
| Bedard [11] | 2017 | - | Yes | - | No | High |
| Brembo [12] | 2017 | Yes | Yes | Yes | Yes | Low |
| Li [13] | 2017 | - | Yes | - | Yes | Medium |
| Pinto [14] | 2017 | Yes | - | - | Yes | Medium |
| Dowsey [15] | 2016 | Yes | No | Yes | Yes | Low |
| Goesling [16] | 2016 | - | No | Yes | Yes | Medium |
| Greene [17] | 2016 | - | Yes | - | Yes | Medium |
| Tilbury [18] | 2016 | Yes | No | No | Yes | Medium |
| Lavernia [19] | 2015 | - | No | No | Yes | High |
| Mannion [20] | 2015 | - | - | Yes | Yes | Medium |
| Nam [3] | 2015 | No | Yes | No | No | High |
| Rajamaki [21] | 2015 | No | No | Yes | Yes | Medium |
| Dowsey [22] | 2014 | - | No | - | Yes | High |
| Greene [23] | 2014 | - | Yes | No | Yes | Medium |
| Judge [24] | 2014 | - | Yes | - | Yes | Medium |
| Lavernia [25] | 2014 | Yes | No | - | Yes | Medium |
| Motaghedi [26] | 2014 | No | No | Yes | No | High |
| Petrovic [27] | 2014 | - | Yes | Yes | Medium | |
| Singh [28] | 2014 | Yes | No | - | Yes | Medium |
| Haverkamp [29] | 2013 | Yes | - | Yes | No | Medium |
| Judge [2] | 2013 | Yes | Yes | Yes | No | Low |
| Krupic [30] | 2013 | - | Yes | - | Yes | Medium |
| Neuburger [31] | 2013 | - | Yes | - | Yes | Medium |
| Pinto [32] | 2013 | Yes | No | No | Yes | Medium |
| Singh [33] | 2013 | Yes | No | - | Yes | Medium |
| Singh [34] | 2013 | Yes | No | - | Yes | Medium |
| Jones [35] | 2012 | Yes | Yes | Yes | Yes | Low |
| Liu [36] | 2012 | No | Yes | - | Yes | Medium |
| Smith [37] | 2012 | Yes | - | No | Yes | Medium |
| Allen Butler [38] | 2011 | Yes | - | Yes | No | Medium |
| Clement [39] | 2011 | Yes | No | - | No | High |
| Clement [40] | 2011 | - | No | - | Yes | High |
| Lavernia [41] | 2011 | - | No | Yes | Yes | Medium |
| Lavernia [42] | 2011 | - | Yes | Yes | Yes | Low |
| Johansson [43] | 2010 | - | - | - | No | High |
| Riediger [44] | 2010 | Yes | - | No | No | High |
| Schafer [45] | 2010 | Yes | No | No | Yes | Medium |
| Singh [46] | 2010 | Yes | No | - | Yes | Medium |
| Lavernia [47] | 2009 | - | - | - | Yes | High |
| Quintana [48] | 2009 | - | Yes | Yes | Yes | Low |
| Rolfson [49] | 2009 | - | Yes | - | Yes | Medium |
| Busato [7] | 2008 | - | Yes | - | Yes | Medium |
| Kessler [50] | 2007 | Yes | - | Yes | Yes | Low |
| Röder [8] | 2007 | - | Yes | - | Yes | Medium |
| Moran [51] | 2005 | Yes | No | Yes | Yes | Low |
| Fortin [52] | 2002 | Yes | Yes | Yes | Yes | Low |
| Holtzman [53] | 2002 | - | Yes | No | Yes | Medium |
| Nilsdotter [54] | 2002 | Yes | No | Yes | No | Medium |
| Jones [55] | 2001 | Yes | Yes | Yes | Yes | Low |
| Nilsdotter [56] | 2001 | - | No | Yes | Yes | Medium |
| Meding [57] | 2000 | Yes | No | Yes | Yes | Low |
| Fortin [58] | 1999 | - | Yes | No | Yes | Medium |
“-”: unable to assess
aAdequate follow-up was defined as a loss to follow-up of < 20% before 1 year or < 30% after 1 year
Preoperative BMI
We found that high BMI was associated with worse pain outcomes or increased opioid use after THA in 9 of 13 studies, although conclusions varied regarding its clinical importance (Table 2). Of the studies, 5 had a low risk of bias, 7 had a medium risk, and 1 had a high risk.
Table 2.
Associations of BMI with pain/opioid use after THA
| First author | Year | Study design | n | Follow-up | BMI groups (% of patient) | Outcome measures | Associations of high BMI with postoperative pain/opioid use |
|---|---|---|---|---|---|---|---|
| Prentice [9] | 2019 | RC | 12,560 | 1 yr |
< 30 (60.8); 30–35 (24.5); > 35 (14.6) |
Opioid usage | Greater postoperative opioid use after initial 90-day recovery period |
| Li [13] | 2017 | RC | 2040 | 6 mo |
25–29.9 (37); 30–34.9 (22); 35–39.9 (10); ≥ 40 (4) |
PCS, HOOS | Worse pain at baseline and 6 months, more improvement postoperatively |
| Rajamaki [21] | 2015 | CC | 54 | 1–2 yr | < 30 (53); 30–35 (31); > 35 (16) | Questionnaire | Higher proportion of patients with pain |
| Judge [24] | 2014 | RS | 1431 | 1 yr |
< 25 (33); 25–30 (42); 30–35 (18); 35–40 (5.5); > 40 (1.7) |
OHS | Worse pain, low clinical difference |
| Motaghedi [26] | 2014 | PC | 60 | 1 d | < 25 (33); 25–30 (33); > 30 (33) | VRS | No association |
| Judge [2] | 2013 | PC | 1431 | 1–5 yr |
< 25 (33); 25–30 (42); 30–35 (18); 35–40 (5.5); > 40 (1.7) |
OHS | Worse pain |
| Jones [35] | 2012 | PC | 231 | 3 yr | > 35 (14) | WOMAC | Worse pain at 6 months; no association at 3 years |
| Liu [36] | 2012 | CC | 428 | 1 d | 30a | VAS for pain | Worse pain, low clinical significance |
| Smith [37] | 2012 | PC | 1318 | 3 yr | NA | HHS | Worse pain |
| Singh [46] | 2010 | CC | 5707, 3289 | 2 yr, 5 yr |
< 25 (24); 25–29.9 (39); 30–34.9 (24); 35–39.9 (8); ≥ 40 (1) |
Questionnaire | Worse pain |
| Busato [7] | 2008 | RC | 20,553 | 3, 6, 9, 12 yr | < 25 (38); 25–30 (44); > 30 (18) | Questionnaire | No association |
| Kessler [50] | 2007 | PC | 67 | 10 d, 3 mo | < 25 (16); 25–30 (54); > 30 (30) | WOMAC | No association |
| Moran [51] | 2005 | PC | 800 | 6, 18 mo | 28a (range, 14–49) | HHS | Worse pain |
BMI Body mass index, CC Case control, CI Confidence interval, HHS Harris Hip Score, HOOS Hip Disability and Osteoarthritis Outcome Score, NA Not available, OHS Oxford Hip Score, OR Odds ratio, PC Prospective cohort, PCS Pain catastrophizing scale, RC Retrospective cohort, SD Standard deviation, VAS Visual analog scale, VRS Verbal rating scale
aExpressed as mean BMI
Preoperative pain and hip function
We found that preoperative pain and function were significant predictors of pain or persistent opioid use after THA in 16 of 20 studies (Table 3). Of the studies, 2 had a low risk of bias, 14 had a medium risk, and 4 had a high risk.
Table 3.
Associations of preoperative pain medication or opioid use and function with pain medication or opioid use after THA
| First author | Year | Study design | n | Follow-up | Outcome measures | Associations of poor preoperative pain/function with postoperative pain/opioid use |
|---|---|---|---|---|---|---|
| Prentice [9] | 2019 | RC | 12,560 | 1 yr | Opioid usage | Number of preoperative opioid prescriptions, preoperative NSAID use, back pain, and non-specific chronic pain associated with greater postoperative opioid use |
| Bedard [11] | 2017 | RC | 37,393 | 1 yr | Opioid usage rate | Greater preoperative opioid use associated with greater postoperative opioid use |
| Pinto [14] | 2017 | PC | 64 | 2 d | NRS | No association |
| Goesling [16] | 2016 | PC | 331 | 6 mo | WOMAC | Greater preoperative opioid use associated with greater postoperative pain and opioid use |
| Dowsey [22] | 2014 | PC | 835 | 1 yr | HHS | No association between preoperative pain and postoperative pain; conflicting results for association between preoperative function and postoperative pain |
| Petrovic [27] | 2014 | CC | 90 | 1 d | NRS | Higher odds of postoperative pain |
| Singh [28] | 2014 | RC | 3823 | 2, 5 yr | VAS for pain | Worse pain in patients using a walking aid |
| Haverkamp [29] | 2013 | PC | 189 | 2.3 yra | VAS, WOMAC | Worse pain |
| Judge [2] | 2013 | PC | 1431 | 1–5 yr | OHS | Worse pain |
| Pinto [32] | 2013 | CC | 48 | 4–6 mo | NRS | Higher odds of postoperative pain |
| Singh [33] | 2013 | RC | 3823 | 2, 5 yr | HHS | Worse hip pain with preoperative ipsilateral knee pain |
| Liu [36] | 2012 | CC | 428 | 1 d | VAS for pain | Higher odds of postoperative pain |
| Smith [37] | 2012 | PC | 1318 | 3 yr | HHS | Worse pain |
| Johansson [43] | 2010 | PC | 75 | 2 yr | WOMAC, HHS, SF-36 | Worse pain |
| Lavernia [47] | 2009 | PC | 127 † | 3 yr | WOMAC | Worse pain |
| Röder [8] | 2007 | RC | 13,766 | ≤ 10 yr | VAS for pain | No association |
| Fortin [52] | 2002 | PC | 86 | 2 yr | WOMAC | Worse pain |
| Holtzman [53] | 2002 | PC | 1046 | 1 yr | VAS for pain | Higher odds of postoperative pain |
| Nilsdotter [56] | 2001 | PC | 162 | 1 yr | WOMAC | Worse pain |
| Fortin [58] | 1999 | PC | 116 | 6 mo | WOMAC | Worse pain |
CC Case–control, CI Confidence interval, HHS Harris Hip Score, NRS Numerical rating scale, OHS Oxford Hip Score, OR Odds ratio, PC Prospective cohort, PCS Physical component summary, RC Retrospective cohort, RR Risk ratio, SF-12 12-Item Short-Form Health Survey, SF-36 36-Item Short-Form Health Survey, VAS Visual analog scale, WOMAC Western Ontario and McMaster Universities Arthritis Index
aMean follow-up. †Included THA and total knee arthroplasty cases
Age
We found an association between patient age and pain or opioid use after THA in 9 of 12 studies, but these results were controversial (Table 4). Of these studies, 3 showed older age to be predictive of persistent pain, whereas 5 found young age to be predictive. One study concluded that two opposite age ranges studied were associated with worse pain, and three studies found no association. Notably, 4 studies had a high risk of bias, 3 had a medium risk, and 5 had a low risk.
Table 4.
Associations of patient age with pain/opioid use after THA
| First author | Year | Study design | n | Age, yr | Follow-up | Outcome measures | Associations of older age with postoperative pain/opioid use |
|---|---|---|---|---|---|---|---|
| Prentice [9] | 2019 | RC | 12,560 | 67 (59–75)b | 1 yr | Opioid usage | Less risk of postoperative opioid use |
| Bedard [11] | 2017 | RC | 37,393 | < 50, 2.7% | 1 yr | Opioid use | Less risk of postoperative opioid use |
| Brembo [12] | 2017 | PC | 223 | 69a (41–91) | 3 mo | WOMAC | Worse pain |
| Nam [3] | 2015 | PC | 196 | 50a, SD = 7.1 | 2.9 yr | Pain scale of 0–5 | Less odds of having pain |
| Dowsey [22] | 2014 | PC | 835 | 68a SD = 9.9 | 12 mo | HHS | Better pain |
| Judge [2] | 2013 | RC | 1431 | 70a | 1–5 yr | OHS | Worse pain in patients aged < 60 or > 70 |
| Liu [36] | 2012 | CC | 428 | 67a SD = 11 | 1 d | VAS for pain | Better pain |
| Smith [37] | 2012 | PC | 1318 | 68.5a SD = 9.9 | 3 yr | HHS | Worse pain |
| Clement [39] | 2011 | PC | 171 | > 80 | 1 yr | OHS | No association |
| 495 | 65–74 | ||||||
| Quintana [48] | 2009 | PC | 291 | > 70 | 2 yr | WOMAC | Worse pain |
| 299 | ≤ 70 | ||||||
| Nilsdotter [54] | 2002 | PC | 124 | 71a | 1 yr | WOMAC | No association |
| Jones [55] | 2001 | PC | 197 | 55–79 (83%), ≥ 80 (17%) | 6 mo | WOMAC, SF-36 | No association |
CC Case–control, CI Confidence interval, HHS Harris Hip Score, OHS Oxford Hip Score, OR Odds ratio, PC Prospective cohort, RC Retrospective cohort, SD Standard deviation, SF-36 36-Item Short-Form Health Survey, WOMAC Western Ontario and McMaster Universities Arthritis Index
aData presented as mean
bData presented as median (interquartile range)
Sex
Female gender was a predictor of worse pain or opioid use after THA in 9 of 11 studies (Table 5). There were no studies with a high risk of bias, and three had low risk.
Table 5.
Associations of female sex with pain/opioid use after THA
| First author | Year | Study design | n | Female sex, % | Follow-up | Outcome measures | Associations of female sex with postoperative pain/opioid use |
|---|---|---|---|---|---|---|---|
| Prentice [9] | 2019 | RC | 12,560 | 59 | 1 yr | Opioid usage | Greater opioid use |
| Brembo [12] | 2017 | PC | 223 | 71 | 3 mo | WOMAC | No association |
| Pinto [14] | 2017 | PC | 64 | 59 | 2 d | NRS | Worse pain |
| Mannion [20] | 2015 | RC | 261 | 50 | 1 yr | OHS, WOMAC, SF-12 | No association |
| Petrovic [27] | 2014 | CC | 90 | 47 | 1 d | NRS | Higher odds of pain |
| Liu [36] | 2012 | CC | 428 | 58 | 1 d | NRS | Worse pain |
| Smith [37] | 2012 | PC | 1318 | NA | 3 yr | HHS | Worse pain |
| Lavernia [41] | 2011 | RC | 658 | 59 | 2 yr | HHS, SF-36, WOMAC | Worse pain |
| Singh [46] | 2010 | PC | 5707, 3289 | 51 | 2 yr, 5 yr | Pain medication use | Greater pain medication use |
| Rolfson [49] | 2009 | RC | 6158 | 57 | 1 yr | VAS | Worse pain |
| Quintana [48] | 2009 | PC | 590 | 49 | 2 yr | WOMAC, SF-36 | Worse pain |
CC Case–control, CI Confidence interval, HHS Harris Hip Score, NA Not available, NRS Numerical rating scale, NSAID Nonsteroidal anti-inflammatory drug, OR Odds ratio, PC Prospective cohort, RC Retrospective cohort, SF-12 12-Item Short-Form Health Survey, SF-36 36-Item Short-Form Health Survey, VAS Visual analog scale, WOMAC Western Ontario and McMaster Universities Arthritis Index
Radiographic severity of arthritis
Of the studies investigated, four examined the association between preoperative radiographic severity of arthritis and postoperative pain. We noted that 3 of these studies reported better pain outcomes in patients with severe arthritis, while one study found no predictive value (Table 6). Regarding risk of bias, 2 studies had a low risk and 2 had a medium risk.
Table 6.
Associations of preoperative radiographic severity of arthritis with pain after THA
| First author | Year | Study design | n | Radiographic grade (% patients) | Follow-up | Outcome measures | Associations of higher-grade osteoarthritis with postoperative pain |
|---|---|---|---|---|---|---|---|
| Tilbury [18] | 2016 | PC | 302 | mK-L grade: 1 or 2 (26) mild, 3 or 4 (74) | 1 yr | HOOS, OHS, SF-36 | Greater pain improvement |
| Dowsey [15] | 2016 | CC | 382 | mK-L grade: 2 (1.4), 3a (6.8), 3b (33), 4a (25), 4b (35) | 1 and 2 yr | HHS | Greater odds of pain improvement |
| Nilsdotter [56] | 2001 | PC | 162 | OARSI grade: 3 (70), 2 (29), 1 (1) | 1 yr | WOMAC, SF-36 | No association |
| Meding [57] | 2000 | PC | 1163 | -independent scale | 32 (6–93) moa | HHS | Less pain |
CC Case–control, HHS Harris Hip Score, HOOS Hip Disability and Osteoarthritis Outcome Score, mK-L modified Kellgren and Lawrence grade, OARSI Osteoarthritis Research Society International, OHS Oxford Hip Score, PC Prospective cohort, SF-36 36-Item Short-Form Health Survey, WOMAC Western Ontario and McMaster Universities Arthritis Index
aExpressed as mean (range)
Socioeconomic status and race/ethnicity
Associations of various socioeconomic parameters and race/ethnicity with pain or opioid use after THA were assessed in 12 studies (Table 7). Three studies had a high risk of bias, 6 had a medium risk, and 3 had a low risk. Of these studies, 4 found worse pain in African Americans at 2–3.5 years postoperatively [10, 19, 38, 42]. Reports on the educational level were mixed. Three studies reported that low socioeconomic status was a risk factor for poor pain outcomes after THA [31, 38, 40].
Table 7.
Associations of race/ethnicity and SES with pain/opioid use after THA
| First author | Year | Study design | n | Follow-up, yr | Outcome measures | Associations of race/ethnicity and SES with postoperative pain/opioid use |
|---|---|---|---|---|---|---|
| Prentice [9] | 2019 | RC | 12,560 | 1 | Opioid usage | Higher opioid use in African Americans, lower opioid use in Asian (compared to white) |
| Goodman [10] | 2018 | RC | 4170 | 2 | WOMAC | Worse pain in African Americans |
| Lavernia [19] | 2015 | RC | 564 | 3.5 (1–9)a | VAS, WOMAC, SF-36 | Worse pain in African Americans |
| Dowsey [22] | 2014 | PC | 835 | 1 | HHS | No association |
| Greene [23] | 2014 | RC | 11,464 | 1 | VAS | Worse pain in patients with low education |
| Neuburger [31] | 2013 | RC | 59,680 | 0.5 | OHS | Worse pain in low SES |
| Krupic [30] | 2013 | RC | 1216 | 1 | VAS | Worse pain in immigrants |
| Allen Butler [38] | 2011 | PR | 119 | 2 | VAS, HHS | Worse pain in African Americans, those with low education, and those with low income |
| Lavernia [42] | 2011 | RC | 739 | 2 | WOMAC, SF-36 | Worse pain in minority patients, especially African Americans |
| Clement [40] | 2011 | PC | 1359 | 1 | OHS | Worse pain in more deprived patients |
| Schafer [45] | 2010 | CC | 1113 | 0.5 | WOMAC | Greater odds of poor pain outcome in patients who are single, living alone, on disability |
| Fortin [58] | 1999 | PC | 116 | 0.5 | WOMAC | No association with education level |
CC Case–control, CI Confidence interval, HHS Harris Hip Score, OHS Oxford Hip Score, OR Odds ratio, PC Prospective cohort, PR Prospective randomized, RC Retrospective cohort, SES Socioeconomic status, SF-36 36-Item Short-Form Health Survey, THA Total hip arthroplasty, VAS Visual analog scale, WOMAC Western Ontario and McMaster Universities Arthritis Index
aData presented as mean (range)
Preoperative comorbidities
Seventeen of 18 studies found a negative association between medical or psychological comorbidities and pain after THA or postoperative opioid use (Table 8). Of these, 2 articles had a high risk of bias, 11 had a medium risk, and 5 had a low risk. Psychological comorbidities were another frequently studied risk factor.
Table 8.
Associations of preoperative medical/psychological comorbidities with pain/opioid use after THA
| First author | Year | Study design | n | Follow-up | Outcome measures | Associations of preoperative comorbidities with postoperative pain/opioid use |
|---|---|---|---|---|---|---|
| Prentice [9] | 2019 | RC | 12,560 | 1 yr | Opioid usage | Higher postoperative opioid prescriptions with anxiety, chronic pulmonary disease, substance abuse, acquired immunodeficiency syndrome (AIDS), peripheral vascular disease, chronic blood loss anemia, congestive heart failure |
| Bedard [11] | 2017 | RC | 37,393 | 1 yr | Opioid use | Higher risk postoperative opioid use with preoperative anxiety, depression, drug use, alcohol use, smoking |
| Brembo [12] | 2017 | PC | 223 | 3 mo | WOMAC | Worse pain with increased medical comorbidities |
| Dowsey [15] | 2016 | PC | 382 | 1 and 2 yr | HHS | Worse pain with poor mental function |
| Greene [17] | 2016 | RC | 17,147 | 1 yr | VAS for pain | Worse pain if using antidepressants |
| Rajamaki [21] | 2015 | PC | 54 | 1–2 yr | NRS | Greater odds of pain in diabetes |
| Lavernia [25] | 2014 | RC | 60 | 11 (3–24) mo | HHS | Worse pain in vitamin D insufficiency |
| Petrovic [27] | 2014 | CC | 90 | 1 d | NRS | Higher odds of pain in type D personality, anxiety, depression |
| Dowsey [22] | 2014 | PC | 835 | 1 yr | HHS | Worse pain with increased medical comorbidities |
| Pinto [32] | 2017 | CC | 48 | 4–6 mo | NRS | Worse pain with poor disease process perception and emotional representation |
| Judge [2] | 2013 | PC | 1431 | 1–5 yr | OHS | Worse pain in medical comorbidities |
| Singh [34] | 2013 | PC | 5707, 3289 | 2 yr, 5 yr | VAS for pain | No association |
| Jones [35] | 2012 | PC | 231 | 3 yr | WOMAC | Worse pain with cardiac disease |
| Smith [37] | 2012 | PC | 1318 | 3 yr | HHS | Worse pain with cardiac disease, hypertension, increase medical comorbidities, NSAID use |
| Allen Butler [38] | 2011 | PR | 119 | 2 yr | VAS, HHS, SF-12 | Worse pain with poor mental component score |
| Singh [46] | 2010 | PC | 5707, 3289 | 2 yr, 5 yr | Pain medication use | Greater odds of pain, NSAID use, and opioid use in depression |
| Riediger [44] | 2010 | PC | 79 | 8 wk | WOMAC, SF-36 | Worse pain in depression and somatoform disorders |
| Rolfson [49] | 2009 | RC | 6158 | 1 yr | VAS for pain | Worse pain in anxiety and depression |
ASA American Society of Anesthesiologists, CAD Coronary artery disease, CC Case–control, CCI Charlson Comorbidity Index, CI Confidence interval, HHS Harris Hip Score, HTN Hypertension, NRS Numerical rating scale, NSAID Nonsteroidal anti-inflammatory drug, OHS Oxford Hip Score, OR Odds ratio, PC Prospective cohort, PR Prospective randomized, RC Retrospective cohort, SF-12 12-Item Short-Form Health Survey, SF-36 36-Item Short-Form Health Survey, VAS 10-cm visual analog scale, WOMAC Western Ontario and McMaster Universities Arthritis Index
Discussion
The most consistent association were found between poor pain outcomes and the female sex, high preoperative pain or low function, and various medical or psychiatric comorbidities. Females not only had worse pain at both short- and long-term follow-ups but also had higher odds of severe acute postoperative pain and long-term opioid use. Although this should not affect the patient selection, an effort should be made to optimize multimodal pain management in women to achieve better short-term pain control, decrease chronic pain, and minimize opioid dependence [59]. Postoperatively, multidisciplinary pain therapy has been shown to provide substantial pain relief and may be a valuable referral [60].
Preoperative pain and loss of function are two primary criteria for performing THA; therefore, they cannot be treated like other modifiable factors. A difference should be noted for patients using chronic pain medication, who are at higher risk of postoperative opioid dependence and may benefit from referral to a pain specialist preoperatively for intervention and a weaning protocol at the cost of delaying surgery [11, 16].
Patients with existing comorbidities are more reluctant to undergo elective surgeries [61]. In THA, they also experience increased complications requiring revisions [62]. Notably, patients with diabetes had eight times higher odds of having persistent pain than those without. Other medical comorbidities had a similar effect. Increased odds of acute and chronic pain, as well as opioid dependence, were repeatedly observed in patients with anxiety or depression. Our data suggest that preoperative medical optimization may be beneficial to pain outcomes. Additionally, treating those with active psychiatric conditions may also improve perceived pain and satisfaction [63].
Less consistent association was seen between poor pain outcomes and high BMI, low radiographic grade, and low socioeconomic status. The difference in pain outcomes among BMI groups was often small when compared with the overall improvement. Although most data show worse postoperative pain scores in patients with high BMI, this may be due to greater preoperative pain rather than a less surgical benefit. Nevertheless, weight loss may be beneficial in decreasing baseline pain, ultimately improving postoperative pain [64].
Advanced preoperative radiographic severity of osteoarthritis was mostly found to be associated with worse pain outcomes. Although the data were not robust, they support the current guidelines of attempting non-operative modalities for those with low-grade radiographic arthritis [65].
With respect to race and socioeconomic factors, most studies found worse pain outcomes in African Americans, immigrants, patients with low educational levels, and patients with low socioeconomic status. Additionally, African Americans and patients of lower socioeconomic status had worse pain on presentation. A lack of access to resources, along with health care disparities affecting these populations, likely contribute to a delayed presentation with greater pain from advanced disease or improper non-operative management [66]. Although it is encouraging that these patients achieved similar improvement from surgery as their counterparts, they may still benefit from attention to pain management and preoperative education.
The relationship between age and pain outcomes is less clear. Studies showed that older age could be associated with better, worse, or no difference in postoperative pain. Possible explanations for worse outcomes in younger patients include an increased level of activity and expectations [67]. Conversely, confounding comorbidities and poor recovery may contribute to persistent pain in older patients. Notably, two studies reported worse outcomes in older patients at 3- and 6-month follow-up, whereas, most studies at later time points showed no effect or the opposite. This may be attributed to decreased healing and rehabilitation potential in older patients who are less healthy and less active. Although results conflict, data exist showing both ends of the age spectrum having worse pain outcomes. We may consider holding off surgery in young patients due to worse pain outcomes, in addition to other complications such as early implant failure [68]. Older patients, if they meet surgical criteria, should not delay the operation, or the recovery and rehabilitation potential is diminished.
This is the first systematic review, to our knowledge, that assessed common preoperative risk factors for pain after THA. A strength of this study is that a large number of studies were included, most of which had a low or medium risk of bias. However, there are several limitations to consider. The majority of outcome-based studies are observational cohorts with varying quality and risk of bias. In retrospective studies, appropriate patient selection and loss of follow-up are difficult to assess. Additionally, not all studies adjusted for confounding factors. Most studies reported follow-up of < 2 years, and only two studies continued beyond 5 years. The effects, if any, that these risk factors may have beyond this time frame are impossible to evaluate. Additionally, it is apparent that there is no consensus on an outcome measure for postoperative pain. The differences in the various questionnaires may also be a source of bias. Although some studies reported the effect of risk factors to be small relative to overall improvement from surgery, the heterogeneity of study design and outcome measures prohibited a meaningful meta-analysis to determine the magnitude of effect for each predictive factor. Future outcomes research will benefit from standardized design and outcome measures that allow for meta-analysis and the production of stronger evidence.
Persistent or severe postoperative pain is often difficult to explain and remains a major detriment to overall patient satisfaction and recovery after THA. Identification and management of preoperative risk factors is crucial. Although age, sex, and certain socioeconomic elements cannot be altered, they provide value in the discussion of surgical benefits and patient expectations. Additionally, recognizing patients at higher risk of worse pain outcomes allows the provider to appropriately manage their pain. Over-prescription of opioids is becoming a dangerous epidemic, and more THA patients are relying on them by the year [11]. Referring patients at high risk of postoperative pain to specialists will provide safer and more reliable pain regimens. Finally, these risk factors hold value in surgical decision-making. Modifiable characteristics such as obesity, mental health, and medical comorbidities present the opportunity to improve pain outcomes with preoperative optimization.
Conclusion
We have identified preoperative risk factors that were consistently predictive of greater postoperative pain after THA, despite the varying quality of studies that prohibit reaching concrete conclusions. Modifiable factors should be optimized preoperatively, whereas non-modifiable factors may be valuable to patient education, shared decision-making, and individualized pain management.
Acknowledgements
None.
Authors’ contributions
The corresponding author attests that all listed authors meet authorship criteria and that no others satisfying the criteria have been omitted. Substantial contributions to conception and design: A.S., J.K.O. and B.Z.; Acquisition or analysis of data: A.S. and B.Z.; Interpretation of data: A.S., B.Z., K.L.M., L.H., N.R., J.K.O. and S.R.; Drafting the article: A.S., B.Z., K.M. and R.R.; Revising the article critically for important intellectual content: B.Z., K.L.M., L.H., N.R., J.K.O., S.R. and R.R.. All authors read and approved the final manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. Original data in the form of articles used in this review are available with public access.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Bo Zhang, Email: bo@jhmi.edu.
Sandesh Rao, Email: srao16@jhmi.edu.
Kevin L. Mekkawy, Email: kevin.mekkawy@gmail.com
Anzar Sarfraz, Email: sarfrazanzar@yahoo.com.
Lauren Hollifield, Email: lhollifield92@gmail.com.
Nick Runge, Email: nickrunge34@gmail.com.
Julius K. Oni, Email: joni1@jhmi.edu
References
- 1.Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86:963–74. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Judge A, Arden NK, Batra RN, Thomas G, Beard D, Javaid MK, et al. The association of patient characteristics and surgical variables on symptoms of pain and function over 5 years following primary hip-replacement surgery: a prospective cohort study. BMJ Open. 2013;3(3):e002453. doi: 10.1136/bmjopen-2012-002453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nam D, Nunley RM, Sauber TJ, Johnson SR, Brooks PJ, Barrack RL. Incidence and location of pain in young, active patients following hip arthroplasty. J Arthroplasty. 2015;30:1971–1975. doi: 10.1016/j.arth.2015.05.030. [DOI] [PubMed] [Google Scholar]
- 4.Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012;2:e000435. doi: 10.1136/bmjopen-2011-000435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hernández C, Diaz-Heredia J, Berraquero ML, Crespo P, Loza E, Ruiz Iban MA. Pre-operative predictive factors of post-operative pain in patients with hip or knee arthroplasty: a systematic review. Reumatol Clin. 2015;11:361–380. doi: 10.1016/j.reuma.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 6.DeMik DE, Bedard NA, Dowdle SB, Elkins JM, Brown TS, Gao Y, et al. Complications and obesity in arthroplasty-A hip is not a knee. J Arthroplasty. 2018;33:3281–3287. doi: 10.1016/j.arth.2018.02.073. [DOI] [PubMed] [Google Scholar]
- 7.Busato A, Roder C, Herren S, Eggli S. Influence of high BMI on functional outcome after total hip arthroplasty. Obes Surg. 2008;18:595–600. doi: 10.1007/s11695-007-9412-8. [DOI] [PubMed] [Google Scholar]
- 8.Röder C, Staub LP, Eggli S, Dietrich D, Busato A, Muller U. Influence of preoperative functional status on outcome after total hip arthroplasty. J Bone Joint Surg Am. 2007;89:11–17. doi: 10.2106/00004623-200701000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Prentice HA, Inacio MCS, Singh A, Namba RS, Paxton EW. Preoperative risk factors for opioid utilization after total hip arthroplasty. J Bone Joint Surg Am. 2019;101(18):1670–1678. doi: 10.2106/JBJS.18.01005. [DOI] [PubMed] [Google Scholar]
- 10.Goodman SM, Mehta B, Zhang M, Szymonifka J, Nguyen JT, Lee L, et al. Disparities in total hip arthroplasty outcomes: census tract data show interactions between race and community deprivation. J Am Acad Orthop Surg. 2018;26:e457–e464. doi: 10.5435/JAAOS-D-17-00393. [DOI] [PubMed] [Google Scholar]
- 11.Bedard NA, Pugely AJ, Dowdle SB, Duchman KR, Glass NA, Callaghan JJ. Opioid use following total hip arthroplasty: trends and risk factors for prolonged use. J Arthroplasty. 2017;32:3675–3679. doi: 10.1016/j.arth.2017.08.010. [DOI] [PubMed] [Google Scholar]
- 12.Brembo EA, Kapstad H, Van Dulmen S, Eide H. Role of self-efficacy and social support in short-term recovery after total hip replacement: a prospective cohort study. Health Qual Life Outcomes. 2017;15:68. doi: 10.1186/s12955-017-0649-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li W, Ayers DC, Lewis CG, Bowen TR, Allison JJ, Franklin PD. Functional gain and pain relief after total joint replacement according to obesity status. J Bone Joint Surg Am. 2017;99:1183–1189. doi: 10.2106/JBJS.16.00960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pinto PR, McIntyre T, Araujo-Soares V, Costa P, Ferrero R, Almeida A. A comparison of predictors and intensity of acute postsurgical pain in patients undergoing total hip and knee arthroplasty. J Pain Res. 2017;10:1087–1098. doi: 10.2147/JPR.S126467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dowsey MM, Nikpour M, Dieppe P, Choong PF. Associations between pre-operative radiographic osteoarthritis severity and pain and function after total hip replacement : Radiographic OA severity predicts function after THR. Clin Rheumatol. 2016;35:183–189. doi: 10.1007/s10067-014-2808-7. [DOI] [PubMed] [Google Scholar]
- 16.Goesling J, Moser SE, Zaidi B, Hassett AL, Hilliard P, Hallstrom B, et al. Trends and predictors of opioid use after total knee and total hip arthroplasty. Pain. 2016;157:1259–1265. doi: 10.1097/j.pain.0000000000000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Greene ME, Rolfson O, Gordon M, Annerbrink K, Malchau H, Garellick G. Is the use of antidepressants associated with patient-reported outcomes following total hip replacement surgery? Acta Orthop. 2016;87:444–451. doi: 10.1080/17453674.2016.1216181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tilbury C, Holtslag MJ, Tordoir RL, Leichtenberg CS, Verdegaal SH, Kroon HM, et al. Outcome of total hip arthroplasty, but not of total knee arthroplasty, is related to the preoperative radiographic severity of osteoarthritis. A prospective cohort study of 573 patients. Acta Orthop. 2016;87:67–71. doi: 10.3109/17453674.2015.1092369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lavernia CJ, Villa JM. Does race affect outcomes in total joint arthroplasty? Clin Orthop Relat Res. 2015;473:3535–3541. doi: 10.1007/s11999-015-4481-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mannion AF, Impellizzeri FM, Naal FD, Leunig M. Women demonstrate more pain and worse function before THA but comparable results 12 months after surgery. Clin Orthop Relat Res. 2015;473:3849–3857. doi: 10.1007/s11999-015-4479-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rajamaki TJ, Jamsen E, Puolakka PA, Nevalainen PI, Moilanen T. Diabetes is associated with persistent pain after hip and knee replacement. Acta Orthop. 2015;86:586–593. doi: 10.3109/17453674.2015.1044389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dowsey MM, Nikpour M, Choong PF. Outcomes following large joint arthroplasty: does socio-economic status matter? BMC Musculoskelet Disord. 2014;15:148. doi: 10.1186/1471-2474-15-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Greene ME, Rolfson O, Nemes S, Gordon M, Malchau H, Garellick G. Education attainment is associated with patient-reported outcomes: findings from the Swedish Hip Arthroplasty Register. Clin Orthop Relat Res. 2014;472:1868–1876. doi: 10.1007/s11999-014-3504-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Judge A, Batra RN, Thomas GE, Beard D, Javaid MK, Murray DW, et al. Body mass index is not a clinically meaningful predictor of patient reported outcomes of primary hip replacement surgery: prospective cohort study. Osteoarthritis Cartilage. 2014;22:431–439. doi: 10.1016/j.joca.2013.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lavernia CJ, Villa JM, Iacobelli DA, Rossi MD. Vitamin D insufficiency in patients with THA: prevalence and effects on outcome. Clin Orthop Relat Res. 2014;472:681–686. doi: 10.1007/s11999-013-3172-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Motaghedi R, Bae JJ, Memtsoudis SG, Kim DH, Beathe JC, Paroli L, et al. Association of obesity with inflammation and pain after total hip arthroplasty. Clin Orthop Relat Res. 2014;472:1442–1448. doi: 10.1007/s11999-013-3282-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Petrovic NM, Milovanovic DR, Ignjatovic Ristic D, Riznic N, Ristic B, Stepanovic Z. Factors associated with severe postoperative pain in patients with total hip arthroplasty. Acta Orthop Traumatol Turc. 2014;48:615–622. doi: 10.3944/AOTT.2014.14.0177. [DOI] [PubMed] [Google Scholar]
- 28.Singh JA, Lewallen D. Dependence on walking aids is associated with pain and mobility limitation after total hip arthroplasty. Arthritis Rheumatol. 2014;66:S82. [Google Scholar]
- 29.Haverkamp D, Brokelman RB, van Loon CJ, van Kampen A. Timing of arthroplasty, what is the influence of nocturnal pain and pain at rest on the outcome? Knee Surg Sports Traumatol Arthrosc. 2013;21:2590–2594. doi: 10.1007/s00167-012-2071-x. [DOI] [PubMed] [Google Scholar]
- 30.Krupic F, Eisler T, Garellick G, Karrholm J. Influence of ethnicity and socioeconomic factors on outcome after total hip replacement. Scand J Caring Sci. 2013;27:139–146. doi: 10.1111/j.1471-6712.2012.01013.x. [DOI] [PubMed] [Google Scholar]
- 31.Neuburger J, Hutchings A, Black N, van der Meulen JH. Socioeconomic differences in patient-reported outcomes after a hip or knee replacement in the English National Health Service. J Public Health (Oxf) 2013;35:115–124. doi: 10.1093/pubmed/fds048. [DOI] [PubMed] [Google Scholar]
- 32.Pinto PR, McIntyre T, Ferrero R, Almeida A, Araujo-Soares V. Risk factors for moderate and severe persistent pain in patients undergoing total knee and hip arthroplasty: a prospective predictive study. PLoS ONE. 2013;8:e73917. doi: 10.1371/journal.pone.0073917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singh JA, Lewallen DG. Ipsilateral lower extremity joint involvement increases the risk of poor pain and function outcomes after hip or knee arthroplasty. BMC Med. 2013;11:144. doi: 10.1186/1741-7015-11-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Singh JA, Lewallen DG. Medical comorbidity is associated with persistent index hip pain after total hip arthroplasty. Pain Med. 2013;14:1222–1229. doi: 10.1111/pme.12153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones CA, Cox V, Jhangri GS, Suarez-Almazor ME. Delineating the impact of obesity and its relationship on recovery after total joint arthroplasties. Osteoarthritis Cartilage. 2012;20:511–518. doi: 10.1016/j.joca.2012.02.637. [DOI] [PubMed] [Google Scholar]
- 36.Liu SS, Buvanendran A, Rathmell JP, Sawhney M, Bae JJ, Moric M, et al. Predictors for moderate to severe acute postoperative pain after total hip and knee replacement. Int Orthop. 2012;36:2261–2267. doi: 10.1007/s00264-012-1623-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smith GH, Johnson S, Ballantyne JA, Dunstan E, Brenkel IJ. Predictors of excellent early outcome after total hip arthroplasty. J Orthop Surg Res. 2012;7:13. doi: 10.1186/1749-799X-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Allen Butler R, Rosenzweig S, Myers L, Barrack RL. The Frank Stinchfield award: the impact of socioeconomic factors on outcome after THA: a prospective, randomized study. Clin Orthop Relat Res. 2011;469:339–347. doi: 10.1007/s11999-010-1519-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Clement ND, MacDonald D, Howie CR, Biant LC. The outcome of primary total hip and knee arthroplasty in patients aged 80 years or more. J Bone Joint Surg Br. 2011;93:1265–1270. doi: 10.1302/0301-620X.93B9.25962. [DOI] [PubMed] [Google Scholar]
- 40.Clement ND, Muzammil A, Macdonald D, Howie CR, Biant LC. Socioeconomic status affects the early outcome of total hip replacement. J Bone Joint Surg Br. 2011;93:464–469. doi: 10.1302/0301-620X.93B4.25717. [DOI] [PubMed] [Google Scholar]
- 41.Lavernia CJ, Alcerro JC, Contreras JS, Rossi MD. Patient perceived outcomes after primary hip arthroplasty: does gender matter? Clin Orthop Relat Res. 2011;469:348–354. doi: 10.1007/s11999-010-1503-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lavernia CJ, Alcerro JC, Contreras JS, Rossi MD. Ethnic and racial factors influencing well-being, perceived pain, and physical function after primary total joint arthroplasty. Clin Orthop Relat Res. 2011;469:1838–1845. doi: 10.1007/s11999-011-1841-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Johansson HR, Bergschmidt P, Skripitz R, Finze S, Bader R, Mittelmeier W. Impact of preoperative function on early postoperative outcome after total hip arthroplasty. J Orthop Surg (Hong Kong) 2010;18:6–10. doi: 10.1177/230949901001800102. [DOI] [PubMed] [Google Scholar]
- 44.Riediger W, Doering S, Krismer M. Depression and somatisation influence the outcome of total hip replacement. Int Orthop. 2010;34:13–18. doi: 10.1007/s00264-008-0688-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schafer T, Krummenauer F, Mettelsiefen J, Kirschner S, Gunther KP. Social, educational, and occupational predictors of total hip replacement outcome. Osteoarthritis Cartilage. 2010;18:1036–1042. doi: 10.1016/j.joca.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 46.Singh JA, Lewallen D. Predictors of pain and use of pain medications following primary Total Hip Arthroplasty (THA): 5,707 THAs at 2-years and 3,289 THAs at 5-years. BMC Musculoskelet Disord. 2010;11:90. doi: 10.1186/1471-2474-11-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lavernia C, D'Apuzzo M, Rossi MD, Lee D. Is postoperative function after hip or knee arthroplasty influenced by preoperative functional levels? J Arthroplasty. 2009;24:1033–1043. doi: 10.1016/j.arth.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 48.Quintana JM, Escobar A, Aguirre U, Lafuente I, Arenaza JC. Predictors of health-related quality-of-life change after total hip arthroplasty. Clin Orthop Relat Res. 2009;467:2886–2894. doi: 10.1007/s11999-009-0868-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rolfson O, Dahlberg LE, Nilsson JA, Malchau H, Garellick G. Variables determining outcome in total hip replacement surgery. J Bone Joint Surg Br. 2009;91:157–161. doi: 10.1302/0301-620X.91B2.20765. [DOI] [PubMed] [Google Scholar]
- 50.Kessler S, Kafer W. Overweight and obesity: two predictors for worse early outcome in total hip replacement? Obesity (Silver Spring) 2007;15:2840–2845. doi: 10.1038/oby.2007.337. [DOI] [PubMed] [Google Scholar]
- 51.Moran M, Walmsley P, Gray A, Brenkel IJ. Does body mass index affect the early outcome of primary total hip arthroplasty? J Arthroplasty. 2005;20:866–869. doi: 10.1016/j.arth.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 52.Fortin PR, Penrod JR, Clarke AE, St-Pierre Y, Joseph L, Belisle P, et al. Timing of total joint replacement affects clinical outcomes among patients with osteoarthritis of the hip or knee. Arthritis Rheum. 2002;46:3327–3330. doi: 10.1002/art.10631. [DOI] [PubMed] [Google Scholar]
- 53.Holtzman J, Saleh K, Kane R. Effect of baseline functional status and pain on outcomes of total hip arthroplasty. J Bone Joint Surg Am. 2002;84-A:1942–8. doi: 10.2106/00004623-200211000-00006. [DOI] [PubMed] [Google Scholar]
- 54.Nilsdotter AK, Lohmander LS. Age and waiting time as predictors of outcome after total hip replacement for osteoarthritis. Rheumatology (Oxford) 2002;41:1261–1267. doi: 10.1093/rheumatology/41.11.1261. [DOI] [PubMed] [Google Scholar]
- 55.Jones CA, Voaklander DC, Johnston DW, Suarez-Almazor ME. The effect of age on pain, function, and quality of life after total hip and knee arthroplasty. Arch Intern Med. 2001;161:454–460. doi: 10.1001/archinte.161.3.454. [DOI] [PubMed] [Google Scholar]
- 56.Nilsdotter AK, Aurell Y, Siosteen AK, Lohmander LS, Roos HP. Radiographic stage of osteoarthritis or sex of the patient does not predict one year outcome after total hip arthroplasty. Ann Rheum Dis. 2001;60:228–232. doi: 10.1136/ard.60.3.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Meding JB, Anderson AR, Faris PM, Keating EM, Ritter MA. Is the preoperative radiograph useful in predicting the outcome of a total hip replacement? Clin Orthop Relat Res. 2000;376:156–60. doi: 10.1097/00003086-200007000-00022. [DOI] [PubMed] [Google Scholar]
- 58.Fortin PR, Clarke AE, Joseph L, Liang MH, Tanzer M, Ferland D, et al. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999;42:1722–1728. doi: 10.1002/1529-0131(199908)42:8<1722::AID-ANR22>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 59.Parvizi J, Miller AG, Gandhi K. Multimodal pain management after total joint arthroplasty. J Bone Joint Surg Am. 2011;93(11):1075–84. doi: 10.2106/JBJS.J.01095. [DOI] [PubMed] [Google Scholar]
- 60.Merle C, Brendle S, Wang H, Streit MR, Gotterbarm T, Schiltenwolf M. Multidisciplinary treatment in patients with persistent pain following total hip and knee arthroplasty. J Arthroplasty. 2014;29:28–32. doi: 10.1016/j.arth.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 61.Greene ME, Rolfson O, Gordon M, Garellick G, Nemes S. Standard comorbidity measures do not predict patient-reported outcomes 1 year after total hip arthroplasty. Clin Orthop Relat Res. 2015;473:3370–3379. doi: 10.1007/s11999-015-4195-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jamsen E, Peltola M, Eskelinen A, Lehto MU. Comorbid diseases as predictors of survival of primary total hip and knee replacements: a nationwide register-based study of 96 754 operations on patients with primary osteoarthritis. Ann Rheum Dis. 2013;72:1975–1982. doi: 10.1136/annrheumdis-2012-202064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hirakawa Y, Hara M, Fujiwara A, Hanada H, Morioka S. The relationship among psychological factors, neglect-like symptoms and postoperative pain after total knee arthroplasty. Pain Res Manag. 2014;19(5):251–6. doi: 10.1155/2014/471529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Springer BD, Carter JT, McLawhorn AS, Scharf K, Roslin M, Kallies KJ, Morton JM, Kothari SN. Obesity and the role of bariatric surgery in the surgical management of osteoarthritis of the hip and knee: a review of the literature. Surg Obes Relat Dis. 2017;13(1):111–118. doi: 10.1016/j.soard.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 65.Levine ME, Nace J, Kapadia BH, Issa K, Banerjee S, Cherian JJ, Mont MA. Treatment of primary hip osteoarthritis for the primary care physician and the indications for total hip arthroplasty. J Long Term Eff Med Implants. 2013;23(4):323–330. doi: 10.1615/JLongTermEffMedImplants.2013010251. [DOI] [PubMed] [Google Scholar]
- 66.Youm J, Chan V, Belkora J, Bozic KJ. Impact of socioeconomic factors on informed decision making and treatment choice in patients with hip and knee OA. J Arthroplasty. 2015;30(2):171–175. doi: 10.1016/j.arth.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 67.Bartelt RB, Yuan BJ, Trousdale RT, Sierra RJ. The prevalence of groin pain after metal-on-metal total hip arthroplasty and total hip resurfacing. Clin Orthop Relat Res. 2010;468:2346–2356. doi: 10.1007/s11999-010-1356-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bayliss LE, Culliford D, Monk AP, Glyn-Jones S, Prieto-Alhambra D, Judge A, Cooper C, Carr AJ, Arden NK, Beard DJ, Price AJ. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study. Lancet. 2017;389(10077):1424–1430. doi: 10.1016/S0140-6736(17)30059-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. Original data in the form of articles used in this review are available with public access.