Abstract
In 2021, over 50% of U.S. adults drank alcohol in the past month with over 25% reporting binge drinking, an increase over previous years. Alcohol use is associated with increased risk of accidents, poor birth outcomes, cancer, chronic diseases, and mortality. During the COVID-19 pandemic alcohol consumption and alcohol-related deaths increased. National organizations recommend screening for unhealthy alcohol use in general health care settings as a prevention strategy.
This observational study examined alcohol screening rates in primary care practices in Boston, MA in the context of the COVID-19 pandemic, from July 2019 through May 2022. Screening rates were mapped, by month, to the number of COVID-19 cases. Alcohol screening dropped substantially during the first COVID-19 surge but steadily increased to baseline between the second and third surges. This decline was likely due to competing pandemic-related priorities (e.g., testing, urgent care) and the transition to telemedicine. While some health screening cannot be completed virtually, screening for alcohol is possible. Innovative workflow strategies (e.g., pre-visit screening via patient portals, support staff screening using virtual rooming processes) should be considered to avoid future interruptions of screening for unhealthy alcohol use in primary care.
Keywords: Covid-19, Alcohol, Screening, Observational study, Case counts, Behavioral health
1. Introduction
In 2021, over 50% of U.S. adults drank alcohol in the past month with over 25% reporting binge drinking (Substance Abuse and Mental Health Services Administration., 2021). Alcohol use is associated with increased risk of accidents, poor birth outcomes including fetal alcohol spectrum disorders, cancer, chronic diseases, and mortality. During the COVID-19 pandemic alcohol consumption (Roberts et al., 2021) and alcohol-related deaths increased (White et al., 2022). Prevention efforts include annual, universal alcohol screening and counseling (US Preventive Services Task Force et al., 2018). According to Lin et al. (Lin et al., 2020), “the COVID-19 pandemic led to a dramatic shift in operational priorities from improving general population health and chronic disease management to identifying patients with and at risk for the virus.” Due to this shift in primary health care priorities and changes in healthcare delivery (Cortez et al., 2021) (i.e., in-person to telemedicine), as well as concerns about increases in alcohol consumption and alcohol-related harms during the pandemic, we examined alcohol screening rates during COVID-19 surges in an urban health system.
2. Methods
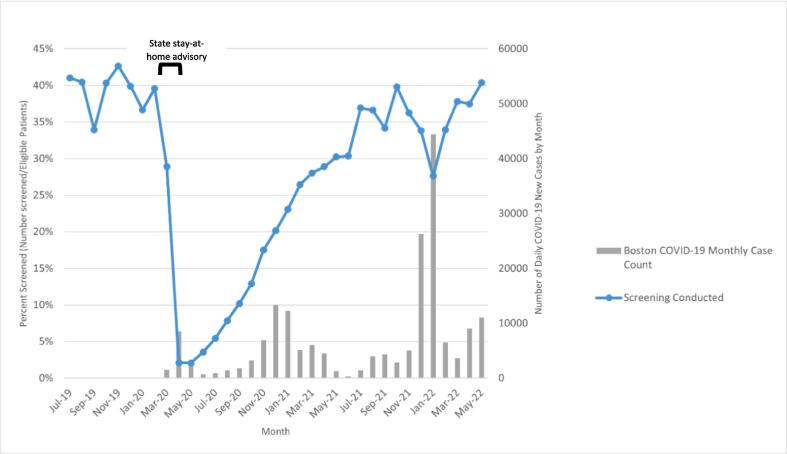
The validated National Institute of Alcohol Abuse and Alcoholism (NIAAA) Single Item Alcohol Screening Question (SISQ) “How many times in the past year have you had X or more drinks in a day, where X is 5 for men and 4 for women, and the response of greater than 1 is considered positive” (Smith et al., 2009) was used to screen for unhealthy alcohol use (Saitz, 2005) within this system and documented in the Electronic Medical Record (i.e., Epic® or OCHIN Epic®). The SISQ is sensitive and specific for the detection of unhealthy alcohol use (including both risky drinking and alcohol use disorder) (Smith et al., 2009). Alcohol screening rates were obtained from a centralized repository of EMR-sourced clinical data in six primary care practices in an urban safety net health system including four community health centers and two hospital-based clinics in Boston, MA from July 2019 through May 2022. This time-period captures 8 months pre-pandemic through 2 years during the pandemic. Monthly aggregated data was reported as a proportion of the number of adults who were eligible and screened (numerator) over the number who attended a visit (in-person or virtual) and were due for annual screening (denominator). Both in-person and virtual screenings were captured in the EMR in the same way and were not differentiated in this dataset. COVID-19 cases in Boston were obtained from a publicly available tracking system (Boston Public Health Commission, 2022) during the same time-period. Screening rates for the participating clinics were mapped, by month, to the COVID-19 cases (Fig. 1). Screening rate data reflect a smaller geographic area (specific clinics in Boston) than COVID-19 cases (all Boston neighborhoods) but still allows for investigation of trends. Data were analyzed in Excel and pivot tables constructed to produce the figure. Approved by the Boston University Medical Campus and Boston Medical Center Institutional Review Board.
Fig. 1.
Monthly Alcohol Screening Rates and COVID-19 Case Counts, Boston MA, July 2019-May 2022.
3. Results
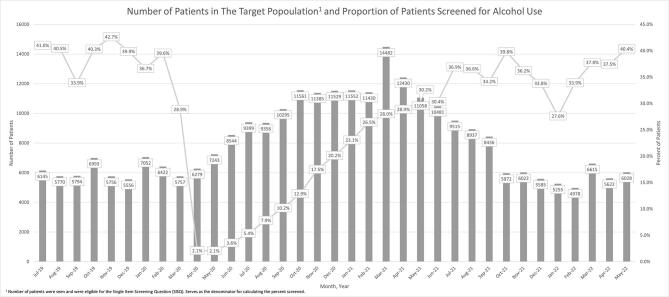
In the eight months prior to the pandemic when the project began data collection (July 2019 through February 2020), the six urban clinics in this study had a monthly average of 6,186 patients (range of 5,556–7,052 patients) seen who were eligible for annual alcohol screening. During the pandemic, from March 2020 to May 2022, the number of patients who were seen and eligible was higher than usual in the first year and a half and then leveled off to pre-pandemic totals (Mean = 8,846, range of 4,978–14,482). Supplemental material has been provided to show these trends.
Prior to the pandemic, alcohol screening rates in participating clinics remained around 40% from July 2019 through February 2020. Changes in screening began in March 2020 coinciding with the state COVID-19 stay-at-home advisory. Screening rates decreased to 2.1% in April and May 2020, during the first spike in COVID-19 cases (8,475 and 3,081 respectively). Screening rates steadily increased to pre-pandemic rates (39.8%) after the stay-at-home advisory ended through the next year (June 2020 to June 2021) despite additional COVID-19 surges. Screening rates decreased to 34.2% in the summer/fall of 2021 as an increase in COVID-19 cases occurred due to the Delta variant. Screening fell to 33.8% in December 2021 as COVID-19 cases (26,308) rose considerably from the previous month (5,030 in November 2021). A more significant dip in screening (27.6%) occurred during the spread of the Omicron variant resulting in unparalleled COVID-19 cases (44,431 in January 2022). After that dramatic increase in cases, screening rates rebounded quickly to pre-pandemic rates of 40.4% by May 2022.
4. Discussion
In this novel study we found that alcohol screening in an urban health system in the United States dropped substantially during the first COVID-19 surge but steadily increased to baseline between the second and third surges. This decline in screening rates occurred during higher than usual visits during the pandemic and was likely due to competing pandemic-related priorities (e.g., testing, urgent care) and the transition to telemedicine (Chudasama et al., 2020). While most routine preventive health screenings cannot be completed virtually (e.g., mammogram, colonoscopy), virtual screening for alcohol is possible but with potential challenges (Ghosh and Sharma, 2021). While not directly examined, we hypothesize about several pandemic-specific challenges to alcohol screening at the patient, clinician, and system-level. During the early stages of the pandemic, urgent care issues were likely prioritized by both patients and clinicians over routine health care maintenance. Shifting to telemedicine also likely impacted alcohol screening at the clinician- and system-level. During virtual visits clinicians are often responsible for all aspects of patient care without the assistance of support staff who regularly oversee and/or perform behavioral health screening (Mertens et al., 2015). There were likely other changes in policies and guidelines within or outside the health system throughout the study period that could have impacted screening rates. Later surges had less impact on screening rates likely due to return of some in-person team-based care, less focus on COVID-related issues during visits and improvements in telemedicine workflows. Some recommended improvements in virtual visits include pre-visit planning (e.g., identifying screening needs) and inter-visit care management (e.g., obtaining self-administered screening data) (Lin et al., 2020, Kamath et al., 2022). While it is possible that increased awareness of alcohol-related harms may have contributed to a return to baseline levels of screening, if this was a primary reason, one would expect alcohol screening to increase above pre-pandemic rates which was not the case in this study.
This study has several limitations. First, as an observational study we cannot demonstrate causality between COVID-19 surges and screening frequency, yet there was an observed pattern of an inverse relationship between COVID-19 cases and screening rates. Second, we do not have patient or provider-level demographics, which doesn’t allow targeted questions about context. While we are unable to adjust for variables not included in the datasets, the data does represent the same general population for the numerator and denominator. Our dataset does not distinguish between in-person versus virtual visits and therefore we were unable to investigate differences in visit type. Finally, we used screening data from the EMR, which relies on accurate provider and staff data entry into the EMR.
Despite the limitations, this study has several strengths. First, the ability to examine smaller time intervals (monthly) allowed us to investigate trends during a time when the context was changing daily and the need for discrete units of time was necessary to observe shifts. Second, both datasets (alcohol screening and COVID-19 cases) represent a population from the same geographic region and over the same time-period; extrapolation of data was unnecessary. Third, we were able to examine screening across multiple clinics due to similarities in EMR and data definitions. Finally, the data collection included time points both before and during the pandemic.
5. Conclusion
Due to the importance of prevention through regular alcohol screening, especially given the increases in alcohol related morbidity and mortality during the pandemic, innovative workflow strategies (e.g., pre-visit screening via patient portals, support staff screening using virtual rooming processes) should be considered and prioritized to avoid interruptions of screening for unhealthy alcohol use in primary care. Future research should explore whether the frequency of screening was different between telemedicine and in-person visits during the same time-period as well as broader explorations of patient-, clinician- and system-level causes for the changes observed. Use of rigorous study designs, such as interrupted time series that allow investigation of impacts across time and settings would provide a deeper understanding about the changes in alcohol screening and effective clinical protocols to avoid disruptions.
CRediT authorship contribution statement
Daniel P. Alford: Conceptualization, Writing – original draft. Jacqueline S. German: Writing – review & editing. Candice Bangham: Data curation, Visualization, Formal analysis, Writing – original draft. Amy Harlowe: Writing – review & editing. Jacey Greece: Conceptualization, Data curation, Writing – original draft.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: None of the authors have any possible, perceived or real financial conflicts of interest or partnerships with commercial interests.
Acknowledgments
Approved by the Boston University Medical Campus and Boston Medical Center Institutional Review Board: expedited review. Funding provided by the U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, cooperative agreement number NU84DD000002.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2023.102197.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Supplementary figure 1.
Data availability
Data will be made available on request.
References
- Boston Public Health Commission, 2022. Boston COVID-19 Dashboard https://bphc-dashboard.shinyapps.io/BPHC-dashboard/ (accessed 1/31/2023).
- Chudasama Y.V., Gillies C.L., Zaccardi F., Coles B., Davies M.J., Seidu S., Khunti K. Impact of COVID-19 on routine care for chronic diseases: a global survey of views from healthcare professionals. Diabetes Metab. Syndr. 2020;14(5):965–967. doi: 10.1016/j.dsx.2020.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortez C, Mansour O, Qato DM, Stafford RS, Alexander GC. Changes in short-term, long-term, and preventive care delivery in the US office-based and telemedicine visits during the COVID-19 pandemic. JAMA Health Forum 2021;2(7):e211529:1-11. [DOI] [PMC free article] [PubMed]
- Ghosh A., Sharma K. Screening and brief intervention for substance use disorders in times of COVID-19: potential opportunities, adaptations, and challenges. Am. J. Drug Alcohol Abuse. 2021;47(2):154–159. doi: 10.1080/00952990.2020.1865996. [DOI] [PubMed] [Google Scholar]
- Kamath C.C., Kelpin S.S., Patten C.A., Rummans T.A., Kremers H.M., Oesterle T.S., Williams M.D., Breitinger S.A. Shaping the screening, behavioral intervention, and referral to treatment (SBIRT) model for treatment of alcohol use disorder in the COVID-19 era. Mayo Clin. Proc. 2022;97(10):1774–1779. doi: 10.1016/j.mayocp.2022.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin S., Sattler A., Smith M. Retooling primary care in the COVID-19 era. Mayo Clin. Proc. 2020;95(9):1831–1834. doi: 10.1016/j.mayocp.2020.06.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertens J.R., Chi F.W., Weisner C.M., Satre D.D., Ross T.B., Allen S., Pating D., Campbell C.I., Lu Y.W., Sterling S.A. Physician versus non-physician delivery of alcohol screening, brief intervention and referral to treatment in adult primary care: the ADVISe cluster randomized controlled implementation trial. Addict. Sci. Clin. Pract. 2015;10(1) doi: 10.1186/s13722-015-0047-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts A., Rogers J., Mason R., Siriwardena A.N., Hogue T., Whitley G.A., Law G.R. Alcohol and other substance use during the COVID-19 pandemic: a systematic review. Drug Alc Depend. 2021;229:109150. doi: 10.1016/j.drugalcdep.2021.109150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R. Unhealthy alcohol use. N. Engl. J. Med. 2005;352(6):596–607. doi: 10.1056/NEJMcp042262. [DOI] [PubMed] [Google Scholar]
- Smith P.C., Schmidt S.M., Allensworth-Davies D., Saitz R. Primary care validation of a single-question alcohol screening test. J. Gen. Intern. Med. 2009;24(7):783–788. doi: 10.1007/s11606-009-0928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. 2021. Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health (HHS Publication No. PEP21-07-01-003, NSDUH Series H-56). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/ (accessed 1/31/2023).
- US Preventive Services Task Force, Curry S.J., Krist A.H., Owens D.K., Barry M.J., Caughey A.B., Davidson K.W., Doubeni C.A., Epling J.W., Jr, Kemper A.R., Kubik M., Landefeld C.S., Mangione C.M., Silverstein M., Simon M.A., Tseng C.W., Wong J.B. Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults: us preventive services task force recommendation statement. J. Am. Med. Assoc. 2018;18:1899–1909. doi: 10.1001/jama.2018.16789. [DOI] [PubMed] [Google Scholar]
- White A.M., Castle I.P., Powell P.A., Hingson R.W., Koob G.F. Alcohol-related deaths during the COVID-19 pandemic. J. Am. Med. Assoc. 2022;17:1704–1706. doi: 10.1001/jama.2022.4308. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.