Abstract
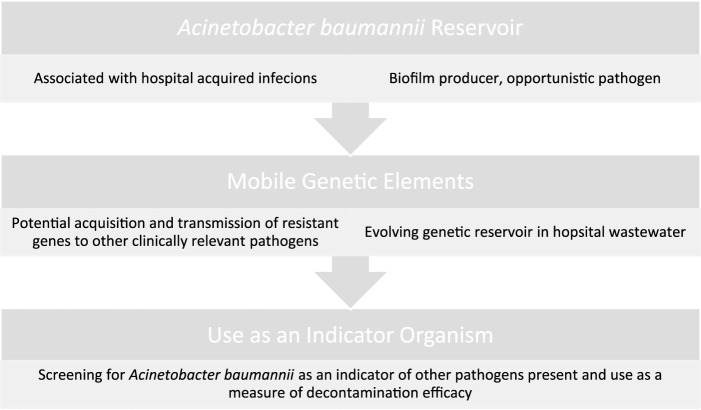
Environmental contamination is estimated to contribute to up to 20% of all hospital acquired infections. Acinetobacter baumannii is an example of one the most prevalent opportunistic pathogens causing severe and persistent infections in immunocompromised patients. It has proven ability to form biofilms, has significant associated multi-drug resistance and is able to transfer mobile genetic elements to other clinically relevant pathogens. All of these factors point to a definite utility of A. baumannii as an indicator organism for effectiveness of decontamination regimens as well as environmental screening. There is an increased cost, both financial and clinical, associated with multi drug resistant organisms, carbapenem resistant A. baumannii. With a dearth of new antimicrobials in development, now is the time to radically transform and lead the introduction of scientifically based environmental screening and microbiological verified decontamination to control the dissemination of further resistance.
Keywords: Acinetobacter, environmental screening, multi-drug resistance, indicator organism, microbiological decontamination
Introduction
There is increasing evidence to suggest that environmental contamination of hospital surfaces contributes significantly to the spread of pathogens, including Multi-Drug Resistant Organisms (MDROs) such as carbapenemase producing Gram-negative Enterobacterales (1). Indeed, there is a growing body of evidence to suggest that hospitals and long-term care facilities, are a rich reservoir of MDROs which have the potential to infect vulnerable patients (2). Screening and infection control measures for such organisms are inconsistent at best, with little or no official guidance as to what preventative screening should be implemented. The National Health Service’s (NHS) specifications for Cleanliness, for example, outlines only general monitoring of hospital environments to be assessed by visible audit, with no recommendation for microbiological screening (3). Similarly lacking, the Irish Health Service Executive’s (HSE) national cleaning standard is based on a 2005 evaluation (4). This current deficit in environmental screening is likely attributable to the extra financial cost of such screens (5) and over-stretched infection prevention and control (IPC) teams, together with the already significant burden of an increasing workload of greater complexity in understaffed microbiology laboratories (6). Nonetheless, environmentally acquired pathogens continue to pose a real and present risk in the form of environmental reservoirs that all too often go unnoticed (7). Immunocompromised patients and those with increased lengths of hospital stays are most at risk (8). The focus of the current review is to highlight the rising problem of one such bacterial strain, using multi drug resistant Acinetobacter baumannii as a model organism of environmental contamination. A. baumannii represents an ideal indicator organism of such environmental reservoirs as it is stress resistant (9), antibiotic resistant (10), a widely attributed opportunistic pathogen (11) and a definite source of virulence genes that have the potential to be acquired by other, clinically relevant pathogens (12).
Impact of Hospital Acquired Infections
A point prevalence study on Hospital Acquired Infections (HAIs) conducted by the European Centre for Disease Prevention and Control (ECDC) across 33 countries in 2011/12, reported a 5.5% HAI prevalence for Europe, 5.9% for the United Kingdom and 5.2% for Ireland (13). This was updated further in 2017 with a Eurosurveillance study carried out on hospitals and long-term care facilities (LTCF). The HAI prevalence on this occasion was 6.1% for Ireland, 6.4% for England and 5.6% for the UK; indicating that both countries are above the previously reported European average. The prevalence of HAIs was highest in intensive care units (24%) and surgical wards (9.1%). The top four types of HAIs documented are pneumonia (28.9% of all HAIs), surgical site infections (18.1%), urinary tract infections (1.5%), and bloodstream infections (9.9%) (14). The economic cost of these HAIs was estimated to be ∼€7 billion per annum in Europe alone, a decade ago (13). The direct risk posed to a patient by a lack of environmental cleanliness, particularly in terms of microbial contamination, is difficult to determine. There are, however, strong links with cross-transmission of pathogens from healthcare workers’ hands, or from indirectly touching contaminated surfaces (15). Herein, we focus on A. baumannii as an indicator organism of environmental contaminants, which in turn represent a significant reservoir of HAIs.
Survivability of Acinetobacter baumannii
A.baumannii are non-motile, non-fastidious, non-fermentative, catalase-positive, oxidative-negative Gram-negative coccobacilli that are most often associated with aquatic environments (16, 17). Responsible for approximately 2%–10% of all Gram negative hospital acquired infections (18), A. baumannii in particular is an extremely stress resistant opportunistic pathogen, with the ability to survive for prolonged periods in the hospital environment, and on medical devices (17). A key virulence and stress associated factor in A. baumannii are OmpA, a member of the outer membrane proteins (OMPs) which causes mitochondrial dysfunction, leading to cell apoptosis (9). The same OmpA surface protein is responsible for the formation of biofilms, a key survival mechanism of Acinetobacter baumannii in the environment (19). The ability of Acinetobacter to colonise and produce biofilms on surfaces leads to chronic and persistent infections, antibiotic resistance, and increased survival in hospital environments (20). Factors controlling biofilm formation include nutrient availability, the presence of pili and outer membrane proteins and macromolecular secretions (19). It has been observed that plasmids and biofilm structure/functions are intertwined through complex interactions, with recent research revealing that lateral gene transfer and biofilm formation are connected processes (21). The horizontal transfer of mobile genetic elements (MGEs) is enhanced by biofilms promoting plasmid stabilisation with horizontal transfer rates being higher in biofilm communities compared with those in planktonic states (21). Biofilm related, ventilator-associated Acinetobacter pneumonia can also be extremely resistant to antibiotics, representing a serious challenge to the clinical management of infections (22). A study by Perez et al. at a New Jersey hospital showed an increase in carbapenem resistant A. baumannii (CRAB) during a surge in COVID-19 which resulted in an increase in ventilator dependent patients (23). Another US study demonstrated that patients colonised with A. baumannii on admission to ICU were 15.2 times more likely to develop a subsequent positive clinical culture and are 1.4 times more likely to die during hospitalisation (24), highlighting the pressing need to definitively ascertain the link between environmental reservoirs and patient transmission potential.
Acinetobacter baumannii—Mechanisms of Resistance
In addition to the direct threat posed by A. baumannii as an opportunistic pathogen, it also represents an important reservoir of stress resistance genes and virulence associated factors, such as ompA, which when acquired by lateral gene transfer can significantly bolster survival and virulence potential when expressed phenotypically by other clinically relevant pathogens (12). In addition to environmental stress tolerance, A. baumannii has also been shown to be extremely antibiotic resistant, with resistance to third generation cephalosporins and carbapenems being reported as early as the 1980s; a phenotype which is known to result from a variety of different genetic mechanisms (10). Horizontal gene transfer can occur by three mechanisms known as transformation, transduction, and conjugation (25). Mobile genetic elements (MGEs) such as bacteriophages, plasmids and conjugative transposons are used during horizontal gene transfer of foreign DNA between bacteria in the same environment (26), with conjugation being the driving force in acquisition of exogenous DNA in Acinetobacter spp. (11). blaOXA23, an acquired subgroup of carbapenem-hydrolysing class D β-lactamases (CHDLs), can be inserted both in the chromosome and in plasmids and can inactivate carbapenems, is now widely distributed in A. baumannii (27). A 2014 report by La et al. describes the unusual detection of a blaOXA23 in a clinical Escherichia coli isolate (28). This was the first description of a plasmid borne blaOXA23 in E. coli and was detected as part of a national surveillance of non-carbapenem susceptible Enterobacterales. Comprehensive PCR sequencing confirmed the blaOXA23 had 100% identity to the A. baumannii blaOXA23. Southern blot hybridization located the blaOXA23 on a 50-kb plasmid, which was shown to be conjugative (28). This concerning discovery re-emphasises the importance of controlling carbapenemase dissemination from non-carbapenemase producing bacteria. Huang et al. reported isolating E. coli, Citrobacter freundii and A. baumannii from the same patient. All isolates had acquired a bla NDM-1 gene, a known carbapenemase producing gene, suggesting gene transfer in same environments (29). A Swiss study also reports the presence of the bla NDM-1 gene in Enterobacterales located on conjugative IncA/C- or IncF-type plasmids. Part of ISAba125, an insertion sequence which causes resistance to third generation cephalosporins and located upstream of ampC gene was present on the plasmid. ISAba125 has previously been identified in bla NDM-1 negative A. baumannii, suggesting that the original source was A. baumannii (30). There is a possibility that horizontal transfer of chromosomally located resistance genes occurs more commonly than previously thought. Furthermore, Maeusli et al showed environmental Acinetobacter baylyi is capable of transferring plasmids harbouring resistance genes to clinical isolates of E. coli on lettuce leaves (31). Interestingly, the same strain of E. coli could colonise the gut microbiome of mice with in vivo transfer of the plasmid to Klebsiella pneumoniae within 5 days (31).
It has been shown that most chronic infections are now biofilm related (32) with bacteria residing in mature biofilms being better protected against antibiotic exposure than their free-living counterparts. Plasmids enhancing survivability of their hosts will therefore enhance their own persistence (21). Dense communities of biofilms expediting the spread of MGEs through a spatial and structural advantage is thought to increase conjugation in biofilm communities (21). Plasmids which are maintained through high transfer frequencies, may only be able to persist in biofilms (33) as conjugation occurs at higher frequencies in biofilm communities. As A. baumannii is an established biofilm forming bacterium, it was proposed that the transfer of bla NDM-1 plasmids could potentially occur more readily in this environment (34). Three clinical and environmental Enterobacterales strains carrying bla NDM-1 were mated to form E. coli J53 bla NDM-1 transconjugants. Donor biofilm A. baumannii showed the successful uptake of the E. coli J53 bla NDM-1 transconjugants in two of the three strains, demonstrating the potential for NDM spread in clinical and environmental settings (34).
Antibiotic release into the environment via human, veterinary and agricultural waste likely represents a significant contributor to the emergence and maintenance of resistance (35). Antibiotic concentrations vary in natural environments, including wastewater from pharmaceutical industries or hospitals, with fluroquinolones frequently reaching the highest levels in milligrams per millilitre concentrations (35). Even at the very low antibiotic concentrations which are present in natural environments, it is sufficient for the maintenance of pre-existing resistant bacterial strains, along with the de novo selection of new mutants (35). A wastewater treatment study by Higgins et al. in Zagreb, Croatia, over a 1-year period concluded that 102/119 A. baumannii isolates retrieved from various stages of wastewater treatment were carbapenem resistant (36). Viable A. baumannii complex isolates are constantly being emitted via effluent into the environment and can survive the technological process of anaerobic mesophilic sludge digestion (36). This further supports the potential community dissemination of antibiotic resistance. Antibiotic resistant Acinetobacter spp. including A. baumannii have also been recovered from vegetables which may provide an additional route into hospitals (37).
Environmental Screening in a Hospital Setting
It is estimated that up to 20% of HCAIs can be attributed to environmental contamination (38). Generally, hospital environments are only sampled in response to an outbreak with routine sampling not usually indicated for healthcare environments. Hospital surface environments act as a reservoir for pathogens where prior room occupants shed organisms onto their environment, posing a risk to the next occupant (see Figure 1). Where the cleaning is sub-optimal, patients have an increased risk of acquiring a HAI when a previous patient has been colonised (39). Most hospitals are currently only visually assessed for cleanliness but include no microbiological auditing. The Health Service Executive (HSE) currently advises microbial settlement monitoring by passive sampling and the efficacy of cleaning should be monitored microbiologically using contact media containing neutralisers (4). Public Health England guidelines, published in 2020 on environmental sampling outlines that risk assessments must be carried out in healthcare facilities, cleaning tasks are documented and the effectiveness of cleanliness is to be monitored [British Standards Institution (40)]. The document states that routine sampling is not usually indicated. There are however guidelines available should screening be required (3). A review of European guidelines in controlling multi-drug resistant Gram-negative bacteria contain broad areas of agreement, however, there is discordance between guidelines. All guidelines agree environmental screening is to be carried out in outbreak settings only, while there are disagreements on the approach to healthcare worker screening during an outbreak (41). Rawlinson et al. reviewed current environmental monitoring of hospital surfaces in non-outbreak settings and how best to sample areas (42). Their results showed that swabs are better than contact plates when recovering Gram-negative pathogens, while still reporting on the optimal selection of culture medium to use when conducting Acinetobacter screening. There are a range of factors that can introduce sampling bias when screening an environment; including the level of contamination, whether the sample is taken from a wet or dry surface, pressure/contact time, and post-test processing. The microbial recovery from surfaces was improved by pre-moistening for all swab type (43), with increases in recovery from 57.5% on dry surfaces to 83.4% with pre-moistening of the same surface (44). When processing environmental samples, the choice is dependent on the target organism, cost, and time available. The choice of extraction solution was found to play a major role in recovering environmental pathogens when using culture methods (45). Furthermore, it has been shown that vortexing can increase recovery yield when using flocked swabs (46). Colony forming units (cfu) used when reporting environmental swabs often do not reflect the true risk to the patient, as it has been shown that surfaces with the highest bioburden are not always the surfaces with the most multi-drug resistant organisms (MDROs), which are of greater clinical concern (47). This can be seen when environmental screening is traditionally carried out for Gram-positive isolates on frequently touched surfaces. There is a lack of available information on how to individually target specific organisms when disinfecting hospital environments, a 2015 study by Havill et al. demonstrates the persistence of A. baumannii complex: after four rounds of manual cleaning and disinfection with a bleach solution, 25% of rooms were still contaminated with A. baumannii (48). Speculation on environmental contamination needs to become scientifically standardised (5).
FIGURE 1.
Threats and usefulness of Acinetobacter baumannii as an environmental contaminant.
A 2015 study by Simor et al. described a multidrug resistant A. baumannii (MDRAB) outbreak in a hospital burn unit, whereby 13% of patients acquired a MDRAB over a 15-month period. Environmental screening recovered MDRAB from healthcare workers hands and the hospital environment. Strict infection control and meticulous environmental cleaning contained the outbreak (49). A study by Al-Hamad et al., using pulse-field gel electrophoresis (PFGE) identified a pair of clinical and environmental bla NDM-1 carbapenem resistant Acinetobacter baumannii (CRAB) isolates from a surgical ward in Saudi Arabia (50). This is particularly concerning and highlights the importance of a targeted pathogen specific screening and decontamination protocol.
Carbapenem Resistance in Acinetobacter spp.
It has been shown that CRAB ICU infections are associated with increased rates of mortality in contrast with other pathogens being associated with increased length of stays and hospital costs (51). It is concerning that only six new antibiotics were released for use between 1985 and 2015 and resistance has already been observed to each of these (52) thus, the importance of following the Association of Professionals in Infection Control and Epidemiology (2010) guide to the elimination of MDRAB transmission in healthcare settings has not been overstated (53). These steps include risk assessment, infection surveillance, strict adherence to hand hygiene, antibiotic stewardship, outbreak recognition and environmental decontamination. The increasing occurrence of MDRAB among vulnerable patients highlights the importance of surveillance as a critical component aimed at preventing the spread of antimicrobial resistance (54). Early detection of CRAB outbreaks is key in preventing uncontrolled outbreaks (55). A 2019 study by Yamamoto et al. discusses the potential for rapid molecular identification of CRAB isolates in vulnerable patients (55). In that study, loop-mediated isothermal identification (LAMP), which is a rapid molecular diagnostic assay, was employed to help control an ICU outbreak. The use of this intervention resulted in the prevalence decreasing from 35.2 per 1,000 patient days in the outbreak phase to 20.9 in the active intervention phase, owing to earlier detection of CRAB facilitating earlier infection control measures. In areas with extensive amounts of environmental contamination, strict infection control measures including isolation, active surveillance cultures and daily environmental cleaning minimises the spread as was seen in a burn unit with an active healthcare associated infection (HCAI) outbreak of MDRAB, showing a decrease in spread of 88% during the period of intervention (56). Another report where patient surroundings were heavily contaminated showed that the burden of contamination correlated with the patient colonisation load, further demonstrating the need to monitor the environment as a CRAB reservoir (39).
Future Prospects
The increase in antibiotic resistance, together with uncertain prospects of new antibiotic development, means that a clear-cut environmental plan is urgently required. A single resistant infection has been estimated to cost approximately €8,500 to €34,000 more than a non-resistant infection, by the Organisation for Economic Cooperation and Development (OECD) (57). Clinical microbiology laboratories are an essential subspecialty in identifying environmental reservoirs and characterising antibiotic profiles of multi drug resistant pathogens. Clinical laboratories contribute directly to patient care at an individual and institutional level in the management of infection (6). A universally standardised policy for pathogen specific decontamination of hospital environments paired with an environmental molecular panel on the ESKAPE (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, A. baumannii, Pseudomonas aeruginosa and Enterobacter spp.) six pathogens used to screen high touch/high risk areas. Increased patient screening on admission is another beneficial method of identifying MDROs that may have potential for widespread transmission. The vital role cleaning staff play in infection prevention and control is not to be understated. Staff should be trained accordingly to understand the importance of microbiological decontamination as opposed to visible cleanliness.
Recommendations
More needs to be done to screen for MDRO in the hospital environment, particularly to identify and effectively decontaminate environmental reservoirs. The only steadfast way of reliably doing this is through microbiological screening and assessment of cleaning protocols. We strongly suggest that this microbiological screening of the hospital environment should use A. baumanii as an indicator organism for the presence of the other ESKAPE organisms. This is primarily due to the triple threat of A. baumannii as an opportunistic pathogen, a biofilm former and as an environmental reservoir of mobile genetic elements. Biomedical scientists are demonstrated leaders when it comes to developing and guiding appropriate infection prevention and control measures and central to good antimicrobial stewardship, although accustomed to being in the back room. However, the urgency of preserving what value remains on antibiotics suggests that as a profession we need to take a lead when it comes to the control of A. baumannii and other nosocomial pathogens.
Ethics Statement
Ethical approval was granted by the Clinical Research Ethics Committee, Cork [Review reference number ECM 4 (q)].
Author Contributions
JO’C: Study, design, supervision, manuscript preparation. RS: Primary supervisor, study, design, supervision, manuscript preparation. BL: Primary supervisor, study, design, supervision, manuscript preparation.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1. Saliba R, Ghelfenstein-Ferreira T, Lomont A, Pilmis B, Carbonnelle E, Seytre D, et al. Risk Factors for the Environmental Spread of Different Multi-Drug-Resistant-Organisms. MDRO; (2020). Research Square, 10.21203/rs.3.rs-59408/v1 [DOI] [PubMed] [Google Scholar]
- 2. Hanczvikkel A, Tóth Á. Quantitative Study about the Role of Environmental Conditions in the Survival Capability of Multidrug-Resistant Bacteria. J Infect Public Health (2018) 11(6):801–6. 10.1016/j.jiph.2018.05.001 [DOI] [PubMed] [Google Scholar]
- 3. Public Health England. Examining Food, Water and Environmental Samples from Healthcare Environments (2020). Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/865369/Hospital_F_W_E_Microbiology_Guidelines_Issue_3_February_2020__1_.pdf (Accessed March 16, 2023). [Google Scholar]
- 4. Health Service Executive. Health Service Executive Standards and Recommended Practices for Central Decontamination Units. (2014), Available from: https://www.hse.ie/eng/about/who/nqpsd/qps-improvement/hse-standards-and-recommended-practices-for-cdus-qpsd-d-003-2-v2-1.pdf (Accessed March 16, 2023).
- 5. Dancer SJ. How Do We Assess Hospital Cleaning? A Proposal for Microbiological Standards for Surface hygiene in Hospitals. J Hosp Infect (2004) 56(1):10–5. 10.1016/j.jhin.2003.09.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Samuel LP, Hansen GT, Kraft CS, Pritt BS. ASM Clinical and Public Health Microbiology Committee. The Need for Dedicated Microbiology Leadership in the Clinical Microbiology Laboratory. J Clin Microbiol (2021) 59(8):e0154919–19. 10.1128/JCM.01549-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Weingarten RA, Johnson RC, Conlan S, Ramsburg AM, Dekker JP, Lau AF, et al. Genomic Analysis of Hospital Plumbing Reveals Diverse Reservoir of Bacterial Plasmids Conferring Carbapenem Resistance. MBio (2018) 9(1):e02011–17. 10.1128/mBio.02011-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Montefour K, Frieden J, Hurst S, Helmich C, Headley D, Martin M, et al. Acinetobacter baumannii: an Emerging Multidrug-Resistant Pathogen in Critical Care. Crit Care Nurse (2008) 28(1):15–25. 10.4037/ccn2008.28.1.15 [DOI] [PubMed] [Google Scholar]
- 9. Choi CH, Lee EY, Lee YC, Park TI, Kim HJ, Hyun SH, et al. Outer Membrane Protein 38 of Acinetobacter baumannii Localizes to the Mitochondria and Induces Apoptosis of Epithelial Cells. Cell Microbiol (2005) 7(8):1127–38. 10.1111/j.1462-5822.2005.00538.x [DOI] [PubMed] [Google Scholar]
- 10. Nigro SJ, Hall RM. Structure and Context of Acinetobacter Transposons Carrying the Oxa23 Carbapenemase Gene. J Antimicrob Chemother (2016) 71(5):1135–47. 10.1093/jac/dkv440 [DOI] [PubMed] [Google Scholar]
- 11. Da Silva GJ, Domingues S. Insights on the Horizontal Gene Transfer of Carbapenemase Determinants in the Opportunistic Pathogen Acinetobacter baumannii . Microorganisms (2016) 4(3):29. 10.3390/microorganisms4030029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gedefie A, Demsis W, Ashagrie M, Kassa Y, Tesfaye M, Tilahun M, et al. Acinetobacter baumannii Biofilm Formation and its Role in Disease Pathogenesis: a Review. Infect Drug Resist (2021) 14:3711–9. 10.2147/IDR.S332051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. European Centre for Disease Prevention and Control. Observed and Predicted Prevalence of HAIs and Antimicrobial Use 2011/12. Available from: https://www.ecdc.europa.eu/en/healthcare-associated-infections-acute-care-hospitals/database/prevalence-hais-and-antimicrobial-use/observed (Accessed March 16, 2023). [Google Scholar]
- 14. Health Protection Surveillance Centre. Point Prevalence Survey of Hospital Acquired Infections & Antimicrobial Use in European Acute Care Hospitals. National Report Ireland; (2017). Available at: https://www.hpsc.ie/a-z/microbiologyantimicrobialresistance/infectioncontrolandhai/surveillance/hospitalpointprevalencesurveys/2017/nationalppsreports/PPS%202017%20National%20Report_FINAL_191218.pdf (Accessed March 16, 2023). [Google Scholar]
- 15. Suleyman G, Alangaden G, Bardossy AC. The Role of Environmental Contamination in the Transmission of Nosocomial Pathogens and Healthcare-Associated Infections. Curr Infect Dis Rep (2018) 20(6):12–1. 10.1007/s11908-018-0620-2 [DOI] [PubMed] [Google Scholar]
- 16. Munoz-Price LS, Weinstein RA. Acinetobacter Infection. New Engl J Med (2008) 358(12):1271–81. 10.1056/NEJMra070741 [DOI] [PubMed] [Google Scholar]
- 17. Howard A, O'Donoghue M, Feeney A, Sleator RD. Acinetobacter baumannii: an Emerging Opportunistic Pathogen. Virulence (2012) 3(3):243–50. 10.4161/viru.19700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Joly-Guillou M-L. Clinical Impact and Pathogenicity of Acinetobacter . Clin Microbiol Infect (2005) 11(11):868–73. 10.1111/j.1469-0691.2005.01227.x [DOI] [PubMed] [Google Scholar]
- 19. Gaddy JA, Actis LA. Regulation of Acinetobacter baumannii Biofilm Formation. Future Microbiol (2009) 4(3):273–8. 10.2217/fmb.09.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yang C-H, Su P-W, Moi S-H, Chuang L-Y. Biofilm Formation in Acinetobacter baumannii: Genotype-Phenotype Correlation. Molecules (2019) 24(10):1849. 10.3390/molecules24101849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Madsen JS, Burmølle M, Hansen LH, Sørensen SJ. The Interconnection between Biofilm Formation and Horizontal Gene Transfer. FEMS Immunol Med Microbiol (2012) 65(2):183–95. 10.1111/j.1574-695X.2012.00960.x [DOI] [PubMed] [Google Scholar]
- 22. Dijkshoorn L, Nemec A, Seifert H. An Increasing Threat in Hospitals: Multidrug-Resistant Acinetobacter baumannii . Nat Rev Microbiol (2007) 5(12):939–51. 10.1038/nrmicro1789 [DOI] [PubMed] [Google Scholar]
- 23. Perez S, Innes GK, Walters MS, Mehr J, Arias J, Greeley R, et al. Increase in Hospital-Acquired Carbapenem-Resistant Acinetobacter baumannii Infection and Colonization in an Acute Care Hospital during a Surge in COVID-19 Admissions - New Jersey, February-July 2020. Morbidity Mortality Weekly Rep (2020) 69(48):1827–31. 10.15585/mmwr.mm6948e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Blanco N, Harris AD, Rock C, Johnson JK, Pineles L, Bonomo RA, et al. Risk Factors and Outcomes Associated with Multidrug-Resistant Acinetobacter baumannii upon Intensive Care Unit Admission. Antimicrob Agents Chemother (2018) 62(1):e01631–17. 10.1128/AAC.01631-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bushman F. Lateral DNA Transfer. Cold Spring Harbor Laboratory Press; (2002). Available at: https://agris.fao.org/agris-search/search.do?recordID=US201300089728 (Accessed March 16, 2023). [Google Scholar]
- 26. Lucey B. Detection of Genetic Elements Among Clinically Relevant Bacteria. Elsevier; (2021):310–9. Available at: https://scholar.google.com/citations?view_op=view_citation&hl=en&user=YNAwZIAAAAAJ&cstart=20&pagesize=80&citation_for_view=YNAwZIAAAAAJ:738O_yMBCRsC (Accessed March 16, 2023). [Google Scholar]
- 27. Higgins PG, Pérez-Llarena FJ, Zander E, Fernández A, Bou G, Seifert H. OXA-235, a Novel Class D β-lactamase Involved in Resistance to Carbapenems in Acinetobacter baumannii . Antimicrob Agents Chemother (2013) 57(5):2121–6. 10.1128/AAC.02413-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. La M-V, Jureen R, Lin RT, Teo JW. Unusual Detection of an Acinetobacter Class D Carbapenemase Gene, Bla OXA-23, in a Clinical Escherichia coli Isolate. J Clin Microbiol (2014) 52(10):3822–3. 10.1128/JCM.01566-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Huang Y-M, Zhong L-L, Zhang X-F, Hu H-T, Li Y-Q, Yang X-R, et al. NDM-1-producing Citrobacter Freundii, Escherichia coli, and Acinetobacter baumannii Identified from a Single Patient in China. Antimicrob Agents Chemother (2015) 59(8):5073–7. 10.1128/AAC.04682-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Poirel L, Schrenzel J, Cherkaoui A, Bernabeu S, Renzi G, Nordmann P. Molecular Analysis of NDM-1-Producing Enterobacterial Isolates from Geneva, Switzerland. J Antimicrob Chemother. 2011;66(8):1730–3. 10.1093/jac/dkr174 [DOI] [PubMed] [Google Scholar]
- 31. Maeusli M, Lee B, Miller S, Reyna Z, Lu P, Yan J, et al. Horizontal Gene Transfer of Antibiotic Resistance from Acinetobacter baylyi to Escherichia coli on Lettuce and Subsequent Antibiotic Resistance Transmission to the Gut Microbiome. Msphere (2020) 5(3):e00329–20. 10.1128/mSphere.00329-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Costerton W, Veeh R, Shirtliff M, Pasmore M, Post C, Ehrlich G. The Application of Biofilm Science to the Study and Control of Chronic Bacterial Infections. J Clin Invest (2003) 112(10):1466–77. 10.1172/JCI20365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lili LN, Britton NF, Feil EJ. The Persistence of Parasitic Plasmids. Genetics (2007) 177(1):399–405. 10.1534/genetics.107.077420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tanner WD, Atkinson RM, Goel RK, Toleman MA, Benson LS, Porucznik CA, et al. Horizontal Transfer of the blaNDM-1 Gene to Pseudomonas aeruginosa and Acinetobacter baumannii in Biofilms. FEMS Microbiol Lett (2017) 364(8). 10.1093/femsle/fnx048 [DOI] [PubMed] [Google Scholar]
- 35. Gullberg E, Cao S, Berg OG, Ilbäck C, Sandegren L, Hughes D, et al. Selection of Resistant Bacteria at Very Low Antibiotic Concentrations. PLoS Pathog (2011) 7(7):e1002158. 10.1371/journal.ppat.1002158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Higgins PG, Hrenovic J, Seifert H, Dekic S. Characterization of Acinetobacter baumannii from Water and Sludge Line of Secondary Wastewater Treatment Plant. Water Res. 2018;140:261–7. 10.1016/j.watres.2018.04.057 [DOI] [PubMed] [Google Scholar]
- 37. Berlau J, Aucken H, Houang E, Pitt T. Isolation of Acinetobacter Spp Including A. baumannii from Vegetables: Implications for Hospital-Acquired Infections. J Hosp Infect (1999) 42(3):201–4. 10.1053/jhin.1999.0602 [DOI] [PubMed] [Google Scholar]
- 38. Weber DJ, Anderson D, Rutala WA. The Role of the Surface Environment in Healthcare-Associated Infections. Curr Opin Infect Dis (2013) 26(4):338–44. 10.1097/QCO.0b013e3283630f04 [DOI] [PubMed] [Google Scholar]
- 39. Nutman A, Lerner A, Schwartz D, Carmeli Y. Evaluation of Carriage and Environmental Contamination by Carbapenem-Resistant Acinetobacter baumannii . Clin Microbiol Infect (2016) 22(11):e5–949. 10.1016/j.cmi.2016.08.020 [DOI] [PubMed] [Google Scholar]
- 40. British Standards Institution. PAS 5748:2014. Specification for the Planning, Application, Measurement and Review of Cleanliness Services in Hospitals. London: BSI; (2014). Available at: https://standardsdevelopment.bsigroup.com/projects/2013-03076 (Accessed March 16, 2023). [Google Scholar]
- 41. Otter J, Mutters N, Tacconelli E, Gikas A, Holmes A. Controversies in Guidelines for the Control of Multidrug-Resistant Gram-Negative Bacteria in EU Countries. Clin Microbiol Infect (2015) 21(12):1057–66. 10.1016/j.cmi.2015.09.021 [DOI] [PubMed] [Google Scholar]
- 42. Rawlinson S, Ciric L, Cloutman-Green E. How to Carry Out Microbiological Sampling of Healthcare Environment Surfaces? A Review of Current Evidence. J Hosp Infect (2019) 103(4):363–74. 10.1016/j.jhin.2019.07.015 [DOI] [PubMed] [Google Scholar]
- 43. Moore G, Griffith C. Problems Associated with Traditional hygiene Swabbing: the Need for In‐house Standardization. J Appl Microbiol (2007) 103(4):1090–103. 10.1111/j.1365-2672.2007.03330.x [DOI] [PubMed] [Google Scholar]
- 44. Landers TF, Hoet A, Wittum TE. Swab Type, Moistening, and Preenrichment for Staphylococcus aureus on Environmental Surfaces. J Clin Microbiol (2010) 48(6):2235–6. 10.1128/JCM.01958-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lutz J, Crawford J, Hoet A, Wilkins J, III, Lee J. Comparative Performance of Contact Plates, Electrostatic Wipes, Swabs and a Novel Sampling Device for the Detection of S Taphylococcus Aureus on Environmental Surfaces. J Appl Microbiol (2013) 115(1):171–8. 10.1111/jam.12230 [DOI] [PubMed] [Google Scholar]
- 46. Dalmaso G, Bini M, Paroni R, Ferrari M. Qualification of High-Recovery, Flocked Swabs as Compared to Traditional Rayon Swabs for Microbiological Environmental Monitoring of Surfaces. PDA J Pharm Sci Technol (2008) 62(3):191–9. Available at: https://www.researchgate.net/profile/Michela-Ferrari-3/publication/51432625_Qualification_of_high-recovery_flocked_swabs_as_compared_to_traditional_rayon_swabs_for_microbiological_environmental_monitoring_of_surfaces/links/58418ed708ae2d2175614070/Qualification-of-high-recovery-flocked-swabs-as-compared-to-traditional-rayon-swabs-for-microbiological-environmental-monitoring-of-surfaces.pdf (Accessed March 16, 2023). [PubMed] [Google Scholar]
- 47. Verran J, Redfern J, Smith L, Whitehead K. A Critical Evaluation of Sampling Methods Used for Assessing Microorganisms on Surfaces. Food Bioproducts Process (2010) 88(4):335–40. 10.1016/j.fbp.2010.09.011 [DOI] [Google Scholar]
- 48. Havill NL, Moore BA, Boyce JM. Comparison of the Microbiological Efficacy of Hydrogen Peroxide Vapor and Ultraviolet Light Processes for Room Decontamination. Infect Control Hosp Epidemiol (2012) 33(5):507–12. 10.1086/665326 [DOI] [PubMed] [Google Scholar]
- 49. Simor AE, Lee M, Vearncombe M, Jones-Paul L, Barry C, Gomez M, et al. An Outbreak Due to Multiresistant Acinetobacter baumannii in a Burn Unit: Risk Factors for Acquisition and Management. Infect Control Hosp Epidemiol (2002) 23(5):261–7. 10.1086/502046 [DOI] [PubMed] [Google Scholar]
- 50. Al-Hamad A, Pal T, Leskafi H, Abbas H, Hejles H, Alsubikhy F, et al. Molecular Characterization of Clinical and Environmental Carbapenem Resistant Acinetobacter baumannii Isolates in a Hospital of the Eastern Region of Saudi Arabia. J Infect Public Health (2020) 13(4):632–6. 10.1016/j.jiph.2019.08.013 [DOI] [PubMed] [Google Scholar]
- 51. Giske CG, Monnet DL, Cars O, Carmeli Y. ReAct-Action on Antibiotic Resistance. Clinical and Economic Impact of Common Multidrug-Resistant Gram-Negative Bacilli. Antimicrob Agents Chemother (2008) 52(3):813–21. 10.1128/AAC.01169-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Kenny C, Furey A, Lucey B. A post-antibiotic Era Looms: Can Plant Natural Product Research Fill the Void? Br J Biomed Sci (2015) 72(4):191–200. 10.1080/09674845.2015.11665752 [DOI] [PubMed] [Google Scholar]
- 53. Rebmann T, Rosenbaum PA. Preventing the Transmission of Multidrug-Resistant Acinetobacter baumannii: an Executive Summary of the Association for Professionals in Infection Control and Epidemiology’s Elimination Guide. Am J Infect Control (2011) 39(5):439–41. 10.1016/j.ajic.2010.08.015 [DOI] [PubMed] [Google Scholar]
- 54. Unal S, Garcia-Rodriguez JA. Activity of Meropenem and Comparators against Pseudomonas aeruginosa and Acinetobacter Spp. Isolated in the MYSTIC Program, 2002–2004. Diagn Microbiol Infect Dis (2005) 53(4):265–71. 10.1016/j.diagmicrobio.2005.10.002 [DOI] [PubMed] [Google Scholar]
- 55. Yamamoto N, Hamaguchi S, Akeda Y, Santanirand P, Chaihongsa N, Sirichot S, et al. Rapid Screening and Early Precautions for Carbapenem-Resistant Acinetobacter baumannii Carriers Decreased Nosocomial Transmission in Hospital Settings: a Quasi-Experimental Study. Antimicrob Resist Infect Control (2019) 8(1):110–8. 10.1186/s13756-019-0564-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Barbut F, Yezli S, Mimoun M, Pham J, Chaouat M, Otter JA. Reducing the Spread of Acinetobacter baumannii and Methicillin-Resistant Staphylococcus aureus on a burns Unit through the Intervention of an Infection Control Bundle. Burns (2013) 39(3):395–403. 10.1016/j.burns.2012.07.007 [DOI] [PubMed] [Google Scholar]
- 57. OECD. Tackling Wasteful Spending on Health. Paris: OECD Publishing; (2017). Available at: https://read.oecd-ilibrary.org/social-issues-migration-health/tackling-wasteful-spending-on-health_9789264266414-en (Accessed March 16, 2023). [Google Scholar]