Abstract
There is an ongoing debate on the COVID-19 infection fatality rate (IFR) and the impact of COVID-19 on overall population mortality. Here, we addressed these issues in a community in Germany with a major superspreader event analyzing deaths over time and auditing death certificates in the community.18 deaths that occurred within the first six months of the pandemic had a positive test for SARS-CoV-2. Six out of 18 deaths had non-COVID-19 related causes of death (COD). Individuals with COVID-19 COD typically died of respiratory failure (75%) and tended to have fewer reported comorbidities (p = 0.029). Duration between first confirmed infection and death was negatively associated with COVID-19 being COD (p = 0.04). Repeated seroprevalence essays in a cross-sectional epidemiological study showed modest increases in seroprevalence over time, and substantial seroreversion (30%). IFR estimates accordingly varied depending on COVID-19 death attribution. Careful ascertainment of COVID-19 deaths is important in understanding the impact of the pandemic.
Subject terms: Adaptive immunity, Health policy, Infectious diseases
Introduction
The COVID-19 pandemic has been associated with considerable mortality at a global level, but estimates about the total number of deaths have varied widely across populations, demographics, and countries1–13. There is ongoing debate on the population-specific COVID-19 fatality rates (IFRs) and on the impact of COVID-19 on overall population mortality in various settings14. It is important to mention that especially countries in Latin America have been deeply affected by the COVID-19 pandemic, where until now Peru, Brazil, and Mexico have the highest mortality rates per 100,000 inhabitants worldwide15.
The IFR would be a robust marker for the severity of a virus-induced disease if the number of infected individuals (IFR denominator), as well as the number of deaths (IFR numerator) could be correctly measured. The number of infected individuals can be inferred by seroprevalence studies, and many such studies have been done16,17. However, biases often exist in such studies. Two main concerns are whether the surveyed sample is representative of the general population and whether people who get infected do not develop or lose their detectable antibodies over time. The validation of the number of COVID-19-related deaths has received less attention, but both over- and under-counting may occur18. COVID-19 deaths may have been underestimated in particular in some locations at the beginning of the pandemic when testing was limited, or because determining the cause of death (COD) in the elderly or those with multiple comorbidities was difficult. Conversely, COVID-19 deaths may have been over-attributed, e.g. if based on a positive SARS-CoV-2 test without a relevant clinical picture. Auditing of death certificates and/or medical records may help re-assess COVID-19 death attribution. For example, auditing efforts decreased the number of COVID-19 deaths in Alameda County and Santa Clara county by about a quarter compared with those that had been originally reported19,20.
Here, we address these issues in a community that witnessed the first major SARS-CoV-2 outbreak in Germany, as carnival festivities around February 15, 2020 were followed by a massive outbreak. To investigate this outbreak, we previously reported a seroepidemiological observational study that found a modest IFR21. However, questions emerged whether early during the pandemic COVID-19-related deaths may have been missed, mislabeled, or underestimated. Therefore, in the currently presented work, we analyzed deaths in the studied community over time and audited death certificates during the early phase of the pandemic. Specifically, we requested official death certificates of individuals who died in the community between March and October of 2020 and analyzed in detail the underlying causes of their deaths. Furthermore, we also assessed seroprevalence with repeated surveys over a year and specifically assessed seroreversion. These analyses allow for obtaining better insights into IFR estimates and on the impact of the pandemic in this intensively-studied community.
Methods
Study design
Our study was designed to understand possible overestimation of COVID-19-related deaths early during the pandemic, as well as the assessment of seroprevalence with repeated surveys over a year in the same community that witnessed the first major SARS-CoV-2 outbreak in Germany. Therefore, the study was divided in two arms: (1) The analyze of death certificates with reference to COVID-19 related causes of death according to WHO guidelines. (2) The assessment of seroprevalence based on a longitudinal cohort study which started early during the pandemic and lasted for 12 months. During this period, pharyngeal swabs and blood samples were collected from study participants at three different time points and analyzed for SARS-CoV-2 RNA in the swabs, as well as the antibody response against SARS-CoV-2 spike (S) and nucleocapsid (N).
Death certificate assessment
Setting and inclusion/exclusion criteria for participants
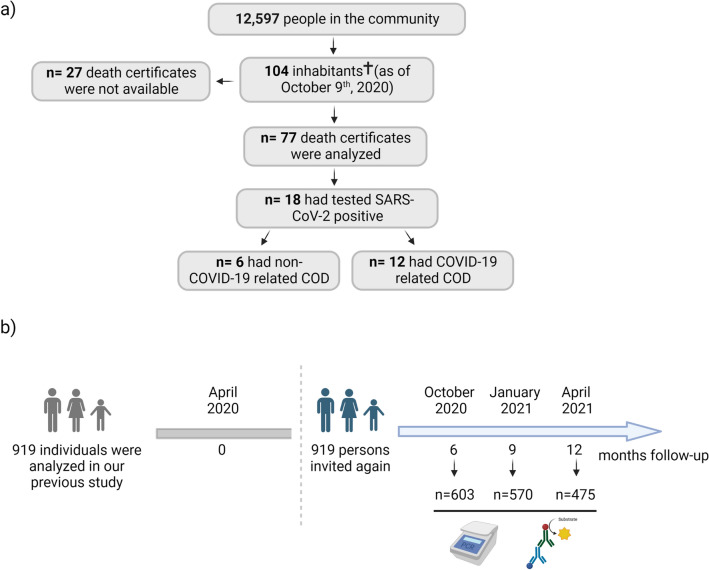
Between March and October 2020, 104 inhabitants of the studied community (n = 12,597) died, according to information we obtained from the state office for information and technology in North Rhine-Westphalia (Germany). With permission from the government of North Rhine-Westphalia (Germany), the state attorneys provided us with the death certificates of 77 subjects. Out of the remaining 27 deaths, none was attributed to COVID-19 (Fig. 1a).
Figure 1.
Illustrations depicting the number of decedents for death certificate assessment and study participants for seroprevalence survey. (a) Between March and October 2020, a total of 104 inhabitants of the studied community died, according to information we obtained from the state office for information and technology in North Rhine-Westphalia (Germany). The death certificates of 77 subjects were screened for information about gender, date of birth, date of death, COD, comorbidities, and history of SARS-CoV-2 infection. (b) Enrollment and flow of participants through the study as well as experimental procedures. In total 919 study participants from our previous 7-day seroepidemiological observational study21 were asked again to participate in at least one of the three follow-up visits (October 2020, January 2021, and April 2021). The only inclusion criterion was enrollment and sampling in our previous study (April 2020). Illustrations were created with bioRender.com premium (publication license available).
Data measurement and variables
All death certificates were assessed by three of the authors (E.R., D.L., and H.S.) and a consensus was achieved by applying the following procedures: We extracted information about gender, date of birth, date of death, COD, comorbidities, and any SARS-CoV-2 infection on record with the corresponding date of the first positive test. We classified causes of death in the following categories: respiratory failure; sepsis; cardiovascular disease (CVD); liver failure; kidney failure; cancer; other as well as comorbidities in the categories: respiratory; sepsis; CVD; liver malfunction; kidney malfunction; cancer; neurological; diabetes; unknown; other. We also compared the number of deaths attributed to COVID-19 in the data submitted by the authorities to the national death counts versus the number of deaths attributed to COVID-19 after our audit. In attributing deaths to COVID-19 in our audit of death certificates, we followed the guidance of the WHO guidelines. Accordingly, the outcome of a COVID-19-related death is defined as resulting from a clinically compatible illness in a probable or confirmed COVID-19 case, unless there is a clear alternative COD that cannot be related to COVID-19 disease (e.g. trauma) and death due to COVID-19 may not be attributed to another disease (e.g. cancer). In addition, there should be no period of complete recovery from COVID-19 between illness and death22. Due to health data protection, we could not obtain medical records for the deceased for further in-depth audit of these records.
Bias
To eliminate potential bias resulting from grouping the deceased based on COVID-19-related COD, three authors independently analyzed the death certificates. Each death was initially classified into categories, and then analyzed strictly in accordance with the guidelines of the WHO, as described above. In the next step, consensus was reached among the three authors, and the deaths were categorized as either COVID-19-related COD or non-COVID-19-related COD. However, since we did not have access to the full medical records of the deceased, we cannot rule out the possibility that some of the certificates indicating COVID-19 as the COD might have failed to report the existence of comorbidities as well.
Statistical methods
Parametric normality assumptions were not applied to avoid distributional misspecifications in moderate to small samples where a central limit theorem may not be applicable. Fisher's exact two-sided test was used to test for independence between two-factor variables with two levels (2 × 2 designs). Pearson’s Chi-squared test was used to test for independence between factor variables and Pearson’s’ Chi-squared goodness-of-fit test was used to test hypotheses about categorical distributions. For both chi-square tests, the p-values were simulated using Monte-Carlo simulations with 50,000 replications to consistently approximate the small sample distributions under the null hypotheses23. The one-sided two-sample Kolmogorov–Smirnov test was applied to test for a location shift in the number of days from a positive COVID-19 test and death between individuals with or without COVID-19 underlying cause of death (COD). The direction of this one-sided test was determined by the ex-ante clinical experience that SARS-CoV-2-associated death occurs relatively early after infection; this experience is confirmed by the data showing an empirical first-order stochastic dominance for the group of individuals who had no COVID-19 underlying COD. A logistic regression model is used to analyze the association between the probability of a SARS-CoV-2-associated death and the number of days from a positive COVID-19 test until death. Missing and unknown values were not imputed since these concerned only very few data points: there were two missing values in the number of days from positive COVID-19 test until death, and there was one missing value in the age variable. Binomial confidence intervals are computed using the Clopper-Pearson method. All confidence intervals were computed using a 95% coverage probability. The statistical analysis was carried out using version 4.1.1 of the R Language for Statistical Computing (R Core Team 2021: R: A Language and Environment for Statistical Computing, R Foundation for Statistical Computing, Vienna, Austria).
Ethical considerations
There are clear data protection laws in Germany under which circumstances researcher can obtain identifiable information. Under §8 of the regional German burial act, we are allowed to analyze death certificates when there is justifiable public interest. Therefore, this analysis was classified as important and the Ministry of Health in North Rhine-Westphalia (Germany) approved the request for access to the death certificates and the district attorney of every city where the patients died provided the certificate. The original study was approved by the Ethics Committee of the Medical Faculty of the University of Bonn (approval number 085/20). However, only a very limited number of employees of the Institute of Virology (Bonn, Germany) had access to the complete death certificates and data from the death certificates which was shared with external contributors (e.g. for statistical analysis) was fully anonymized.
Seroprevalence survey in repeated visits
Setting and inclusion/exclusion criteria for participants
To assess seroprevalence in the same community, we conducted a longitudinal cohort study with participants who were already enrolled in our 7-day seroepidemiological observational study in April 202021. This provided us with the advantage of having baseline data for time point 0 in our longitudinal survey. The criteria for initial enrollment was described in Streeck et al.21. Briefly, enrollment was based on a sample of 600 persons contained in the civil register of the community. Sampling was done randomly with the side condition that all 600 persons had different surnames, as it was assumed that different surnames were likely to indicate different households. In total, a dataset from 919 participants was analyzed in the original study. For the seroprevalence follow-up survey described here, these 919 participants were invited again via letter to participate in at least one of the three follow-up visits in October 2020 (Visit 1), January 2021 (Visit 2), and April 2021 (Visit 3). The only inclusion criterion was enrollment and sampling in our previous study. The exclusion criteria for participation were individuals who were unavailable on the day of sampling and requested a later appointment, or did not want to provide blood specimen and/or a pharyngeal swab, or had medical issues that made sampling impossible. However, individuals who did not participate in visit 1 were not excluded from being invited to visit 2 and 3. The total number of participants was 603 and for each visit was: Visit 1 (603), Visit 2 (570), and Visit 3 (475) (Fig. 1b). In addition, the following numbers of participants had to be excluded due to non-sampling: Visit 1 (20), Visit 2 (2), and Visit 3 (1).
Data measurement and variables
The study participants were invited to a study acquisition center and after having provided written and informed consent, study participants completed a questionnaire querying demographics, underlying diseases, previous SARS-CoV-2 infection, as well as their COVID-19 vaccination status. For children under 18 years, written and informed consent was provided by the persons with care and custody of the children following aged-adapted participant information. Furthermore, study participants were asked to provide blood specimens and pharyngeal swabs. Afterwards, samples were transported to the Institute of Virology of the UKB and the cold chain remained uninterrupted during transport. Blood was centrifuged at 600×g for 10 min with breaks on to separate the EDTA-containing plasma from the remaining blood. Next, plasma was aliquoted, and stored overnight at 4 °C till Anti-SARS-CoV-2 antibody detection as well as the remaining aliquots at − 80 °C. In the rare case that the ELISA did not provide reliable data, a cryopreserved plasma aliquot was used to repeat ELISA analysis. Plasma was used to determine Anti-SARS-CoV-2 IgG (against S1 domain) using enzyme-linked immunosorbent assays (ELISA) on the EUROIMMUN Analyzer I platform. According to the manufacturer’s instructions, a result was considered positive when a ratio (extinction of sample/extinction of calibrator) of 0.8 or higher was reached. In addition, the Roche Elecsys® N ELISA was used to determine antibody response against the nucleocapsid (N) of SARS-CoV-2. The result is given in COI (cutoff index), which is positive between 1.0 and approximately 250. Further, we estimated for each visit after the original one how many participants had undergone seroreversion, defined as a ratio of IgG below 0.8. For SARS-CoV-2 RT-PCR, first viral RNA isolation from pharyngeal swabs was performed on the day of sampling on the chemagic™ Prime™ instrument platform (Perkin Elmer) using the chemagic Viral 300 assay, or via the AltoStar® Purification Kit 1.5 (CE-IVD) on the AltoStar® AM16, according to manufacturer’s instructions, respectively. RT-PCR for two viral targets (E and S genes) was performed on isolated RNA samples via the RealStar® SARS-CoV-2 RT-PCR kit 1.0 (Altona Diagnostics). Internal control Ct values were within an acceptable range in all assays.
Data management and quality control
Planning and conduct of the study were supported by the Clinical Study Core Unit of the Study Center Bonn (SZB). Support included protocol and informed consent development following specifications of the WHO with regards to pandemic events, data management, submission to the ethics committee, clinical trial monitoring and quality control. Study data were collected and managed using REDCap electronic data capture tool. REDCap is a secure, web-based software platform designed to support data capture for research studies, providing (1) an intuitive interface for validated data capture; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages; and (4) procedures for data integration and interoperability with external sources. Questionnaire data were recorded on site using paper case report forms and were entered into the electronic study database using double data entry by trained study personnel.
Bias
Especially during the early phase of the SARS-CoV-2 pandemic, poorly or incorrectly executed pharyngeal swabs had a negative impact on the quality and results of SARS-CoV-2 RNA detection via PCR. To prevent differences in quality, all pharyngeal swabs in this study were performed by trained medical personnel to ensure consistent quality. Furthermore, it is known that the IgG-ELISA used from EUROIMMUNE had a sensitivity of 90.9% and a specificity of 99.1% according to the manufacture. To eliminate this bias, IgG values were corrected for sensitivity and specificity.
Statistical analysis
For sample size calculations, see the previous study21. Infection rates obtained from IgG measurements were corrected for misclassification bias using the matrix method24, based on sensitivity and specificity values reported by the manufacturer ELISA (Euroimmun, Lübeck, Germany; validation data sheet—version April 7th, 2020). Confidence intervals for the infection rates were computed using a bootstrap procedure based on 10,000 bootstrap samples with clustering on household-level by resampling individuals in household clusters with replacement25. As the bootstrapped data do not show severe abnormalities and the sample sizes are large, we estimate confidence intervals by the 2.5th and 97.5th percentiles of the bootstrap distribution. The generated bootstrap distribution was symmetrical and close to Gaussian (as indicated by normal quantile–quantile plots, with a mean of 0.153 and a standard deviation of 0.016). To analyze seroreversion, defined as IgG values below the ratio of 0.8, we analyzed participants who were IgG(+) at baseline and participated at least in one of the three follow-up visits. Important to note, we excluded participants who were SARS-CoV-2 vaccinated, which would cause an increase in IgG levels. Wilcoxon sign-rank tests are used to statistically evaluate the change of IgG ratio with time. Here, the resulting p-values were adjusted for multiple testing following the Bonferroni-Holm procedure. Confidence Intervals (CIs) for the IFR were computed by dividing the number of deaths by the CI limits of the estimated number of infected. We estimated IFR using different acquisition periods (7, 20, 35, and 60 days after the initial seroprevalence survey21) as this has been a debated issue in previous meta-analyses of IFR26,27. The numbers of SARS-CoV-2-associated deaths in the studied community for given lengths of acquisition periods can be considered fixed as the data acquisition corresponded to a complete survey of all recorded SARS-CoV-2-associated deaths in the community during the study period. In addition, we generated also separate IFR estimates for the ages groups 0–54, 55–74, and > 75 years. Additional statistical analysis is described in the Supplementary Information. All confidence intervals were computed using a 95% coverage probability. The statistical analysis was carried out using version 4.1.1 of the R Language for Statistical Computing (R Core Team 2021: R: A Language and Environment for Statistical Computing, R Foundation for Statistical Computing, Vienna, Austria).
Ethical considerations and Declaration of Helsinki
The original study was approved by the Ethics Committee of the Medical Faculty of the University of Bonn (approval number 085/20) and has been registered at the German Clinical Trials Register (https://www.drks.de, identification number DRKS00021306). The study was conducted in accordance with good clinical (GCP) and epidemiological practice (GEP) standards as well as comply with the guidelines of the Declaration of Helsinki (2013) and applied the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.
Results
Out of the 77 deceased persons, 18 were positive for COVID-19, with a median age of 78 years
In total, we analyzed the death certificates of 77 individuals who died between March 7th and October 9th, 2020 in the studied community (Fig. 1a). The median age was 82 years [range 28–98] and 55.8% were male. Among the 77 deaths, overall 18 individuals had tested SARS-CoV-2 positive, of whom 61.1% were male, and the median age was 78 [range 56–86]. Among the remaining 59 individuals we screened for potential signs of COVID-19 infection but no case of acute respiratory distress syndrome (ARDS) or similar causes of death that may be related to COVID-19 was found, thus we excluded the possibility of an undiagnosed SARS-CoV-2 infection. For the 18 individuals who had tested positive for SARS-CoV-2, we analyzed the date of death as well as the main COD (Table 1). 10 out of 18 individuals died in March and April 2020, seven individuals between May and August 2020, and one individual in October 2020. Deaths per month and age stratum from the 77 deaths we were able to examine are shown in Supplementary Table 1 and they suggest a possible clustering of deaths in March 2020 only in the > 70 years stratum. A total of 236 people (1.9% of the community population) lived in nursing homes during 2020 (80 males, 156 females).
Table 1.
All individuals who were SARS-CoV-2 positive and died on COVID-19 underlying and non-COVID-19 underlying causes of death in the studied community.
| PatID | Days between positive PCR test and death |
Cause of death |
|---|---|---|
| SARS-CoV-2 positive, COVID-19 underlying cause of death | ||
| 1 | 1 | Hypoxic lung failure, coronary heart disease |
| 2 | 5 | Hypoxic lung failure |
| 3 | 0 | Pneumonia |
| 4 | 3 | Acute respiratory distress syndrome (ARDS), pneumonia |
| 5 | Unknown | ARDS, septic shock, heart failure |
| 6 | 7 | Pneumonia, multiple organ failure |
| 7 | 6 | Multiple organ failure |
| 8 | 24 | Circulatory failure, septic shock |
| 9 | 40 | ARDS, pneumonia |
| 10 | Unknown | Global respiratory failure, pneumonia |
| 11 | 32 | Pneumonia, multiple organ failure, septic shock, |
| 12 | 62 | Global respiratory failure, pneumonia |
| SARS-CoV-2 positive, different underlying cause of death | ||
| 13 | 24 | Acute kidney failure, lactic acidosis (diabetes type II) |
| 14 | 103 | Cardiovascular failure, respiratory failure |
| 15 | 92 | Acute kidney failure (exsiccosis) |
| 16 | 122 | Liver and kidney failure |
| 17 | 156 | Oesophageal cancer |
| 18 | 187 | Decompensated cardiac insufficiency |
Note that patient 14 was fully recovered from COIVD-19.
33% of individuals who tested positive for SARS-CoV-2 and died had a non-COVID-19 related COD
We determined 12 out of 18 deaths (67% (95% CI: [41%, 87%])) with cases of ARDS and respiratory failure, pneumonia, septic shock, and multi organ failure as COD. The death certificates of these 12 patients stated that they were admitted to the hospital with an acute SARS-CoV-2 infection, where their state of health deteriorated rapidly. Most of the cases were admitted with already advanced pneumonia, which developed into ARDS with subsequent multiple organ failure or septic shock as additional COD. Conversely, in six out of 18 deaths (33% (95% CI: [13%, 59%])) with confirmed SARS-CoV-2 infection, we identified other factors to be the underlying COD. Two individuals died as a result of acute kidney failure after lactic acidosis and exsiccosis. They both had a medical history of diabetes mellitus type II, chronic obstructive pulmonary disease (COPD), and dementia, and in both cases their state of health deteriorated rapidly due to the underlying diabetes mellitus. Additionally, they had refused to eat and drink as a result of dementia, which ultimately led to acute kidney failure and exsiccosis. One individual had decompensated cardiac insufficiency with a medical history of food refusal, COPD, epilepsy, and Korsakov's disease, while another had a history of advanced and metastasized oesophageal carcinoma. The death certificates of these cases described a progressively deteriorating general condition of the patient, with eventual death from their underlying illnesses. Lastly, there was one case of acute liver and kidney failure as stated COD with no documented comorbidity on the death certificate and one case of cardiovascular failure as well as respiratory insufficiency with a medical history of diabetes and cardiovascular disease. In the latter case, it was noted, that the individual had previously recovered from SARS-CoV-2 infection. In addition, five out of the six individuals died three to six months after confirmed SARS-CoV-2 infection and more importantly the death certificates of all six cases reported recovery from COVID-19, which implies a period of complete recovery from COVID-19 between illness and death. Therefore, these cases do not fulfill the criteria of the WHO guidelines to be counted as COVID-19 deaths. Overall, only 12 out of 18 deaths with confirmed SARS-CoV-2 infection died because of COVID-19 between March and October 2020. During the same time period (March to October 2020), the authorities had reported 15 COVID-19 deaths to the national COVID-19 death counts28.
Individuals with COVID-19 COD typically died of respiratory failure and tended to have fewer reported comorbidities
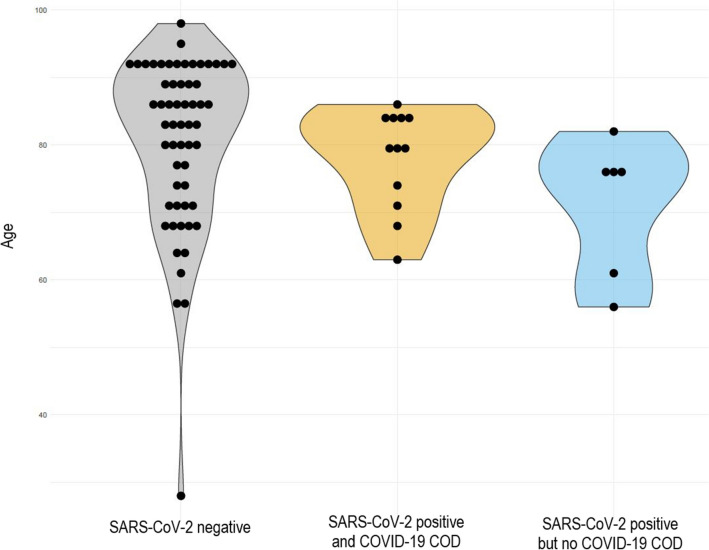
Next, we analyzed differences in age, COD, and comorbidities among all deaths that had occurred in the studied community. Therefore, we grouped the 77 deaths into three mutually exclusive groups (SARS-CoV-2 negative; SARS-CoV-2 positive and COVID-19 underlying COD; SARS-CoV-2 positive but no COVID-19 underlying COD). There were no statistically significant differences in the age distribution (median 84.5 [28–98], 80 [56–86], 75 [56–82], respectively, p = 0.1597) (Fig. 2) between these groups. However, while individuals with confirmed SARS-CoV-2 infection and no SARS-CoV-2-associated death had no common COD, individuals with confirmed SARS-CoV-2 infection were more likely to have died from respiratory failure compared to other COD (sepsis and CVD) (75% versus 25%, p = 0.01). Moreover, only 8% of the individuals without COVID-19 underlying COD had no comorbidity listed on the death certificate, whereas this was the case for 33% of individuals with COVID-19 underlying COD (p = 0.029).
Figure 2.
Age differences. All 77 deaths were differentiated into three groups: SARS-CoV-2 negative, SARS-CoV-2 positive, and COVID-19 underlying COD as well as SARS-CoV-2 positive but no COVID-19 underlying COD. There were no significant differences in the age distribution among COVID-19 infected or non-infected individuals.
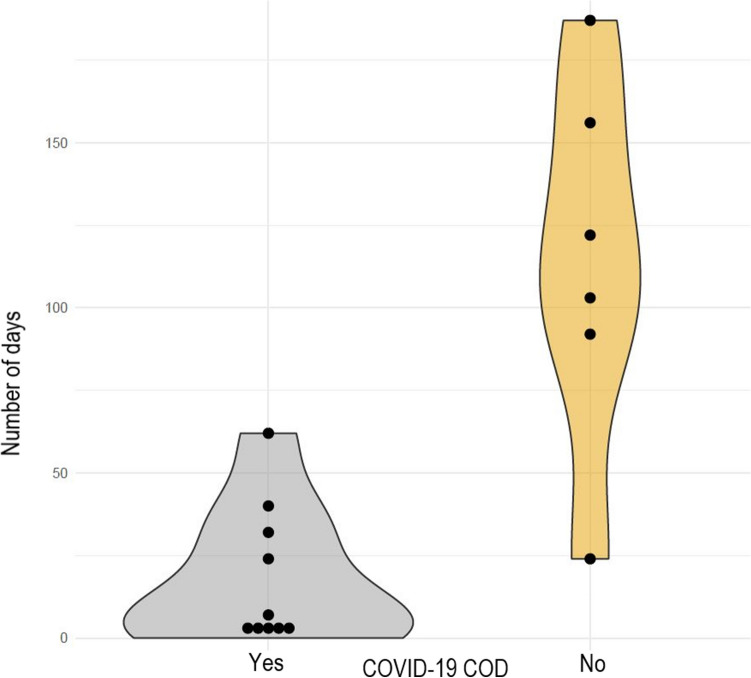
Duration between first confirmed infection and death was negatively associated to COVID-19 being COD
In individuals with SARS-CoV-2-associated deaths a median of 18 days [0–62] passed between positive PCR-test and death, a shorter time span compared to individuals with SARS-CoV-2 infection but no COVID-19 underlying COD (median 144 days [24–187]) (Fig. 3). The number of days from a positive COVID-19 test to death was higher (p = 0.005) for individuals who had no SARS-CoV-2-associated death. In logistic regression, the probability to die of COVID-19 decreases (p = 0.04) for larger numbers of survived days after a positive COVID-19 test. Overall, the likelihood to die of COVID-19 decreased markedly 100 days or more after confirmed SARS-CoV-2 infection (Supplementary Fig. 1).
Figure 3.
Number of days between confirmed SARS-CoV-2 PCR test and death of the individual. Stratified by COVID-19 underlying cause of death. Individuals with SARS-CoV-2-associated deaths had a median of 18 days [range 0–62] between positive PCR-test and death, a shorter time span compared to individuals with SARS-CoV-2 infection but no COVID-19 underlying COD with a median of 144 days [range 24–187].
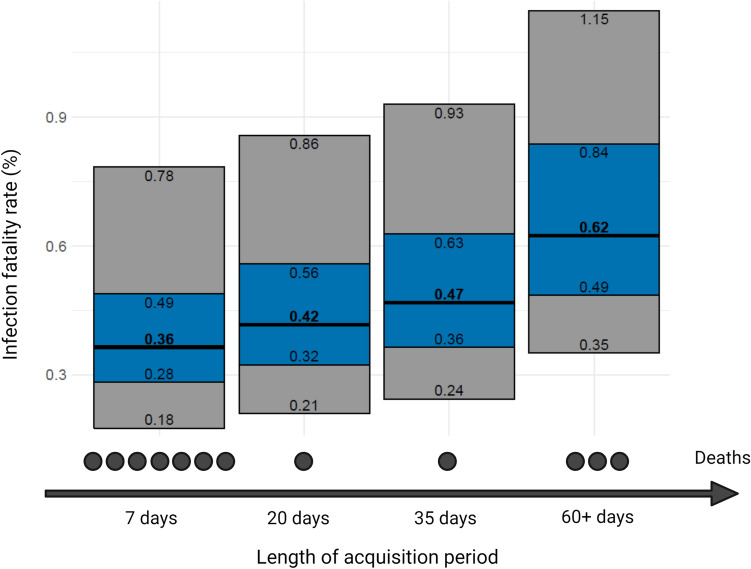
IFR estimates from 0.36% to 0.62% in an acquisition period ranging from 7 to 60+ days
Figure 4 shows the estimated IFR with different acquisition periods ranging from 7 days (7 deaths), 20 days (8 deaths), 35 days (9 deaths), and 60 days (12 deaths). Extending the observation period further did not lead to a change in the IFR depending on the acquisition period. The IFR estimates ranged accordingly from 0.36% to 0.62%, the 95% confidence intervals ranged from 0.28% to 0.84% and this confidence range would become 0.18% to 1.15% when introducing also uncertainty in the number of deaths. Table 2 shows the IFR estimates for age strata 0–50, 55–74, and > 75 years. As no deaths occurred in the age stratum 0–50, the IFR estimates are all 0.0% For the 55–74 years the IFR estimates range from 0.18% to 0.74% and the 95% confidence intervals extend from 0.13% to 1.19% For people > 75 years old, the IFR ranges from 3.21% to 4.28% and the 95% confidence intervals extend from 1.87% to 9.21%.
Figure 4.
Newly calculated infection fatality rate (IFR) with 95% confidence intervals (blue) and 95% credibility intervals (gray) additionally accounting for uncertainty in the number of deaths. Figure was modified with bioRender.com premium (publication license available).
Table 2.
Estimates of infection fatality rate (in %) and 95% confidence intervals in age strata with different acquisition windows.
| 0–54 years | 55–74 years | > 75 years | |
|---|---|---|---|
| Acquisition period | |||
| 7 days acquisition period | 0 [0.0] | 0.18 [0.13, 0.30] | 3.21 [1.87, 6.91] |
| 20 days acquisition period | 0 [0.0] | 0.18 [0.13, 0.30] | 3.75 [2.18, 8.06] |
| 35 days acquisition period | 0 [0.0] | 0.37 [0.25, 0.60] | 3.75 [2.18, 8.06] |
| 60+ days acquisition period | 0 [0.0] | 0.74 [0.50, 1.19] | 4.28 [2.50, 9.21] |
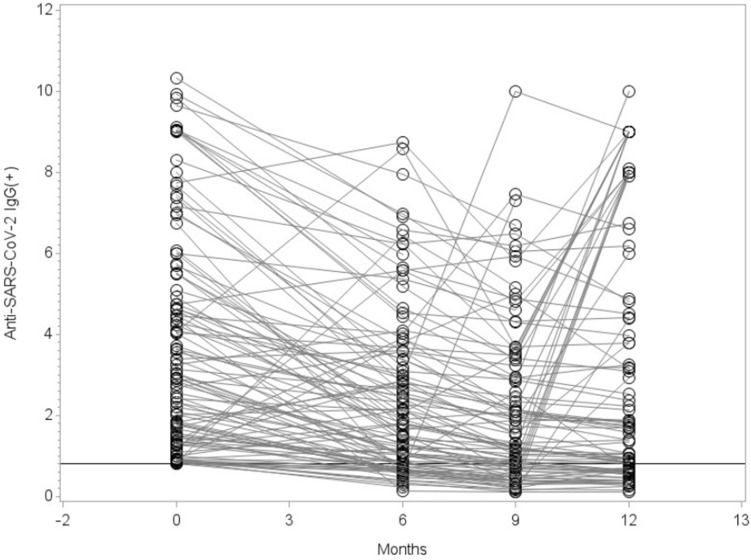
30% of individuals who had Anti-SARS-CoV-2 IgG antibodies seroreversed after 12 months
We next investigated the seroprevalence in the same community in which we already analyzed the death certificates. Therefore, we contacted again 919 study participants, who we already enrolled in our previous seroepidemiological observational study in April 202021, and ask them to participate in at least one of the three follow-up visits (Fig. 1B). The total number of participants was 603 and for each visit was: 603 (48.2% male) for visit 1, 570 (47.1% male) for visit 2 and 475 (46.3% male) for visit 3. The median age for visit 1 was 55 years [range 4–92], for visit 2 was 54 years [range 4–91] and for visit 3 was 57 years [range 4–92]. While 18.1% (95% CI: [13.7%, 23.0%]) of all study participants were found to be IgG(+) 6 months after the original study was conducted (baseline), this number increased 9 and 12 months later (21.0% [16.2%, 26.1%]; 35.9% [30.0, 42.0] respectively). Values were corrected for sensitivity and specificity of IgG (sensitivity 90.9%; specificity 99.1%). Next, we wanted to understand how many participants had undergone seroreversion, defined as IgG values below the ratio of 0.8. Therefore, we analyzed participants who were IgG(+) at baseline and participated at least in one of the three follow-up visits. We could see differences in the IgG levels of the participants already 6 months after the initial visit. IgG was significantly decreased over time and showed reduced antibody titers at 6 and 9 months (p < 0.0001) (Fig. 5). In total 27 (30%) out of 90 participants (95% CI: [20.5%; 39.5%]), who were IgG(+) at time point 0, seroreversed and showed no detectable IgG levels after 12 months. It should be noted that we excluded IgG values from participants who had received at least one dose of SARS-CoV-2 vaccine (Visit 2: n = 15, Visit 3: n = 46). This is because the ELISA we used is specific for SARS-CoV-2 spike protein, making it impossible to distinguish between an IgG response to natural infection or vaccination. Finally, we analyzed the pharyngeal swabs via RT-PCR to identify active SARS-CoV-2 infection. Overall, only 2 participants tested positive in our cohort over the 12 months of follow-up. One participant at 6 months, who was IgG(+) at baseline but had no detectable IgG antibodies 6 months later. The second participant was RT-PCR(+) at 9 months and was IgG negative at 0 and 6 months. More importantly, the proportion with positive PCR in our seroprevalence-tested cohort was far smaller (2 out of 603 tested participants, i.e. 0.3%) than the respective proportion in the overall population of the community (n = 374 PCR confirmed cases, i.e. 3.0%) in the same period of time, between October 2020 and April 2021.
Figure 5.
IgG levels over time of participants who were IgG(+) at baseline and participated at least in one of the three follow-up visits (6, 9, and 12 months after our previous study in April 202021) were analyzed. Time point 0 months refers to the published data values of the original study. 27 participants who developed IgG values below the ratio of 0.8 (Limit of Quantification) were considered as seroreversed. Statistical significance was assessed using Wilcoxon sign-rank test and the resulting six p-values were adjusted for multiple testing following the Bonferroni-Holm procedure. Visit 1 vs. 0: p < 0.0001; Visit 2 vs. 0: p < 0.0001; Visit 3 vs. 0: p = 0.0016; Visit 1 vs. 2: p < 0.0001; Visit 1 vs. 3: p = 0.0053; Visit 2 vs. 3: p < 0.0001. All comparisons show a decreasing trend with time. It is important to note, that although the graph only shows those with IgG ratio ≥ 0.8 at visit 0, all subjects who contribute data for visit 0 and at least one of the following visits are included in the test (without restriction at visit 0). In addition, we excluded IgG values from participants who had received at least one dose of SARS-CoV-2 vaccine (Visit 2: n = 15, Visit 3: n = 46). This is because the ELISA we used is specific for SARS-CoV-2 spike protein, making it impossible to distinguish between an IgG response to natural infection or vaccination.
Discussion
In this study, we audited and analyzed the deaths occurring in a German community between March and October of 2020 at the beginning of the SARS-CoV-2 pandemic. In total 18 dying individuals were reported positive for SARS-CoV-2, but COVID-19 was the underlying COD in only 12 out of the 18 deaths with confirmed SARS-CoV-2 infection. Therefore, one-third of individuals with confirmed SARS-CoV-2 infection died with non-COVID-19 related COD. The duration between confirmed SARS-CoV-2 infection and death was significantly higher in individuals without COVID-19 related COD compared to those with COVID-19 related COD. Moreover, the number of deaths reported to national authorities as COVID-19 deaths were 25% higher than the truly “causal” COVID-19 deaths. This overestimation of COVID-19 deaths is similar to the rates seen in audits in US counties19,20. Overestimation of COVID-19 deaths may apply also to other settings, especially in high-income countries where intensive testing is performed18.
We also observed that more SARS-CoV-2 positive individuals with non-COVID-19 underlying COD had listed comorbidities on the death certificates compared to individuals with COVID-19 underlying COD. This finding needs to be interpreted with caution given the small numbers and the possibility that comorbidities are often not fully reported in death certificates. Unfortunately, we could not have access to the full medical records. Thus we cannot exclude the possibility that some of the certificates where the COD was COVID-19 simply failed to report also existing comorbidities.
The published WHO guidelines define a COVID-19-associated death as a death resulting from a clinically compatible illness, in a probable or confirmed COVID-19 case, unless there is a clear alternative cause of death22. Our analysis of death certificates underlines the importance of more accurately confirming the COD of individuals who have died with a confirmed SARS-CoV-2 infection, especially when the elapsed time between the first SARS-CoV-2 positive test and death is long. We could show that 33% with confirmed SARS-CoV-2 infection had other factors to be the underlying COD, and taking into account the CI of (95% CI: [13%, 59%]) this is coherent with the recently published cause-of-death statistics of 2020 for Germany from the Federal Statistical Office26. Interestingly, during the same time period (March to October 2020), the authorities had reported 15 COVID-19 deaths to the national COVID-19 death counts28. Therefore, apparently three of the deaths that were not caused by COVID-19 had been officially reported as COVID-19 deaths.
Recent publications have highlighted difficulties in counting deaths with COVID-19 underlying COD and the need for continuous surveillance of mortality records27,29. Reported studies of COVID-19-associated deaths in Germany and the UK determined septic shock, multi organ failure, and respiratory failure as the most common immediate COVID-19 underlying COD, often due to suppurative pulmonary infection and diffuse alveolar damage30–32. Our findings for our studied community are consistent with this, as 75% of the COVID-19-associated deaths died from respiratory failure in combination with septic shock and multi organ failure. Furthermore, it was described that smoking, or some comorbidities like cancer and chronic liver disease had stronger associations with non-COVID than COVID-19 deaths in association with age30. Although we do not see significant associations with age or specific comorbidities (probably due to the low number of cases), we determined kidney failure, lactic acidosis or cancer as the main causes in non-COVID-19 associated deaths. These findings support the importance of looking more carefully into the deaths of individuals with a confirmed SARS-CoV-2 infection and taking into account the individual’s medical history along with their most recent medical data and symptoms.
Recent publications on COVID-19 disease progression analyzed the length of stay in the hospital and survival time33–35. It was reported that the median length between symptom onset and hospitalization ranged between three and 10.4 days, depending on the age of the patient34. However, the length of stay in hospital for patients who died eventually was an additional six to seven days as reported in a Belgian study34, and for China35 the estimated mean time from symptom onset to death was 18.8 days. Although a positive PCR test for SARS-CoV-2 does not necessarily coincide with the onset of symptoms, the results are consistent with our findings. Individuals in our studied community with SARS-CoV-2-associated deaths had a median of 18 days between positive PCR-test and death, whereas individuals with no COVID-19-underlying COD had a longer time span with a median of 144 days. The likelihood to die of COVID-19 decreased sharply with longer follow-up markedly after confirmed SARS-CoV-2 infection.
Evaluation of the deaths per month and age stratum showed a peak of deaths in March 2020 and it was concentrated in people over 70, consistent with the age of the early COVID-19 fatalities. We could not retrieve information on how many of these individuals might have been nursing home residents. However, this specific community has a high proportion of its population residing in nursing homes (about two times larger than the average for Germany [731,000 people, 0.9% of the German population])36. It is possible that many of the COVID-19 fatalities in the community might have been in people with limited life expectancy, regardless of whether they were institutionalized or not. Obviously, one has to be cautious with these inferences, especially given the relatively small number of deaths. Of note, eventually the overall number of deaths in the community for the calendar year 2020 (n = 157) was similar to the calendar years 2018 (n = 156) and 2015 (n = 158) but higher than other previous recent years. However, this was likely influenced by the hard lockdown in the community in March and April 2020.
Furthermore, repeated seroprevalence surveys showed that seroprevalence changed only modestly in the fall of 2020 and beyond as compared with our previously published results on seroprevalence in April 202021. However, we documented substantial rates of seroreversion, which is in agreement with some other studies37–44. Although IgM, IgA, and IgG antibodies can arise nearly simultaneously, it is known that IgM/IgA antibodies decay more rapidly than IgG, which can persist for at least several months45,46. Nevertheless, some studies have found higher rates of seroreversion, e.g. one investigation found a median time to seroreversion for IgG being only 55 days38, but this may include false positives at initial screening. Nonetheless, seroreversion likely causes the number of infected individuals to be substantially underestimated and thus the IFR to be overestimated37,38. This may apply even to our early April 2020 survey that happened within two months of the superspreader event.
Estimates of the number of people infected in the population may also be affected by the representativeness of the surveyed sample. In our original seroprevalence survey in April 202021, we noticed that the tested sample had a lower proportion of documented RT-PCR infections than the overall community population (2.39% versus 3.08%). Correction for this factor would decrease IFR estimates by 29% (e.g. from 0.36%–0.62% to 0.28%–0.48%). The sampling deviation was seen also, even more prominently in the follow-up surveys, where only 2 participants tested positive by RT-PCR (tenfold less than in the general population). It may reflect the fact that participants (especially those who return also for follow-up visits) may be more health conscious; or alternatively, less likely to perform RT-PCR testing since they are tested for antibodies. We also observed that our original seroprevalence study sample was under-representative of individuals infected during the main carnival event, the Kappensitzung, where participants had very high infection rates47, three times higher than the general population of the community by April 2020. It should be noted that different studies have shown the possibility that individuals were already infected with SARS-CoV-2 prior to the first documented COVID-19 case in the community, which can also contribute to higher infection rates and should be considered for mortality profiles48–50. Due to the small number of cases, we were not able to exclude that this may have been entirely due to chance but the pattern is consistent with the possibility that seroprevalence is underestimated (and, correspondingly, IFR overestimated). These observations highlight the difficulty of using seroprevalence samples and repeated surveys to assess the number of infected individuals in a population.
Our observations show that the calculation of IFRs needs to be done very carefully and that their interpretations need to take into account all possible influencing factors. In our study, overestimation of COVID-19 deaths and underestimation of seroprevalence may have inflated the IFR estimate. Additional variability in the estimates may be introduced by the time window used for capturing deaths, its relationship to the time window of the seroprevalence, and the assumptions made about the delay in developing antibodies and in dying after infection. In the case of this specific community, these uncertainties would probably still be captured by the original confidence interval that we reported for IFR in our original publication and that allowed for uncertainty in the number of deaths (95% CI, 0.17% to 0.77%). Moreover, the exact case mix of infected individuals can have a major impact on the IFR, given the extremely steep age gradient that has been documented before and which we also saw prominently in the community data5,51. It should be noted that due to the study design, the results of this study can only be representative for this specific community. Overall, in seroprevalence studies where only a tiny portion of the population is selected for serological testing (e.g. typically 0.01–1% in nationwide surveys52) one should remain cautious, as errors in counting deaths, seroprevalence, and other sources of uncertainty may have a larger impact.
Limitations
Possible limitations of this study include the following: (1) as shown in Supplementary Table 1 and already mentioned in our previous 7-day seroepidemiological observational study in April 202021, the age group of 70 years or older is over-represented within the death certificates and the 919 invited individuals compared to the studied community, the state of NRW and Germany. The reasons for this could be that elderly people have higher risk because severe cases are presumed to be more likely to occur in this age group; and secondly, due to retirement may have had more time to participate in a seroepidemiological observational study. (2) There was no access to the full medical records of the deceased due to data protection laws in Germany. Under §8 of the regional German burial act, we were allowed to analyze death certificates when there is justifiable public interest. We are aware that this cannot substitute for the full medical records and therefore, we cannot exclude the possibility that some of the certificates where the COD was COVID-19 simply failed to report also existing comorbidities.
Conclusions
In conclusion, our in-depth assessment of the fatality impact of COVID-19 in the studied community shows a relatively low fatality rate in this community with deaths concentrated entirely in the elderly, but seroprevalence estimates that go into IFR calculations need careful considerations of their time window, potential seroreversion, and representativeness. Importantly, COVID-19 deaths may have been over counted and the relative contribution of over- and under-counting of COVID-19 deaths needs careful auditing across multiple other locations.
Supplementary Information
Acknowledgements
We would like to thank all the subjects who participated in our repeated seroprevalence surveys. Furthermore, we would like to thank the following people who helped with the study: Maximilian Baum, Celina Beta Schlüter, Jasmin Zorn, Hannah Proksch, Melanie Geiger, Annika Breuer, Julia König, Karola Mai, Antonia Büning, Paulina Tarnow, Annina Hahn, Désirée Deloud, Anna-Lena Suchan, Sven Kohrn, Monika Eschbach-Bludau, Tobias Höller as well as the local government and physicians for their support to conduct the study.
Author contributions
E.R., D.L., J.P.A.I., and H.S. contributed to the conception, design, and interpretation of the work. E.R., D.L., B.S., N.L., T.H., C.F., J.P.A.I. and H.S. contributed to the data acquisition and analysis of the data. K.H.J. revised the work critically for important intellectual content. E.R., D.L., J.P.A.I., and H.S. wrote the manuscript. While conducting our study in the field, local physicians performed both blood sampling and pharyngeal swabs. They were paid for this in accordance with the German Medical Act.
Funding
Open Access funding enabled and organized by Projekt DEAL. The government of North Rhine-Westphalia (Germany) financially supported part of the study as well as the Viral NRW Network (grant number: CPS-1-1C acquired by H.S.).
Data availability
The datasets are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-023-32441-7.
References
- 1.Stang A, et al. Excess mortality due to COVID-19 in Germany. J. Infect. 2020;81:797–801. doi: 10.1016/j.jinf.2020.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weinberger DM, et al. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Intern. Med. 2020;180:1336–1344. doi: 10.1001/jamainternmed.2020.3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vestergaard LS, et al. Excess all-cause mortality during the COVID-19 pandemic in Europe - preliminary pooled estimates from the EuroMOMO network, March to April 2020. Euro Surveill. 2020;25:26. doi: 10.2807/1560-7917.Es.2020.25.26.2001214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Michelozzi P, et al. Mortality impacts of the coronavirus disease (COVID-19) outbreak by sex and age: Rapid mortality surveillance system, Italy, 1 February to 18 April 2020. Euro Surveill. 2020;25:19. doi: 10.2807/1560-7917.Es.2020.25.19.2000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williamson EJ, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ortiz-Prado E, et al. Analysis of excess mortality data at different altitudes during the COVID-19 outbreak in Ecuador. High Alt. Med. Biol. 2021;22:406–416. doi: 10.1089/ham.2021.0070. [DOI] [PubMed] [Google Scholar]
- 7.Ramírez-Soto MC, Ortega-Cáceres G. Analysis of excess all-cause mortality and COVID-19 mortality in Peru: Observational study. Trop. Med. Infect. Dis. 2022;7:44. doi: 10.3390/tropicalmed7030044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Palacio-Mejía LS, et al. Leading causes of excess mortality in Mexico during the COVID-19 pandemic 2020–2021: A death certificates study in a middle-income country. Lancet Reg. Health Am. 2022;13:100303. doi: 10.1016/j.lana.2022.100303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nucci LB, et al. Excess mortality associated with COVID-19 in Brazil: 2020–2021. J. Public Health (Oxf.) 2021 doi: 10.1093/pubmed/fdab398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scherbov S, Gietel-Basten S, Ediev D, Shulgin S, Sanderson W. COVID-19 and excess mortality in Russia: Regional estimates of life expectancy losses in 2020 and excess deaths in 2021. PLoS ONE. 2022;17:e0275967. doi: 10.1371/journal.pone.0275967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alfaro T, Martinez-Folgar K, Vives A, Bilal U. Excess mortality during the COVID-19 pandemic in cities of Chile: Magnitude, inequalities, and urban determinants. J. Urban Health. 2022;99:922–935. doi: 10.1007/s11524-022-00658-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu J, et al. Excess mortality in Wuhan city and other parts of China during the three months of the covid-19 outbreak: Findings from nationwide mortality registries. BMJ. 2021;372:415. doi: 10.1136/bmj.n415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Msemburi W, et al. The WHO estimates of excess mortality associated with the COVID-19 pandemic. Nature. 2023;613:130–137. doi: 10.1038/s41586-022-05522-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ioannidis JPA. Reconciling estimates of global spread and infection fatality rates of COVID-19: An overview of systematic evaluations. Eur. J. Clin. Invest. 2021;51:e13554. doi: 10.1111/eci.13554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schwalb A, Armyra E, Méndez-Aranda M, Ugarte-Gil C. COVID-19 in Latin America and the Caribbean: Two years of the pandemic. J. Intern. Med. 2022;292:409–427. doi: 10.1111/joim.13499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bobrovitz N, et al. Global seroprevalence of SARS-CoV-2 antibodies: A systematic review and meta-analysis. PLoS ONE. 2021;16:e0252617. doi: 10.1371/journal.pone.0252617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arora RK, et al. SeroTracker: A global SARS-CoV-2 seroprevalence dashboard. Lancet Infect. Dis. 2021;21:e75–e76. doi: 10.1016/s1473-3099(20)30631-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ioannidis JPA. Over- and under-estimation of COVID-19 deaths. Eur. J. Epidemiol. 2021;36:581–588. doi: 10.1007/s10654-021-00787-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.News, A. Alameda County revises COVID-19 death count by 25%, https://abc7news.com/covid-death-count-alameda-county-deaths-19-cases/10755419/ (2021).
- 20.Bayarea, N. Santa Clara County's COVID-19 Death Toll Drops by 505 After Data Change, https://www.nbcbayarea.com/news/local/santa-clara-countys-covid-19-death-toll-drops-by-505-after-data-change/2585739/ (2021).
- 21.Streeck H, et al. Infection fatality rate of SARS-CoV2 in a super-spreading event in Germany. Nat. Commun. 2020;11:5829. doi: 10.1038/s41467-020-19509-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.(WHO), W. H. O. International Guidelines for Certifcation and Classification (Coding) of COVID-19 as Cause of Death. https://www.who.int/classifications/icd/Guidelines_Cause_of_Death_COVID-19.pdf (2020).
- 23.Hope ACA. A simplified Monte Carlo significance test procedure. J. Roy. Stat. Soc. Ser. B (Methodol.) 1968;30:582–598. doi: 10.1111/j.2517-6161.1968.tb00759.x. [DOI] [Google Scholar]
- 24.Rogan WJ, Gladen B. Estimating prevalence from the results of a screening test. Am. J. Epidemiol. 1978;107:71–76. doi: 10.1093/oxfordjournals.aje.a112510. [DOI] [PubMed] [Google Scholar]
- 25.Davison, A. C. & Hinkley, D. V. Bootstrap Methods and their Application (Cambridge University Press, 1997).
- 26.(Destatis), F. S. O. First provisional results of the 2020 causes of death statistics including data on COVID-19 and suicides.https://www.destatis.de/EN/Press/2021/07/PE21_327_23211.html;jsessionid=5589D6A47B553BBC0609D57308A2563F.live721 (2021).
- 27.Fedeli U, et al. Different approaches to the analysis of causes of death during the COVID-19 epidemic. Eur. Rev. Med. Pharmacol. Sci. 2021;25:3610–3613. doi: 10.26355/eurrev_202105_25844. [DOI] [PubMed] [Google Scholar]
- 28.Gangelt, C. O. Coronavirus im Kreis Heinsberg. https://www.gangelt.de/news/226-erster-corona-fall-in-nrw (2022).
- 29.Amoretti MC, Lalumera E. COVID-19 as the underlying cause of death: Disentangling facts and values. Hist Philos. Life Sci. 2021;43:4. doi: 10.1007/s40656-020-00355-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bhaskaran K, et al. Factors associated with deaths due to COVID-19 versus other causes: Population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet Reg. Health Eur. 2021;6:100109. doi: 10.1016/j.lanepe.2021.100109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Elezkurtaj S, et al. Causes of death and comorbidities in hospitalized patients with COVID-19. Sci. Rep. 2021;11:4263. doi: 10.1038/s41598-021-82862-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Khan MMA, et al. Effects of underlying morbidities on the occurrence of deaths in COVID-19 patients: A systematic review and meta-analysis. J. Glob. Health. 2020;10:020503. doi: 10.7189/jogh.10.020503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Verma V, Vishwakarma RK, Verma A, Nath DC, Khan HTA. Time-to-Death approach in revealing chronicity and severity of COVID-19 across the World. PLoS ONE. 2020;15:e0233074. doi: 10.1371/journal.pone.0233074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Faes C, et al. Time between symptom onset, hospitalisation and recovery or death: Statistical analysis of Belgian COVID-19 patients. Int. J. Environ. Res. Public Health. 2020;17:7560. doi: 10.3390/ijerph17207560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Verity R, et al. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect. Dis. 2020;20:669–677. doi: 10.1016/s1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ärzteblatt. Mehr als 730.000 Menschen leben in Deutschland in Pflegeeinrichtungenhttps://www.aerzteblatt.de/nachrichten/117722 (2020).
- 37.Chen S, Flegg JA, White LJ, Aguas R. Levels of SARS-CoV-2 population exposure are considerably higher than suggested by seroprevalence surveys. PLoS Comput. Biol. 2021;17:e1009436. doi: 10.1371/journal.pcbi.1009436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.David MH, et al. Duration of SARS-CoV-2 sero-positivity in a large longitudinal sero-surveillance cohort: The COVID-19 Community Research Partnership. BMC Infect. Dis. 2021;21:889. doi: 10.1186/s12879-021-06517-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peghin M, et al. The fall in antibody response to SARS-CoV-2: A longitudinal study of asymptomatic to critically ill patients up to 10 months after recovery. J. Clin. Microbiol. 2021;59:e0113821. doi: 10.1128/jcm.01138-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peluso MJ, et al. SARS-CoV-2 antibody magnitude and detectability are driven by disease severity, timing, and assay. Sci. Adv. 2021;7:31. doi: 10.1126/sciadv.abh3409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shioda K, et al. Estimating the cumulative incidence of SARS-CoV-2 infection and the infection fatality ratio in light of waning antibodies. Epidemiology. 2021;32:518–524. doi: 10.1097/ede.0000000000001361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Harris RJ, et al. Serological surveillance of SARS-CoV-2: Six-month trends and antibody response in a cohort of public health workers. J. Infect. 2021;82:162–169. doi: 10.1016/j.jinf.2021.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Manisty C, et al. Time series analysis and mechanistic modelling of heterogeneity and sero-reversion in antibody responses to mild SARS-CoV-2 infection. EBioMedicine. 2021;65:1032599. doi: 10.1016/j.ebiom.2021.103259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Self WH, et al. Decline in SARS-CoV-2 antibodies after mild infection among frontline health care personnel in a multistate hospital network—12 States, April-August 2020. MMWR Morb. Mortal Wkly. Rep. 2020;69:1762–1766. doi: 10.15585/mmwr.mm6947a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Qu J, et al. Profile of immunoglobulin G and IgM antibodies against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Clin. Infect. Dis. 2020;71:2255–2258. doi: 10.1093/cid/ciaa489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Iyer AS, et al. Persistence and decay of human antibody responses to the receptor binding domain of SARS-CoV-2 spike protein in COVID-19 patients. Sci. Immunol. 2020;5:52. doi: 10.1126/sciimmunol.abe0367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wessendorf L, et al. Analysis of the dynamics, outcome, and prerequisites of the first German SARS-CoV-2 superspreading event. medRxiv. 2021 doi: 10.1101/2021.09.01.21262540. [DOI] [Google Scholar]
- 48.Apolone G, et al. Unexpected detection of SARS-CoV-2 antibodies in the prepandemic period in Italy. Tumori. 2021;107:446–451. doi: 10.1177/0300891620974755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gurgel RQ, et al. SARS-CoV-2 has been circulating in northeastern Brazil since February 2020: Evidence for antibody detection in asymptomatic patients. J. Infect. 2021;82:186–230. doi: 10.1016/j.jinf.2020.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gray WK, Navaratnam AV, Day J, Wendon J, Briggs TWR. COVID-19 hospital activity and in-hospital mortality during the first and second waves of the pandemic in England: An observational study. Thorax. 2022;77:1113–1120. doi: 10.1136/thoraxjnl-2021-218025. [DOI] [PubMed] [Google Scholar]
- 51.Ioannidis JPA, Axfors C, Contopoulos-Ioannidis DG. Population-level COVID-19 mortality risk for non-elderly individuals overall and for non-elderly individuals without underlying diseases in pandemic epicenters. Environ. Res. 2020;188:109890. doi: 10.1016/j.envres.2020.109890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Neuhauser H, et al. Germany’s low SARS-CoV-2 seroprevalence confirms effective containment in 2020: Results of the nationwide RKI-SOEP study. medRxiv. 2020 doi: 10.1101/2021.11.22.21266711. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets are available from the corresponding author on reasonable request.