Abstract
The physiological and psychological changes after anterior cruciate ligament reconstruction (ACLR) do not always allow a return to sport in the best condition and at the same level as before. Moreover, the number of significant re-injuries, especially in young athletes should be considered and physical therapists must develop rehabilitation strategies and increasingly specific and ecological test batteries to optimize safe return to play. The return to sport and return to play of athletes after ACLR must progress through the recovery of strength, neuromotor control, and include cardiovascular training while considering different psychological aspects. Because motor control seems to be the key to a safe return to sport, it should be associated with the progressive development of strength, and cognitive abilities should also be considered throughout rehabilitation.
Periodization, the planned manipulation of training variables (load, sets, and repetitions) to maximize training adaptations while minimizing fatigue and injury, is relevant to the optimization of muscle strengthening, athletic qualities, and neurocognitive qualities of athletes during rehabilitation after ACLR. Periodized programming utilizes the principle of overload, whereby the neuromuscular system is required to adapt to unaccustomed loads. While progressive loading is a well-established and widely used concept for strengthening, the variance of volume and intensity makes periodization effective for improving athletic skills and attributes, such as muscular strength, endurance, and power, when compared with non-periodized training. The purpose of this clinical commentary is to broadly apply concepts of periodization to rehabilitation after ACLR.
Keywords: periodization, motor control, anterior cruciate ligament reconstruction, return to sport, cognitive phase/mesocycle
INTRODUCTION
Non-contact injury of the anterior cruciate ligament (ACL) is a common sports-related injury typically warranting extensive rehabilitation time andreconstructive surgery followed by rehabilitation. After a sports injury, the first question asked by most athletes (and coaches) is: ‘When will I (the athlete) be able to compete again?’ The answer to this question is rarely straightforward and is influenced by many factors. However, in most cases the goals of the injured athlete and the treating clinician (plus other stakeholders in the decision-making team, such as coaches, parents, and managers) are the same—to facilitate a timely and safe return to sport.1
Athletes that return to play are at an elevated risk for re-injury or injury to the contralateral limb with an estimated 1 in 4 (25%) athletes suffering a second injury after returning to high-level sport.2 The high re-injury rate among injured athletes has been a focus for researchers attempting to identify modifiable risk factors and different rehab protocols according the graft choice, type of surgery, type of injury (meniscus or medial collateral ligament, involvement, etc.) for rehabilitation strategies to improve return-to-sport (RTS) outcomes.3 Periodization is probably one of the most important and fundamental concepts in training and it is important to consider the use of this concept in rehabilitation of injuries to the ACL and after ACL reconstruction (ALCR).4 Periodization consists of a ‘training cycle’ divided into different training or rehab phases with distinct physical and physiological objectives – to enable the best performance from athletes in competition (i.e. peak performance, injury prevention). Theoretically, using the periodization concept, peak performance is achieved in a controlled way, as a result of the summation of the particular adaptations provided by each training-rehab phase (mesocycle; Figure 1).5
Figure 1. Periodization training cycles.
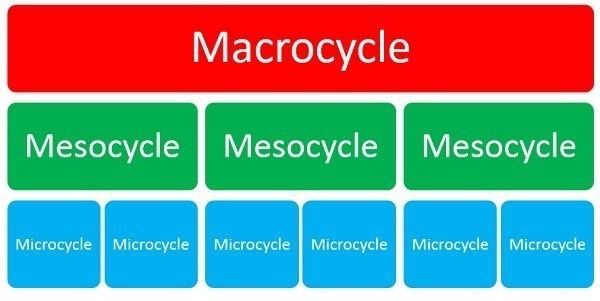
Various models of periodization exist. The two most common are linear and non-linear. Linear periodization adjusts exercise volume and load across a series of predictable phases or mesocycles. This stepwise progression from one training stage to another based on intended goals is similar to advancing a rehabilitation protocol from one stage of recovery to the next. Non-linear periodization, on the other hand, involves a more frequent change of volume and load within a mesocycle.
However, when examining the role of the use of the periodization concept in achieving the maximum specific performance in selected sports events (e.g. a season’s best result), an important drawback emerges: very low rates of effectiveness.6 The high frequency of competition, together with the increasing physical demands of competition over the season,7 has served to accentuate the physical and mental load incurred by elite athletes from different sports. As a consequence of these demands, the importance of recovery and rehabilitation strategies designed to alleviate player fatigue, minimize injury risk, and enhance performance is of paramount importance to clubs and national federations responsible for managing the elite player health.8 The use of periodization in long standing rehabilitation programs after ACLR needs more research and data to become accepted by health professionals. Therefore, the purpose of this clinical commentary is to broadly apply concepts of periodization to rehabilitation after ACLR.
CAN PERIODIZATION BE APPLIED IN LONG-TERM REHABILITATION, SUCH AS AFTER ACL INJURY?
Over the years, the pursuit of greater human performance through training has led to athletes, coaches, and physical therapists engaging in higher training volumes and often greater intensity. When coupled with ever increasing competition demands and fixture congestion the interest in exercise recovery strategies is extremely important to consider within the training and competition calendar.8,9 Rehabilitation programs have traditionally used a basic progressive overload approach primarily focusing on the injured area. Periodized training is a safe method of training for healthy athletes, as well as those in pain or following an injury.10 The ideas and concepts presented in this commentary have not been tested in randomized controlled trials, however they may stimulate further suitable studies investigating the application of periodization in rehab.
Periodization is the planned manipulation of training variables (load, sets, and repetitions) to maximize training adaptations while minimizing fatigue. Periodized programming utilizes the principle of overload, whereby the neuromuscular system adapts to unaccustomed loads. While progressive overload is a well-established and widely used concept for strengthening, the variance of volume and intensity makes periodization effective at improving athletic performance attributes, such as muscular strength, endurance, and power, compared with non-periodized training.10
The traditional periodization model assumes that a relatively prolonged period of basic training/rehab (general preparation / rehabilitation stages) is a prerequisite to a more specific phase (special preparation / cognitive phase). During general preparation, rehabilitation specialists aim to improve cardiorespiratory endurance and strength, even in athletes competing in power-speed sports disciplines.11
Another common belief related to strength-power development, is that the so-called ‘strength foundation phase’ will provide positive transfer of maximum strength to the ability to produce muscle power in the subsequent training phases or rehab stages. To date, there is no strong evidence supporting this belief, mostly held in traditional literature written on the basis of authors’ personal experiences and not supported by research. Conversely, there are studies showing that training using heavy-loads (i.e. maximum strength training) results in improvements only in the high-force/low-velocity portion of the force-velocity curve, without necessarily affecting the ability to produce higher amounts of force at high velocities (muscle power). It appears that the parametric relationship between force and velocity (i.e. the higher the load, the lower the velocity) plays a key role in modulating chronic neuromechanical adaptations and may be helpful in preventing re-injury.12
For instance, in endurance sports, athletes appear to benefit from performing high volumes of low-intensity training (i.e. below lactate thresholds) during their basic/specific periods of preparation.11 Furthermore, coaches and physiotherapists use prolonged periods of basic training on muscle-tendon tissues adaptation and injury prevention cannot be ignored. However, it is likely that these positive adaptations in muscle, tendons and ligaments may also be obtained by typical strength power exercises, which can be directly implemented during the course of a rehab period.
PERIODIZATION CONCEPTS DURING ACL REHABILITATION: PRACTICAL APPLICATIONS
The initial post-operative phase of ACLR rehabilitation focuses on pain and swelling management, restoration of range of motion, quadriceps recruitment, and normalizing gait mechanics. Once an athlete meets these goals, they can begin a periodized resistance training program. To determine the appropriate load for an exercise prescription, clinicians must establish a one-repetition maximum (1RM) for each exercise. Injured or healing tissues pose a challenge to determining 1RMs when they require limited loading.13 Indeed, for most sports disciplines, make it extremely difficult for strength and conditioning coaches and physical therapists to adopt this classic and theoretical method used with healthy athletes to those recovering from injury or surgery.14,15
The injury-induced reduction in physical and mental function associated with sports training and competition infers that it is illogical that a single recovery strategy and/or a generic one-size-fits-all approach would address a player’s recovery requirements. Alternatively, a framework where strategies are sequenced systematically at independent time points to match the source of physiological stress, alongside consideration to favorable adaptation might be a preferred approach in sports.16
From a practical standpoint, monitoring athletes using a battery of tests (Y-Balance test, hop tests, etc.) which best correlate to actual sports performance and RTS after injury is much more important than following theoretical concepts, which subjectively state that form might be predictable and controlled.17 With this simple and applied thought, strength and conditioning coaches and rehabilitation specialists may select better ways to control fluctuations in the competitiveness of individuals and teams, in addition to the already well-established variations in traditional training components (i.e. volume and intensity). Monitoring will help physical therapists and coaches to detect unexpected adaptations in the athletes’ fitness traits and adjust rehab and training loads according to these measured responses.18 In this regard, the use of validated methods for daily assessment (like GPS) of the internal training loads might be a useful strategy to quantify/modulate training intensity and its respective dose-response relationship with the specific changes in physical and mental qualities and quantities (cognitive load and fatigue assessment).19
THE NEUROCOGNITIVE MESOCYCLE: THE MISSING LINK IN ACL PERIODIZATION
ACL rehabilitation is a complex and multifaceted process involving physiological and psychological parameters which need to be constantly evolving to optimize individual athlete recovery needs and physiological adaptation.20 The relative importance of recovery versus adaptation will vary according to the needs of the athlete within the context of the procedure. This raises the idea of using rehab strategies in a manner that is periodized to mirror the demands of the sport, and to adequately recover from the stress, but also consider the need for an adaptive response. Sports injury rehabilitation must move beyond the traditional emphasis on mechanics and muscle strength and consider the need to address nuanced sensorimotor control deficits to ensure complete recovery and readiness for RTS demands.21 ACL injuries during sport are predominantly non-contact, suggesting injury may be a product of sensorimotor errors that result in a neuromuscular control fault unable to accommodate deleterious joint loading.22 Further, the vast majority of non-contact injury events occur while athletes are cognitively distracted, attending to complex visual demands or environmental stimuli, suggesting that neural mechanisms may directly contribute to the athlete’s ability to safely interact with the dynamic sport environment.23 Neurocognitive tasks, such as those measuring reaction time, processing speed, visual memory, and verbal memory, are well established in the neuropsychology literature as indirect measures of cerebral performance.
Situational awareness, arousal, and attentional resources of the individual may influence several areas of neurocognitive function, affecting the complex integration of vestibular, visual, and somatosensory information needed for neuromuscular control.24 Neuroplasticity deficits following ACL injury and surgery may at least in part be caused by physiotherapy protocols that do not engage differential learning and dual-tasking during (engaging more demanding aspects of the cognitive arsenal) exercises.
Over the course of rehabilitation following ACLR, excitability of the motor cortex for quadriceps contractions decreases, at least partially from the lack of differential exercise approaches that do not force the motor cortex to reintegrate the memory trace for quadriceps motor control before each repetition and action.25,26 Neurophysiological data across the stages of rehabilitation are lacking. Neuroimaging has been used to quantify brain activation differences between subjects with ACL deficiency who did not return to previous levels of physical activity and a healthy control group.27 In this phase, patients will focus on sport-specific exercises that are intended to be extremely challenging both physically and cognitively while performed in a controlled environment. All of the previously mentioned multimodal tasks can be implemented with a major focus on motor learning, cognitive loading and sensory re-weighting that are real-to sport and require quick decision making from unanticipated events.28,29
CONCLUSION
Sports rehabilitation specialists especially physical therapists and sports medicine physicians should have a basic understanding of periodization theory. Such an understanding can help sport medicine teams to better interact with the competitive mindset of athletes, their coaches, and their goals. A basic understanding of periodization theories and models may help sports rehabilitation specialists to skillfully plan rehabilitation programs that then progress toward the realization of the patients’ treatment goals.
With recent evidence in support of neurological contributions to ACL injury and rate of recovery, rehabilitation protocols may benefit from incorporation of approaches that target the sensorimotor and cognitive system. Periodization can incorporate the integration of motor learning principles (external focus and differential learning, anticipation, and reaction) and/or new technologies may bolster current ACL rehabilitation protocols and improve patient recovery and timing. Research has traditionally focused on administering a single rehab intervention whereas, in the applied setting, athletes are more likely to administer multiple interventions in varying sequences. Future research using robust rehabilitation technique protocols and large-scale randomized control trials is needed to better understand the influence of various techniques and the application of periodization concepts on the stress-injury-adaptation continuum.
Conflicts of interest
The authors report no conflicts of interest.
References
- Reconstruction, rehabilitation and return-to-sport continuum after anterior cruciate ligament injury (ACLR3-continuum): Call for optimized programs. Rambaud Alexandre JM, Neri Thomas, Edouard Pascal. Jun;2022 Annals of Physical and Rehabilitation Medicine. 65(4):101470. doi: 10.1016/j.rehab.2020.101470. doi: 10.1016/j.rehab.2020.101470. [DOI] [PubMed] [Google Scholar]
- Ardern Clare L, Glasgow Philip, Schneiders Anthony, Witvrouw Erik, Clarsen Benjamin, Cools Ann, Gojanovic Boris, Griffin Steffan, Khan Karim M, Moksnes Håvard, Mutch Stephen A, Phillips Nicola, Reurink Gustaaf, Sadler Robin, Grävare Silbernagel Karin, Thorborg Kristian, Wangensteen Arnlaug, Wilk Kevin E, Bizzini Mario. British Journal of Sports Medicine. 14. Vol. 50. BMJ; 2016 Consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern; pp. 853–864. [DOI] [PubMed] [Google Scholar]
- The modifying factors that help improve anterior cruciate ligament reconstruction rehabilitation: a narrative review. Rambaud Alexandre JM, Neri Thomas, Dingenen Bart, Parker David, Servien Elvire, Gokeler Alli, Edouard Pascal. Jun;2022 Annals of Physical and Rehabilitation Medicine. 65(4):101601. doi: 10.1016/j.rehab.2021.101601. doi: 10.1016/j.rehab.2021.101601. [DOI] [PubMed] [Google Scholar]
- Periodization in anterior cruciate ligament rehabilitation: a novel framework. Kakavas George, Malliaropoulos Nikolaos, Bikos Georgios, Pruna Ricard, Valle Xavier, Tsaklis Panagiotis, Maffulli Nicola. 2021Medical Principles and Practice. 30(2):101–108. doi: 10.1159/000511228. doi: 10.1159/000511228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Periodization training focused on technical-tactical ability in young soccer players positively affects biochemical markers and game performance. Aquino Rodrigo, Cruz Gonçalves Luiz G., Palucci Vieira Luiz H., Oliveira Lucas P., Alves Guilherme F., Pereira Santiago Paulo R., Puggina Enrico F. Oct;2016 Journal of Strength and Conditioning Research. 30(10):2723–2732. doi: 10.1519/jsc.0000000000001381. doi: 10.1519/jsc.0000000000001381. [DOI] [PubMed] [Google Scholar]
- Barnes C., Archer D., Hogg B., Bush M., Bradley P. International Journal of Sports Medicine. 13. Vol. 35. Georg Thieme Verlag KG; The evolution of physical and technical performance parameters in the english premier league; pp. 1095–1100. [DOI] [PubMed] [Google Scholar]
- Brown Freddy, Gissane Conor, Howatson Glyn, van Someren Ken, Pedlar Charles, Hill Jessica. Sports Medicine. 11. Vol. 47. Springer Science and Business Media LLC; Compression garments and recovery from exercise: a meta-analysis; pp. 2245–2267. [DOI] [PubMed] [Google Scholar]
- The use of recovery strategies by Spanish first division soccer teams: a cross-sectional survey. Altarriba-Bartes Albert, Peña Javier, Vicens-Bordas Jordi, Casals Martí, Peirau Xavier, Calleja-González Julio. 2021The Physician and Sportsmedicine. 49(3):297–307. doi: 10.1080/00913847.2020.1819150. doi: 10.1080/00913847.2020.1819150. [DOI] [PubMed] [Google Scholar]
- Block periodization versus traditional training theory: a review. Issurin V. 2008J Sports Med Phys Fitness. 48(1):65–75. [PubMed] [Google Scholar]
- Non-linear periodization for general fitness & athletes. Fleck Steven. Sep 1;2011 Journal of Human Kinetics. 29A(Special-Issue):41–45. doi: 10.2478/v10078-011-0057-2. doi: 10.2478/v10078-011-0057-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Integration of strength and conditioning principles into a rehabilitation program. Reiman M.P., Lorenz D.S. 2011Int J Sports Phys Ther. 6(3):241–253. [PMC free article] [PubMed] [Google Scholar]
- Short-term training for explosive strength causes neural and mechanical adaptations: Neuromuscular adaptations with explosive strength training. Tillin Neale A., Pain Matthew T. G., Folland Jonathan P. Apr 4;2012 Experimental Physiology. 97(5):630–641. doi: 10.1113/expphysiol.2011.063040. doi: 10.1113/expphysiol.2011.063040. [DOI] [PubMed] [Google Scholar]
- Upgraded hardware─what about the software? Brain updates for return to play following ACL reconstruction. Grooms Dustin R, Myer Gregory D. 2017British Journal of Sports Medicine. 51(5):418–419. doi: 10.1136/bjsports-2016-096658. doi: 10.1136/bjsports-2016-096658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The combined impact of a perceptual–cognitive task and neuromuscular fatigue on knee biomechanics during landing. Mejane Jeremy, Faubert Jocelyn, Romeas Thomas, Labbe David R. Jan;2019 The Knee. 26(1):52–60. doi: 10.1016/j.knee.2018.10.017. doi: 10.1016/j.knee.2018.10.017. [DOI] [PubMed] [Google Scholar]
- ‘What’s my risk of sustaining an ACL injury while playing football (soccer)?’ A systematic review with meta-analysis. Montalvo Alicia M, Schneider Daniel K, Silva Paula L, Yut Laura, Webster Kate E, Riley Michael A, Kiefer Adam W, Doherty-Restrepo Jennifer L, Myer Gregory D. 2019British Journal of Sports Medicine. 53(21):1333–1340. doi: 10.1136/bjsports-2016-097261. doi: 10.1136/bjsports-2016-097261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naclerio Ayllón Fernando, Moody Jeremy, Chapman Mark. Journal of Human Sport and Exercise. 2. Vol. 8. Journal of Human Sport and Exercise; Applied periodization: a methodological approach; pp. 350–366. [DOI] [Google Scholar]
- Neuroplasticity and Anterior Cruciate Ligament Injury. Kakavas George, Malliaropoulos Nikolaos, Pruna Ricard, Traster David, Bikos Georgios, Maffulli Nicola. Jan 31;2020 Indian Journal of Orthopaedics. 54(3):275–280. doi: 10.1007/s43465-020-00045-2. doi: 10.1007/s43465-020-00045-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball heading and subclinical concussion in soccer as a risk factor for anterior cruciate ligament injury. Kakavas George, Malliaropoulos Nikolaos, Blach Wieslaw, Bikos Georgios, Migliorini Filippo, Maffulli Nicola. Sep 19;2021 Journal of Orthopaedic Surgery and Research. 16(1):566. doi: 10.1186/s13018-021-02711-z. doi: 10.1186/s13018-021-02711-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Changed cortical activity after anterior cruciate ligament reconstruction in a joint position paradigm: an EEG study: acl and cortical activity. Baumeister J., Reinecke K., Weiss M. Dec 7;2007 Scandinavian Journal of Medicine & Science in Sports. 18(4):473–484. doi: 10.1111/j.1600-0838.2007.00702.x. doi: 10.1111/j.1600-0838.2007.00702.x. [DOI] [PubMed] [Google Scholar]
- The influence of musculoskeletal injury on cognition: implications for concussion research. Hutchison Michael, Comper Paul, Mainwaring Lynda, Richards Doug. Jul 18;2011 The American Journal of Sports Medicine. 39(11):2331–2337. doi: 10.1177/0363546511413375. doi: 10.1177/0363546511413375. [DOI] [PubMed] [Google Scholar]
- Concussion frequency associates with musculoskeletal injury in retired nfl players. Pietrosimone BRIAN, Golightly YVONNE M., Mihalik JASON P., Guskiewicz KEVIN M. Nov;2015 Medicine & Science in Sports & Exercise. 47(11):2366–2372. doi: 10.1249/mss.0000000000000684. doi: 10.1249/mss.0000000000000684. [DOI] [PubMed] [Google Scholar]
- Zimny Marilyn L., Schutte Michael, Dabezies Eugene. The Anatomical Record. 2. Vol. 214. Wiley; Mechanoreceptors in the human anterior cruciate ligament; pp. 204–209. [DOI] [PubMed] [Google Scholar]
- Mechanoreceptors in human cruciate ligaments. A histological study. Schultz R A, Miller D C, Kerr C S, Micheli L. Sep;1984 The Journal of Bone & Joint Surgery. 66(7):1072–1076. doi: 10.2106/00004623-198466070-00014. doi: 10.2106/00004623-198466070-00014. [DOI] [PubMed] [Google Scholar]
- Neural anatomy of the human anterior cruciate ligament. Schutte M J, Dabezies E J, Zimny M L, Happel L T. Feb;1987 The Journal of Bone & Joint Surgery. 69(2):243–247. doi: 10.2106/00004623-198769020-00011. doi: 10.2106/00004623-198769020-00011. [DOI] [PubMed] [Google Scholar]
- Kennedy John C., Alexander Ian J., Hayes Keith C. The American Journal of Sports Medicine. 6. Vol. 10. SAGE Publications; Nerve supply of the human knee and its functional importance; pp. 329–335. [DOI] [PubMed] [Google Scholar]
- Proprioception and function after anterior cruciate reconstruction. Barrett DS. Sep;1991 The Journal of Bone and Joint Surgery. British volume. 73-B(5):833–837. doi: 10.1302/0301-620x.73b5.1894677. doi: 10.1302/0301-620x.73b5.1894677. [DOI] [PubMed] [Google Scholar]
- Borsa Paul A., Lephart Scott M., Irrgang James J., Safran Marc R., Fu Freddie H. The American Journal of Sports Medicine. 3. Vol. 25. SAGE Publications; The effects of joint position and direction of joint motion on proprioceptive sensibility in anterior cruciate ligament-deficient athletes; pp. 336–340. [DOI] [PubMed] [Google Scholar]
- The anterior cruciate ligament deficiency as a model of brain plasticity. Kapreli Eleni, Athanasopoulos Spyridon. Jan;2006 Medical Hypotheses. 67(3):645–650. doi: 10.1016/j.mehy.2006.01.063. doi: 10.1016/j.mehy.2006.01.063. [DOI] [PubMed] [Google Scholar]
- Gamma loop dysfunction in quadriceps on the contralateral side in patients with ruptured acl. Konishi YU, Konishi HIROYUKI, Fukubayashi TORU. Jun;2003 Medicine & Science in Sports & Exercise. 35(6):897–900. doi: 10.1249/01.mss.0000069754.07541.d2. doi: 10.1249/01.mss.0000069754.07541.d2. [DOI] [PubMed] [Google Scholar]


