Abstract
Anterior cruciate ligament reconstruction (ACLR) with a bone-patellar tendon-bone (BPTB) or hamstring tendon (HT) autograft has traditionally been the preferred surgical treatment for patients returning to Level 1 sports. More recently, international utilization of the quadriceps tendon (QT) autograft for primary and revision ACLR has increased in popularity. Recent literature suggests that ACLR with the QT may yield less donor site morbidity than the BPTB and better patient-reported outcomes than the HT. Additionally, anatomic and biomechanical studies have highlighted the robust properties of the QT itself, with superior levels of collagen density, length, size, and load-to-failure strength compared to the BPTB. Although previous literature has described rehabilitation considerations for the BPTB and HT autografts, there is less published with respect to the QT. Given the known impact of the various ACLR surgical techniques on postoperative rehabilitation, the purpose of this clinical commentary is to present the procedure-specific surgical and rehabilitation considerations for ACLR with the QT, as well as further highlight the need for procedure-specific rehabilitation strategies after ACLR by comparing the QT to the BPTB and HT autografts.
Level of Evidence
Level 5
Keywords: anterior cruciate ligament reconstruction, autograft, physical therapy, quadriceps tendon autograft, rehabilitation
INTRODUCTION
Rupture of the anterior cruciate ligament is a well-known sports injury, with a higher injury incidence in females and those who participate in Level 1 sports.1–4 Traditionally, anterior cruciate ligament reconstruction (ACLR) with a bone-patellar tendon-bone (BPTB) or hamstring tendon (HT) autograft has been the preferred surgical procedure for managing complete tears of the anterior cruciate ligament, with a surgeon-preference towards the BPTB as the standard of care.5–9 Recently, international utilization of the quadriceps tendon (QT) autograft for primary and revision ACLR has increased in popularity10–13; ACLR with the QT may yield less graft harvest site morbidity than the BPTB and better patient-reported outcomes than the HT.14–16 However, revision ACLR outcomes from the Danish Knee Ligament Reconstruction Registry suggests higher graft laxity and failure rates when performing primary ACLR with the QT than both the BPTB and HT17; these findings have been debated,18,19 along with other literature reporting similar graft survivorship between the QT, BPTB and HT.14–16,20
Justifying the increased utilization of the QT for ACLR, anatomic and biomechanical studies have highlighted the robust properties of the QT itself, with superior levels of collagen density, length, size and load-to-failure strength than the BPTB.21–25 However, due to the multiple muscular origins of the quadriceps tendon, the QT has the potential for more variation in laminar structure and fiber orientation than the BPTB and HT.26–28 This non-uniformity of the quadriceps tendon, along with variation in surgeon skill and reconstruction technique, has been suggested as a reason for the higher QT failure rates within the Danish Knee Ligament Reconstruction Registry.17–19
In addition to intra-graft characteristics, graft-specific considerations for ACLR should also include fixation technique, management of the graft harvest site and the overall graft ligamentization process. For example, graft fixation with an interference screw may facilitate better graft incorporation than suspensory fixation and reduce the incidence of bone tunnel widening.29–31 Regarding the graft harvest site, ACLR with the QT and BPTB may produce more postoperative quadriceps weakness than the HT,14,32–34 whereas a higher incidence of kneeling-related knee pain has been reported with the BPTB than both the QT and HT autografts.14,15 Lastly, the bone-to-bone healing of the BPTB within the bone tunnels facilitates graft osteointegration, which is a more efficient incorporation process than the fibrovascular healing of an all soft-tissue graft35; these considerations influence surgical decision-making and the rehabilitation plan-of-care, to which the rehabilitation specialist must tailor their exercise prescription in an effort to optimize outcomes after ACLR.
Although previous literature has described rehabilitation considerations for the BPTB and HT autografts,28,36–39 there is less published with respect to the QT.39–41 Therefore, the purpose of this clinical commentary is to present the graft-specific surgical and rehabilitation considerations for ACLR with the QT, as well as further highlight the need for graft-specific rehabilitation strategies after ACLR by comparing the QT to the BPTB and HT autografts.
ANATOMIC AND BIOMECHANICAL CONSIDERATIONS
The quadriceps and hamstring tendons are different than the patellar tendon in their innate function to connect muscle-to-bone, whereas the patellar tendon connects bone-to-bone. Considering this, differences in stiffness and elastic properties are known to exist between autograft tissue used for ACLR,42–44 with the quadriceps tendon producing more absolute stiffness than both the patellar and semitendinosus tendons but a lower elastic modulus and relative strain tolerance than the patellar tendon24,28,44–46 (Table 1).
Table 1. Biomechanical characteristics of the native anterior cruciate ligament and common autografts used for anterior cruciate ligament reconstruction.
| Graft Type |
Cross-Sectional Area
(mm2) |
Maximal
Load To Failure (N) |
Ultimate Stiffness
(N/mm) |
Ultimate Stress
(N/mm2) |
Ultimate Strain
(%) |
Common Failure Location |
|---|---|---|---|---|---|---|
| Native ACL*§ | 44 | 2160 | 242 | 49 | 20 | |
| BPTB Autograft†ǁ≠ | 48 | 1580-1810 | 278-324 | 69.9 | 14 | Deep Layer of Patellar Interface / Femoral Origin / Mid-substance |
| HT Autograft‡§ǁ≠ | 11 (1-strand) 23 (2-strand) |
1060 (1-Stand) 2330 (2-stand) 1750 (4-stand) |
213 (1-Stand) 469 (2-stand) 433 (4-stand) |
99 (1-Stand) 100 (2-stand) |
11.6 (4-stand) | Mid-Substance / Universal Stretch |
|
B-QT†≠ (Full Thickness) |
91 | 1450-2186 | 370-466 | 49 | 11.2 | Bone-Tendon Interface |
|
S-QT≠ (Full Thickness) |
1260 | 257 | Proximal Graft / Universal Stretch | |||
|
S-QT≠ (Partial Thickness) |
972 | 228 | Distal Graft / Universal Stretch |
ACL; anterior cruciate ligament, BPTB; bone-patellar tendon-bone, HT; hamstring tendon, B-QT; quadriceps tendon with a patellar bone block; S-QT, all soft-tissue quadriceps tendon; *includes data from Woo et al42; †includes data from Shani et al24; ‡ includes data from Hamner et al45; § includes data from Schilaty et al43; ǁ includes data from Strauss et al44; ≠ includes data from Magnussan et al47
While these findings reflect total-graft biomechanical properties, previous work has highlighted the fact that regional variation in tendon elasticity and stiffness may also exist; the tendon region closest to the myotendinous junction is less stiff than the tendon region adjacent to the enthesis.48 This is an important consideration, as biomechanically-induced graft failure studies have reported a difference in failure location for the QT harvested with a patellar bone block (B-QT) than that of the BPTB and multiple-strand HT autografts; failure of the B-QT was most common at the bone-tendon interface,28,44 whereas universal stretch/mid-substance failures have been reported with the all soft-tissue QT (S-QT), BPTB and multiple-strand HT.28,43–45,47 These observations suggest the B-QT has more within-graft variation in regional elasticity and structure, creating increased stress at the bone-tendon interface and the observed graft failure-location.26,44,49
Compared to the HT and BPTB, more variation in laminar structure is present with the QT. In contrast to the continuous structure of the hamstring and patellar tendons, the quadriceps tendon is typically described as a common tendon with a three-layered arrangement; a superficial layer derived from rectus femoris, an intermediate layer from vastus medialis and vastus lateralis, and a deep layer from vastus intermedius.26–28 Although the extent to which laminar structure contributes to graft fixation pull-through is unknown, a biomechanical study by Arakagi et al50 reported significant suspensory fixation pull-through with a 150-newton load on the S-QT relative to a bone-block control.
GRAFT COMPOSITION AND HARVESTING TECHNIQUE CONSIDERATIONS
The harvesting technique of the QT can vary, and along with this, different rehabilitation considerations for graft composition are warranted. The B-QT facilitates partial graft osteointegration as early as 4-6 weeks after ACLR through the bone-to-bone healing of the single bone block within the bone tunnel,51,52 but likewise, carries a 1.4-8.8% risk of patellar fracture due to bone block harvest.53–55 Conversely, the S-QT is harvested without a patellar bone block and mitigates the risk of patellar fracture,54 but will take a minimum of 10 to 12-weeks for the fibrovascular interface to form between the S-QT and the bone tunnels.28,56–58 This between-graft difference in integration, in conjunction with the findings of Arakagi et al,50 suggests accelerated rehabilitation approaches may be less appropriate for the S-QT fixated with suspensory fixation, especially as graft tension is highly dependent on fixation until biological integration of the graft within the bone tunnels has occurred. While this is an extrapolated suggestion, short-term increases in graft laxity have been reported with the early introduction of open-kinetic-chain (OKC) quadriceps resistance training after ACLR, to which slightly increased levels of graft laxity were reported with the HT relative to the BPTB when OKC quadriceps resistance training with distal tibial load was initiated between 0-45 degrees of knee flexion weeks 6-12 after ACLR.59
The theoretical advantage of graft osteointegration with the B-QT is not currently supported by the literature.28,56–58 Specifically, a higher incidence of postoperative rotatory instability (16% vs 0%) and atraumatic graft ruptures (24% vs 0%) have been observed after ACLR with the B-QT compared to the S-QT54; these findings suggest ACLR with the S-QT may yield better postoperative stability than the B-QT. However, evidence is still limited,54 and the full-thickness B-QT appears to be more biomechanically similar to the BPTB than the S-QT, as well as may better-replicate the tissue properties of the native anterior cruciate ligament42,44 (Table 1). Lastly, ACLR with the S-QT may not provide adequate quadriceps tendon graft-length in some populations,60 especially women,61 and cosmetic retraction of the rectus femoris is a known complication related to proximal QT harvest.28,53,55
Outcomes comparing the full-thickness QT (F-QT) to the partial-thickness QT (P-QT) are limited with only one direct comparison published within the literature.62 QT thickness does not appear to influence donor site pain, failure rates or patient-reported outcomes.63 However, the biomechanical properties of the P-QT appear to be less robust than the F-QT44 (Table 1).
The F-QT produces a larger diameter graft and causes deeper disruption of the tissue at the graft harvest site. With this, violation of the suprapatellar pouch with F-QT harvest can produce a suprapatellar hematoma,53 which is a known complication after ACLR with the F-QT.40 More postoperative quadriceps inhibition may also be theorized with the F-QT relative to the P-QT, as full-thickness quadriceps tendon harvest will disrupt the laminar layers associated with the vastus medialis, vastus lateralis and vastus intermedius.26,27,64 Along with the inevitable increase in suprapatellar scarring, the high collagen density and graft-specific stiffness of the QT are suggested reasons for the observed incidence of arthrofibrosis after ACLR with the QT,20,40,65,66 to which the F-QT may exacerbate.67
EXTENSOR MECHANISM CONSIDERATIONS
Harvesting the P-QT may reduce the tensile strength of the quadriceps tendon by as much as 34%, which is greater than the 25% reduction in patellar tendon tensile strength after BPTB harvest.23 These findings have implications for rehabilitation, as greater impairments in quadriceps strength have been observed after ACLR with the QT and BPTB than with the HT.14,32–34,68 Following QT harvest, reduced quadriceps activation and strength may initially create a more protective healing environment at the graft harvest site. However, long-term reductions in quadriceps strength are detrimental to knee function and are one of the reasons why it may take longer to achieve performance testing milestones after ACLR with the QT and BPTB than with the HT.33,38,39,68
Considering P-QT harvest reduces the tensile strength of the quadriceps tendon by more than a third,23 a greater initial reduction in quadriceps strength may be expected after ACLR with the QT compared to the BPTB and HT.68 Quadriceps weakness from extensor mechanism graft harvest appears most extreme during the first three months after ACLR,68 suggesting any difference in quadriceps strength between ACLR with the QT and BPTB may only be distinguishable during the first three to four months after ACLR34,68; this suggestion is supported by the fact quadriceps strength is not statistically different between the QT and the BPTB at six to 24 month follow-up.34,68,69
REHABILITATION CONSIDERATIONS
Early Phase (Postoperative Weeks 0-8)
After ACLR with the QT, the graft’s composition and fixation method should be communicated to the rehabilitation specialist, as these factors dictate the overall graft ligamentization process35,70–72; the amount of tissue trauma at the graft harvest site44; and the durability of the graft-bone tunnel construct.29–31,50,73 ACLR with the F-QT carries the risk of developing a suprapatellar hematoma55,63; pain and focal swelling at the graft harvest site is indicative of a hematoma and should be differentiated from a postoperative knee effusion.40 If a suprapatellar hematoma is identified, the surgical team should be notified as physician follow-up may be indicated.
The early restoration of passive knee extension is a crucial component of rehabilitation after ACLR, regardless of graft type.74 ACLR with the QT may carry an elevated risk of postoperative stiffness due to the larger graft size,67 presence of suprapatellar scarring and ongoing quadriceps inhibition.20,40,65,66 Interventions to improve patellar mobility, knee range-of-motion and soft tissue compliance should be implemented immediately after surgery. Failure to restore passive knee extension by postoperative week eight may indicate the need for a subsequent lysis-of-adhesions procedure.20,65
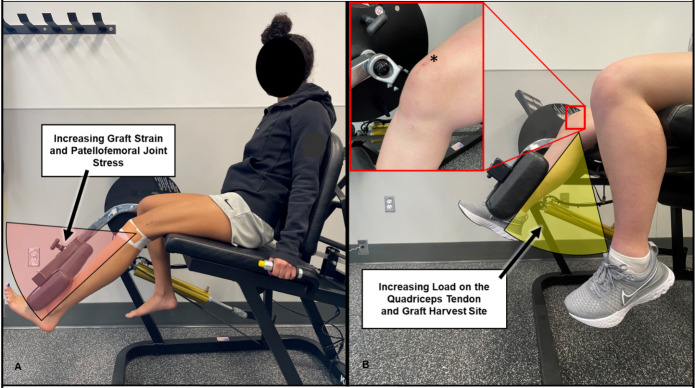
Like the BPTB, ACLR with the QT requires an isolated quadriceps training load-progression to be a cornerstone of the rehabilitation program.33,34,75,76 Early phase quadriceps rehabilitation should include quadriceps setting and other activation exercises into terminal knee extension (TKE), with the goal of restoring active knee extension as soon as possible (Table 2). The early implementation of neuromuscular electrical stimulation and/or blood flow restriction during quadriceps exercise may improve neuromuscular recruitment and help mitigate thigh muscle atrophy,77–80 as well as facilitate improvements in muscle size and strength throughout rehabilitation.81–83 The quadriceps muscle load-progression should start with quadriceps setting and straight-leg raises in non-weightbearing, and progress onto closed-kinetic-chain (CKC) positions which emphasize the restoration of knee control in weightbearing (Table 2).84 The CKC quadriceps load-progression should begin with the double-leg squat exercise and incorporate body-weight isometric and isotonic contractions in low levels of knee flexion (Figure 1A) (Table 2).85
Table 2. Example of a quadriceps muscle/tendon load-progression after anterior cruciate ligament reconstruction with an all soft-tissue quadriceps tendon autograft fixated with suspensory fixation.
| Postoperative Month |
Single-Leg
Progression |
Split-Squat
Progression |
Open-Kinetic-Chain
Progression |
|---|---|---|---|
| Month 0-1 |
Banded TKE (Sitting at Edge of Surface) Prescription Type: Neuromuscular Reeducation and Muscle Activation F: 3-4 times/day I: Elastic resistance band exercise (light to heavy) T: Isotonic (concentric/eccentric phase) T: 10-15 minutes each exposure V: 2-4 sets of 10-20 repetition with a 1-3 second isometric contraction in TKE P: Progression of elastic resistance band level; superimposition of NMES with exercise; progression onto blood flow restriction exercise (1-2 times/day, 3-4 set to volitional fatigue at 80% LOP) |
Quadriceps Setting (Straight Leg Raise) Prescription Type: Neuromuscular Reeducation and Muscle Activation F: 3-6 times/day I: Progressive increase in contraction intensity onto the straight leg raise exercise T: Isometric quadriceps contraction training T: 8-10 minutes each exposure V: 2-4 sets of 10-20 repetition with a 1-3 second isometric contraction in TKE P: Progression of body position and/or onto the straight leg raise exercise (with/without external resistance at the ankle); superimposition of NMES with exercise; progression onto blood flow restriction exercise (1-2 exposures/day, 3-4 set to volitional fatigue at 80% LOP) |
Short/Long-Arc Quad (AROM) Prescription Type: Neuromuscular Reeducation and Muscle Activation F: 3-4 times/day I: Weight of lower leg T: Isotonic (concentric/eccentric phase) T: 10-15 minutes each exposure V: 2-4 sets of 10-20 repetition with a 1-3 second isometric contraction in TKE P: Progression of contraction intensity and knee flexion angle during exercise; superimposition of NMES with exercise; progression onto blood flow restriction exercise (1-2 times/day, 3-4 set to volitional fatigue at 80% LOP) |
| Month 1-2 |
Banded TKE (Standing) Prescription Type: Neuromuscular Reeducation and Muscle Activation F: 2-3 times/day I: Elastic resistance band (light to heavy) T: Isotonic (concentric/eccentric phase) T: 10-15 minutes each exposure V: 3-4 sets of 10-20 repetition with a 1-3 second isometric contraction in TKE P: Progression of elastic resistance band level; progression onto blood flow restriction exercise (1-2 times/day, 3-4 set to volitional fatigue at 80% LOP) |
Double-Leg Squat (0-60 Degrees of Knee Flexion) Prescription Type: Neuromuscular Reeducation and Muscle Activation F: 2-3 times/day I: Body weight (0-60 degrees of knee flexion) T: Isotonic (concentric/eccentric phase) or Isometric T: 10-15 minutes each exposure V: 3-4 sets of 10-15 repetition followed by a 45-90 second isometric contractions in 45-60 degrees of knee flexion | 30-90-second rest periods between sets P: Progression of knee flexion angle, positive shin angle and duration of isometric contraction; redistribution of weight toward the surgical limb |
Long-Arc Quad (AROM with Blood Flow Restriction) Prescription Type: Cell Swelling/Atrophy Mitigation/Hypertrophy F: 1-2 times/day I: Weight of lower leg, blood flow restriction at 80% LOP T: Isotonic (concentric/eccentric phase) | 0-90+ degrees of knee flexion T: 10-20 minutes each exposure V: 3-4 sets to volitional fatigue | 30-90-second rest periods between sets P: Addition of progressive isometric contractions at 45-90 degrees of knee flexion with/without the superimposition of NMES |
| Month 2-3 |
Double-Leg Wall Squat (60-90+ Degrees of Knee Flexion) Prescription Type: Extensor Mechanism Load-Tolerance/Hypertrophy F: 3-5 times/week I: Body weight (60-90+ degrees of knee flexion) T: Isometric T: 5-10 minutes each exposure V: 3-4 sets of 45-90 second isometric contractions | 2-5-minute rest periods between sets P: Progression of knee flexion angle, positive shin angle, or duration of isometric contraction; pressure redistribution of additional weight onto the surgical limb |
Split-Squat (0-60 Degrees of Knee Flexion) Prescription Type: Neuromuscular Reeducation and Muscle Activation F: 2-3 times/day I: Body weight (0-60 degrees of knee flexion) on involved limb T: Isotonic (concentric/eccentric phase) or Isometric T: 5-10 minutes each exposure V: 3-4 sets of 10-15 repetition followed by a 45-60 second isometric contractions in shallow knee flexion | 30-90-second rest periods between sets P: Progression of knee flexion angle, positive shin angle or duration of isometric contraction; redistribution of weight onto the surgical limb |
Knee Extension Machine (Single-Leg with Blood Flow Restriction) Prescription Type: Hypertrophy/Strength F: 3-5 times/week I: 15-30 RM (<40-65% 1-RM) of involved limb, blood follow restriction at 80% LOP T: Isotonic (concentric/eccentric phase) | 45-90+ degrees of knee flexion T: 5-10 minutes each exposure V: 3-4 sets to volitional fatigue | 2-5-minute rest periods between sets P: Progression of external resistance at the distal tibia |
| Month 3-4 |
Leg Press Machine (Single-Leg with Blood Flow Restriction) Prescription Type: Hypertrophy/Strength F: 2-4 times/week I: 10-20 RM (40-75% 1-RM) on the involved limb, blood follow restriction at 80% limb occlusion pressure T: Isotonic (concentric/eccentric phase) T: 5-10 minutes each exposure V: 3-4 sets to volitional fatigue | 2-5-minute rest periods between sets P: Progression of knee flexion angle, positive shin angle or external resistance |
Split -Squat (60-90+ Degrees Knee Flexion) Prescription Type: Hypertrophy/Strength F: 2-4 times/week I: Body weight (60-90+ degrees of knee flexion) on the involved limb T: Isometric T: 5-10 minutes each exposure V: 3-4 sets of 45-90 second isometric contractions in progressively deeper knee flexion | 2-5-minute rest periods between sets P: Progression of knee flexion angle, positive |
Knee Extension Machine (Single-Leg with Blood Flow Restriction) Prescription Type: Hypertrophy/Strength F: 2-4 times/week I: 15-20 RM (40-65% 1-RM) of involved limb, blood follow restriction at 80% limb occlusion pressure T: Isotonic (concentric/eccentric phase) | 0-90+ degrees of knee flexion T: 5-10 minutes each exposure V: 3-4 sets to volitional fatigue | 2-5-minute rest periods between sets P: Progression of external resistance at the distal tibial |
| Month 4-6 |
Leg Press (Single-Leg with Increasing Load) Prescription Type: Hypertrophy/Strength F: 2-4 times/week I: 6-15 RM (65-85% 1-RM) on the involved limb T: Isotonic (concentric/eccentric phase) T: 5-10 minutes each exposure V: 3-4 sets to volitional fatigue | 2-5-minute rest periods between sets P: Progression of knee flexion angle, positive shin angle or external resistance |
Split-Squat (Rearfoot-Elevated Position) Prescription Type: Hypertrophy/Strength F: 2-4 times/week I: 6-15 RM (65-85% 1-RM) on the involved limb T: Isotonic (concentric/eccentric phase) T: 5-10 minutes each exposure V: 3-4 sets to volitional fatigue | 2-5-minute rest periods between sets P: Progression of knee flexion angle, positive shin angle or external resistance |
Knee Extension Machine (Single-Leg with Increasing Load) Prescription Type: Hypertrophy/Strength F: 2-4 times/week I: 6-15 RM (65-85% 1-RM) on the involved limb T: Isotonic (concentric/eccentric phase) | 0-90+ degrees of knee flexion T: 5-10 minutes each exposure V: 3-4 sets to volitional fatigue | 2-5-minute rest periods between sets P: Progression of external resistance at the distal tibial |
| Month 6+ |
Eccentric Leg Press (2-Legs Up Concentric / 1-Leg Down Eccentric) Prescription Type: Hypertrophy/ Eccentric Strength F: 2-3 times/week I: 1-5 RM (85-100% 1-RM) on the involved limb T: Eccentric resistance training T: 5-10 minutes each exposure V: 3-4 sets of 8-15 eccentric repetitions | 2-5-minute rest periods between sets P: Progression of knee flexion angle, positive shin angle or external resistance greater than a 1-RM (e.g., 120% 1-RM) |
Split-Squat Jumps (Lunge or Rearfoot-Elevated Position) Prescription Type: Power F: 2-4 times/week I: Body weight to 40-60% 1-RM on the involved limb T: Isotonic (concentric/eccentric phase), emphasis on speed/effort during the concentric phase of the movement T: 5-10 minutes each exposure V: 4-5 sets of 3-5 reps | 2-5-minute rest period between sets P: Progression of knee flexion angle, positive shin angle, contraction speed or external load |
Eccentric Knee Extension Machine (2-Legs Up Concentric / 1-Leg Down Eccentric) Prescription Type: Hypertrophy/ Eccentric Strength F: 2-3 times/week I: 1-5 RM (85-100% 1-RM) on the involved limb T: Eccentric resistance training | 0-90+ degrees of knee flexion T: 5-10 minutes each exposure V: 3-4 sets of 8-15 eccentric repetitions | 2-5-minute rest periods between sets P: Progression of external resistance greater than a 1-RM (e.g., 110% 1-RM) |
F, frequency; I, intensity; T, type; T, time; V, volume; P, progression; AROM, active range-of-motion; TKE, terminal knee extension; LOP, limb occlusion pressure, RM, repetition maximum, 1-RM, 1-repetition maximum
Figure 1. Closed-kinetic-chain load-progression for the surgical limb.
Suboptimal progression of unilateral loading from a double leg regression (A) to a rear-foot elevated split-squat (B) with a subsequent increase in knee flexion angle and external resistance (C). Theoretically proper progression of unilateral loading from a double leg regression (A) to a split-squat (D) with the subsequent addition of external resistance (E). No change in knee flexion angle throughout progression (A-D-E). Red dash-arrow, approximate ground reaction force-vector; white lines, depiction of joint angles; red lines, depiction of increasing knee flexion; yellow lines in (A-D-E), depiction of knee/quadriceps-dominant movement with a positive shin angle; yellow shading, depiction of external knee flexion moment related to knee/quadriceps-dominant movement; red circles, improper exercise selection; green circles, proper exercise selection.
Graft osteointegration with the B-QT supports the implementation of an accelerated resistance training approach within the first 4-6 weeks after ACLR,59 such as OKC quadriceps resistance training with distal tibial load between 0-45 degrees of knee flexion86; the combined utilization of the B-QT with interference screw fixation may further justify this clinical decision29–31,44,50,70,71,87 (Table 3). The S-QT fixated with suspensory fixation may warrant a more traditional approach to resistance training the first 10-12 weeks after ACLR59,72,73,87,88 (Table 2); healing time is needed to mitigate the risk of fixation slippage,50,73,85,89 graft laxity and bone tunnel widening with an all soft-tissue graft,17,29–31,50 as well as facilitate optimal fibrovascular integration of the graft within the bone tunnels72,87,89–93 (Table 3).
Table 3. Rehabilitation Overview.
| Consideration | Location | Description of Consideration(s) | |
|---|---|---|---|
| Early Phase Rehabilitation Considerations (Postoperative Weeks 0-8) |
Graft Composition | Intra-Articular |
B-QT
S-QT
F-QT
|
| OKC Quadriceps Resistance Training / Graft Fixation | Intra-Articular |
OKC Exercise with Interference Screw Fixation (B-QT)
OKC Exercise with Suspensory Fixation (S-QT)
|
|
| Graft Harvest Site | Extra-Articular |
B-QT
F-QT
|
|
| Middle Phase Rehabilitation Considerations (Postoperative Weeks 8-16) |
Graft Composition | Extra-Articular |
P-QT
F-QT
|
| Graft Harvest Site | Extra-Articular |
Gradual and Progressive Quadriceps Loading into Deep Knee Flexion
|
|
| Late Phase Rehabilitation Considerations (Postoperative Weeks 16+) |
Graft Harvest Site | Extra-Articular |
Ongoing Quadriceps Strengthening Program
Progression of Energy Storage Activities into Increasing Knee Flexion
|
B-QT, quadriceps tendon autograft with patellar bone-block; S-QT, all soft-tissue quadriceps tendon autograft; F-QT, full-thickness quadriceps tendon autograft; OKC, open-kinetic-chain; AROM, active range-of-motion; P-QT, partial-thickness quadriceps tendon autograft; CKC, closed-kinetic-chain
Middle Phase (Postoperative Weeks 8-16)
As goals related to joint homeostasis are achieved, the focus of rehabilitation transitions from resolving impairments in muscle activation and knee range-of-motion, to rebuilding the surgical limb’s functional capacity to manage load. Ongoing quadriceps weakness is expected after ACLR with the QT,14,15,33,34,75 and knee-specific load-progressions should be designed to best-manage the graft harvest site while stimulating improvements in quadriceps size and strength. Prior research has highlighted associations between knee position and extensor mechanism biomechanics,94–96 from which the quadriceps training load-progressions can be derived (Table 2).
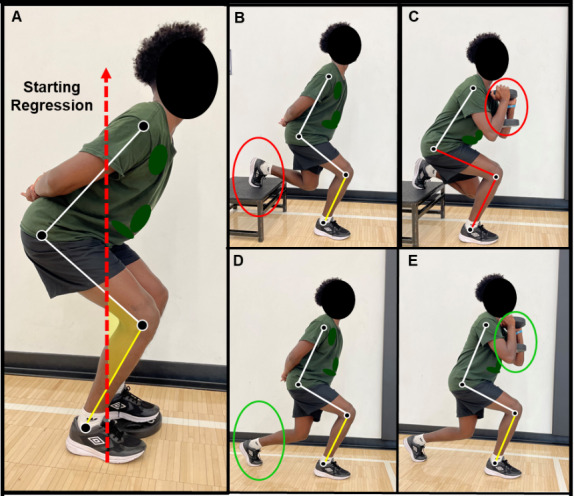
As the knee moves into deeper knee flexion, preferential loading of the quadriceps tendon increases relative to the patellar tendon.94 This load-transition is the result of an improving patellar tendon mechanical advantage with a concurrent increase in passive tension within the quadriceps.94,95 Considering the laminar structure of the quadriceps tendon, variations in quadriceps length-tension can predispose the quadriceps tendon to greater levels of shear/compressive load, as well as non-uniform intratendinous force-transmission. Specifically, performing the prone knee flexion stretch will preferentially tension the superficial layer of the quadriceps tendon by maximally lengthening rectus femoris, compressing/shearing the deeper layers of the tendon95,97,98; this unique type of tendon loading can be prescribed in addition to strength training to mobilize the graft harvest site and may help stimulate quadriceps tendon remodeling (Figure 2).
Figure 2. Selective tensioning of the superficial layer of the quadriceps tendon.
Selective tensioning of the superficial layer of the quadriceps tendon is achieved by maximally lengthening rectus femoris into the combined motion of hip extension and knee flexion; low-velocity stretching may be therapeutically prescribed to shear/mobilize the graft harvest site (A), whereas high-velocity activities should be thoughtfully progressed with ongoing monitoring of the graft harvest site for any increase in tissue irritability. Asterisk, quadriceps tendon autograft harvest site; white lines, depiction of joint angles; black dash-arrow, high-velocity eccentric lengthening of the quadriceps muscle during the wind-up phase of kicking
Months 2-4 after ACLR with the QT, the CKC quadriceps load-progression should include isometric or isotonic contractions with a light to moderate external resistance. Initially, body weight isometric exercise in low levels of knee flexion may best manage graft harvest site irritability94,99 (Figure 1A) (Table 2). As exercise tolerance improves, the quadriceps load-progression should be advanced by monitoring the graft harvest site for any increase in pain/irritability with exercise while gradually progressing external resistance or the level of knee flexion95 (Figure 1A-D-E). The rehabilitation specialist should not advance too many variables at once, as simultaneously increasing external resistance and the level of knee flexion can exponentially load the quadriceps tendon and may provoke graft harvest site pain94,95 (Figure 1C).
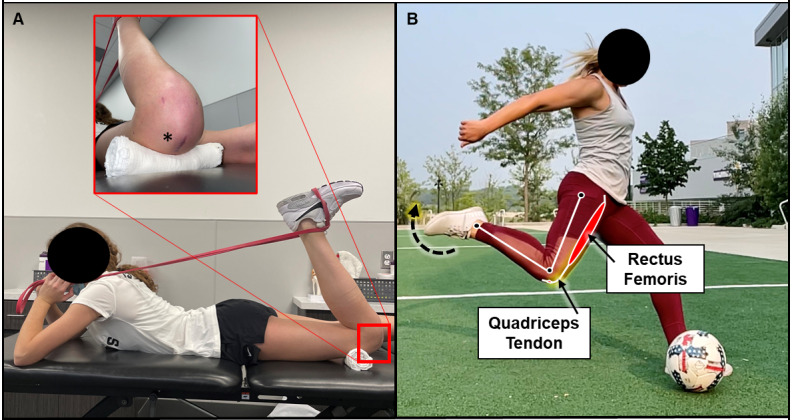
Graft-specific load-progressions for the P-QT may also exist, in which more specific targeting of the superficial layer of the quadriceps tendon/rectus femoris with OKC exercise may be indicated.98,100 The long-arc-quad exercise should be advanced from active range-of-motion during the early phase of rehabilitation,85 to OKC quadriceps resistance training on a knee extension machine (Table 2); the rehabilitation specialist may elect to perform OKC quadriceps resistance training with the hip positioned in lower levels of hip flexion to preferentially load rectus femoris (i.e., performing OKC quadriceps resistance training with the trunk positioned in supine).95,97,98 External resistance should be thoughtfully progressed, as performing OKC quadriceps resistance training between 0-45 degrees of knee flexion will increase patellofemoral compartment stress and preferentially strain the reconstructed ACL graft85,86,101 (Figure 3A), whereas performing OKC quadriceps resistance training in deeper levels of knee flexion will preferentially load the quadriceps tendon and may provoke irritability at the graft harvest site94,95 (Figure 3B).
Figure 3. Considerations for open-kinetic-chain quadriceps resistance training with distal tibial load.
Performing quadriceps resistance training between 0-45 degrees of knee flexion with distal tibial load will produce higher patellofemoral joint stress and increase strain on the reconstructed anterior cruciate ligament (A), whereas performing resisted knee extensions in deeper levels of knee flexion will preferentially load the quadriceps tendon relative to the patellar tendon. Red arc, 0-45 degrees of knee flexion; yellow arc, >45 degrees of knee flexion; Black asterisk, quadriceps tendon autograft harvest site
Late Phase (Postoperative Weeks 16+)
As the surgical limb develops the capacity to perform higher-load activities at slow contraction velocities, higher demand exercise progressions should be introduced. Patients participating in physically demanding activities, such as Level 1 sports, will benefit from exposure to plyometric and ballistic-type exercise progressions. The rehabilitation specialist should consider the quadriceps tendon a rate-limiting tissue for the introduction of plyometric exercise,23 as the QT harvest site must store and transfer energy during these progressions. Plyometric exercise should be initiated with knee-specific regressions that temper the demand for elastic energy-storage within the quadriceps tendon, such as running drills in triple-extension or frontal plane plyometric exercise94,102,103 (Figure 4).
Figure 4. Sagittal deceleration task vs lateral plyometric task.
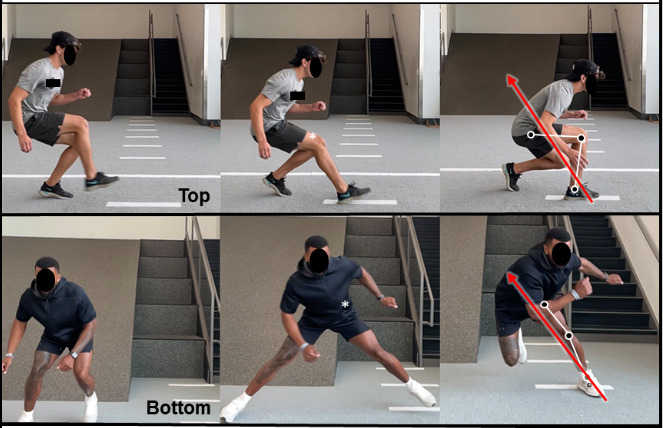
The resultant ground reaction force during a sagittal plane deceleration task (top sequence from left to right) places a large amount of load on the knee and quadriceps tendon, whereas a lateral plyometric task places more relative load proximally on the lateral hip and trunk (bottom sequence from left to right). Red arrows, resultant ground reaction force-vector; white lines, depiction of joint angels; asterisks, area of high load-demand during task.
As mentioned previously, specific consideration should be given for ballistic activities that require the quadriceps tendon to transfer load while in the combined position of hip extension and knee flexion, such as the wind-up phase of kicking or high-velocity running104,105 (Figure 2B); these activities combine high angular velocities and tendinous compressive/shear force by the selective-tensioning of the superficial layer of the quadriceps tendon running continuous with rectus femoris.95,97 Sagittal plane deceleration training will also preferentially load the quadriceps tendon. During deceleration, the combination of large external knee flexion moments, increasing knee flexion angles, and high-force eccentric quadriceps contractions can produce exponentially higher load-transmission within the quadriceps tendon (Figure 4); sagittal plane deceleration training must be thoughtfully progressed per exercise-tolerance and symptom-response at the graft harvest site.
RETURN TO ACTIVITY CONSIDERATIONS
Regardless of the graft type used for ACLR, most individuals expect to restore knee joint stability and function to a level that supports the return to their pre-injury activity level.106 However, only 65% of individuals may return to their pre-injury level of sports participation,107 with knee re-injury rates between 20-30% within higher-risk cohorts.108–110 Equally troubling is the unclear association between return-to-activity testing batteries and the subsequent risk of knee re-injury within various cohorts,111–117 and although the restoration of limb function on objective performance tests appears to improve return-to-sport rates,118–120 the use of performance testing cut-points as strict, medically-required, return-to-activity criteria remains controversial.112,121–123 Recent literature has highlighted the importance of shared decision-making after ACLR,124,125 to which the use of a decision-making framework may improve the return-to-activity decision-making process.124,126–129
To best inform shared decision-making, serial physical examinations and performance testing batteries should be completed throughout rehabilitation.130,131 Physical examinations should include the assessment of knee homeostasis (effusion and irritability), stability and range-of-motion.132 After ACLR with the QT, quadriceps strength testing should be a fundamental component of the performance testing battery, as quadriceps strength appears most affected by QT harvest,33,34,68 and quadriceps strength deficits are common 9-12 months after ACLR.34 Other components of a performance testing battery may include jump/hop testing and the assessment of movement quality; these tests should include both qualitative and quantitative measurements.132 Collectively, this information can be utilized throughout rehabilitation to confirm the effectiveness of exercise interventions, adjust the exercise prescription(s), and inform return-to-activity decision-making.133
Of the various data synthesized for return-to-activity decision-making, some information may be more important than others. The timeframe between ACLR and return-to-activity has been observed to be a modifiable risk factor for knee re-injury,111,134 with the suggestion that most individuals should wait a minimum of nine months before returning to unrestricted sports participation.111,122,132 Risk calculator algorithms formulated to predict the risk of revision ACLR have been recently validated for clinical use135,136; these algorithms are based upon data that is specific to the individual of interest, including age, body mass index, preoperative knee laxity, activity level and graft type.135,136 The ACL-Return to Sport after Injury (ACL-RSI) is a validated psychometric scale, and should be used to assess an individual’s psychological readiness for sports participation after ACLR.132
Comprehensive rehabilitation and return-to-sport programming can facilitate improved limb function on objective performance tests,133,137 achieve higher return-to-sport rates and reduce the risk of knee re-injury.133,138–141 Comprehensive programming should include formal strength and conditioning sessions, as well as the integration of jumping/hopping, cutting and sport-specific load-progressions. Late phase load-progressions should include a period of on-field rehabilitation with all relevant stakeholders (e.g., athlete, coach, guardian, and rehabilitation specialist) in agreement with the return-to-practice and competition progressions.131,133,142 On-field rehabilitation should follow the control-chaos continuum and facilitate graded exposure to sports participation.133,135,142,143
Prior to commencing unrestricted activity, a final physical examination and performance testing battery should be completed with all relevant information clearly synthesized for analysis within the shared decision-making framework.124–129,133 If the individual is returning to an activity with a high risk of knee re-injury, such as Level 1 sports, secondary injury reduction strategies should be implemented regardless of performance testing status.144 Pre-activity neuromuscular warmups, such as the FIFA 11+, appear highly effective at mitigating known biomechanical risk factors for anterior cruciate ligament injury,145–148 and can significantly reduce the overall injury incidence rate.149
Conflicts of Interest
The above authors have no financial disclosures or conflicts of interest related to the development and publication efforts of this manuscript
Acknowledgments
Acknowledgements
We extend a special thank you to Dr. George Davies, DPT, and Dr. Steven Stovitz, MD for their gift of time, mentoring, and teaching within their respective sports medicine communities.
Thank you to the physical therapists, sports scientists, and licensed athletic trainers at Training HAUS for their ongoing teamwork and support, as well as the research department at Twin Cities Orthopedics for their support with ongoing research projects.
Funding Statement
No grant support was provided to aid in the development and publication efforts of this manuscript
References
- Arendt Elizabeth, Dick Randall. The American Journal of Sports Medicine. 6. Vol. 23. SAGE Publications; Knee injury patterns among men and women in collegiate basketball and soccer; pp. 694–701. [DOI] [PubMed] [Google Scholar]
- Gwinn David E., Wilckens John H., McDevitt Edward R., Ross Glen, Kao Tzu-Cheg. The American Journal of Sports Medicine. 1. Vol. 28. SAGE Publications; The relative incidence of anterior cruciate ligament injury in men and women at the United States Naval Academy; pp. 98–102. [DOI] [PubMed] [Google Scholar]
- Hewett Timothy E., Myer Gregory D., Ford Kevin R. The American Journal of Sports Medicine. 2. Vol. 34. SAGE Publications; Anterior cruciate ligament injuries in female athletes: Part 1, mechanisms and risk factors; pp. 299–311. [DOI] [PubMed] [Google Scholar]
- ‘What’s my risk of sustaining an ACL injury while playing football (soccer)?’ A systematic review with meta-analysis. Montalvo Alicia M, Schneider Daniel K, Silva Paula L, Yut Laura, Webster Kate E, Riley Michael A, Kiefer Adam W, Doherty-Restrepo Jennifer L, Myer Gregory D. 2019British Journal of Sports Medicine. 53(21):1333–1340. doi: 10.1136/bjsports-2016-097261. doi: 10.1136/bjsports-2016-097261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beliefs and attitudes of members of the American Academy of orthopaedic surgeons regarding the treatment of anterior cruciate ligament injury. Marx Robert G, Jones Edward C, Angel Michael, Wickiewicz Thomas L, Warren Russell F. Sep;2003 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 19(7):762–770. doi: 10.1016/s0749-8063(03)00398-0. doi: 10.1016/s0749-8063(03)00398-0. [DOI] [PubMed] [Google Scholar]
- Why bone-patella tendon-bone grafts should still be considered the gold standard for anterior cruciate ligament reconstruction. Carmichael J. R, Cross M. J. Mar 8;2009 British Journal of Sports Medicine. 43(5):323–325. doi: 10.1136/bjsm.2009.058024. doi: 10.1136/bjsm.2009.058024. [DOI] [PubMed] [Google Scholar]
- Gifstad Tone, Foss Olav A., Engebretsen Lars, Lind Martin, Forssblad Magnus, Albrektsen Grethe, Drogset Jon Olav. The American Journal of Sports Medicine. 10. Vol. 42. SAGE Publications; Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia; pp. 2319–2328. [DOI] [PubMed] [Google Scholar]
- Sundemo David, Hamrin Senorski Eric, Karlsson Louise, Horvath Alexandra, Juul-Kristensen Birgit, Karlsson Jon, Ayeni Olufemi R, Samuelsson Kristian. BMJ Open Sport & Exercise Medicine. 1. Vol. 5. BMJ; Generalised joint hypermobility increases ACL injury risk and is associated with inferior outcome after ACL reconstruction: a systematic review; p. e000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Generalized joint laxity Is associated with increased failure rates of primary anterior cruciate ligament reconstructions: a systematic review. Krebs Nathan M., Barber-Westin Sue, Noyes Frank R. Jul;2021 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 37(7):2337–2347. doi: 10.1016/j.arthro.2021.02.021. doi: 10.1016/j.arthro.2021.02.021. [DOI] [PubMed] [Google Scholar]
- “Anatomic” anterior cruciate ligament reconstruction: a systematic review of surgical techniques and reporting of surgical data. van Eck Carola F., Schreiber Verena M., Mejia Hector A., Samuelsson Kristian, van Dijk C. Niek, Karlsson Jon, Fu Freddie H. Sep;2010 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 26(9):S2–S12. doi: 10.1016/j.arthro.2010.03.005. doi: 10.1016/j.arthro.2010.03.005. [DOI] [PubMed] [Google Scholar]
- Middleton K. K., Hamilton T., Irrgang J. J., Karlsson J., Harner C. D., Fu F. H. Knee Surgery, Sports Traumatology, Arthroscopy. 7. Vol. 22. Springer Science and Business Media LLC; Anatomic anterior cruciate ligament (ACL) reconstruction: a global perspective. Part 1; pp. 1467–1482. [DOI] [PubMed] [Google Scholar]
- Editorial Commentary: Quadriceps tendon autograft use for anterior cruciate ligament reconstruction predicted to increase. Lubowitz James H. Jan;2016 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 32(1):76–77. doi: 10.1016/j.arthro.2015.11.004. doi: 10.1016/j.arthro.2015.11.004. [DOI] [PubMed] [Google Scholar]
- Quadriceps tendon autograft is becoming increasingly popular in revision ACL reconstruction. Winkler Philipp W., Vivacqua Thiago, Thomassen Stephan, Lovse Lisa, Lesniak Bryson P., Getgood Alan M. J., Musahl Volker. 2022Knee Surgery, Sports Traumatology, Arthroscopy. 30(1):149–160. doi: 10.1007/s00167-021-06478-y. doi: 10.1007/s00167-021-06478-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction: a systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone-patellar tendon-bone and hamstring-tendon autografts. Mouarbes Dany, Menetrey Jacques, Marot Vincent, Courtot Louis, Berard Emilie, Cavaignac Etienne. Feb 21;2019 The American Journal of Sports Medicine. 47(14):3531–3540. doi: 10.1177/0363546518825340. doi: 10.1177/0363546518825340. [DOI] [PubMed] [Google Scholar]
- Quadriceps tendon autograft versus bone-patellar tendon-bone and hamstring tendon autografts for anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Dai Wenli, Leng Xi, Wang Jian, Cheng Jin, Hu Xiaoqing, Ao Yingfang. Sep 8;2021 The American Journal of Sports Medicine. 50(12):3425–3439. doi: 10.1177/03635465211030259. doi: 10.1177/03635465211030259. [DOI] [PubMed] [Google Scholar]
- Quadricep ACL reconstruction techniques and outcomes: an updated ccoping review of the quadricep tendon. Cohen Dan, Slawaska-Eng David, Almasri Mahmoud, Sheean Andrew, de Sa Darren. Nov 10;2021 Current Reviews in Musculoskeletal Medicine. 14(6):462–474. doi: 10.1007/s12178-021-09726-3. doi: 10.1007/s12178-021-09726-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quadriceps tendon autograft for anterior cruciate ligament reconstruction is associated with high revision rates: results from the Danish Knee Ligament Registry. Lind Martin, Strauss Marc J., Nielsen Torsten, Engebretsen Lars. 2020Knee Surgery, Sports Traumatology, Arthroscopy. 28(7):2163–2169. doi: 10.1007/s00167-019-05751-5. doi: 10.1007/s00167-019-05751-5. [DOI] [PubMed] [Google Scholar]
- Low surgical routine increases revision rates after quadriceps tendon autograft for anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction Registry. Lind Martin, Strauss Marc J., Nielsen Torsten, Engebretsen Lars. 2021Knee Surgery, Sports Traumatology, Arthroscopy. 29(6):1880–1886. doi: 10.1007/s00167-020-06220-0. doi: 10.1007/s00167-020-06220-0. [DOI] [PubMed] [Google Scholar]
- Ollivier Matthieu, Jacquet Christophe, Pailhe Régis, Cognault Jérémy, Cavaignac Etienne, Seil Romain. Knee Surgery, Sports Traumatology, Arthroscopy. 11. Vol. 28. Springer Science and Business Media LLC; Higher re-rupture rate in quadriceps tendon ACL reconstruction surgeries performed in Denmark: let’s return to the mean; pp. 3655–3656. [DOI] [PubMed] [Google Scholar]
- Schmücker Malte, Haraszuk Jørgen, Hölmich Per, Barfod Kristoffer W. The American Journal of Sports Medicine. 8. Vol. 49. SAGE Publications; Graft failure, revision ACLR, and reoperation rates after ACLR with quadriceps tendon versus hamstring tendon autografts: a registry study with review of 475 patients; pp. 2136–2143. [DOI] [PubMed] [Google Scholar]
- Central quadriceps tendon for anterior cruciate ligament reconstruction. Part I: morphometric and biomechanical evaluation. Harris N. Lindsay, Smith David A. B., Lamoreaux Lisa, Purnell Mark. Jan;1997 The American Journal of Sports Medicine. 25(1):23–28. doi: 10.1177/036354659702500105. doi: 10.1177/036354659702500105. [DOI] [PubMed] [Google Scholar]
- Comparative analysis of the morphologic structure of quadriceps and patellar tendon: a descriptive laboratory study. Hadjicostas Panayiotis T., Soucacos Panayotis N., Berger Irina, Koleganova Nadezda, Paessler Hans H. Jul;2007 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 23(7):744–750. doi: 10.1016/j.arthro.2007.01.032. doi: 10.1016/j.arthro.2007.01.032. [DOI] [PubMed] [Google Scholar]
- Residual strength of the quadriceps versus patellar tendon after harvesting a central free tendon graft. Adams Douglas J., Mazzocca Augustus D., Fulkerson John P. Jan;2006 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 22(1):76–79. doi: 10.1016/j.arthro.2005.10.015. doi: 10.1016/j.arthro.2005.10.015. [DOI] [PubMed] [Google Scholar]
- Biomechanical comparison of quadriceps and patellar tendon grafts in anterior cruciate ligament reconstruction. Shani Raj H., Umpierez Erica, Nasert Michael, Hiza Elise A., Xerogeanes John. Jan;2016 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 32(1):71–75. doi: 10.1016/j.arthro.2015.06.051. doi: 10.1016/j.arthro.2015.06.051. [DOI] [PubMed] [Google Scholar]
- Current trends in the anterior cruciate ligament part II: evaluation, surgical technique, prevention, and rehabilitation. Musahl Volker, Engler Ian D., Nazzal Ehab M., Dalton Jonathan F., Lucidi Gian Andrea, Hughes Jonathan D., Zaffagnini Stefano, Della Villa Francesco, Irrgang James J., Fu Freddie H., Karlsson Jon. 2022Knee Surgery, Sports Traumatology, Arthroscopy. 30(1):34–51. doi: 10.1007/s00167-021-06825-z. doi: 10.1007/s00167-021-06825-z. [DOI] [PubMed] [Google Scholar]
- Waligora Andrew C., Johanson Norman A., Hirsch Bruce Elliot. Clinical Orthopaedics and Related Research®. 12. Vol. 467. Ovid Technologies (Wolters Kluwer Health); Clinical anatomy of the quadriceps femoris and extensor apparatus of the knee; pp. 3297–3306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New insight in the architecture of the quadriceps tendon. Grob Karl, Manestar Mirjana, Filgueira Luis, Ackland Timothy, Gilbey Helen, Kuster Markus S. Nov 3;2016 Journal of Experimental Orthopaedics. 3(1):32. doi: 10.1186/s40634-016-0068-y. doi: 10.1186/s40634-016-0068-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehran Nima, Damodar Dhanur, Shu Yang Justin. Journal of the American Academy of Orthopaedic Surgeons. 2. Vol. 28. Ovid Technologies (Wolters Kluwer Health); quadriceps tendon autograft in anterior cruciate ligament reconstruction; pp. 45–52. [DOI] [PubMed] [Google Scholar]
- Nebelung W., Becker R., Urbach D., Röpke M., Roessner A. Archives of Orthopaedic and Trauma Surgery. 4. Vol. 123. Springer Science and Business Media LLC; Histological findings of tendon-bone healing following anterior cruciate ligament reconstruction with hamstring grafts; pp. 158–163. [DOI] [PubMed] [Google Scholar]
- Comparison of three techniques of anterior cruciate ligament reconstruction with bone-patellar tendon-bone graft. Differences in anterior tibial translation and tunnel enlargement with each technique. Otsuka Hironori, Ishibashi Yasuyuki, Tsuda Eiichi, Sasaki Kazuhiro, Toh Satoshi. Mar;2003 The American Journal of Sports Medicine. 31(2):282–288. doi: 10.1177/03635465030310022101. doi: 10.1177/03635465030310022101. [DOI] [PubMed] [Google Scholar]
- Rodeo Scott A., Kawamura Sumito, Kim Hyon-Jeong, Dynybil Christian, Ying Liang. The American Journal of Sports Medicine. 11. Vol. 34. SAGE Publications; Tendon healing in a bone tunnel differs at the tunnel entrance versus the tunnel exit: an effect of graft-tunnel motion? pp. 1790–1800. [DOI] [PubMed] [Google Scholar]
- Bone-patellar tendon-bone versus hamstring tendon autografts for primary anterior cruciate ligament reconstruction: a systematic review of overlapping meta-analyses. Schuette Hayden B., Kraeutler Matthew J., Houck Darby A., McCarty Eric C. Nov;2017 Orthopaedic Journal of Sports Medicine. 5(11):2325967117736484. doi: 10.1177/2325967117736484. doi: 10.1177/2325967117736484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston Peta T., Feller Julian A., McClelland Jodie A., Webster Kate E. Knee Surgery, Sports Traumatology, Arthroscopy. 4. Vol. 30. Springer Science and Business Media LLC; Knee strength deficits following anterior cruciate ligament reconstruction differ between quadriceps and hamstring tendon autografts; pp. 1300–1310. [DOI] [PubMed] [Google Scholar]
- Knee muscle strength after quadriceps tendon autograft anterior cruciate ligament reconstruction: systematic review and meta-analysis. Johnston Peta T., McClelland Jodie A., Feller Julian A., Webster Kate E. 2021Knee Surgery, Sports Traumatology, Arthroscopy. 29(9):2918–2933. doi: 10.1007/s00167-020-06311-y. doi: 10.1007/s00167-020-06311-y. [DOI] [PubMed] [Google Scholar]
- Hamstring tendons or bone-patellar tendon-bone graft for anterior cruciate ligament reconstruction? Thaunat Mathieu, Fayard Jean Marie, Sonnery-Cottet Bertrand. Feb;2019 Orthopaedics & Traumatology: Surgery & Research. 105(1):S89–S94. doi: 10.1016/j.otsr.2018.05.014. doi: 10.1016/j.otsr.2018.05.014. [DOI] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction, hamstring versus bone–patella tendon–bone grafts: a systematic literature review of outcome from surgery. Herrington Lee, Wrapson Charlotte, Matthews Martyn, Matthews Helen. Jan;2005 The Knee. 12(1):41–50. doi: 10.1016/j.knee.2004.02.003. doi: 10.1016/j.knee.2004.02.003. [DOI] [PubMed] [Google Scholar]
- The outcome at 15 years of endoscopic anterior cruciate ligament reconstruction using hamstring tendon autograft for ‘isolated’ anterior cruciate ligament rupture. Bourke H. E., Gordon D. J., Salmon L. J., Waller A., Linklater J., Pinczewski L. A. May;2012 The Journal of Bone and Joint Surgery. British volume. 94-B(5):630–637. doi: 10.1302/0301-620x.94b5.28675. doi: 10.1302/0301-620x.94b5.28675. [DOI] [PubMed] [Google Scholar]
- Smith Angela Hutchinson, Capin Jacob J., Zarzycki Ryan, Snyder-Mackler Lynn. Journal of Orthopaedic & Sports Physical Therapy. 5. Vol. 50. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); Athletes with bone-patellar tendon-bone autograft for anterior cruciate ligament reconstruction were slower to meet rehabilitation milestones and return-to-sport criteria than athletes with hamstring tendon autograft or soft tissue allograft : secondary analysis from the ACL-SPORTS trial; pp. 259–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brinlee Alexander W., Dickenson Scott B., Hunter-Giordano Airelle, Snyder-Mackler Lynn. Sports Health: A Multidisciplinary Approach. 5. Vol. 14. SAGE Publications; ACL reconstruction rehabilitation: clinical data, biologic healing, and criterion-based milestones to inform a return-to-sport guideline; pp. 770–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Implications for early postoperative care after quadriceps tendon autograft for anterior cruciate ligament reconstruction: a technical note. Hunnicutt Jennifer L., Slone Harris S., Xerogeanes John W. May 12;2020 J Athl Train. 55(6):623–627. doi: 10.4085/1062-6050-172-19. doi: 10.4085/1062-6050-172-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quadriceps tendon anterior cruciate ligament reconstruction: A systematic review of postoperative rehabilitation and complication profiles. Zhang Kailai, Beshay Tony, Murphy Ben, Sheean Andrew, de SA Darren. 2021Arthroscopy: The Journal of Arthroscopic & Related Surgery. 38(6):2062–2072. doi: 10.1016/j.arthro.2021.12.020. doi: 10.1016/j.arthro.2021.12.020. [DOI] [PubMed] [Google Scholar]
- Woo Savio L-Y., Debski Richard E., Withrow John D., Janaushek Marsie A. The American Journal of Sports Medicine. 4. Vol. 27. SAGE Publications; Biomechanics of knee ligaments; pp. 533–543. [DOI] [PubMed] [Google Scholar]
- Mechanics of cadaveric anterior cruciate ligament reconstructions during simulated jump landing tasks: lessons learned from a pilot investigation. Schilaty Nathan D., Martin R. Kyle, Ueno Ryo, Rigamonti Luca, Bates Nathaniel A. Jun;2021 Clinical Biomechanics. 86:105372. doi: 10.1016/j.clinbiomech.2021.105372. doi: 10.1016/j.clinbiomech.2021.105372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Full thickness quadriceps tendon grafts with bone had similar material properties to bone-patellar tendon-bone and a four-strand semitendinosus grafts: a biomechanical study. Strauss Marc J., Miles Jon W., Kennedy Mitchell L., Dornan Grant J., Moatshe Gilbert, Lind Martin, Engebretsen Lars, LaPrade Robert F. 2022Knee Surgery, Sports Traumatology, Arthroscopy. 30(5):1786–1794. doi: 10.1007/s00167-021-06738-x. doi: 10.1007/s00167-021-06738-x. [DOI] [PubMed] [Google Scholar]
- Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. Hamner DYSON L., Brown CHARLES H., Steiner MARK E., Hecker AARON T., Hayes WILSON C. Apr;1999 The Journal of Bone & Joint Surgery. 81(4):549–57. doi: 10.2106/00004623-199904000-00013. doi: 10.2106/00004623-199904000-00013. [DOI] [PubMed] [Google Scholar]
- Stäubli Hans U., Schatzmann Lukas, Brunner Peter, Rincón Liliana, Nolte Lutz-P. The American Journal of Sports Medicine. 1. Vol. 27. SAGE Publications; Mechanical tensile properties of the quadriceps tendon and patellar ligament in young adults; pp. 27–34. [DOI] [PubMed] [Google Scholar]
- ACL graft failure location differs between allografts and autografts. Magnussen Robert A, Taylor Dean C, Toth Alison P, Garrett William E. Jun 14;2012 Sports Medicine, Arthroscopy, Rehabilitation, Therapy & Technology. 4(1):22. doi: 10.1186/1758-2555-4-22. doi: 10.1186/1758-2555-4-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regional variation of tibialis anterior tendon mechanics is lost following denervation. Arruda Ellen M., Calve Sarah, Dennis Robert G., Mundy Kevin, Baar Keith. Oct;2006 Journal of Applied Physiology. 101(4):1113–1117. doi: 10.1152/japplphysiol.00612.2005. doi: 10.1152/japplphysiol.00612.2005. [DOI] [PubMed] [Google Scholar]
- Thomopoulos Stavros, Birman Victor, Genin Guy M., editors. Structural interfaces and attachments in biology. Springer New York; [DOI] [Google Scholar]
- Biomechanical comparison of three suspensory techniques for all soft tissue central quadriceps tendon graft fixation. Arakgi Michelle E., Burkhart Timothy A., Hoshino Takashi, Degen Ryan, Getgood Alan. Jun;2022 Arthroscopy, Sports Medicine, and Rehabilitation. 4(3):e843–e851. doi: 10.1016/j.asmr.2021.12.008. doi: 10.1016/j.asmr.2021.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Augmentation of bone tunnel healing in anterior cruciate ligament grafts: application of calcium phosphates and other materials. Baxter F. R., Bach J. S., Detrez F., Cantournet S., Corté L., Cherkaoui M., Ku D. N. Jan;2010 Journal of Tissue Engineering. 1(1):712370. doi: 10.4061/2010/712370. doi: 10.4061/2010/712370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graft maturity of the reconstructed anterior cruciate ligament 6 months postoperatively: a magnetic resonance imaging evaluation of quadriceps tendon with bone block and hamstring tendon autografts. Ma Yong, Murawski Christopher D., Rahnemai-Azar Amir Ata, Maldjian Catherine, Lynch Andrew D., Fu Freddie H. 2015Knee Surgery, Sports Traumatology, Arthroscopy. 23(3):661–668. doi: 10.1007/s00167-014-3302-0. doi: 10.1007/s00167-014-3302-0. [DOI] [PubMed] [Google Scholar]
- Quadriceps tendon autograft for anterior cruciate ligament reconstruction: a comprehensive review of current literature and systematic review of clinical results. Slone Harris S., Romine Spencer E., Premkumar Ajay, Xerogeanes John W. Mar;2015 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 31(3):541–554. doi: 10.1016/j.arthro.2014.11.010. doi: 10.1016/j.arthro.2014.11.010. [DOI] [PubMed] [Google Scholar]
- Bone versus all soft tissue quadriceps tendon autografts for anterior cruciate ligament reconstruction: a systematic review. Crum Raphael J., Kay Jeffrey, Lesniak Bryson P., Getgood Alan, Musahl Volker, de SA Darren. Mar;2021 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 37(3):1040–1052. doi: 10.1016/j.arthro.2020.10.018. doi: 10.1016/j.arthro.2020.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh Harasees, Glassman Isaac, Sheean Andrew, Hoshino Yuichi, Nagai Kanto, de SA Darren. Knee Surgery, Sports Traumatology, Arthroscopy. 2. Vol. 31. Springer Science and Business Media LLC; Less than 1% risk of donor-site quadriceps tendon rupture post-ACL reconstruction with quadriceps tendon autograft: a systematic review; pp. 572–585. [DOI] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction utilizing central quadriceps free tendon. Theut Peter C, Fulkerson John P, Armour E.F, Joseph Michael. Jan;2003 Orthopedic Clinics of North America. 34(1):31–39. doi: 10.1016/s0030-5898(02)00068-8. doi: 10.1016/s0030-5898(02)00068-8. [DOI] [PubMed] [Google Scholar]
- Quadriceps Tendon—A reliable alternative for reconstruction of the anterior cruciate ligament. DeAngelis Joseph P., Fulkerson John P. Oct;2007 Clinics in Sports Medicine. 26(4):587–596. doi: 10.1016/j.csm.2007.06.005. doi: 10.1016/j.csm.2007.06.005. [DOI] [PubMed] [Google Scholar]
- Tendon healing in bone tunnel after human anterior cruciate ligament reconstruction: a systematic review of histological results. Lu Hongbin, Chen Can, Xie Shanshan, Tang Yifu, Qu Jin. 2019The Journal of Knee Surgery. 32(05):454–462. doi: 10.1055/s-0038-1653964. doi: 10.1055/s-0038-1653964. [DOI] [PubMed] [Google Scholar]
- Heijne Annette, Werner Suzanne. Knee Surgery, Sports Traumatology, Arthroscopy. 4. Vol. 15. Springer Science and Business Media LLC; Early versus late start of open kinetic chain quadriceps exercises after ACL reconstruction with patellar tendon or hamstring grafts: a prospective randomized outcome study; pp. 472–473. [DOI] [PubMed] [Google Scholar]
- Patients with a quadriceps tendon shorter than 60 mm require a patellar bone plug autograft in anterior cruciate ligament reconstruction. Yamasaki Shinya, Hashimoto Yusuke, Han Changhun, Nishino Kazuya, Hidaka Noriaki, Nakamura Hiroaki. 2021Knee Surgery, Sports Traumatology, Arthroscopy. 29(6):1927–1935. doi: 10.1007/s00167-020-06261-5. doi: 10.1007/s00167-020-06261-5. [DOI] [PubMed] [Google Scholar]
- Yuksel Yavuz, Kose Ozkan, Torun Ebru, Ergun Tarkan, Yardibi Fatma, Sarikcioglu Levent. Archives of Orthopaedic and Trauma Surgery. 8. Vol. 142. Springer Science and Business Media LLC; Estimating the adequacy of the free quadriceps tendon autograft length using anthropometric measures in anterior cruciate ligament reconstruction; pp. 2001–2010. [DOI] [PubMed] [Google Scholar]
- Comparison of single- and double-bundle anterior cruciate ligament reconstruction using quadriceps tendon–bone autografts. Kim Sung-Jae, Jo Seung-Bae, Kumar Praveen, Oh Kyung-Soo. Jan;2009 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 25(1):70–77. doi: 10.1016/j.arthro.2008.09.004. doi: 10.1016/j.arthro.2008.09.004. [DOI] [PubMed] [Google Scholar]
- No difference between full thickness and partial thickness quadriceps tendon autografts in anterior cruciate ligament reconstruction: a systematic review. Kanakamedala Ajay C., de Sa Darren, Obioha Obianuju A., Arakgi Michelle E., Schmidt Patrick B., Lesniak Bryson P., Musahl Volker. 2019Knee Surgery, Sports Traumatology, Arthroscopy. 27(1):105–116. doi: 10.1007/s00167-018-5042-z. doi: 10.1007/s00167-018-5042-z. [DOI] [PubMed] [Google Scholar]
- Farahmand Farzam, Sejiavongse Wongwit, Amis Andrew A. Journal of Orthopaedic Research. 1. Vol. 16. Wiley; Quantitative study of the quadriceps muscles and trochlear groove geometry related to instability of the patellofemoral joint; pp. 136–143. [DOI] [PubMed] [Google Scholar]
- Risk Factors for manipulation under anesthesia and/or lysis of adhesions after anterior cruciate ligament reconstruction. Huleatt Joel, Gottschalk Michael, Fraser Kelsey, Boden Allison, Dalwadi Poonam, Xerogeanes John, Hammond Kyle. Sep;2018 Orthopaedic Journal of Sports Medicine. 6(9):2325967118794490. doi: 10.1177/2325967118794490. doi: 10.1177/2325967118794490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perioperative complications and early clinical outcomes following ACL reconstruction with soft tissue quadriceps tendon autograft in adolescent athletes. Jasty Naveen, Cook Danielle, Liotta Elizabeth, Hayworth Benton. Jul 1;2021 Orthopaedic Journal of Sports Medicine. 9(7) doi: 10.1177/2325967121s00223. doi: 10.1177/2325967121s00223. [DOI] [Google Scholar]
- Localized anterior arthrofibrosis after soft-tissue quadriceps tendon anterior cruciate ligament reconstruction is more common in patients who are female, undergo meniscal repair, and have grafts of larger diameter. Haley Rebecca M., Lamplot Joseph D., Myer Gregory D., Diekfuss Jed A., Reed Joan, Hash Regina, Simon Janet E., Xerogeanes John W. Dec;2022 Arthroscopy: The Journal of Arthroscopic & Related Surgery. doi: 10.1016/j.arthro.2022.11.027. doi: 10.1016/j.arthro.2022.11.027. [DOI] [PubMed]
- Quadriceps strength following anterior cruciate ligament reconstruction: normative values based on sex, graft type and meniscal status at 3, 6 & 9 months. Schwery Nicole A., Kiely Michael T., Larson Christopher M., Wulf Corey A., Heikes Christie S., Hess Ryan W., Giveans M. Russell, Solie Braidy S., Doney Chrisopher P. Apr 1;2022 Int J Sports Phys Ther. 17(3) doi: 10.26603/001c.32378. doi: 10.26603/001c.32378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction: quadriceps versus patellar autograft. Han Hyuk Soo, Seong Sang Cheol, Lee Sahnghoon, Lee Myung Chul. Jan;2008 Clin Orthop Relat Res. 466(1):198–204. doi: 10.1007/s11999-007-0015-4. doi: 10.1007/s11999-007-0015-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bone-patellar tendon–bone autograft maturation is superior to double-bundle hamstring tendon autograft maturation following anatomical anterior cruciate ligament reconstruction. Fukuda Hideaki, Ogura Takahiro, Asai Shigehiro, Omodani Toru, Takahashi Tatsuya, Yamaura Ichiro, Sakai Hiroki, Saito Chikara, Tsuchiya Akihiro, Takahashi Kenji. 2022Knee Surgery, Sports Traumatology, Arthroscopy. 30(5):1661–1671. doi: 10.1007/s00167-021-06653-1. doi: 10.1007/s00167-021-06653-1. [DOI] [PubMed] [Google Scholar]
- Graft maturity of the reconstructed anterior cruciate ligament 6 months postoperatively: a magnetic resonance imaging evaluation of quadriceps tendon with bone block and hamstring tendon autografts. Ma Yong, Murawski Christopher D., Rahnemai-Azar Amir Ata, Maldjian Catherine, Lynch Andrew D., Fu Freddie H. 2015Knee Surgery, Sports Traumatology, Arthroscopy. 23(3):661–668. doi: 10.1007/s00167-014-3302-0. doi: 10.1007/s00167-014-3302-0. [DOI] [PubMed] [Google Scholar]
- Mechanisms of anterior cruciate ligament neovascularization and ligamentization. Scranton P E, Jr., Lanzer W L, Ferguson M S, Kirkman T R, Pflaster D S. Oct;1998 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 14(7):702–716. doi: 10.1016/s0749-8063(98)70097-0. doi: 10.1016/s0749-8063(98)70097-0. [DOI] [PubMed] [Google Scholar]
- Soft tissue fixation strategies of human quadriceps tendon grafts: a biomechanical study. Michel Philipp A., Domnick Christoph, Raschke Michael J., Kittl Christoph, Glasbrenner Johannes, Deitermann Lucas, Fink Christian, Herbort Mirco. Nov;2019 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 35(11):3069–3076. doi: 10.1016/j.arthro.2019.05.025. doi: 10.1016/j.arthro.2019.05.025. [DOI] [PubMed] [Google Scholar]
- Minimum 10-year results after anterior cruciate ligament reconstruction: how the loss of normal knee motion compounds other factors related to the development of osteoarthritis after surgery. Shelbourne K.Donald, Gray Tinker. 2009The American Journal of Sports Medicine. 37(3):471–480. doi: 10.1177/0363546508326709. doi: 10.1177/0363546508326709. [DOI] [PubMed] [Google Scholar]
- Association between neuromuscular variables and graft harvest in soft tissue quadriceps tendon versus bone-patellar tendon-bone anterior cruciate ligament autografts. Letter Michael, Beauperthuy Andrew, Parrino Rosalia L., Posner Kevin, Baraga Michael G., Best Thomas M., Kaplan Lee D., Eltoukhy Moataz, Strand Keri L., Buskard Andrew, Signorile Joseph F. Oct 1;2021 Orthopaedic Journal of Sports Medicine. 9(10) doi: 10.1177/23259671211041591. doi: 10.1177/23259671211041591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short-term isokinetic and isometric strength outcomes after anterior cruciate ligament reconstruction in adolescents. Weaver Adam, Ness Brandon M., Roman Dylan P., Giampetruzzi Nicholas, Cleland Joshua A., Pace J. Lee, Crepeau Allison E. Jan;2022 Physical Therapy in Sport. 53:75–83. doi: 10.1016/j.ptsp.2021.11.009. doi: 10.1016/j.ptsp.2021.11.009. [DOI] [PubMed] [Google Scholar]
- Effect of early implementation of electrical muscle stimulation to prevent muscle atrophy and weakness in patients after anterior cruciate ligament reconstruction. Hasegawa Satoshi, Kobayashi Masahiko, Arai Ryuzo, Tamaki Akira, Nakamura Takashi, Moritani Toshio. Aug;2011 Journal of Electromyography and Kinesiology. 21(4):622–630. doi: 10.1016/j.jelekin.2011.01.005. doi: 10.1016/j.jelekin.2011.01.005. [DOI] [PubMed] [Google Scholar]
- Selective fatigue of fast motor units after electrically elicited muscle contractions. Hamada Taku, Kimura Tetsuya, Moritani Toshio. Oct;2004 Journal of Electromyography and Kinesiology. 14(5):531–538. doi: 10.1016/j.jelekin.2004.03.008. doi: 10.1016/j.jelekin.2004.03.008. [DOI] [PubMed] [Google Scholar]
- The effect of neuromuscular electrical stimulation in association with whey protein supplementation after anterior cruciate ligament reconstruction. Mendonça GABRIELA OTÍLIA, Severino MARIA LUIZA BIANCHINI, Oliveira KELLE MOREIRA de, OLIVEIRA MARCELO LIMA DE, SOUZA GIOVANE GALDINO DE, SIMÃO ADRIANO PRADO, LOBATO DANIEL FERREIRA MOREIRA, ANDRADE RANIELLY ALVES, FRANCO RICARDO ZENUN, CRUZ MARCELO STEGMANN DA, CARVALHO LEONARDO CÉSAR. Dec;2021 Acta Ortopédica Brasileira. 29(6):316–322. doi: 10.1590/1413-785220212906237983. doi: 10.1590/1413-785220212906237983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- A systematic review of the effects of blood flow restriction training on quadriceps muscle atrophy and circumference post ACL reconstruction. Charles Derek, White Ryan, Reyes Caleb, Palmer Drew. Dec;2020 International Journal of Sports Physical Therapy. 15(6):882–891. doi: 10.26603/ijspt20200882. doi: 10.26603/ijspt20200882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuromuscular electrical stimulation is effective in strengthening the quadriceps muscle after anterior cruciate ligament surgery. Hauger Annette V., Reiman M. P., Bjordal J. M., Sheets C., Ledbetter L., Goode A. P. 2018Knee Surgery, Sports Traumatology, Arthroscopy. 26(2):399–410. doi: 10.1007/s00167-017-4669-5. doi: 10.1007/s00167-017-4669-5. [DOI] [PubMed] [Google Scholar]
- Blood flow restriction training in rehabilitation following anterior cruciate ligament reconstructive surgery: a review. Hughes Luke, Rosenblatt Ben, Paton Bruce, Patterson Stephen David. Jun;2018 Techn Orthop. 33(2):106–113. doi: 10.1097/bto.0000000000000265. doi: 10.1097/bto.0000000000000265. [DOI] [Google Scholar]
- Kilgas Matthew A., Lytle Lydia L.M., Drum Scott N., Elmer Steven J. International Journal of Sports Medicine. 10. Vol. 40. Georg Thieme Verlag KG; Exercise with blood flow restriction to improve quadriceps function long after ACL reconstruction; pp. 650–656. [DOI] [PubMed] [Google Scholar]
- Anterior cruciate ligament strain and tensile forces for weight-bearing and non-weight-bearing exercises: a guide to exercise selection. Escamilla Rafael F., Macleod Toran D., Wilk Kevin E., Paulos Lonnie, Andrews James R. Mar;2012 Journal of Orthopaedic & Sports Physical Therapy. 42(3):208–220. doi: 10.2519/jospt.2012.3768. doi: 10.2519/jospt.2012.3768. [DOI] [PubMed] [Google Scholar]
- Loaded open-kinetic-chain exercises stretch the anterior cruciate ligament more than closed-kinetic-chain exercises: In-vivo assessment of anterior cruciate ligament length change. Wang Cong, Qiu Jiayu, Wang Yufan, Li Changzhao, Kernkamp Willem A., Xi Xin, Yu Yan, Li Pingyue, Tsai Tsung-Yuan. Feb;2023 Musculoskeletal Science and Practice. 63:102715. doi: 10.1016/j.msksp.2022.102715. doi: 10.1016/j.msksp.2022.102715. [DOI] [PubMed] [Google Scholar]
- Anterior cruciate ligament strain in-vivo: A review of previous work. Beynnon Bruce D, Fleming Braden C. Jun;1998 Journal of Biomechanics. 31(6):519–525. doi: 10.1016/s0021-9290(98)00044-x. doi: 10.1016/s0021-9290(98)00044-x. [DOI] [PubMed] [Google Scholar]
- Tendon healing in bone tunnel after human anterior cruciate ligament reconstruction: A systematic review of histological results. Lu Hongbin, Chen Can, Xie Shanshan, Tang Yifu, Qu Jin. 2019The Journal of Knee Surgery. 32(05):454–462. doi: 10.1055/s-0038-1653964. doi: 10.1055/s-0038-1653964. [DOI] [PubMed] [Google Scholar]
- Perriman Alyssa, Leahy Edmund, Semciw Adam Ivan. Journal of Orthopaedic & Sports Physical Therapy. 7. Vol. 48. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); The effect of open- versus closed-kinetic-chain exercises on anterior tibial laxity, strength, and function following anterior cruciate ligament reconstruction: a systematic review and meta-analysis; pp. 552–566. [DOI] [PubMed] [Google Scholar]
- RSA can measure ACL graft stretching and migration. Khan Rashid, Konyves Arpad, Rama K R. Boddu Siva, Thomas Rhidian, Amis Andrew A. Jul;2006 Clinical Orthopaedics and Related Research. 448:139–145. doi: 10.1097/01.blo.0000224016.42669.17. doi: 10.1097/01.blo.0000224016.42669.17. [DOI] [PubMed] [Google Scholar]
- Isometry testing for anterior cruciate ligament reconstruction revisited. Morgan Craig D., Kalmam Victor R., Grawl Daniel M. Dec;1995 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 11(6):647–659. doi: 10.1016/0749-8063(95)90104-3. doi: 10.1016/0749-8063(95)90104-3. [DOI] [PubMed] [Google Scholar]
- The effect of anterior cruciate ligament graft fixation site at the tibia on knee stability: evaluation using a robotic testing system. Ishibashi Yasuyuki, Rudy Theodore W., Livesay Glen A., Stone Jeffrey D., Fu Freddie H., Woo Savio L.-Y. Apr;1997 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 13(2):177–182. doi: 10.1016/s0749-8063(97)90152-3. doi: 10.1016/s0749-8063(97)90152-3. [DOI] [PubMed] [Google Scholar]
- Brand Jeff, Weiler Andreas, Caborn David N. M., Brown Charles H., Johnson Darren L. The American Journal of Sports Medicine. 5. Vol. 28. SAGE Publications; Graft fixation in cruciate ligament reconstruction; pp. 761–774. [DOI] [PubMed] [Google Scholar]
- Anatomy and biomechanics of the native and reconstructed anterior cruciate ligament: surgical implications. Kraeutler Matthew J., Wolsky Ryan M., Vidal Armando F., Bravman Jonathan T. Mar 1;2017 Journal of Bone and Joint Surgery. 99(5):438–445. doi: 10.2106/jbjs.16.00754. doi: 10.2106/jbjs.16.00754. [DOI] [PubMed] [Google Scholar]
- Multiplane loading of the extensor mechanism alters the patellar ligament force/quadriceps force ratio. Powers Christopher M., Chen Yu-Jen, Scher Irving S., Lee Thay Q. Jan 29;2010 J Biomech Eng. 132(2) doi: 10.1115/1.4000852. doi: 10.1115/1.4000852. [DOI] [PubMed] [Google Scholar]
- Sprague Andrew, Epsley Scott, Silbernagel Karin Grävare. Journal of Orthopaedic & Sports Physical Therapy. 9. Vol. 49. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); Distinguishing quadriceps tendinopathy and patellar tendinopathy: semantics or significant? pp. 627–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Three-dimensional modelling of human quadriceps femoris forces. Chiu Loren Z.F., Daehlin Torstein E. May;2021 Journal of Biomechanics. 120:110347. doi: 10.1016/j.jbiomech.2021.110347. doi: 10.1016/j.jbiomech.2021.110347. [DOI] [PubMed] [Google Scholar]
- Stiffness of individual quadriceps muscle assessed using ultrasound shear wave elastography during passive stretching. Xu Jingfei, Hug François, Fu Siu Ngor. Apr;2018 Journal of Sport and Health Science. 7(2):245–249. doi: 10.1016/j.jshs.2016.07.001. doi: 10.1016/j.jshs.2016.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Localization of muscle damage within the quadriceps femoris induced by different types of eccentric exercises. Maeo S., Saito A., Otsuka S., Shan X., Kanehisa H., Kawakami Y. 2018Scandinavian Journal of Medicine & Science in Sports. 28(1):95–106. doi: 10.1111/sms.12880. doi: 10.1111/sms.12880. [DOI] [PubMed] [Google Scholar]
- Isometric contractions are more analgesic than isotonic contractions for patellar tendon pain. Rio Ebonie, van Ark Mathijs, Docking Sean, Moseley G. Lorimer, Kidgell Dawson, Gaida Jamie E., van den Akker-Scheek Inge, Zwerver Johannes, Cook Jill. May;2017 Clin J Sport Med. 27(3):253–259. doi: 10.1097/jsm.0000000000000364. doi: 10.1097/jsm.0000000000000364. [DOI] [PubMed] [Google Scholar]
- Enocson A.G., Berg H.E., Vargas R., Jenner G., Tesch P.A. European Journal of Applied Physiology. 4. Vol. 94. Springer Science and Business Media LLC; Signal intensity of MR-images of thigh muscles following acute open- and closed chain kinetic knee extensor exercise – index of muscle use; pp. 357–363. [DOI] [PubMed] [Google Scholar]
- Biomechanical considerations for rehabilitation of the knee. McGinty Gerald, Irrgang James J, Pezzullo Dave. Mar;2000 Clinical Biomechanics. 15(3):160–166. doi: 10.1016/s0268-0033(99)00061-3. doi: 10.1016/s0268-0033(99)00061-3. [DOI] [PubMed] [Google Scholar]
- The effects of frontal- and sagittal-plane plyometrics on change-of-direction speed and power in adolescent female basketball players. McCormick Brian T., Hannon James C., Newton Maria, Shultz Barry, Detling Nicole, Young Warren B. Jan;2016 Int J Sports Physiol Perform. 11(1):102–107. doi: 10.1123/ijspp.2015-0058. doi: 10.1123/ijspp.2015-0058. [DOI] [PubMed] [Google Scholar]
- Lower-limb joint mechanics during maximum acceleration sprinting. Schache Anthony G., Lai Adrian K. M., Brown Nicholas A. T., Crossley Kay M., Pandy Marcus G. Jan 1;2019 J Exp Biol. 1 doi: 10.1242/jeb.209460. doi: 10.1242/jeb.209460. [DOI] [PubMed] [Google Scholar]
- Effect of running speed on lower limb joint kinetics. Schache ANTHONY G., Blanch PETER D., Dorn TIM W., Brown NICHOLAS A. T., Rosemond DOUG, Pandy MARCUS G. Jul;2011 Med Sci Sports Exerc. 43(7):1260–1271. doi: 10.1249/mss.0b013e3182084929. doi: 10.1249/mss.0b013e3182084929. [DOI] [PubMed] [Google Scholar]
- Rectus femoris muscle injuries in football: a clinically relevant review of mechanisms of injury, risk factors and preventive strategies. Mendiguchia Jurdan, Alentorn-Geli Eduard, Idoate Fernando, Myer Gregory D. 2013British Journal of Sports Medicine. 47(6):359–366. doi: 10.1136/bjsports-2012-091250. doi: 10.1136/bjsports-2012-091250. [DOI] [PubMed] [Google Scholar]
- Webster Kate E., Feller Julian A. The American Journal of Sports Medicine. 3. Vol. 47. SAGE Publications; Expectations for return to preinjury sport before and after anterior cruciate ligament reconstruction; pp. 578–583. [DOI] [PubMed] [Google Scholar]
- Ardern Clare L, Taylor Nicholas F, Feller Julian A, Webster Kate E. British Journal of Sports Medicine. 21. Vol. 48. BMJ; Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors; pp. 1543–1552. [DOI] [PubMed] [Google Scholar]
- Webster Kate E., Feller Julian A., Leigh Warren B., Richmond Anneka K. The American Journal of Sports Medicine. 3. Vol. 42. SAGE Publications; Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction; pp. 641–647. [DOI] [PubMed] [Google Scholar]
- Webster Kate E., Feller Julian A. The American Journal of Sports Medicine. 11. Vol. 44. SAGE Publications; Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction; pp. 2827–2832. [DOI] [PubMed] [Google Scholar]
- Paterno Mark V., Rauh Mitchell J., Schmitt Laura C., Ford Kevin R., Hewett Timothy E. The American Journal of Sports Medicine. 7. Vol. 42. SAGE Publications; Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport; pp. 1567–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grindem Hege, Snyder-Mackler Lynn, Moksnes Håvard, Engebretsen Lars, Risberg May Arna. British Journal of Sports Medicine. 13. Vol. 50. BMJ; Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study; pp. 804–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehabilitation and return to sport testing after anterior cruciate ligament reconstruction: where are we in 2022? Gokeler Alli, Dingenen Bart, Hewett Timothy E. Jan;2022 Arthroscopy, Sports Medicine, and Rehabilitation. 4(1):e77–e82. doi: 10.1016/j.asmr.2021.10.025. doi: 10.1016/j.asmr.2021.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Is there an association in young patients between quadriceps or hamstring strength after ACL reconstruction and graft rupture? Blucher Nicola C., Feller Julian A., Devitt Brian M., Klemm Haydn J., Whitehead Timothy S., McClelland Jodie A., Webster Kate E. Jun 1;2022 Orthopaedic Journal of Sports Medicine. 10(6):232596712211010. doi: 10.1177/23259671221101003. doi: 10.1177/23259671221101003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Predicting anterior cruciate ligament reinjury from return-to-activity assessments at 6 months postsurgery: a prospective cohort study. Bodkin Stephan G., Hertel Jay, Diduch David R., Saliba Susan A., Novicoff Wendy M., Brockmeier Stephen F., Miller Mark D., Gwathmey F. Winston, Werner Brian C., Hart Joseph M. 2022J Athl Train. 57(4):325–333. doi: 10.4085/1062-6050-0407.20. doi: 10.4085/1062-6050-0407.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Are 6-month functional and isokinetic testing measures risk factors for second anterior cruciate ligament injuries at long term follow-up? Marigi Erick M., Hale Rena F., Bernard Christopher D., Bates Nathaniel, Stuart Michael J., Hewett Timothy E., Krych Aaron J. Jun 10;2022 The Journal of Knee Surgery. 10:2022. doi: 10.1055/s-0042-1748824. doi: 10.1055/s-0042-1748824. [DOI] [PubMed] [Google Scholar]
- King Enda, Richter Chris, Daniels Katherine A.J., Franklyn-Miller Andy, Falvey Eanna, Myer Gregory D., Jackson Mark, Moran Ray, Strike Siobhan. The American Journal of Sports Medicine. 4. Vol. 49. SAGE Publications; Biomechanical but not strength or performance measures differentiate male athletes who experience ACL reinjury on return to Level 1 sports; pp. 918–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Return to sport: Does excellent 6-month strength and function following ACL reconstruction predict midterm outcomes? Sousa Paul L., Krych Aaron J., Cates Robert A., Levy Bruce A., Stuart Michael J., Dahm Diane L. 2017Knee Surgery, Sports Traumatology, Arthroscopy. 25(5):1356–1363. doi: 10.1007/s00167-015-3697-2. doi: 10.1007/s00167-015-3697-2. [DOI] [PubMed] [Google Scholar]
- Young athletes after ACL reconstruction with quadriceps strength asymmetry at the time of return-to-sport demonstrate decreased knee function 1 year later. Ithurburn Matthew P., Altenburger Alex R., Thomas Staci, Hewett Timothy E., Paterno Mark V., Schmitt Laura C. 2018Knee Surgery, Sports Traumatology, Arthroscopy. 26(2):426–433. doi: 10.1007/s00167-017-4678-4. doi: 10.1007/s00167-017-4678-4. [DOI] [PubMed] [Google Scholar]
- Age, gender, quadriceps strength and hop test performance are the most important factors affecting the achievement of a patient-acceptable symptom state after ACL reconstruction. Cristiani Riccardo, Mikkelsen Christina, Edman Gunnar, Forssblad Magnus, Engström Björn, Stålman Anders. 2020Knee Surgery, Sports Traumatology, Arthroscopy. 28(2):369–380. doi: 10.1007/s00167-019-05576-2. doi: 10.1007/s00167-019-05576-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Symmetries in muscle torque and landing kinematics are associated with maintenance of sports participation at 5 to 10 years after ACL reconstruction in young men. Hetsroni Iftach, Wiener Yohay, Ben-Sira David, Iacono Antonio Dello, Marom Niv, van Stee Mischa, Ayalon Moshe. Jun 1;2020 Orthopaedic Journal of Sports Medicine. 8(6) doi: 10.1177/2325967120923267. doi: 10.1177/2325967120923267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- A minority of athletes pass symmetry criteria in a series of hop and strength tests irrespective of having an ACL reconstructed knee or being noninjured. Markström Jonas L., Naili Josefine E., Häger Charlotte K. Jun 27;2022 Sports Health: A Multidisciplinary Approach. 15(1):45–51. doi: 10.1177/19417381221097949. doi: 10.1177/19417381221097949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster Kate E., Hewett Timothy E. Sports Medicine. 6. Vol. 49. Springer Science and Business Media LLC; What is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? a systematic review and meta-analysis; pp. 917–929. [DOI] [PubMed] [Google Scholar]
- Kaplan Yonatan, Witvrouw Erik. Sports Health: A Multidisciplinary Approach. 4. Vol. 11. SAGE Publications; When is it safe to return to sport after ACL reconstruction? reviewing the criteria; pp. 301–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Characteristics of complex systems in sports injury rehabilitation: examples and implications for practice. Yung Kate K., Ardern Clare L., Serpiello Fabio R., Robertson Sam. Feb 22;2022 Sports Medicine - Open. 8(1):24. doi: 10.1186/s40798-021-00405-8. doi: 10.1186/s40798-021-00405-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dingenen Bart, Gokeler Alli. Sports Medicine. 8. Vol. 47. Springer Science and Business Media LLC; Optimization of the return-to-sport paradigm after anterior cruciate ligament reconstruction: A critical step back to move forward; pp. 1487–1500. [DOI] [PubMed] [Google Scholar]
- Shrier Ian. British Journal of Sports Medicine. 20. Vol. 49. BMJ; Strategic assessment of risk and risk tolerance (StARRT) framework for return-to-play decision-making; pp. 1311–1315. [DOI] [PubMed] [Google Scholar]
- Shrier Ian. Return to Sport after ACL Reconstruction and Other Knee Operations. Springer International Publishing; return to sport decision-based models; pp. 53–65. [DOI] [Google Scholar]
- return-to-play in sport: a decision-based model. Creighton David W, Shrier Ian, Shultz Rebecca, Meeuwisse Willem H, Matheson Gordon O. Sep;2010 Clin J Sport Med. 20(5):379–385. doi: 10.1097/jsm.0b013e3181f3c0fe. doi: 10.1097/jsm.0b013e3181f3c0fe. [DOI] [PubMed] [Google Scholar]
- A framework for clinicians to improve the decision-making process in return to sport. Yung Kate K., Ardern Clare L., Serpiello Fabio R., Robertson Sam. Apr 13;2022 Sports Medicine - Open. 8(1):52. doi: 10.1186/s40798-022-00440-z. doi: 10.1186/s40798-022-00440-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- How much time is needed between serial “return to play” assessments to achieve clinically important strength gains in patients recovering from anterior cruciate ligament reconstruction? Bodkin Stephan G., Rutherford Margaret H., Diduch David R., Brockmeier Stephen F., Hart Joe M. 2020The American Journal of Sports Medicine. 48(1):70–77. doi: 10.1177/0363546519886291. doi: 10.1177/0363546519886291. [DOI] [PubMed] [Google Scholar]
- Patient function in serial assessments throughout the post-ACL reconstruction progression. Bodkin S.G., Hertel J., Bruce A.S., Diduch D.R., Saliba S.A., Novicoff W.M., Hart J.M. Jan;2021 Physical Therapy in Sport. 47:85–90. doi: 10.1016/j.ptsp.2020.11.025. doi: 10.1016/j.ptsp.2020.11.025. [DOI] [PubMed] [Google Scholar]
- Return to sport after anterior cruciate ligament injury: panther symposium ACL injury return to sport consensus group. Meredith Sean J., Rauer Thomas, Chmielewski Terese L., Fink Christian, Diermeier Theresa, Rothrauff Benjamin B., Svantesson Eleonor, Hamrin Senorski Eric, Hewett Timothy E., Sherman Seth L., Lesniak Bryson P., Bizzini Mario, Chen Shiyi, Cohen Moises, Villa Stefano Della, Engebretsen Lars, Feng Hua, Ferretti Mario, Fu Freddie H., Imhoff Andreas B., Kaeding Christopher C., Karlsson Jon, Kuroda Ryosuke, Lynch Andrew D., Menetrey Jacques, Musahl Volker, Navarro Ronald A., Rabuck Stephen J., Siebold Rainer, Snyder-Mackler Lynn, Spalding Tim, van Eck Carola, Vyas Dharmesh, Webster Kate, Wilk Kevin, the Panther Symposium ACL Injury Return to Sport Consensus Group Jun 1;2020 Orthopaedic Journal of Sports Medicine. 8(6):232596712093082. doi: 10.1177/2325967120930829. doi: 10.1177/2325967120930829. [DOI] [PubMed] [Google Scholar]
- Return to elite-level basketball after surgical reconstruction of the anterior cruciate ligament and medial collateral ligament of the knee with meniscal repairs– it takes teamwork and time to restore performance: a case report. Solie B., Kiely M., Doney C., Schwery N., Jones J., Bjerke B. 2022J Orthop Sports Phys Ther Cases. 2(4):1–22. [Google Scholar]
- Beischer Susanne, Gustavsson Linnéa, Senorski Eric Hamrin, Karlsson Jón, Thomeé Christoffer, Samuelsson Kristian, Thomeé Roland. Journal of Orthopaedic & Sports Physical Therapy. 2. Vol. 50. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); Young athletes who return to sport before 9 months after anterior cruciate ligament reconstruction have a rate of new injury 7 times that of those who delay return; pp. 83–90. [DOI] [PubMed] [Google Scholar]
- Martin R. Kyle, Wastvedt Solvejg, Pareek Ayoosh, Persson Andreas, Visnes Håvard, Fenstad Anne Marie, Moatshe Gilbert, Wolfson Julian, Lind Martin, Engebretsen Lars. Knee Surgery, Sports Traumatology, Arthroscopy. 2. Vol. 30. Springer Science and Business Media LLC; Machine learning algorithm to predict anterior cruciate ligament revision demonstrates external validity; pp. 368–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmura Hana, Getgood Alan M.J., Spindler Kurt P., Kattan Michael W., Briskin Isaac, Bryant Dianne M. The American Journal of Sports Medicine. 7. Vol. 49. SAGE Publications; Validation of a risk calculator to personalize graft choice and reduce rupture rates for anterior cruciate ligament reconstruction; pp. 1777–1785. [DOI] [PubMed] [Google Scholar]
- The muscle strength of the knee joint after ACL reconstruction depends on the number and frequency of supervised physiotherapy visits. Czamara Andrzej, Krzemińska Katarzyna, Widuchowski Wojciech, Dragan Szymon Lukasz. Oct 9;2021 International Journal of Environmental Research and Public Health. 18(20):10588. doi: 10.3390/ijerph182010588. doi: 10.3390/ijerph182010588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franck Florent, Saithna Adnan, Vieira Thais Dutra, Pioger Charles, Vigne Gregory, Le Guen Meven, Rogowski Isabelle, Fayard Jean-Marie, Thaunat Mathieu, Sonnery-Cottet Bertrand. Sports Health: A Multidisciplinary Approach. 4. Vol. 13. SAGE Publications; Return to sport composite test after anterior cruciate ligament reconstruction (K-STARTS): factors affecting return to sport test score in a retrospective analysis of 676 patients; pp. 364–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patient characteristics and predictors of return to sport at 12 months after anterior cruciate ligament reconstruction: the importance of patient age and postoperative rehabilitation. Edwards Peter K., Ebert Jay R., Joss Brendan, Ackland Timothy, Annear Peter, Buelow Jens-Ulrich, Hewitt Ben. Sep;2018 Orthopaedic Journal of Sports Medicine. 6(9):232596711879757. doi: 10.1177/2325967118797575. doi: 10.1177/2325967118797575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson Jessica L., Capin Jacob J., Arundale Amelia J.H., Zarzycki Ryan, Smith Angela H., Snyder-Mackler Lynn. Journal of Orthopaedic & Sports Physical Therapy. 9. Vol. 50. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); A secondary injury prevention program may decrease contralateral anterior cruciate ligament injuries in female athletes: 2-year injury rates in the ACL-SPORTS randomized controlled trial; pp. 523–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Two year ACL reinjury rate of 2.5%: outcomes report of the men in a secondary ACL injury prevention program (ACL-SPORTS) Arundale Amelia J.H., Capin Jacob J., Zarzycki Ryan, Smith Angela H., Snyder-Mackler Lynn. Jun;2018 International Journal of Sports Physical Therapy. 13(3):422–431. doi: 10.26603/ijspt20180422. doi: 10.26603/ijspt20180422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckthorpe Matthew. Sports Medicine. 7. Vol. 49. Springer Science and Business Media LLC; Optimising the late-stage rehabilitation and return-to-sport training and testing process after ACL reconstruction; pp. 1043–1058. [DOI] [PubMed] [Google Scholar]
- Taberner Matt, Allen Tom, Cohen Daniel Dylan. British Journal of Sports Medicine. 18. Vol. 53. BMJ; Progressing rehabilitation after injury: consider the ‘control-chaos continuum’; pp. 1132–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahr Roald. British Journal of Sports Medicine. 13. Vol. 50. BMJ; Why screening tests to predict injury do not work—and probably never will…: a critical review; pp. 776–780. [DOI] [PubMed] [Google Scholar]
- Do exercises used in injury prevention programmes modify cutting task biomechanics? A systematic review with meta-analysis. Pappas Evangelos, Nightingale Elizabeth J, Simic Milena, Ford Kevin R, Hewett Timothy E, Myer Gregory D. 2015British Journal of Sports Medicine. 49(10):673–680. doi: 10.1136/bjsports-2014-093796. doi: 10.1136/bjsports-2014-093796. [DOI] [PubMed] [Google Scholar]
- The effects of injury prevention programs on the biomechanics of landing tasks: a systematic review with meta-analysis. Lopes Thiago Jambo Alves, Simic Milena, Myer Gregory D., Ford Kevin R., Hewett Timothy E., Pappas Evangelos. 2018The American Journal of Sports Medicine. 46(6):1492–1499. doi: 10.1177/0363546517716930. doi: 10.1177/0363546517716930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Age influences biomechanical changes after participation in an anterior cruciate ligament injury prevention program. Thompson-Kolesar Julie A., Gatewood Corey T., Tran Andrew A., Silder Amy, Shultz Rebecca, Delp Scott L., Dragoo Jason L. 2018The American Journal of Sports Medicine. 46(3):598–606. doi: 10.1177/0363546517744313. doi: 10.1177/0363546517744313. [DOI] [PubMed] [Google Scholar]
- Biomechanical changes during a 90o cut in collegiate female soccer players with participation in the 11+ Dix Celeste, Arundale Amelia, Silvers-Granelli Holly, Marmon Adam, Zarzycki Ryan, Snyder-Mackler Lynn. Jun 2;2021 Int J Sports Phys Ther. 16(3) doi: 10.26603/001c.22146. doi: 10.26603/001c.22146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- A majority of anterior cruciate ligament injuries can be prevented by injury prevention programs: a systematic review of randomized controlled trials and cluster–randomized controlled trials with meta-analysis. Huang Yu-Lun, Jung Jaehun, Mulligan Colin M.S., Oh Jaekeun, Norcross Marc F. 2020The American Journal of Sports Medicine. 48(6):1505–1515. doi: 10.1177/0363546519870175. doi: 10.1177/0363546519870175. [DOI] [PubMed] [Google Scholar]