Abstract
Background
Despite the recommendations for delirium assessment in clinical settings, it stills remain a serious clinical problem associated with prolonged mechanical ventilation, stress on the patient and family, and mortality. There is paucity of data regarding delirium assessment and prevention in developing world. The Confusion Assessment Method for Intensive Care Unit (CAM-ICU) was developed to aid in the assessment of delirium. There is no documented assessment of delirium and prevention in Uganda. This study evaluated the effect of an educational intervention on nurses’ knowledge and practices of delirium assessment using the CAM–ICU tool.
Methods
We used a quasi-experimental and recruited a convenience sample of 29 nurses from ICU and ER. The assessment before and after the interventions was conducted using a self-completed questionnaire from October 2020 to January 2021. The interventions were delivered through face-to-face presentations, demonstrations, watching videos, and hands on practice. Data were entered into excel, cleaned and exported to Stata version 14. Median and interquartile ranges were used for continuous variables, and frequencies and percentages for categorical variables. The mean knowledge score was calculated before and after the intervention. A paired t-test was used to compare Pre- and Post-test knowledge and practice scores at P <0.05.
Results
Majority (62%) were female, 48% were Diploma holders, median age was 30 (IQR = 28–32) years and median years of experience 3.5 (IQR = 3–4). The Mean knowledge scores was 10.7 (SD = 2.36) pretest and 19 (0.94) posttest. The mean practice score was 2 (SD = 0.83) pretest and 6 (0.35) posttest. There were significant differences in mean knowledge and practice scores before and after intervention mean of (t (28) =17.32, p < 0.001) and (t (28) = 25.04, p<0.001), respectively.
Conclusion
Educational intervention Improved nurses’ knowledge and practice of delirium assessment. Continuous nursing education could improve nurses’ knowledge of delirium assessment and thus quality of patient care.
Keywords: nurse, delirium, assessment, knowledge, practice, CAM-ICU
Background
Delirium is a common condition faced by critically ill patients in intensive care units and is a top priority worldwide. Between 30% and 80% of patients admitted to ICUs develop delirium, leading to prolonged hospitalization, self-extubation, prolonged mechanical ventilation, and mortality.1–5 Delirium is defined as an acute brain dysfunction characterized by an alteration in cognitive levels, with the patient exhibiting signs and symptoms of inattention, disorientation, memory impairment, decreased consciousness, emotional changes and perseveration.6–9
Delirium in the ICU presents with behavioral problems such as hallucinations, delusions, anxiety, agitation, restlessness and insomnia.10 The ICU patients with hyperactive delirium show agitation, hallucination, and delusions, while those with hypoactive delirium appear calm and lethargic, and those who vacillate between are identified as mixed delirium.11–13 Despite the severity of delirium in ICU and advances in practice guidelines to encourage ongoing delirium assessment, many health care professionals have low awareness of delirium.14,15 As a result, 50% to 72% of the cases are overlooked, misdiagnosed or unrecognized by attending physician and nurses, further increasing morbidity and mortality rates.16,17 Previous studies have demonstrated that delirium is often not recognized because of insufficient knowledge and minimal educational emphasis in medical and nursing schools.18 In prior studies, 75% of the nurses interviewed stated that, even after they received formal education on the topic of delirium, they could not differentiate between delirium and dementia.19 Although education might play an important role in boosting delirium recognition, the optimal strategies to improve recognition and their usefulness are currently unclear, and several authors have pointed out the limitations of standard delirium teaching methods20
Delirium assessment, prevention, and treatment should be performed in all critically ill patients in the ICU using standardized tools such as Confusion assessment method for Intensive care unit (CAM-ICU) and now widely used around the world and the management of ICU delirium includes use of antipsychotic drugs like haloperidol and other pharmacological drugs like dexmedetomidine, however non-pharmacological measures remain the cornerstone of delirium management.;21–24 however, studies have pointed out that nurses need adequate knowledge and skills in delirium recognition to use the tools.25,26 In a multicenter study in Kampala using the CAM-ICU tool, researchers found that 51% of ICU patients developed delirium which if not treated could result into increased morbidity and mortality. Regardless of this high incidence and known negative outcomes nurses in the study still did not perform regular delirium assessments resulting in missing even more cases.27
Early detection of delirium depends on the knowledge and the experience of the critical care team. Nurses have the closest contact with patients and are the most equipped personnel to detect changes in the patient’s mental status or behavior at an early stage.28 Nursing staff Knowledge and practices are key in identifying delirium in ICU. Education and training are necessary to improve the knowledge and skills of care givers in using delirium assessment tools effectively.
Methodology
Study Design
A descriptive quasi-experimental design with pre- and post-test was used on nurses working in the ICU and a highly dependent unit. Basic knowledge of delirium assessment was established using a self –administered questionnaire, followed by an educational intervention and a post-test to determine effect. The study was carried out from October 2020 – January 2021.
Study Area
The study was conducted at the Mbarara Regional Referral Hospital (MRRH) in southwestern Uganda. The place of study is a public university teaching hospital with a capacity of 1000 beds. The Intensive care unit has a capacity of 8 beds and the ward for highly dependent patients has a capacity of 7 beds with a 24-hour nursing service. These two units treat critically ill patients who are at risk of delirium. The hospital serves as the regional referral hospital for south-western Uganda and receives patients from districts in south-western Uganda. It offers inpatient and outpatient healthcare services.
Study Population
Nurses working in the intensive care unit and high care unit at MRRH participated in the study. Most of these nurses are not specialized but have gained some work experience. A total of 29 nurses worked in these units. Because MRRH is at the top in this region that region, most critically ill patients may be referred there and therefore these nurses will most likely treat these patients, therefore their level of delirium assessment can provide insight into nurses’ knowledge of delirium and delirium assessment and prevention. The two service areas were chosen because they care for critically ill patients who are most prone to delirium.
Sample Size
The two units ICU and HDU has 29 nurses caring for critically ill patients. For a paired test analysis, a prior power analysis resulted in a total sample size of 22 participants to detect a large effect. (Cohen’s d = 0.5) with = 0.05 and 1-β=0.95 (Faul et al, 2009). Expecting a 10% turnover, the researcher aimed to have all 29 nurses participate in the study.
Sampling Technique
Because the number of nurses working in the Intensive Care Unit and high care unit was small, the researcher used a population sampling approach, recruiting all eligible nurses working in the ICU and HDU for the study.
Inclusion
Nurses who were working in the ICU and HDU at the time of data collection and had at least 3 months of experience working directly with critically ill patients were eligible to participate in the study. This was done to ensure maximum patient care experience.
Exclusion
Nursing professionals who were on vacation and had other commitments and who had not yet spent at least 3 months at the time of data collection for basic knowledge were considered ineligible to participate.
Data Collection Instruments
Tools Were Used
Tool one was a self-administered questionnaire used pre and post intervention to measure knowledge. The pre-interventions tool included a demographic section including age, gender, level of education and years of experiences. It also had 15 items adopted from a tool developed by29 with necessary modifications and some items on perceptions dropped because they were not relevant to the study. The tool was further reviewed by expert nurses in critical care one Senior ICU physician and one senior psychiatrist experienced in care of critically ill patients with delirium with a content validity index of 0.86. The knowledge questions related to delirium, its presentation, risk factors, and prevention and management. Knowledge questions on a Likert scale were dichotomized as “Yes” for strongly agree and agree and “No” for strongly disagree and disagree, 1 for “Yes” and 0 for “No”. Knowledge questions that were not on a Likert scale were coded “Yes=1” for the correct response and “No=0” for an incorrect response.
Tool 2: This handout was used to help respondents assess delirium. It was developed by the researcher after reviewing the related literature.
Tool 3: The Confusion Assessment Method for Intensive Care Unit (CAM-ICU), the tool non-psychiatric nurses are expected to use to detect delirium, has been validated both in western world and has sensitivity of 93–100%, a specificity of 98%–100%, and high inter-rater reliability (κ = 0.96) in detecting delirium, and the tool takes about 3 to 5 minutes to assess delirium.30 Another study by31 it was found that the CAM-ICU inter-rater reliability Kappa (= 0.85) and Cronbach’s alpha coefficient 0.69 (95% CI: 0.57–0.79).
Tool 4: The Richmond Agitation-Sedation Scale (RASS), is an arousal scale commonly used in intensive care units to assess for depth of sedation.32 But has been incorporated into several delirium assessments to assess for level of consciousness.33 RASS is a 10-point scale with four levels of anxiety or agitation (+1 to +4 [combative]), one level to denote a calm and alert state (0), and 5 levels of sedation (−1 to −5) culminating in unarousable (−5). The RASS has inter-rate reliability k = 0.80 (95% CI 0.69–0.90).
Data Collection Procedures
Ethical approval was obtained from Mbarara University of Science and Technology Ethics Committee (MUST-REC) #MUREC 1/7-20. We sought approval from the management of Mbarara Regional Referral Hospital. The researcher contacted the senior nurses of the two wards and arranged a meeting with the nurses, where the researcher explained the purpose of the study and the relevant details. Written consent was obtained from the study participants before they were given the pretest questionnaire. The data to measure intervention outcome were collected by the main researcher.
Pre-intervention phase: The Pre-intervention data using tool one was collected one week before the Intervention phase using a self –administered pretest questionnaire. The outcome of this data was used to measure previous knowledge and to modify teaching based on their knowledge. Respondents answered the questionnaire in an average of 30 minutes, were not allowed to cite any sources and gave it to the researcher immediately after completing it.
Intervention phase: A one and half hour face to face educational session was provided during the intervention phase. The sessions were provided twice a day for a period of three weeks to include nurses on the different shifts and this was done after the nurses eight hour shift to avoid disruptions with unit duties for both day and evening nurses.; both sessions were held on the same day and four nurses were attending the sessions two from each unit. The training session aimed to increase nurses’ knowledge of delirium in ICU, risk factors, and types of delirium, delirium assessment and delirium management. The validated CAM-ICU assessment tool was introduced. Participants were shown two five-minute videos, adapted by the Critical Illness, Brain Dysfunction, and Survivorship (CIBS) Center, showing how the CAM-ICU assessment tool is administered in clinical practice. This was followed by a case study scenario, adapted from CAM-ICU Training Manual, Revised edition to test the nurses’ understanding of the use of the CAM-ICU tool.34
Respondents received a folder containing delirium informational pamphlets, a pocket card containing the Richmond Agitation–Sedation Scale (RASS) and CAM-ICU tool, a pen, assessment forms, and a set of case study scenarios. The RASS was provided because CAM-ICU is used concurrently with RASS for the patients who are sedated as this determines when assessment of delirium should start.
Post Intervention phase: The participants were asked to complete the Post intervention test one-month post-formal instruction and monitoring of the tool to assess the effects of the educational intervention on the nurses’ knowledge on the use of the CAM –ICU in the management of delirium.
Data Management and Analysis
Data were analyzed using STATA version 14 for statistical analysis using descriptive statistics. For continuous variables, mean values and standard deviations (SD) or medians and interquartile ranges were used after fulfilling the assumption of normality using skewness and kurtosis. In addition to the overall assessment, each item was analyzed separately. A paired t-test was used to compare participants’ knowledge and practice of delirium assessment before and after the intervention.
Results
The median age of nurses was 30 (IQR = 28 to 32) and 62% were females. Of the all participants 48% had diploma as the highest level of education with the median years of experience of 3.5 years on an interquartile range1 of 3 to 4 years as shown in Table 1.
Table 1.
Descriptive Statistics of Characteristics of Respondents N=29
| Characteristic | N (%) |
|---|---|
| Gender | |
| Male | 11 (38) |
| Female | 18 (62) |
| Level of education | |
| Certificate | 8 (28) |
| Diploma | 14 (48) |
| Bachelor’s | 5 (17) |
| Master | 2 (7) |
| Years of experience (median(IQR)) | 3.5 (3–4) |
| Age (years) (Median (1QR)) | 30 (28–32) |
Nurses’ Delirium Knowledge Assessment
For better interpretation of knowledge, the total mean sum score of nurses knowledge on delirium assessment before education intervention was 10.7 (SD = 12.36) and after the intervention it was 19 (SD = 0.94). A paired t-test was performed to compare total knowledge scores before and after the test to determine the significance of the difference in nurses’ knowledge in the delirium. There was a statistically significant mean increase in nurses’ knowledge of delirium assessment (t(28)=17.32, p < 0.001) (Table 2). Table 3 shows the scores for each item for the pre- and post-intervention phases; similar to how there was an improvement in those respondents who answered the questions correctly in the post-intervention phase. Highly significant differences between pre- and post-intervention were found for six items, definition of delirium, cardinal signs of delirium, diagnosis of delirium treatment and prevention, and risk factors of delirium.
Table 2.
Paired t-Test Results of Scores on the Nurses’ Delirium Knowledge Assessment Before and After the Educational Intervention (N = 29)
| Mean | Standard Deviation | t-test | P-value | |
|---|---|---|---|---|
| Pre-score | 10.7 | 12.36 | 17.32 | p<0.001 |
| Post-score | 19 | 0.94 |
Table 3.
Nurses’ Knowledge Pre and Post Educational Intervention Questions (N = 29)
| Knowledge Assessment | Pre Test | Post Test | |
|---|---|---|---|
| Yes N (%) | Yes N (%) | P-value | |
| Delirium is an acute change in mental status associated with physical or mental illness | 12(41) | 26(90) | 0.025 |
| Do you know the cardinal signs of delirium | 2(7) | 28(97) | 0.031 |
| There is no blood, electrophysiological or imaging test for ICU delirium | 16(55) | 26(90) | 0.042 |
| Do you know the outcomes of ICU delirium | 6(21) | 23(79) | 0.160 |
| Increasing sedation at night does not shorten duration of delirium | 10(34) | 26(90) | 0.184 |
| A patient who is comatose cannot be screened for delirium | 16(55) | 28(97) | 0.259 |
| A patient who meets criteria for delirium but does not score high enough for positive delirium screening is Subsyndromal delirium | 7(24) | 26(90) | 0.302 |
| Haloperidol(Haldol) is a pharmacological agent of choice for treatment of delirium | 11(38) | 28(97) | 0.028 |
| Dexmedetomidine hydrochloride(Precedex) is associated with decreased incidence of delirium | 3(10) | 28(97) | 0.030 |
| Patients with delirium are always physically and verbally aggressive | 18(62) | 4(14) | 0.566 |
| Delirious Patient faces difficulty in following conversation | 22(76) | 27(93) | 0.067 |
| Mechanical ventilation is a risk factor for delirium | 19(66) | 28(97) | 0.460 |
| Electrolyte imbalance is a risk factor for delirium | 20(69) | 27(93) | 0.029 |
| History of dementia is a risk factor for delirium | 18(62) | 27(93) | 0.061 |
| Age increases the risk of delirium | 18(62) | 27(93) | 0.252 |
| Drugs like benzodiazepine increases the risk of delirium | 17(59) | 26(90) | 0.050 |
| Neurological conditions are risk factors of delirium | 25(86) | 25(86) | 0.484 |
| History of smoking is a risk factor for delirium | 15(52) | 28(97) | 0.326 |
| Being post -operative is a risk factor for delirium | 15(52) | 28(97) | 0.292 |
| Alcoholism is a risk factor for delirium | 23(79) | 28(97) | 0.046 |
| Comatose state at any point during admission is a risk factor | 16(55) | 28(97) | 0.129 |
Nurses Practices for Delirium Assessment
Participants’ total mean sum scores on delirium assessment before intervention were 2 (SD 0.83) and 6 (SD 0.35) after the intervention. A paired t- test compared pre-intervention assessment total score with post-intervention total score to ascertain the significance in the difference of participant knowledge. There was a statistically significant mean increase in nurses’ practices (28) = 25.04, p < 0.001. There was a statistically significant mean increase in nurses; practices of delirium assessment (t(28)=17.32, p < 0.001) (Table 4). There was a statistically significant mean increase in nurses’ practices (28) = 25.04, p < 0.001. There was a statistically significant mean increase in nurses’ practices on delirium assessment (t (28) = 17.32, p < 0.001) (Table 4). Table 5 shows the scores for each item for the pre- and post-intervention phases; similar to how there was an improvement in those respondents who answered the questions correctly in the post-intervention phase. Significant differences between pre- and post-intervention were found for four items: presence of a sedation protocol, frequency of sedation assessment, presence of a delirium assessment tool, delirium assessment, and the usual and used delirium assessment methods that referred any abnormal behavior to a psychiatrist.
Table 4.
Nurses’ Practice Questions Before and After Intervention (N = 29)
| Practice | Pre-Test | Post-Test | |
|---|---|---|---|
| Yes | Yes | P-value | |
| N (%) | N (%) | ||
| ICU has a sedation protocol/guideline | 20(69) | 28(97) | 0.029 |
| Sedation protocol specify frequency for delirium assessment | 6(21) | 28(97) | 0.003 |
| Level of sedation is frequently assessed | 13(45) | 27(93) | 0.641 |
| ICU has delirium assessment tools | 2(7) | 28(97) | 0.032 |
| Presence of delirium is frequently assessed | 2(7) | 27(93) | 0.690 |
| Delirium assessment is done once every eight hour shift | 2(7) | 28(97) | 0.027 |
Table 5.
Paired t-Test Results of Scores on the Nurses’ Practices on Delirium Assessment Before and After the Educational Intervention (N = 29)
| Mean | Standard Deviation | t-test | P-value | |
|---|---|---|---|---|
| Pre-score | 2 | 0.83 | 25.04 | p<0.001 |
| Post-score | 4 | 0.35 |
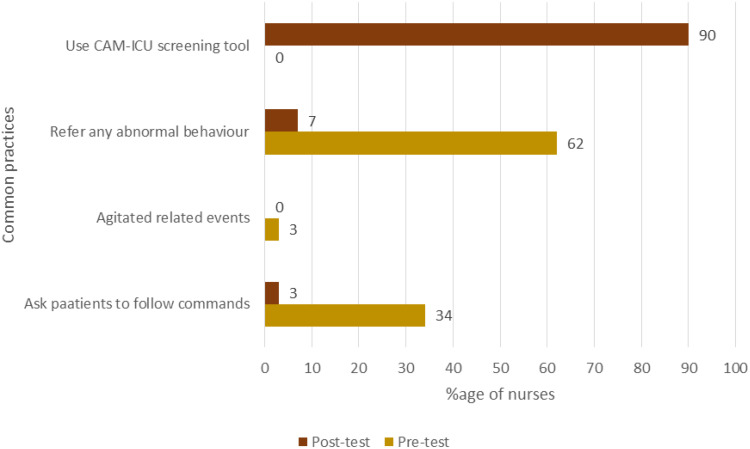
Three common methods were used to assess delirium prior to intervention. These included referring any abnormal behavior to psychiatry, asking patients to follow commands, and identifying agitated related events. After the intervention, the common assessment method was the use of the CAM-ICU tool (Figure 1).
Figure 1.
A graph showing common methods used to assess patients for delirium stratified by Pre and Post- test.
Discussion
Participants had not received any training in diagnosing delirium. This would also be attributed to the limited scope of practices for the participants, insufficient organizational support for their continuing education, as well as the lack of delirium assessment in their nursing curriculum at their training level. The mean total score of nurses’ knowledge of delirium assessment prior to the training intervention (10.7, SD 12.36) is relatively low compared to baseline means reported in other studies.35 A possible reason for the different results could be that nurses in this field of study were registered nurses who may not have this topic of delirium in their curriculum. However, at the post-intervention level, a significantly higher mean knowledge score was found (19, SD 0.94), showing that a brief educational intervention had a significant impact on nurses’ knowledge of delirium assessment and intervention.
Inadequate knowledge of definitions, outcomes, signs of ICU delirium, and the preventive measures reflected a low level of education on this topic. This is in line with the results of several studies.35–37 The greatest discrepancy was in knowledge of cardinal signs, definition of ICU delirium, and outcomes. This could be due to lack of awareness by the nurses of ICU delirium. The majority of participants were unaware that haloperidol is the pharmacological agent of choice for the treatment of delirium in the ICU, despite its broad recommendations in most of the literature. This is consistent with a study conducted in Jordan which found that nurses had insufficient knowledge of how delirium is managed in the ICU.38,39 However, this is in contrary to a study by40 in which nurses were aware of haloperidol as the pharmacological agent of choice for the treatment of delirium in the ICU. However, the nurses in that study had received some critical care training and continuous in service education prior to the study.
Although participants’ knowledge in this study improved after the intervention, it was found that scores for some of the questions did not improve significantly, particularly those related to general risk factors for delirium. As reported in previous studies, nurses in general have some difficulties in identifying risk factors for delirium.41
In this study, the majority of nurses reported that they did not have delirium assessment tools in their departments and reported that they assessed delirium at most once in their eight-hour shift. These actions may reflect that the nurses do not recognize delirium as a serious problem, had little or no knowledge about delirium, and there were no delirium guideline in the unit. This is consistent with a study done by42,43 where the nurses stated that they never did delirium assessment in their twelve hour shift, frequently of delirium assessment were not specified, and they had no delirium tools on their units. The findings are also consistent with a study done by38 where the majority of the nurses had never assessed for ICU delirium.44 These findings contrasts with38 where the respondents had delirium assessment tools in their unit and assessed delirium every eight hour shift. In this study, the common methods used for assessing delirium were agitated related events, the patient’s ability to follow commands, and a psychiatry consult for any abnormal behavior (once or more per shift) 34% and 62% consequently. While agitated related events were rarely used to evaluate the presence of delirium (3%). ICDSC and CAM – ICU were never being used by all nurses. This could be due to the fact that the hospital and the unit management have not established a delirium guideline or does not have a formal policy that specifies the correct and easy method to use in the assessment of delirium. These findings are in line with37 where nurses reported utilizing psychiatric consult as well as asking patients to follow commands and that CAM-ICU was never utilized by the majority of the participants despite its wide recommendation in the established literature.
Study Limitations
The main study limitation was the small sample size that limited generalizability. The hospital departments studied were representative of other general hospitals and the results may be of use to other clinicians. Due to the nature of the study design as applied to this study, there was no control group to compare the results to and this may have affected the internal validity of the study. Intervention studies generally recommend a minimum of 6 weeks to collect data post-intervention. In this study, however, we performed post-intervention data collection at 4 weeks, as adopted from some studies that considered a minimum of 4 weeks post-intervention to be sufficient. The argument is that the participants’ memories of the training content may have been quite fresh, with seemingly very good results. Intervention studies generally recommend a minimum of 6 weeks to collect data post-intervention. However, in this study; we performed post-intervention data collection at 4 weeks, as adopted from some studies that assumed a minimum of 4 weeks.
Conclusion
Prior to the educational intervention, there was generally little basic knowledge of delirium assessment among nurses. On the other hand, the educational intervention significantly improved nurses’ knowledge and practices on delirium assessment. Delirium assessment could be included in the hospital’s continuing medical education plans so that information about delirium can be shared and well explained to all nurses to improve their knowledge of delirium. Also an appropriate assessment tool and training of nurses in delirium assessment contributes to the majority of nurses assessing delirium and therefore having an impact on delirium assessment in critically ill patients.
Recommendations
Based on the results of this study, there is a need to organize regular training for nurses on delirium assessment in critically ill patients. This equips staff with knowledge and skills to improve the quality of patient care. Delirium assessment, including delirium assessment of critically ill patients, should be included in the curricula of nurses at various levels of nursing education where those nurses are expected to work in critical care to provide quality care. There are reliable and valid tools that can be used to do this, and hospital unit policies should include the tools and necessary services for nurses to ensure the appropriate standard of care.
Acknowledgments
Research reported in this publication was supported by the first Mile project. The content is solely the responsibility of the authors and does not necessarily represent the official views of the first mile project.
Funding Statement
Research reported in this publication was supported by the first Mile project. The content is solely the responsibility of the authors and does not necessarily reflect the official views of the first mile project.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declared no potential conflicts of interest in relation to the research, authorship, and/or publication of this article.
References
- 1.Salluh JI, Wang H, Schneider EB, et al. Outcome of delirium in critically ill patients: systematic review and meta-analysis. BMJ. 2015;350(may19 3):h2538. doi: 10.1136/bmj.h2538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Faria R, Moreno RP. Delirium in intensive care: an under-diagnosed reality. Revista Brasileira de terapia intensiva. 2013;25(2):137–147. doi: 10.5935/0103-507X.20130025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Witlox J, Eurelings LSM, de Jonghe JFM, et al. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA. 2010;304(4):443–451. doi: 10.1001/jama.2010.1013 [DOI] [PubMed] [Google Scholar]
- 4.Agarwal V, OʼNeill PJ, Cotton BA, et al. Prevalence and risk factors for development of delirium in burn intensive care unit patients. J Burn Care Res. 2010;31(5):706–715. doi: 10.1097/BCR.0b013e3181eebee9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klouwenberg PMK, Zaal IJ, Spitoni C, et al. The attributable mortality of delirium in critically ill patients: prospective cohort study. BMJ. 2014;349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramoo V, Abu H. Educational intervention on delirium assessment using confusion assessment method‐ICU (CAM‐ICU) in a general intensive care unit. Journal of clinical nursing. 2018;27(21–22):4028–4039. [DOI] [PubMed] [Google Scholar]
- 7.Blevins CS, DeGennaro R. Educational intervention to improve delirium recognition by nurses. Am j Critical Care. 2018;27(4):270–278. doi: 10.4037/ajcc2018851 [DOI] [PubMed] [Google Scholar]
- 8.Vahia VN. Diagnostic and statistical manual of mental disorders 5: a quick glance. Indian J Psychiatry. 2013;55(3):220. doi: 10.4103/0019-5545.117131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jackson P, Khan A. Delirium in critically ill patients. Crit Care Clin. 2015;31(3):589–603. doi: 10.1016/j.ccc.2015.03.011 [DOI] [PubMed] [Google Scholar]
- 10.Jain G, Chakrabarti S, Kulhara P. Symptoms of delirium: an exploratory factor analytic study among referred patients. Gen Hosp Psychiatry. 2011;33(4):377–385. doi: 10.1016/j.genhosppsych.2011.05.001 [DOI] [PubMed] [Google Scholar]
- 11.Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit: executive summary. Am J Health Sys Pharmacy. 2013;70(1):53–58. doi: 10.1093/ajhp/70.1.53 [DOI] [PubMed] [Google Scholar]
- 12.Bruno JJ, Warren ML. Intensive care unit delirium. Critical Care Nursing Clinics. 2010;22(2):161–178. doi: 10.1016/j.ccell.2010.03.003 [DOI] [PubMed] [Google Scholar]
- 13.Wells LG. Why don’t intensive care nurses perform routine delirium assessment? A discussion of the literature. Australian Critical Care. 2012;25(3):157–161. doi: 10.1016/j.aucc.2012.03.002 [DOI] [PubMed] [Google Scholar]
- 14.Bellelli G, Morandi A, Zanetti E, et al. Recognition and management of delirium among doctors, nurses, physiotherapists, and psychologists: an Italian survey. Int Psychogeriatrics. 2014;26(12):2093–2102. doi: 10.1017/S1041610214001653 [DOI] [PubMed] [Google Scholar]
- 15.Ista E, Trogrlic Z, Bakker J, et al. Improvement of care for ICU patients with delirium by early screening and treatment: study protocol of iDECePTIvE study. Implementation Sci. 2014;9(1):1–10. doi: 10.1186/s13012-014-0143-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Teodorczuk A, Reynish E, Milisen K. Improving recognition of delirium in clinical practice: a call for action. BMC Geriatr. 2012;12(1):55. doi: 10.1186/1471-2318-12-55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Devlin JW, Brummel NE, Al-Qadheeb NS. Optimising the recognition of delirium in the intensive care unit. Best Pract Res Clin Anaesthesiol. 2012;26(3):385–393. doi: 10.1016/j.bpa.2012.08.002 [DOI] [PubMed] [Google Scholar]
- 18.Akechi T, Ishiguro C, Okuyama T, et al. Delirium training program for nurses. Psychosomatics. 2010;51(2):106–111. doi: 10.1016/S0033-3182(10)70670-8 [DOI] [PubMed] [Google Scholar]
- 19.Marquis Foreman R. Consequences of not recognizing delirium superimposed on dementia in hospitalized individuals. J Gerontol Nurs. 2000;26(1):30. doi: 10.3928/0098-9134-20000101-09 [DOI] [PubMed] [Google Scholar]
- 20.Devlin JW, Marquis F, Riker RR, et al. Combined didactic and scenario-based education improves the ability of intensive care unit staff to recognize delirium at the bedside. Critical Care. 2008;12(1):1–6. doi: 10.1186/cc6793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marra A, Ely EW, Pandharipande PP, et al. The ABCDEF bundle in critical care. Crit Care Clin. 2017;33(2):225–243. doi: 10.1016/j.ccc.2016.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Estrup S, Kjer CKW, Poulsen LM, et al. Delirium and effect of circadian light in the intensive care unit: a retrospective cohort study. Acta Anaesthesiol Scand. 2018;62(3):367–375. doi: 10.1111/aas.13037 [DOI] [PubMed] [Google Scholar]
- 23.Kenes MT, Stollings JL, Wang L, et al. Persistence of delirium after cessation of sedatives and analgesics and impact on clinical outcomes in critically ill patients. Pharmacotherapy. 2017;37(11):1357–1365. doi: 10.1002/phar.2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miranda F, Arevalo‐Rodriguez I, Díaz G, et al. Confusion Assessment Method for the intensive care unit (CAM‐ICU) for the diagnosis of delirium in adults in critical care settings. Cochrane Database Sy Rev. 2018;2018(9):87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eastwood GM, Peck L, Bellomo R, et al. A questionnaire survey of critical care nurses’ attitudes to delirium assessment before and after introduction of the CAM-ICU. Australian Critical Care. 2012;25(3):162–169. doi: 10.1016/j.aucc.2012.01.005 [DOI] [PubMed] [Google Scholar]
- 26.Bannon L, McGaughey J, Clarke M, et al. Designing a nurse-delivered delirium bundle: what intensive care unit staff, survivors, and their families think? Australian Critical Care. 2018;31(3):174–179. doi: 10.1016/j.aucc.2018.02.007 [DOI] [PubMed] [Google Scholar]
- 27.Kwizera A, Nakibuuka J, Ssemogerere L, et al. Incidence and Risk Factors for Delirium among Mechanically Ventilated Patients in an African Intensive Care Setting: an Observational Multicenter Study. Crit Care Res Pract. 2015;2015:491780. doi: 10.1155/2015/491780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leonard A. Evaluating the usability and knowledge testing of the delirium assessment tool, confusion assessment method for intensive care unit, for nurses in medical surgical intensive care unit. 2016.
- 29.Devlin WJJFLFJ. Assessment of delirium in the intensive care unit: nursing practices and perceptions. American Journal of Critical Care. 2008;17(6):555–565. [PubMed] [Google Scholar]
- 30.Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 2001;286(21):2703–2710. doi: 10.1001/jama.286.21.2703 [DOI] [PubMed] [Google Scholar]
- 31.Kwizera A, Nakibuuka J, Ssemogerere L, et al. Incidence and risk factors for delirium among mechanically ventilated patients in an African intensive care setting: an observational multicenter study. Crit Care Res Pract. 2015;2015:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sessler CN, Gosnell MS, Grap MJ, et al. The Richmond Agitation–Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166(10):1338–1344. doi: 10.1164/rccm.2107138 [DOI] [PubMed] [Google Scholar]
- 33.Han JH, Wilson A, Vasilevskis EE, et al. Diagnosing delirium in older emergency department patients: validity and reliability of the delirium triage screen and the brief confusion assessment method. Ann Emerg Med. 2013;62(5):457–465. doi: 10.1016/j.annemergmed.2013.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stollings JL, Devlin JW, Lin JC, et al. Best practices for conducting interprofessional team rounds to facilitate performance of the ICU liberation (ABCDEF) bundle. Crit Care Med. 2020;48(4):562–570. doi: 10.1097/CCM.0000000000004197 [DOI] [PubMed] [Google Scholar]
- 35.Christensen M. An exploratory study of staff nurses’ knowledge of delirium in the medical ICU: an Asian perspective. Intensive Critical Care Nursing. 2014;30(1):54–60. doi: 10.1016/j.iccn.2013.08.004 [DOI] [PubMed] [Google Scholar]
- 36.Elliott SR. ICU delirium: a survey into nursing and medical staff knowledge of current practices and perceived barriers towards ICU delirium in the intensive care unit. Intensive Critical Care Nursing. 2014;30(6):333–338. doi: 10.1016/j.iccn.2014.06.004 [DOI] [PubMed] [Google Scholar]
- 37.Rowley-Conwy G. Critical care nurses’ knowledge and practice of delirium assessment. British Journal of Nursing. 2017;26(7):412–417. doi: 10.12968/bjon.2017.26.7.412 [DOI] [PubMed] [Google Scholar]
- 38.Ozsaban A, Acaroglu R. Delirium assessment in intensive care units: practices and perceptions of Turkish nurses. Nurs Crit Care. 2016;21(5):271–278. doi: 10.1111/nicc.12127 [DOI] [PubMed] [Google Scholar]
- 39.Hamdan-Mansour AM, Farhan NA, Othman EH, et al. Knowledge and nursing practice of critical care nurses caring for patients with delirium in intensive care units in Jordan. J Contin Educ Nurs. 2010;41(12):571–576. doi: 10.3928/00220124-20100802-01 [DOI] [PubMed] [Google Scholar]
- 40.Ely WE, Stephens RK, Jackson JC, et al. Current opinions regarding the importance, diagnosis, and management of delirium in the intensive care unit: a survey of 912 healthcare professionals. Critical care medicine. 2004;32(1):106–112. doi: 10.1097/01.CCM.0000098033.94737.84 [DOI] [PubMed] [Google Scholar]
- 41.Varghese NC, Macaden L, Premkumar B, et al. Delirium in older people in hospital: an education programme. Br J Nursing. 2014;23(13):704–709. doi: 10.12968/bjon.2014.23.13.704 [DOI] [PubMed] [Google Scholar]
- 42.Matoke R. Factors influencing nurses perceptions and practices regardind delirium among intensive care unit patients at Kenyatta hospital Kenya. University of Nairobi; 2016. [Google Scholar]
- 43.Xing J. Perceptions, attitudes, and current practices regards delirium in China. A survey of 917 critical care nurses and physicians in China. Medicine. 2017;96:348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Khadija Lafi DAHS. Nurses’ Perceptions & Practices towards Delirium in the Intensive Care Units. J Nursing Health Sci. 2018;7:36. [Google Scholar]