Abstract
Background
Pre-exposure prophylaxis (PrEP) is an emerging biomedical prevention intervention. Documenting PrEP service delivery models (SDMs) that promote linkage to and continuation of PrEP will inform guidelines and maximise roll-out.
Objectives
To synthesise and appraise the effectiveness and feasibility of PrEP SDMs designed to promote linkage to PrEP care among adolescent girls and young women (AGYW) and men in sub-Saharan Africa (SSA).
Eligibility criteria
Primary quantitative and qualitative studies published in English and conducted in SSA were included. No restrictions on the date of publication were applied.
Sources of evidence
Methodology outlined in the Joanna Briggs Institute reviewers’ manual was followed. PubMed, Cochrane library, Scopus, Web of Science and online-conference abstract archives were searched.
Charting methods
Data on article, population, intervention characteristics and key outcomes was charted in REDCap.
Results and conclusion
Of the 1204 identified records, 37 (met the inclusion criteria. Health facility-based integrated models of PrEP delivery with family planning, maternal and child health or sexual and reproductive services to AGYW resulted in PrEP initiation of 16%–90%. Community-based drop-in centres (66%) was the preferred PrEP outlet for AGYW compared with public clinics (25%) and private clinics (9%). Most men preferred community-based delivery models. Among individuals who initiated PrEP, 50% were men, 62% were <35 years old and 97% were tested at health fairs compared with home testing. Integrated antiretroviral therapy (ART)-PrEP delivery was favoured among serodiscordant couples with 82.9% of couples using PrEP or ART with no HIV seroconversions. PrEP initiation within healthcare facilities was increased by perceived client-friendly services and non-judgemental healthcare workers. Barriers to PrEP initiation included distance to travel to and time spent at health facilities and perceived community stigma. PrEP SDMs for AGYW and men need to be tailored to the needs and preferences for each group. Programme implementers should promote community-based SDMs to increase PrEP initiation among AGYW and men.
Keywords: public health, HIV & AIDS, public health
STRENGTHS AND LIMITATIONS OF THIS STUDY.
A comprehensive search strategy was developed, and the search was carried out across multiple databases and conference archives.
The methodology used in the scoping review was robust and included double data screening, extraction and synthesis.
All included studies underwent critical appraisal of sources of evidence using approved tools.
Studies not conducted in sub-Saharan Africa and that were published in non-English languages were excluded.
Most of the included studies were from Kenya, Uganda and South Africa limiting the generalisability of the results.
Background
Recent reports indicate a decline in new HIV infections globally. However, this decline is occurring at a slower pace in regions with generalised HIV epidemics such as sub-Saharan Africa (SSA). In 2017, SSA accounted for 64% of new HIV infections globally.1 Two underserved populations that are critical to drive the decline in new HIV infections are adolescent girls and young women (AGYW; 15–24 years) and men (25–65 years). AGYW are at substantial risk for HIV-infection with an estimated 310 000 new infections globally in 2018—86% of which was in SSA.1 Men, on the other hand, account for more AIDS-related deaths globally than women—400 000 deaths in men in 2018 compared with 270 000 in woman.1
For differing reasons, AGYW and men show lower health seeking behaviour because of interpersonal and structural factors. AGYW’s access to health services is limited by stigma, negative attitudes from healthcare workers and inconvenient clinic operating hours.2 However, ‘man unfriendly clinics’ are characterised by inaccessible clinic hours/locations, difficulty in engaging with female staff and gender norms that discourage men from accessing health services.3 4
Among the 2020 Global Prevention Targets and Commitments is the reduction in the number of AGYW newly infected with HIV globally to below 100 000, and to ensure that 3 million people at substantial risk of contracting HIV have access to pre-exposure prophylaxis (PrEP).5 To achieve these targets, primary prevention programmes should be structured around five central pillars: (1) combination prevention for AGYW; (2) combination prevention with key populations; (3) voluntary medical male circumcision (VMMC) and sexual and reproductive health services (SRHS) for men and boys; (4) comprehensive condom programmes and (5) rapid introduction of PrEP.5 PrEP for HIV refers to the use of antiretroviral drugs among HIV-negative people to prevent the acquisition of HIV.6
PrEP has shown effectiveness in reducing HIV acquisition among couples, sex workers, men who have sex with men (MSM), transgender and people who inject drugs and AGYW.7 The impact of PrEP on the HIV epidemic depends on the extent of PrEP initiation among people at substantial risk for HIV infection (WHO defined substantial risk of HIV acquisition as HIV incidence of 3 per 100 person-years or higher in the absence of PrEP).7 8 Since September 2015, the WHO recommended offering oral PrEP to every person at substantial risk of contracting HIV.7 In the current South African guidelines for PrEP, specific populations considered to be at substantial risk of HIV infection include AGYW, MSM, people with more than one sexual partner, people who inject drugs, people with a recent history of sexually transmitted infections, people who recognise their own risk and request PrEP, serodiscordant couples if the HIV positive partner is not virally suppressed and sex workers.9 10
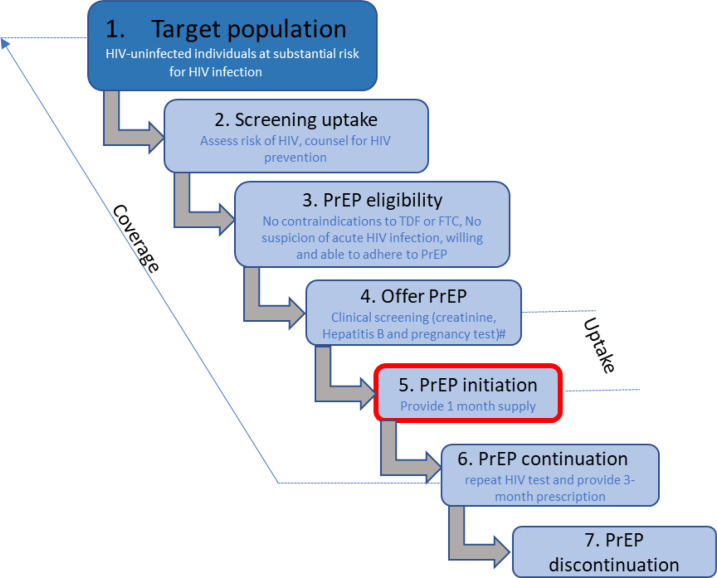
Literature on PrEP has largely been focused on knowledge, attitudes and interest in PrEP. As countries scale up use of PrEP as part of their combination prevention packages, evidence on service delivery models (SDMs) that promote initiation and continuation on PrEP are needed especially among vulnerable and hard to reach populations such as AGYW and men. HIV prevention cascades have been proposed as a logical framework to monitor populations at substantial risk for HIV acquisition as they navigate the steps from HIV testing to assessing the risk of the individual to determining PrEP eligibility before PrEP initiation and continuation or discontinuation.8 PrEP initiation (step 5) represents a critical step in the PrEP cascade (figure 1),8 10 because it reflects people’s awareness and interest in lowering their risk for HIV. Differentiated models, which are centred around clients’ needs and expectations and relieving unnecessary burdens on the health system while targeting behavioural and structural determinants of AGYW and men, can potentially increase acceptability and accessibility of PrEP. These include innovative strategies that streamline HIV testing, link AGYW and men to HIV prevention services, provide differentiating medication access points, reduce stigma and barriers of parental consent for PrEP initiation.11 PrEP SDMs should be designed with the populations being served central to the design.12
Figure 1.
Oral PrEP cascade: Adapted from Dunbar et al (2018).8 Following an HIV-negative diagnosis (step 1), an individual is assessed for risk of HIV (step 2). An individual at substantial risk of HIV acquisition or who requests PrEP is assessed for eligibility for PrEP (step 3). After documenting eligibility for PrEP use, several baseline clinical investigations are conducted (step 4 PrEP is initiated (step 5) on the same-day as HIV testing. The recommended regimen is tenofovir (TDF)/emtricitabine (FTC) one tablet by mouth daily. PrEP continuation visits (step 6) include: month 1, every 3 months. PrEP is discontinued (step 7) if the individual tests HIV positive, develops renal disease, is non-adherent, does not want or need PrEP, no longer meets eligibility criteria or if there are safety concerns. PrEP, pre-exposure prophylaxis.
There is a gap in knowledge on the characteristics of AGYW and men who initiate PrEP compared with those who do not initiate PrEP. This information is critical for informing national policies and implementation guidelines for PrEP roll-out. As such, the aim of this review was to synthesise and appraise the effectiveness and feasibility of PrEP SDMs designed to promote linkage to care among AGYW and men eligible for PrEP in SSA. The objectives were to (A) summarise SDMs that promote PrEP initiation and (B) explore users’ perceptions, and barriers and facilitators of these PrEP models.
Methods
We used a scoping review design to map existing literature, explore the research studies conducted and identify research and knowledge gaps in models used to deliver PrEP.13 Scoping reviews can be of particular use when the topic has not yet been extensively reviewed or is of a complex or heterogeneous nature.14 The research question was defined using the Population-Intervention-Comparison-Outcome framework (table 1). We defined our outcomes as (1) Linkage to PrEP care (defined as the proportion of AGYW or men who are initiated on PrEP following an HIV-negative diagnosis, step 7 of figure 1) and (2) perceptions, barriers and facilitators of PrEP SDMs. The SDM was defined as the setting used for delivery of PrEP viz. facility-only, community-only, research-only, mobile-only and a hybrid model encompassing two or more of the above settings.
Table 1.
Scoping review population, intervention and outcome
| Population | Heterosexual females (15–24 years) and men (25–65 years) |
| Intervention | Interventions (SDMs) designed to improve PrEP initiation |
| Comparison | Not applicable |
| Outcome | Linkage to PrEP care (defined as the proportion of AGYW or men who are initiated on PrEP following a HIV-negative diagnosis) and perceptions on SDMs |
AGYW, adolescent girls and young women; PrEP, pre-exposure prophylaxis; SDMs, service delivery models.
Protocol and registration
This review was conducted and reported in line with the Joanna Briggs Institute (JBI) reviewer’s manual and structured using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR).15 16 A review protocol for this scoping review was registered with the Open Science Framework (DOI 10.17605/OSF.IO/EG9TD).
Patient and public involvement
No patients or public were involved in the study.
Eligibility criteria
We included primary studies on PrEP SDM for AGYW and men, with both qualitative and quantitative study designs published in English and conducted in SSA. No restrictions on the date of publication were applied (last literature search was conducted in July 2021). Table 2 details the inclusion criteria applied to studies. We excluded studies that were focused exclusively on key population groups in HIV programmes such as lesbian, gay, bisexual, MSM, etc and publication types (eg, systematic reviews, case studies).
Table 2.
Eligibility criteria describing study inclusion criteria for the scoping review
| Study type | Quantitative studies including randomised clinical trials (RCTs), quasi-randomised and non-RCTs, longitudinal observational (historical cohorts, prospective cohorts, case–control and before-and-after studies), analytical cross-sectional studies and non-comparative studies |
| Qualitative studies using any study design | |
| Population | Study population included heterosexual females (15–24 years) and males (25–65 years) |
| Outcomes | Focus of research: PrEP SDMs, that is, service provision/implementation science/models of care/differentiated care/linkage to care/intervention |
| Papers reporting on barriers and facilitators of PrEP SDMs | |
| Papers on user perceptions of PrEP SDMs | |
| Setting | Sub-Saharan African countries—based on the World Bank’s country classification78 |
PrEP, pre-exposure prophylaxis; SDMs, service delivery models.
Information sources and search strategy
PubMed, Cochrane library, Scopus and Web of Science including three online conference archives (AIDS conference, Conference on Retroviruses and Opportunistic Infections and International AIDS Society Conference on HIV Science) were searched. The reference list of systematic reviews was checked to identify relevant primary studies. The three-step search strategy recommended by the JBI Reviewer’s Manual was used.15 During the first step, one author (WC) conducted an elementary search on PubMed to establish the volume of relevant articles on the topic. Two authors (WC and TR) then screened the title and abstract of the retrieved articles to identify keywords and index terms which were used to build a search strategy (see online supplemental appendix 1). The final search results were exported into EndNote,17 and duplicates were removed.
bmjopen-2022-061503supp001.pdf (77.9KB, pdf)
Selection of sources of evidence
Titles and abstracts were double screened in Rayyan18 by any two of a group of eight independent authors (TR, WC, KJ, NJ, DG, TMA, MH and EBT). There was no restriction placed on age range during the screening phase to ensure that articles with age disaggregated analysis were included. Full text articles and conference abstracts, including articles from the 2020 AIDS conference were retrieved and independently double screened by WC and TR.
Data charting process and data items
Using a predesigned data-charting form, key and relevant information were systematically extracted from full-text articles in REDCap19 by any 2 of a group of 10 independent authors (TR, WC, TMA, NJ, DG, BZ, CM, MH, EBT and EN). We charted data on article characteristics, population characteristics, intervention characteristics and key outcomes (table 1).
Critical appraisal of individual sources of evidence
Information for quality assessment was incorporated into the data charting form on REDCap.19 Due to the different study designs and research methodologies adopted in the included studies, we used three different tools to appraise the articles. For comparative studies including randomised trials, non-randomised trials, interrupted time series and controlled before-and-after studies, we used the risk of bias criteria recommended by the Effective Practice and Organisation of Care.20 For qualitative studies, we used the Critical Appraisal Skills Programme (CASP) checklist.21 For other studies, we used the Ways of Evaluating Important and Relevant Data (WEIRD) tool.22 Modelling studies were excluded from the appraisal step.
Analysis
For quantitative studies we used a narrative analysis and tabulated data by gender and by SDM. We summarised the settings, populations and sample for each group, along with the interventions and findings. For qualitative studies, we did a thematic analysis that resulted in organising the data into themes, authors’ interpretations, and quotes and integrated these findings to support the quantitative data. We tabulated the data by SDMs (health facility, community, research or mobile) and by population (AGYW only, men only or models for both). Furthermore, we determined the existing gaps in the different categories of interventions that can be strengthened to promote initiation and continuation on PrEP among AGYW and men.
Results
Selection of sources of evidence
Our search identified 1604 citations. After duplicates (413) were removed, a total of 1204 titles and abstracts were identified from searches of electronic databases and 13 from other sources including conferences. The PRISMA flow diagram (figure 2) illustrates the screening process to identify records that meet the study inclusion criteria. Based on the screening of title and abstracts, 1102 records were excluded, with 102 full text articles and conference abstracts to be retrieved and assessed for eligibility. From the review of full text articles, 67 were excluded for the following reasons: editorials/commentaries/reviews/protocols, interviews with stakeholders, articles on topical PrEP, wrong outcome and focus on key populations. During data charting, two additional articles were excluded. Four additional articles were added after the initial search process, these articles were identified following the 2020 AIDS conference in July. The final number of studies that were considered eligible for this scoping review were 37 (27 studies and 10 conference abstracts).
Figure 2.
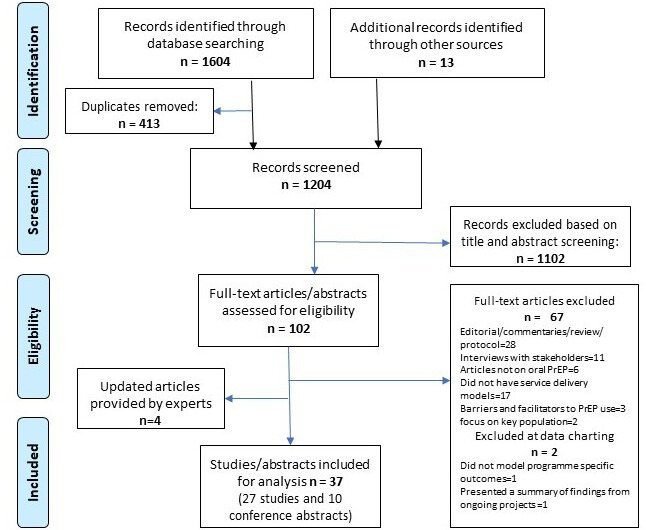
PRISMA flow diagram adapted from: Moher et al.79 PrEP, pre-exposure prophylaxis; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Description of sources of evidence
A description of the characteristics, setting, SDMs and intervention modalities of the included studies are provided in online supplemental appendix 2. There was a mixture of quantitative (n=23), qualitative (n=11) and mixed-method studies (n=3). Most studies were demonstration/IS projects (n=10) while other methodological approaches included randomised controlled trials (RCTs) (n=5) and cross-sectional studies (n=5). Most were conducted in Kenya (n=17), with the remainder conducted in Uganda (n=10), South Africa (n=10), Tanzania (n=3), Malawi (n=2), Mozambique (n=2) and Zimbabwe (n=1). These studies reported evidence on the following PrEP SDMs; health facility (6), mobile (1), research site (8), community (6), hybrid (10) and not described/not applicable (6). Thirteen studies focused on AGYW, 19 studies focused on AGYW and men, 1 study focused on men only and 4 were classified as other (ie, age categories were not specified). PrEP services were offered in 25 of the 37 studies while PrEP perceptions/opinions were assessed in the other 12 studies.
bmjopen-2022-061503supp002.pdf (255.6KB, pdf)
Critical appraisal of evidence
Full-text articles appraised using the WEIRD tool were mostly assessed as having either no or very minor or moderate concerns for items that were unclear in the article (see online supplemental appendix 3). Most of the qualitative studies or abstracts performed well on all items except on items 4 (the recruitment strategy was appropriate to the aims), 8 (the rigour of the data analysis) and 10 (the value of the research in terms of its contribution to the literature and/or policy and process). Due to limited information in the abstracts to clearly answer the items using the WEIRD tool, most of the abstracts were appraised as either having an unclear or serious risk of bias.23–28
bmjopen-2022-061503supp003.pdf (79.4KB, pdf)
Results of sources of evidence
PrEP SDMs for AGYW
Among AGYW, PrEP SDMs were found in Health facility-based (HF-B) (n=6), hybrid (mobile clinic-healthcare facility or community-healthcare facility, n=3), research site (n=2) and mobile clinic (n=1) (see online supplemental appendix 2).
Health facility
Three studies from Kenya evaluated a HF-B delivery modality by integrating PrEP delivery into routine services. Mugwanya et al29 evaluated a PrEP-dedicated nurse-led integrated delivery of PrEP in family planning (FP) clinics while Kinuthia et al and Pintye et al evaluated approaches to integrate PrEP into maternal and child health (MCH) clinics providing antenatal care (ANC) and post-natal care.30 31 Integration of universal screening and counselling for PrEP in FP and MCH clinics resulted in PrEP initiation of 16% and 49.2%, respectively, among AGYW. Younger women (≤24 years) who initiated PrEP at MCH clinics were significantly more likely to return for a PrEP refill at month 3 compared with women >24 years (54.9% vs 45.1%) (p=0.05).30 These studies used nurses dedicated to providing PrEP services only, which may limit applicability in a sub-Saharan setting where facilities have a limited clinical workforce. A study by Ngure et al which integrated PrEP with FP services found that PrEP dispensation was more frequent among those concurrently using effective contraception, (adjusted relative risk (aRR)=1.19; 95% CI =1.08 to 1.32) and contraceptive use was more common among those on PrEP (aRR 1.63; 95% CI 1.18 to 2.25), highlighting the importance of SDMs that integrate PrEP with FP services.32 Pintye et al found that participants who initiated PrEP at MCH clinics took an additional 18 min for PrEP related activities over and above the time spent at the clinic to receive routine MCH services. The additional time could deter AGYW from initiating and continuing PrEP and depending on healthcare facility size and patient volume integrating PrEP into these routine services could result in several additional hours of work for nurses.31 A recent study in Malawi comparing four SDMs (model 1: standard of care (SoC), model 2: integrated youth-friendly services, model 3: model 2 plus a small-group behavioural intervention, and model 4: model 3 plus cash transfer) found that PrEP initiation will best be promoted in youth-friendly locations such as schools because of ease of access and comfort in the absence of adult patients and family members.
Hybrid (community-health facility)
Two studies evaluated the scaling up of PrEP in Kenya through integration into routine health services in drop-in centres (DICEs), public and private health facilities designed primarily for sex workers.26 33 Ongwen et al reported that within the context of the Jilinde project, which implements oral PrEP as a routine service at a public health scale in Kenya, 6.5% (n=1851) AGYW initiated PrEP, and DICEs were the preferred PrEP outlet for adolescent girls with 66% accessing services in DICEs, 25% in public clinics and 9% in private clinics. Among AGYW who initiated PrEP, the entry channel into the PrEP pathway was through peer educators and networks (50%); community outreaches (20%) and within health facilities (30%).26 Were et al found that among all individuals eligible for PrEP in the study which included female sex workers and MSM, 11% of AGYW initiated PrEP.33 The majority (81%) of clients initiated PrEP through DICEs, whereas 14% and 5% were initiated through public and private facilities, respectively. The majority of AGYW did not persist on PrEP use at month 1 (68% drop off) and month 3 (94% drop off) follow-ups. Qualitative evidence from this study found that AGYW who initiated PrEP in public and private health facilities reported insensitive referral and access to the PrEP delivery pathways where ‘The (HIV) testing place is different from the place I was asked questions and the place for collecting the medicine is also different. We took long because we were walking form one place to another’.33
Research site
Delany-Moretlwe conducted an RCT in Tanzania and South Africa to evaluate whether empowerment clubs increased PrEP initiation and continuation among AGYW. Participants were randomised to the SoC, which included comprehensive SRHS, with counselling and short message service reminders for PrEP users, or to empowerment clubs plus SoC. Facilitators-led small group sessions and clinic follow-up visits for sexually active AGYW on PrEP. Across both arms, 97% initiated PrEP. PrEP continuation did not vary significantly by study arm and diminished with time (73% at month 1, 61% at month 3 and 34% at month 6).34 Donnell et al found that HIV incidence declined significantly after on-site provision of PrEP at the research sites.35 Hill et al found that epidemiologic HIV risk scores were positively associated with PrEP interest, and that high numbers of AGYW both above and below the high-risk cut-off were very interested in PrEP (68% vs 63%).36
Mobile
A South African study found that integrating PrEP with SRHS and delivering it via an adolescent-friendly mobile clinic led to an increase in both PrEP initiation and contraception. AGYW who were using contraception were significantly more likely to initiate PrEP (76%) on the same-day compared with those who were not using contraception and declined PrEP (66%) (p=0.001). Contraception was initiated by 44% of AGYW on the same-day as PrEP initiation compared with 30% who declined PrEP (p=0.003).27 No qualitative evidence on the acceptability and feasibility of mobile delivery models were identified.
Overall perceptions of SDMs by AGYW
In a study conducted in Malawi, Maseko et al found high levels of hypothetical PrEP acceptability among AGYW who reported that interest in PrEP depends on confidential access and discrete packaging (cartons or bottles that resemble treatment for common ailments) of the drug. Moreover, AGYW reported that youth-friendly delivery modalities such as schools and youth-friendly sections of health centres that provide ‘…a place for the youths to be comfortable getting these drugs…’ may facilitate the initiation of PrEP as a prevention strategy.37
PrEP SDMs for men
We found one mixed-method study among young South African men. PrEP was not provided, but hypothetical perceptions, barriers and enablers of PrEP initiation were assessed. While only 11% of men were aware of PrEP, 62% reported that they were very likely to take it. The young men preferred to keep PrEP use a secret from their partners, friends and family. PrEP initiation was also dependent on the SDM used. Receiving PrEP from the clinic was reported as a barrier to PrEP usage as this could incite community stigma. Young men reported that ‘…they (community) would immediately think that you are HIV positive already, not that you are taking the prevention one…’
PrEP SDMs for AGYW and men
We found 19 studies that assessed various SDMs for linkages to PrEP for AGYW and men. Among AGYW and men, PrEP SDMs included hybrid (research site-healthcare facility or community-healthcare facility, n=8), community (n=5) and research site (n=6). These studies either recruited serodiscordant couples or included AGYW and men as individual participants.
Hybrid
We identified seven studies that used a hybrid model to deliver PrEP.38–44
One study from Kenya and Uganda by Heffron et al involved a hybrid (research site health facility) model that integrated PrEP delivery into antiretroviral therapy (ART) treatment services for high-risk HIV serodiscordant couples.38 The intervention was mainly couples-based and involved HIV prevention counselling; safer conception counselling or contraceptives; counselling and HIV testing for HIV-negative partner; PrEP initiation/prescription; and referral to a local health facility for the HIV infected partner for ART. The results showed high uptake of integrated PrEP and ART with an estimated 96% reduction in HIV incidence (82.9% of couples used PrEP or ART and there were no HIV seroconversions, 14.5% used some ART and/or PrEP and 2.6% used neither PrEP nor ART).38
Qualitative evidence that explored HIV serodiscordant couple’s decision making and motivations to initiate PrEP through this integrated ART-PrEP approach showed that a positive clinical encounter with a healthcare provider and client-friendly services played a critical role in the couple’s decisions to initiate and continue PrEP.43 Clear messaging, in-depth counselling and friendly, non-judgemental/stigmatising services provided by healthcare workers empowered, reassured and promoted PrEP initiation among HIV serodiscordant couples with some describing it as ‘service beyond the medicine’.43 Furthermore, being at a place where service is offered to both couple (ART for the HIV positive partner and PrEP for the HIV-negative partner) motivated their decision.43
Five studies used a hybrid mobile testing approach implemented at community health fairs, home or local health facility.24 39–42 Two studies from Kenya and Uganda showed that PrEP initiation was high (>75%) among individuals who received HIV testing on the same-day.39 41 Mayer et al found that 39% of participants initiated PrEP within 4 weeks of the community health campaign.40 However, the distance between the participants and the healthcare provider influenced PrEP initiation.
Koss et al and Camlin et al who explored barriers influencing PrEP initiation using the hybrid (community-health facility) model,24 42 found that PrEP initiation was hindered by HIV/ART-related stigma which emanated from the colour of the pill being the same as HIV treatment regimens, and access of PrEP services at the same facility where HIV care is provided.42 Men reported that the ‘… majority of us fear to go to the health center’ and suggested alternatives such as designating a clinic day for PrEP or ‘…distribute [PrEP] to the people…’. Participants reported that healthcare workers should deliver PrEP or find delivery methods that are easily accessible by the community ‘…just like they did with condoms’. Young adults who attended school outside the community could not initiate PrEP given that PrEP was only provided within study communities. Furthermore, school attendance made initiating and continuing PrEP challenging.24 42
Community
Two South African studies conducted in a community setting explored the hypothetical opinions of PrEP among salon owners, stylists and clients.45 46 Ninety-five per cent of owners and stylists and 77% of clients were comfortable with PrEP being offered at hair salons,46 which provide a geographically convenient and conducive environment for receiving health services.45 46 A third community-based study which used a 90 s PrEP demand creation video and informational brochures, found that 68% and 56% of young women, respectively, reported that they were definitely interested in learning more about and initiating PrEP. The study also found that young women preferred realistic visuals that they could identify with, rather than highly stylised models. Data evaluated by Lubwama et al showed that 69.2% of key populations which included AGYW and serodiscordant couples were reached through DICEs and community-based outreach centres providing PrEP versus fixed public health facilities.47 The proportion that returned for PrEP was higher among serodiscordant couples (3 months: 56.9%, 6 months: 46.8%) compared with sex workers (3 months: 37.5%, 6 months: 26.3%).
Clinical research site
In three of the six studies conducted at a clinical research site,25 38 48–52 PrEP was integrated with ART or with ART and other interventions such as VMMC.38 49 50 Across the three studies, ≥95% of the HIV-negative partner within serodiscordant couples initiated PrEP. The use of PrEP in combination with ART or other prevention interventions (VMMC) or conception strategies resulted in reduced HIV incidence. Serodiscordant couples found that the ‘couples-focused’ services provided through the integrated PrEP-ART strategy strengthened their relationships.
Overall perceptions of SDMs by AGYW and men
Several studies explored factors that influence PrEP initiation, non-initiation and discontinuation in individuals who received PrEP through the different SDMs.24 25 42–44 52 Motivators to initiate PrEP included: perception of high risk, preference of PrEP over other HIV prevention methods, protection from unwanted/forced sexual encounters, love for one’s partner, knowledge about PrEP and the belief it is effective, partner support belief that PrEP supported life goals and a positive clinical encounter.24 25 42–44 52 53 Females preferred a product that was delivered at a health clinic over accessing it at a pharmacy.54 Barriers to PrEP initiation included daily pill burden, side effects, mixed dosing messaging, living with parents or attending school, partners consent or partners reaction to use and HIV-related stigma.24 25 42–44 52 53
Other models
We identified four other studies that explored other methods of promoting PrEP initiation among AGYW and men.55–58 Jani et al explored male partners support for hypothetical PrEP use by AGYW.57 Male partners highlighted that their support would be contingent on their early involvement in the decision-making process regarding PrEP which would alleviate suspicion of infidelity. AGYW suggested that not including male partners may result in social harms (partner violence, dissolution of relationships). Strategies recommended by male partners included couples counselling, educating and providing PrEP to men and community sensitisation. Makyao et al explored parental support of AGYW’s hypothetical use of PrEP. Parents supported PrEP availability acknowledging the risks faced by AGYW.58 However, support was also influenced by social norms (promoting promiscuity or condoning sexual activity). Differential parenting roles influenced the type of support: mothers suggested providing a conducive environment (good diet) for PrEP use while fathers suggested providing operational support (transport money). Cremin et al and Irungu et al reported that providing time-limited PrEP during periods of increased exposure would be a novel, efficient and cost-effective strategy for providing PrEP.55 56
Discussion
The purpose of this review was to synthesise and appraise the effects on PrEP initiation and the acceptability and feasibility of PrEP SDMs designed to promote linkage to care among AGYW and men eligible for PrEP in SSA. Given the challenging interactions between AGYW and men and the health system, we reviewed evidence of PrEP initiation in a range of SDMs that is, health facility, mobile, community based or hybrid models, and we explored the perceptions, barriers and facilitators of these models. This scoping review identified 27 primary studies and 10 conference abstracts.
Delivery of PrEP to AGYW included HF-B models which integrated PrEP into routine FP/MCH/ SRH/ANC services, hybrid models which allowed AGYW to initiate PrEP either at community-based venues or private or public facilities and mobile models. Whereas integrated models provided at a public health facility offer a potential ‘one-stop’ location for AGYW to initiate PrEP while accessing other services, the additional time spent on PrEP-related activities may deter AGYW from initiation. Roche et al found in a study on integrated PrEP-FP service delivery that youth-friendly clinics are ‘low-hanging fruit’ for PrEP delivery. The youth-friendly approach and clinic flow implemented at one of the clinics required less room-to-room movement thus making PrEP delivery to AGYW easier. The second clinic which offered PrEP like any other outpatient service, with clients receiving HIV testing services at HTS points, PrEP counselling and clinical review in consultation rooms, and prescription dispensing at the pharmacy was not favoured by AGYW who did not want to queue at each service point and discuss their sexual activity in crowded FP consultation rooms.59 Integrated delivery of PrEP provides an opportunity to respond to potential syndemics in AGYW who are eligible for PrEP; however, we found mixed results regarding the effectiveness of integrated models on PrEP initiation. Two studies in which PrEP was initiated in an FP or MCH clinic showed PrEP initiation of <50% with initiation being higher in women >24 years.29 30 A third multicountry study which integrated PrEP with SRHS at FP clinics showed 90% PrEP initiation.28 These studies were primarily implementation studies without a comparator, and PrEP-related activities were provided by a PrEP-dedicated nurse. This task-shifting strategy removed this additional service from the workload of already overburdened routine nurses; however, the feasibility of this approach requires further evaluation considering the human resources challenges in SSA. Integration of HIV services and other health services has shown to be a useful strategy to improve linkage to HIV care, ART initiation and viral suppression. The most common forms of integration were (1) HIV testing and counselling added to non-HIV services and (2) non-HIV services added to ART. The most commonly integrated non-HIV services were maternal and child healthcare, tuberculosis testing and treatment, primary healthcare, FP and SRHSs.60 Innovative adaptations are needed at public primary health facility level to overcome PrEP delivery challenges and barriers that are faced by users and staff. Irungu et al reported adaptations within integrated models such as fast tracking PrEP users to minimise waiting times and clinicians dispensing PrEP from clinical rooms which removed waiting times at the pharmacy and mitigated any stigma associated with being seen at a pharmacy that mainly dispenses ART.61
Adolescent-friendly clinics or adolescent-friendly sections within health facilities were also shown to promote initiation of PrEP.27 28 37 However, a New York study of adolescents’ PrEP awareness showed that 86% of adolescents eligible for PrEP reported never being informed about PrEP by their healthcare professionals.62 Taggart et al found that provider attitudes and recommendations within a healthcare facility influence adolescents’ willingness or unwillingness to use PrEP.63 Our results show that AGYW favour community-based youth-friendly delivery modalities of PrEP such as DICEs or schools over delivery via public and private health facilities. These findings concur with other studies which have shown that factors that influence US women’s decision-making about the use of PrEP include the ease of accessing services and medication close to their homes.64 65 Moreover, women highlighted the importance of community peers in influencing their decisions to initiate PrEP.65
We identified only one study among young, heterosexual men that explored the hypothetical perceptions of PrEP initiation. Men reported that if PrEP was available, they would use it. However, initiation was dependent on SDM and a HF-B model was not favoured due to community stigma.23 Heterosexual men are not classified as a key or vulnerable population in the HIV prevention response, as such research that focuses on PrEP initiation or SDMs among heterosexual men is limited. Increasing the engagement of men with health services requires an understanding of the structural barriers that limit their access and requires targeted and adaptive interventions to meet the needs of men. Differentiated SDMs (eg, facility-based and/or community-based adherence clubs and quick pharmacy pick-up) has been shown to improve uptake and retention of men in HIV treatment services.66 Gender-transformative interventions such as ‘One Man Can’, a rights-based gender equality and health programme intervention, and Decentralised Medication Delivery have also shown success in reducing masculinity-related barriers to engaging in HIV prevention services.67 A recent study conducted in South Africa revealed that these differentiated SDMs have the potential to increase adherence to medication among men in particular.68 Other interventions/ models designed to help South African men initiate ART and remain in care such as the MINA and Coach Mpilo campaigns, which provide men with information and support that help them to get tested for HIV, to initiate and remain in care, could also be used to promote PrEP initiation among men.69 70
In studies that targeted both women (including AGYW) and men, SDMs included a hybrid approach (research site-community or community-health facility), community-based models and those based at research sites. PrEP delivery to serodiscordant couples involved integrated models such as delivery of PrEP and ART to serodiscordant couples allows both partners to interact with the health system. In such models, PrEP is initiated and continued only until the HIV infected partner achieves viral suppression which may be a cost-effective approach if viral suppression is achieved timeously.38 However, in a sub-Saharan setting where <65% of people living with HIV have suppressed viral load (VL) (<1000 copies/mL) and there are health systems challenges with VL testing and turn-around-time, integrated delivery of PrEP and ART may not be feasible.1 71 Our findings have shown that community-based models which involve same-day HIV testing and PrEP initiation are favourable especially among men.41 Furthermore, the delivery of PrEP through innovative community-based venues such as hair salons which provided a comfortable and familiar environment yielded high interest in PrEP initiation.45 Many participants reported the convenience of pharmacies located close to public transport routes, as many did not have access to cars or did not want to bear the cost of fuel incurred travelling to the clinic.72
Both AGYW, men and serodiscordant couples have expressed that PrEP initiation is influenced by the setting, that is, a friendly environment and by the attitude of healthcare workers, that is, non-judgemental/non-stigmatising.28 43 This suggests that the successful delivery of PrEP to AGYW or men using HF-B models either through integrated or standalone approaches requires healthcare workers to play an essential role.73 74 Structural barriers to PrEP initiation included: the distance to travel to and time spent at health facilities. To address these barriers, there is an increasing need for differentiated SDMs that provide alternative access options especially considering that PrEP is a prevention intervention delivered to individuals who are generally of good health and who may be disinclined to travel long distances and wait in long queues to access PrEP.75
Policy and programme recommendations and future research areas
Notably, literature on PrEP SDMs for AGYW and more especially heterosexual men is limited thus calling for more research in these areas. In order to increase PrEP initiation, country programme implementers need to understand which SDM/s work for AGYW or men and to adapt these to best suit the unique needs of the users.76 Opportunities exist for integrated strategies of PrEP delivery at a health facility or mobile clinic. However, we need to understand which integrated strategy (eg, integration with ART, SRHS or contraceptive services) is most acceptable and scalable for AGYW and men. Further research is needed among couples where one partner is on PrEP, to understand if the perception of risk changes in the partner who is not on PrEP. We identified only one conference abstract that targeted PrEP SDM among heterosexual men. This study was also limited as PrEP was not provided, but hypothetical perceptions of PrEP were assessed. This dearth of published literature highlights a major gap in the knowledge with considerably more research needed to investigate SDMs among men. Training and retraining of healthcare workers on PrEP guidelines is essential to equip them with the skills to ensure that PrEP is delivered in a friendly and safe space by non-stigmatising healthcare workers. To mitigate the time burden and travel expenses incurred by AGYW and men, same-day initiation of PrEP to those eligible and multi-months dispensing of refills should be considered.11 75 77
Furthermore, task-shifting among healthcare workers along the PrEP cascade will avoid additional burden on the health system. Further studies are required to evaluate the feasibility of PrEP-dedicated nurses. Differentiated SDMs are needed to take PrEP to where users live, socialise and work.11 These models include home deliveries, pharmacies, DICEs, salons, mobile clinics and telemedicine-assisted models in both the public and private health sectors. Mobile clinics near schools could be successful but need to be regular, reliable and sustainable. Furthermore, considering that eligibility for continuation on PrEP requires repeat HIV testing, there is a need for interventions (eg, HIV self-testing) to address this challenge when PrEP is delivered at non- HF-B settings.
Strengths and limitations
The strengths of this review include the inclusion of multiple databases across disciplines and broad inclusion criteria. We also used a comprehensive search strategy that followed the JBI reviewer’s manual and structured using PRISMA-ScR guidelines, and robust methods that included double data screening, extraction and review. Another strength is that we included grey literature and unpublished reports which minimises the chances of missing studies with negative or null findings.
Limitations include the exclusion of studies conducted in non-SSA and that were published in non-English languages. In addition, due to a lag in adding and indexing articles in various online databases, our review could fail to locate the most recent publications and research on SDMs for PrEP initiation. Another limitation was that most of the included studies were from three countries (Kenya, Uganda and South Africa) hence the generalisability of the results to SSA might be limited. Furthermore, there were limitations in the sources of evidence as many of the studies evaluated the hypothetical perceptions of PrEP initiation and some of the feasibility and acceptability is theoretical which may not translate to actual realities. Additionally, sub analyses specifically for heterosexual men could not be done since results from some of the studies were not disaggregated by gender. Also, the extraction focuses on synthesising the setting where PrEP is offered, which is only one component of the SDM and does not focus on other components such as the strategies or individuals providing PrEP. Due to the dearth of literature on SDMs among AGYW and men and considering that PrEP roll-out in this population in many SSA countries has only recently been maximised, we included research studies to understand the SDMs in this setting. Although the recruitment criteria in a research setting may have resulted in a higher initiation of PrEP, the lessons learnt from this setting could contribute to improving the roll-out of PrEP in AGYW and men. Critical appraisal of evidence from conference abstracts was limited by the information provided in the abstract. As such, many items for conference abstracts on the CASP tool were adjudicated as cannot tell or unclear risk.
Conclusions
We conducted a scoping review on PrEP SDMs, summarising evidence on PrEP initiation using existing models among AGYW and men and explored the users’ perceptions, and barriers and facilitators of these PrEP models. These models were mostly found to be hybrid approaches (research site-health facility or community-health facility), community-based or based at a research site. Community-based models at convenient locations were favoured by AGYW. Integrated strategies delivered at friendly health facilities by non-stigmatising healthcare providers was also a preferred PrEP delivery channel. The successful initiation of PrEP by AGYW and men will be dependent on the service setting where it is offered and cannot be considered as a one size fits all approach. Care must be taken to find the delivery method best suited to each subpopulation. Future research should focus on what differentiated SDMs work for AGYW and heterosexual men to identify which approach is most successful in improving PrEP initiation and to understand their individual needs when using these models.
Supplementary Material
Footnotes
TR and WC contributed equally.
Contributors: All authors contributed to conceptualising and designing the study. TR and WC conducted the literature search. WC, TR, KJ, NJ and DG independently performed screening. WC, TR, CM, EN, EBT, MH, TMA, NJ, DG, BZ, WB and FCM independently performed data extraction. EN developed the data charting form on REDCap. TR and WC performed initial data synthesis and interpretation and all authors refined it. WC and TR drafted the manuscript. All authors contributed to writing and reviewing the manuscript. EN is the guarantor for the manuscript.
Funding: This work was supported by the US President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centres for Disease Control and Prevention, under the terms of Cooperative Agreement Number 1 NU2GGH002193-01-00.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The scoping review focuses on published research in the public domain therefore no ethics approval is required.
References
- 1.UNAIDS . AIDSinfo. 2020. Available: https://aidsinfo.unaids.org/ [Accessed 21 Apr 2020].
- 2.UNAIDS . We’ve got the power: women, adolescent girls and the HIV response 2019. Available: https://www.unaids.org/sites/default/files/media_asset/2020_women-adolescent-girls-and-hiv_en.pdf [Accessed 21 Apr 2020].
- 3.Pascoe L, Peacock D, Stemple L. Reaching men: addressing the blind spot in the HIV response. IJMSCH 2018;1:e57–70. 10.22374/ijmsch.v1iSP1.3 [DOI] [Google Scholar]
- 4.Colvin CJ. Strategies for engaging men in HIV services. Lancet HIV 2019;6:e191–200. 10.1016/S2352-3018(19)30032-3 [DOI] [PubMed] [Google Scholar]
- 5.UNAIDS . HIV prevention 2020 road map. Geneva: Joint United Nations Programme on HIV, 2017. Available: https://www.unaids.org/sites/default/files/media_asset/hiv-prevention-2020-road-map_en.pdf [Google Scholar]
- 6.World Health Organization . Guidance on pre-exposure oral prophylaxis (prep) for serodiscordant couples, men who have sex with men and transgender women at high risk of HIV. Geneva: World Health Organization, 2012. [PubMed] [Google Scholar]
- 7.World Health Organization . Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. Geneva Switzerland: World Health Organization, 2016. [PubMed] [Google Scholar]
- 8.Dunbar MS, Kripke K, Haberer J, et al. Understanding and measuring uptake and coverage of oral pre-exposure prophylaxis delivery among adolescent girls and young women in Sub-Saharan Africa. Sex Health 2018;15:513–21. 10.1071/SH18061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ajayi AI, Mudefi E, Yusuf MS, et al. Low awareness and use of pre-exposure prophylaxis among adolescents and young adults in high HIV and sexual violence prevalence settings. Medicine (Baltimore) 2019;98:e17716. 10.1097/MD.0000000000017716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Department of Health South Africa . Guidelines for expanding combination prevention and treatment options: oral pre-exposure prophylaxis (prep) and test and treat (T&T). 2017. [Google Scholar]
- 11.O’Malley G, Barnabee G, Mugwanya K. Scaling-up PreP delivery in sub-Saharan Africa: what can we learn from the scale-up of art? Curr HIV/AIDS Rep 2019;16:141–50. 10.1007/s11904-019-00437-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Venter WDF. Pre-exposure prophylaxis: the delivery challenge. Front Public Health 2018;6:188. 10.3389/fpubh.2018.00188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 14.Mays N, Roberts E, Popay J. Synthesising research evidence. 2001. [Google Scholar]
- 15.Aromataris E, Munn Z, eds. Joanna briggs institute reviewer’s manual. The Joanna Briggs Institute, 2017. [Google Scholar]
- 16.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-scr): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 17.EndNote [program . EndNote X7 version. Philadelphia, PA: Clarivate, 2013. [Google Scholar]
- 18.Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile APP for systematic reviews. Syst Rev 2016;5:210. 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (redcap) -- a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cochrane Effective Practice and Organisation of Care (EPOC) . Suggested risk of bias criteria for EPOC reviews. EPOC resources for review authors. 2017. Available: https://protect-za.mimecast.com/s/vgZ1C8qzwAFjg8EMIndz5c [Accessed 1 Apr 2020].
- 21.Critical Appraisal Skills Programme . Qualitative checklist. 2018. Available: https://casp-uk.net/casp-tools-checklists/ [Accessed 1 Apr 2020].
- 22.Lewin S, Langlois E, Tuncalp Ö, et al. WEIRD (ways of evaluating important and relevant data) tool: questions to guide assessment / critical appraisal of programme descriptions, implementation descriptions and other mainly descriptive types of evidence. Oslo: Norwegian Institute of Public Health, 2019. Available: https://epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/Resources-for-authors2017/weird_tool.pdf [Google Scholar]
- 23.Bell J, Sharma S, Hasen N, et al. Awareness of prep and drivers and barriers to use among men aged 20-34 in Mpumalanga and Kwazulu-Natal South Africa [abstract]. IAS 2019; Mexico City, Mexico, 2019 [Google Scholar]
- 24.Koss CA, Ayieko J, Owaraganise A, et al. Survey of early barriers to prep uptake among clients and community members in the SEARCH study in rural Kenya and Uganda [abstract]. IAS 2017; Paris, France, 2017 [Google Scholar]
- 25.Atujuna M, Newman PA, Wallace M, et al. Contexts of vulnerability and the acceptability of new biomedical HIV prevention technologies among key populations in South Africa: a qualitative study. PLoS One 2018;13:e0191251. 10.1371/journal.pone.0191251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ong’wen P, Musau A, D W, et al. Adolescent girls on prep: findings from kenya’s oral prep scale-up supported by Jilinde [abstract]. IAS 2019; Mexico City, Mexico, 2019 [Google Scholar]
- 27.Rousseau E, Baeten J, Morton J, et al. Association between contraceptive use and prep uptake and continuation in adolescent girls and young women in Cape Town, South Africa [abstract]. IAS 2019; Mexico City, Mexico, 2019 [Google Scholar]
- 28.Travill D, Bekker L, Delany-Moretlwe S, et al. Sexual behavior and prep uptake among young african women in a demonstration project about prep delivery [abstract]. AIDS 2018; Amsterdam, Netherlands, 2018 [Google Scholar]
- 29.Mugwanya KK, Pintye J, Kinuthia J, et al. Integrating preexposure prophylaxis delivery in routine family planning clinics: a feasibility programmatic evaluation in Kenya. PLoS Med 2019;16:e1002885. 10.1371/journal.pmed.1002885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kinuthia J, Pintye J, Abuna F, et al. Pre-exposure prophylaxis uptake and early continuation among pregnant and post-partum women within maternal and child health clinics in kenya: results from an implementation programme. Lancet HIV 2020;7:e38–48. 10.1016/S2352-3018(19)30335-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pintye J, Kinuthia J, Roberts DA, et al. Brief report: integration of PreP services into routine antenatal and postnatal care: experiences from an implementation program in Western Kenya. J Acquir Immune Defic Syndr 2018;79:590–5. 10.1097/QAI.0000000000001850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ngure K, Velloza J, Patel RC, et al. Alignment of PreP use and effective contraceptive use among East African women in HIV serodiscordant partnerships. Int J STD AIDS 2020;31:1263–71. 10.1177/0956462420951501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Were D, Musau A, Mutegi J, et al. Using a HIV prevention cascade for identifying missed opportunities in prep delivery in Kenya: results from a programmatic surveillance study. J Int AIDS Soc 2020;23 Suppl 3:e25537. 10.1002/jia2.25537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Delany-Moretlwe S, Chersich M, Harvey S, et al. Empowerment clubs did not increase prep continuation among adolescent girls and young women in South Africa and Tanzania - results from the EMPOWER randomised trial [abstract]. AIDS 2018; Amsterdam, Netherlands, 2018 [Google Scholar]
- 35.Donnell D, Beesham I, Welch JD, et al. Incorporating oral prep into standard prevention services for South African women: a nested interrupted time-series study. The Lancet HIV 2021;8:e495–501. 10.1016/S2352-3018(21)00048-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hill LM, Maseko B, Chagomerana M, et al. HIV risk, risk perception, and prep interest among adolescent girls and young women in Lilongwe, Malawi: operationalizing the prep cascade. J Int AIDS Soc 2020;23 Suppl 3:e25502. 10.1002/jia2.25502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maseko B, Hill LM, Phanga T, et al. Perceptions of and interest in HIV pre-exposure prophylaxis use among adolescent girls and young women in Lilongwe, Malawi. PLoS One 2020;15:e0226062. 10.1371/journal.pone.0226062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Heffron R, Ngure K, Odoyo J, et al. Pre-exposure prophylaxis for HIV-negative persons with partners living with HIV: uptake, use, and effectiveness in an open-label demonstration project in East Africa. Gates Open Res 2017;1:3. 10.12688/gatesopenres.12752.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Koss CA, Ayieko J, Mwangwa F, et al. Early adopters of human immunodeficiency virus preexposure prophylaxis in a population-based combination prevention study in rural Kenya and Uganda. Clin Infect Dis 2018;67:1853–60. 10.1093/cid/ciy390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mayer CM, Owaraganise A, Kabami J, et al. Distance to clinic is a barrier to PreP uptake and visit attendance in a community in rural Uganda. J Int AIDS Soc 2019;22:e25276. 10.1002/jia2.25276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Koss CA, Charlebois ED, Ayieko J, et al. Uptake, engagement, and adherence to pre-exposure prophylaxis offered after population HIV testing in rural Kenya and Uganda: 72-week interim analysis of observational data from the search study. Lancet HIV 2020;7:e249–61. 10.1016/S2352-3018(19)30433-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Camlin CS, Koss CA, Getahun M, et al. Understanding demand for prep and early experiences of prep use among young adults in rural Kenya and Uganda: a qualitative study. AIDS Behav 2020;24:2149–62. 10.1007/s10461-020-02780-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ngure K, Heffron R, Curran K, et al. I knew I would be safer. experiences of kenyan HIV serodiscordant couples soon after pre-exposure prophylaxis (prep) initiation. AIDS Patient Care STDS 2016;30:78–83. 10.1089/apc.2015.0259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gombe MM, Cakouros BE, Ncube G, et al. Key barriers and enablers associated with uptake and continuation of oral pre-exposure prophylaxis (prep) in the public sector in Zimbabwe: qualitative perspectives of general population clients at high risk for HIV. PLoS One 2020;15:e0227632. 10.1371/journal.pone.0227632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bassett IV, Govere S, Millham L, et al. Contraception, HIV services, and PreP in South African hair salons: a qualitative study of owner, stylist, and client perspectives. J Community Health 2019;44:1150–9. 10.1007/s10900-019-00698-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bassett IV, Xu A, Govere S, et al. Contraception and prep in South African hair salons: owner, stylist, and client views. J Acquir Immune Defic Syndr 2018;79:e78–81. 10.1097/QAI.0000000000001794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lubwama J, Alamo S, Ajulong C, et al. Preexposure prophylaxis for key populations in uganda: early scale-up lessons [abstract]. CROI 2019; Seattle, Washington, 2019 [Google Scholar]
- 48.Baeten JM, Heffron R, Kidoguchi L, et al. Integrated delivery of antiretroviral treatment and pre-exposure prophylaxis to HIV-1–serodiscordant couples: a prospective implementation study in Kenya and Uganda. PLoS Med 2016;13:e1002099. 10.1371/journal.pmed.1002099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Heffron R, Ngure K, Velloza J, et al. Implementation of a comprehensive safer conception intervention for HIV-serodiscordant couples in Kenya: uptake, use and effectiveness. J Int AIDS Soc 2019;22:e25261. 10.1002/jia2.25261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Heffron R, Thomson K, Celum C, et al. Fertility intentions, pregnancy, and use of PreP and art for safer conception among East African HIV serodiscordant couples. AIDS Behav 2018;22:1758–65. 10.1007/s10461-017-1902-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Morton JF, Myers L, Gill K, et al. Evaluation of a behavior-centered design strategy for creating demand for oral PreP among young women in Cape town, South Africa. Gates Open Res 2020;4:29. 10.12688/gatesopenres.13103.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ware NC, Pisarski EE, Nakku-Joloba E, et al. Integrated delivery of antiretroviral treatment and pre-exposure prophylaxis to HIV-1 serodiscordant couples in East Africa: a qualitative evaluation study in Uganda. J Int AIDS Soc 2018;21:e25113. 10.1002/jia2.25113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sack DE, De Schacht C, Paulo P, et al. Pre-Exposure prophylaxis use among HIV serodiscordant couples: a qualitative study in Mozambique. Glob Health Action 2021;14:1940764. 10.1080/16549716.2021.1940764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Minnis AM, Atujuna M, Browne EN, et al. Preferences for long-acting pre-exposure prophylaxis (PreP) for HIV prevention among South African youth: results of a discrete choice experiment. J Int AIDS Soc 2020;23:e25528. 10.1002/jia2.25528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cremin I, Morales F, Jewell BL, et al. Seasonal prep for partners of migrant miners in southern mozambique: a highly focused prep intervention. J Int AIDS Soc 2015;18:19946. doi:19946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Irungu EM, Sharma M, Maronga C, et al. The incremental cost of delivering PreP as a bridge to art for HIV serodiscordant couples in public HIV care clinics in Kenya. AIDS Res Treat 2019;2019:4170615. 10.1155/2019/4170615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jani N, Pilgrim N, Saria V, et al. Will male partners of adolescent girls and young women (AGYW) support their prep use? A comparative analysis of AGYW and male partners of AGYW views in Tanzania [abstract]. AIDS 2018; Amsterdam, Netherlands, 2018 [Google Scholar]
- 58.Makyao N, Saria V, Jani N, et al. How will social norms about parenting influence parental support of adolescent girls and young women’s (AGYW) use of prep? Perspectives from parents in Tanzania [abstract]. AIDS 2018; Amsterdam, Netherlands, 2018 [Google Scholar]
- 59.Roche SD, Barnabee G, Omollo V, et al. Implementation strategies for integrating pre-exposure prophylaxis for HIV prevention and family planning services for adolescent girls and young women in Kenya: a qualitative study. BMC Health Serv Res 2022;22:422. 10.1186/s12913-022-07742-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bulstra CA, Hontelez JAC, Otto M, et al. Integrating HIV services and other health services: a systematic review and meta-analysis. PLoS Med 2021;18:e1003836. 10.1371/journal.pmed.1003836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Irungu E, Ngure K, Mugwanya K, et al. Surmounting PrEP delivery challenges through adaptation of implementation guidelines: lessons learned from HIV care clinics in kenya [The Atrium, Southern Gate, Chichester PO19 8SQ, W Sussex, England: John Wiley & Sons Ltd]. J Int AIDS Soc 2019;22:89. [Google Scholar]
- 62.Santos RP, Adams ME, Lepow M, et al. 1288. adolescents’ knowledge and acceptance of pre-exposure prophylaxis (prep) in the capital district region of New York. Open Forum Infect Dis 2018;5:S393–4. 10.1093/ofid/ofy210.1121 [DOI] [Google Scholar]
- 63.Taggart T, Liang Y, Pina P, et al. Awareness of and willingness to use PreP among black and latinx adolescents residing in higher prevalence areas in the United States. PLoS One 2020;15:e0234821. 10.1371/journal.pone.0234821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Aaron E, Blum C, Seidman D, et al. Optimizing delivery of HIV preexposure prophylaxis for women in the United States. AIDS Patient Care STDS 2018;32:16–23. 10.1089/apc.2017.0201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Auerbach JD, Kinsky S, Brown G, et al. Knowledge, attitudes, and likelihood of pre-exposure prophylaxis (PreP) use among US women at risk of acquiring HIV. AIDS Patient Care STDS 2015;29:102–10. 10.1089/apc.2014.0142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mukumbang FC. Leaving no man behind: how differentiated service delivery models increase men’s engagement in HIV care. Int J Health Policy Manag 2021;10:129–40. 10.34172/ijhpm.2020.32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fleming PJ, Colvin C, Peacock D, et al. What role can gender-transformative programming for men play in increasing men’s HIV testing and engagement in HIV care and treatment in South Africa? Cult Health Sex 2016;18:1251–64. 10.1080/13691058.2016.1183045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fox MP, Pascoe S, Huber AN, et al. Adherence clubs and decentralized medication delivery to support patient retention and sustained viral suppression in care: results from a cluster-randomized evaluation of differentiated art delivery models in South Africa. PLoS Med 2019;16:e1002874. 10.1371/journal.pmed.1002874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hlongwa M, Cornell M, Malone S, et al. Uptake and short-term retention in HIV treatment among men in South Africa: the coach mpilo pilot project. Glob Health Sci Pract 2022;10:e2100498. 10.9745/GHSP-D-21-00498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.The Aurum Institute . Men’s health month: aurum partners to implement campaigns supporting men living with HIV. 2021. Available: https://www.auruminstitute.org/component/content/article/28-blog/aurum-news/455-men-s-health-month-mina-and-coach-mpilo-fight-the-stigma-for-men-living-with-hiv?Itemid=101 [Accessed 26 Nov 2021].
- 71.Lecher S, Williams J, Fonjungo PN, et al. Progress with scale-up of HIV viral load monitoring — seven sub-Saharan African countries, January 2015–June 2016. MMWR Morb Mortal Wkly Rep 2015;65:1332–5. 10.15585/mmwr.mm6547a2 [DOI] [PubMed] [Google Scholar]
- 72.Smith DK, Toledo L, Smith DJ, et al. Attitudes and program preferences of African-American urban young adults about pre-exposure prophylaxis (PreP). AIDS Educ Prev 2012;24:408–21. 10.1521/aeap.2012.24.5.408 [DOI] [PubMed] [Google Scholar]
- 73.Rubtsova A, Wingood GM, Dunkle K, et al. Young adult women and correlates of potential adoption of pre-exposure prophylaxis (PreP): results of a national survey. Curr HIV Res 2013;11:543–8. 10.2174/1570162x12666140129104952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wingood GM, Dunkle K, Camp C, et al. Racial differences and correlates of potential adoption of preexposure prophylaxis: results of a national survey. J Acquir Immune Defic Syndr 2013;63 Suppl 1:S95–101. 10.1097/QAI.0b013e3182920126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sullivan PS, Mena L, Elopre L, et al. Implementation strategies to increase prep uptake in the south. Curr HIV/AIDS Rep 2019;16:259–69. 10.1007/s11904-019-00447-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mugo NR, Ngure K, Kiragu M, et al. PrEP for Africa: what we have learnt and what is needed to move to program implementation. Curr Opin HIV AIDS 2016;11:80. 10.1097/COH.0000000000000224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Siegler AJ, Steehler K, Sales JM, et al. A review of HIV pre-exposure prophylaxis streamlining strategies. Curr HIV/AIDS Rep 2020;17:643–53. 10.1007/s11904-020-00528-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.World Bank . Sub-saharan africa. 2019. Available: https://data.worldbank.org/region/sub-saharan-africa [Accessed 25 Nov 2019].
- 79.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-061503supp001.pdf (77.9KB, pdf)
bmjopen-2022-061503supp002.pdf (255.6KB, pdf)
bmjopen-2022-061503supp003.pdf (79.4KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information.