Abstract
Background
Traumatic spinal cord injury (TSCI) is a highly fatal and disabling event, and its incidence rate is increasing in China. Therefore, we collated the epidemiological factors of TSCI in different regions of China to update the earlier systematic review published in 2018.
Method
We searched four English and three Chinese electronic databases from 1978 to October 1, 2022. From the included reports, information on sample characteristics, incidence, injury characteristics, prognostic factors, and economic burden was extracted. The selection of data was based on the PRISMA statement. The quality of the included studies was assessed by the Agency for Healthcare Research and Quality (AHRQ) tool. The results of the meta-analysis were presented in the form of pooled frequency and forest plots.
Results
A total of 59 reports (60 studies) from 23 provinces were included, of which 41 were in the Chinese language. The random pooled incidence of TSCI in China was estimated to be 65.15 per million (95% CI: 47.20–83.10 per million), with a range of 6.7 to 569.7 per million. The pooled male-to-female ratio was 1.95:1. The pooled mean age of the cases at the time of injury was 45.4 years. Motor vehicle accidents (MVAs) and high falls were found to be the leading causes of TSCI. Incomplete quadriplegia and AISA/Frankel grade D were the most common types of TSCI. Cervical level injury was the most prevalent. The pooled in-hospital mortality and complication rates for TSCI in China were 3% (95% CI: 2–4%) and 35% (95% CI: 23–47%). Respiratory problems were the most common complication and the leading cause of death.
Conclusion
Compared with previous studies, the epidemiological data on TSCI in China has changed significantly. A need to update the data over time is essential to implement appropriate preventive measures and formulate interventions according to the characteristics of the Chinese population.
Keywords: traumatic spinal cord injury, epidemiological factors, incidence, China, systematic review and meta-analysis
Introduction
Rationale
Traumatic spinal cord injury (TSCI) is one of the most devastating and catastrophic injury types, with high mortality and disability rates, causing physical and emotional hardship to patients as well as imposing a significant burden on society and families (1–3). TSCI refers to injuries that damage neural structures in the spinal canal, such as the spinal cord, nerve roots, and cauda equine, due to traumatic factors (4). TSCI is usually accompanied by sensory, motor, reflex, defecation, and other dysfunctions (5). Disability resulting from TSCI may be permanent, and medical care may not be sufficient to abrogate it (6). Over the past 40 years, China has witnessed rapid urbanization and an increase in its aging population, which led to a noticeable increase in the TSCI (7–9).
Objectives
This study aims to update the previous research (10) published in 2018 through systematic synthesis and meta-analysis. Toward this goal, we extracted the latest epidemiological data, categorized them based on the geographical divisions of China, and the differences between the North and South regions were evaluated. Additionally, by determining the risk factors for complications or premature death, this study could also improve public awareness of preventive measures and provide a framework for health resource allocation and policy formulation.
Methods
Design
This systematic review and meta-analysis of the literature were performed according to the PRISMA 2020 guidelines (11).
Search strategy
We searched the original peer-reviewed studies from the earliest record in 1978 to October 1, 2022, in the following databases: PubMed, EMBASE, Web of Science, EBSCO, China National Knowledge Infrastructure (CNKI), Wan Fang Data, and the China Science and Technology Journal Database (VIP). The search strategy we employed is described in detail in Supplementary Table 1. We searched all the fields of the database records, combining the relevant epidemiological terms and TSCI-related terms. Since there were too many irrelevant documents in PubMed and EMBASE, we added the restrictive word “human.” Examples of search terms used for searching the Web of Science were: [(“spinal cord injury” or “Traumatic spinal cord injury”) and (epidemiology or incidence or etiology or prevalence) and China)]. We also checked the references of eligible studies, retrieved them, and identified any missing systematic reviews related to TSCI that were missing from the database search. In addition, we collected relevant summaries from the TSCI-related meeting minutes and checked the availability of the full text.
Eligibility criteria
We used the CoCoPop model (condition, context, and population) as the inclusion structure instead of the traditional PICO approach (population, intervention, comparator, and outcome). Because it is more relevant to the issue of incidence and epidemiology (12). The inclusion and exclusion criteria are shown in Table 1.
Table 1.
Summary of inclusion and exclusion criteria.
| Inclusion | Exclusion | |
|---|---|---|
| Context | Any study published in any year, language or setting about TSCI in China | Reviews, animal studies, basic science studies, case reports or studies out of China |
| Population | All ages, occupations and genders | Specific ages (pediatric or geriatric), specific occupations (workers or drivers) |
| Condition | Sample characteristics (number of cases, mean age, male/female ratio, incidence), injury characteristics (etiology, severity of injury), prognostic factors (complications, in-hospital mortality, additional concurrent trauma), economic burden | Specific etiological focus (road traffic injuries, earthquake disaster), unrelated specific topics (depression, sleep disorder), specific injury level (cervical spine injury), non-traumatic spinal cord injury or singe traumatic spinal fracture |
Data selection and collection
Two authors (YH and LL) independently screened the title and abstract of each article according to the inclusion and exclusion criteria. The full text of the selected articles was evaluated, and data was extracted. The third author (TL) rechecked the accuracy and integrity of the extracted data before analysis. Any disagreements were settled by consensus or by the third author (TL).
Data synthesis and analysis
We used the tabular summary method to synthesize the data from the systematic review (12). The “metan” function of STATA software version 16.0 was used to develop a moment-based random model for estimating the hazard ratio, pooled effect of the incidence, percentages of in-hospital mortality, and complications (13). Forest plots were drawn to visualize the heterogeneity and the results of the meta-analysis (14). I2 values obtained by Cochrane's Q test were used to evaluate the heterogeneity. The I2 values of 25, 50, and 75% correspond to low, medium, and high heterogeneity, respectively (15). We also performed a sensitivity analysis using case-by-case exclusion to assess the impact of individual studies on the overall meta-analysis estimates. Due to the high heterogeneity between the studies, we also conducted a subgroup analysis.
Quality assessment
Since all included studies were cross-sectional, two independent authors (YH and LL) evaluated the quality of the included studies using the Agency for Healthcare Research and Quality (AHRQ) tool (Supplementary Table 2). The AHRQ tool assessed the risk of bias in five domains: selection bias, implementation bias, follow-up bias, measurement bias, and reporting bias. Further, it consists of 11 items, with a scoring system of 1 point for “yes” and 0 points for “no” or “unclear.” Based on the scores the studies were categorized as poor quality (0–3 points), medium quality (4–7 points), and good quality (8–11 points) (16). Disagreements, if any, were settled by consensus or by the third author (TL).
Results
Study selection and characteristics
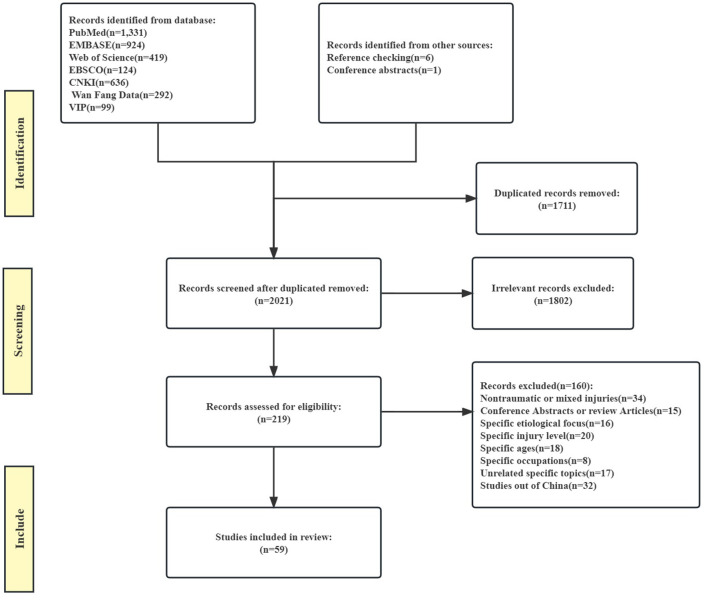
We recognized a total of 3,825 records from the initial database search and pooled them into the EndNote X9 software. The flow diagram of each study stage according to PRISMA guidelines is illustrated in Figure 1. After reviewing the abstract and the full texts, 60 relevant studies were identified (*1–*59, *52 contains two different studies, which were divided into *52A and *52B, see the Supplementary Appendix for the list of references).
Figure 1.
Flow diagram of each study stage.
Methodological quality
We then performed a quality assessment of the included studies. The results of the quality assessment are summarized in Supplementary Table 3. Notably, almost all studies received a ”yes“ for questions on the sources and time of inclusion (items 1, 3). On the contrary, the questions about continuous sources (item 5) and the handling of follow-up and missing data (items 9–11) were answered ”yes“ less frequently. The total study score ranged from 2 to 7, with a median of 4. We assessed each study thoroughly for potential bias and did not exclude any studies.
Sample characteristics
Table 2 displays the basic descriptive features of the 60 studies, including study authors, year of publication, region, incidence period, sample size, source population, source case, male to female ratio, and mean age. The publication period of the included studies spanned 44 years, with 40 studies published in the past 10 years (after 2012). Majority of studies were based on the review of hospital records, except for two studies (*53, *54) which were based on national registers information. The maximum sample size was 54,484 from the Taiwan National Health Insurance (NHI) database (*53), while the smallest sample size was only 35 (*38, *39). The mean age of TSCI cases at the time of injury was between 31.5 and 50.1 years, with a pooled mean age of 45.4 years. In all studies, the proportion of male patients was higher, with a highest male to female ratio of 15.3:1 (*13). And the pooled proportion of male to female ratio was 1.95:1 with a median of 4.0:1. We then extracted the top two occupations of TSCI patients from each study with largest number of TSCI patients, and found that the most vulnerable were workers, followed by farmers.
Table 2.
Sample characteristics and etiology of TSCI in China.
| References | Region | Incidence period | Source population | Case source | Total cases | Leading causes | Second causes | Gender ratio | Mean age | |
|---|---|---|---|---|---|---|---|---|---|---|
| North | Liu et al. (17) | Beijing | 2017–2019 | China rehabilitation research center | Hospitals records | 252 | MVAs | High fall | 4.1:1 | 41.2 |
| Liu et al. (18) | Beijing | 2013–2019 | Beijing Boai Hospital | Hospitals records | 2,448 | Low fall | Assault | 3.0:1 | 39.1 ± 16.7 | |
| Cai et al. (19) | Tianjin | 2013–2017 | Three general hospitals in Tianjin city | Hospitals records | 2,471 | Low fall | High fall | 2.9:1 | 49.2 ± 14.2 | |
| Li et al. (20) | Inner Mongolia | 2012–2019 | The second affiliated hospital of Medical University | Hospitals records | 956 | High fall | MVAs | 2.3:1 | 49.9 ± 20.7 | |
| Wang et al. (21) | Beijing | 2012–2015 | PLA general hospital | Hospitals records | 625 | High fall | MVAs | 4.5:1 | 38.2 ± 12.8 | |
| Liu et al. (22) | Beijing | 2011–2019 | China rehabilitation research center | Hospitals records | 590 | High fall | MVAs | 4.7:1 | 46.3 ± 15.5 | |
| Yuan et al. (23) | Shanxi | 2011–2014 | Yuncheng central hospital | Hospitals records | 58 | MVAs | High fall | 4.0:1 | – | |
| Yang et al. (24) | Beijing | 2009–2014 | The first affiliated hospital of PLA general hospital | Hospitals records | 1,027 | MVAs | High fall | 3.6:1 | 42.5 ± 12.4 | |
| Zhou et al. (25) | Tianjin | 2009–2014 | General Hospital of Tianjin Medical University | Hospitals records | 354 | MVAs | Low fall | 2.3:1 | 50.1 ± 15.5 | |
| Xu et al. (26) | Beijing | 2008–2011 | Beijing Boai Hospital | Hospitals records | 260 | High fall | 9.0:1 | 43.7 | ||
| Wang et al. (27) | Beijing | 2005–2016 | PLA General Hospital | Hospitals records | 1,395 | MVAs | High fall | 4.1:1 | 32.1 ± 12.5 | |
| Ning et al. (28) | Tianjin | 2004–2008 | Major general hospitals in Tianjin city | Hospitals records | 869 | Low fall | MVAs | 5.6:1 | 46.0 ± 14.2 | |
| Jiang et al. (29) | Beijing | 2002–2011 | The 322nd Hospital of the PLA | Hospitals records | 423 | Struck by object | High fall | 15.3:1 | 40.0 ± 11.0 | |
| Hua et al. (30) | Beijing | 2001–2010 | General Hospital of the Chinese Armed Police Force | Hospitals records | 561 | MVAs | High fall | 4.1:1 | 34.7 ± 12.2 | |
| Li et al. (31) | Tianjin | 1999–2016 | General Hospital of Tianjin Medical University | Hospitals records | 735 | MVAs | Low fall | 2.9:1 | 49.7 ± 15.2 | |
| Feng et al. (32) | Tianjin | 1998–2009 | Tianjin Medical University General Hospital | Hospitals records | 239 | Low fall | MVAs | 4.6:1 | 45.4 ± 14.1 | |
| Hao et al. (33) | Beijing | 1992–2006 | China Rehabilitation Research Center and Beijing Boai Hospital | Hospitals records | 1,264 | MVAs | High fall | 4.0:1 | 34.9 | |
| Diao et al. (34) | Beijing | 1982–1986 | A sample of spinal cord patients in Beijing hospitals | Hospitals records | 310 | High fall | Low fall | – | – | |
| Yu et al. (35) | Tianjin | 2007 | Major general hospitals in Tianjin city | Hospitals records | 73 | Low fall | MVAs | 3.6:1 | 51.3 ± 14.6 | |
| Wei et al. (36) | Beijing | 2005 | A sample of spinal cord patients in Beijing hospitals | Hospitals records | 254 | MVAs | High fall | 2.3:1 | 41.0 ± 14.3 | |
| Li et al. (37) | Beijing | 2002 | A sample of spinal cord patients in Beijing hospitals | Hospitals records | 264 | High fall | MVAs | 3.1:1 | 41.7 | |
| Northeast | Liu et al. (38) | Liaoning | 2013–2018 | Seven hospitals in Shenyang and Xi'an | Hospitals records | 2,416 | High fall | Low fall | 2.9:1 | 49.2 ± 14.4 |
| Ru et al. (39) | Liaoning | 2010–2012 | Eight general hospitals in Dalian | Hospitals records | 1,155 | MVAs | Low fall | 2.4:1 | 50.1 ± 15.9 | |
| Xu et al. (40) | Jilin | 2010–2011 | Jilin University Sino–Japanese Friendship Hospital | Hospitals records | 1,274 | Struck by object | High fall | 2.3:1 | 43.6 | |
| Chen et al. (41) | Heilongjiang | 2009–2013 | The Fourth Affiliated Hospital of Harbin Medical University | Hospitals records | 232 | MVAs | High fall | 4.0:1 | 45.4 ± 14.4 | |
| Eastern | Niu et al. (42) | Jiangsu | 2015–2019 | The First Hospital of Soochow University | Hospitals records | 422 | MVAs | High fall | 3.2:1 | 51.1 ± 14.2 |
| Tang et al. (43) | Shandong | 2014–2019 | Affiliated Hospital of Qingdao University | Hospitals records | 332 | – | – | 3.7:1 | 49.2 ± 13.7 | |
| Feng et al. (44) | Shandong | 2013–2017 | Liaocheng Peoples Hospital | Hospitals records | 338 | Low fall | MVAs | 3.1:1 | 50.1 ± 14.1 | |
| Wu et al. (45) | Jiangxi | 2012–2018 | The Affiliated Hospital of Nanchang University | Hospitals records | 1,290 | MVAs | Low fall | 7.1:1 | 53.1 ± 16.2 | |
| Niu et al. (46) | Jiangsu | 2009–2014 | Major general hospitals in Suzhou city | Hospitals records | 859 | High fall | MVAs | 2.4:1 | 47.5 ± 15.5 | |
| Wang et al. (47) | Anhui | 2007–2010 | Two general hospitals in Anhui Province | Hospitals records | 761 | High fall | MVAs | 3.4:1 | 45.0 | |
| Pan et al. (48) | Shanghai | 2005–2007 | Several hospitals in Pudong area | Hospitals records | 200 | High fall | MVAs | 3.0:1 | 44.5 | |
| Yang et al. (49) | Fujian | 2004–2013 | The 175th Hospital of the PLA | Hospitals records | 1,089 | High fall | MVAs | 3.5:1 | 44.7 | |
| Duan et al. (50) | Jiangxi | 2003–2007 | The First Affiliated Hospital of Nanchang University | Hospitals records | 650 | – | – | 2.1:1 | 46.5 | |
| Chen et al. (51) | Shandong | 2002–2007 | Affiliated Hospital of Qingdao University Medical College | Hospitals records | 251 | High fall | MVAs | 3.5:1 | 40.4 | |
| Hu et al. (52) | Shanghai | 1983–1991 | Shanghai Ruijin Hospital and Songjiang County People's Hospital | Hospitals records | 153 | High fall | MVAs | 3.3:1 | 41.3 | |
| Cheng et al. (53) | Shanghai | 1977–2007 | Shanghai Tongji University Hospital | Hospitals records | 676 | High fall | MVAs | 1.7:1 | 42.2 | |
| Sun et al. (54) | Shandong | 2011 | Affiliated Hospital of Qingdao University | Hospitals records | 35 | MVAs | High fall | 10.7:1 | 50.1 | |
| Feng et al. (55) | Jiangsu | 1991 | Six hospitals in Wuxi | Hospitals records | 35 | High fall | Struck by object | 7.8:1 | – | |
| South | Zhang et al. (56) | Guangdong | 2013–2018 | Guangzhou Red Cross Hospital | Hospitals records | 62 | High fall | MVAs | 2.7:1 | 36.0 ± 14.4 |
| Central | Huang et al. (57) | Guangdong | 2012–2016 | Guangdong Work Injury Rehabilitation Hospital | Hospitals records | 397 | High fall | MVAs | 4.0:1 | 40.1 |
| Yi et al. (58) | Hunan | 2012–2014 | Several general hospitals in Hunan | Hospitals records | 1,274 | Low fall | MVAs | 2.3:1 | 43.6 | |
| Deng et al. (59) | Hubei | 2012–2014 | Taihe Hospital Affiliated to Hubei Medical College | Hospitals records | 424 | High fall | MVAs | 1.6:1 | 46.5 | |
| Lv et al. (60) | Henan | 2008–2017 | Henan Provincial People's Hospital | Hospitals records | 692 | MVAs | High fall | 2.6:1 | 46.3 ± 15.9 | |
| Tang et al. (61) | Guangxi | 2006–2010 | Affiliated Hospital of Guangxi Medical University | Hospitals records | 221 | MVAs | High fall | 6.4:1 | 38.3 ± 12.4 | |
| Zhu et al. (62) | Hunan | 2005–2009 | Second Xiangya Hospital, Central South University | Hospitals records | 163 | MVAs | High fall | 3.8:1 | 37.0 ± 10.9 | |
| Yang et al. (63) | Guangdong | 2003–2011 | Several hospitals in Guangdong | Hospitals records | 1,340 | High fall | MVAs | 3.5:1 | 41.6 ± 14.7 | |
| Chen et al. (64) | Guangdong | 1995–2010 | Zhujiang Hospital of Southern Medical University | Hospitals records | 286 | High fall | MVAs | 7.4:1 | 36.3 ± 10.1 | |
| Southwest | Ning et al. (65) | Chongqing | 2009–2013 | Chongqing Xinqiao Hospital | Hospitals records | 554 | High fall | MVAs | 4.3:1 | 45.6 ± 13.8 |
| Mao et al. (66) | Sichuan | 1996–2002 | Huaxi Hospital of Sichuan University | Hospitals records | 132 | MVAs | High fall | 2.5:1 | 31.5 ± 7.8 | |
| Northwest | Hao et al. (67) | Shaanxi | 2011–2013 | Xi'an Honghui Hospital | Hospitals records | 2,565 | Low fall | High fall | 4.7:1 | 41.5 ± 11.2 |
| Zhang et al. (68) | Shaanxi | 2018 | Xi'an Honghui Hospital | Hospitals records | 382 | High fall | Low fall | 3.0:1 | 50.0 ± 15.2 | |
| Taiwan | Yang et al. (69) | Taiwan | 2000–2003 | National Health Insurance (NHI) database | National register | 54,484 | – | – | 1.0:1 | – |
| Wu et al. (70) | Taiwan | 1998–2008 | National Health Insurance (NHI) database | National register | 41,586 | MVAs | High fall | 1.5:1 | – | |
| Chen et al. (71) | Taiwan | 1992–1996 | Medical centers and general hospitals in Taiwan | Hospitals records | 1 586 | MVAs | High fall | 3.0:1 | 46.1 | |
| Lan et al. (72) | Taiwan | 1986–1990 | Four general hospitals in Taiwan | Hospitals records | 99 | MVAs | High fall | 4.0:1 | 44.5 | |
| Chen et al. (73) | Taiwan | 1978–1981 | Medical centers and general hospitals in Taiwan | Hospitals records | 560 | MVAs | High fall | 4.9:1 | 36.2 | |
| Nationwide | Zhang et al. (68) | Whole | 2018 | National stratified whole group sampling | Hospitals records | 4,404 | High fall | Low fall | 3.0:1 | 51.6 ± 15.3 |
| Hao et al. (74) | Whole | 2018 | National stratified whole group sampling | Hospitals records | 4,134 | MVAs | Low fall | 3.0:1 | 50.8 | |
| Jiang et al. (75) | Whole | 2013 | National stratified whole group sampling | Hospitals records | 394 | Low fall | MVAs | 1.9:1 | 43.7 ± 17.1 |
These 60 studies include data from 23 provinces, representing about 1,129.4 million people (2020 census). The remaining 11 regions (Zhejiang, Yunnan, Guizhou, Xinjiang, Hainan, Gansu, Qinghai, Tibet, Ningxia, Hong Kong, and Macau) have not published any epidemiological studies related to TSCI. For the convenience of statistics and search, we categorized the studies into the following groups according to their geographical division: North (*1–*21), Northeast (*22–*25), East (*26–*39), South Central (*40–*48), Southwest (*49–*50), Northwest (*51–*52A), Taiwan (*53–*57), and Nationwide (*52B, *58–*59).
Injury characteristics
Following these preliminary analyses, we looked at the characteristics of the TSCI cases. We found that the most frequent causes of TSCI were motor vehicle accidents (MVAs), which accounted for 40.7% of all the cases, followed by high falls (39.8%). The detailed causes of TSCI are summarized in Table 2. The level of injury was reported in forty-four studies, which showed the majority of injuries occurred at the cervical level, followed by the lumbosacral level (Table 3). Of note, 41 studies used the AISA/Frankel grade in describing injury severity, while 21 studies measured the extent of the injury (complete or incomplete) and the neurological level of the injury (tetraplegia or paraplegia). Eleven studies did not report the severity of injuries. According to 24 studies, AISA D was the most common grade with a highest proportion of 68.4% (*23), followed by grade A, as reported by 13 studies. Further, incomplete injuries were more prevalent than complete injuries, with incomplete quadriplegia being the most common.
Table 3.
Level and severity of TSCI in China.
| References | C (%) | T (%) | L (%) | AISA A (%) | AISA B (%) | AISA C (%) | AISA D (%) | AISA E (%) | IQ (%) | IP (%) | CP (%) | CQ (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Liu et al. (17) | 47.2 | 43.3 | 9.5 | 48.0 | 15.1 | 14.3 | 22.6 | – | – | – | – | – |
| Liu et al. (18) | – | – | – | – | – | – | – | – | – | – | – | – |
| Cai et al. (19) | 63.7 | 21.1 | 15.1 | 37.9 | 9.6 | 13.4 | 39.1 | – | 37.2 | 18.9 | 25.6 | 18.3 |
| Li et al. (20) | 52.9 | 31.5 | 15.6 | 43.5 | 12.5 | 23.0 | 21.0 | – | – | – | – | – |
| Wang et al. (21) | 32.8 | 51.0 | 16.2 | 52.5 | 14.7 | 17.0 | 15.0 | 0.8 | 17.9 | 29.0 | 38.1 | 15.0 |
| Liu et al. (22) | 54.9 | 32.7 | 12.4 | 33.1 | 13.6 | 24.5 | 28.8 | – | – | – | – | – |
| Yuan et al. (23) | 55.0 | 17.0 | 28.0 | 66.0 | 14.0 | 10.0 | 10.0 | – | – | – | – | – |
| Yang et al. (24) | – | – | – | 34.6 | 7.9 | 17.7 | 16.2 | 3.3 | – | – | – | – |
| Zhou et al. (25) | 59.3 | 22.0 | 18.7 | 20.4 | 7.6 | 23.2 | 48.8 | – | – | – | – | – |
| Xu et al. (26) | 14.6 | 53.8 | 31.6 | 80.8 | 16.2 | 3.0 | 0.0 | – | 19.2# | – | 80.8# | – |
| Wang et al. (27) | – | – | – | 52.2 | 11.8 | 15.0 | 21.0 | – | – | – | – | – |
| Ning et al. (28) | 71.5 | – | – | 25.2 | 18.2 | 14.7 | 41.9 | – | – | – | – | – |
| Jiang et al. (29) | – | – | – | 45.4 | 3.1 | 17.7 | 30.0 | 3.8 | – | – | – | – |
| Hua et al. (30) | – | – | – | – | – | – | – | – | – | – | – | – |
| Li et al. (31) | – | – | – | – | – | – | – | – | 52.5 | 23.8 | 8.3 | 15.4 |
| Feng et al. (32) | 82.0 | – | – | 32.6 | 12.1 | 16.3 | 38.9 | 0.0 | 54.4 | 22.6 | 10.1 | 7.9 |
| Hao et al. (33) | 31.5 | 21.4 | 28.1 | – | – | – | – | – | 43.3# | – | 56.7# | – |
| Diao et al. (34) | – | – | – | – | – | – | – | – | – | – | – | – |
| Yu et al. (35) | 83.6 | 9.6 | 6.8 | 26.4 | 11.1 | 18.1 | 43.1 | 1.4 | – | – | – | – |
| Wei et al. (36) | 31.9 | 21.3 | 8.7 | – | – | – | – | – | 46.9# | – | 35.8# | – |
| Li et al. (37) | 4.9 | 28.0 | 66.7 | – | – | – | – | – | – | – | – | – |
| Liu et al. (38) | 55.1 | 29.9 | 14.9 | 29.8 | 5.0 | 10.9 | 54.3 | – | 39.1 | – | – | – |
| Ru et al. (39) | 57.6 | 14.7 | 27.7 | 19.6 | 2.4 | 9.6 | 68.4 | – | 52.7 | 31.5 | 8.3 | 6.3 |
| Xu et al. (40) | 32.5 | 19.5 | 52.8 | – | – | – | – | – | – | – | – | – |
| Chen et al. (41) | 76.3 | 10.3 | 13.4 | 14.2 | 15.1 | 32.8 | 37.9 | – | 63.4 | 18.5 | 5.2 | 12.9 |
| Niu et al. (42) | 69.4 | 12.8 | 17.8 | – | – | 28.7 | 52.1 | – | – | – | – | – |
| Tang et al. (43) | 56.4 | 35.2 | 35.2 | 25.8 | 19.8 | 24.6 | 29.9 | – | – | – | – | – |
| Feng et al. (44) | 77.2 | – | – | 29.3 | 5.3 | 16.3 | 48.5 | 0.6 | – | – | – | – |
| Wu et al. (45) | – | – | – | 13.4 | 19.2 | 27.2 | 40.2 | – | – | – | – | – |
| Niu et al. (46) | 43.2 | 11.5 | 33.9 | 19.4 | 5.2 | 31.5 | 36.9 | 4.2 | – | – | – | – |
| Wang et al. (47) | 46.3 | 20.4 | 33.3 | 25.6 | 11.8 | 27.3 | 35.2 | – | – | – | – | – |
| Pan et al. (48) | 29.0 | 35.0 | 36.0 | 17.5 | 20.0 | 38.5 | 24.0 | – | – | – | – | – |
| Yang et al. (49) | 63.0 | 19.5 | 17.5 | 29.6 | 7.0 | 18.9 | 27.0 | 17.5 | 61.3 | 6.2 | 15.2 | 17.3 |
| Duan et al. (50) | 41.7 | 7.1 | 51.2 | – | – | – | – | – | 51.7# | – | 48.3# | – |
| Chen et al. (51) | 29.1 | 4.8 | 36.7 | 27.1 | 4.0 | 17.5 | 51.4 | – | – | – | – | – |
| Hu et al. (52) | – | – | – | – | – | – | – | – | – | 21.6 | 18.3 | – |
| Cheng et al. (53) | 17.4 | 27.0 | 55.6 | 17.6 | 4.9 | 12.0 | 38.7 | 26.8 | – | – | – | – |
| Sun et al. (54) | – | – | – | 34.3 | 20.0 | 20.0 | 25.7 | – | 65.7# | – | 34.3# | – |
| Feng et al. (55) | 31.4 | 34.3 | 34.3 | 17.1 | 42.9 | 17.1 | 22.9 | – | – | – | – | – |
| Zhang et al. (56) | 53.2 | 30.7 | 16.1 | 27.4 | 22.6 | 12.9 | 21.0 | 16.1 | – | – | – | – |
| Huang et al. (57) | 39.8 | 39.6 | 20.6 | – | – | – | – | – | 85.9# | – | 14.1# | – |
| Yi et al. (58) | 51.7 | 3.8 | 40.7 | 11.5 | 4.0 | 31.9 | 34.9 | 0.4 | 42.5 | 9.2 | 15.2 | 12.3 |
| Deng et al. (59) | 20.2 | 31.5 | 48.3 | 9.4 | 1.7 | 4.5 | 27.8 | 56.6 | – | – | – | – |
| Lv et al. (60) | 70.1 | 11.7 | 17.8 | 24.1 | 19.3 | 15.8 | 40.8 | – | 54.4 | 19.3 | 9.2 | 17.1 |
| Tang et al. (61) | 56.6 | 21.2 | 22.2 | 23.5 | 18.6 | 26.7 | 31.2 | – | – | – | – | – |
| Zhu et al. (62) | 25.2 | 36.2 | 38.7 | 25.2 | 49.1 | 21.5 | 4.3 | – | – | – | – | – |
| Yang et al. (63) | 56.7 | 20.5 | 22.8 | – | – | – | – | – | 73.6# | – | 26.4# | – |
| Chen et al. (64) | 28.7 | 46.9 | 24.4 | – | – | – | – | – | 38.8# | – | 61.2# | – |
| Ning et al. (65) | 54.0 | 30.3 | 15.7 | 39.4 | 8.7 | 21.0 | 30.8 | – | – | – | – | – |
| Mao et al. (66) | – | – | – | 42.0 | 13.0 | 29.0 | 16.0 | – | – | – | – | – |
| Hao et al. (67) | 51.8 | 14.1 | 34.1 | 27.8 | 16.2 | 11.5 | 36.7 | 7.8 | – | – | – | – |
| Zhang et al. (68) | – | – | – | 15.7 | 7.9 | 19.7 | 48.3 | 8.4 | – | – | – | – |
| Yang et al. (69) | – | – | – | – | – | – | – | – | – | – | – | – |
| Wu et al. (70) | – | – | – | – | – | – | – | – | – | – | – | – |
| Chen et al. (71) | 49.9 | 13.3 | 34.6 | – | – | – | – | – | – | – | – | – |
| Lan et al. (72) | – | – | – | – | – | – | – | – | – | – | – | – |
| Chen et al. (73) | 46.8 | – | – | – | – | – | – | – | – | – | – | |
| Zhang et al. (68) | 63.4 | 24.2 | 12.4 | 19.5 | 10.4 | 27.9 | 42.2 | – | 80.4# | – | 19.6# | – |
| Hao et al. (74) | 64.5 | 12.1 | 23.4 | – | – | 28.0 | 43.66 | – | 55.2 | 26.6 | – | – |
| Jiang et al. (75) | – | – | – | – | – | – | – | – | – | – | – | – |
C, Cervical; T, Thoracic; L, Lumbosacral; IQ, Incomplete Quadriplegia; IP, Incomplete Paraplegia; CQ, Complete Quadriplegia; CP, Complete Paraplegia; # means that only complete or incomplete injuries were reported.
AISA A-E; AISA/Frankel grade A-E.
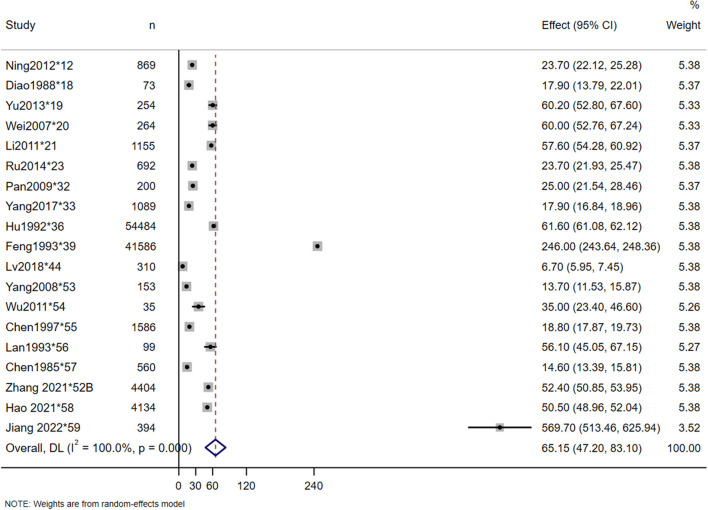
Incidence
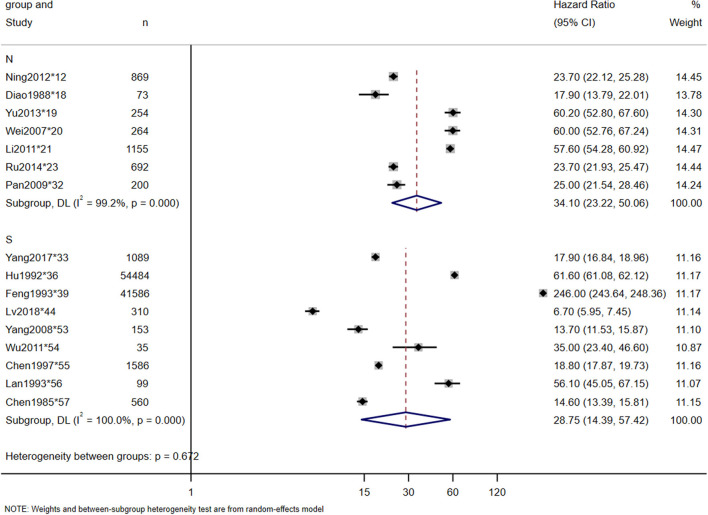
The incidence rates in this study were calculated by dividing the number of new-onset TSCI cases in a given area during a given period of time by the total at-risk population during the same period. A total of 19 studies reported the incidence of TSCI, which ranged from 6.7 per million in 1988 (*18) to 569.7 per million in 2022 (*59). The estimated incidence rate of TSCI in China was 65.15 per million (95% CI: 47.20–83.10 per million, heterogeneity test: I2 = 100%, p-value = 0) (Figure 2). Owing to the high heterogeneity between the studies, we also conducted a North-South subgroup analysis to explore the causes. In the subgroup analysis, a total of 7 and 9 studies were included in the North and South subgroups, respectively, and 3 studies that were conducted nationwide were excluded. The subgroup analyses showed that the incidence of TSCI in the North was 34.10 per million (95% CI: 23.22–50.06 per million, heterogeneity test: I2 = 99.2%, p-value = 0), and in the South was 28.75 per million (95% CI: 14.39–57.42 per million, heterogeneity test: I2 = 100%, p-value = 0) (Figure 3). The hazard ratio's pooled effect was used to estimate the incidence rate. Heterogeneity test between groups: p-value = 0.672. We also performed a sensitivity analysis using case-by-case exclusion, and no study was excluded (Supplementary Figure 1).
Figure 2.
Incidence of TSCI meta-analysis in nationwide.
Figure 3.
Incidence of TSCI meta-analysis in North-South subgroup.
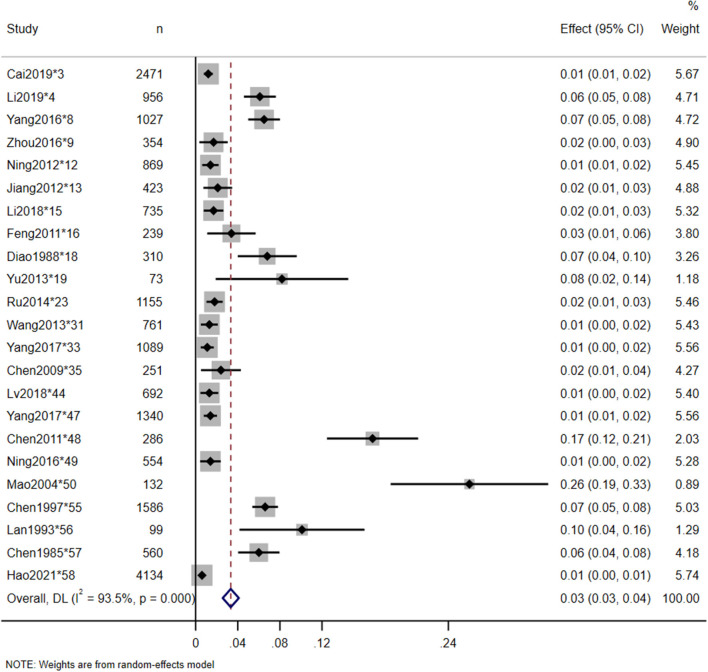
Prognostic factors
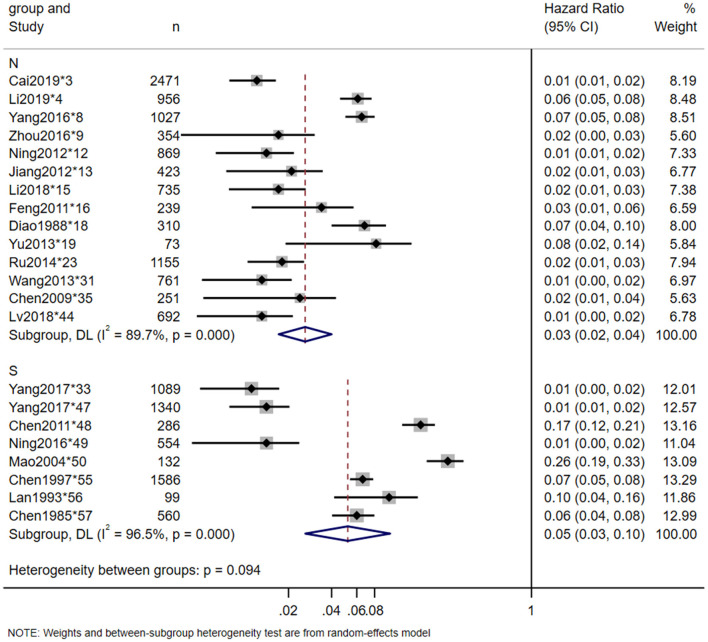
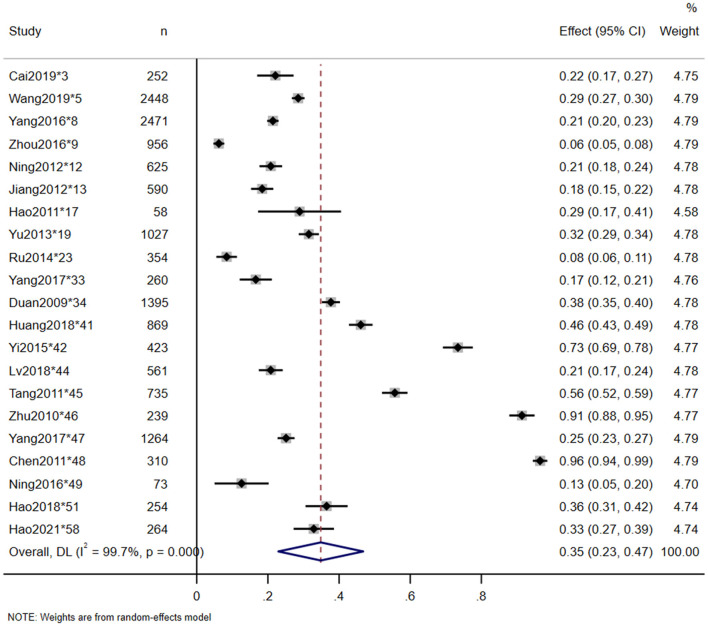
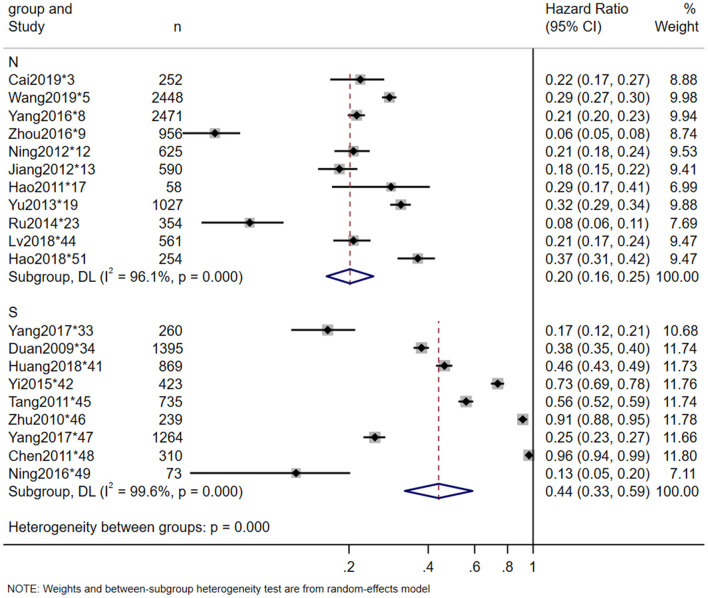
Twenty-three studies reported the in-hospital mortality of TSCI, and 20 studies reported the major causes of death. The pooled estimate for the in-hospital mortality of TSCI in China was 3% (95% CI: 3–4%, heterogeneity test: I2 = 93.5%, p-value = 0) (Figure 4). In the subgroup analysis, the estimation of TSCI in-hospital mortality in the North was 3% (95% CI: 2–4%, heterogeneity test: I2 = 89.7%, p-value = 0), and in the South was 5% (95% CI: 3–10%, heterogeneity test: I2 = 96.5%, p-value = 0). Heterogeneity test between groups: p-value = 0.094 (Figure 5). The most frequent cause of death from TSCI was respiratory failure, as reported by 15 studies. A total of 11 studies mentioned the incidence of additional concurrent trauma, ranging from 51.0% (*15) to 94.6% (*51), the pooled estimate for the proportion of additional concurrent trauma in China was 71% (95% CI: 60–81%, heterogeneity test: I2 = 99.6%, p-value = 0) (Supplementary Figure 2). The main additional concurrent trauma was spinal fracture. Thirty studies mentioned complications from TSCI, among which respiratory diseases and urinary diseases were the most common. Further, 21 studies reported the complication rate of TSCI, ranging from 6.2% (*9) to 96.5% (*48). Our analysis shows that the pooled estimate for the proportion of in-hospital mortality in China was 35% (95% CI: 23–47%, heterogeneity test: I2 = 99.7%, p-value = 0) (Figure 6). Our subgroup analysis in Figure 7, shows that the in-hospital mortality in the North was 20% (95% CI: 16–25%, heterogeneity test: I2 = 96.1%, p-value = 0) and in the South was 44% (95% CI: 33–59%, heterogeneity test: I2 = 99.6%, p-value = 0). Heterogeneity test between groups: p-value = 0. No study was excluded due to sensitivity analysis (Supplementary Figures 3, 4).
Figure 4.
In-hospital mortality of TSCI meta-analysis in nationwide.
Figure 5.
In-hospital mortality of TSCI meta-analysis North-South subgroup.
Figure 6.
Complication rate of TSCI meta-analysis in nationwide.
Figure 7.
Complication rate of TSCI meta-analysis in North-South subgroup.
Economic burden
Twelve studies mentioned the economic burden of TSCI, 10 of which mentioned the average hospitalization costs, ranging from 4.1 thousand RMB in 1988 (*18) to 252.3 thousand RMB in 2020 (*1). The pooled estimate for the economic burden of TSCI was 48.5 thousand RMB.
Discussion
In this study, we conducted the first meta-analysis of the epidemiological data on TSCI in China and updated the previous study published in 2018 (10). We searched 7 databases and identified 59 papers (60 studies), representing 23 provinces and about 1,129.4 million people. Three studies reported epidemiological data through stratified sampling nationwide. While 11 provinces have no reports of TSCI epidemiology, 15 provinces (65.2%) have only 1–2 studies. Among all the reports, 19 studies, all from Beijing and Tianjin, accounted for 31.7% of the total. The imbalance in the number of publications in different provinces has significantly affected the analysis of the national epidemiological data. Taking this disparity into account, along with the difference in economic levels in different regions of China, we conducted a North-South region-wise subgroup analysis to explore the sources of heterogeneity in the meta-analysis. Based on the region, we included thirty-three studies in the northern group and 24 in the southern group. The demarcation between north and south China is often considered to be the Qinling mountain range and the Huaihe river. The economic levels of the North and South had an obvious disparity revealed by the gross domestic product (GDP) of the South, which accounted for about 62% of the national total in 2018. Moreover, the industrial landscape is quite different between these regions. The northern region was biased toward heavy industry, while the southern region vigorously developed the economy through software and internet services industry. However, the net inflow of population in large cities in the southern region is on the rise, presenting a pattern of population flow from north to south, accompanied by a significantly faster urbanization rate compared to the northern region.
Our data points out that the annual incidence of TSCI ranged from 6.7 to 569.7 per million in China, and the random pooled incidence was estimated to be 65.15 per million. The annual incidence of TSCI in China reported in 2018 ranged from 13 to 60 per million (10), while the incidence of TSCI in Asia reported in 2012 ranged from 12.06 to 61.6 per million (76). Furthermore, the global TSCI incidence in 2011 was estimated to be 23 per million (77). Compared with other studies, the incidence of TSCI in China is higher than that in Asia and the rest of the world and still exhibiting an increasing trend. In the subgroup analysis, the estimated incidence of 28.75 per million in the south is lower than that of 34.10 per million in the north and much lower than the national average. This reduction is explained by the exclusion of three nationwide studies, especially the 569.7 per million reported in 2013(*52B). Of note, the industrial structure in the north is biased toward heavy industry, which exposes workers to high-risk environments and could explain the increased incidence of TSCI in the north compared to the south. Coal miners, for example, were the most common occupation for those with TSCI in Tianjin (*13). Comparing the incidence rate of TSCI at different time points in the same province, for example, the incidence rate of Beijing was 6.7 per million (* 18) in 1988 to 60.2 per million (* 20) in 2007, we can find an increasing TSCI incidence over time.
We found that the mean age at the time of injury reported worldwide was 33 years, down from 45.4 years in this study. We also noticed a correlation between increasing age and TSCI when comparing studies conducted in the same province at different time points. This may be related to China's transition toward an aging society, where a higher proportion of people over the age of 35 are engaging in high-risk occupations (78). Moreover, we found that there was a significant gender difference in TSCI incidence. The proportion of male TSCI patients was higher in almost all studies, with the highest male-to-female ratio of 15.3:1 (*13) and the pooled estimate for the male-to-female ratio was 1.95:1. This could be due to male workers engaging in high-risk work, such as truck driving and high-altitude construction work, more than their female counterparts. In addition, male drivers are more likely to engage in risky behaviors. For example, Chen et al. reported violence and alcoholism as potential causes for TSCI (*57).
In our analysis, motor vehicle accidents and high falls were the most common etiologies of TSCI, which was consistent with the 2018 study (10). This is related to the increase in the usage of private cars, urbanization, and the rapid economic growth after a change in China's economic policies. In the severity assessment of TSCI, the AISA/Frankel grade is the most commonly used method for classification. Most patients were classified as grade A in Asia (76) and in previous study (10). On the contrary, we found that grade D was the most prevalent, followed by grade A. This is also consistent with our finding that the most common neurological injury associated with TSCI was incomplete quadriplegia. This could be because of the increase in the aging population in China and their associated lifestyle of staying alone resulting in an increased chance of low falls. In this study, low fall was found to be the third most common cause of TSCI.
The report on in-hospital mortality and complications can help us understand the risks of TSCI, guide treatment to reduce and avoid complications, and ultimately achieve the goal of reducing mortality. The pooled in-hospital mortality rate in this study was estimated at 3%, and the main cause of death was respiratory failure. Some studies mentioned the death of respiratory failure due to cervical spinal cord compression in the acute stage, and the death of pulmonary infection after tracheotomy due to respiratory system related complications in the subacute stage. But this may be an underestimate, as up to 46% of injury deaths on death certificates between 2006 and 2016 did not have an S or T code (N code) for the nature of the injury (79). Besides, the number of TSCI patients who may have died at the scene or en route to the hospital is undetermined and the tradition in some regions of China is to take seriously ill patients home to spend the last time with their families or give up treatment due to financial burden. The high disability rate of TSCI is not only reflected in nervous system damage, but also in the increased complications. The complication rate of TSCI in China was estimated at 35%, and the major secondary complications were respiratory and urinary diseases. However, after comparing the results with the developing countries (80), the results showed that pressure ulcers and urinary tract infections were the most common. In the subgroup analysis, the in-hospital mortality and complication rates in the south were higher than those in the north. Since the main complications and causes of death were respiratory related diseases, the difference between the south and north may be related to the difference in climate or medical factors.
Our study has several limitations, as follows: (1) Most of the reports we included were retrospective studies of hospital records in individual provinces, with very limited community-based studies, and hence may suffer from publication bias. (2) The diagnostic criteria of these studies were inconsistent and lacked objective indicators such as MRI rates. Most studies only used AISA/Frankel grade to evaluate, so it was difficult to conduct a meta-analysis in such instances. (3) This study focused on TSCI survivors, which excluded those who died before reaching the hospital or who returned home due to tradition or economic burden, and there were few studies describing the additional concurrent trauma at admission, which may have an impact on the outcome of the study. (4) It is unclear whether the hospitals that conducted the study are representative of the region or whether there are other hospitals in the region that also treat TSCI, leaving a possibility that the epidemiological data may be inaccurate. (5) There were few large-scale national epidemiological surveys on TSCI, and these studies were mainly concentrated in the provinces with better resources. Due to the aforementioned limitations, accurate epidemiological data on TSCI are difficult to obtain in China.
Conclusion
Traumatic spinal cord injury can usually be reduced by early prevention, and the government should issue appropriate policies based on epidemiological survey data and the different regions in the north and south. The increasing incidence of TSCI in China suggests that an urgent emphasis on prevention of the occurrence of TSCI in high-risk occupations and prevention of treatment complications is required. It is proposed that the standardization of TSCI epidemiological reports should be established in the future. Future research that are prospective, nationwide, and multicenter are required for establishing the epidemiology and TSCI. Finally, we hope that this review can provide guidance for traumatic spinal cord injury prevention, treatment, and rehabilitation in China.
Author contributions
YH and LL conceived the idea and performed data collection and extraction. TL and CF contributed to data inspection and synthesis. YH, YX, FY, and BH analyzed the data and wrote the manuscript. JZ and YW completed the critical review of manuscript. YY and XF supervised the project. All authors discussed the results and and approved the final version for publication.
Funding Statement
This research was supported by the grants from Sichuan Provincial Administration of Traditional Chinese Medicine (23NSFSC2298 and 2021MS003) and Chengdu Science and Technology Bureau (2022-YF05-02035-SN and 2019-YF08-00186-GX).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2023.1131791/full#supplementary-material
References
- 1.Pickelsimer E, Shiroma EJ, Wilson DA. Statewide investigation of medically attended adverse health conditions of persons with spinal cord injury. J Spinal Cord Med. (2010) 33:221–31. 10.1080/10790268.2010.11689699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Divanoglou A, Westgren N, Bjelak S, Levi R. Medical conditions and outcomes at 1 year after acute traumatic spinal cord injury in a Greek and a Swedish region: a prospective, population-based study. Spinal Cord. (2010) 48:470–6. 10.1038/sc.2009.147 [DOI] [PubMed] [Google Scholar]
- 3.Azarhomayoun A, Aghasi M, Mousavi N, Shokraneh F, Vaccaro AR, Haj Mirzaian A, et al. Mortality rate and predicting factors of traumatic thoracolumbar spinal cord injury; a systematic review and meta-analysis. Bull Emerg Trauma. (2018) 6:181–94. 10.29252/beat-060301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang H, Young W, Skaper S, Chen L, Moviglia G, Saberi H, et al. Clinical neurorestorative therapeutic guidelines for spinal cord injury (IANR/CANR version 2019). J Orthop Translat. (2020) 20:14–24. 10.1016/j.jot.2019.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adriaansen JJ, Ruijs LE, van Koppenhagen CF, van Asbeck FW, Snoek GJ, van Kuppevelt D, et al. Secondary health conditions and quality of life in persons living with spinal cord injury for at least ten years. J Rehabil Med. (2016) 48:853–60. 10.2340/16501977-2166 [DOI] [PubMed] [Google Scholar]
- 6.McCammon JR, Ethans K. Spinal cord injury in Manitoba: a provincial epidemiological study. J Spinal Cord Med. (2011) 34:6–10. 10.1179/107902610X12923394765733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reilly P. The impact of neurotrauma on society: an international perspective. Prog Brain Res. (2007) 161:3–9. 10.1016/S0079-6123(06)61001-7 [DOI] [PubMed] [Google Scholar]
- 8.Chen C, Qiao X, Liu W, Fekete C, Reinhardt JD. Epidemiology of spinal cord injury in China: a systematic review of the chinese and english literature. Spinal Cord. (2022) 60:1050–61. 10.1038/s41393-022-00826-6 [DOI] [PubMed] [Google Scholar]
- 9.Zhou M, Wang H, Zhu J, Chen W, Wang L, Liu S, et al. Cause-specific mortality for 240 causes in China during 1990-2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. (2016) 387:251–72. 10.1016/S0140-6736(15)00551-6 [DOI] [PubMed] [Google Scholar]
- 10.Chen X, Chen D, Chen C, Wang K, Tang L, Li Y. The epidemiology and disease burden of traumatic spinal cord injury in China: a systematic review. Chinese. J Evid-Based Med. (2018) 18:143–50. [Google Scholar]
- 11.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj. (2021) 372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. (2015) 13:147–53. 10.1097/XEB.0000000000000054 [DOI] [PubMed] [Google Scholar]
- 13.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. (1997) 315:629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Duval S Tweedie Trim R and fill . A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. (2000) 56:455–63. 10.1111/j.0006-341X.2000.00455.x [DOI] [PubMed] [Google Scholar]
- 15.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. (2010) 1:97–111. 10.1002/jrsm.12 [DOI] [PubMed] [Google Scholar]
- 16.Hu J, Dong Y, Chen X, Liu Y, Ma D, Liu X, et al. Prevalence of suicide attempts among Chinese adolescents: a meta-analysis of cross-sectional studies. Compr Psychiatry. (2015) 61:78–89. 10.1016/j.comppsych.2015.05.001 [DOI] [PubMed] [Google Scholar]
- 17.Liu J, Gao F, Li JJ. Epidemiology of patients with traumatic spinal cord injury and study on the influencing factors of hospitalization costs. [Chinese] Chinese J Rehabil. (2020) 35:139–42. [Google Scholar]
- 18.Liu HW, Liu J, Shen MX, Yang XH, Du LJ, Yang ML, et al. The changing demographics of traumatic spinal cord injury in Beijing, China: a single-centre report of 2448 cases over 7 years. Spinal Cord. (2021) 59:298–305. 10.1038/s41393-020-00564-7 [DOI] [PubMed] [Google Scholar]
- 19.Cai ZW. Regional Epidemiological Investigation of Traumatic Spinal Cord Injury. [Chinese] [Master]: Tianjin Medical University (2019). [Google Scholar]
- 20.Li WX, Li RF, Yu BL. Epidemiological analysis of 956 inpatients with traumatic spinal cord injury from 2012 to (2019). [Chinese]. Chinese J Spine Spinal Cord. (2021) 31:626–31. [Google Scholar]
- 21.Wang L, Zhou J, Shi XX, Hu Y, Qin J, Yin JK, et al. Advances in studies on the factors related to traumatic spinal cord injury. [Chinese] Chinese J Bone Joint. (2017) 6:139–44. [Google Scholar]
- 22.Liu J, Liu HW, Gao F, Li J, Li JJ. Epidemiological features of traumatic spinal cord injury in Beijing, China. J Spinal Cord Med. (2022) 45:214–20. 10.1080/10790268.2020.1793505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yuan YK. Epidemiological analysis of patients with spinal cord injury. [Chinese] Grassroots Med Forum. (2015) 19:4316–7. [Google Scholar]
- 24.Yang XX Yu QJ, Qin J, Li ZH, Song KR, Ren DF, et al. Epidemiological analysis of 1027 inpatients with spinal cord injury. [Chinese] J Spinal Surg. (2016) 14:301–5. [Google Scholar]
- 25.Zhou Y, Wang XB, Kan SL, Ning GZ Li YL, Yang B, et al. Traumatic spinal cord injury in Tianjin, China: a single-center report of 354 cases. Spinal Cord. (2016) 54:670–4. 10.1038/sc.2015.173 [DOI] [PubMed] [Google Scholar]
- 26.Xu Q, Yuan L, Gao F, Zhou HJ, Liu WG, LI JJ, et al. “Investigation and analysis of anorectal and perianal diseases in patients with spinal cord injury. [Chinese],” In Proceedings of the 14th Congress of Chinese Association of Spinal Cord. (2012), 63–65. [Google Scholar]
- 27.Wang PS, Wang S, Liu XB, An YH. Analysis of the causes and clinical characteristics of traumalicspinal cord injury based on 1395 cases. [Chinese] Chin J Emerg Resuse Disaster Med. (2020) 15:340–4. [Google Scholar]
- 28.Ning GZ. Study on Epidemiology of Spinal Cord Injury in Tianjin. [Chinese] [Doctor]: Tianjin Medical University (2012). [Google Scholar]
- 29.Jiang JC, Zhu LQ, Ye CQ, Sun TS, Xu ST. Characteristics of Spinal Cord Injury in Hospital: 423 Cases Report. [Chinese] Chin J Rehabil Theory Pract. (2012) 18:665–8. [Google Scholar]
- 30.Hua R, Shi J, Wang X, Yang J, Zheng P, Cheng H, et al. Analysis of the causes and types of traumatic spinal cord injury based on 561 cases in China from 2001 to (2010). Spinal Cord. (2013) 51:218–21. 10.1038/sc.2012.133 [DOI] [PubMed] [Google Scholar]
- 31.Li HL. A Single Center Study on Epidemiological Characteristics of Spinal Cord Injury during 1999-2016 in Tianjin. [Chinese] [Master]: Tianjin Medical University (2018). [Google Scholar]
- 32.Feng HY, Ning GZ, Feng SQ Yu TQ, Zhou HX. Epidemiological profile of 239 traumatic spinal cord injury cases over a period of 12 years in Tianjin, China. J Spinal Cord Med. (2011) 34:388–94. 10.1179/2045772311Y.0000000017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hao CX, Li JJ, Zhou HJ, Kang HQ, Li SQ, Liu GL, et al. Epidemiology Characteristics of Spinal Cord Injury in Hospital: (1264). Cases Report. [Chinese]. Chinese J Rehabilit Theory Pract. 2007:1011–3. [Google Scholar]
- 34.Beijing Spinal Cord Injury Investigation Group. A five-year retrospective survey of spinal cord injury in beijing. [Chinese]. Chinese J Rehabil. (1988) 02:59–62. [Google Scholar]
- 35.Yu TQ. Epidemiology of Traumatic Spinal Cord Injuries in Urban of Tianjin in 2007. [Chinese] [Master]: Tianjin Medical University (2010). [Google Scholar]
- 36.Wei B. The Primary Investigation into the Epidemiology of Spinal Cord Injury in Beijing in 2005. [Chinese] [Doctor]: Capital Medical University (2007). [Google Scholar]
- 37.Li JJ, Zhou HJ, Hong Y, Ji JP, Liu GL, Li SQ, et al. Spinal cord injuries in Beijing: a municipal epidemiological survey in (2002). [Chinese]. Chinese J Rehabil Theory Pract. (2004) 07:32–3.21383758 [Google Scholar]
- 38.Liu L. Reginal Retrospective Investigation of Spinal Cord Injury Epidemiology. [Chinese] [Master]: Tianjin Medical University (2019). [Google Scholar]
- 39.Ru QC. Epidemiological Study of Spinal Cord Injury in Dalian. [Chinese] [Master]: Dalian Medical University (2014). [Google Scholar]
- 40.Xu CG, Gu R, Wang TB, Jiang BG. Epidemiological analysis of 1274 cases of spinal trauma. [Chinese] JIN RI JIAN KANG. (2016) 15:19–20. [Google Scholar]
- 41.Chen R, Liu X, Han S, Dong D, Wang Y, Zhang H, et al. Current epidemiological profile and features of traumatic spinal cord injury in Heilongjiang province, Northeast China: implications for monitoring and control. Spinal Cord. (2017) 55:399–404. 10.1038/sc.2016.92 [DOI] [PubMed] [Google Scholar]
- 42.Niu SJ, Zhou QQ, Zhang DW. Epidemiological analysis of 422 hospitalized patients with traumatic spinal cord injury. [Chinese] Bao Jian Wen Hui. (2021) 22:21–3. [Google Scholar]
- 43.Tang YL. Study of the status of urinary tract infection and bladder management and related risk factors in patients with spinal cord injury. [Chinese] [Master]: Qingdao University. (2021). [Google Scholar]
- 44.Feng H, Xu H, Zhang H, Ji C, Luo D, Hao Z, et al. Epidemiological profile of 338 traumatic spinal cord injury cases in Shandong province, China. Spinal Cord. (2022) 60:635–40. 10.1038/s41393-021-00709-2 [DOI] [PubMed] [Google Scholar]
- 45.Wu F, Zheng Y, Ren B, Huang L, Yang D. Current epidemiological profile and characteristics of traumatic cervical spinal cord injury in Nanchang, China. J Spinal Cord Med. (2022) 45:556–63. 10.1080/10790268.2021.1949188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Niu SJ. Epidemiologic analysis of spinal cord injury in Suzhou and clinical study of related factors. [Chinese] [Master]: Soochow University (2016). [Google Scholar]
- 47.Wang HF, Yin ZS, Chen Y, Duan ZH, Hou S, He J. Epidemiological features of traumatic spinal cord injury in Anhui Province, China. [Chinese] Spinal Cord. (2013) 51:20–2. 10.1038/sc.2012.92 [DOI] [PubMed] [Google Scholar]
- 48.Pan J, Li X, Zeng C, Qian L, Li LJ, Tan J. Retrospective study of acute spinal cord injury between 2005 and 2007 in Pudong New Area, Shanghai. [Chinese] J Tongji Univ (Medical Science). (2009) 30:131–5. [Google Scholar]
- 49.Yang WQ. Epidemiological Investigation Of 1089. Hospitalized Patients With Spinal Cord Injury [Chinese] [Master]: Fujian Medical University (2015). [Google Scholar]
- 50.Duan MS, Shu Y, Cao K, Han ZM, Huang SH. Clinical analysis of early complications and related factors in 650 patients with acute spinal cord injury. [Chinese] Chinese J Physic Med Rehabilit. (2009) 09:632–4. [Google Scholar]
- 51.Chen J, Chen BH. Clinical analysis of 251 cases of traumatic spinal cord injury. [Chinese] Chinese Commun Doct. (2009) 11:69.30010044 [Google Scholar]
- 52.Hu GY, Tang HF, Tang LA. Epidemiological investigation of spinal cord injury in Songjiang County, Shanghai. [Chinese] Chin J Spine Spinal Cord. (1992) 04:177–9. [Google Scholar]
- 53.Cheng LM, Zeng ZL, Yang ZY, Zhou JL, Yuan F, Zhang SM, et al. Epidemiologic features and effects of surgical treatment of spinal injudes treated in one medical center. [Chinese]. Chin J Orthop Trauma. (2008) 03:245–8. [Google Scholar]
- 54.Sun ZY, Chen BH, Hu YG, Ma XX, Yuan B. The value of china national spinal cord injury database in the analysis of patients with acute apinal cord injury. [Chinese] Acta Aacademiae Medicinae Qingdao Universitatis. (2012) 48:115–7. [Google Scholar]
- 55.Pang QN. Epidemiological survey of traumatic SCI in Wuxi in (1991). [Chinese] Chin J Spine Spinal Cord. (1993) 6:266. [Google Scholar]
- 56.Zhang SP, Cao LJ, Zhou BQ, Zhong C. Analysis of the characteristics of acute spinal cord injury in the urbanrural fringe of Guangzhou. [Chinese]. China Modern Med. (2020) 27:163-165+184. [Google Scholar]
- 57.Huang Y, Ye L, Fen HY, Liu WW. Epidemiology Characteristics of 397 cases of Spinal Cord Injury in Hospital. [Chinese] Chinese Manipulat Rehabilit Med. (2018) 9:38–40.35254231 [Google Scholar]
- 58.Yi CR. Epidemiological Features of 261 Hospitalized Patients with Spinal Cord Injury from Multiple Hospitals in Hunan Province. [Chinese] [Master]: University of South China (2015). [Google Scholar]
- 59.Deng L, Shang H, Chang W, Wu YP, Li BK, Guo ZK, et al. Epidemiologic analysis of 424 cases of spine and spinal cord injuries. [Chinese]. Chinese J Clinic Res. (2015) 28:858-860+864.17413460 [Google Scholar]
- 60.Lv DB. Epidemiological Investigation of Spinal Cord Injury. [Chinese] [Master]: Zhengzhou University (2018). [Google Scholar]
- 61.Tang ZS. Epidemiological Characteristics and Correlative Analysis of Inpatients with Spinal Cord Injury :221 Cases Report. [Chinese] [Master]: Guangxi Medical University (2011). [Google Scholar]
- 62.Zhu CJ. Clinical Observation on Early Rehabilitation Treatment of Spinal Cord Injury. [Chinese] [Master]: Central South University. (2010). [Google Scholar]
- 63.Yang R, Guo L, Huang L, Wang P, Tang Y, Ye J, et al. Epidemiological characteristics of traumatic spinal cord injury in Guangdong, China. Spine (Phila Pa 1976: ). (2017). 42(9):E555-E561. 10.1097/BRS.0000000000001896 [DOI] [PubMed] [Google Scholar]
- 64.Chen YH, Liu M, He JH. Epidemiological survey of patients with spinal cord injury. [Chinese] Chinese J Practic Med. (2011) 27:1032–4.17586966 [Google Scholar]
- 65.Ning GZ, Mu ZP, Shangguan L, Tang Y, Li CQ, Zhang ZF, et al. Epidemiological features of traumatic spinal cord injury in Chongqing, China. J Spinal Cord Med. (2016) 39:455–60. 10.1080/10790268.2015.1101982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mao Q, Liu YH, Mao BY. Analysis of the associated factors of spinal cord injuries with multi+traumas. [Chinese] J Sichuan Univ. (2004) 02:244–6. [PubMed] [Google Scholar]
- 67.Hao DJ, He BR, Yan L, Wang Y, Zhang Q, Liu CC, et al. Epidemiological profile of spinal cord injury from 2011 through 2013 at Xi'an Honghui Hospital. [Chinese] Chinese J Traumatol. (2015) 31:632–6. [Google Scholar]
- 68.Zhang JJ. The Disease Burden and Outcome of Hospitalized Patients with Traumatic Spinal Cord Injury in China. [Chinese] [Master]: Chinese Center for Disease Control and Prevention. (2021). [Google Scholar]
- 69.Yang NP, Deng CY, Lee YH, Lin CH, Kao CH, Chou P. The incidence and characterisation of hospitalised acute spinal trauma in Taiwan–a population-based study. Injury. (2008) 39:443–50. 10.1016/j.injury.2007.12.007 [DOI] [PubMed] [Google Scholar]
- 70.Wu JC, Chen YC, Liu L, Chen TJ, Huang WC, Cheng H, et al. Effects of age, gender, and socio-economic status on the incidence of spinal cord injury: an assessment using the eleven-year comprehensive nationwide database of Taiwan. J Neurotrauma. (2012) 29:889–97. 10.1089/neu.2011.1777 [DOI] [PubMed] [Google Scholar]
- 71.Chen HY, Chiu WT, Chen SS, Lee LS, Hung CI, Hung CL, et al. A nationwide epidemiological study of spinal cord injuries in Taiwan from July 1992 to June (1996). Neurol Res. (1997) 19:617–22. 10.1080/01616412.1997.11740870 [DOI] [PubMed] [Google Scholar]
- 72.Lan C, Lai JS, Chang KH, Jean YC, Lien IN. Traumatic spinal cord injuries in the rural region of Taiwan: an epidemiological study in Hualien county, 1986-1990. Paraplegia. (1993) 31:398–403. 10.1038/sc.1993.66 [DOI] [PubMed] [Google Scholar]
- 73.Chen CF, Lien IN. Spinal cord injuries in Taipei, Taiwan, 1978-1981. Paraplegia. (1985) 23:364–70. 10.1038/sc.1985.58 [DOI] [PubMed] [Google Scholar]
- 74.Hao D, Du J, Yan L, He B, Qi X, Yu S, et al. Trends of epidemiological characteristics of traumatic spinal cord injury in China, 2009-2018. Eur Spine J. (2021) 30:3115–27. [DOI] [PubMed] [Google Scholar]
- 75.Jiang B, Sun D, Sun H, Ru X, Liu H, Ge S, et al. Prevalence, Incidence, and External Causes of Traumatic Spinal Cord Injury in China: A Nationally Representative Cross-Sectional Survey. Front Neurol. (2022) 12:784647. 10.3389/fneur.2021.784647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ning GZ, Wu Q, Li YL, Feng SQ. Epidemiology of traumatic spinal cord injury in Asia: a systematic review. J Spinal Cord Med. (2012) 35:229–39. 10.1179/2045772312Y.0000000021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lee BB, Cripps RA, Fitzharris M, Wing PC. The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord. (2014) 52:110–6. 10.1038/sc.2012.158 [DOI] [PubMed] [Google Scholar]
- 78.Wyndaele M, Wyndaele JJ. Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord. (2006) 44:523–9. 10.1038/sj.sc.3101893 [DOI] [PubMed] [Google Scholar]
- 79.Li B, Qi J, Cheng P, Yin P, Hu G, Wang L, et al. Traumatic spinal cord injury mortality from 2006 to 2016 in China. J Spinal Cord Med. (2021) 44:1005–1010. 10.1080/10790268.2019.1699355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Golestani A, Shobeiri P, Sadeghi-Naini M, Jazayeri SB, Maroufi SF, Ghodsi Z, et al. Epidemiology of traumatic spinal cord injury in developing countries from 2009 to 2020: a systematic review and meta-analysis. Neuroepidemiology. (2022) 56:219–39. 10.1159/000524867 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.