Background:
Research and reporting of mortality indicators typically focus on a single underlying cause of death selected from multiple causes recorded on a death certificate. The need to incorporate the multiple causes in mortality statistics—reflecting increasing multimorbidity and complex causation patterns—is recognized internationally. This review aims to identify and appraise relevant analytical methods and practices related to multiple causes.
Methods:
We searched Medline, PubMed, Scopus, and Web of Science from their incept ion to December 2020 without language restrictions, supplemented by consultation with international experts. Eligible articles analyzed multiple causes of death from death certificates. The process identified 4,080 items of which we reviewed 434 full-text articles.
Results:
Most articles we reviewed (76%, n = 332) were published since 2001. The majority of articles examined mortality by “any– mention” of the cause of death (87%, n = 377) and assessed pairwise combinations of causes (57%, n = 245). Since 2001, applications of methods emerged to group deaths based on common cause patterns using, for example, cluster analysis (2%, n = 9), and application of multiple-cause weights to re-evaluate mortality burden (1%, n = 5). We describe multiple-cause methods applied to specific research objectives for approaches emerging recently.
Conclusion:
This review confirms rapidly increasing international interest in the analysis of multiple causes of death and provides the most comprehensive overview, to our knowledge, of methods and practices to date. Available multiple-cause methods are diverse but suit a range of research objectives. With greater availability of data and technology, these could be further developed and applied across a range of settings.
Keywords: Comorbidity, Death certificates, Mortality, Multiple causes of death, Population health
Mortality statistics are crucial to population health as they provide fundamental information about health status, disease etiology, trends, and patterns of diseases in different populations. They inform health services, health policy development, and planning, as well as research, and can be used to evaluate the impact of health intervention programs.1,2 Therefore, it is critical that accurate and reliable information about the diseases and health conditions that cause death are appropriately analyzed.
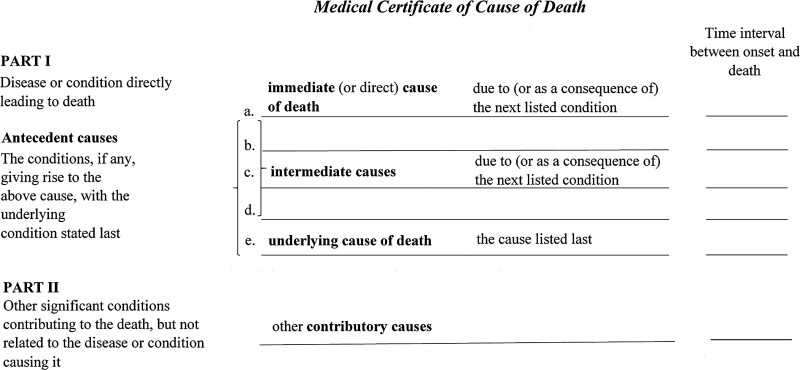
Death typically results from the interplay between multiple health conditions. The standard international format of the death certificate (Figure 1) facilitates recording the certifying doctor’s medical opinion of all diseases and conditions involved in the death including the underlying and nonunderlying (intermediate and immediate) causes in Part I, and other important contributing causes in Part II. If the certificate is completed correctly, the underlying cause reflects the initiating condition, that is, one that could be avoided by some preventative mechanism to interrupt the sequence leading to death. The medical certification process reflects the multifaceted pathological processes leading to death. However, the recording of a single disease as the underlying cause can be complex, and misclassification of the underlying cause can occur when several causal pathways are involved.3–8 Following the medical certification of the cause of death, an international coding standard is applied to all causes reported on the death certificate to endorse the reported underlying cause or select a more appropriate alternative to be used for statistical reporting (including international comparisons) and epidemiological studies.9 Causes of death data thus contain the standardized underlying cause and all other causes that were involved in the death (associated causes).
FIGURE 1.
Layout of a standard international form of Medical Certificate of Cause of Death.
Despite the vast amount of information that is collected about the causes of deaths, mortality statistics typically use only the (single) underlying cause. Researchers have long recognized that the underlying cause alone does not adequately describe the pathologic processes responsible for most deaths,10–12 and potentially understates the importance of other significant contributing causes of death.1,13 International support for the need to assess the multiple causes of death to complement statistics based on the underlying cause approach is well established but the methods used are diverse. To adequately inform population health initiatives, it is essential that all diseases and conditions contributing to death receive appropriate attention.
Previous studies10,14–16 have attempted to appraise and summarise the assortment of methods used to measure the involvement of all causes on the death certificate, however, they are limited in scope and were performed over a decade ago thus not capturing recent methodological advances in the analysis of multiple causes of death. This review, supplemented by consultations with subject experts, aims to identify and appraise the methods used in analyses of data on multiple causes of death, providing a comprehensive and up-to-date account of methods and practices that are used to describe and measure the involvement of multiple health conditions in causing death.
METHODS
Search Strategy
To identify articles that analyze data on multiple causes of death, we searched the Medline, PubMed, Scopus, and Web of Science databases, each from inception to December 31, 2020, for original research without any restriction on language or country of study. To maximize the number of relevant articles related to multiple causes of death, we included search terms covering “multiple*” AND “cause*” AND (“death” OR “mortality”) and other variations such as (“associated” OR “contributory” OR “underlying”) AND “cause*” (eAppendix, eTable 1; http://links.lww.com/EDE/C14).
Selection of Articles
Two authors (K.B. and S.B.) each independently screened 50% of titles and abstracts of the identified articles, beginning with a random sample of 5% of articles in duplicate. Disagreements were solved by consensus.
Eligibility Criteria
Articles were eligible if they: reported using death registration or death certificate data and applied a multiple-cause method to calculate a multiple-cause indicator; or derived a measure of mortality based on the multiple causes of death. We considered all study designs except case reports, case series, and forensic reports. We excluded research that used only the underlying cause of death for analysis, or that used multiple-cause data but did not apply or report a measure based on multiple causes. We also excluded articles based on verbal autopsy, narrative, reviews, and non-peer-reviewed literature.
Data Extraction
For the included articles, we extracted study characteristics (authors’ names, journal name, year published, study design, study period, country, source of multiple-cause data, and main cause of interest) and decedent characteristics (age, sex, and the number of deaths evaluated) using a full-text review. We categorized each article into one or more categories according to the objectives of the application of multiple cause methods as articles that: described cause-related mortality based on “any mention” of a cause; assessed the joint involvement of causes according to pairwise disease occurrence on death certificates; described mortality for clusters of more than 2 commonly co-occurring causes; and measured cause-related mortality burden by weighting multiple causes.
Audit of Experts
To identify unpublished methods in practice, we supplemented the search strategy by consultation with subject experts. Contacts were identified from affiliations of relevant articles and recommendations from experts in the field and included representatives from agencies such as the Multiple Causes-of-Death Network (https://mcod.web.ined.fr), the World Health Organization Family of International Classification collaborating centers, and national statistical offices of countries, including the United States, England, Canada, New Zealand, Italy, and Australia. During December 2020, we sent emails to 261 contacts asking regarding their awareness of relevant studies, particularly recently accepted or unpublished articles or reports that used multiple-cause methodology. We received 41 responses resulting in a response rate of 16%.
Statistical Methods
We classified articles included in full-text review based on a priori selected mutually exclusive categories of statistical methods used to analyze multiple causes of death as: methods based on any mention; methods to assess the pairwise occurrence of causes; methods based on groups of more than two co-contributing causes; and methods based on the weighting of multiple causes. Following the full-text review, we classified included articles published from 2015 onwards based on the main research objective into 4 categories: describe cause-related mortality; identify co-contributing causes; assess relationships between co-contributing causes; assess impact of risk factors; and other objectives. For articles published between 2015 and 2020, we mapped the research objectives against the multiple-cause methods that were used to achieve them. We did not evaluate publication bias as this review focussed on methodologic practices applied in each article rather than on results.
RESULTS
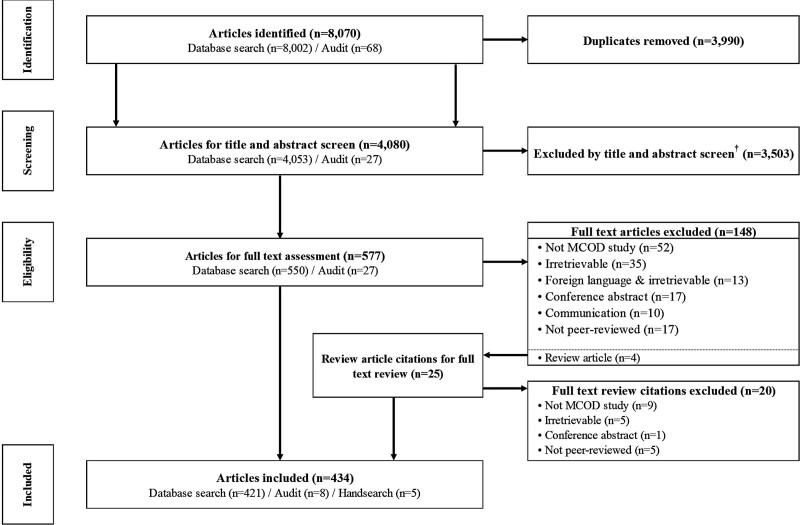
We identified 8,070 articles overall: 8,002 from the database search and 68 from responses to the consultations. After removing duplicates, we selected 4080 articles for title and abstract screening (Figure 2). Due to a large number of articles and limited resources, we excluded 101 articles that appeared to only use methods based on any mention without full-text review. We identified 4 review articles in the screening, and a manual search of these identified a further 25 potentially eligible articles. We selected a total of 602 articles for full-text review, including 25 from the consultations (Figure 2). From these, we included 434 articles, and we assessed the multiple-cause methods applied in each. The remaining 168 articles did not meet the inclusion criteria: 4 were reviews, 61 were not in scope, 53 were irretrievable (including 13 in a foreign language), 28 were communications or conference abstracts, and 22 were non-peer-reviewed articles (none of them employed methods other than those a priori identified) that we excluded from the full-text review.
FIGURE 2.
Study flow diagram. † Due to high volume and limited resources, 101 articles that appeared to only apply a method based on any-mention were excluded without full-text review.
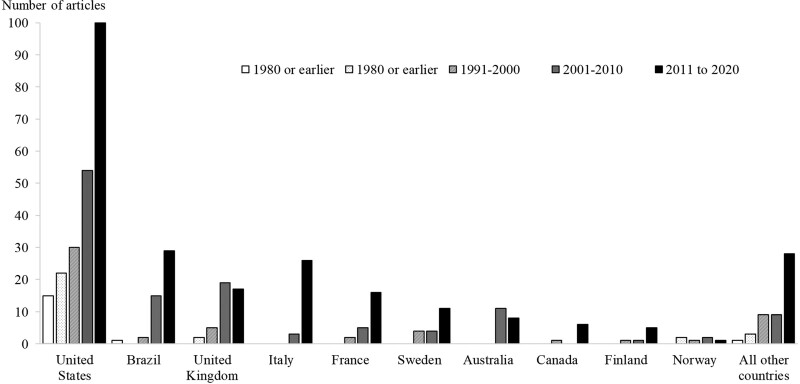
A summary of the characteristics of included articles is presented in Table 1. The number of articles using multiple causes methods increased over time; more than 3-quarters (n = 332, 76%) were published after 2001 (Table 1). Most articles assessed deaths registered in the United States (n = 222, 13%), Brazil (n = 47, 3%), and the United Kingdom (n = 43, 3%) (Table 1). In most countries, the application of multiple-cause methods rose over time, with notable increases during 2001–2020 (Figure 3). Infectious diseases (largely HIV/AIDS) were the most common cause of interest in the application of multiple-cause methods (n = 76, 18% articles), followed by external causes (n = 69, 16% articles) of which most assessed drug-related deaths. We found the population-level analysis of all causes of death using multiple-cause methods in 44 (10%) articles. Cross-sectional evaluation of deaths was the most common study design (n = 352, 81% articles). Most articles reviewed were in English (n = 416, 96%) and Portuguese (n = 13, 3%).
TABLE 1.
Characteristics of Articles Included in the Study.
| Number | Percent | |
|---|---|---|
| Total number of articles | 434 | |
| Year published | ||
| 1980 or earlier | 19 | 4 |
| 1981–1990 | 29 | 7 |
| 1991–2000 | 54 | 12 |
| 2001–2010 | 114 | 26 |
| 2011 to present | 218 | 50 |
| Country of dataa | ||
| United States | 222 | 13 |
| Brazil | 47 | 3 |
| United Kingdom | 43 | 3 |
| Italy | 30 | 2 |
| France | 23 | 1 |
| Sweden | 19 | 1 |
| Australia | 19 | 1 |
| Canada | 7 | <1 |
| Finland | 7 | <1 |
| Norway | 6 | <1 |
| All other countries | 50 | 3 |
| Research focusa | ||
| Population level analysis of all causes | 44 | 10 |
| Specific causes of death | ||
| Infectious diseases | 76 | 18 |
| HIV/AIDS | 22 | 5 |
| Hepatitis | 9 | 2 |
| Sepsis | 8 | 2 |
| External causes | 69 | 16 |
| Drug-related | 23 | 5 |
| Alcohol-related | 15 | 4 |
| Cardiovascular diseases | 50 | 12 |
| Endocrine diseases | 43 | 10 |
| Diabetes | 37 | 9 |
| Neurological diseases | 35 | 8 |
| Cancer | 25 | 6 |
| Respiratory diseases | 23 | 5 |
| Digestive diseases | 13 | 3 |
| Musculoskeletal conditions | 12 | 3 |
| Mental conditions | 11 | 3 |
| All other causes | 33 | 8 |
| Study design | ||
| Cross-sectional | 352 | 81 |
| Cohort/longitudinal | 69 | 16 |
| Case control | 7 | 2 |
| Other | 6 | 1 |
| Language of article | ||
| English | 416 | 96 |
| Portuguese | 13 | 3 |
| Other | 5 | 1 |
Numbers may not sum to the total as multiple categories apply.
FIGURE 3.
Number of articles by country and year of publication.
We broadly categorized articles by the methods applied in analyzing multiple causes of death as those describing mortality based on any mention of a cause; examination of pairwise occurrence of diseases on death certificates; assessment of mortality based on groupings of more than 2 co-contributing causes; and calculation of cause-related mortality burden based on weighted multiple causes. The results for each category are described in detail below. There were no new methods identified from the audit of experts.
Descriptive Measures of Multiple Causes Based on Any Mention
Of the 434 articles included in the full-text review, 377 (87%) articles assessed cause-related mortality based on any mention of the cause (Table 2; eAppendix, eTable 2; http://links.lww.com/EDE/C14); this excludes 101 articles without full-text review that appeared to only use methods based on any mention. The methods applied in these articles included basic summary (or univariate)17 statistics applied to a specific index cause. Examples of specific methods include multiple cause indicators that describe the number of causes (n) involved in each death, the average number of causes per death, and frequency or percentage distributions of n, each illustrating the extent to which multiple causes occur in the death data. Also included here were articles that aimed to evaluate cause-related mortality using rates based on any mention of a cause; that is, by counting each death that mentions the cause of interest anywhere on the death certificate.18–21 Some evaluated the leading causes of death using any mention22–27 to understand the most common causes involved in deaths. Assessment of temporal trends in rates based on any mention against rates based on the underlying cause was used to highlight changes in certification or coding practices and changing patterns of disease contribution to death.28–30 Comparisons between countries in multiple cause indicators can be used to emphasize differences in certification practices between countries.3,31–33
TABLE 2.
Summary of Approaches to Assess Multiple Causes of Death in the 434 Articles Included in the Study
| Methodologic Approach | Selected Examples [Record Number]a |
|---|---|
| 1. Methods based on any mention (n = 377, 87%) | [1–377] |
| Uses: to assess the extent of multiple causes and compare measures based on underlying causes to measures based on multiple causes Examples: average number of causes; rates by “any mention”; comparisons using the standardized ratio of multiple to underlying causes Strengths: identifies causes less visible using an underlying cause approach Limitations: metrics based on any mention inflate mortality estimates as deaths are counted more than once |
Wall 2005 [361] Goldacre 2006 [240] Desesquelles 2014 [37] Goldberger 2015 [60] Zoppini 2018 [377] Simmons 2019 [343] Sampaio 2020 [151] Cano 2020 [383] |
| 2. Methods to assess pairwise occurrence of causes (n = 245, 57%) | [1–191, 378–431] |
| Uses: to identify and assess co-contributing causes of death Examples: leading underlying causes for a specific associated cause; mortality odds ratios for the presence of specific causes Strengths: identifies most commonly occurring comorbid conditions at death; measures the strength of association between two co-contributing causes on the death certificate (e.g. odds ratio, cause of death association indicator) Limitations: does not measure causality; can overlook relationships between two non-underlying causes |
Redelings 2005 [412] Rockett 2007 [418] Redelings 2007 [414] Desesquelles 2012 [36] Duncan 2014 [42] Chazal 2018 [20] Turner 2018 [171] Quast 2020 [409] |
| 3. Methods based on groups of >2 co-contributing causes (n = 9, 2%) | [55, 162, 173, 188, 192, 196, 219, 433, 434] |
| Uses: to identify frequently co-occurring causes and assess mortality trends due to grouped causes Examples: combine causes based on known risk associations or cluster analysis, social network analysis and data mining according to patterns in multiple causes Strengths: identifies highly correlated diseases and risk conditions among large datasets Limitations: data-driven methods are difficult to replicate or apply across different settings |
Stallard 2002 [162] Frova 2009 [55] Yoon 2011 [188] Barbieri 2017 [196] Hassanzadeh 2017 [433] Jiang 2017 [434] Egidi 2018 [219] Villela 2018 [173] Adair 2020 [192] |
| 4. Methods based on weighting of multiple causes (n = 5, 1%)b | [246, 306, 322, 371, 432] |
| Uses: to re-evaluate mortality metrics based on weighted multiple causes Examples: ascribing fixed or variable weights to each cause such that the weights in each death sum to one Strengths: can prescribe causal responsibility to selected diseases (e.g. antecedent conditions); incorporates a mortality contribution of all relevant conditions Limitations: difficult to ascribe causal responsibility across cause of death data so weights are arbitrary |
Piffaretti 2016 [322] Moreno-Betancur 2017 [306] González 2019 [246] Breger 2020 [432] Xie 2020 [371] |
Record Number: See eAppendix, eTable2 for full reference.
Articles that applied multiple cause weighting methods and data-driven methods for grouping deaths based on multiple cause patterns were all applied since 2016.
Rate ratios were commonly applied to indicate the extent to which a cause occurs as the underlying cause versus nonunderlying cause. A common approach compared the occurrence of the cause as any mention to its occurrences as the underlying cause (the approach varies according to whether counts or rates are used in the ratio and whether the any mention versus nonunderlying mentions are compared to the underlying cause).10 One form of this measure, the standardized ratio of multiple to underlying causes,13,34 encourages a harmonized approach to calculating this indicator; here the rate ratio is calculated as the age-standardized rate for any mention of the cause compared to the age-standardized rate when the cause is the underlying cause. This indicator describes the extent to which the cause is selected as nonunderlying cause relative to the underlying cause (with a value of 1 indicating the cause is always the underlying cause, 2 indicating equal representation as the underlying cause and nonunderlying cause, and 2 or more indicating the cause is more often a nonunderlying cause). Country comparisons of this method can be used to assess variation in certification.32
Articles that used counts or rates of any mention of causes to derive other summary measures of mortality, for example, potential years of life lost35 and life expectancy36–41 were also included in this category. Further examples of articles that applied these methods are in Table 2.
Assessing Pairwise Contribution to Mortality
We categorized here articles that investigated the relationships between 2 causes of death reported on the same death certificate; this was true of 57% (n = 245) of the 434 articles included in the full-text review (Table 2; eAppendix, eTable 2; http://links.lww.com/EDE/C14). A distinguishing feature of these methods is that the joint frequencies of just 2 causes are the focus of the analysis. To investigate relationships between 2 causes, researchers assessed the involvement of a specific underlying cause with one or more associated causes or vice versa (e.g. the nature and spread of an associated or immediate cause for an underlying cause of interest). Typically, the objective is to understand which comorbid conditions commonly occur with a specific cause using frequency or percentage distributions of the most common associated causes for a specific underlying cause and vice versa.42–45
We found more comprehensive applications of odds ratios (mortality odds ratios) and relative rates in articles that aimed to measure the associations between comorbid medical conditions involved in the death for a specific cause of interest. Mortality odds ratios were used to assess the odds of any mention of a specific cause with other comorbidities at death.9,35,46–57 Rate ratios were used to assess mortality burden according to whether another specific cause was present or absent, or to deaths in general.58,59 In most cases the application of mortality odds ratios disregards the role of the cause, thereby enabling relationships between 2 nonunderlying causes to be included in the assessment. Previous reviews of measures of association for multiple cause of death discuss the applicability of several approaches including: matched mortality odds ratios, matched exposure odds ratios,15 and Yules Q, Positive Matching Index, Forbes’ coefficient, and Wise and Sorvillo ratio,14 concluding the most suitable to be those that do not consider nonmatches.
A more recently introduced measure, the cause of death association indicator compares the standardized rate of involvement of a cause of interest reported together with a specific underlying cause to its involvement in death overall (that is with any underlying cause).13,34,60 The cause of death association indicator aids understanding of whether a nonunderlying cause of interest is more common in the presence of a specific underlying cause than with all underlying causes combined. In this indicator, the role of the causes is fixed thereby requiring reverse comparisons for each underlying cause and nonunderlying cause of interest.
Assessing Mortality Patterns for Grouped Causes of Deaths
Articles categorized here aimed to assess mortality from either a cluster of decedents where the grouping is based on patterns in the multiple causes or by known disease associations or by a cluster of specific causes grouped according to some measure of “similarity” or closeness. These approaches were applied in 2% (n = 9) articles and were considered as newly emerging methods, with all but 1 article published since 2009 (Table 2; eAppendix, eTable 2; http://links.lww.com/EDE/C14). Articles largely used methods for grouping multiple causes of death to understand more complex relationships between multiple causes of death or to highlight patterns of disease that commonly co-contribute to death with more than 2 causes of interest. In some articles, the groupings were user-specified combinations of causes11,61–63 while others used data-driven methods such as cluster analysis,64,65 social network analysis,66 and more exploratory methods of data mining.67,68 Social network analysis identified links (and their strengths) between causes of death, cluster analysis methods grouped decedents based on similarity between causes, that is, based on the causes of death that commonly co-contribute to death, and data mining techniques were applied to identify complex patterns in mortality data68 and assess temporal evolution of the leading clusters of conditions that cause death.67
Multiple-cause Weighting Methods
We identified 5 (1%) articles that aimed to calculate cause-related mortality by ascribing weights to each cause in the death record1,69–72 (Table 2, eAppendix, eTable 2; http://links.lww.com/EDE/C14). The multiple cause weighting methods identified in this review assigned weights to each cause such that, within each death, the weights summed to 1.0. With this approach, the counting unit (deaths) is preserved enabling measures of cause-related mortality (rates, years of life lost, etc) to be recalculated based on the weighted counts of deaths. The included articles illustrated their proposed method by estimating socioeconomic inequalities in mortality,69 conditions whose contribution to death is underestimated,1,70 proportional mortality,72 and the relative risk of cause-specific mortality among individuals with human immunodeficiency virus versus those without.71
We noted various strategies for ascribing weights, for example, weighting all causes equally as 1/n where n is the number of causes involved in the death, weighting the underlying cause a fixed amount (e.g. 50%) with the remaining amount (in this case 50%) apportioned equally across the other causes, or weighting the underlying cause twice as much as other causes. The strategies also varied according to the causes included for weighting—all causes versus the underlying cause plus contributing causes from Part II of the death certificate.
Among included texts, 46% (n = 198) applied more than 1 multiple-cause method; most frequently (n = 187) an any-mention method and a pairwise assessment of causes of death (eAppendix, eTable 3; http://links.lww.com/EDE/C14). Four of five applications of weighting methods also reported indicators using any-mention.
Across all applications of multiple-cause methods, the techniques varied in regard to (1) whether the study included a comparison of multiple to underlying causes; (2) whether the study used all non-underlying causes, or a specified set based, for example, on the location on the death certificate (Part I or Part II); (3) whether ill-defined or external causes of death were considered; and (4) whether duplicate mentions of the cause of interest were excluded.
Research Objectives
The objectives for applying multiple causes analyses varied. Some broad themes were identified in the aims: to describe cause-related mortality using multiple causes; to identify co-contributing causes (that is, the associated causes for a specific underlying cause and vice-versa); to assess relationships between causes using a measure of association; or assess the impact of risk factors on mortality. A residual category of “other” objectives captured articles that intended to measure the contribution of all causes of death in a population using multiple-cause methods and those with aims that centered around exploring the multiple-cause data. In this subset of articles published between 2015 and 2020 (n = 133), most (55%, n = 73) aimed to describe the cause of interest using multiple causes of death and applied methods based on any mention in 66 articles and pairwise assessment in 39 (eAppendix, eTable 4; http://links.lww.com/EDE/C14). Of the 28 articles whose main aim was to identify co-contributing causes for a specific cause of interest, nearly all applied methods based on any mention (n = 24) and pairwise assessment of causes on the death certificate (n = 25) with only one that grouped more than 2 causes for analysis. Most notable were the applications of emerging approaches to analyzing multiple causes. Foremost were whole population analyses to quantify the contribution of all causes that contributed to death by weighting each one as described above.1,69 Though weights were arbitrary, these novel methods lend to capturing all causal contributions at a population level, which by restricting the selection of causes can convey the mortality contributed by antecedent causes1,69 or if required, only the complications of diseases for targeted prevention efforts.73 Other examples of recently emerging methods assessed the impact of risk factors by quantifying the contributing causes of death (using weighting) among known AIDS cases for comparison of causes of death by exposure to injecting drug use,71 assessing the impact on mortality trends of deaths reporting the presence of conditions known to be associated with obesity,61 and by using cluster analysis techniques to assess mortality differentials between clusters of discrete groupings of causes associated with obesity.64
DISCUSSION
Our review and audit confirm rapidly increasing international interest in the use of multiple causes of death data in mortality research and provide the most comprehensive overview of methods and practices to date. Most articles identified were published since 2011 and were from countries with health information management systems enabling the collection and recording of multiple causes of death. Articles analyzing multiple causes of death were highly skewed towards those using descriptive measures applied to any mention of a cause of death and those assessing the pairwise contribution of causes to mortality. Cluster analysis techniques and weighting multiple causes were found to be newly emerging applications, applied only since 2016 and used in less than 3% of articles. Irrespective of the methodological approach, all the included articles demonstrated that multiple cause analysis complements the single underlying cause approach by increasing the descriptive utility of the data and improving the quantification of causal attribution to mortality at both individual and population level.
Improved data quality and access to population-level mortality data from vital registration systems may have facilitated increased use of multiple causes data over time.74 The review showed that for descriptive research questions, simple measures such as the number of deaths as well as death proportions and rates based on any mention of a specific disease or condition may be sufficient in many cases. However, the complexity in the structure of multiple causes data in terms of differentiating between causes listed in Part 1 and Part II of the death certificate, the application of rules for selection of the underlying cause of death, and variations in death certification practices between countries and over time, pose challenges in interpreting analyses using multiple causes.3,32,61,75,76 Interpretation of Coronavirus disease (COVID-19) mortality patterns is currently a major challenge, where there is considerable uncertainty as to whether COVID-19 infection was the underlying cause of death (referred to as “death from COVID-19”), or whether it was a contributory cause (“death with COVID-19”).77,78 There are varying perceptions among certifiers, epidemiologists, and policy makers on the interpretation of deaths for which COVID-19 is a multiple cause, underscoring the need for clear guidelines on definitions of each outcome, with the illustration of some approaches to data interpretation.79 In view of the critical importance of the placement of COVID-19 in Part 1 and Part II of the death certificate as a driver of determining death from or with COVID-19, adequate attention should be paid to proper medical certification of the cause of death in these cases.2 The high frequency of analyses on drug-related mortality among the included articles likely arises as the International Classification of Diseases (ICD)-10 coding mechanisms stipulate that the manner of death (intentional/unintentional poisoning) is routinely reported as the underlying cause with the drug class represented by the associated causes. Although deaths from accidental and intentional overdoses can be distinguished based on the underlying cause alone and multiple cause analyses enable identification of drug class, incorporating other information such as the use of literal text search to identify the type of drug involved in deaths80,81 and social determinants associated with deaths61,82 can improve mortality surveillance.
Our audit of international experts coincided with a peak in the COVID-19 cases in Europe; the reliance on these public health experts during a period of heavy workload and uncertainty may have contributed to the low response rate. Furthermore, analysis of multiple causes of death requires data from vital registries, which are not available in all countries, thereby limiting the audit to high-income countries.
We could not identify a previous review capturing all contemporary methods used to assess multiple causes of death. Of the 4 narrative reviews identified from our search: 2 were published before 199010,16 at which time there were 47 articles (81% based on US deaths data) and the other 214,15 were published over a decade ago and neither assessed the range of analytical methods that had been used. Only methods based on any mention and pairwise assessment of causes were captured in the existing reviews.
The 4 groups of methods that we identified are distinct but complementary, and each has important practical applications. Although descriptive analyses based on any-mention provide useful contextual information, changes in coding practices over time may influence the magnitude of underlying cause mortality from death certificates. This was observed in the case of diabetes4 and other conditions29,83,84 from the transition between the 9th and 10th revisions on the International Classification of Diseases; hence, analyses of “any-mention” rates might offer a better perspective of mortality trends than rates based on the underlying cause. While cause-related rates based on any mention are simple to apply, they can be misleading in the context of overall mortality as each death is counted as many times as there are mentions.69
Methods to assess the pairwise occurrence of causes were used frequently in external cause epidemiology, specifically to assess the nature of poisoning and injury related to exposure to drugs and alcohol.85–89 While the nature of the coding process mandates the use of multiple causes of death for assessing injuries sustained from external causes, descriptive pairwise analysis has also been applied to infectious diseases90–94 and chronic diseases.3,95–101 More complex applications such as the assessment of mortality odds ratios were applied to assess the strength of relationships between diseases on the death certificates.49,59,102–105 However, it is important to note that the disease associations based on deaths data alone do not imply causation; they evaluate whether the presence of a particular cause increases or decreases the probability of death from another cause,14,47 and statistical tests pertaining to the strength of association between the causes should be interpreted with some caution13 as statistical assumptions, for example, of independence of causes, may not be valid because both causes contributed to death. Indeed, the associations between several causes mentioned on the death certificates are more frequent than would be expected by a random occurrence of the causes.13 Further, nearly all estimates of the associations between causes mentioned on the death certificates may be influenced by some level of Berkson’s paradox or collider bias.47,106 This is a form of selection bias that occurs when both the exposure and outcome variables (the 2 causes of death) influence the inclusion of participants in a study (death certificate data).47 Methods for grouping causes of death facilitate the assessment of the complex relationships between causes that may go unnoticed by pairwise analysis. The pattern of diseases and risks leading to death may not be homogenous for the whole population, and methods that cluster deaths according to patterns in contributing causes can identify groups of individuals with a specific combination of causes of death providing additional insight for setting targeted preventative interventions.64 A challenge with cluster analysis methods for grouping causes of death is that they are exploratory in nature and different clustering algorithms may result in different outcomes.107–109 Being data-driven, the characteristics of the clusters are limited to the data, making it difficult to generalize the findings to populations in other settings. Furthermore, applications such as social network analysis map and measure the relationships between causes of death, but further quantification of cause-related mortality is not possible. On the other hand, user-defined groupings of causes, for example, those based on known disease-risk associations, are especially useful for examining the joint contribution and impact on mortality trends61 that cannot be captured by pairwise comparison. The release of the ICD-11 for current implementation worldwide offers additional flexibility designed to enhance the evidence for informing better health systems.110,111 Of specific importance is the postcoordination feature, which allows combining specific codes into a cluster of relevant clinical attributes. While specific applications have not yet been defined for mortality, future application of multiple-cause methods that group diseases based on multiple-cause patterns or according to known disease-risk associations, could provide evidence to inform meaningful clusters for application in ICD-11.
Multiple-cause weighting methods have been developed to facilitate the measurement of the overall magnitude of the contribution of a specific cause to population levels of mortality.1,69 A major advantage of these methods is the preservation of the counting unit (deaths) enabling the derivation of a broad range of mortality indicators based on the weighted counts of each cause (e.g. age-standardized rates and years of life lost). This method overcomes the limitation of double-counting deaths for as many causes as present when using any-mention approaches.69 While the arbitrary nature of weights in multiple-cause weighting strategies poses a limitation, the incorporation of methods for considering causal pathways of diseases by weighting only the underlying cause and causes in Part II of the death certificate, and application of multiple-cause weighting methods require careful consideration of the weighting strategy, the cause list and the handling of ill-defined causes,73 these methods offer a richer perspective for population health monitoring.69
The choice of methods for analyzing multiple causes is dependent on the research question of interest. Irrespective of the methodologic approach, multiple cause analysis complements the single underlying cause approach, uses useful information that is usually ignored, and offers an additional perspective of the causes that contribute to death. Though there are distinct limitations around individual multiple-cause methods, the broad range of methods described here offers a toolkit, which in combination can offer a richer perspective for population health monitoring and policy development.
To the best of our knowledge, this study is the largest review to date, comprehensively capturing statistical methods used for analyzing multiple cause of death data, including many articles (>430) with 2 independent reviewers supplemented by an audit of international experts. A further strength is the use of a systematic approach to identify relevant studies, considering articles published in multiple languages. The inclusion of articles from a range of years, countries, and languages revealed the breadth and diversity of applications of multiple cause analysis.
This review is atypical of systematic reviews in that the statistical significance of results and publication bias was not relevant. Publications largely represent data from countries with national vital statistics collections.
The very specific methods are not always apparent in the articles included here. For example, there is often little transparency around how duplicate mentions of causes and ill-defined causes are handled. As well, the terminologies used can be inconsistent (for example, contributing causes is often used to refer to nonunderlying causes, but can also have a specific meaning referring to the causes reported in Part II of the death certificate). Additionally, factors that are known to affect multiple causes statistics such as the size and structure of the death certificate13,24,60 are not always apparent.
Our review showed that infectious diseases are commonly assessed using multiple-cause methods, for example, to ascertain socio-demographic differentials, to identify associated health conditions, and to assess the impact of health interventions to inform targeted prevention strategies.71,91,112,113 With new and emerging infectious diseases, multiple-cause data is crucial for descriptive epidemiology and for providing evidence to inform prevention strategies. Since the declaration of COVID-19 as a pandemic in March 2020, the WHO implemented rules for ascertaining when death was due to COVID-19 (i.e. the underlying cause), noting that under certain circumstances COVID-19 should be recorded somewhere on the death certificate.114 While we identified only one COVID-related article (due to the timing of our database search), multiple-cause methods have since been applied to ascertain associations between contributing conditions and complications, assess changes in the pathological patterns, and identify noteworthy sociodemographic variation in COVID-related deaths,115–118 leading in some circumstances to improved survival.119 Importantly, the recent emergence of COVID-19 as a leading underlying cause120 may substantially alter proportional mortality from other underlying causes. As such future analyses of multiple causes will be necessary for monitoring trends in COVID-related mortality as well as the impact of COVID-19 on other causes of death. As well, future sensitivity analyses that assess the impact of removing the nonunderlying condition (by varying the weight ascribed to the underlying cause)69 may facilitate the assessment of competing causes of death where COVID-19 has become a major underlying cause.
Conclusion
The results from this review confirm that international interest in multiple causes of death is ongoing and increasing. This review provides the most comprehensive overview of relevant analytical methods and practices. The diversity of methods offers a toolkit for the analysis of these data, which are becomingly increasingly important for understanding the complex involvement of multiple diseases in causing death across a range of settings including surveillance, policy, planning, and research.
Supplementary Material
Footnotes
This work was supported by the National Health and Medical Research Council of Australia Project Grant (grant number 1163214) and was undertaken in collaboration with the Australian Bureau of Statistics and the Australian Institute of Health and Welfare. Emily Banks is supported by a Principal Research Fellowship from the National Health and Medical Research Council of Australia (reference number 1136128).
The authors report no conflicts of interest.
The review included publicly available original research articles; ethics approval is not relevant for the review. The review was supplemented by consultation with subject experts; ethics protocol was approved by the Australian National University Science and Medical Delegated Ethical Review Committee (Protocol number 2019/022).
The review included publicly available original research articles. Full reference list articles included in full text review is provided in eAppendix, eTable2.
The abstract and references for this article were previously published in an online appendix: International Journal of Epidemiology,dyac167, https://doi.org/10.1093/ije/dyac167
Published: 19 August 2022.
Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.epidem.com).
REFERENCES
- 1.Piffaretti C, Moreno-Betancur M, Lamarche-Vadel A, Rey G. Quantifying cause-related mortality by weighting multiple causes of death. Bull World Health Organ. 2016;94:870–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rao C. Medical certification of cause of death for COVID-19. Bull World Health Organ. 2020;98:298–298A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Desesquelles A, Demuru E, Salvatore MA, et al. Mortality from Alzheimer’s disease, Parkinson’s disease, and dementias in France and Italy: a comparison using the multiple cause-of-death approach. J Aging Health. 2014;26:283–315. [DOI] [PubMed] [Google Scholar]
- 4.Morrell S, Taylor R, Nand D, Rao C. Changes in proportional mortality from diabetes and circulatory disease in Mauritius and Fiji: possible effects of coding and certification. BMC Public Health. 2019;19:481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nguyen-Nielsen M, Moller H, Tjonneland A, Borre M. Causes of death in men with prostate cancer: results from the Danish Prostate Cancer Registry (DAPROCAdata). Cancer Epidemiol. 2019;59:249–257. [DOI] [PubMed] [Google Scholar]
- 6.Pinault L, Brauer M, Crouse DL, et al. Diabetes status and susceptibility to the effects of PM2.5 exposure on cardiovascular mortality in a national Canadian cohort. Epidemiology. 2018;29:784–794. [DOI] [PubMed] [Google Scholar]
- 7.D’Amico M, Agozzino E, Biagino A, Simonetti A, Marinelli P. Ill-defined and multiple causes on death certificates--a study of misclassification in mortality statistics. Eur J Epidemiol. 1999;15:141–148. [DOI] [PubMed] [Google Scholar]
- 8.Mannino DM, Brown C, Giovino GA. Obstructive lung disease deaths in the United States from 1979 through 1993. An analysis using multiple-cause mortality data. Am J Respir Crit Care Med. 1997;156(3 Pt 1):8148148–8148818. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. International statistical classification of diseases and related health problems. - 10th revision, Fifth edition. Vol. 2. World Health Organization; 2016. [Google Scholar]
- 10.Israel RA, Rosenberg HM, Curtin LR. Analytical potential for multiple cause-of-death data. [Review] [59 refs]. Am J Epidemiol. 1986;124:16116179–16116179. [DOI] [PubMed] [Google Scholar]
- 11.Stallard E. Underlying and multiple case mortality advanced ages: United States 1980-1998. N Amer Actuarial J. 2002;6:64–87. [Google Scholar]
- 12.Chamblee RF, Evans MC. New dimensions in cause of death statistics. Am J Public Health. 1982;72:1265–1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Desesquelles A, Salvatore MA, Frova L, et al. Revisiting the mortality of France and Italy with the multiple-cause-of-death approach. Demogr Res. 2010;23:771–805. [Google Scholar]
- 14.Bah S. Using multiple-cause mortality data to resolve conflicting information on trends in maternal mortality in South Africa. S Afr Med J. 2006;96:308. [PubMed] [Google Scholar]
- 15.Bah S, Rahman MM. On measures of association for multiple cause mortality: do we need more measures? Canadian Stud Popul. 2011;38:93–104. [Google Scholar]
- 16.Puffer RR. New approaches for epidemiologic studies of mortality statistics. Bull Pan Am Health Organ. 1989;23:365–383. [PubMed] [Google Scholar]
- 17.Bah S. Measures of multiple-cause mortality: a synthesis and a notational framework. Genus. 2009;65:29–43. [Google Scholar]
- 18.Paik JM, Golabi P, Biswas R, Alqahtani S, Venkatesan C, Younossi ZM. Nonalcoholic fatty liver disease and alcoholic liver disease are major drivers of liver mortality in the United States. Hepatol Commun. 2020;4:890–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodriguez F, Blum MR, Falasinnu T, et al. Diabetes-attributable mortality in the United States from 2003 to 2016 using a multiple-cause-of-death approach. Diabetes Res Clin Pract. 2019;148:169–178. [DOI] [PubMed] [Google Scholar]
- 20.Simmons R, Ireland G, Ijaz S, Ramsay M, Mandal S. Causes of death among persons diagnosed with hepatitis C infection in the pre- and post-DAA era in England: a record linkage study. J Viral Hepat. 2019;26:873–880. [DOI] [PubMed] [Google Scholar]
- 21.Avouac J, Amrouche F, Meune C, Rey G, Kahan A, Allanore Y. Mortality profile of patients with rheumatoid arthritis in France and its change in 10 years. Semin Arthritis Rheum. 2017;46:537–543. [DOI] [PubMed] [Google Scholar]
- 22.Park CB, Yokoyama E, Tokuyama GH. Medical conditions at death among the caucasian and Japanese elderly in Hawaii - analysis of multiple causes of death, 1976-78. J Clin Epidemiol. 1991;44:519–530. [DOI] [PubMed] [Google Scholar]
- 23.Garcia Benavides F, Godoy C, Perez S, Bolumar F. Codificación Múltiple de las Causas de Muerte: de Morir «Por» a Morir «Con». Gac Sanit. 1992;6:53–57. [DOI] [PubMed] [Google Scholar]
- 24.Wall MM, Huang J, Oswald J, McCullen D. Factors associated with reporting multiple causes of death. BMC Med Res Methodol. 2005;5:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zargar AH, Wani AI, Masoodi SR, et al. Causes of mortality in diabetes mellitus: data from a tertiary teaching hospital in India. Postgrad Med J. 2009;85:227–232. [DOI] [PubMed] [Google Scholar]
- 26.Nembhard WN, Pathak EB, Schocken DD. Racial/ethnic disparities in mortality related to congenital heart defects among children and adults in the United States. Ethn Dis. 2008;18:442–449. [PubMed] [Google Scholar]
- 27.Thomas SL, Griffiths C, Smeeth L, Rooney C, Hall AJ. Burden of mortality associated with autoimmune diseases among females in the United Kingdom. Am J Public Health. 2010;100:2279–2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goldacre MJ, Duncan M, Griffith M, Turner MR. Trends in death certification for multiple sclerosis, motor neuron disease, Parkinson’s disease and epilepsy in English populations 1979-2006. J Neurol. 2010;257:706–715. [DOI] [PubMed] [Google Scholar]
- 29.Goldacre MJ, Duncan ME, Griffith M, Cook-Mozaffari P. Psychiatric disorders certified on death certificates in an English population. Soc Psychiatry Psychiatr Epidemiol. 2006;41:409–414. [DOI] [PubMed] [Google Scholar]
- 30.Jansson B, Johansson LA, Rosen M, Svanstrom L. National adaptations of the ICD rules for classification--a problem in the evaluation of cause-of-death trends. J Clin Epidemiol. 1997;50:367–375. [DOI] [PubMed] [Google Scholar]
- 31.Lu TH, Hsiao A, Chang PC, et al. Counting injury deaths: a comparison of two definitions and two countries. Inj Prev. 2013;21(e1):e127–e132. [DOI] [PubMed] [Google Scholar]
- 32.Goldberger N, Applbaum Y, Meron J, Haklai Z. High Israeli mortality rates from diabetes and renal failure - Can international comparison of multiple causes of death reflect differences in choice of underlying cause? Isr J Health Policy Res. 2015;4:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Désesquelles A, Gamboni A, Demuru E, et al. We only die once... but from how many causes? Popul Soc. 2016;534:1–4. [Google Scholar]
- 34.Désesquelles A, Demuru E, Egidi V, Grova L, Meslé F, Pappagallo M, Salvatore MA. Cause-specific mortality analysis: is the underlying cause of death sufficient? Revue Quetel. 2014;2:119–135. [Google Scholar]
- 35.Cummings PL, Kuo T, Javanbakht M, Sorvillo F. Trends, productivity losses, and associated medical conditions among toxoplasmosis deaths in the United States, 2000-2010. Am J Trop Med Hyg. 2014;91:959–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Manton KG, Stallard E, Poss SS. Estimates of U.S. multiple cause life tables. Demography. 1980;17:85–102. [PubMed] [Google Scholar]
- 37.Manton KG, Stallard E. Temporal trends in U. S. multiple cause of death mortality data: 1968 to 1977. Demography. 1982;19:527–547. [PubMed] [Google Scholar]
- 38.Manton KG, Baum HM. CVD mortality, 1968-1978: observations and implications. Stroke. 1984;15:451–457. [DOI] [PubMed] [Google Scholar]
- 39.Manton KG. Cause specific mortality patterns among the oldest old: multiple cause of death trends 1968 to 1980. J Gerontol. 1986;41:282–289. [DOI] [PubMed] [Google Scholar]
- 40.Moussa MA, El Sayed AM, Sugathan TN, Khogali MM, Verma D. Analysis of underlying and multiple-cause mortality data. Genus. 1992;48:89–105. [PubMed] [Google Scholar]
- 41.Makela P. Alcohol-related mortality by age and sex and its impact on life expectancy - Estimates based on the Finnish death register. Eur J Public Health. 1998;8:43–51. [Google Scholar]
- 42.Li SQ, Cunningham J, Cass A. Renal-related deaths in Australia 1997-1999. Intern Med J. 2004;34:259–265. [DOI] [PubMed] [Google Scholar]
- 43.Yoon YH, Stinson FS, Yi HY, Dufour MC. Accidental alcohol poisoning mortality in the United States, 1996-1998. Alcohol Res Health. 2003;27:110–118. [PMC free article] [PubMed] [Google Scholar]
- 44.Mannino DM, Ford E, Giovino GA, Thun M. Lung cancer deaths in the United States from 1979 to 1992: an analysis using multiple-cause mortality data. Int J Epidemiol. 1998;27:159–166. [DOI] [PubMed] [Google Scholar]
- 45.Chamblee RF, Evans MC, Patten DG, Pearce JS. Injuries causing death: their nature, external causes, and associated diseases. J Safety Res. 1983;14:21–35. [Google Scholar]
- 46.McCoy L, Redelings M, Sorvillo F, Simon P. A multiple cause-of-death analysis of asthma mortality in the United States, 1990-2001. J Asthma. 2005;42:757–763. [DOI] [PubMed] [Google Scholar]
- 47.Redelings MD, Wise M, Sorvillo F. Using multiple cause-of-death data to investigate associations and causality between conditions listed on the death certificate. Am J Epidemiol. 2007;166:104–108. [DOI] [PubMed] [Google Scholar]
- 48.Wickramasekaran RN, Sorvillo F, Kuo T. Legionnaires’ disease and associated comorbid conditions as causes of death in the U.S., 2000-2010. Public Health Rep. 2015;130:222–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wilkins K, Parsons GF, Gentleman JF, Forbes WF. Deaths due to dementia: an analysis of multiple-cause-of-death data. Chronic Dis Can. 1999;20:26–35. [PubMed] [Google Scholar]
- 50.Arif N, Yousfi S, Vinnard C. Deaths from necrotizing fasciitis in the United States, 2003-2013. Epidemiol Infect. 2016;144:1338–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Barragan NC, Moschetti K, Smith LV, Sorvillo F, Kuo T. Differential declines in syphilis-related mortality in the United States, 2000-2014. Am J Infect Control. 2017;45:417–420. [DOI] [PubMed] [Google Scholar]
- 52.Croker C, Reporter R, Redelings M, Mascola L. Strongyloidiasis-related deaths in the United States, 1991-2006. Am J Trop Med Hyg. 2010;83:422–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cummings PL, Sorvillo F, Kuo T. Salmonellosis-related mortality in the United States, 1990-2006. Foodborne Pathog Dis. 2010;7:1393–1399. [DOI] [PubMed] [Google Scholar]
- 54.Barragan NC, Sorvillo F, Kuo T. Cryptococcosis-related deaths and associated medical conditions in the United States, 2000-2010. Mycoses. 2014;57:741–746. [DOI] [PubMed] [Google Scholar]
- 55.Rockett IR, Lian Y, Stack S, Ducatman AM, Wang S. Discrepant comorbidity between minority and white suicides: a national multiple cause-of-death analysis. BMC Psychiatry. 2009;9:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rockett IR, Wang S, Lian Y, Stack S. Suicide-associated comorbidity among US males and females: a multiple cause-of-death analysis. Inj Prev. 2007;13:311–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vinnard C, Longworth S, Mezochow A, Patrawalla A, Kreiswirth BN, Hamilton K. Deaths related to nontuberculous mycobacterial infections in the United States, 1999-2014. Ann Am Thorac Soc. 2016;13:1951–1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Whiteside YO, Selik R, An Q, et al. Comparison of rates of death having any death-certificate mention of heart, kidney, or liver disease among persons diagnosed with HIV infection with those in the general US population, 2009-2011. Open AIDS J. 2015;9:14–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fedeli U, Avossa F, Guzzinati S, Bovo E, Saugo M. Trends in mortality from chronic liver disease. Ann Epidemiol. 2014;24:522–526. [DOI] [PubMed] [Google Scholar]
- 60.Desesquelles AF, Salvatore MA, Pappagallo M, et al. Analysing multiple causes of death: which methods for which data? An application to the cancer-related mortality in France and Italy. Eur J Popul Revue Eur De Demographie. 2012;28:467–498. [Google Scholar]
- 61.Adair T, Lopez AD. The role of overweight and obesity in adverse cardiovascular disease mortality trends: an analysis of multiple cause of death data from Australia and the USA. BMC Med. 2020;18:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yoon YH, Chen CM, Yi HY, Moss HB. Effect of comorbid alcohol and drug use disorders on premature death among unipolar and bipolar disorder decedents in the United States, 1999 to 2006. Compr Psychiatry. 2011;52:453–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Villela PB, Klein CH, Oliveira GMM. Cerebrovascular and hypertensive diseases as multiple causes of death in Brazil from 2004 to 2013. Public Health. 2018;161:36–42. [DOI] [PubMed] [Google Scholar]
- 64.Barbieri M, Desesquelles A, Egidi V, et al. Obesity-related mortality in France, Italy, and the United States: a comparison using multiple cause-of-death analysis. Int J Public Health. 2017;62:623–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Alexander MJ, Kiang MV, Barbieri M. Trends in black and white opioid mortality in the United States, 1979-2015. Epidemiology. 2018;29:707–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Egidi V, Salvatore MA, Rivellini G, D’Angelo S. A network approach to studying cause-of-death interrelations. Demogr Res. 2018;38:373–400. [Google Scholar]
- 67.Jiang H, Wu H, Wang MD. Causes of death in the United States, 1999 to 2014. 2017 IEEE EMBS International Conference on Biomedical and Health Informatics, BHI. 2017;177–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hassanzadeh HR, Sha Y, Wang MD. DeepDeath: Learning to predict the underlying cause of death with big data. 2017 39th Annual International Conference of the Ieee Engineering in Medicine and Biology Society. IEEE; 2017:3373–3376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Moreno-Betancur M, Sadaoui H, Piffaretti C, Rey G. Survival analysis with multiple causes of death extending the competing risks model. Epidemiology. 2017;28:12–19. [DOI] [PubMed] [Google Scholar]
- 70.Gonzalez LF, Jo AHS, Garcia CAR. Weighted mortality method according to multiple causes of death. Finlay. 2019;9:197–209. [Google Scholar]
- 71.Breger TL, Edwards JK, Cole SR, et al. Estimating a set of mortality risk functions with multiple contributing causes of death. Epidemiology. 2020;31:704–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Xie SH, Chen H, Lagergren J. Causes of death in patients diagnosed with gastric adenocarcinoma in Sweden, 1970-2014: a population-based study. Cancer Sci. 2020;111:2451–2459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bishop KA, Moreno-Betancur M, Balogun S, et al. Quantifying cause-related mortality in Australia incorporating multiple causes: observed patterns, trends, and practical considerations. Int J Epidemiology. 2022;52:284–294. doi: 10.1093/ije/dyac167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rao C, Adair T, Bain C, Doi SA. Mortality from diabetic renal disease: a hidden epidemic. Eur J Public Health. 2011;22:280–284. [DOI] [PubMed] [Google Scholar]
- 75.Lu TH, Hsu PY, Bjorkenstam C, Anderson RN. Certifying diabetes-related cause-of-death: a comparison of inappropriate certification statements in Sweden, Taiwan and the USA. Diabetologia. 2006;49:2878–2881. [DOI] [PubMed] [Google Scholar]
- 76.Adair T, Rao C. Changes in certification of diabetes with cardiovascular diseases increased reported diabetes mortality in Australia and the United States. J Clin Epidemiol. 2010;63:199–204. [DOI] [PubMed] [Google Scholar]
- 77.Trabsky M, Hempton C. “Died from” or “died with” COVID-19? We need a transparent approach to counting coronavirus deaths. Conversation. 2020. https://theconversation.com/died-from-or-died-with-covid-19-we-need-a-transparent-approach-to-counting-coronavirus-deaths-145438. [Google Scholar]
- 78.Slater TA, Straw S, Drozd M, Kamalathasan S, Cowley A, Witte KK. Dying “due to” or “with” COVID-19: a cause of death analysis in hospitalised patients. Clin Med (Lond). 2020;20:e189–e190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Oliver D. David Oliver: Mistruths and misunderstandings about COVID-19 death numbers. BMJ. 2021;372:n352. [DOI] [PubMed] [Google Scholar]
- 80.Shiue KY, Naumann RB, Proescholdbell S, Cox ME, Aurelius M, Austin AE. Differences in overdose deaths by intent: unintentional & suicide drug poisonings in North Carolina, 2015-2019. Prev Med. 2022;163:107217. [DOI] [PubMed] [Google Scholar]
- 81.Trinidad JP, Warner M, Bastian BA, Minino AM, Hedegaard H. Using literal text from the death certificate to enhance mortality statistics: characterizing drug involvement in deaths. Natl Vital Stat Rep. 2016;65:1–15. [PubMed] [Google Scholar]
- 82.Australian Bureau of Statistics. Psychosocial risk factors as they relate to coroner-referred deaths in Australia [Internet]. ABS; 2019. [Google Scholar]
- 83.Goldacre MJ, Duncan ME, Griffith M. Death rates for asthma in English populations 1979-2007: comparison of underlying cause and all certified causes. Public Health. 2012;126:386–393. [DOI] [PubMed] [Google Scholar]
- 84.Jansson B, Ahmed N. Epilepsy and injury mortality in Sweden--the importance of changes in coding practice. Seizure. 2002;11:361–370. [DOI] [PubMed] [Google Scholar]
- 85.Chitty KM, Schumann JL, Moran LL, Chong DG, Hurzeler TP, Buckley NA. Reporting of alcohol as a contributor to death in Australian national suicide statistics and its relationship to post-mortem alcohol concentrations. Addiction. 2021;116:506–513. [DOI] [PubMed] [Google Scholar]
- 86.Kiadaliri AA, Petersson IF, Englund M. Educational inequalities in mortality associated with rheumatoid arthritis and other musculoskeletal disorders in Sweden. BMC Musculoskelet Disord. 2019;20:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kiadaliri AA, Rosengren BE, Englund M. Fracture-related mortality in southern Sweden: a multiple cause of death analysis, 1998-2014. Injury. 2018;49:236–242. [DOI] [PubMed] [Google Scholar]
- 88.Turner C, Chandrakumar D, Rowe C, Santos GM, Riley ED, Coffin PO. Cross-sectional cause of death comparisons for stimulant and opioid mortality in San Francisco, 2005-2015. Drug Alcohol Depend. 2018;185:305–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Parks SE, Kegler SR, Annest JL, Mercy JA. Characteristics of fatal abusive head trauma among children in the USA: 2003-2007: an application of the CDC operational case definition to national vital statistics data. Inj Prev. 2012;18:193–199. [DOI] [PubMed] [Google Scholar]
- 90.Fedeli U, Grande E, Grippo F, Frova L. Mortality associated with hepatitis C and hepatitis B virus infection: a nationwide study on multiple causes of death data. World J Gastroenterol. 2017;23:1866–1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ford MM, Desai PS, Maduro G, Laraque F. Neighborhood inequalities in Hepatitis C mortality: spatial and temporal patterns and associated factors. J Urban Health. 2017;94:746–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Grande E, Zucchetto A, Suligoi B, et al. Multiple cause-of-death data among people with AIDS in Italy: a nationwide cross-sectional study. Popul Health Metr. 2017;15:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pechholdova M. Sepsis-related mortality in the Czech Republic: multiple causes of death analysis. Epidemiol Mikrobiol Imunol. 2017;66:73–79. [PubMed] [Google Scholar]
- 94.da Silva LR, Araújo ETH, Carvalho ML, et al. Epidemiological situation of acquired immunodeficiency syndrome (Aids)-related mortality in a municipality in northeastern brazil. a retrospective cross-sectional study. Sao Paulo Med J. 2018;136:37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Duncan ME, Pitcher A, Goldacre MJ. Atrial fibrillation as a cause of death increased steeply in England between 1995 and 2010. Europace. 2014;16:797–802. [DOI] [PubMed] [Google Scholar]
- 96.Garcia-Ptacek S, Kareholt I, Cermakova P, Rizzuto D, Religa D, Eriksdotter M. Causes of death according to death certificates in individuals with dementia: a cohort from the Swedish dementia registry. J Am Geriatr Soc. 2016;64:e137–e142. [DOI] [PubMed] [Google Scholar]
- 97.Takamori A, Takahashi I, Kasagi F, Suyama A, Ozasa K, Yanagawa T. Mortality analysis of the Life Span Study (LSS) cohort taking into account multiple causes of death indicated in death certificates. Radiat Res. 2017;187:20–31. [DOI] [PubMed] [Google Scholar]
- 98.Seuc AH, Fernandez-Gonzalez L, Mirabal M. Comparative disease assessment: a multi-causal approach for estimating the burden of mortality. J Public Health. 2020;30:665–673. [Google Scholar]
- 99.Amaral TLM, Amaral CA, Miranda Filho AL, Monteiro GTR. Trends and multiple causes of death due to chronic renal failure in a municipality in the Brazilian Amazon. Cien Saude Colet. 2018;23:3821–3828. [DOI] [PubMed] [Google Scholar]
- 100.Fedeli U, Schievano E, Lisiero M, Avossa F, Mastrangelo G, Saugo M. Descriptive epidemiology of chronic liver disease in northeastern Italy: an analysis of multiple causes of death. Popul Health Metr. 2013;11:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Fedeli U, Schievano E, Targher G, Bonora E, Corti MC, Zoppini G. Estimating the real burden of cardiovascular mortality in diabetes. Eur Rev Med Pharmacol Sci. 2019;12:6700–6706. [DOI] [PubMed] [Google Scholar]
- 102.Redelings MD, Lee NE, Sorvillo F. Pressure ulcers: more lethal than we thought? Adv Skin Wound Care. 2005;18:367–372. [DOI] [PubMed] [Google Scholar]
- 103.Ramos AN, Jr, Matida LH, Hearst N, Heukelbach J. Mortality in Brazilian children with HIV/AIDS: the role of non-AIDS-related conditions after highly active antiretroviral therapy introduction. AIDS Patient Care STDS. 2011;25:713–718. [DOI] [PubMed] [Google Scholar]
- 104.Chang CY, Lu TH, Cheng TJ. Trends in reporting injury as a cause of death among people with epilepsy in the U.S., 1981-2010. Seizure. 2014;23:836–843. [DOI] [PubMed] [Google Scholar]
- 105.Grippo F, Pappagallo M, Burgio A, Crialesi R. Drug induced mortality: a multiple cause approach on italian causes of death register. Epidemiol Biostat Public Health. 2015;12:e–1. [Google Scholar]
- 106.Laanani M, Viallon V, Coste J, Rey G. Collider and Reporting Biases Involved in the Analyses of Cause of Death Associations in Death Certificates: an Illustration with Cancer and Suicide. Prepr Res Square. 2021:1–18. doi:10.21203/rs.3.rs-377726/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Newcomer SR, Steiner JF, Bayliss EA. Identifying subgroups of complex patients with cluster analysis. Am J Manag Care. 2011;17:e324–e332. [PubMed] [Google Scholar]
- 108.Frova L, Salvatore MA, Pappagallo M, Egidi V. The multiple cause of death approach to analyse mortality patterns. Genus. 2009;65:1–21. [Google Scholar]
- 109.Roso-Llorach A, Violán C, Foguet-Boreu Q, et al. Comparative analysis of methods for identifying multimorbidity patterns: a study of ‘real-world’data. BMJ open. 2018;8:e018986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Mabon K, Steinum O, Chute CG. Postcoordination of codes in ICD-11. BMC Med Inform Decis Mak. 2022;21(Suppl 6):379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.World Health Organization. International Classification of Diseases Eleventh Revision (ICD-11). World Health Organization; 2022. [Google Scholar]
- 112.Domingues CSB, Waldman EA. Causes of death among people living with AIDS in the Pre- and Post-HAART eras in the city of S(a)over-tildeo Paulo, Brazil. PLoS One. 2014;9:e114661e114661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Goldstein E, Lipsitch M. The relation between prescribing of different antibiotics and rates of mortality with sepsis in US adults. BMC Infect Dis. 2020;20:169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.World Health Organization. International Guidleines for Certification and Classification (Coding) of COVID-19 as Cause of Death. World Health Organization; 2020. [Google Scholar]
- 115.Grippo F, Navarra S, Orsi C, et al. ; Italian National Institute of Health Covid-Mortality G. The role of COVID-19 in the death of SARS-CoV-2-positive patients: a study based on death certificates. J Clin Med. 2020;9:3459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Christensen RAG, Arneja J, St Cyr K, Sturrock SL, Brooks JD. The association of estimated cardiorespiratory fitness with COVID-19 incidence and mortality: a cohort study. PLoS One. 2021;16:e0250508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Nogales Vasconcelos AM, Ishitani L, Abreu DMX, Franca E. Covid adult mortality in Brazil: an analysis of multiple causes of death. Front Public Health. 2021;9:788932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Woodward M, Peters SAE, Harris K. Social deprivation as a risk factor for COVID-19 mortality among women and men in the UK Biobank: nature of risk and context suggests that social interventions are essential to mitigate the effects of future pandemics. J Epidemiol Community Health. 2021;75:1050–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Grippo F, Grande E, Maraschini A, et al. ; Italian National Institute of Health C-MG. Evolution of pathology patterns in persons who died from COVID-19 in Italy: a national study based on death certificates. Front Med (Lausanne). 2021;8:645543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Woolf SH, Chapman DA, Lee JH. COVID-19 as the leading cause of death in the United States. JAMA. 2021;325:123–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.