Abstract
Profound knowledge of nerve variations is essential for clinical practice. It is crucial for interpreting the large variability of a patient's clinical presentation and the different mechanisms of nerve injury. Awareness of nerve variations facilitates surgical safety and efficacy. Clinically significant anatomical variations can be classified into two main groups: variability in the course of the nerve and variability of structures surrounding the nerve. In this review article we focus on the most common nerve variants of the upper extremity and their clinical relevance.
Keywords: Keywords, nerve variants, median nerve, ulnar nerve, neuropathy
Anatomical variations of the peripheral nerves are important because they may have clinical consequences. In general, they are classified into two groups: The first is variation of the nerve course or distribution. This scenario can lead to diagnostic mistakes and even surgical errors, a challenge preoperatively or intraoperatively. Preoperative errors may result from an incorrect diagnosis or localization of a nerve lesion, leading to a misguided surgical plan. If surgical decisions are based on regular anatomical assumptions without being mindful of anatomical variations, intraoperative errors may arise.
The second group of anatomical variations is associated with structures surrounding the nerve (e.g., accessory muscles, ligaments, or osseous foramina) that may compress or entrap nerves, leading to focal mononeuropathies. 1 We discuss some of the most common variations of the main nerves of the upper extremity after their division from the brachial plexus.
Median Nerve
There are numerous communicating branches between the nerves of the upper extremity. Most commonly, the communications arise between the anterior division of nerves that share similar spinal origins, such as the musculocutaneous nerve (MCN) with the median nerve (MN) and the MN with the ulnar nerve (UN). 2
The incidence of communicating branches between the MN and the MCN is approximately 10 to 54%. In most cases, a branch of the MCN joins to the MN. 3 Usually a single fascicle joins the nerve. 4 5 6 Knowledge of the existence of communicating branches between those two nerves is relevant for clinical practice. It allows assessment and appropriate management of disorders of the upper limbs caused by peripheral nerve lesions and allows proper planning of the surgical approach.
Variations at the elbow mainly impact the relationship between the MN and the pronator teres muscle. In most cases (95%), the nerve passes between both heads of the pronator teres muscle. Rarely, the MN passes between the pronator teres muscle and the flexor digitorum profundus muscle, or it goes through the humeral head of the muscle or the brachialis muscle.
The occurrence of anatomical variations of the coracobrachialis muscle, including the presence of an additional head attaching to the distal humerus or medial epicondyle, may also result in potential compression on the MN and the MCN, especially during surgical procedures. 7 8 Compression can also occur between the two heads of the pronator teres, as well as the site where the MN crosses the palmaris longus tendon. 9 10 An accessory head of the flexor pollicis longus (Gantzer's muscle) may also lead to entrapment neuropathy of the anterior interosseous nerve (AIN). The muscle was found in 20 to 50% of extremities and was supplied by the AIN. It arose from the medial humeral epicondyle in 85% of extremities and had a dual origin from the epicondyle and coronoid process in the remaining 15% and inserted to the ulnar part of the flexor pollicis longus and its tendon. Gantzer's muscle is always located posterior to both the MN and AIN; therefore it should be considered in MN and AIN compressions due to its proximity to these nerves. 11 12 When Struthers' ligament (an anatomical variation found in 1–3% of the population) is present, the MN passes behind it, possibly a further potential compression site. 13 14
In 1977 Lanz published a detailed anatomical study investigating the course of the MN in 246 hands by extensive anatomical dissection. In 12%, a variation of the branching of the MN was found. Accessory branches of the MN in the distal carpal tunnel were found in 7%. In 3%, a high division of the MN was observed. In 2%, accessory branches proximal to the carpal tunnel were seen. 15 16 17
The branches of the MN in the hand region may also show variability. An often found variation of the MN at the carpal tunnel is the bifid MN. It has a prevalence of ∼ 15.4% in the normal population. 18 Whether the bifid MN increases the risk of developing carpal tunnel syndrome (CTS) is questionable, but it is important to know that in sonographic assessment of CTS, the bifid MN has a higher cut-off value. Values of up to 4 mm 2 are considered “normal” compared with 2.5 mm 2 in normal MN 19 20 21 22 ( Fig. 1 ).
Fig. 1.
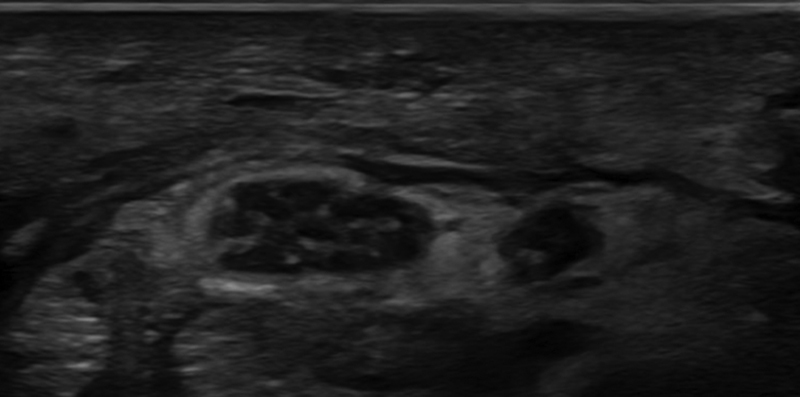
Axial ultrasonographic image of a swollen bifid median nerve inside the carpal tunnel.
Together with a bifid MN, a persistent median artery (PMA) can be seen in some cases. There are reports of a median artery not located dorsal to the flexor retinaculum (FR). Feintisch et al 23 found the PMA was interposed between the palmar aponeurosis and the FR. It was accompanied by two concomitant veins, positioned directly in line with the incision for carpal tunnel release. Although rare, surgeons must be aware of this anatomical variation to prevent inadvertent injury to what may be an important vascular supply to the distal MN ( Fig. 2 ).
Fig. 2.
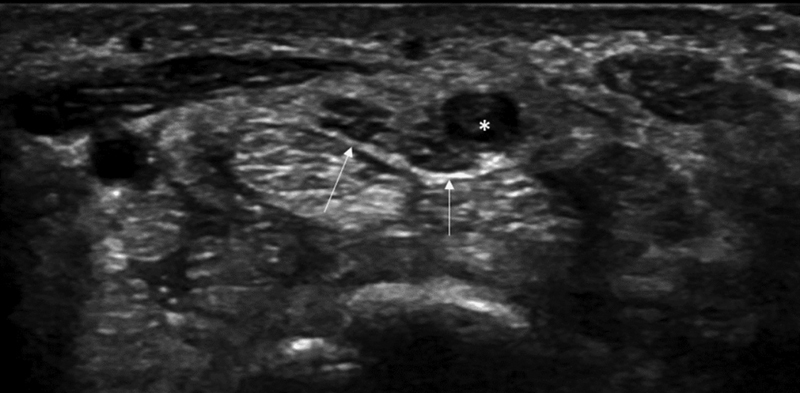
A 35-year-old man with acute onset of severe symptoms of carpal tunnel syndrome. Axial ultrasonographic image at the entrance of the carpal tunnel shows a bifurcated-bifid median nerve (arrows) with a persistent median artery (asterisk) that is significantly enlarged due to thrombosis.
Chiew et al 24 reported an anatomical variation of the palmar cutaneous branch of the median nerve (PCBMN) that coursed superficially and radially to the flexor carpi radialis tendon, reinforcing the need for meticulous subcutaneous dissection to protect the nerve during a volar approach to the distal radius. In this case, identification of the PCBMN variant warranted a modified surgical approach, ulnar to the flexor carpi radialis instead of radial to avoid iatrogenic injury.
In addition to the variable courses of the MN in the hand region are some very important and frequently encountered anastomoses.
Martin-Gruber Anastomosis
In a study by Sur et al, 25 the Martin-Gruber anastomosis (MGA) occurred with a prevalence of 15.7%. The MGA emerges as a communicating branch in the cubital fossa from the main trunk of the MN, crossing superficially to the flexor digitorum superficialis or flexor digitorum profundus muscles before joining the UN. The MGA is mainly reported to supply motoric innervation of the thenar, hypothenar, and dorsal interosseous muscles; however, some sensory fibers have also been identified with variable clinical presentations. 26 27
Riché-Cannieu Anastomosis
The Riché-Cannieu anastomosis (RCA) has a prevalence of 55.5%. 26 The RCA is a palmar anastomosis between the recurrent branch of the MN and the deep branch of the UN, combining fibers of the UN with the MN, leading to innervation of the thenar muscles. 28
Berrettini Anastomosis
The Berrettini anastomosis is an ulnar-to-median sensory nerve connection with a reported prevalence of 61%. 26 With its superficial position and close relation to the FR, usually at the region of the third digit, it is particularly vulnerable to iatrogenic injuries. Although it is usually clinically silent, it may be associated with atypical patterns of sensory innervation leading to a complex neurologic assessment and unexpected patterns of sensory disturbance. 29 30
The presence of such anastomoses may risk iatrogenic injury during surgical procedures and make it difficult to interpret electrophysiologic studies in the diagnosis of neuropathies. These anatomical variations must be differentiated from incomplete nerve lesions. The innervation variations of these small muscles are of high clinical importance because in the case of a complete lesion of the MN or UN, some of these muscles may or may not be paralyzed, possibly leading to the erroneous conclusion of a partial rather than complete lesion. 28 31
Profound knowledge of these anastomoses is essential for accurate interpretation of clinical findings and to avoid the risk of iatrogenic injuries during surgical procedures. 32
Musculocutaneous Nerve
The MCN, after passing under the pectoralis minor muscle, enters a narrow space located between the coracobrachialis muscle and the upper third of the humerus. It can undergo dynamic compression at this location, causing paresthesia in the anterolateral surface of the forearm. This rare compression occurs in athletes and bodybuilders due to muscle hypertrophy, presenting pain in the anterior face of the arm and atrophy of the anterior surface of the arm muscles (biceps and brachial) in chronic stages. The presence of fibrous bands between the biceps and brachial muscles may compress the MCN. 6
Variations in the course of the MCN are quite common and occur in ∼ 11% of patients. 33 A number of variations in the anatomy of the MCN have been described and were classified by Le Minor 34 including variations in the origin of the MCN and MN. Type I is defined by a lack of communication between the MCN and MN and reported as the most common formation of the MN. In type II, some fibers of the lateral cord contribute to the MN, pass through the MCN, and join the MN at a second point distally in the midarm. In type III, fibers of the lateral cord contribute to the MN, pass along the MCN, and exit to form the lateral cord of the MN. Type IV is defined by fibers of the MCN coalescing with the lateral cord to the MN before the MCN arises from the MN properly more distally. In type V, there is no proper MCN, and branches of the MCN appear to arise from the coalesced MCN and MN 33 ( Fig. 3 ).
Fig. 3.
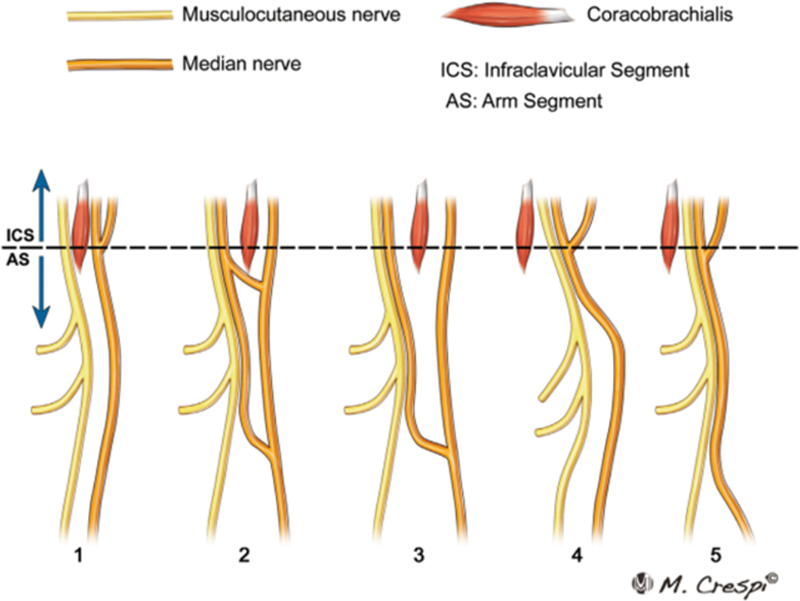
Communicating branches between the median nerve and the musculocutaneous nerve.
In the case of a missing MCN, the MN innervates the muscles of the anterior flexor compartments of the arms including the biceps brachii and brachialis. The lateral cutaneous nerve of the forearm can also derive from the MN. In a proximal MN injury, a variation of an absent MCN may not only result in typical MN palsy of the forearm and hand, but also palsy in the arm that manifests as deficiencies in both shoulder and elbow flexion, as well as cutaneous sensory loss of the lateral forearm. 35 36
Ulnar Nerve
The UN is the major branch of the medial cord of the brachial plexus. It contains fibers of the C8 and T1 root, but it often receives additional contribution of the C7 root. In the axilla, the UN is located medial to the axillary artery, and at a high humeral level it remains close and medial to the brachial artery. 37
From its origin it moves distally and penetrates the anterior compartment of the upper arm and then crosses from the anterior compartment to the posterior compartment through the medial intermuscular septum. During its posterior course, it descends vertically to enter the ulnar groove. 38
Anomalous formations of the UN and its unusual communication to neighboring nerves in the axilla at a high humeral level should be noted because they may present a complicating factor during surgical procedures. 37
At the ulnar groove are two important anatomical variations that may lead to entrapment of the UN: Osborn's ligament and Struthers' ligament and arcade.
Osborne's ligament is a band of tissue that connects the two heads of the flexor carpi ulnaris and thus forms the roof of the cubital tunnel. 39 Karatas et al 40 reported an incidence of ∼ 8%, but overall, the numbers are very inconsistent in the literature.
The second variation is Struthers' ligament or arcade. The Struthers' ligament is a fibrous band that originates from the supracondylar humeral process and inserts into the medial humeral epicondyle, potentially compressing the MN, UN, and brachial artery.
Furthermore, a supracondylar process of the humerus has been described by anatomists and anthropologists; it is considered phylogenetically a vestige of the supracondylar foramen, found in reptiles, marsupials, and some mammals. Its occurrence in humans is very rare, observed in 0.7 to 2.5% of the population 41 ( Fig. 4 ).
Fig. 4.
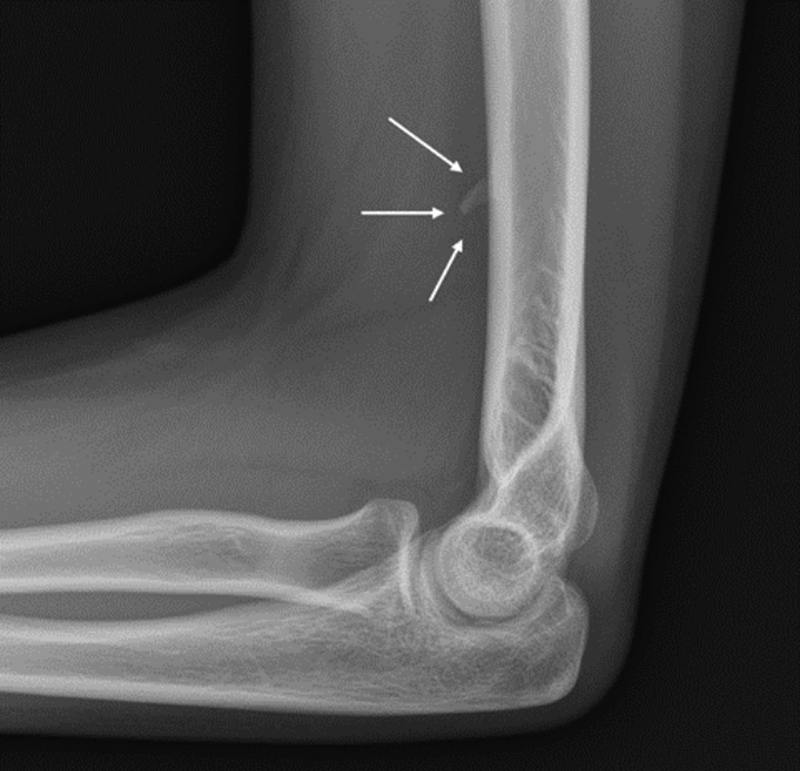
Radiograph of an accessory supracondylar process (arrows).
Struthers' arcade is a musculotendinous structure extending from the medial intermuscular septa to the medial head of the triceps brachii muscle at a variable distance above the medial humeral epicondyle that might compress the UN.
In a meta-analysis by Mizia et al, the overall estimated pooled prevalence of the ligament was 1.8% and was 52.6% for the arcade. 42
The presence of accessory muscles like the anconeus epitrochlearis muscle, thought to be a muscular execution of Osborne's ligament, is important because it can lead to nerve entrapment. It occurs in > 18% of the European population 43 44 ( Fig. 5 ).
Fig. 5.
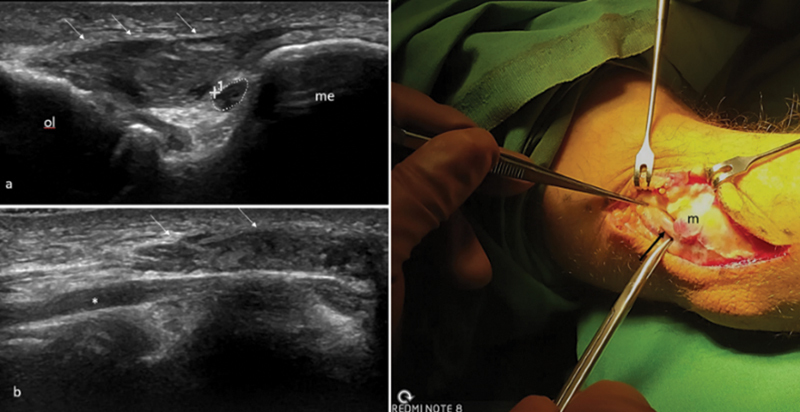
A 45-year-old patient with symptoms of mild ulnar neuropathy. ( a ) Axial ultrasonographic (US) image and ( b ) longitudinal US image of the cubital tunnel shows a large anomalous anconeus epitrochlearis muscle (arrows), extending between the olecranon (ol) and the medial epicondyle (me) overlying a slightly enlarged ulnar nerve (asterisk) (cross-sectional area = 10 mm 2 ). ( c ) Photograph taken during surgical decompression of the cubital tunnel, confirming the presence of the large anomalous muscle belly (m) and the ulnar nerve (arrow) lying deep to it.
Most Variations of the UN Occur in the Hand Region
Descending from the arm, the UN enters the hand via Guyon's canal, situated between the pisiform bone and the hook of the hamate in the proximal hypothenar. Within Guyon's canal, the UN usually lies beneath the ulnar artery and concomitant veins. It measures ∼ 40 to 45 mm in length, extending from the proximal edge of the palmar carpal ligament to the fibrous arch of the hypothenar muscles at the level of the hook of the hamate. 45 Within the Guyon's canal, the UN usually lies beneath the ulnar artery and veins.
Murata et al 46 classified the various division patterns of the UN inside the Guyon's canal. The most frequent pattern is bifurcation of the UN into a deep motoric branch and a superficial trunk distal to the pisiform bone. The superficial trunk further divides into the ring finger common digital nerve and the ulnar proper digital nerve of the little finger. This type has a frequency of occurrence from 66% to 86%. The main ulnar trunk may trifurcate into a deep motor branch, the fourth common digital nerve and the ulnar proper palmar digital nerve of the little finger just past the distal border of the pisiform bone. Trifurcation of the UN has been described in the literature, occurring in 13 to 22% of people. 45 47
Aberrant positioning of the UN inside the carpal tunnel is a rare anatomical variation. A few studies have described this unusual variation with an incidence < 0.1%. Awareness of this anatomical variation and adequate visualization of the UN, along with the surrounding structures, is crucial to avoid iatrogenic injuries during carpal tunnel release. 48 49
There are also cases of aberrant transligamentous sensory branches of the UN entering the distal transverse carpal ligament. Hand surgeons should be aware of this anatomical variation because its location puts it at risk of iatrogenic injury during open and endoscopic carpal tunnel release. 50
The anatomy of the ulnar-palmar region of the wrist is complex and bears numerous different anatomical variations. Therefore, sonography should be used to assess related disorders and interventional planning. 51
Radial Nerve
The radial nerve (RN) is the main branch of the posterior cord of the brachial plexus. It gives branches to the medial head of triceps before passing through the lower triangular space to enter the posterior compartment of the arm. After supplying the long head of triceps, it crosses to the posterior surface of the humerus in the spiral groove where it gives branches to the lateral head of triceps and anconeus. Then it pierces the lateral intermuscular septum to enter the anterior compartment of the arm. At the level of the lateral epicondyle, it divides into superficial and deep branches. 52 Depending on the location of the RN on the humerus or the spot where it pierces the intermuscular septum, it may be at risk during operative procedures of the humerus (e.g., in fixation of a humerus fracture). 53
At the level of the elbow, the RN usually divides into a superficial branch (SB) and a deep branch. An accessory brachioradialis muscle can cause entrapment in that region. 54 The SB originates from the cubital fossa and continues distally along the forearm accompanying the radial vessels, covered by the belly of the brachioradialis muscle. It leaves the lateral compartment of the forearm by penetrating the antebrachial fascia, branches numerously, and continues distally within the subcutaneous tissue over tendons surrounding the radial foveola at the wrist, innervating the dorsolateral aspect of the hand and the lateral two and half fingers. 55 Overall, eight innervation patterns have been described regarding the innervation of the dorsal hand or the fingers. 56 A rare variation is a duplicated SB with a duplicated brachioradialis muscle. It occurs with a prevalence of ∼ 1.4% and may cause complications while performing various surgical procedures in the forearm. Moreover, it might be a rare cause of Wartenberg's syndrome. 55 An SB penetrating the brachioradialis muscle also increases the risk of Wartenberg's syndrome. 57
Summary
US with its high-resolution capabilities is a unique imaging modality, able to identify small branches and variability in the course of nerves and surrounding structures. However, more work is needed to explore how US can contribute to a better understanding of clinical presentations, as well as pre- and postoperative evaluation.
Footnotes
Conflict of Interest None declared.
References
- 1.Mahan M, Spinner R. Philadelphia, PA: Elsevier; 2015. Clinical importance of anatomic variation of the nerves of the upper extremity. [Google Scholar]
- 2.Tagliafico A, Cadoni A, Fisci E. Nerves of the hand beyond the carpal tunnel. Semin Musculoskelet Radiol. 2012;16(02):129–136. doi: 10.1055/s-0032-1311764. [DOI] [PubMed] [Google Scholar]
- 3.Guerri-Guttenberg R A, Ingolotti M. Classifying musculocutaneous nerve variations. Clin Anat. 2009;22(06):671–683. doi: 10.1002/ca.20828. [DOI] [PubMed] [Google Scholar]
- 4.Choi D, Rodríguez-Niedenführ M, Vázquez T, Parkin I, Sañudo J R. Patterns of connections between the musculocutaneous and median nerves in the axilla and arm. Clin Anat. 2002;15(01):11–17. doi: 10.1002/ca.1085. [DOI] [PubMed] [Google Scholar]
- 5.Loukas M, Aqueelah H. Musculocutaneous and median nerve connections within, proximal and distal to the coracobrachialis muscle. Folia Morphol (Warsz) 2005;64(02):101–108. [PubMed] [Google Scholar]
- 6.Caetano E B, Vieira LÂ, Cavalheiro C S, Razuk M, Almargo M A, Caetano M F. Anatomic Study of the nervous communication between the median and musculocutaneous nerve. Acta Ortop Bras. 2016;24(04):200–203. doi: 10.1590/1413-785220162404159372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olewnik Ł, Zielinska N, Karauda P, Duparc F, Georgiev G P, Polguj M. The co-occurrence of a four-headed coracobrachialis muscle, split coracoid process and tunnel for the median and musculocutaneous nerves: the potential clinical relevance of a very rare variation. Surg Radiol Anat. 2021;43(05):661–669. doi: 10.1007/s00276-020-02580-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olewnik Ł, Paulsen F, Tubbs R S. Potential compression of the musculocutaneous, median and ulnar nerves by a very rare variant of the coracobrachialis longus muscle. Folia Morphol (Warsz) 2021;80(03):707–713. doi: 10.5603/FM.a2020.0085. [DOI] [PubMed] [Google Scholar]
- 9.Olewnik Ł, Wysiadecki G, Polguj M, Podgórski M, Jezierski H, Topol M. Anatomical variations of the palmaris longus muscle including its relation to the median nerve—a proposal for a new classification. BMC Musculoskelet Disord. 2017;18(01):539. doi: 10.1186/s12891-017-1901-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olewnik Ł, Podgórski M, Polguj M, Wysiadecki G, Topol M. Anatomical variations of the pronator teres muscle in a Central European population and its clinical significance. Anat Sci Int. 2018;93(02):299–306. doi: 10.1007/s12565-017-0413-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Torun Bİ, Balaban M. Prevalence and clinical implications of the Gantzer's muscle. Surg Radiol Anat. 2022;44(09):1297–1303. doi: 10.1007/s00276-022-03006-6. [DOI] [PubMed] [Google Scholar]
- 12.al-Qattan M M. Gantzer's muscle. An anatomical study of the accessory head of the flexor pollicis longus muscle. J Hand Surg [Br] 1996;21(02):269–270. doi: 10.1016/s0266-7681(96)80114-8. [DOI] [PubMed] [Google Scholar]
- 13.Nulle K, Jaudzema A. Ultrasonographic evaluation of the median nerve: normal and variant anatomy and appearance. J Ultrason. 2021;21(87):e318–e325. doi: 10.15557/JoU.2021.0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Soubeyrand M, Melhem R, Protais M, Artuso M, Crézé M. Anatomy of the median nerve and its clinical applications. Hand Surg Rehabil. 2020;39(01):2–18. doi: 10.1016/j.hansur.2019.10.197. [DOI] [PubMed] [Google Scholar]
- 15.Lanz U. Anatomical variations of the median nerve in the carpal tunnel. J Hand Surg Am. 1977;2(01):44–53. doi: 10.1016/s0363-5023(77)80009-9. [DOI] [PubMed] [Google Scholar]
- 16.Kadar I A, Virág T H, Matei I R, Georgescu A V. High division of the median nerve with unusually high origin of the 3rd space common digital nerve. Injury. 2020;51 04:S96–S102. doi: 10.1016/j.injury.2020.03.024. [DOI] [PubMed] [Google Scholar]
- 17.Demircay E, Civelek E, Cansever T, Kabatas S, Yilmaz C. Anatomic variations of the median nerve in the carpal tunnel: a brief review of the literature. Turk Neurosurg. 2011;21(03):388–396. doi: 10.5137/1019-5149.JTN.3073-10.1. [DOI] [PubMed] [Google Scholar]
- 18.Granata G, Caliandro P, Pazzaglia C. Prevalence of bifid median nerve at wrist assessed through ultrasound. Neurol Sci. 2011;32(04):615–618. doi: 10.1007/s10072-011-0582-8. [DOI] [PubMed] [Google Scholar]
- 19.Klauser A S, Halpern E J, De Zordo T. Carpal tunnel syndrome assessment with US: value of additional cross-sectional area measurements of the median nerve in patients versus healthy volunteers. Radiology. 2009;250(01):171–177. doi: 10.1148/radiol.2501080397. [DOI] [PubMed] [Google Scholar]
- 20.Klauser A S, Halpern E J, Faschingbauer R. Bifid median nerve in carpal tunnel syndrome: assessment with US cross-sectional area measurement. Radiology. 2011;259(03):808–815. doi: 10.1148/radiol.11101644. [DOI] [PubMed] [Google Scholar]
- 21.Klauser A S, Faschingbauer R, Bauer T. Entrapment neuropathies II: carpal tunnel syndrome. Semin Musculoskelet Radiol. 2010;14(05):487–500. doi: 10.1055/s-0030-1268069. [DOI] [PubMed] [Google Scholar]
- 22.Klauser A S, Buzzegoli T, Taljanovic M S. Nerve entrapment syndromes at the wrist and elbow by sonography. Semin Musculoskelet Radiol. 2018;22(03):344–353. doi: 10.1055/s-0038-1641577. [DOI] [PubMed] [Google Scholar]
- 23.Feintisch A M, Ayyala H S, Datiashvili R. An anatomic variant of persistent median artery in association with carpal tunnel syndrome: case report and review of the literature. J Hand Surg Asian Pac Vol. 2017;22(04):523–525. doi: 10.1142/S0218810417720388. [DOI] [PubMed] [Google Scholar]
- 24.Chiew J, Satkunanantham M, Sechachalam S. An anatomical variant of the palmar cutaneous branch of the median nerve: a case report. J Hand Surg Asian Pac Vol. 2022;27(01):191–194. doi: 10.1142/S242483552272002X. [DOI] [PubMed] [Google Scholar]
- 25.Sur A, Sinha M M, Ughade J M. Prevalence of Martin-Gruber anastomosis in healthy subjects: an electrophysiological study from Raigarh, Chhattisgarh. Neurol India. 2021;69(04):950–955. doi: 10.4103/0028-3886.325369. [DOI] [PubMed] [Google Scholar]
- 26.Roy J, Henry B M, PĘkala P A. Median and ulnar nerve anastomoses in the upper limb: a meta-analysis. Muscle Nerve. 2016;54(01):36–47. doi: 10.1002/mus.24993. [DOI] [PubMed] [Google Scholar]
- 27.Rodriguez-Niedenführ M, Vazquez T, Parkin I, Logan B, Sañudo J R. Martin-Gruber anastomosis revisited. Clin Anat. 2002;15(02):129–134. doi: 10.1002/ca.1107. [DOI] [PubMed] [Google Scholar]
- 28.Caetano E B, Vieira L A, Sabongi Neto J J, Caetano M F, Sabongi R G. Riché-Cannieu anastomosis: structure, function, and clinical significance. Rev Bras Ortop. 2019;54(05):564–571. doi: 10.1016/j.rbo.2017.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marton A, Ahmed S, Jarvis G E, Brassett C, Grant I, Gaunt M E. The Berrettini palmar neural communicating branch: a study of 27 cadaveric specimens and determination of a high-risk surgical zone. J Hand Surg Eur Vol. 2022;47(08):851–856. doi: 10.1177/17531934221095401. [DOI] [PubMed] [Google Scholar]
- 30.Seidel G K, Seidel M E, Hakopian D. Frequency of electrodiagnostically measurable Berrettini anastomosis. J Clin Neurophysiol. 2020;37(03):214–219. doi: 10.1097/WNP.0000000000000622. [DOI] [PubMed] [Google Scholar]
- 31.Noh J S, Park J W, Kwon H K. Palmar digital neuropathy with anatomical variation of median nerve: usefulness of orthodromic technique: a case report. Ann Rehabil Med. 2019;43(03):341–346. doi: 10.5535/arm.2019.43.3.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Martin S P, Schauer K T, Czyrny J J, Ablove R H. Electrophysiological findings in common median-ulnar nerve interconnections and their clinical implications. J Hand Surg Am. 2019;44(10):884–894. doi: 10.1016/j.jhsa.2019.04.010. [DOI] [PubMed] [Google Scholar]
- 33.Bhardwaj P, Venkatramani H, Sivakumar B, Graham D J, Vigneswaran V, Sabapathy S R. Anatomic variations of the musculocutaneous nerve and clinical implications for restoration of elbow flexion. J Hand Surg Am. 2022;47(10):970–978. doi: 10.1016/j.jhsa.2022.07.014. [DOI] [PubMed] [Google Scholar]
- 34.Le Minor J M. A rare variation of the median and musculocutaneous nerves in man [in French] Arch Anat Histol Embryol. 1990;73:33–42. [PubMed] [Google Scholar]
- 35.Hunter D D, Skrzat J, Zdilla M J. Bilateral absence of the musculocutaneous nerve: implications for humerus fracture and atypical median nerve palsy. Folia Med Cracov. 2020;60(03):27–32. doi: 10.24425/fmc.2020.135793. [DOI] [PubMed] [Google Scholar]
- 36.Raza K, Singh S, Rani N, Mishra R, Mehta K, Kaler S. Anomalous innervation of the median nerve in the arm in the absence of the musculocutaneous nerve. Sultan Qaboos Univ Med J. 2017;17(01):e106–e108. doi: 10.18295/squmj.2016.17.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guru A, Kumar N, Ravindra Shanthakumar S. Anatomical study of the ulnar nerve variations at high humeral level and their possible clinical and diagnostic implications. Anat Res Int. 2015;2015:378063. doi: 10.1155/2015/378063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Athlani L, Delgove A, Dautel G, Casoli V. Anatomy of the ulnar nerve in the posterior compartment of the upper arm: relationships with the triceps brachii muscle. Morphologie. 2020;104(345):85–90. doi: 10.1016/j.morpho.2019.11.001. [DOI] [PubMed] [Google Scholar]
- 39.Granger A, Sardi J P, Iwanaga J. Osborne's ligament: a review of its history, anatomy, and surgical importance. Cureus. 2017;9(03):e1080. doi: 10.7759/cureus.1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Karatas A, Apaydin N, Uz A, Tubbs R, Loukas M, Gezen F. Regional anatomic structures of the elbow that may potentially compress the ulnar nerve. J Shoulder Elbow Surg. 2009;18(04):627–631. doi: 10.1016/j.jse.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 41.Caetano E B, Sabongi Neto J J, Vieira L A, Caetano M F. The arcade of Struthers: an anatomical study and clinical implications. Rev Bras Ortop. 2017;52(03):331–336. doi: 10.1016/j.rboe.2016.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mizia E, Zarzecki M P, Pekala J R. An anatomical investigation of rare upper limb neuropathies due to the Struthers' ligament or arcade: a meta-analysis. Folia Morphol (Warsz) 2021;80(02):255–266. doi: 10.5603/FM.a2020.0050. [DOI] [PubMed] [Google Scholar]
- 43.Kowalska B, Sudoł-Szopińska I. Ultrasound assessment of selected peripheral nerves pathologies. Part II: Entrapment neuropathies of the lower limb. J Ultrason. 2012;12(51):463–471. doi: 10.15557/JoU.2012.0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Suwannakhan A, Chaiyamoon A, Yammine K. The prevalence of anconeus epitrochlearis muscle and Osborne's ligament in cubital tunnel syndrome patients and healthy individuals: An anatomical study with meta-analysis. Surgeon. 2021;19(06):e402–e411. doi: 10.1016/j.surge.2020.12.006. [DOI] [PubMed] [Google Scholar]
- 45.Fadel Z T, Samargandi O A, Tang D T. Variations in the anatomical structures of the Guyon canal. Plast Surg (Oakv) 2017;25(02):84–92. doi: 10.1177/2292550317694851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Murata K, Tamai M, Gupta A. Anatomic study of variations of hypothenar muscles and arborization patterns of the ulnar nerve in the hand. J Hand Surg Am. 2004;29(03):500–509. doi: 10.1016/j.jhsa.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 47.Niitsu M, Kokubo N, Nojima S. Variations of the ulnar nerve in Guyon's canal: in vivo demonstration using ultrasound and 3 T MRI. Acta Radiol. 2010;51(08):939–946. doi: 10.3109/02841851.2010.503193. [DOI] [PubMed] [Google Scholar]
- 48.Veltre D R, Naito K, Li X, Stein A B. Aberrant positioning of the ulnar nerve found during carpal tunnel release: a case report. Orthop Rev (Pavia) 2019;11(03):7795. doi: 10.4081/or.2019.7795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Papanastasiou S, Sood M. Aberrant position of the ulnar nerve within the carpal canal. Microsurgery. 2004;24(01):24–25. doi: 10.1002/micr.10196. [DOI] [PubMed] [Google Scholar]
- 50.Vargas C R, Chepla K J. Report of a transligamentous ulnar nerve sensory branch. Hand (N Y) 2020;15(01):NP11–NP13. doi: 10.1177/1558944719831338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bianchi S, Beaulieu J Y, Poletti P A. Ultrasound of the ulnar-palmar region of the wrist: normal anatomy and anatomic variations. J Ultrasound. 2020;23(03):365–378. doi: 10.1007/s40477-020-00468-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sapage R, Pereira P A, Vital L, Madeira M D, Pinho A. Surgical anatomy of the radial nerve in the arm: a cadaver study. Eur J Orthop Surg Traumatol. 2021;31(07):1457–1462. doi: 10.1007/s00590-021-02916-2. [DOI] [PubMed] [Google Scholar]
- 53.Welle K, Prangenberg C, Hackenberg R K, Gathen M, Dehghani F, Kabir K. Surgical anatomy of the radial nerve at the dorsal region of the humerus: a cadaveric study. J Bone Joint Surg Am. 2022;104(13):1172–1178. doi: 10.2106/JBJS.21.00482. [DOI] [PubMed] [Google Scholar]
- 54.Spinner R J, Spinner M. Superficial radial nerve compression at the elbow due to an accessory brachioradialis muscle: a case report. J Hand Surg Am. 1996;21(03):369–372. doi: 10.1016/S0363-5023(96)80346-7. [DOI] [PubMed] [Google Scholar]
- 55.Herma T, Slezak J, Baca V, Kachlik D.Duplicated superficial branch of the radial nerve and brachioradialis muscle belly: prevalence and significanceFolia Morphol (Warsz)2022 [DOI] [PubMed]
- 56.Hemmi S, Kurokawa K, Nagai T. Anatomical variations of the superficial branch of the radial nerve and the dorsal branch of the ulnar nerve: a detailed electrophysiological study. Muscle Nerve. 2021;63(06):913–918. doi: 10.1002/mus.27221. [DOI] [PubMed] [Google Scholar]
- 57.Tryfonidis M, Jass G K, Charalambous C P, Jacob S. Superficial branch of the radial nerve piercing the brachioradialis tendon to become subcutaneous: an anatomical variation with clinical relevance. Hand Surg. 2004;9(02):191–195. doi: 10.1142/s0218810404002224. [DOI] [PubMed] [Google Scholar]


