Abstract
Introduction The purpose of the study was to evaluate the results of treatment of the nonunion of long bones using nonvascularized iliac crest grafts (ICGs) or vascularized bone grafts (VBGs), such as medial femoral condyle corticoperiosteal flaps (MFCFs) and fibula flaps (FFs). Although some studies have examined the results of these techniques, there are no reports that compare these treatments and perform a multifactorial analysis.
Methods The study retrospectively examined 28 patients comprising 9 women and 19 men with an average age of 49.8 years (range: 16–72 years) who were treated for nonunion of long bones between April 2007 and November 2018. The patients were divided into two cohorts: group A had 17 patients treated with VBGs (9 patients treated with MFCF and 8 with FF), while group B had 11 patients treated with ICG. The following parameters were analyzed: radiographic patterns of nonunion, trauma energy, fracture exposure, associated fractures, previous surgeries, diabetes, smoking, age, and donor-site morbidity.
Results VBGs improved the healing rate (HR) by 9.42 times more than the nonvascularized grafts. Treatment with VBGs showed a 25% decrease in healing time. Diabetes increased the infection rate by 4.25 times. Upper limbs showed 70% lower infection rate. Smoking among VBG patients was associated with a 75% decrease in the HR, and diabetes was associated with an 80% decrease.
Conclusion This study reports the highest success rates in VBGs. The MFCFs seem to allow better clinical and radiological outcomes with less donor-site morbidity than FFs.
Keywords: iliac crest bone graft, nonunion of long bone, medial femoral condyle, vascularized bone grafts, vascularized fibular graft
Introduction
Nonvascularized bone grafts (NVBGs) for nonunion of long bones are widely used in traumatology because of their reproducibility and low cost, despite their biological and structural limits. 1 2 NVBGs could present mechanical failures because of slow neovascularization of the graft with reduced strength. 3 There is a general perception in practice that a vascular supply should be used when large bone graft is used, particularly those greater than 6 cm in length. 4 5
The spreading of microvascular techniques in the past 30 years has increased the use of vascularized bone grafts (VBGs) for the treatment of nonunions. 3 4 5 6 7 8 9 10 VBGs are technically demanding and have longer surgical procedures and greater donor-site morbidity. Furthermore, they may be more difficult to match to the geometry of the recipient site. 8 In contrast, the vascular supply remains intact in VBGs, so that healing occurs by simple fracture union rather than “creeping substitution.” 3
Many studies have described the clinical results of singular surgical techniques for nonunion, few data are available for the comparison of VBGs and NVBGs in long-bone nonunion. 11 12 The reason is the different treatment indications and the biomechanical properties of the grafts, which make them difficult to compare with each other. To better understand the risks and benefits of these techniques, this study analyzes the clinical and radiological results of nonunion of long bones treated with VBGs (fibula flap [FF] and the medial femoral condyle corticoperiosteal flap [MFCF]) and NVBGs (iliac crest bone grafts [ICGs]). To the best of our knowledge, no other reports have compared these treatments together and performed a multifactorial analysis.
Methods
Study Design and Population
All procedures followed were performed in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Declaration of Helsinki 1975 (as revised in 2008). Informed consent was obtained from each patient. All patients treated for nonunion of long bones between April 2007 and November 2018 were examined retrospectively. The inclusion criteria were patients aged 16 years or older, bone gap of at least 4 mm, an interval of at least 6 months of the traumatic event, no evidence of fracture consolidation in at least three radiographs in two projections performed in 6 months after the traumatic event, and no radiographic evidence of infection at the site of nonunion.
For all treated patients, the previous fixation was removed and a locking compression plate or external fixator was used. All the patients treated with FFs receive a skin island to check the vitality of the flap. The patients were divided into two groups: group A was treated with VBGs, and group B was treated with iliac crest bone grafts. In group A, we also distinguished between patients who were treated with MFCFs and patients treated with FFs ( Tables 1 and 2 ).
Table 1. Cohort A (FF/MFCF).
| Age | Sex | Site of nonunion | Initial exposition | Number of previous surgeries | VBG | Bone defect (mm) | |
|---|---|---|---|---|---|---|---|
| Case 1 | 64 | F | Radius | No | 2 | MFCF | 15 |
| Case 2 | 43 | F | Ulna | No | 2 | MFCF | 12 |
| Case 3 | 28 | M | Humerus | No | 0 | MFCF | 16 |
| Case 4 | 65 | M | Humerus | No | 0 | MFCF | 25 |
| Case 5 | 40 | M | Tibia | Yes | 2 | MFCF | 5 |
| Case 6 | 51 | M | Femur | Yes | 1 | MFCF | 9 |
| Case 7 | 69 | F | Humerus | No | 0 | MFCF | 20 |
| Case 8 | 72 | F | Humerus | No | 1 | MFCF | 4 |
| Case 9 | 16 | M | Radius | No | 1 | MFCF | 6 |
| Case 10 | 61 | M | Tibia | Yes | 3 | FF | 75 |
| Case 11 | 24 | M | Tibia | Yes | 2 | FF | 80 |
| Case 12 | 43 | M | Tibia | Yes | 11 | FF | 111 |
| Case 13 | 47 | M | Tibia | No | 2 | FF | 45 |
| Case 14 | 72 | M | Tibia | Yes | 1 | FF | 50 |
| Case 15 | 52 | M | Tibia | Yes | 4 | FF | 50 |
| Case 16 | 40 | M | Tibia | Yes | 2 | FF | 58 |
| Case 17 | 21 | M | Tibia | Yes | 2 | FF | 20 |
Abbreviations: FF, fibula flap; MFCF, medial femoral condyle corticoperiosteal flap; VBG, vascularized bone graft.
Table 2. Cohort B (ICG).
| Age | Sex | Site of nonunion | Initial exposition | Number of previous surgeries | Bone defect (mm) | |
|---|---|---|---|---|---|---|
| Case 1 | 57 | F | Humerus | No | 4 | 8 |
| Case 2 | 66 | F | Humerus | No | 3 | 12 |
| Case 3 | 45 | M | Femur | Yes | 2 | 9 |
| Case 4 | 47 | F | Radius | Yes | 2 | 15 |
| Case 5 | 66 | F | Ulna | No | 1 | 15 |
| Case 6 | 36 | M | Humerus | No | 2 | 8 |
| Case 7 | 48 | M | Radius | Yes | 3 | 5 |
| Case 8 | 66 | M | Ulna | Yes | 1 | 3 |
| Case 9 | 53 | M | Humerus | No | 1 | 8 |
| Case 10 | 62 | M | Tibia | Yes | 4 | 75 |
| Case 11 | 43 | F | Ulna | No | 1 | 12 |
Abbreviation: ICG, iliac crest graft.
Statistical Analysis
The primary outcomes considered were the healing rate (HR) of the fracture and the healing time (HT), which were compared between groups A and B. The secondary outcome was defined as the risk of developing infection. The same outcomes were evaluated in group A as a function of the type of flap (FF vs. MFCF). Healing was defined by the presence of callus at the fracture site of at least three cortices. Multiple logistic regression models were used for binary outcomes (HT and infection), and Poisson multiple regression models were used for bone gap and HT. The following variables were collected and analyzed as covariates for the multiple regression models: radiographic pattern of nonunion, trauma energy, fracture exposure, associated fractures, previous surgery in the same fracture, diabetes, smoking, and age.
The Bayesian regularization technique was applied using a noninformative Cauchy distribution as prior to both regression models to obtain more robust estimates in the case of rare outcomes and perfect or quasi-perfect separation between dependent and independent variables. 13 A nonparametric bootstrap with 5,000 repetitions was applied to assess statistical uncertainty and generate bootstrapped 95% confidence intervals (CIs). 14 Data are described as mean ± standard deviation and range for quantitative variables and as number (%) for categorical variables. For each regression model, the effect sizes and the bootstrapped 95% CIs are reported with adjusted odds ratios (aORs) for logistic regressions and as adjusted incident rate ratios (aIRRs) for Poisson regressions. Estimates for which the 95% CIs do not cross unity are considered as statistically significant.
Results
A total of 28 patients were enrolled, including 9 (32.1%) women and 19 (67.9%) men with an average age of 49.9 ± 15.6 years (range: 16–72 years). There were 17 (60.7%) patients who were treated with bone flaps (group A), of which 9 (52.9% of group A) patients had MFCFs, and 8 (47.1%) patients had FFs. The 11 patients (39.3% of the total) in group B were treated with ICG.
The upper limb was affected by nonunion in 16 (57.1%) cases, including 9 atrophic nonunions (4 humerus, 2 ulnae, and 3 radius cases), 6 oligotrophic nonunion (2 ulna, 3 humerus, and 1 radius cases), and 1 case of hypertrophic nonunion of the humerus. The lower limbs were affected in 12 cases (42.9%), including 10 tibial nonunions (8 atrophic and 2 oligotrophic) and 2 femur nonunions (1 oligotrophic and 1 hypertrophic). The mean initial bone gap was 27.5 ± 28.8 mm (range: 3–111 mm). Ten patients presented low-energy trauma, while 18 (64.3%) patients were involved in high-energy trauma (road traffic accidents), with 14 (50%) cases of open fractures at the time of injury. Thirteen (46.4%) patients had a second fracture during the same trauma, and 5 patients had multiple associated fractures. In group A, patients underwent an average of 2.12 ± 2.52 previous surgeries (range: 0–11), while in group B, the average was 2.18 ± 1.17 (range: 1–4) previous surgeries. None of the patients received NVBGs or VBGs in the previous surgeries.
The regression analysis as a function of groups A and B ( Table 3 ) indicated the following results. Using bone flaps increased the chances of recovery by 9.42 times compared with bone grafts (aOR: 9.42; 95% CI: [1.28, 75.1]), while bone flaps decreased the HT by 25% (aIRR: 0.754; 95% CI: [0.32, 0.98]), and diabetes increased the HT by 1.43 times (aIRR: 1.43; 95% CI: [0.903, 3.76]). Male sex was related to a 48% shorter HT (aIRR: 0.529; 95% CI: [0.122, 0.895]). In these groups, smoking and age did not strongly affect HT.
Table 3. Multiple regression analysis in function of groups A and B (VBGs vs. NVBGs).
| Healing (yes/no) a | Healing time (m) b | Infection (yes/no) | |
|---|---|---|---|
| Surgery | |||
| ICG (baseline) | |||
| VBGs | 9.42 (1.28, 75.1) | 0.754 (0.321, 0.98) | 5.63 (3.67, 66) |
| Nonunion pattern | |||
| Atrophic | |||
| Oligotrophic | 0.866 (0.111, 5.44) | 0.934 (0.376, 1.65) | 0.224 (0.0344, 0.473) |
| Hypertrophic | 2.27 (1.41, 9.15) | 0.831 (0.4, 1.18) | 0.254 (0.0555, 0.488) |
| Limb | |||
| Lower limb (baseline) | |||
| Upper limb | 1.28 (0.305, 4.54) | 0.425 (0.0548, 0.194) | 0.3 (0.12, 1.03) |
| Trauma energy | |||
| High (baseline) | |||
| Low | 0.224 (0.00729, 0.302) | 0.92 (0.364, 1.84) | 1.79 (1.39, 19.1) |
| Open fracture | |||
| No (baseline) | |||
| Yes | 0.148 (0.0141, 0.353) | 1.47 (0.365, 1.08) | 3.34 (1.33, 18.9) |
| Associated fractures (number) | |||
| 0 (baseline) | |||
| 1 | 0.772 (0.0386, 2.6) | 1.53 (1.15, 3.35) | 1.65 (0.368, 4.52) |
| 2 | 0.119 (0.0137, 0.36) | 1.43 (0.419, 1.57) | 1.62 (0.283, 7.2) |
| 3 | 2.43 (1.09, 6.15) | 0.783 (0.568, 2.25) | 0.85 (0.74, 1.49) |
| Previous surgeries | 1.42 (0.846, 3.38) | 0.784 (0.571, 0.956) | 1.42 (0.666, 2.6) |
| Smoking | |||
| No (baseline) | |||
| Yes | 0.719 (0.206, 4.54) | 0.816 (0.321, 1.66) | 2.85 (0.474, 21.1) |
| Pack year | 0.972 (0.871, 1.12) | 1.04 (0.934, 1.12) | 0.983 (0.888, 1.09) |
| Diabetes | |||
| No (baseline) | |||
| Yes | 0.447 (0.0552, 2.78) | 1.43 (0.903, 3.76) | 4.25 (2.07, 64) |
| Age | 1.01 (0.953, 1.1) | 0.983 (0.955, 1.01) | 1.02 (0.929, 1.11) |
| Sex | |||
| F (baseline) | |||
| M | 0.626 (0.0593, 1.85) | 0.529 (0.122, 0.895) | 3.45 (1.94, 17.3) |
Abbreviations: NVBG, nonvascularized bone graft; VBG, vascularized bone graft,
Adjusted odds ratios (95% confidence interval).
Adjusted incidence rate ratios (95% confidence interval).
Upper limb nonunion had 70% lower infection risk than lower limbs (aOR: 0.3; 95% CI: [0.12, 1.03]). Cases of open fractures had 3.34 times higher infection risk than closed ones (aOR: 2.34; 95% CI: [1.33, 18.9]). Diabetes increased the probability of infection by 4.25 times (aOR: 4.25; 95% CI: [2.07, 64]) ( Fig. 1 ).
Fig. 1.

Boxplot of the results of the regression analysis as a function of the type of treatment (vascularized bone grafts vs. nonvascularized bone grafts).
The multiple regression analysis of group A ( Table 4 ) as a function of the microsurgical techniques (FF vs. MFCF) indicated the following results. Smoking was associated with a 75% decrease of the HR (0.25; 95% CI: [0.07, 0.35]), and diabetes was associated with an 80% decrease of HR (0.2; 95% CI: [0.08, 0.262]). Low-energy traumas were associated with 31% shorter HT (0.69; 95% CI: [0.31, 0.91]), while open fractures increased the infection rate by 2.45 times (2.45; 95% CI: [1.59, 10.5]). Diabetes increases the infection rate by 5.11 times (5.11 infection, 95% CI: [4.11, 13.8]) ( Fig. 2 ). The failure rates were 36.4% in patients treated with ICGs (four patients), 25% for patients treated with FFs, and 11% in patients treated with MFCFs.
Table 4. Multiple regression analysis in group A, as a function of the microsurgical techniques (FF vs. MFCF).
| Healing (yes/no) a | Healing time (mo) b | Infection (yes/no) | |
|---|---|---|---|
| Surgery | |||
| ICG (baseline) | |||
| VBGs | 0.786 (0.196, 1.27) | 0.812 (0.405, 1.82) | 4.74 (2.27, 37.9) |
| Nonunion pattern | |||
| Atrophic | |||
| Oligotrophic | 3.54 (3.32, 22.6) | 1.02 (0.787, 1.79) | 0.33 (0.0448, 0.475) |
| Hypertrophic | 1.85 (1.13, 3.02) | 0.845 (0.328, 1.36) | 0.338 (0.15, 0.854) |
| Limb | |||
| Lower limb (baseline) | |||
| Upper limb | 0.783 (0.548, 1.41) | 0.593 (0.198, 0.505) | 1.05 (0.741, 2.47) |
| Trauma energy | |||
| High (baseline) | |||
| Low | 0.525 (0.374, 1.11) | 0.695 (0.31, 0.912) | 1.4 (0.837, 2.85) |
| Open fracture | |||
| No (baseline) | |||
| Yes | 0.783 (0.105, 0.579) | 1.4 (1.26, 2.94) | 2.45 (1.59, 10.5) |
| Associated fractures (number) | |||
| 0 (baseline) | |||
| 1 | 3.12 (1.51, 13.5) | 1.43 (0.625, 2.87) | 0.745 (0.254, 1.71) |
| 2 | 0.462 (0.0717, 0.99) | 1.27 (0.936, 2.24) | 0.529 (0.21, 1.93) |
| 3 | 1.7 (0.623, 1.7) | 0.821 (0.408, 1.21) | 1.16 (0.753, 2.2) |
| Previous surgeries | 1.07 (0.793, 1.66) | 0.904 (0.58, 1.31) | 1.16 (0.753, 2.2) |
| Smoking | |||
| No (baseline) | |||
| Yes | 0.253 (0.0757, 0.349) | 1.09 (0.474, 3.62) | 2.69 (0.371, 6.78) |
| Pack year | 0.988 (0.953, 1.62) | 1.01 (0.852, 1.13) | 1.06 (0.711, 1.08) |
| Diabetes | |||
| No (baseline) | |||
| Yes | 0.2 (0.0868, 0.262) | 0.695 (0.31, 0.912) | 5.11 (4.11, 13.8) |
| Age | 1 (0.99, 1.01) | 0.999 (0.996, 1) | 1 (0.99, 1) |
| Sex | |||
| F (baseline) | |||
| M | 0.482 (0.469, 1.19) | 0.682 (0.0855, 1.01) | 3 (1.29, 5.25) |
Abbreviations: FF, fibula flap; ICG, iliac crest graft; MFCF, medial femoral condyle corticoperiosteal flap; VBG, vascularized bone graft.
Adjusted odds ratios (95% confidence interval [CI]).
Adjusted incidence rate ratios (95% CI).
Fig. 2.
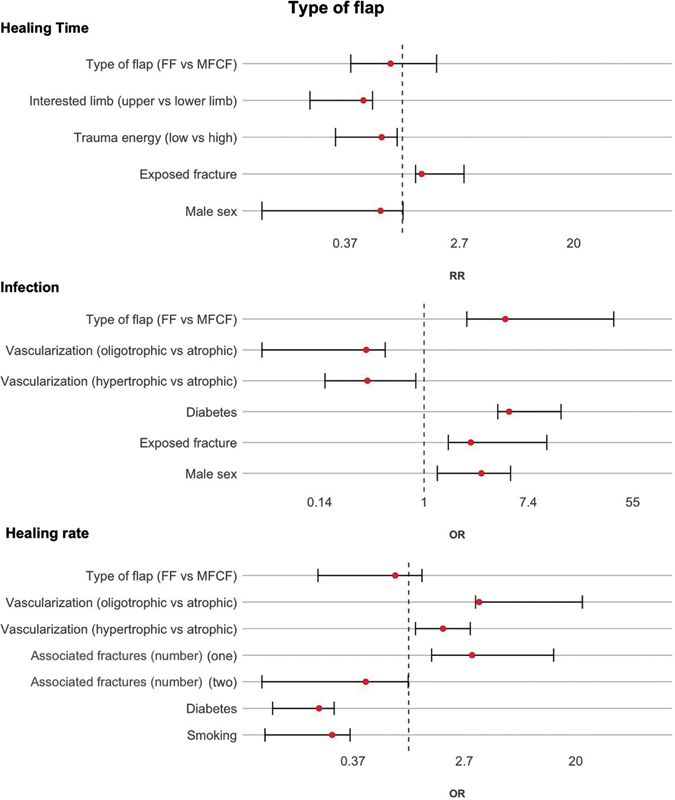
Boxplot of the results of the regression analysis as a function of the type of vascularized bone graft (VBG) (fibula flap [FF] vs. medial femoral condyle corticoperiosteal flap [MFCF]).
Discussion
The recent spread of VBGs compared with NVBGs is mainly due to their biological properties and the limited donor-site morbidity. 7 8 9 The excellent osteogenic ability of these flaps has been substantially demonstrated in the literature. The 6-cm rule as a boundary for VBGs has been cited in many studies, 15 16 17 but the evidence for using VBGs rather than NVBGs for longer defects is limited. In an extensive systematic review, Allsopp et al did not find any clear evidence that grafts longer than 6 cm need to be vascularized. 12 However, the preservation of the vascularization is crucial for ensuring osteocyte survival and the physiological process of fracture healing without creeping substitution. 3 6 7
FF transfer is considered the most reliable autograft for reconstruction of long-bone defects because of its cylindrical shape and mechanical strength ( Fig. 3 ). 7 8 9 MFCFs are a reliable option that can be used in nonunions without a substantial bone defect ( Fig. 4 ). 10 11 Moreover, because of its thickness and its adaptability to the anatomical characteristics of the receiving site, MFCFs can be used to fill nonlongitudinal bone defects, where other grafts are not suitable. MFCFs can be easily wrapped around a long bone or placed in the nonunion site. ICGs are relatively easy to perform without expensive tools and with a fast learning curve ( Fig. 5 ).
Fig. 3.

A 19-year-old patient with and atrophic nonunion of the tibia treated with wide resection, fibula flap and external fixator ( A, B ). Removal of the external fixator at 8 months with a complete healing of the flap ( C ).
Fig. 4.

A 38-year-old patient with oligotrophic nonunion of the radius and ulna after open forearm fracture with recoplate breakage ( A , white arrow ), treated with plate removal, new osteosynthesis with LCP with medial femoral condyle corticoperiosteal flap ( B , white asterisk ). ( C, D ) Follow-up at 6 months with healing of the radius fracture ( black asterisk ).
Fig. 5.

A 43-year-old patient. Open forearm fracture treated with K wires ( A, B ). Because of the bone defect of the radius with an oligotrophic fracture, after 5 months, we decided to use a nonvascularized bone graft (iliac crest graft [ICG]). ( C, D ) Follow-up at 6 months postoperatively after reosteosynthesis and ICG with a complete healing of the site.
There is a paucity of data on the comparison of NVBGs and VBGs in nonunion of long bones in the literature. Thus far, the present study is the only one to compare three surgical techniques with a multifactorial statistical analysis. In 2019, Ciclamini et al 11 were the first who presented the results of MFCFs and ICGs in long-bone nonunions. They reported HRs of 100% in a group treated with MFCFs and 90% in a cohort treated with nonvascularized ICGs. Nwagbara 18 reported a 17% failure rate after autologous bone grafts, while Fuchs et al 19 reported a 100% HR in patients with clavicle nonunion treated with MFCFs. Guzzini et al 20 reported a 100% union rate as well in 14 patients treated with MFCFs for upper limb nonunion.
Choudry et al 21 reported 12 cases of long-bone nonunion treated with FFs, and the overall HR was 92%. Muramatsu et al 22 emphasized that results were satisfactory in 10 patients with humeral nonunion treated with MFCFs, FFs, and scapular flaps. Han et al 23 reported a large series of 160 patients with free iliac crests or FFs with a union rate of 61%.
The different treatment indications in bone defects and the biomechanical properties of the grafts make them difficult to compare with each other. However, this in-depth statistical analysis of a single trauma center with a microsurgery unit confirms some of the risk factors of decreased HR. In the present study, VBGs seem to favor the healing of long-bone nonunion by 9.42 times more than ICGs. Some studies have described a correlation between nonunion and several factors (multiple associated fractures, number of surgeries, smoking, and diabetes). 24 25 However, in the present research, there was no statistically significant evidence of a strong association with the primary outcome of HT in the analysis between groups A and B. Open fractures and diabetes are related to an increased risk of infection, as shown by previous studies. 26 27
There was no statistically significant difference in all the outcomes between nonunions of the upper limbs and lower limbs. In the analysis of the two flap subgroups (FF vs. MFCF), smoking was associated with a 75% decrease in HR, while diabetes presented an 80% decrease. This is probably caused by the effects of these factors on microcirculation, especially in patients treated with microsurgery. Stopping smoking and blood sugar control should be mandatory before and after microsurgery.
The failure rates of the examined groups were 36.4% (four patients) in those treated with ICGs, 25% in the group treated with FFs (two patients), and 11% (one patient) in those treated with MFCFs. All patients with failed procedures were retreated, including four with an induced membrane technique 28 and two with a new corticoperiosteal flap. Healing occurred in all patients within a mean follow-up of 9 months.
The absence of any residual pain in the donor site constitutes one of the main advantages of MFCFs over the other bone grafts. The percentage of patients with chronic pain (more than 6 months) at the donor site was 8% for ICG (17 patients) and 7% for FFs (18 patients), while it was negligible for MFCFs. 29 30 Vail and Urbaniak 31 studied the donor-site morbidity while harvesting FFs. Muscle weakness of the ankle was found in 25 (10%) of the 247 limbs at 3 months postoperation and in 2 (3%) of the 74 limbs evaluated in 5 years of follow-up. In our cohort, patients treated with FFs presented the highest donor-site morbidity with two cases of delayed wound healing, chronic pain in the peroneal region (one patient), one case of reduced muscle strength of the ankle, five patients with loss of strength of the extensor hallucis longus, and four cases of paresthesia of the lateral side of the leg. The extensor hallucis longus seems susceptible to denervation because it is usually innervated by only one of the two branches of the deep peroneal nerve. 32 In the ICG group, four patients presented chronic pain localized at the harvest site.
Conclusion
The present multifactorial analysis indicates that the use of VBGs is an important surgical advantage. The potential costs and risks of microsurgical operations are compensated by faster consolidation times compared with ICGs ( Table 5 ). 33 34 35 For a long time, NVBGs have been the gold standard in nonunion treatment and are still a feasible technique, especially in hospitals without microsurgical experience. Nevertheless, surgeons must be aware of their biological and mechanical limits and the risk of bone resorption.
Table 5. Recent systematic reviews and meta-analysis about VBGs and NVBGs.
| Article | Year | Journal | Title | No. of examined articles | No. of patients | Conclusions |
|---|---|---|---|---|---|---|
| Feltri et al 33 | 2021 | Arch Orthop Trauma Surg | Vascularized fibular grafts for the treatment of long-bone defects: pros and cons. A systematic review and meta-analysis | 110 | 2,226 | Overall, good functional results were documented and a union rate of 80.1% was found, with a 39.4% complication rate. Good long-term outcomes both in the upper and lower limbs |
| Weir et al 34 | 2020 | Arch Orthop Trauma Surg | Free vascularized medial femoral condyle periosteal flaps in recalcitrant long-bone nonunion: a systematic review | 14 | 117 | Free vascularized periosteal flaps are promising with pooled data showing a 99% success rate in achieving union in refractory long bone nonunion |
| Azi et al 35 | 2016 | BMC Musculoskelet Disord | Autologous bone graft in the treatment of posttraumatic bone defects: a systematic review and meta-analysis | 34 | 749 | Vascularized graft was associated with a lower risk of infection after surgery when compared with nonvascularized graft |
Limitations
There are inherent limitations to this study, such as the retrospective analysis, small sample size, and the heterogeneous cohorts. The inability to obtain two homogenous groups is closely linked to the small number of patients treated for this disease. Furthermore, it was difficult to assess the degree of influence of the osteosynthesis material replacement with a more stable plating in the healing of hypertrophic pseudoarthrosis. An additional confounding factor may be the different biomechanics of fractures of the long bones of the upper and lower limbs. Therefore, it will be necessary to continue to study the use of these techniques for more comprehensive understanding of their benefits and risks in bone defect reconstruction.
Acknowledgment
The authors would like to thank Miss Bettina Reichl for her support in the literature search and her help in the graphic renderings.
Funding Statement
Funding None.
Conflict of Interest The authors declared no potential conflict of interest with respect to the research, authorship, and/or publication of this article. Dr. Calcagni reports nonfinancial support from Sobi, nonfinancial support from Medartis, nonfinancial support from Silk Biomaterials, nonfinancial support from DyCare, outside the submitted work.
Authors' Contribution
M.G. and M.G. researched literature and conceived the study. M.G., M.G., C.C., R.M.L., B.S.K., I.S.B., M.R., S.L., M.C., and D.P. were involved in protocol development, data analysis, and correction of the manuscript. M.G. wrote the draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
References
- 1.Campbell W C. The autogenous bone graft. J Bone Joint Surg. 1939;21:694. [Google Scholar]
- 2.Ahlmann E, Patzakis M, Roidis N, Shepherd L, Holtom P. Comparison of anterior and posterior iliac crest bone grafts in terms of harvest-site morbidity and functional outcomes. J Bone Joint Surg Am. 2002;84(05):716–720. doi: 10.2106/00004623-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Weiland A J, Moore J R, Daniel R K. The efficacy of free tissue transfer in the treatment of osteomyelitis. J Bone Joint Surg Am. 1984;66(02):181–193. [PubMed] [Google Scholar]
- 4.Foster R D, Anthony J P, Sharma A, Pogrel M A. Vascularized bone flaps versus nonvascularized bone grafts for mandibular reconstruction: an outcome analysis of primary bony union and endosseous implant success. Head Neck. 1999;21(01):66–71. doi: 10.1002/(sici)1097-0347(199901)21:1<66::aid-hed9>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 5.Soucacos P N, Kokkalis Z T, Piagkou M, Johnson E O. Vascularized bone grafts for the management of skeletal defects in orthopaedic trauma and reconstructive surgery. Injury. 2013;44 01:S70–S75. doi: 10.1016/S0020-1383(13)70016-0. [DOI] [PubMed] [Google Scholar]
- 6.Tang C H. Reconstruction of the bones and joints of the upper extremity by vascularized free fibular graft: report of 46 cases. J Reconstr Microsurg. 1992;8(04):285–292. doi: 10.1055/s-2007-1006709. [DOI] [PubMed] [Google Scholar]
- 7.Beris A E, Lykissas M G, Korompilias A V. Vascularized fibula transfer for lower limb reconstruction. Microsurgery. 2011;31(03):205–211. doi: 10.1002/micr.20841. [DOI] [PubMed] [Google Scholar]
- 8.Taylor G I, Miller G D, Ham F J. The free vascularized bone graft. A clinical extension of microvascular techniques. Plast Reconstr Surg. 1975;55(05):533–544. doi: 10.1097/00006534-197505000-00002. [DOI] [PubMed] [Google Scholar]
- 9.González del Pino J, Bartolomé del Valle E, Graña G L, Villanova J F. Free vascularized fibular grafts have a high union rate in atrophic nonunions. Clin Orthop Relat Res. 2004;(419):38–45. doi: 10.1097/00003086-200402000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Doi K, Sakai K. Vascularized periosteal bone graft from the supracondylar region of the femur. Microsurgery. 1994;15(05):305–315. doi: 10.1002/micr.1920150505. [DOI] [PubMed] [Google Scholar]
- 11.Ciclamini D, Tos P, Guzzini M, Soldati A, Crosio A, Battiston B. The medial femoral condyle free corticoperiosteal flap versus traditional bone graft for treatment of nonunions of long bones: a retrospective comparative cohort study. Injury. 2019;50 05:S54–S58. doi: 10.1016/j.injury.2019.10.049. [DOI] [PubMed] [Google Scholar]
- 12.Allsopp B J, Hunter-Smith D J, Rozen W M. Vascularized versus nonvascularized bone grafts: what is the evidence? Clin Orthop Relat Res. 2016;474(05):1319–1327. doi: 10.1007/s11999-016-4769-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gelman A, Jakulin A, Pittau M G, Su Y S. A weakly informative default prior distribution for logistic and other regression models. Ann Appl Stat. 2008;2:1360–1383. [Google Scholar]
- 14.Davison A C, Hinkley D V. Cambridge, UK: Cambridge University Press; 1997. Bootstrap Methods and Their Application. Vol. 1. [Google Scholar]
- 15.Godina M. Early microsurgical reconstruction of complex trauma of the extremities. Plast Reconstr Surg. 1986;78(03):285–292. doi: 10.1097/00006534-198609000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Yazar S, Lin C H, Wei F C. One-stage reconstruction of composite bone and soft-tissue defects in traumatic lower extremities. Plast Reconstr Surg. 2004;114(06):1457–1466. doi: 10.1097/01.prs.0000138811.88807.65. [DOI] [PubMed] [Google Scholar]
- 17.Bumbasirevic M, Stevanovic M, Bumbasirevic V, Lesic A, Atkinson H D. Free vascularised fibular grafts in orthopaedics. Int Orthop. 2014;38(06):1277–1282. doi: 10.1007/s00264-014-2281-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nwagbara I C. Osseous union in cases of non-union in long bones treated by osteosynthesis. Niger J Clin Pract. 2010;13(04):436–440. [PubMed] [Google Scholar]
- 19.Fuchs B, Steinmann S P, Bishop A T. Free vascularized corticoperiosteal bone graft for the treatment of persistent nonunion of the clavicle. J Shoulder Elbow Surg. 2005;14(03):264–268. doi: 10.1016/j.jse.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 20.Guzzini M, Lanzetti R M, Perugia D. The treatment of long bones nonunions of upper limb with microsurgical cortico-periosteal free flap. Injury. 2017;48 03:S66–S70. doi: 10.1016/S0020-1383(17)30661-7. [DOI] [PubMed] [Google Scholar]
- 21.Choudry U H, Bakri K, Moran S L, Karacor Z, Shin A Y. The vascularized medial femoral condyle periosteal bone flap for the treatment of recalcitrant bony nonunions. Ann Plast Surg. 2008;60(02):174–180. doi: 10.1097/SAP.0b013e318056d6b5. [DOI] [PubMed] [Google Scholar]
- 22.Muramatsu K, Doi K, Ihara K, Shigetomi M, Kawai S. Recalcitrant posttraumatic nonunion of the humerus: 23 patients reconstructed with vascularized bone graft. Acta Orthop Scand. 2003;74(01):95–97. doi: 10.1080/00016470310013734. [DOI] [PubMed] [Google Scholar]
- 23.Han C S, Wood M B, Bishop A T, Cooney W P., III Vascularized bone transfer. J Bone Joint Surg Am. 1992;74(10):1441–1449. [PubMed] [Google Scholar]
- 24.Patel RA, Wilson RF, Patel PA, Palmer RM. The effect of smoking on bone healing: a systematic review. Bone Joint Res. 2013;2(06):102–111. doi: 10.1302/2046-3758.26.2000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kwiatkowski T C, Hanley E N, Jr, Ramp W K. Cigarette smoking and its orthopedic consequences. Am J Orthop. 1996;25(09):590–597. [PubMed] [Google Scholar]
- 26.Kline A J, Gruen G S, Pape H C, Tarkin I S, Irrgang J J, Wukich D K. Early complications following the operative treatment of pilon fractures with and without diabetes. Foot Ankle Int. 2009;30(11):1042–1047. doi: 10.3113/FAI.2009.1042. [DOI] [PubMed] [Google Scholar]
- 27.Widenfalk B, Pontén B, Karlström G. Open fractures of the shaft of the tibia: analysis of wound and fracture treatment. Injury. 1979;11(02):136–143. doi: 10.1016/s0020-1383(79)80011-x. [DOI] [PubMed] [Google Scholar]
- 28.Masquelet A C. Induced membrane technique: pearls and pitfalls. J Orthop Trauma. 2017;31 05:S36–S38. doi: 10.1097/BOT.0000000000000979. [DOI] [PubMed] [Google Scholar]
- 29.Dimitriou R, Mataliotakis G I, Angoules A G, Kanakaris N K, Giannoudis P V. Complications following autologous bone graft harvesting from the iliac crest and using the RIA: a systematic review. Injury. 2011;42 02:S3–S15. doi: 10.1016/j.injury.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 30.Ling X F, Peng X. What is the price to pay for a free fibula flap? A systematic review of donor-site morbidity following free fibula flap surgery. Plast Reconstr Surg. 2012;129(03):657–674. doi: 10.1097/PRS.0b013e3182402d9a. [DOI] [PubMed] [Google Scholar]
- 31.Vail T P, Urbaniak J R. Donor-site morbidity with use of vascularized autogenous fibular grafts. J Bone Joint Surg Am. 1996;78(02):204–211. doi: 10.2106/00004623-199602000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Shpitzer T, Neligan P, Boyd B, Gullane P, Gur E, Freeman J. Leg morbidity and function following fibular free flap harvest. Ann Plast Surg. 1997;38(05):460–464. doi: 10.1097/00000637-199705000-00005. [DOI] [PubMed] [Google Scholar]
- 33.Feltri P, Solaro L, Errani C, Schiavon G, Candrian C, Filardo G.Vascularized fibular grafts for the treatment of long bone defects: pros and cons. A systematic review and meta-analysis Arch Orthop Trauma Surg 2021 10.1007/s00402-021-03962-5. PMID: 34110477. [DOI] [PubMed] [Google Scholar]
- 34.Weir J C, Osinga R, Reid A, Roditi G, MacLean A D, Lo S J. Free vascularised medial femoral condyle periosteal flaps in recalcitrant long bone non-union: a systematic review. Arch Orthop Trauma Surg. 2020;140(11):1619–1631. doi: 10.1007/s00402-020-03354-1. [DOI] [PubMed] [Google Scholar]
- 35.Azi M L, Aprato A, Santi I, Kfuri M, Jr, Masse A, Joeris A. Autologous bone graft in the treatment of post-traumatic bone defects: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2016;17(01):465. doi: 10.1186/s12891-016-1312-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


