Abstract
Problem
The determinants of COVID-19 vaccine acceptance, hesitancy, and refusal remain poorly understood. We assessed the general population of Pune after visiting tertiary care hospital for their willingness to accept the vaccine and the reason for their hesitancy and refusal.
Methodology
A six-month descriptive cross-sectional study with 386 community members over the age of 18 who visited the Tertiary Hospital OPD was conducted. The vaccine acceptance and hesitancy was assessed using a self designed detailed questionnaire with a one-time face-to-face interview.
Results
Acceptance for vaccine was observed in 235 (60.8%) participants, while 151 (39.2%) hesitated and refused. Participants with lower education (P < 0.00001), no employment did not readily accept the vaccine (P < 0.00001). Pregnant, breast-feeding women (21.8%) hesitated vaccine because of lack of evidence regarding vaccine safety. Participants (73.6%) were readily accepting (third dose) booster dose of vaccine when available. The reason for vaccine hesitance was the concern about side effects (58.2%) and reason for acceptance was to get immunity against COVID-19 (76.1%). Vaccine information source appears to be an influential aspect, as participants who obtained vaccination information from healthcare providers had no concerns regarding vaccination.
Conclusion
The study has found a link between average education level, unemployment and vaccine acceptance and hesitancy. Factors influencing vaccine hesitancy include lack of vaccine information, vaccine side effects, and misinformation spread via social media. Clinical pharmacists can play an important role in boosting up vaccine acceptance by providing appropriate information in community.
Keywords: Immunisation programs, SARS-CoV-2, Vaccine perception, COVID-19, Acceptance and hesitancy
1. Introduction
WHO declared the illness to be pandemic and launched a global prevention campaign following the COVID-19 outbreak in December 2019.1 There has been a clear call for the development of a vaccine, which has led to the discovery of numerous vaccines and their testing in numerous trials. Nevertheless, the development of a safe and effective vaccine is the only essential tool for pandemic control. By the first quarter of 2021, 23 vaccines had reached stage 3 clinical trials, and more than a dozen of those had already been given the go-ahead for emergency use in numerous countries.2 In addition to vaccine safety, efficacy, and cost-effectiveness, public acceptance plays a significant role in measuring overall effectiveness and success of vaccination drive.3 The public's perception of the vaccine use amongst the community is highly dependent on the information propagated through various broadcasts/mass media, health bulletins. Thus there is a strong need to comprehend the root causes of vaccine hesitancy and the drivers of vaccine acceptance in order to successfully eradicate the current pandemic.
India has already experienced two COVID-19 waves, inspite of which it was not far behind in developing the world's largest COVID-19 vaccination programme in early 2021.4 The ChAdOxl nCoV-19 vaccine from Oxford AstraZeneca and the COVID-19 VACCINE (COVAXIN®) from BHARAT BIOTECH are both authorised for use in India in the early months of 2021. While effective and equitable distribution of COVID-19 vaccines is a top priority, ensuring acceptance is equally critical. Vaccination hesitancy persists even in areas where vaccines are made available, despite the difficulty in vaccine availability and distribution.3 On the other hand, vaccine rejection and misinformation act as impediments to achieving high coverage and community immunity against the infection.5 , 6
The WHO's Strategic Advisory Group of Experts on Immunization defined vaccine hesitation as "delay in accepting or refusing immunisation despite the availability of vaccination services".7 Even for routine vaccinations, vaccine hesitancy and refusal to accept vaccines are a growing concern around the world. India has one of the highest rates of vaccine hesitancy and refusal. Thus, hesitation to receive the COVID-19 vaccine is neither new nor unexpected.8 Additionally, misinformation disseminated via a variety of media may significantly affect how well-received a COVID-19 vaccination is.9 Authorities and societies must assess the current state of peoples' willingness to receive COVID-19 vaccinations, which may be safe and effective, and they must also identify any signs of vaccine acceptance or reluctance.
Despite the vaccine's availability, there is paucity of data regarding vaccine acceptance amongst community.10 This study aimed to determine Covid 19 vaccine acceptance and predictors towards government allocated vaccines, as well as to understand the reasons underlying vaccine hesitancy or refusal amongst community.
1.1. Design and sample
A 6 months descriptive cross-sectional study was conducted during 2021. Participants were enrolled using a random sample technique when they visited the Tertiary Hospital OPD. A detailed one-time face-to-face interview was conducted for 30 min, using a self-designed questionnaire. Data from duly filled questionnaires was retrieved and statistical analysis was performed. A sample size of at least 386 complete responders would provide a confidence level of 95% with margin of error of 5% to estimate vaccine acceptance rate among a population visiting at Tertiary Hospital at the time of survey assumed maximum standard deviation. Since the study was interview based and due to time constraint most of the patients were unwilling to participate in the study as the study was conducted after OPD. Informed consent was obtained from all subjects (none under the age of 18 and who were volunteered to participate in the study was included). The survey questionnaire was administered by the Clinical Pharmacist and Data were collected anonymously, and no personally identifying information was collected. Participants were divided into two groups based on their vaccination status: VA (Vaccine Acceptance) who received (single/both doses) and VH (Vaccine Hesitance) who did not receive the dose.
1.2. Sample size calculation
n = Z2pq/e2Where, n = sample size.
We considered confidence interval 95% for which Z score is 1.96.
| n= (1.96)2 × 0.5 × 0.5 / (0.05)2 = 386 |
1.3. Survey questionnaire and variable definitions
The questionnaires were developed to assess acceptance, hesitancy, and refusal of the COVID 19 vaccine. Initially questionnaire was developed in English and then translated into native languages of Hindi and Marathi. The questionnaire was divided into five sections: demographic data, vaccine acceptance/hesitance, perceptions toward vaccines refusal and COVID-19pandemic and vaccine related information. The questionnaire was developed and tested for reliability using a reliability scale and a Cronbach's alpha, with a satisfactory (=0.78) result.
1.4. Demographic data
General baseline data including age, gender and marital-status, level of education, personal health issue (Hypertension, diabetes, cancer, asthma, etc.), smoking status and monthly income were collected.
1.5. Vaccine acceptance/hesitancy
In the beginning, we questioned participants about their vaccination status (partially/fully vaccinated) and the source of their immunization along with factors related to willingness or reluctance toward receiving a COVID-19 vaccine with response options yes, maybe and no. If the vaccine becomes available in the future, respondents were also asked if they would recommend vaccination to family members, friends, and children, with same response choices.
1.6. Perceptions toward vaccines refusal
Using closed ended questions (yes/no), we measured participants reasons for refusal to covid-19 vaccination. Participants were asked to respond to a set of statements such as ‘you refuse vaccine due to religious beliefs’ and ‘vaccine refusal due to trypanophobia.’ Concerns regarding COVID-19vaccine safety were evaluated by responses to the following sentences: ‘you are refusing the vaccine since new variants of COVID are emerging and it requires new vaccine for prevention’ and you had a past Covid infection’.
1.7. COVID-19 pandemic and vaccine related information
Participants were questioned about the primary informational sources they use to obtain news about the covid epidemic and vaccines.
1.8. Statistical analysis
Baseline Characteristics of the participants were represented as frequencies and percentages and a student's "T" test was used to analyse the demographic differences between the groups (VA/VH). Numbers and percentages were used to represent the qualitative variables. The qualitative variables that differed between the groups were analysed using the chi-square test. The chi-square test was also used to compare any two groups percentages is due to chance, or if it is due to a relationship between the variables. P value of less than 0.05 was considered significant. Data were prepared in Microsoft Excel sheet 2019 and the Statistical Package for Social Sciences (SPSS) version 20 was used to analyse the data.
2. Result
Total of 386 participants were grouped into two parts: Study VA (Vaccine Acceptance), which included 235 individuals who received the vaccine during the study period, and Study VH (Vaccine Hesitance), which included 151 individuals who expressed reluctance to receive the vaccine.
2.1. Variables associated with acceptance of COVID-19 vaccine
In a total of 235 study VA group, the majority of the participants (33.9%) were females between the ages of 29 and 39, and this age group's vaccination rate was (33.6%) (p 0.015) in comparison to other age groups. Male participants aged 40–59 were more likely to accept the vaccine (15.3%), despite the potential of co-morbidities and infection risk, while participants aged 60 and older showed the lowest acceptance rate (5.5%). Majority of the participants with higher vaccine acceptance were Undergraduates (57.4%), Postgraduates (22.1%), and School education (7.6%) (p 0.00001).
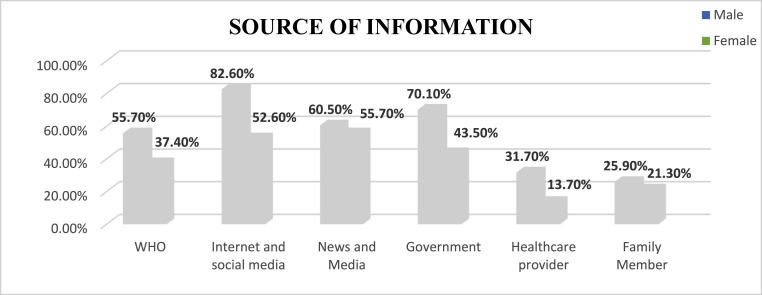
Social media and internet (82.60%) were the most trusted sources of information for the majority of participants, followed by news and media (57.8%) and official government sources (55.3%) (see Fig. 1 ).
Fig. 1.
Source of information of COVID-19 vaccination.
In the vaccinated group, 67.2% received two doses of vaccine, while 32.7% received a single dose of vaccine. Easy vaccine availability, low cost, easy accessibility and other factors could be the reason that majority of participants (59.5%) received the COVID-19 vaccine from government hospitals, while 40.4% received the vaccine from private hospital Furthermore, because of their low education level and lack of vaccine knowledge, the majority of participants (56.1%) were unaware of the COVID-19 antibody test (p 0.021). 82.9% of participants thought the COVID-19 vaccine should be made mandatory (p0.001), and 73.6% said they would accept a booster dose if it became available in the future (p 0.00001).
2.2. Variables associated with hesitancy of COVID-19 vaccine
In study VH group vaccine reluctance was influenced by factors such as child bearing age, pregnancy, and lactation in the majority of women aged 29 to 39 (13.9%) at the time of the study. While 11.9% of male participants in the same age group were apprehensive about receiving the vaccine due to potential side effects. Education level and vaccine hesitancy were attributable factors, as vaccine hesitancy was higher in participants with low literacy (65.9%). A significantly higher proportion of participants (63.5%) (p0.083) learned about post-vaccine side effects from the internet, social media, and other media, so they believed it and avoided the vaccine (see Fig. 1).
Male participants (68.4%) were the most likely to believe that the vaccine's benefit outweighed their risk (p 0.009). Furthermore, 76.7% of participants believe that there is no difference in their immunity after vaccination because even vaccinated individuals became infected and thus refused the vaccine. 57.5% of males were also discouraged from accepting the vaccine by their peers, family, and through social media. While 50% of female participants were unwilling to vaccinate their children if the vaccine became available for children in the future. The majority of participants (52.9%) had a negative vaccination experience that discouraged them from being vaccinated (p0.003).
The participants refused the vaccine because they had previously been infected with COVID-19 and believed that they had adequate antibodies and that the vaccine was not required for infection prevention or protection (p 0.004). Another reason for vaccine refusal by majority of participants (71.5%) is, they believed that new COVID-19 variants would necessitate a newer and better vaccine than the currently available vaccine (p 0.042).
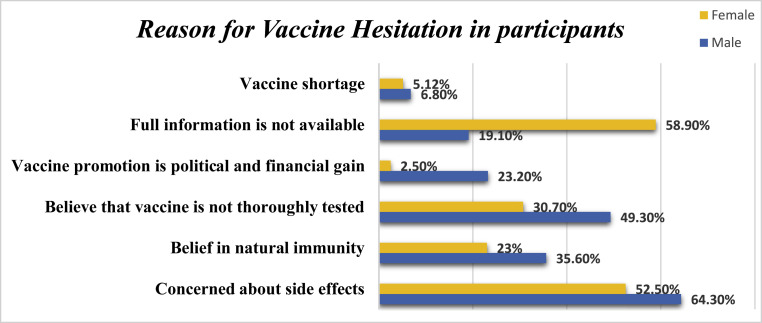
As vaccine is new and immediate vaccine that was developed in a very short time frame and is approved for emergency use, thus it was refused by (69.5%) of participants because. 63% of male participants (n = 46) are also sceptical of vaccines produced by large pharmaceutical companies (see Fig. 3).
Fig. 3.
Reason for vaccine hesitation among the participants.
2.3. A comparison between study VA and VH (vaccine acceptance vs hesitancy vs refusal)
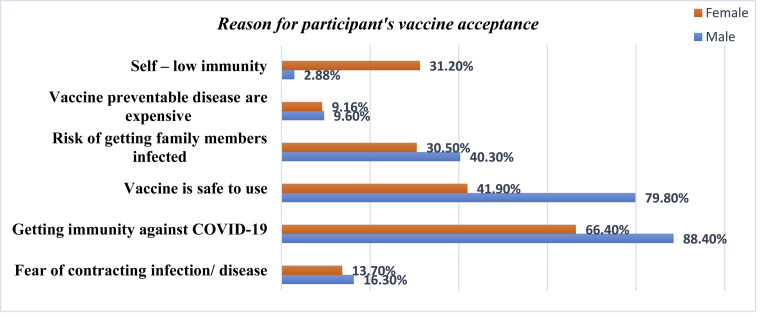
Acceptance of the vaccine was attributed to immunity against the COVID-19-19 virus in (88.4%) male and (66.0%) female participants. (See Fig. 2 ). 79.8% male believed that the vaccine is safe to use and only 41.9% female participant agree to it. Participants who believed vaccination would help protect people against COVID-19 had a significant correlation. There was also a link between willingness to take the vaccine and its safety and efficacy. Evidently, 31.2% of female participants were more concerned about their low immunity than male participants and readily accepted vaccines.
Fig. 2.
Reason for vaccine acceptance among the participants.
Concerns about vaccine hesitancy include the vaccine's side effects, insufficient information, and political interest in vaccination (See Fig. 3). 49.3% of males thought the vaccine was not thoroughly tested and had safety issues. And 35.6% of men believed in their natural immunity and were thus hesitant. Unexpectedly, 23.2% of male participants believed that vaccine promotion was motivated by political and financial gain. The majority of female participants (58.9%) lacked knowledge about the vaccine.
2.4. Discussion
The main reason of the study participants of both genders to get vaccinated was to get immunity against the disease,followed by their belief that vaccine was safe to use, while their reason for vaccine hesitation of both genders was their concern about side effects and belief that the vaccine are not thoroughly tested and lack of information.Female participants were more likely to accept the vaccine, especially within the age group of 29–39 years of age, our study finding is similar to a study by Paul A et al.11 When comparing with Study VH, the same age group women were hesitant to receive the vaccine since they are of childbearing age, there is a lack of research and evidence about the safety and efficacy of the use of vaccine in pregnancy, breastfeeding, and female participants are also concerned about the use of vaccine in hormonal disorders and expressed uncertainty about its side effects on oral contraceptives.12 While male participants of age group 36–59 years showed higher acceptance vaccine rate and participants of age group of 60 years and above were hesitant about vaccine this observation is similar to a previous study conducted by Godasi GR et al. in South India which observed negative attitude was prevalent amongst elderly people.13 The older age group is the most likely to become infected with the coronavirus. These age groups are vulnerable due to reduced immunity, co-morbidities, and certain impairment/disability. Their hesitation directs to their level of education as well as their inability to understand and accept the concept of introducing foreign substances into their body. Clinical pharmacists and healthcare professionals would be crucial in overcoming their hesitation.
In our study, the majority of participants had received two doses of vaccination. The majority of participants obtained vaccine through government hospitals or government-funded mass vaccination centres, demonstrating the relationship between unemployment and willingness to accept free vaccines. However, 56.1% of participants were unaware of the antibody test, which is a quick means of detecting antigens or antibodies for COVID-19.11 Official sources like as the ICMR and WHO communicated information through bulletins, but because the majority of research participants learned about the vaccination from the internet, social networks, news, and other media sources, they were unaware of this test.
A significant no of participants (73.6) was willing to take booster dose of the vaccine if available in the future. Due to the coronavirus infection rate, mortality rate and financial burden was increased following hospitalisation. On a worldwide scale, millions of lives were lost. Children were orphaned, and families were destroyed. Fearful people chose for the vaccine because it reduces the risks of infection and hospitalisation. Booster dose, as the name indicates, boosts immunity to the infection.
Factors influencing for the increase in vaccine hesitancy in the present pandemic is the current misrepresentation, with social media facilitating the spread of misinformation about the vaccine and its related conspiracies.14 Similar finding was observed in our study, participants were hesitant to take vaccine because of false allegations about side effects after vaccination. As observed male participants obtained their information from internet and social media, while female participants were keener and got information from news and media. While 66.8% participants with a believed that there is no benefit of taking vaccine since a vaccinated person could get infected with COVID-19 and assumed that there is no difference in their immunity hence hesitated to take vaccine. Our study findings are similar with a previous study which showed participants were discouraged by their family and peers, since they were not sure about the vaccine and its content.14 A study conducted by Akhmetzhanova Z et al. in Kazakhstan showed similar results that parents were hesitant to provide vaccination for their children,higher educational status of parents is associated with better immunization coverage in previous studies conducted in India, educated parents are more likely to remember dates, understand the importance of timely vaccination and interact more freely with health workers.15 Participants who had unfortunate past experiences with vaccine were afraid to undergo the same conditions and thus hesitated the vaccine. 69.5% participants in our study were hesitant to take vaccine since it's a new and immediate vaccine development with shorter development timeline and received emergency approval from WHO for its use in public.16 Participants also believed that the vaccine developed were for the benefit of pharmaceutical companies and for political gain and thus hesitated.
Many conspiracy theories were in highlight after the vaccine was introduced, where it described vaccine as a tool with a chip for monitoring public, and will damage DNA permanently. 29.8% participants in this study were hesitant to take vaccine because of their religious and cultural belief, similar observation was seen in a previous study ‘that immunizations are unnecessary because they have complete belief in God’ vaccine conspiracy ideas are being propagated by some religious leaders.17 Few participants believed that because they had previously been infected with COVID-19 and survived the disease, they would have enough antibodies to resist the infection again, therefore they hesitated the vaccine. Reported prevalence rates of needle phobia widely diverge in the literature ranging from 3.5% to 20%.18 Few participants had fear of injections (Trypanophobia) and thus hesitant to the COVID-19 vaccine. The fact that the new mutations of the COVID-19 variants were more fatal and thus requiring the more effective vaccines.19 These findings were similar to our study wherein the participants hesitated the vaccine since new variants of the coronavirus are emerging and they require better vaccine then the previous for protection against infection.
2.5. Conclusion
Our study found that females had a higher rate of COVID-19 vaccine acceptance than males, irrespective of the fact that most women were hesitant to receive the vaccine. The most important factors influencing COVID-19 vaccine hesitancy were low vaccine literacy, family or social media influence, and fear of vaccine side effects. Vaccine acceptance disparities among the population can be managed by the healthcare workers, especially clinical pharmacist as they poised to address the accessible, consistent and genuine information regarding vaccine safety, which can boost up the vaccine drive and can effectively prevent the COVID-19 spread.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for – profit sectors.
Declaration of competing interest
There is no Conflict Of Interest in this study.
References
- 1.Cascini F., Pantovic A., Al-Ajlouni Y., Failla G., Ricciardi W. Attitudes, acceptance and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: a systematic review. EClinicalMedicine. 2021 Oct 1;40 doi: 10.1016/j.eclinm.2021.101113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Solís Arce J.S., Warren S.S., Meriggi N.F., et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat Med. 2021 Aug 1;27(8):1385–1394. doi: 10.1038/s41591-021-01454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sirikalyanpaiboon M., Ousirimaneechai K., Phannajit J., et al. COVID-19 vaccine acceptance, hesitancy, and determinants among physicians in a university-based teaching hospital in Thailand. BMC Infect Dis. 2021 Dec 1;21(1) doi: 10.1186/s12879-021-06863-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fakonti G., Kyprianidou M., Toumbis G., Giannakou K. Attitudes and acceptance of COVID-19 vaccination among nurses and midwives in Cyprus: a cross-sectional survey. Front Public Health. 2021 Jun 16;9 doi: 10.3389/fpubh.2021.656138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Larson H.J., Jarrett C., Eckersberger E., Smith D.M.D., Paterson P. vol. 32. Elsevier BV; 2014. pp. 2150–2159. (Understanding Vaccine Hesitancy Around Vaccines and Vaccination from a Global Perspective: A Systematic Review of Published Literature). 2007-2012. Vaccine. [DOI] [PubMed] [Google Scholar]
- 6.Lane S., MacDonald N.E., Marti M., Dumolard L. Vaccine hesitancy around the globe: analysis of three years of WHO/UNICEF Joint Reporting Form data-2015–2017. Vaccine. 2018 Jun 18;36(26):3861–3867. doi: 10.1016/j.vaccine.2018.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MacDonald N.E., Eskola J., Liang X., et al. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015 Aug 14;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 8.Danabal K.G.M., Magesh S.S., Saravanan S., Gopichandran V. Attitude towards COVID 19 vaccines and vaccine hesitancy in urban and rural communities in Tamil Nadu, India – a community based survey. BMC Health Serv Res. 2021 Dec 1;21(1) doi: 10.1186/s12913-021-07037-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Westmoreland D.A., Berry A., Zimba R., et al. Spread and sources of information and misinformation about COVID-19 early during the pandemic in a U.S. national cohort study. medRxiv. 2021 Jan 2021.03.10.21252851. [Google Scholar]
- 10.Dzieciolowska S., Hamel D., Gadio S., et al. Covid-19 vaccine acceptance, hesitancy, and refusal among Canadian healthcare workers: a multicenter survey. Am J Infect Control. 2021;49(9):1152–1157. doi: 10.1016/j.ajic.2021.04.079. [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paul A., Sikdar D., Mahanta J., et al. Peoples' understanding, acceptance, and perceived challenges of vaccination against COVID-19: a cross-sectional study in Bangladesh. PLoS One. 2021 Aug 1;16(8 August) doi: 10.1371/journal.pone.0256493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dagan N., Barda N., Biron-Shental T., et al. Effectiveness of the BNT162b2 mRNA COVID-19 vaccine in pregnancy. Nat Med. 2021 Oct 1;27(10):1693–1695. doi: 10.1038/s41591-021-01490-8. [DOI] [PubMed] [Google Scholar]
- 13.Godasi G.R., Donthu R.K., Mohammed A.S., Pasam R.S., Tiruveedhula S.L. Attitude towards COVID-19 vaccine among the general public in south India: a cross sectional study. Arch Ment Heal. 2021 Jan 1;22(1):28–35. [Google Scholar]
- 14.Cordina M., Lauri M.A., Lauri J. Attitudes towards covid-19 vaccination, vaccine hesitancy and intention to take the vaccine. Pharm Pract. 2021;19(1) doi: 10.18549/PharmPract.2021.1.2317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cherian V. Vaccine hesitancy for childhood vaccinations in slum areas of Siliguri: a critical commentary. Indian J Publ Health. 2019;63(2):160. doi: 10.4103/ijph.IJPH_57_19. [DOI] [PubMed] [Google Scholar]
- 16.Akhmetzhanova Z., Sazonov V., Riethmacher D., Aljofan M. Vaccine adherence: the rate of hesitancy toward childhood immunization in Kazakhstan. Expert Rev Vaccines. 2020 Jun 2;19(6):579–584. doi: 10.1080/14760584.2020.1775080. [DOI] [PubMed] [Google Scholar]
- 17.Kanozia R., Arya R. Fake news. religion, and COVID-19 vaccine hesitancy in India, Pakistan, and Bangladesh. Media Asia. 2021 Oct 2;48(4):313–321. doi: 10.1080/01296612.2021.1921963. [Internet] [DOI] [Google Scholar]
- 18.Love A.S., Love R.J. Considering needle phobia among adult patients during mass COVID-19 vaccinations. J. Prim. Care and Commun. Health. 2021;12 doi: 10.1177/21501327211007393. SAGE Publications Inc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bian L., Gao Q., Gao F., et al. Impact of the Delta variant on vaccine efficacy and response strategies. Expet Rev Vaccine. 2021;20:1201–1209. doi: 10.1080/14760584.2021.1976153. Taylor and Francis Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]