Abstract
Background:
Brown tumors (BTs) are rare non-neoplastic lesions that arise secondary to hyperparathyroidism largely involving mandible, ribs, pelvis, and large bones. Spinal involvement is extremely rare and may result in cord compression.
Case Description:
A 72-year-old female with the primary hyperparathyroidism developed a thoracic spine BT causing T3–T5 spinal cord compression warranting operative decompression.
Conclusion:
BTs should be included in the differential diagnosis in lytic-expansive lesions involving the spine. For those who develop neurological deficits, surgical decompression may be warranted followed by parathyroidectomy.
Keywords: Brown tumor, Primary hyperparathyroidism, Spinal cord compression

INTRODUCTION
Brown tumors (BTs) are rare benign and non-neoplastic lesions that arise secondary to hyperparathyroidism (i.e., primary, or rarely secondary).[6-11] They most commonly involve the mandible, ribs, pelvis, and large bones, and only rarely the spine.[7] Here, a T3–T5 thoracic BT, arising secondary to hyperparathyroidism, contributed to cord compression and a paraparetic deficit that resolved following decompressive surgery.
CASE REPORT
Clinical presentation
A 72-year-old female presented with the upper back pain of 6 months’ with one month of acute worsening associated with the onset of paraparesis (i.e., 3/5 deficit). Laboratory studies showed; a serum calcium level of 144 mg/L (normal: 90–105 mg/L) and a slightly high parathyroid hormone level (pg/mL; normal is 10–53 pg/mL). A thyroid ultrasound proved negative, but the parathyroid scintigraphy with Tc-99 m showed focal activity in the inferior right thyroid lobe consistent with a parathyroid adenoma.
Spine computed tomography (CT) and magnetic resonance (MR) studies showing cord compression due to BT at T3–T5 levels
Both the CT and MR studies showed BTs compressing the cord from T3 to T5 secondary to hyperparathyroidism. The thoracic CT demonstrated multiple osteolytic lesions of the vertebral bodies and posterior elements from Th3 to Th5 level [Figure 1]. The thoracic MR thoracic revealed a large expansile T3–T5 vertebral mass with extradural extension resulting in significant cord compression; it was isointense on T1, and hyperintense on T2-weighted images [Figure 2].
Figure 1:
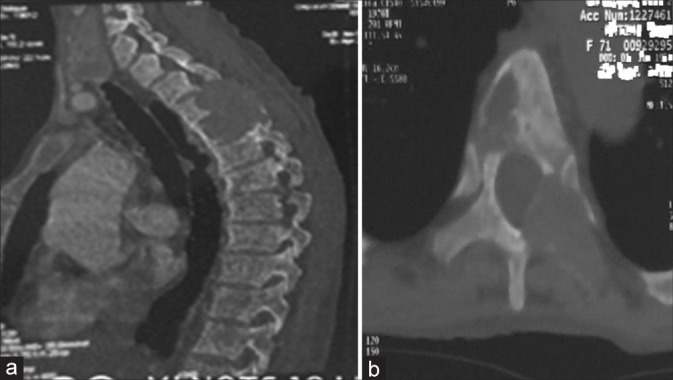
Computed tomography of the thoracic spine sagittal (a) and axial (b) images showing an osteolytic lesion regarding T3-T4-T5 with endocanalar extension.
Figure 2:
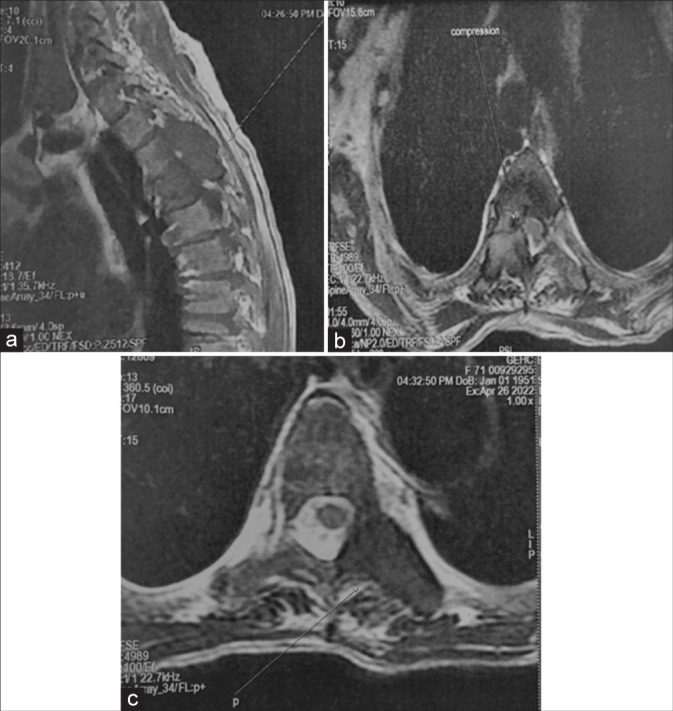
Sagittal T1-weighted (a), axial T2-weighted (b and c) images showing an expansile mass lesion with spinal cord compression at T3-4-5 level.
Surgery, pathology, and outcome
Following an emergent Th3-5 laminectomy, the extradural mass was totally excised, and the cord was adequately decompressed. The histopathological examination confirmed a BT secondary to hyperparathyroidism. Postoperatively, the patient’s symptoms resolved within 3 weeks. Subsequently, she was referred for a parathyroidectomy.
DISCUSSION
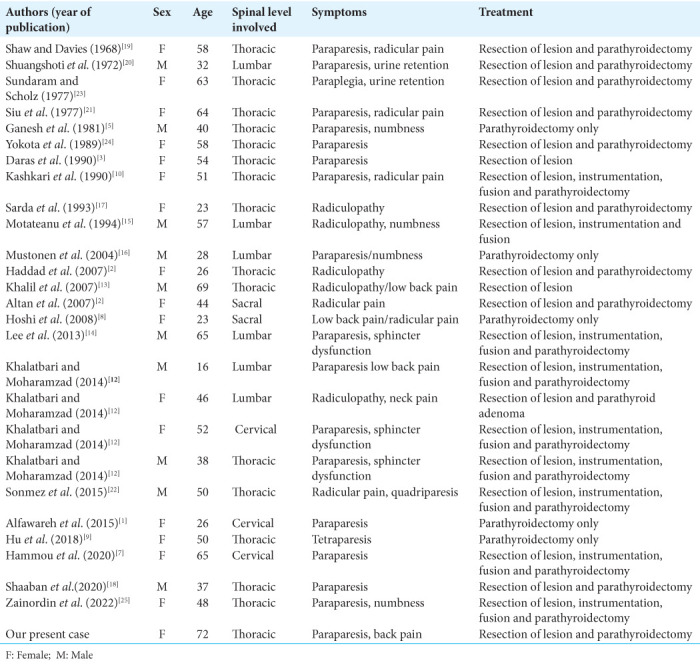
We identified 25 similar cases of BTs attributed primary hyperparathyroidism impacting the spine (since 1968 to present) [Table 1].[1-25] Most patients were female (62.9 %) averaging 46.5 years of age who presented with predominant thoracic lesions (59%) contributing to varying degrees of myelopathy [Table 1].[7-22] Surgical options included; biopsy, decompression/resection, or decompression/ instrumentation with fusion. Of the 25, 23 benefitted from parathyroidectomy. Typically, CT imaging documented BTs as well-defined soft-tissue masses with local bony erosion, expansion, while on magnetic resonance imaging studies, these lesions appear hypointense on T1, hypo- or hyperintense on T2-weighted images, with homogenous contrast enhancement.[7-22] The differential diagnoses these spinal lesions included; metastatic tumors, multiple myeloma, plasmacytoma, giant cell tumors, lymphoma, and aneurysmal bone cysts.[12-18]
Table 1:
Reported cases of spinal brown tumor secondary to primary hyperparathyroidism.
The gold standard for the treatment for BTs due to primary hyperparathyroidism remains gross total removal of the spine lesion (i.e., biopsy, decompression with/without fusion for those with neurological deficits) followed by parathyroidectomy.[7-18]
CONCLUSION
BTs should be included in the differential diagnosis of spinal lytic-expansive lesions with or without neurological deficits. The standard treatment is gross spinal total tumor excision followed by parathyroidectomy.
Footnotes
How to cite this article: Elmi SM, Djimrabeye A, Makoso JD, Hamdaoui R. Spinal cord compression caused by a brown tumor secondary to primary hyperparathyroidism. Surg Neurol Int 2023;14:108.
Contributor Information
Saad Moussa Elmi, Email: saad.elmi@yahoo.com.
Alngar Djimrabeye, Email: drdjimrabeye@gmail.com.
José Dimbi Makoso, Email: dimbijose@gmail.com.
Rayhane Hamdaoui, Email: Hamdaoui.rayhane@gmail.com.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Alfawareh MD, Halawani MM, Attia WI, Almusrea KN. Brown tumor of the cervical spines: A case report with literature review. Asian Spine J. 2015;9:110–20. doi: 10.4184/asj.2015.9.1.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Altan L, Kurtŏglu Z, Yalçınkaya U, Aydınlı U, Ertürk E. Brown tumor of the sacral spine in a patient with low-back pain. Rheumatol Int. 2007;28:77–81. doi: 10.1007/s00296-007-0380-z. [DOI] [PubMed] [Google Scholar]
- 3.Daras M, Georgakopoulos T, Avdelidis D, Gravani A, Tuchman AJ. Spinal cord compression in primary hyperparathyroidism: Report of a case and review of the literature. Spine Phila Pa. 1990;15:238–40. doi: 10.1097/00007632-199003000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Fargen KM, Lin CS, Jeung JA, Yachnis AT, Jacob RP, Velat GJ. Vertebral brown tumors causing neurologic compromise. World Neurosurg. 2013;79:208.e1–6. doi: 10.1016/j.wneu.2010.02.022. [DOI] [PubMed] [Google Scholar]
- 5.Ganesh A, Kuriant S, John L. Complete recovery of spinal cord compression following parathyroidectomy. Postgrad Med. 1981;57:652–3. doi: 10.1136/pgmj.57.672.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haddad FH, Malkawi OM, Sharbaji AA, Jbara IF, Rihani HR. Primary hyperparathyroidism. A rare cause of spinal cord compression. Saudi Med J. 2007;28:783–6. [PubMed] [Google Scholar]
- 7.Hammou O, Azzouzi H, Ichchou L. Spinal cord compression secondary to brown tumor as first manifestation of primary hyperparathyroidism. World Neurosurg. 2020;137:384–8. doi: 10.1016/j.wneu.2020.02.076. [DOI] [PubMed] [Google Scholar]
- 8.Hoshi M, Takami M, Kajikawa M, Teramura K, Okamoto T, Yanagida I, et al. A case of multiple skeletal lesions of brown tumors mimicking carcinoma metastases. Arch Orthop Trauma Surg. 2008;128:149–54. doi: 10.1007/s00402-007-0312-0. [DOI] [PubMed] [Google Scholar]
- 9.Hu J, He S, Yang J, Ye C, Yang X, Xiao J. Management of brown tumor of spine with primary hyperparathyroidism: A case report and literature review. Medicine (Baltimore) 2019;98:e15007. doi: 10.1097/MD.0000000000015007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kashkari S, Kelly TR, Bethem D, Pepe RG. Osteitis fibrosa cystica (brown tumor) of the spine with cord compression: Report of a case with needle aspiration biopsy findings. Diagn Cytopathol. 1990;6:349–53. doi: 10.1002/dc.2840060512. [DOI] [PubMed] [Google Scholar]
- 11.Kaya RA, Çavuşoğlu H, Tanik C, Kahyaoglu O, Dilbaz S, Tuncer C, et al. Spinal cord compression caused by a brown tumor at the cervicothoracic junction. Spine J. 2007;7:728–32. doi: 10.1016/j.spinee.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 12.Khalatbari MR, Moharamzad Y. Brown tumor of the spine in patients with primary hyperparathyroidism. Spine (Phila Pa 1976) 2014;39:E1073–9. doi: 10.1097/BRS.0000000000000455. [DOI] [PubMed] [Google Scholar]
- 13.Khalil PN, Heining SM, Huss R, Ihrler S, Siebeck M, Hallfeldt K, et al. Natural history and surgical treatment of brown tumor lesions at various sites in refractory primary hyperparathyroidism. Eur J Med Res. 2007;12:222–30. [PubMed] [Google Scholar]
- 14.Lee JH, Chung SM, Kim HS. Osteitis fibrosa cystica mistaken for malignant disease. Clin Exp Otorhinolaryngol. 2013;6:110–3. doi: 10.3342/ceo.2013.6.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Motateanu M, D´eruaz JP, Fankhauser H. Spinal tumour due to primary hyperparathyroidism causing sciatica: Case report. Neuroradiology. 1994;36:134–6. doi: 10.1007/BF00588079. [DOI] [PubMed] [Google Scholar]
- 16.Mustonen AO, Kiuru MJ, Stahls A, Bohling T, Kivioja A, Koskinen SK. Radicular lower extremity pain as the first symptom of primary hyperparathyroidism. Skeletal Radiol. 2004;33:467–72. doi: 10.1007/s00256-004-0803-9. [DOI] [PubMed] [Google Scholar]
- 17.Sarda AK, Arunabh, Vijayaraghavan M, Kapur M. Paraplegia due to osteitis fibrosa secondary to primary hyperparathyroidism: Report of a case. Surg Today. 1993;23:1003–5. doi: 10.1007/BF00308978. [DOI] [PubMed] [Google Scholar]
- 18.Shaaban AT, Ibrahem M, Saleh A, Haider A, Alyafai A. Brown tumor due to primary hyperparathyroidism resulting in acute paraparesis: Case report and literature review. Surg Neurol Int. 2020;11:355. doi: 10.25259/SNI_653_2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shaw MT, Davies M. Primary hyperparathyroidism presenting as spinal cord compression. Br Med J. 1968;4:230–31. doi: 10.1136/bmj.4.5625.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shuangshoti S, Hongsaprabhas C, Chandraprasert S, Rajatapiti B. Parathyroid adenoma, brown tumor and cauda equina compression. J Med Assoc Thai. 1972;55:251–8. [PubMed] [Google Scholar]
- 21.Siu K, Sundaram M, Schultz C, Kirwan L. Primary hyperparathyroidism presenting as spinal cord compression: Report of a case. Aust N Z J Surg. 1977;47:668–72. doi: 10.1111/j.1445-2197.1977.tb06601.x. [DOI] [PubMed] [Google Scholar]
- 22.Sonmez E, Tezcaner T, Coven I, Terzi A. Brown tumor of the thoracic spine: First manifestation of primary hyperparathyroidism. J Korean Neurosurg Soc. 2015;58:389–92. doi: 10.3340/jkns.2015.58.4.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sundaram M, Scholz C. Primary hyperparathyroidism presenting with acute paraplegia. AJR Am J Roentgenol. 1977;128:674–6. doi: 10.2214/ajr.128.4.674. [DOI] [PubMed] [Google Scholar]
- 24.Yokota N, Kuribayashi T, Nagamine M, Tanaka M, Matsukura S, Wakisaka S. Paraplegia caused by brown tumor in primary hyperparathyroidism: Case report. J Neurosurg. 1989;71:446–8. doi: 10.3171/jns.1989.71.3.0446. [DOI] [PubMed] [Google Scholar]
- 25.Zainordin NA, Azraai AM, Shah FZ, Ghani RA. Primary hyperparathyroidism presenting with sudden onset paraplegia. SAGE Open Med Case Rep. 2022;10:2050313-X221089759. doi: 10.1177/2050313X221089759. [DOI] [PMC free article] [PubMed] [Google Scholar]


