Highlights
-
•
Seizures arising from the occipito- temporal region may lead to face perception changes, or ‘prosopometamorphopsia’.
-
•
Ictal experiences may have significant psychosocial and developmental consequences, particularly in young people.
-
•
Tattoos may be rich sources of insight into patient experiences and facilitate a therapeutic process.
Keywords: Tattoos, Epilepsy, Prosopometamorphopsia, Neuropsychiatry, Social anxiety, Cognitive behavioural therapy
Abstract
We present a case of a young man with frightening ictal disturbance of face perception, or prosopometamorphopsia, arising from the left temporo-occipital region, leading to significant psychosocial impairment. A vivid forearm tattoo of the ictal experience conveyed its nature to the treating team and facilitated a psychotherapeutic process leading to significant psychosocial recovery. This case highlights the marked psychosocial and developmental impacts of epilepsy and the benefit of incorporating these into assessment and treatment.
Introduction
Although ‘insight’ is typically preserved in cases of organic perceptual disturbance, such experiences can be fear-provoking and lead to significant psychiatric disability and developmental deviation. We report a case that highlights the infrequent ictal phenomenon of prosopometamorphopsia and its impact on a young man’s psychosocial development in adolescence. We illustrate that, as well as improving his seizure control, attending to the tattoos that represented his ictal experiences also enabled a psychotherapeutic process and psychosocial recovery.
Case
A previously well, left-handed, 12yo boy reported experiencing the sudden onset of facial perceptual distortion – out of nowhere, whilst alone in his bedroom, he visualised the faces of friends and loved ones morph and meld into a hideous amalgam, a feeling of impending doom simultaneously rising. These “melting zombie faces” then became a formed, complex hallucination of a tall, shrouded figure looming over his bed before falling on top of him. Fighting through this figure, terrified, he ran to his parents’ bedroom, only to see the doorknob move higher and higher out of his reach before he collapsed into a focal to bilateral tonic-clonic seizure (FBTCS). Investigations later revealed a focal epilepsy arising in the left posterior cerebral quadrant, and he was treated with combination antiseizure medications (ASM) (oxcarbazepine, clobazam and topiramate).
Frightening auras, often progressing to FBTCS, continued to occur intermittently. As a teenager, he began describing additional simple and complex visual phenomena as part of his aura, at times without the perceptual face distortion; these would often evolve into periods of impaired awareness and FBTCS. This newer semiology would consist of elemental visual hallucinations of red lines in the right upper visual field, impaired depth perception and a sensation of 'reduced vision’ in the right visual field. Together, these led to increasing phobic avoidance of associated triggers; whilst ongoing worry about having a seizure in public led to worsening social isolation and agoraphobia, and significant developmental and social regression – from being outgoing, confident and sporty, the patient increasingly spent time at home, with limited social contact or occupation.
At age 19, the patient underwent a comprehensive inpatient epilepsy evaluation. MRI brain and FDG-PET scans were within normal limits. Language fMRI was consistent with left language lateralisation. During 5-day Video EEG monitoring (VEM), a single FBTCS with frightening ictal prosopometamorphopsia at seizure-onset was captured, arising focally from the left temporo-occipital region (Fig. 1B-G).
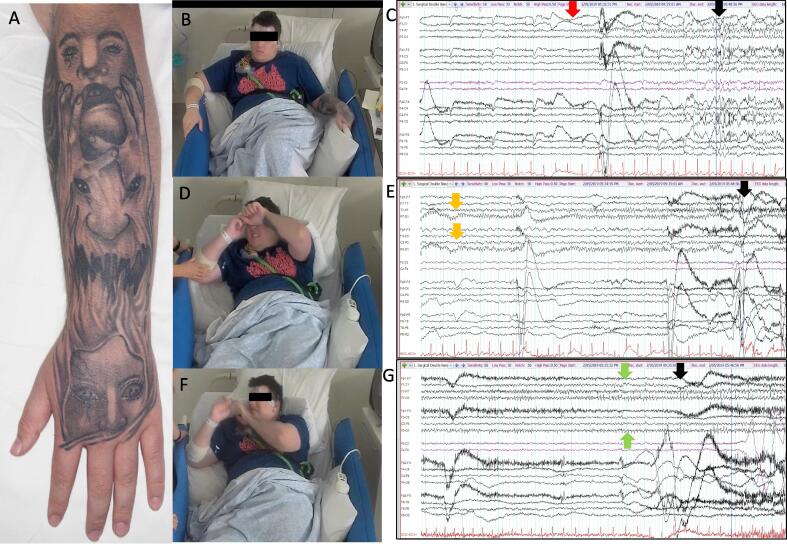
Fig. 1.
(A) Left dorsal foreman tattoos of ictal prosopometamorphopsia. B -G: Electroclinical seizure featuring frightening ictal prosopometamorphopsia. C, E, G: 10–20 EEG array, 20 s epochs displayed (high pass 0.5 Hz, low pass 30 Hz). Solid arrows indicate the timepoint corresponding to adjacent picture. The ictal onset is localised to left temporo-occipital region (maximal at electrode P7, red arrow, C) and precedes the clinical onset by 20 s. Clinically the seizure begins with a gradual appearance of discomfort and scared facial expression. Early in the seizure, the patient tells the nurse he feels - “not good” (B). Electrographically the seizure propagates across the left posterior quadrant (E: orange arrows, 2min40sec after onset) coinciding with the patient displaying a marked passive fear response (D: covering eyes, protecting face with arms and fearful facial expression). The seizure spreads across the left hemisphere (G: green arrows, 2min50sec after onset) and a more dramatic fearful response is observed with crying out and gaze preference to the right (F). This precedes forced version (not shown) and FBTCS. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Neuropsychiatric assessment during the VEM admission revealed severe agoraphobia with panic, accompanied by a moderate major depressive disorder. Also noted was a striking tattoo covering the dorsum of the left forearm, a composite of the illusions and hallucinations experienced throughout his teens (Fig. 1A).
Following the VEM admission, he was maintained on combination ASM and was further evaluated for epilepsy surgery. The patient was also commenced on sertraline and referred for exposure-based cognitive behavioural therapy (CBT). On review 6 months later, he reported significant improvements in mood and reductions in anxiety and social isolation. He had subsequently augmented his forearm tattoo so that the reverse side was covered in large script stating his surname. Exploration of the meaning of this, and of the original tattoo, facilitated a therapeutic dialogue around the place of epilepsy in his life and the reclamation of his identity, despite his illness and the frightening visions that had accompanied it [1].
Discussion
Although reported rarely, prosopometamorphopsia is typically seen with structural or functional pathologies arising from the complex face-processing networks of the fusiform and ventral occipito-temporal cortices [2], [3], and may also be associated with elemental and complex visual hallucinations (CVH). The latter may also result from other visual system or ascending projection lesions, or from global cerebral insults [4]. Although insight into the basis of these CVHs is usually preserved, the content may be disturbing and highly aversive. Unpleasant and even grotesque facial metamorphopsia have been previously described as an ictal phenomenon localising to the right temporo-occipital junction [5] and can be induced with cortical stimulation to this face sensitive area [6].
A recent review compiling previously published cases of prosopometamorphopsia suggests a disseminated network of facial gestalt perception incorporating bilateral temporo-occipital regions, corpus callosal and frontal regions [3]. In the current case, the presumed temporo-occipital epileptogenic zone, based upon anatamo-clinical correlations, is consistent with the literature’s localisation of these complex visual phenomena. This case provides evidence that these semiological features are not exclusively lateralised to the non-dominant hemisphere, and is in keeping with cortical stimulation evidence that both left and right fusiform gyri are face-selective areas [7].
Tattoos have been long-used as markings of group affiliation, rites of passage, and individual identity, and have become increasingly mainstream. As symbolic representations of individual meaning, tattoos can be fertile sources of connection with patients, enriching therapeutic dialogue. They may also enhance the descriptive phenomenology and semiology of patient experience [8].
Ethical statement
Written consent was obtained from the patient, and institutional approval obtained for the study.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Roggenkamp H., Nicholls A., Pierre J.M. Tattoos as a window to the psyche: How talking about skin art can inform psychiatric practice. World J Psychiatr. 2017;7(3):148–158. doi: 10.5498/wjp.v7.i3.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.ffytche DH, Blom JD, Catani M. 2010. Disorders of visual perception. J Neurol Neurosurg Psychiatry; 81: 1280-1287. [DOI] [PubMed]
- 3.Blom J.D., ter Meulen B.C., Dool J., ffytche D.H. A century of prosopometamorphopsia studies. Cortex. 2021;139:298–308. doi: 10.1016/j.cortex.2021.03.001. [DOI] [PubMed] [Google Scholar]
- 4.Mocellin R., Walterfang M., Velakoulis D. Neuropsychiatry of complex visual hallucinations. Aust N Z J Psychiatry. 2016;40:742–751. doi: 10.1080/j.1440-1614.2006.01878.x. [DOI] [PubMed] [Google Scholar]
- 5.Heo K., Cho Y.J., Lee S.-K., et al. Single-photon emission computed tomography in a patient with ictal metamorphopsia. Seizure. 2004;13(4):250–253. doi: 10.1016/S1059-1311(03)00194-8. [DOI] [PubMed] [Google Scholar]
- 6.Jonas J., Jacques C., Liu-Shuang J., Brissart H., Colnat-Coulbois S., Maillard L., et al. A face-selective ventral occipito-temporal map of the human brain with intracerebral potentials. Proc Natl Acad Sci. 2016;113(28) doi: 10.1073/pnas.1522033113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keller C.J., Davidesco I., Megevand P., Lado F.A., Malach R., Mehta A.D. Tuning face perception with electrical stimulation of the fusiform gyrus. Hum Brain Mapp. 2017 Jun;38(6):2830–2842. doi: 10.1002/hbm.23543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lemma I. (2010). Ink, holes and scars. in Under the Skin: A Psychoanalytic Study of Body Modification. Taylor and Francis, Florence. 148-171.