Abstract
In the wake of mass COVID-19 vaccination campaigns in 2021, significant differences in vaccine skepticism emerged across Europe, with Eastern European countries in particular facing very high levels of vaccine hesitancy and refusal. This study investigates the determinants of COVID-19 vaccine hesitancy and refusal, with a focus on these differences across Eastern, Southern and Western Europe. The statistical analyses are based on individual-level survey data comprising quota-based representative samples from 27 European countries from May 2021. The study finds that demographic variables have complex associations with vaccine hesitancy and refusal. The relationships with age and education are non-linear. Trust in different sources of health-related information has significant associations as well, with people who trust the Internet, social networks and ‘people around’ in particular being much more likely to express vaccine skepticism. Beliefs in the safety and effectiveness of vaccines have large predictive power. Importantly, this study shows that the associations of demographic, belief-related and other individual-level factors with vaccine hesitancy and refusal are context-specific. Yet, explanations of the differences in vaccine hesitancy across Eastern, Southern and Eastern Europe need to focus on why levels of trust and vaccine-relevant beliefs differ across regions, because the effects of these variables appear to be similar. It is the much higher prevalence of factors such as distrust of national governments and medical processionals as sources of relevant medical information in Eastern Europe that are relevant for explaining the higher levels of vaccine skepticism observed in that region.
Keywords: Covid-19, Media consumption, Public opinion, Trust, Vaccination, Vaccine hesitancy
1. Introduction
The approval of vaccines against COVID-19 in late 2020 brought hope to citizens and policymakers that the raging pandemic soon will be curtailed and that harsh restrictive societal lockdowns will no longer be necessary to contain the spread of the virus. Moving with different speeds, most European countries rolled out mass vaccination campaigns throughout 2021. While in the beginning insufficient vaccine supply was the limiting factor for the success of the vaccination efforts, soon a different obstacle became evident – namely, vaccine hesitancy amongst some parts of the population [1].
Vaccine hesitancy, defined as ‘delay in acceptance or refusal of vaccination despite availability of vaccination services’ [2], is not a new phenomenon. Trends of increasing vaccine hesitancy among different social groups in various countries had been noted by social scientists and public health experts already [i.a. [3], [4], for recent systematic reviews, see [5], [6]]. However, the scale of vaccine hesitancy in many parts of Europe was still surprising, especially given a context where the virus and the associated disease targeted by the vaccines presented such a clear and immediate danger. Moreover, vaccine hesitancy proved largely resistant to government appeals and only weakly responsive to policy interventions [7].
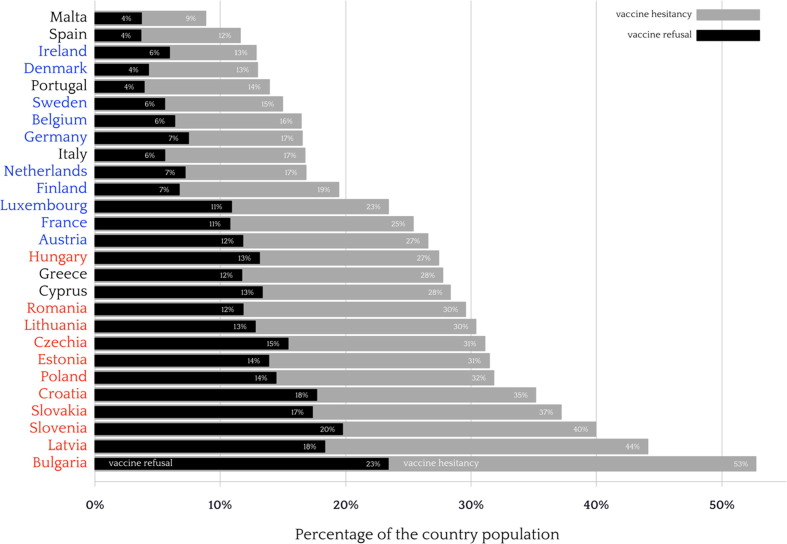
As of May 2021, very significant differences in vaccine hesitancy in different regions of Europe emerged. Fig. 1 shows the rankings of 27 members of the European Union with respect to the country averages of vaccine refusals (respondents who declare that they will never get a COVID-19 vaccine) and vaccine hesitancy (a broader concept that also includes those who say they will delay getting a vaccine or have not decided yet) [8]. The highest levels of vaccine refusal and hesitancy were observed in Bulgaria – where more than half of the population expressed hesitancy or refusal to vaccinate, followed by Latvia and Slovenia. The lowest levels were observed in Spain and Malta. Altogether, the top 10 vaccine-sceptic populations in the European Union were in the Eastern part of the continent. The Southern European countries were dispersed in the middle (Cyprus, Greece) and bottom of the ranking. From the Western European countries, Austria, France and Luxembourg exhibited relatively high levels of vaccine hesitancy (between 27% and 23% of the population) and refusal (between 12% and 11%).
Fig. 1.
Prevalence of vaccine refusal (black bars) and hesitancy (dark-grey bars) in the Europe Union, per country. Country names are coloured per region (Eastern in red, Western in blue and Southern in black). Estimates are adjusted by post-stratification weights. Data: Flash Eurobarometer 494, May 2021. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
This article addresses the puzzle of significant variation in vaccine attitudes across Eastern, Southern and Western Europe. It tests whether the effects 1 of demographic variables, trust-related attitudes and COVID-19-related beliefs and experiences differ across these regions. The statistical analyses show that the effects of these factors are largely similar across regions, but their levels differ markedly. Hence, it is not different attitude structures that explain vaccine hesitancy across Europe, but different levels of the relevant explanatory factors, such as trust in government, the medical profession, using the internet as a source of medical information, and experience with COVID-19.
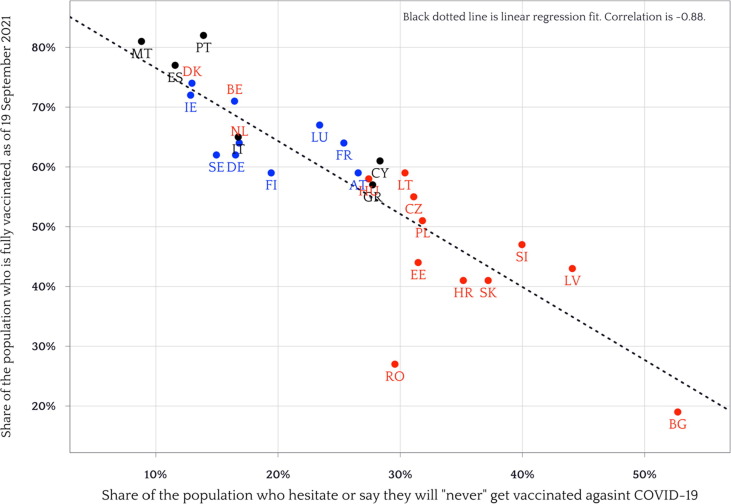
The importance and policy relevance of these attitudes is demonstrated by their very strong relationship with actual levels of vaccine uptake. At the country level, with 27 observations, the correlation is −0.88 and the link is quite linear (see Fig. 2 for the plot), with Romania being a notable outlier, as its vaccination rate is lower than the one predicted by its level of vaccine hesitancy.
Fig. 2.
Relationship between vaccine hesitancy and vaccination rates in 27 member states of the European Union (ISO 3166–1 alpha-2 country codes). Attitude data: Flash Eurobarometer 494, May 2021. Vaccination data: Our World in Data, as of 19 September 2021.
The main contributions of the article are three. First, it provides a comprehensive analysis of the influence of a large number of demographic and trust-related variables, as well as COVID-related experiences and beliefs for a large number of European states. Second, it identifies the difference in levels of vaccine hesitancy predictors in Eastern Europe rather than differential effects of these variables as potential explanations for the much higher levels of vaccine hesitancy and refusal in the region. Third, it shows that the effects of age and education are non-linear and the one of age is direct and indirect (via vaccine-related beliefs). Overall, the article contributes to understanding how social and political attitudes, which significantly affect the fight against pandemics [9], are formed and sustained.
2. Theoretical considerations
Existing scholarship already draws attention to the problem of vaccine hesitancy [i.a. 3] and provides important insights about its possible causes and predictors [10]. For example, Sallam draws attention to the low levels of COVID-19 vaccine acceptance in the Middle East, Russia, Africa and some Eastern European countries [11]. Obregon et al. [12] also note that the prevalence in vaccine hesitancy has been increasing in countries in Eastern Europe and Central Asia. Neumann-Böhme et al. [13] draw attention to high and increasing vaccine hesitancy with regard to COVID-19 vaccines.
Based on existing literature we can identify several clusters of variables that might be significant predictors of vaccine hesitancy with respect to COVID-19 vaccines [c.f. 14]. The first cluster refers to demographic factors, the second one refers to trust in different sources of vaccine-relevant information and the third one refers to experiences with (personal exposure to) and beliefs about COVID-19 itself.
The large comparative study of 19 countries reported in Lazarus et al. (2020) reports that several demographic factors are significantly associated with vaccine hesitancy [10, see also 15]. There are well-documented differences in vaccine hesitancy between men and women [16], [17]. The associations, however, are complex and differ across studies, with some finding the women are more likely to be vaccine hesitant (also with respect to COVID-19 vaccines) [18] and others finding the opposite pattern [19]. With respect to age, younger people (than 65) are more likely to be vaccine deniers [17]. Lazarus et al. [18] also find that people older than 50 are more likely to accept vaccines in most countries they study, with the important exception of China. The effect of education is even more complex and heterogeneous. According to Lazarus et al. [18], higher education is positively associated with vaccine acceptance in Ecuador, France, Germany, India, and the US, but negatively associated in Canada, Spain, and the UK. There is further evidence that higher education is associated with lower vaccine hesitancy in the UK [20] and in the US [21]. Sylvester [22] concludes that coronavirus knowledge is influenced by both political ideology and education level.
In-depth studies convincingly argue that vaccine hesitancy is not necessarily a low education phenomenon. One study identifies five groups that are more likely to be under-vaccinated: Orthodox (Reformed) Protestant communities, Anthroposophists, Roma, Irish Travellers, and Orthodox Jewish communities. The Anthroposophists are particularly interesting, because they tend to be highly educated. Their vaccine hesitancy stems from a belief that ‘a healthy life, a good nutrition (e.g., breastfeeding for babies), and a safe environment (e.g. mothers who stay at home to take care of their children)’ lead to a strong immune system of their children, which can better fight infections diseases so that vaccine are not necessary [23, see also 24].
In addition to age, sex, and education, other socio-demographic factors that have been shown to be possible predictors and causes of vaccine hesitancy include employment, income [20] and occupation. In fact, according to [17], the economic situation was the strongest predictor of vaccine hesitancy and refusal, with significant differences between (self-)employed, retired and respondents with other (non–)working status.
The second cluster of variables that are potential predictors of vaccine hesitancy relate to the source of medical and vaccine-related information that people consider trustworthy [3], which is related to (mis)information about the safety and effectiveness of vaccines. Overall, trust in doctors and nurses was strongly associated with trust in vaccines, but relatively to a smaller extent in Europe than in other parts of the world, according to data from the 2018 Wellcome Global Monitor Report [12]. According to the comparative study of Lindholt et al. [10], vaccine hesitancy was associated with ‘lack of trust in authorities and scientists, conspiratorial thinking, and a lack of concern about COVID-19′. More generally, trust in government has been shown to be related to compliance with COVID-19 related restrictions, although the effects differ across countries [25], and with vaccination intentions [26].
But people get information about vaccines from various sources, not restricted to the medical community. Television was identified as the primary source for information about vaccination in a recent study [27]. But the importance of the Internet and online social networks as sources for health-related information is growing. The usage, however, is heterogeneous [28]. Information from social media was one of the main causes of vaccine hesitancy with regard to measles [29, see also 30]. Internet access, and the associated spread of misinformation, might account for the higher levels of vaccine hesitancy observed in richer countries [31]. Information from friends and other acquaintances might be important as well, as personal connections have been shown to influence compliance with COVID-19 related public policies [32].
The political character of the media consumed by the citizens is important as well, at least in the US [33]. Relatedly, in the US conspiracy beliefs were found to mediate the effects of demographic variables [21]. More generally, political attitudes have been linked with vaccine hesitancy in the context of COVID-19. For example, in France the intention to vaccinate against COVID-19 was related to political attitudes, with people supporting extreme parties – both on the Left and on the Right – and people not feeling close to any party being least likely to (intend to) vaccinate [34]. In the US, political affiliation was one of the two most salient factors associated with vaccine hesitancy [35]. A study of seven European countries concluded that Leftists were less likely to be vaccine hesitant that people on the political Right and those who refused to place themselves on the Left-Right scale [36]. Stoeckel et al. however found little evidence that partisanship mattered for support for COVID-19 ‘vaccine passports’ in France, Germany and Sweden [37]. While the current study does not test the effects of political attitudes directly, it explores the connection with trust in government as a source of information, which is significantly correlated with support for political extremism and non-participation.
The third cluster of theoretically-important variables relate to beliefs about (COVID-19) vaccines and beliefs about and personal exposure to the disease itself. Poor knowledge of COVID-19 and compliance with government COVID-19 guidelines were predictive of distrust in vaccines in the UK [20]. Fear of vaccine side effects was the most often mentioned complaint about COVID-19 vaccination [38]. Cross-country studies also find that fear and personal perceptions of risk of COVID-19 infection are major factors related to the willingness to vaccinate [39]. Knowing someone who was severely affected by the virus increased the willingness to be vaccinated [17]. Prior to COVID-19, studies had also found that knowledge about the effectiveness and safety of vaccination increases the probability of having received a vaccination in the past five years [27].
All factors and studies considered so far work at the individual level. There is less work focused on explaining cross-country differences in vaccination attitudes. Sturgis et al. (2021) conclude that ‘[i]n countries with a high aggregate level of trust in science, people are more likely to be confident about vaccination, over and above their individual-level scientific trust. Additionally, … societal consensus around trust in science moderates these individual-level and country-level relationships’ [40].
The (post)communist background of countries has also been linked to higher levels of vaccine hesitancy. The explanation lies ‘in a wider distrust in public and state institutions resulting from the exposure to Soviet communism.’, according to Costa-Font et al. [41]. Studies of particular post-communist countries exist as well. In Slovenia ‘higher intention to get vaccinated is associated with men, older respondents, physicians and medical students, respondents who got the influenza vaccination, those who knew someone who had gotten hospitalised or died from COVID-19 and those who have more trust in experts, institutions and vaccines.’ In addition, nurses and technicians were found to be less likely to get vaccinated [42]. In Poland, the fear the fear of vaccines’ side effects, beliefs in conspiracy theories and physical fitness were identified as major predictors of COVID-19 vaccine hesitancy [43]. The broader phenomenon of vaccine hesitancy in Poland has been linked to the political phenomenon of populism in Eastern Europe, and the anti-Enlightenment and anti-Western shift in the public sphere in the region [44] and with the spread of fake news [45]. Pronkina et al. [46] found that ‘exposure to the Communist regime in East Germany decreased one's probability to get vaccinated against COVID-19 by 8 percentage points and increased that of refusing the vaccine by 4 percentage points.’ The lower level of social capital in East Germany accounted for a small but significant part of the gap.
Overall, the existing literature identifies a large number of demographic and other variables with significant associations with vaccine hesitancy and refusal. The effects of these variables, however, are very heterogeneous, which necessitates cross-country comparative analyses that can account for how the effects differ across countries and regions. Furthermore, most of the studies do not attempt to establish the causal ordering of the covariates. To address these limitations, the analyses reported below cover a large number of countries, allow the effects to vary across regions, and introduce mediation models in which trust in sources of vaccine-related information and vaccine-related beliefs mediate the effects of demographic variables, such as age and education.
3. Data and operationalization
The empirical part of this article analyzes the data from Flash Eurobarometer 494. This comparative survey of public attitudes was fielded in May 2021 at the request of the European Commission by Ipsos European Public Affairs, Brussels [cf. 4]. The survey was based on quota-based nationally-representative samples from the 27 member states of the EU. The interviews were web-based and conducted via self-administered questionnaires. The sample size for most countries was around 1,000 respondents (Malta, Cyprus and Luxembourg had a smaller number of respondents at around 515 each). Descriptive statistics of all variables used in the empirical analyses are reported in Table S1 in the Supplementary material.
3.1. Outcome variables
The main outcome variables of interest are COVID-19 vaccine hesitancy and vaccine refusal. Respondents are considered ‘vaccine hesitant’ if they responded that they will get vaccinated against COVID-19 ‘Later’ (but not ‘some time in 2021′) or ‘Never’, or replied ‘Don’t know’ or preferred not to answer the question. This operationalization captures active demand for rather than passive acceptance of vaccines [cf. 47]. It is also in line with the definition of vaccine hesitancy as ‘a psychological state of indecisiveness that people may experience when making a decision regarding vaccination’ [48]. To probe the robustness of our results, we also report results based on an alternative operationalization of vaccine hesitancy that excludes ‘Don’t know’ and missing answers.
Vaccine refusal refers only to those who declared that they will ‘Never’ get vaccinated. The original formulation of the survey question is: ‘When would you like to get vaccinated against COVID-19 (coronavirus)?’ and the remaining answer categories, in addition to the ones mentioned above, are ‘As soon as possible’, ‘Some time in 2021′, and ‘I have already been vaccinated’.
3.2. Demographic predictors
The main demographic predictors of interest are age (measured in years), education (measured as the age at which full-time education was stopped), gender, place of residence (‘Large town/city’ vs. ‘Small or medium-sized town’ and ‘A rural area of village’), and professional occupation (with four categories: ‘Self-employed’, ‘Employee’, ‘Manual worker’, and ‘Without a professional activity').
3.3. Trust
Trust in different authorities with respect to COVID-19-related information is measured via the question ‘Among the following sources, which ones would you trust more to give you reliable information on COVID-19 vaccines?’, with multiple answers possible from the following categories: ‘The European Union’, ‘The National Government’, ‘The National Health Authorities’, ‘The regional or local public authorities’, ‘Health professionals, doctors, nurses and pharmacists’, ‘Media (television, radio, newspapers’, ‘Websites’, ‘Online social networks’, ‘People around you (colleagues, friends and family)’ and ‘Don’t know’). Each respondent gets a value of ‘1′ for each information source if this source had been picked as trustworthy and ‘0′ otherwise.
3.4. Vaccine-related beliefs
Two vaccine-related beliefs are measured: ‘Vaccines are safe’ and ‘Vaccines are effective’. Originally, answers to both are recorded on 4-point agreement scales, which have been collapsed in two categories (‘Agree totally or tend to agree’ vs. ‘Disagree totally or tend to disagree’).
3.5. Personal exposure and affect towards COVID-19
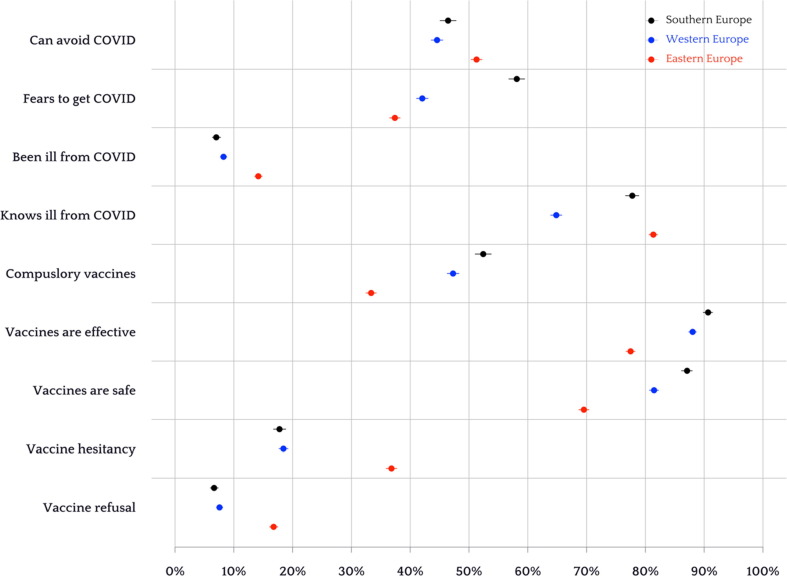
Several items related to personal exposure and affect towards COVID-19 are used: whether the respondent knows people who have tested positive or have been ill (‘knows ill from COVID-19′), whether the respondent has tested positive or has been ill (‘was ill from COVID-19′), and whether the respondent fears to be infected with COVID-19 in the future (‘fears infection from COVID-19′). In addition, in the descriptive analysis (Fig. 3 ), the belief whether one can avoid being infected from COVID-19 without having been vaccinated and the attitude towards compulsory vaccinations against COVID-19 are explored.
Fig. 3.
Personal exposure and affect towards COVID-19, as well as beliefs and attitudes towards COVID-19 vaccines in three regions of the Europe (Eastern in red, Western in blue, Southern in black. Unweighted region-level averages of the country-level point estimates of the proportions in the population and 95% confidence intervals (based on the Wilson method). Data: Flash Eurobarometer 494, May 2021. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3.6. Regions of Europe
As explained above, we group the countries of the respondents into three sets based on geographical location, historical legacies and political culture: Eastern Europe (Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Lithuania, Poland, Romania, Slovakia, Slovenia), Western Europe (Austria, Belgium, Denmark, Finland, France, Germany, Ireland, Luxembourg, the Netherlands, Sweden) and Southern Europe (Cyprus, Greece, Italy, Malta, Portugal, Spain). The countries in Eastern Europe share a communist past and post-communist patterns of political competition and political culture. The countries in Southern Europe are characterized by lower levels of political trust than countries in the West of the continent and have relatively lower levels of economic development and administrative capacities, compared to the West.
4. Empirical results
4.1. Levels of variables per region
We begin the empirical analysis with a descriptive overview of the variables per region to demonstrate the differences in levels. Fig. 3 shows the means of the country-level estimates per region (data is not weighted: differences in country size are not taken into account). At the bottom of the figure, we can see the confirmation of the patterns already visible in the Fig. 1: in Eastern Europe, levels of vaccine refusal and hesitancy are significantly higher (in fact, both are more than twice as high) than in the South and West of the continent. Beliefs that COVID-19 vaccines are safe and effective are also much lower in Eastern Europe, as is support for compulsory vaccination. However, people in Eastern Europe are actually more likely to report that they personally know someone who has been ill from COVID-19 (especially compared to Western Europe) and that they have been ill themselves. At the same time, Eastern Europeans are less likely to fear getting infected with COVID-19 and more likely to believe that they can avoid it without vaccination. When we consider the comparison between Southern and Western Europe, the most striking differences are with respect to fears to get COVID-19 and knowing someone who has been ill, both of which are much higher in the South. What we can conclude so far is that the much higher vaccine hesitancy and refusal in Eastern Europe might be related to beliefs about the effectiveness, safety and necessity of the vaccines, but not to lack of direct or indirect experience with COVID-19.
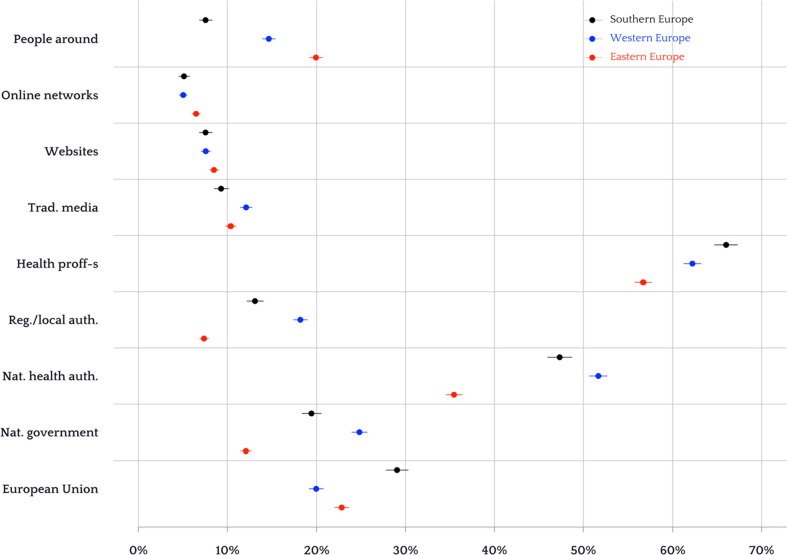
Since beliefs about vaccines appear important, we examine which sources of information on COVID-19 vaccines respondents consider to be trustworthy. Fig. 4 shows the means of the country-level estimates of the proportions of respondents who trust different actors per region. As with Fig. 3, data is unweighted. There are some striking differences, with East Europeans being much more likely to trust ‘people around you (colleagues, friends and family)’ and online social networks, rather than ‘health professionals, doctors, nurses and pharmacists’, national health authorities, regional and national governments. What is peculiar to the pattern in Southern Europe is that trust in the national and local governments is lower than in the West (but not as low as in the East), while trust in the EU and health professionals is higher. Importantly, trust in the traditional media (television, radio, newspapers) is lowest in Southern Europe.
Fig. 4.
Trust in different ‘sources of reliable information about COVID-19 vaccines’ in three regions of the Europe (Eastern in red, Western in blue, Southern in black. Unweighted region-level averages of the country-level point estimates of the proportions in the population and 95% confidence intervals (based on the Wilson method). Data: Flash Eurobarometer 494, May 2021. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
So far, we considered only aggregate regional statistics, which are suggestive of possible explanations for the differences in vaccine attitudes we observe between regions, but to probe these explanations further, we move the analysis to the individual level.
4.2. Non-parametric effects of age and education
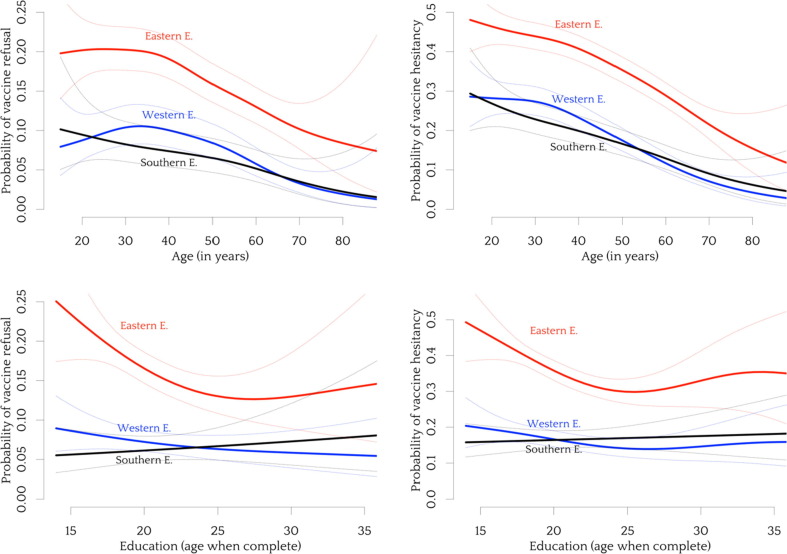
First, we consider the effects of two demographic variables – age and education. We cannot assume that the effects of these variables are linear, so we use general additive models [49], which allow for flexible forms of the associations. Fig. 5 shows the probabilities of vaccine refusal (left) and hesitancy (right) per region. While greater age is altogether associated with lower levels of vaccine refusal and hesitancy, in Eastern Europe the effects are relatively flat until middle age (38 years or so), especially with regard to refusal.
Fig. 5.
Non-linear effects of age (top row) and education (bottom row) on vaccine refusal (left column) and vaccine hesitancy (right column) in each of three regions of Europe. Semi-parametric smooth estimates of the effects based on generalized additive models (GAM). Dotted lines indicate the boundaries of the 95% confidence intervals.
In Western Europe the probability of refusal actually increases between age 20 and 30, while in Southern Europe the decline of the probability of vaccine refusal with age is linear.
The patterns differ across regions even more when it comes to the effects of education. In Southern Europe, the probability of vaccine refusal is increasing with education (age at which education was complete) and the probability of vaccine hesitancy is flat. In Western Europe the probability of vaccine refusal slightly declines and the probability of hesitancy drops until a point, but then stabilizes and even increases a bit. The pattern is similar in Eastern Europe as well, but starting from a much higher level for the lower educated. We conclude that the bivariate effects of age and education on vaccine hesitancy and refusal are altogether negative, but possibly non-linear and heterogenous across European regions.
4.3. Effects of trust in different information sources, demographics and COVID-19 beliefs and experiences
Next, we move to multivariate logistic regression models of vaccine hesitancy. Table 1 summarizes three models: the first one only features the trust-related predictors, the second one adds demographic variables, and the third one adds beliefs about COVID-19 vaccines and experiences related to COVID-19. The reason to present the three models separately is to examine how the effects of the information-based variables change once we add the possibly-confounding demographic variables and when we add the possibly-mediating COVID-19 beliefs and experiences.
Table 1.
Multivariate logistic regression models of vaccine hesitancy in the EU.
| Characteristic | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Region Eastern Europe | — | — | — |
| Southern Europe | 0.45 [0.41, 0.49]*** | 0.44 [0.39, 0.49]*** | 0.61 [0.54, 0.68]*** |
| Western Europe | 0.45 [0.42, 0.48]*** | 0.43 [0.39, 0.46]*** | 0.45 [0.41, 0.50]*** |
| Trust.EU.info | 0.47 [0.43, 0.51]*** | 0.37 [0.33, 0.42]*** | 0.46 [0.41, 0.52]*** |
| Trust.gov.info | 0.58 [0.52, 0.64]*** | 0.52 [0.45, 0.60]*** | 0.63 [0.54, 0.72]*** |
| Trust.health.info | 0.34 [0.32, 0.37]*** | 0.34 [0.31, 0.37]*** | 0.46 [0.42, 0.50]*** |
| Trust.local.info | 0.73 [0.64, 0.82]*** | 0.64 [0.55, 0.76]*** | 0.67 [0.56, 0.80]*** |
| Trust.doctors.info | 0.42 [0.40, 0.45]*** | 0.44 [0.41, 0.47]*** | 0.63 [0.58, 0.69]*** |
| Trust.media.info | 0.74 [0.66, 0.83]*** | 0.72 [0.62, 0.83]*** | 0.85 [0.73, 0.99]* |
| Trust.web.info | 1.32 [1.18, 1.48]*** | 1.35 [1.18, 1.55]*** | 1.26 [1.09, 1.46]** |
| Trust.networks.info | 1.56 [1.37, 1.78]*** | 1.65 [1.40, 1.93]*** | 1.52 [1.28, 1.81]*** |
| Trust.people.info | 1.20 [1.11, 1.31]*** | 1.10 [0.99, 1.21] | 1.08 [0.96, 1.20] |
| Age [years] | 0.97 [0.97, 0.97]*** | 0.97 [0.97, 0.98]*** | |
| Education [years] | 0.99 [0.98, 1.00]* | 1.00 [0.99, 1.01] | |
| Sex [male] | 0.78 [0.73, 0.84]*** | 0.76 [0.70, 0.82]*** | |
| Residence [city] | 0.89 [0.83, 0.96]** | 0.93 [0.85, 1.01] | |
| Occupation Employee | — | — | |
| Manual worker | 1.77 [1.53, 2.05]*** | 1.63 [1.38, 1.92]*** | |
| No activity | 1.36 [1.24, 1.50]*** | 1.31 [1.18, 1.46]*** | |
| Self-employed | 1.31 [1.17, 1.47]*** | 1.26 [1.11, 1.43]*** | |
| Vaccines are safe | 0.34 [0.31, 0.38]*** | ||
| Vaccines are effective | 0.37 [0.33, 0.42]*** | ||
| Knows ill from COVID-19 | 0.79 [0.72, 0.87]*** | ||
| Was ill from COVID-19 | 1.23 [1.08, 1.39]** | ||
| Fears infection from COVID-19 | 0.38 [0.35, 0.42]*** | ||
| Number of observations | 26,106 | 19,944 | 19,944 |
| McFadden's Pseudo R-squared | 0.16 | 0.20 | 0.31 |
p < 0.05.
p < 0.01.
p < 0.001.
The models reported in Table 1 are estimated on the combined sample of respondents from all countries and regions in the EU (region fixed effects are included). In the next section we will explore how the effects differ per region using interaction effects. Table 1 shows the exponentiated logistic regression coefficients (odds ratios), so that values lower than 1 imply lower odds and probability of being vaccine hesitant and values higher than 1 imply higher odds and probability. For example, the ratio of the odds of being vaccine hesitant for males vs. females is 0.78 (Model 2 in Table 1), so the odds for males are about 22% lower that the odds for females.
All the trust-related variables have significant effects on vaccine hesitancy, with trust in health authorities, the EU, and the medical profession having the biggest negative ones, and trust in Internet information, online social networks and ‘people around’ having positive effects (increasing the odds that someone is vaccine hesitant). Interestingly, the effect of trust in ‘people around’ (as a reliable source of vaccine information) is greatly reduced in size when we add the demographic predictors and turns insignificant when we add the COVID-19 vaccine beliefs. This implies that age and education confound the positive effect of trust in ‘people around’ on vaccine hesitancy and that, net of beliefs in the safety and efficacy of vaccines, the effect is undistinguishable from zero.
In the presence of the demographic variables, the other information-based predictors do not diminish in importance, and some actually increase in size (e.g., trust in the EU). However, net of beliefs about vaccines and personal exposure to COVID-19, the effects of trust in doctors and in the media are halved in size. From the demographic variables, the effects of age in the full sample is estimated to be negative (but see the previous section for the complex possibly non-linear nature of the effect, which is not captured in these models). The effect of education is negative only in the absence of the COVID-19 beliefs and experiences. Males and city-dwellers are significantly less likely to be vaccine hesitant and the effects are stable. Compared to employees, manual workers, respondents with no economic activities and the self-employed are significantly more likely to be vaccine hesitant as well.
Unsurprisingly, beliefs in the safety and efficacy of vaccines have large and significant negative associations with vaccine hesitancy, as does the fear of getting infected. The negative effect of knowing someone who has been ill from the disease is significant but smaller in size. Having been sick with COVID-19 is positively associated with being hesitant to get a vaccine, perhaps on the belief that the experience grants immunity. In the Supplementary material we present the same set of models estimated on vaccine refusal as the outcome variable, but altogether the results are very similar (Table S2).
4.4. Varying effects in the different regions of Europe
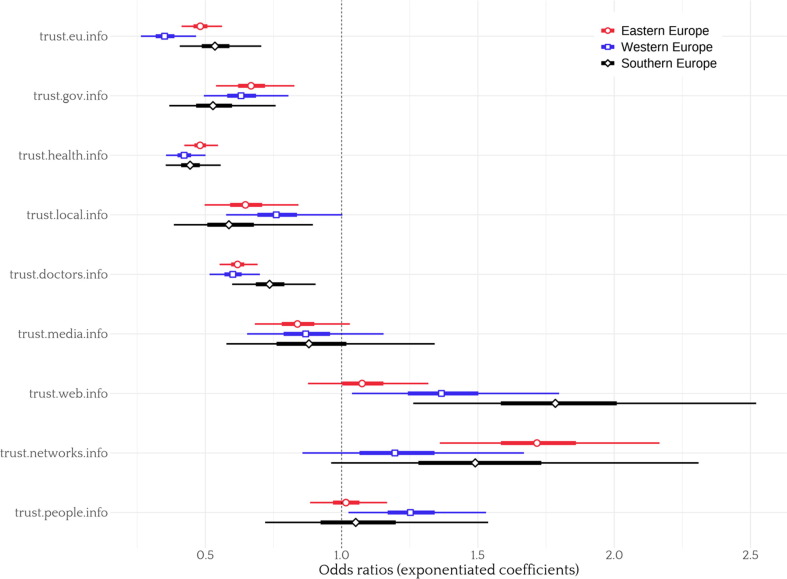
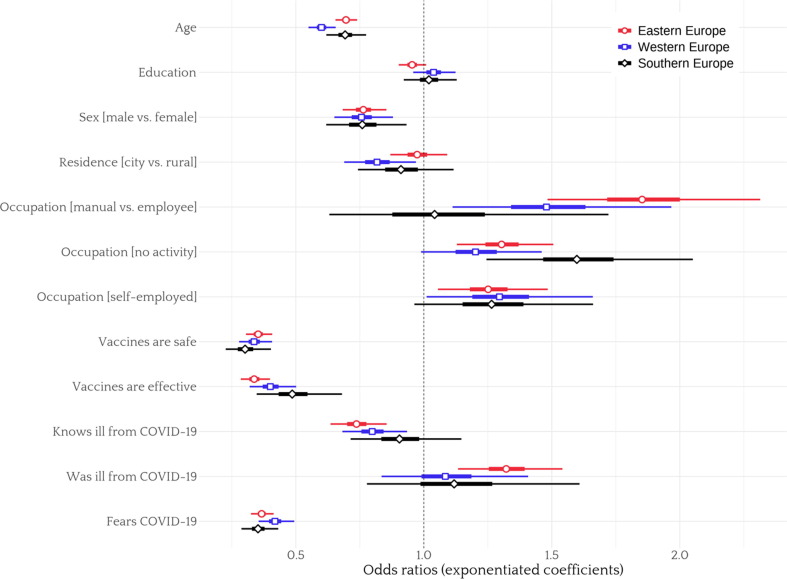
Next, we explore how the effects discussed above differ in Eastern, Western and Southern Europe. We report a version of Model 3 with interactions of all variables with region in the Supplementary material (Table S4), and we illustrate the effects in Fig. 6, Fig. 7 , which plot the estimated coefficients and 95% confidence intervals per region. Looking first at trust in different information sources, the effect of trust in the EU is significantly smaller in Western Europe than in Eastern Europe. The effect of trust in the Internet is significantly higher in Southern Europe. The effect of trust in online social networks is smaller and the effect of trust in people is bigger in Western Europe than in the East. The effects of some demographic predictors also differ per region. The effects of age and city are smaller in Western Europe, while the effect of education is bigger. The effect of being in the ‘manual workers’ category is much smaller, while the effect of belief in vaccine effectiveness is significantly bigger. Despite the presence of significant interactions, however, overall the variance explained by the models does not increase very much. That is, the interactions add little to the explanatory power of the models. This implies that differential effects of the variables included in the regressions are not responsible to a great extent for the observed differences in vaccine hesitancy in Eastern, Southern and Western Europe. The results are very similar with respect to vaccine refusal (also reported in Table S4, Model A8).
Fig. 6.
Odds ratios (exponentiated coefficients) of trust in different ‘sources of reliable information about COVID-19 vaccines’ on vaccine hesitancy in three regions of the Europe (Eastern in red, Western in blue, Southern in black, with 50% and 95% confidence intervals. Models estimated separately for each region. For statistical tests of the cross-region differences, see Model A1 in Table S4 in the Supplementary material. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 7.
Odds ratios (exponentiated coefficients) of demographic variables and COVID-19-related beliefs and experiences on vaccine hesitancy in three regions of the Europe (Eastern in red, Western in blue, Southern in black, with 50% and 95% confidence intervals. Models estimated separately for each region. For statistical tests of the cross-region differences, see Model A1 in Table S4 in the Supplementary material. Age and Education have been mean-centered and scaled by 1 s.d. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
To probe whether the causal nature of the effects of age and education, we conduct mediation analyses, reported in the Supplementary material. In short, the analyses find that age has a larger direct negative effect and smaller indirect effects exercised via vaccine beliefs and via trust in the Internet. The total effect of education is also estimated to be negative and is mostly exercised directly (Figure S3). These structures are similar in Western and Eastern Europe, but the model for Southern Europe has all direct and indirect effects of education as insignificant.
5. Conclusion
This article used comparative data from 27 European countries to examine the individual-level predictors of COVID-19 vaccine hesitancy and refusal at an important point in time – May 2021 – when mass vaccination campaigns were in their early stages. In line with existing literature, the analyses showed that several demographic factors have significant associations with vaccine hesitancy and refusal. Age exhibited negative effects, but ones that are possibly non-linear. The effect of education is also negative and non-linear, but smaller and heterogenous across European regions. Males, city dwellers and employees were consistently less likely to be vaccine hesitant. The mediation analyses also found that the effects of age is both and indirect, via trust in different sources of information on COVID-19 vaccines and via beliefs in the safety of vaccines.
The article reported strong evidence that the types of information sources that people trust has substantively big and statistically significant associations with vaccine hesitancy and refusal. People who tend to trust EU, national and local governments, as well as people who trust medical professionals and health authorities are much less likely to be vaccine hesitant, while people how tend to trust the Internet, online social networks and ‘people around’ show the opposite tendency. These inferences are consistent with existing literature about trust and the influence of non-traditional media sources on health-related beliefs and behaviors. But it still remains unclear to what extent the effects of trust are causal in a strict sense rather than being confounded by more general socio-political orientations (e.g. trust in government as such) and patterns of media consumption. The mediation analyses reported in this article suggest that trust in the Internet as a source of information on COVID-19 vaccines has both a direct effect, as well as an indirect effect via belief in the safety of vaccines.
Beliefs in the safety and effectiveness of vaccines had significant predictive power for vaccine hesitancy, but for these variables concerns about endogeneity loom even larger when we consider whether they have causal effects as such. Beliefs about and personal exposure to COVID-19 had significant predictive power as well, with people fearing infection and knowing people who have been sick from the diseases less likely to report vaccine hesitancy and refusal. But people who had had the disease themselves were more likely to be vaccine hesitant (but not refuse vaccines altogether).
A major motivation of this study was to shed light on the reasons why vaccines hesitancy and refusal were much higher in Eastern compared to Southern and Western Europe. The analyses showed some evidence for differential effects of the demographic and trust-related variables. For example, the effect of education is non-existent in Southern Europe and the effect of age is flatter until middle age in Eastern Europe. But, altogether, it is differences in levels of the variables across regions that can account for the differences in vaccine hesitancy and refusal than differential effects of these variables. The reasons endorsed for or against vaccination also do not show major differences across European regions (see Figures A1 and A2 in the Supplementary material). Therefore, we have to conclude that the structures explaining vaccine hesitancy do not seem to differ much across regions. Rather, it is the much higher prevalence of variables such as distrust of national governments and medical processionals as sources of relevant information in Eastern Europe that are relevant.
Some of the practical implications of this work echo recommendations from the existing literature. The importance of trust in different media sources and beliefs about the safety and efficacy of the vaccines calls both for public information campaigns that explain how vaccines work and are developed, as well as for more general measures clarifying why certain sources of vaccine and medical information are most trustworthy than others [12], [38], [50]. But the significant heterogeneity in relevant attitudes and beliefs across Europe means that interventions need to take into account the local context [cf. 15].
The results of this article imply that some countries and regions in Europe – in particular in Eastern Europe - have more work to do in order to increase the vaccine acceptance of their populations and prepare their governance systems for the management of future pandemics. This work needs to include increasing trust in medical doctors, health professionals, local and central governments and improving the quality of medical information on the internet and social media.
It is important to highlight that this study focused on a period (May 2021) soon after the development of COVID-19 vaccines and near the start of mass vaccination campaigns. As more time passed, these campaigns managed to reach more people and overcome some of the vaccine hesitancy and refusal. But this early period has been very important for the containment of the pandemic and limiting its toll. Focusing on this crucial period delivers insights for the management of future pandemics, in periods when uncertainty about the effectiveness and dangers of new vaccines is still high.
To be on firmer ground when endorsing recommendations about addressing vaccine hesitancy, future research should probe further the causal nature of the associations explored in this article. The observational nature of the evidence presented here precludes strong causal claims, even if the multivariate regressions and the mediation analyses in particular addressed some concerns about confounders and causal ordering. Another important limitation of this research is that the 27 European states were grouped in three clusters, defined on the basis of shared historical legacies (communist rule in particular) and broad socio-political similarities. Different ways to address the heterogeneity of vaccine-related attitudes across countries are possible, including defining different clusters (for example, separating Northern and South-Eastern countries from Western and Eastern Europe, respectively). Finally, future research should strive to link the variables studied in this article to more general social and political attitudes, which – despite the theoretical importance – was not possible to be done in this study due to the limitations of the public opinion survey used as a data source. A more comprehensive understanding of vaccine hesitancy needs to consider the broader socio-political environment in which European citizens process relevant information and form attitudes and beliefs.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
The observational nature of the data used in this study is not well-suited for making strong claims about the identification of causal ‘effects’ in the strict sense. In this article, I use ‘effect’ as a reference to the residual correlation of a variable with the outcome of interest, net of the other variables included in the statistical model. These partial regression coefficients may be given causal interpretation only under strong assumptions.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2023.03.030.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
The data is already publicly available. Analysis code is available at: https://github.com/demetriodor/vaccination-attitudes-in-europe.
References
- 1.Cadeddu C., Rosano A., Villani L., Coiante G.B., Minicucci I., Pascucci D., et al. Planning and Organization of the COVID-19 Vaccination Campaign: An Overview of Eight European Countries. Vaccines. 2022:10. doi: 10.3390/vaccines10101631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.MacDonald N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 3.Yaqub O., Castle-Clarke S., Sevdalis N., Chataway J. Attitudes to vaccination: A critical review. Soc Sci Med. 2014;112:1–11. doi: 10.1016/j.socscimed.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 4.Stoeckel F., Carter C., Lyons B.A., Reifler J. The politics of vaccine hesitancy in Europe. Eur J Public Health. 2022;32:636–642. doi: 10.1093/eurpub/ckac041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anakpo G., Mishi S. Hesitancy of COVID-19 vaccines: Rapid systematic review of the measurement, predictors, and preventive strategies. Hum Vaccin Immunother. 2022;18:2074716. doi: 10.1080/21645515.2022.2074716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pires C. Global Predictors of COVID-19 Vaccine Hesitancy: A Systematic Review. Vaccines. 2022:10. doi: 10.3390/vaccines10081349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siani A., Tranter A. Is vaccine confidence an unexpected victim of the COVID-19 pandemic? Vaccine. 2022;40:7262–7269. doi: 10.1016/j.vaccine.2022.10.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stoeckel F., Carter C., Lyons B.A., Reifler J. Association of vaccine hesitancy and immunization coverage rates in the European Union. Vaccine. 2021;39:3935–3939. doi: 10.1016/j.vaccine.2021.05.062. [DOI] [PubMed] [Google Scholar]
- 9.Barberia L., Plümper T., Whitten G.D. The political science of Covid-19: An introduction. Soc Sci Q. 2021;102:2045–2054. doi: 10.1111/ssqu.13069. [DOI] [Google Scholar]
- 10.Lindholt M.F., Jørgensen F., Bor A., Petersen M.B. Public acceptance of COVID-19 vaccines: cross-national evidence on levels and individual-level predictors using observational data. BMJ Open. 2021;11:e048172. doi: 10.1136/bmjopen-2020-048172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sallam M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines. 2021:9. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Obregon R., Mosquera M., Tomsa S., Chitnis K. Vaccine Hesitancy and Demand for Immunization in Eastern Europe and Central Asia: Implications for the Region and Beyond. J Health Commun. 2020;25:808–815. doi: 10.1080/10810730.2021.1879366. [DOI] [PubMed] [Google Scholar]
- 13.Neumann-Böhme S., Varghese N.E., Sabat I., Barros P.P., Brouwer W., van Exel J., et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Heal Econ. 2020;21:977–982. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Callaghan T., Moghtaderi A., Lueck J.A., Hotez P., Strych U., Dor A., et al. Correlates and disparities of intention to vaccinate against COVID-19. Soc Sci Med. 2021;272 doi: 10.1016/j.socscimed.2020.113638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salomoni M.G., Di Valerio Z., Gabrielli E., Montalti M., Tedesco D., Guaraldi F., et al. Hesitant or Not Hesitant? A Systematic Review on Global COVID-19 Vaccine Acceptance in Different Populations. Vaccines. 2021:9. doi: 10.3390/vaccines9080873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lewis A., Duch R. Gender differences in perceived risk of COVID-19. Soc Sci Q. 2021;102:2124–2133. doi: 10.1111/ssqu.13079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bergmann M, Hannemann T, Bethmann A, Schumacher AT. Determinants of SARS-CoV-2 Vaccinations in the 50+ Population 2021.
- 18.Lazarus J.V., Wyka K., Rauh L., Rabin K., Ratzan S., Gostin L.O., et al. Hesitant or Not? The Association of Age, Gender, and Education with Potential Acceptance of a COVID-19 Vaccine: A Country-level Analysis. J Health Commun. 2020;25:799–807. doi: 10.1080/10810730.2020.1868630. [DOI] [PubMed] [Google Scholar]
- 19.Khemlani S., Bello P., Briggs G., Harner H. The Mental Representation of Omissive Relations. Front Psychol; Much Ado About Nothing: 2021. Wasylyshyn C; p. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Paul E., Steptoe A., Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. Lancet Reg Heal - Eur. 2021:1. doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stroope S., Kroeger R.A., Williams C.E., Baker J.O. Sociodemographic correlates of vaccine hesitancy in the United States and the mediating role of beliefs about governmental conspiracies. Soc Sci Q. 2021;102:2472–2481. doi: 10.1111/ssqu.13081. [DOI] [Google Scholar]
- 22.Sylvester S.M. COVID-19 and Motivated Reasoning: The Influence of Knowledge on COVID-Related Policy and Health Behavior. Soc Sci Q. 2021;102:2341–2359. doi: 10.1111/ssqu.12989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fournet N., Mollema L., Ruijs W.L., Harmsen I.A., Keck F., Durand J.Y., et al. Under-vaccinated groups in Europe and their beliefs, attitudes and reasons for non-vaccination; two systematic reviews. BMC Public Health. 2018;18:196. doi: 10.1186/s12889-018-5103-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ten Kate J., De K.W., Van der Waal J. “Following Your Gut” or “Questioning the Scientific Evidence”: Understanding Vaccine Skepticism among More-Educated Dutch Parents. J Health Soc Behav. 2021;62:85–99. doi: 10.1177/0022146520986118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Becher M., Stegmueller D., Brouard S., Kerrouche E. Ideology and compliance with health guidelines during the COVID-19 pandemic: A comparative perspective. Soc Sci Q. 2021;102:2106–2123. doi: 10.1111/ssqu.13035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trent M., Seale H., Chughtai A.A., Salmon D., MacIntyre C.R. Trust in government, intention to vaccinate and COVID-19 vaccine hesitancy: A comparative survey of five large cities in the United States, United Kingdom, and Australia. Vaccine. 2022;40:2498–2505. doi: 10.1016/j.vaccine.2021.06.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anastasiou O.E., Heger D. Understanding the Influence of Individual and Systemic Factors on Vaccination Take-Up in European Citizens Aged 55 or Older. Vaccines. 2021:9. doi: 10.3390/vaccines9020169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alvarez-Galvez J., Salinas-Perez J.A., Montagni I., Salvador-Carulla L. The persistence of digital divides in the use of health information: a comparative study in 28 European countries. Int J Public Health. 2020;65:325–333. doi: 10.1007/s00038-020-01363-w. [DOI] [PubMed] [Google Scholar]
- 29.Wawrzuta D., Jaworski M., Gotlib J., Panczyk M. Social Media Sharing of Articles About Measles in a European Context: Text Analysis Study. J Med Internet Res. 2021;23:e30150. doi: 10.2196/30150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilson S.L., Wiysonge C. Social media and vaccine hesitancy. BMJ Glob Heal. 2020;5:e004206. doi: 10.1136/bmjgh-2020-004206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lunz Trujillo K., Motta M. How Internet Access Drives Global Vaccine Skepticism. Int J Public Opin Res. 2021;33:551–570. doi: 10.1093/ijpor/edab012. [DOI] [Google Scholar]
- 32.Leiter D., Reilly J., Vonnahme B. The crowding of social distancing: How social context and interpersonal connections affect individual responses to the coronavirus*. Soc Sci Q. 2021;102:2435–2451. doi: 10.1111/ssqu.13060. [DOI] [Google Scholar]
- 33.Romer D., Jamieson K.H. Conspiratorial thinking, selective exposure to conservative media, and response to COVID-19 in the US. Soc Sci Med. 2021;291 doi: 10.1016/j.socscimed.2021.114480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ward J.K., Alleaume C., Peretti-Watel P., Peretti-Watel P., Seror V., Cortaredona S., et al. The French public’s attitudes to a future COVID-19 vaccine: The politicization of a public health issue. Soc Sci Med. 2020;265 doi: 10.1016/j.socscimed.2020.113414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Piltch-Loeb R., Silver D.R., Kim Y., Norris H., McNeill E., Abramson D.M. Determinants of the COVID-19 vaccine hesitancy spectrum. PLoS One. 2022;17:e0267734. doi: 10.1371/journal.pone.0267734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heyerdahl L.W., Vray M., Lana B., Tvardik N., Gobat N., Wanat M., et al. Conditionality of COVID-19 vaccine acceptance in European countries. Vaccine. 2022;40:1191–1197. doi: 10.1016/j.vaccine.2022.01.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stoeckel F., Stöckli S., Phillips J., Lyons B., Mérola V., Barnfield M., et al. Stamping the vaccine passport? Public support for lifting COVID-19 related restrictions for vaccinated citizens in France, Germany, and Sweden. Vaccine. 2022;40:5615–5620. doi: 10.1016/j.vaccine.2022.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marco-Franco J.E., Pita-Barros P., Vivas-Orts D., González-de-Julián S., Vivas-Consuelo D. COVID-19, Fake News, and Vaccines: Should Regulation Be Implemented? Int J Environ Res Public Heal. 2021;18. doi: 10.3390/ijerph18020744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Capurro G., Maier R., Tustin J., Jardine C.G., Michelle D.S. “They’re trying to bribe you and taking away your freedoms”: COVID-19 vaccine hesitancy in communities with traditionally low vaccination rates. Vaccine. 2022;40:7280–7287. doi: 10.1016/j.vaccine.2022.10.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sturgis P., Brunton-Smith I., Jackson J. Trust in science, social consensus and vaccine confidence. Nat Hum Behav. 2021;5:1528–1534. doi: 10.1038/s41562-021-01115-7. [DOI] [PubMed] [Google Scholar]
- 41.Costa-Font J., Garcia-Hombrados J., Nicińska A. The Institutional Origins of Vaccines Distrust. Evidence from Former-Communist Countries. 2021 doi: 10.1371/journal.pone.0282420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Petravić L., Arh R., Gabrovec T., Jazbec L., Rupčić N., Starešinič N., et al. Factors Affecting Attitudes towards COVID-19 Vaccination: An Online Survey in Slovenia. Vaccines. 2021;9. doi: 10.3390/vaccines9030247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sowa P., Kiszkiel Ł., Laskowski P.P., Alimowski M., Szczerbiński Ł., Paniczko M., et al. COVID-19 Vaccine Hesitancy in Poland—Multifactorial Impact Trajectories. Vaccines. 2021;9. doi: 10.3390/vaccines9080876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Żuk P., Żuk P., Lisiewicz-Jakubaszko J. The anti-vaccine movement in Poland: The socio-cultural conditions of the opposition to vaccination and threats to public health. Vaccine. 2019;37:1491–1494. doi: 10.1016/j.vaccine.2019.01.073. [DOI] [PubMed] [Google Scholar]
- 45.Waszak P.M., Kasprzycka-Waszak W., Kubanek A. The spread of medical fake news in social media - The pilot quantitative study. Heal Policy Technol. 2018;7:115–118. doi: 10.1016/j.hlpt.2018.03.002. [DOI] [Google Scholar]
- 46.Pronkina E., Berniell I., Fawaz Y., Laferrère A., Mira P. The COVID-19 curtain: Can past communist regimes explain the vaccination divide in Europe? Soc Sci Med. 2023;321 doi: 10.1016/j.socscimed.2023.115759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dubé E., Laberge C., Guay M., Bramadat P., Roy R., Bettinger J.A. Vaccine hesitancy Hum Vaccin Immunother. 2013;9:1763–1773. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bussink-Voorend D., Hautvast J.L.A., Vandeberg L., Visser O., Hulscher M.E.J.L. A systematic literature review to clarify the concept of vaccine hesitancy. Nat Hum Behav. 2022;6:1634–1648. doi: 10.1038/s41562-022-01431-6. [DOI] [PubMed] [Google Scholar]
- 49.Wood S.N. CRC Press; 2017. Generalized additive models: an introduction with R. [Google Scholar]
- 50.Paladini A., Regazzi L., Castagna C., Sapienza M., Rosano A., Ricciardi W., et al. Public opinion on vaccines: the role of the scientific community in Italy. Eur J Public Health. 2021;31:ckab165.469. doi: 10.1093/eurpub/ckab165.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data is already publicly available. Analysis code is available at: https://github.com/demetriodor/vaccination-attitudes-in-europe.