Chronic myeloid leukemia (CML) is a clonal myeloproliferative disorder, arising from a hematopoietic stem cell (HSC) that acquires the chromosomal translocation t(9;22), resulting in the BCR-ABL oncoprotein. While BCR-ABL-targeting tyrosine kinase inhibitors (TKI) eliminate the majority of CML cells, the most primitive disease-initiating leukemic stem cells (LSC) are frequently spared. CML development is accompanied by increasing levels of inflammatory cytokines, such as IL-1α, IL-1β, IL-6, or TNF. Correspondingly, LSC are characterized by a TKI-persisting, inflammatory cytokine response pattern that was observed even during prolonged therapy.1 Our preliminary work confirmed that TNF signaling is active in murine CML stem cells and TNF-targeted antibody treatment enhanced therapeutic efficiency of TKI treatment.2 Moreover IKK-dependent activation of NF-kB has been shown to contribute to BCR-ABL-induced myeloid and lymphoid leukemogenesis.3,4 In CML stem and progenitor cells, an autocrine TNF loop and NF-kB signaling were found to persist during TKI treatment in vitro.5 NF-kB serves as a central inflammatory hub as several cytokines induce IKK-dependent phosphorylation at serine 32/36 and subsequent degradation of IkBα, which releases the NF-kB complex, allowing its activation by phosphorylation at serine 536 and transport to the nucleus.6 Thereby, NF-kB induces transcription of target genes such as several cytokines or the NF-kB signaling molecules themselves.7 Here we confirmed TKI-persistent TNF-induced NF-kB signaling in CML mice and human cells. As TNF can induce pro-proliferative signaling via NF-kB but also pro-apoptotic cascades via RIPK1-induced CASP8 activation, we here aimed to specifically inhibit the pro-proliferative activity by targeting IKK2. Therefore, we performed pharmacologic IKK2 inhibition, using the small molecule IKK2 inhibitor LY2409881 (LY), previously shown to be well tolerable in pre-clinical application.8 Combined BCR-ABL/IKK2-targeting blocked malignant NF-kB signaling and enhanced apoptosis in TKI-sensitive but also TKI-resistant cells. In vivo, NF-kB-mediated TNF activity was elevated despite nilotinib (NIL) treatment. IKK2 targeting severely reduced LSC, which was further reflected by preventing disease onset upon secondary transplantation. As TNF-induced NF-kB-signaling was evident in chronicphase (CP) but likewise blast crisis (BC) CML, IKK2 targeting affected the clonogenic potential in both disease stages. Finally, in CP CML CD34+ cells, combined BCR-ABL/IKK2 inhibition significantly induced apoptosis, also in quiescent LSC showing that this approach enables the eradication of the TKI-persisting malignant stem cell population in CML.
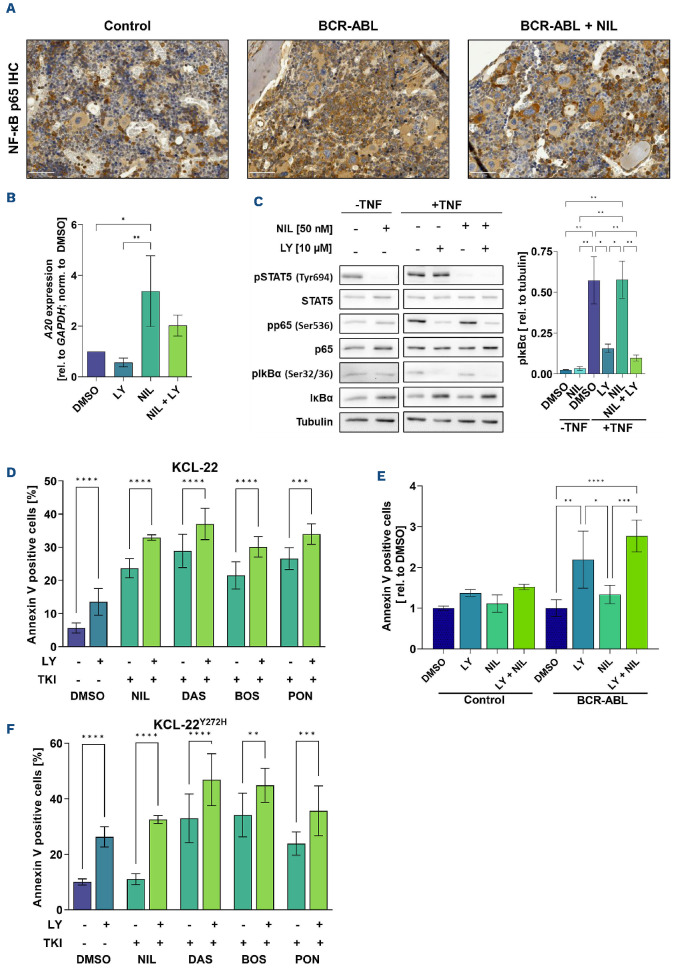
Aiming to get insight into the role of malignant TNF signaling in CML, we started to compare BCR-ABL-positive with ABL-negative cell lines. We observed significant up-regulation of TNF signaling in 32D BCR-ABL versus empty vector control cells, as represented by increased expression of relevant TNF targets in BCR-ABL positive cells (IkBα, fold change (fc): 1.9; Nf-kb, fc: 2.2, A20, fc: 6.5; Online Supplementary Figure S1A). In order to mimic the malignant inflammatory niche, TNF was subsequently added to both cell types at a physiological concentration and this still resulted in increased TNF target gene expression in BCR-ABL versus control cells (IkBα, fc: 1.7; Nf-kb, fc: 3, A20, fc: 3.4). Notably, this upregulation of TNF signaling persisted in the presence of NIL (Online Supplementary Figure S1A). TKI-persistent NF-kB activation was likewise evident in vivo, as shown by bone marrow (BM) immunoh-istochemical p65 staining of Scl-tTa-BCR-ABL or Scl-tTa control mice (Figure 1A). Although NIL slightly reduced p65 protein expression, reversion to healthy control levels was not achieved.
Next, we studied the effects induced by pharmacologic inhibition of the IkB-kinase-subunit, IKK2 using LY. The small molecule inhibitor prevents IKK2 phosphorylation and subsequent degradation of IkBα, which thus remains bound to the NF-kB complex to block its phosphorylation. This prevents nuclear translocation of NF-kB and thereby expression of target genes. Analysis of A20 expression in human KCL22 CML cells suggested a NIL-induced upregulation (Figure 1B; fc: 3.37), that was reduced by LY treatment (A20, fc: 2.02). We observed similar effects when adding imatinib (IM) or dasatinib (DAS) (Online Supplementary Figure S1B). We studied signaling activity via western blot analyses in KCL-22 cells (Figure 1C). As expected, phosphorylation of NF-kB subunit p65 was not reduced by NIL treatment alone. Moreover, pIkBα at serine 32/36 was significantly inhibited by LY single treatment (fc: 0.27) and this was still achieved in the presence of NIL (fc: 0.17), as shown by significant downregulation as compared to the corresponding DMSO control or NIL single treatment, in the presence of TNF. This further resulted in reduced phosphorylation of p65 at serine 536 in the presence of LY (fc: 0.42) or both drugs (fc: 0.29), as compared to the corresponding DMSO control.
Annexin V staining of treated KCL-22 cells showed the advantage of IkB kinase inhibition as this induced a significant increase in apoptosis by IKK2 inhibition alone (fc: 2.4) that further enhanced NIL-induced cell death by 1.4-fold (Figure 1D). The therapeutic effect of IKK2 inhibition was also evaluated in the context of other clinically relevant TKI. For all TKI tested, we observed increased apoptosis levels upon combined treatment (DAS fc: 1.3, BOS fc: 1.4, PON fc: 1.3) (Figure 1D). We next treated isolated lin- BM cells from Scl-tTa-BCR-ABL or Scl-tTa control mice (Figure 1E), showing that control cells remained largely unaffected whereas apoptosis was induced upon LY monotherapy (fc: 2.2) in murine primary CML cells. Moreover, combined LY and NIL treatment enhanced NIL-induced apoptosis by 2.1-fold.
Figure 1.
Targeting tyrosine kinase inhibitor-persistent TNF-signaling by pharmacological IKK2 inhibition. (A) Elevated and tyrosine kinase inhibitor (TKI)-persisting NF-kB activation in chronic myeloid leukemia (CML) mice is shown by a representative immunohistochemical bone marrow (BM) staining of NF-kB p65 (brown) and hematoxylin (blue) in BM sections from mice, which were either transplanted with Scl-tTa-BCR-ABL or Scl-tTa control BM and subsequently treated using nilotinib (NIL) or vehicle control for 3 weeks. White scale bar represents 50 mm. (B) CML KCL-22 cells were treated using Ly2409881 (LY) (10 mM), NIL (50 nM), or LY + NIL, in the presence of 1 ng/mL TNF for 16 hours (h). Expression of A20 was analyzed via quantitative real time polymerase chain reaction (qRT-PCR) and is expressed as % of GAPDH. Shown are mean values of n=3, normalized to DMSO control. (C) Western blot analysis of KCL-22 cells using the indicated antibodies, pretreated with 1 ng/mL TNF for 1 h and subsequently treated using NIL (50 nM) and/or LY (5 mM) for again 1 h. Shown is 1 representative result of n=3 (left panel). Phosphorylation was quantified using densitometry (n=3, right panel). Shown are means ± standard error of the mean. (D) Flow cytometry analysis of Annexin V-positive KCL-22 cells in the presence of 1 ng/mL TNF after 48 h of treatment using LY (5 mM), NIL (50 nM), LY + NIL, dasatinib (DAS) (10 nM), LY + DAS, bosutinib (BOS) (5 nM), LY + BOS, ponatinib (PON) (5 nM), LY + PON. (E) Annexin V flow cytometry analysis of BM lin- MACS-isolated cells from Scl-tTa or Scl-tTa-BCR-ABL mice that were induced to express BCR-ABL for 10 days prior to BM-isolation. In vitro treatment was performed using LY (10 mM), NIL (50 nM), LY + NIL or DMSO control in the presence of 1 ng/mL TNF for 16 h (n=3). (F) Flow cytometry analysis of Annexin V-positive KCL-22Y272H cells after 48 h of treatment using LY (5 mM), NIL (50 nM), LY + NIL, DAS (10 nM), LY + DAS, BOS (5 nM), LY + BOS, PON (5 nM), LY + PON in the presence of TNF (1 ng/mL; n=3). Significance was calculated using one or two-way ANOVA; Mean ± standard deviation; *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001.
In order to study the role of TNF signaling in BCR-ABL ki-nase-mutated TKI resistance, we utilized the KCL-22Y272H9 and KCL-22T315I-cell lines.10 In KCL-22Y272H cells, LY therapy induced apoptosis, while NIL alone had no effect (Figure 1F). As DAS, bosutinib (BOS), and ponatinib (PON) could bypass the P-loop mutation, these TKI indeed induced KCL-22Y272H cell death that was further elevated with IKK2 inhibition, as reflected by a further rise in Annexin V positivity (DAS fc: 1.4, BOS fc: 1.3, PON fc: 1.5). In KCL-22T315I cells, effects were very modest with LY application only slightly inducing apoptosis and this was unaffected by TKI treatment (Online Supplementary Figure S1C).
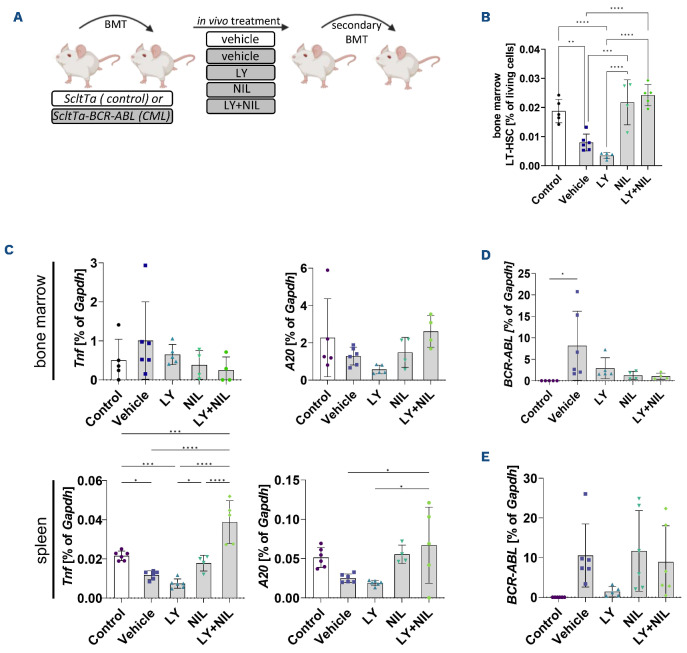
In order to investigate whether IKK2 targeting could affect TKI-persistent LSC, we implemented the Scl-tTa-BCR-ABL mouse model (Figure 2A). As expected, splenomegaly and white blood cell count were normalized by NIL treatment (Online Supplementary Figure S2A, B). Comprehensive immunophenotyping revealed a predominant expansion of malignant B cells (B220low) that responded to BCR-ABL inhibition (Online Supplementary Figure S2C, D). Moreover, we confirmed our previous findings on reduced BM-derived long-term (LT)-HSC (Lin-, Sca1+, c-kit+, CD48low, CD150+) upon disease development (Figure 2B).11 In line with the concept that TKI treatment selects for primitive LSC, we observed increased LT-HSC in NIL- or NIL/LY-treated mice. Interestingly, LY monotherapy decreased LT-HSC by 2.3-fold. While Tnf expression was decreased upon treatment in BM, NIL monotherapy, as well as combined NIL/LY therapy apparently increased Tnf transcript levels in the spleen (Figure 2C). As TNF acts both, autocrine and paracrine, this likely resulted in elevated A20 expression in both organs (Figure 2C). In light of this, A20 is not only described to be increased in response to TNF, but also known to protect cells from TNF–induced apoptosis.12 Treatment efficacy was further shown by a reduction of BCR-ABL expression, with the strongest reduction upon combined BCR-ABL- and IKK2 inhibtion (Figure 2D). We assessed the malignant stem cell potential via serial transplantation of BM cells into irradiated wild-type recipients (Figure 2A). In line with our finding that BM-derived LT-HSC are spared by TKI or TKI + LY treatment, secondary recipients showed disease recurrence, accompanied by slightly increased spleen weights (Online Supplementary Figure S2E), as well as elevated BCR-ABL transcript levels (Figure 2E). Interestingly, LY monotherapy prevented spleen expansion and severely impaired re-expansion of malignant cells as shown by only residual BCR-ABL transcript levels, in secondary recipients.
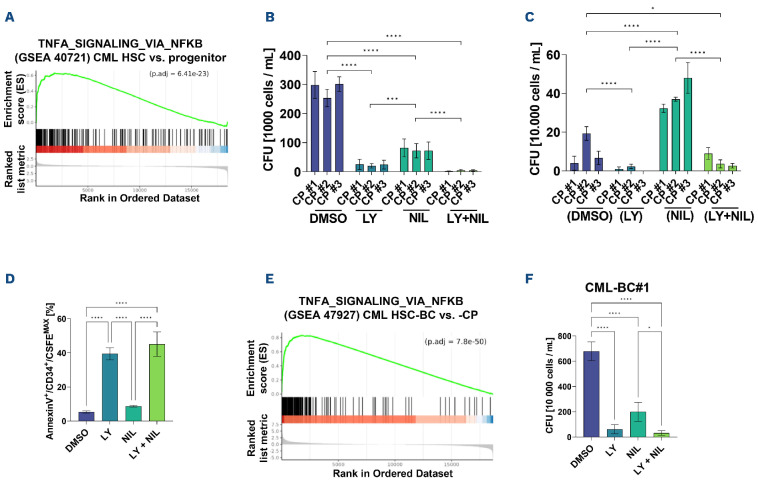
In order to determine whether TNF-signaling is specifically active in LSC, we re-analyzed microarray data (GSE40721) revealing upregulation of TNF signaling via NF-kB in CD34+CD38- stem cells versus CD34+CD38+ progenitor cells (Figure 3A). We proceeded to evaluate the clonogenic potential in CML CD34+ cells upon treatment and this was strongly reduced by both single treatments, as compared to DMSO control (LY: 12.1-fold, NIL: 3.8-fold) and almost completely abrogated upon combined IKK2 and BCR-ABL targeting (77.5-fold; Figure 3B). In order to assess the effect on most primitive cells, replating was performed without any further treatment and this showed that previous NIL treatment had spared malignant stem cells while LY-treated cells were severely impaired in the ability to form colonies (Figure 3C), suggesting that LY monotherapy targets the most primitive malignant stem cells. In healthy donor-derived CD34+ cells, IKK2 inhibition showed an effect in two of six samples (Online Supplementary Figure S3A). As these cells were partially provided by osteoarthritis patients, we assume that IKK2 inhibition could affect these samples, as pro-inflammatory cytokines could be likewise involved.13 In order to dissect if IKK2 targeting induces apoptosis in the most primitive CML cells we performed Annexin V staining in CD34+/CFSEMAX quiescent LSC. Indeed, in vitro apoptosis was significantly increased by IKK2 inhibition alone (fc: 7.4) or in combination with NIL (fc: 8.5; Figure 3D), suggesting that LY treatment exerts its anti-leukemic effects observed upon secondary transplantation at least partially by induction of apoptosis within the LSC compartment.
Figure 2.
IKK2 inhibition reduces long-term hematopoietic stem cells and inhibits disease re-initiation in vivo. (A) Schematic overview of the experimental setup: 2x106 bone marrow (BM) cells of either FVB/N Scl-tTa or Scl-tTa-BCR-ABL mice were transplanted into irradiated wild-type FVB/N recipients. Expression of BCR-ABL was induced 1 week after transplantation and treatment was started at 2 weeks after transplant and continued for 3 weeks. During that time, LY2409881 (LY) was administered via intraperitoneal injection, 3 times per week (50 mg/kg body weight, dissolved in 5% dextrose) and/or nilotinib (NIL) treatment was performed via oral gavage, daily (50 mg/kg body weight, dissolved in 10% N-methyl-2-pyrrolidon and 90% polyethylene glycol) and/or the corresponding vehicle control for 3 weeks daily. Following treatment groups were evaluated: ScltTa (vehicle, designated as control) or Scl-tTa-BCR-ABL (vehicle, LY, NIL, and LY + NIL). After sacrifice, 2x106 BM cells of treated animals were transplanted into secondary irradiated recipients. These mice were sacrificed for analyses 6 weeks after transplantation. (B) BM-derived long-term hematopoietic stem cells (LT-HSC) (lin-,Sca1+,ckit+,CD48low,CD150+) of treated recipients, shown as % of living cells. (C) Quantitative real time polymerase chain reaction (qRT-PCR) analyses of Tnf and A20 mRNA expression in BM and spleen of treated primary recipients is shown relative to Gapdh (%). (D) BCR-ABL mRNA expression in BM of primary and secondary (E) recipients. Significance was calculated using one or two-way ANOVA; mean ± standard deviation; *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001.
Figure 3.
Targeting elevated NF-kB signaling substantially reduces chronic phase and blast crisis chronic myeloid leukemia stem cells. (A) Gene set enrichment analysis (GSEA) of published expression data set GSE40721 comparing CML CD34+;CD38+ progenitor cells with CML CD34+;CD38- stem cells for the ‘HALLMARK_TNFA_SIGNALING_VIA_NFKB’ gene set. (B) Colony-forming unit (CFU) assays using primary patient-derived CD34+ bone marrow (BM) cells after being treated for 72 hours (h) using LY2409881 (LY) (10 mM), nilotinib (NIL) (50 nM), LY + NIL or DMSO control, in the presence of TNF (1 ng/mL). (C) CFU counts upon serial-plating using cells obtained in (B), without any further treatment. (D) Analysis of apoptotic and CFSEMax/Annexin V CD34+ chronic phase chronic myeloid leukemia (CML-CP) patient-derived BM cells after being treated for 72 h using LY (10 mM), NIL (50 nM), LY + NIL, or DMSO control, in the presence of TNF (1 ng/mL). Shown is 1 of 3 representative results. (E) GSEA of published expression data set GSE47927 comparing CML-CP hematopoietic stem cells (HSC) with blast crisis CML (CML-BC) HSC analyzed for the ‘HALLMARK_TNFA_SIGNALING_VIA_NFKB’-gene set. (F) CFU assays of BC-CML-derived mononucleated (MNC) BM cells being treated for 72 h using LY (10 mM), NIL (50 nM), LY + NIL, or DMSO control in the presence of TNF (1 ng/mL). Significance was calculated using one or two-way ANOVA; mean ± standard deviation; *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001.
As further LSC persistence-mediating cytokines activate the NF-kB pathway, we next tested the treatment effect in the presence of physiological IL-1α or IL-1b levels (Online Supplementary Figure S3B). Again, colony formation was significantly reduced by inhibition of IKK2 alone (IL-1α: 1.5fold, IL-1b: 1.7-fold) as well as by combined IKK2- and BCR-ABL-targeting (IL-1α: 3.4-fold, IL-1b: 5.2-fold), suggesting that IKK2 targeting could exerts its effects by inhibiting, not only TNF-mediated NF-kB activation but also due to targeting further pro-leukemic inflammatory signaling.
In the context of progressed disease, IKK2 was described as a resistance-associated gene.14
In line with this, TNF signaling increased in BM CD34+ cells upon CML progression (Figure 3E). Therefore, we studied IKK2 targeting also in primary BC-CML samples, showing that impaired colony formation was evident upon LY exposure in all patient samples tested (CML-BC #1: 10.9-fold; #2: 7.4-fold; #3: 13.9-fold; Figure 3F; Online Supplementary Figure S3C). Again, in combination this was further reduced by NIL (CML-BC #1: 21.4-fold; #2: 42-fold; #3: 93.7-fold). In conclusion, our results underline the potential of NF-kB targeting, via IKK2-inhibition, to eliminate TKI-persisting LSC. In vivo treatment revealed the complexity. While NIL alone and in combination was able to reduce leukemic cells, LSC persisted and re-initiated the disease upon secondary transplant. Treatment with NIL expanded CD3+ T cells, which was still observed when combined with LY but not in LY mono-therapy-treated mice (Online Supplementary Figure S2C). As T cells in CML display a TNF-dominated cytokine secretion profile,15 we assume this could be a source of enhanced splenic Tnf expression, probably exerting paracrine effects on the BM, thereby potentially protecting BM-residing LSC.
Supplementary Material
Acknowledgments
The authors thank Dr. Vignir Helgason and Dr. Eric Kalkman for providing KCL22 T315I cells, Julia Plum and Kristina Pannen for excellent technical assistance, and Dr. Jörg Eschweiler for providing healthy donor-derived cells. This work was supported by the IHC (immunohistochemistry) facility, a core facility of the Interdisciplinary Center for Clinical Research (IZKF) Aachen, within the Faculty of Medicine at RWTH Aachen University. Figures were created with BioRender.com.
Funding Statement
Funding: This work was supported by the Clinical Research Group entitled “Untangling and Targeting Mechanisms of Myelofibrosis in Myeloproliferative Neoplasms (MPN)” (CRU344) funded by the German Research Foundation (DFG) (SCHE 1938/3-1 [AOBJ 659838]), in the framework of the Research Training Group “Tumor-targeted Drug Delivery" grant 331065168 as well as by the START-Program of the Faculty of Medicine, RWTH Aachen (grant 691706).
References
- 1.Giustacchini A, Thongjuea S, Barkas N, et al. Single-cell transcriptomics uncovers distinct molecular signatures of stem cells in chronic myeloid leukemia. Nat Med. 2017;23(6):692-702. [DOI] [PubMed] [Google Scholar]
- 2.Herrmann O, Kuepper MKMK, Bütow M, et al. Infliximab therapy together with tyrosine kinase inhibition targets leukemic stem cells in chronic myeloid leukemia. BMC Cancer. 2019;19(658):1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hsieh MY, Van Etten RA. IKK-dependent activation of NF-kB contributes to myeloid and lymphoid leukemogenesis by BCR-ABL1. Blood. 2014;123(15):2401-2411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yamashita M, Passegué E. TNF-α coordinates hematopoietic stem cell survival and myeloid regeneration. Cell Stem Cell. 2019;25(3):357-372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gallipoli P, Pellicano F, Morrison H, et al. Autocrine TNF-α production supports CML stem and progenitor cell survival and enhances their proliferation. Blood. 2013;122(19):3335-3339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sakurai H, Suzuki S, Kawasaki N, et al. Tumor necrosis factor-α-induced IKK phosphorylation of NF-kB p65 on serine 536 is mediated through the TRAF2, TRAF5, and TAK1 signaling pathway. J Biol Chem. 2003;278(38):36916-36923. [DOI] [PubMed] [Google Scholar]
- 7.Brenner D, Blaser H, Mak TW. Regulation of tumour necrosis factor signalling: live or let die. Nat Rev Immunol. 2015;15(6):362-374. [DOI] [PubMed] [Google Scholar]
- 8.Deng C, Lipstein M, Rodriguez R, et al. The novel IKK2 inhibitor LY2409881 potently synergizes with histone deacetylase inhibitors in preclinical models of lymphoma through the downregulation of NF-kB. Clin Cancer Res. 2015;21(1):134-145. [DOI] [PubMed] [Google Scholar]
- 9.Kuepper MKMK, Bütow M, Herrmann O, et al. Stem cell persistence in CML is mediated by extrinsically activated JAK1-STAT3 signaling. Leukemia. 2019;33(8):1964-1977. [DOI] [PubMed] [Google Scholar]
- 10.Yuan H, Wang Z, Gao C, et al. BCR-ABL Gene expression is required for its mutations in a novel KCL-22 cell culture model for acquired resistance of chronic myelogenous leukemia. J Biol Chem. 2010;285(7):5085-5096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schemionek M, Elling C, Steidl U, et al. BCR-ABL enhances differentiation of long-term repopulating hematopoietic stem cells. Blood. 2010;115(16):3185-3195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Priem D, Devos M, Druwé S, et al. A20 protects cells from TNF-induced apoptosis through linear ubiquitin-dependent and -independent mechanisms. Cell Death Dis. 2019;10(10):692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhao Y, Li Y, Qu R, et al. Cortistatin binds to TNF-α receptors and protects against osteoarthritis. EBioMedicine. 2019;41:556-570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Villuendas R, Steegmann JL, Pollán M, et al. Identification of genes involved in imatinib resistance in CML: a gene-expression profiling approach. Leukemia. 2006;20(6):1047-1054. [DOI] [PubMed] [Google Scholar]
- 15.Westermann J, Van Lessen A, Schlimper C, et al. Simultaneous cytokine analysis by cytometric bead array for the detection of leukaemia-reactive T cells in patients with chronic myeloid leukaemia. Br J Haematol. 2006;132(1):32-35. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.