Abstract
Purpose
Various surgical modalities are available to treat Neer types 2 and 5 unstable fractures of lateral end clavicle but none of them are standardized. Arthroscopic fixation of the displaced lateral end clavicle fractures provides good short-term results but mid- to long-term outcomes are not available. The purpose of this study was to show the mid- to long-term radiological and functional outcomes of these fractures treated arthroscopically by a TightRope device, and to show the complications associated with this procedure.
Methods
A retrospective study was conducted over 2 years from January 2014 to December 2015 with a minimum 5-year follow-up. Active patients aged 18–50 years with acute (less than 3 weeks) displaced fracture of lateral end of the clavicle, with a minimum 5-year follow-up were included in the study. Patients with associated fractures of the proximal humerus, glenoid, scapula and acromioclavicular joint injuries were excluded from the study along with open fractures and neurovascular injuries. The outcomes were assessed by objective (complications and radiographic examination) and subjective criteria (quick disabilities of the arm, shoulder and hand score, the Constant-Murley score and the visual pain analogue scale). The data were analyzed by SPSS version 21.0.
Results
Totally, 42 patients were operated during the study period and 37 were available with a minimum 5-year follow-up. Thirty were male and 7 were female with a mean age of 29.5 years and a mean follow-up of 6.1 years. The mean quick disabilities of the arm, shoulder and hand score was 68.2 ± 4.6 preoperatively and 1.27 ± 2.32 at final follow-up (p < 0.001); the mean visual pain analogue scale score was 6.85 ± 2.2 preoperatively and 0.86 ± 1.60 at final follow-up (p < 0.001). The average Constant-Murley score was 93.38 ± 3.25 at the end of the follow-up. There were 2 fixation failures, with established non-union and 3 patients developed radiographic acromioclavicular joint arthritis.
Conclusions
Arthroscopic TightRope fixation of displaced lateral end clavicular fractures provides good radiological and functional outcomes at mid- to long-term follow-up. With the low complication rates and high patient satisfaction, this technique can be considered as a primary option in the surgical treatment of these fractures.
Keywords: TightRope, Lateral end clavicle, Fracture, Arthroscopy
Introduction
Lateral end clavicle fractures account for about 10%–20% of all clavicle fractures.1, 2, 3, 4 Successful management of lateral third clavicle fractures is dependent upon distinguishing subtle variations in the fracture pattern, that are indicative of potential fracture instability.5 Neer classified these fractures based on fracture locations of the coracoclavicular (CC) ligaments and acromioclavicular (AC) joint and the integrity of CC ligaments.6 Neer types 1 and 3 are considered stable with intact CC ligaments and are treated non-operatively.7 Neer types 2 and 5 (Craig modification of Neer classification)8 are considered unstable fracture patterns. Multiple deforming forces act on these fracture patterns due to the pull of attached musculature on the fragments and the weight of the arm, in the setting of torn CC ligaments, which displace the fracture fragments. This results in a high chance of non-union if these are treated non-operatively. They account for nearly half of overall clavicle fracture non-unions,6,9 hence, surgical treatment is recommended. However, the surgical modality is yet to be standardized.10,11
Various surgical modalities have been described such as open reduction and internal fixation with tension band wiring, Kirschner wires,12 Knowles pin,13 CC screws,14 etc., which provide rigid fixation and may restrict clavicular mobility. Modalities for open treatment that can conserve clavicular mobility include hook plate fixation15 and pre-contoured locking plates, but these techniques are associated with a high complication rate due to painful or prominent hardware.
Indirect fixation of these fractures by CC stabilization has been described as both open16,17 and arthroscopically assisted18,19 approaches. Studies utilizing both these approaches show good short-term results. To our knowledge, no study describes mid- to long-term outcome of displaced lateral end clavicle fractures treated by arthroscopic CC stabilization using the TightRope device as the sole modality of fixation.
The aim of this study was (1) to show the mid- to long-term radiological and functional outcomes of displaced lateral end clavicle fractures treated by arthroscopic CC stabilization using a TightRope device, and (2) to show the complication associated with this procedure. The hypothesis was that arthroscopically assisted fixation of displaced lateral end clavicle fractures by using a TightRope device would provide good functional and radiological outcomes with low complications.
Methods
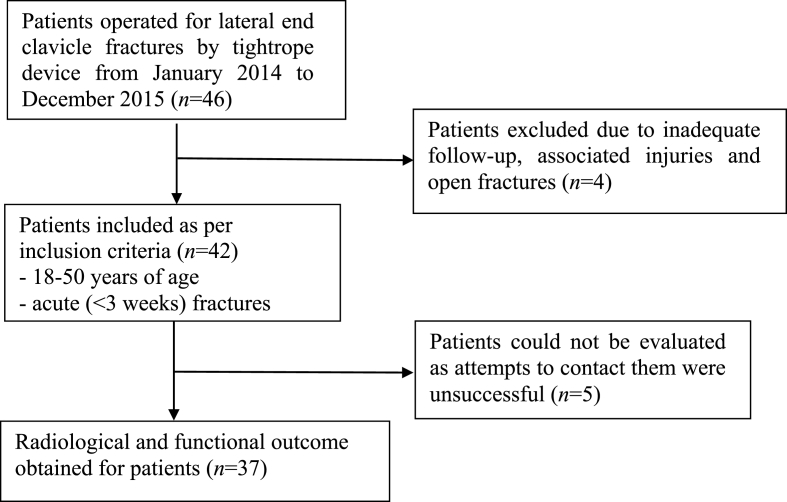
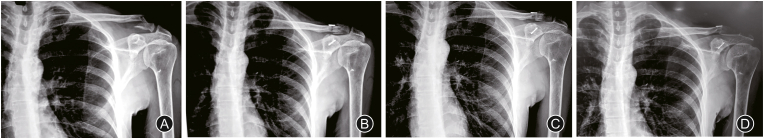
This was a single-center, retrospective study evaluating patients that had undergone arthroscopically assisted fixation of displaced lateral end clavicle fractures by using a TightRope device, over 2 years from January 2014 to December 2015 (Fig. 1). Ethical approval was obtained from the Ethics Committee of the Institution. Active patients aged 18–50 years with acute (less than 3 weeks) displaced fracture of lateral end of the clavicle, with a minimum 5-year follow-up were included in the study. Patients with associated fractures of the proximal humerus, glenoid, scapula and AC joint injuries were excluded from the study along with open fractures and neurovascular injuries. Forty-two patients were identified and patient data were compiled with the following parameters: age, sex, side of injury, days from injury, fracture type, follow-up duration, intraoperative and postoperative complications, radiological outcomes, clinical outcomes, and functional scoring (Table 1). The outcomes were assessed by objective and subjective criteria. The objective assessment included complications, radiographic examination (X-ray at preoperative (Fig. 2A), immediate postoperative (Fig. 2B) at 1-year follow-up (Fig. 2C) and 5-year follow-up (Fig. 2D) period) to evaluate maintenance of fracture reduction and fracture healing. Subjective assessment was done using the quick disabilities of the arm, shoulder, and hand (QuickDASH) score, the Constant-Murley score and the visual pain analogue scale (VAS); done preoperatively and at final follow-up.
Fig. 1.
Workflow diagram.
Table 1.
Demographic and mid-term outcome data of the study population.
| Variables | Results | p value |
|---|---|---|
| Age (year) | 29.5 (7.48) | |
| Sex | ||
| Male | 30 | |
| Female | 7 | |
| Side | ||
| Left | 18 | |
| Right | 19 | |
| Days from injury | 7.43 (2.9) | |
| Fracture type (Neer classification) | ||
| 2a | 12 | |
| 2b | 19 | |
| 5 | 6 | |
| Follow-up (year) | 6.1 (1.1) | |
| QuickDASH score | < 0.001 | |
| Preoperatively | 68.2 (4.6) | |
| Final follow-up | 1.27 (2.32) | |
| VAS | < 0.001 | |
| Preoperatively | 6.85 (2.2) | |
| Final follow-up | 0.86 (1.60) | |
| Constant-Murley score | 93.38 (3.25) | |
| Complications | ||
| Implant failure and non-union | 2 | |
| AC joint arthritis | 3 | |
| Bone resorption around the coracoid button | 3 | |
Note: Data in results expressed as n or mean (SD).
VAS: visual pain analogue scale; AC: acromioclavicular; DASH: disabilities of the arm, shoulder, and hand.
Fig. 2.
(A) Preoperative X-ray of displaced lateral end clavicle fracture; (B) Immediate post-operative X-ray showing reduction of fracture by TightRope; (C) X-ray at 1-year follow-up showing anatomical reduction and fracture consolidation and (D) At 5-year follow-up X-ray showing maintenance of reduction and fracture consolidation.
All procedures were carried out under general anesthesia in the beach chair position with image intensification. Standard portals were used. Diagnostic arthroscopy of the glenohumeral joint was performed initially. The anterolateral portal, made approximately 1.5 cm lateral to the acromion and in line with its anterior border to visualize the coracoid. The TightRope drill guide was placed on the inferior surface of the base of the coracoid through an anterosuperior portal, aiming to keep it centered on the coracoid base. An incision of about 10 mm was placed, in the plane of the coracoid, midway between the anterior and posterior borders of the clavicle, medial to the fracture site. The other end of the drill guide, with drill sleeve, was then placed at a distance of 10 mm from the fracture. Under arthroscopic visualization and C-arm confirmation, with the drill guide maintained in position, a guidewire was passed from the clavicle to the base of the coracoid keeping it as close to the center as possible. The TightRope reamer was then used to collinearly drill the clavicle and the base of the coracoid to make the tunnel. The flip button TightRope device that is composed of 2 metal buttons, one oblong and the other rounded, connected by a loop of fiber wire was taken. The device was inserted into the loop, passing through the clavicle and the base of the coracoid. The button was flipped under arthroscopic visualization and positioned at the coracoid base using a suture retriever. The medial clavicular fragment was pushed inferiorly manually or using a bone tamp and superior force was applied on the elbow and arm to aid in reducing the fracture. The flip button was then tied down over the round button on the superior surface of the clavicle after reduction was obtained under the image intensifier. Standard closure of the portals and incisions was done. Patients were discharged on the second postoperative day. The shoulder was immobilized in a brace for about 3 weeks after which the brace was discarded and mobilization was started.
Continuous variables were reported as mean ± SD and median. The data were entered in MS EXCEL spreadsheet and analysis was done using SPSS version 21.0.
Results
Among the 42 identified patients, radiological and functional outcomes were obtained for 37 patients. Attempts to contact 5 of the patients were unsuccessful. Of these patients, 30 were male and 7 were female. The mean age of the patients was 29.5 years (range 19–46 years) and the mean follow-up duration was 6.1 years. There were 15 Neer type 2a fractures and 22 type 2b fractures in the 37 patients. The last of the patients was assessed in January 2021.
None of the patients had any intraoperative or immediate post-operative complications. The mean QuickDASH score was 68.2 ± 4.6 preoperatively and 1.27 ± 2.32 at final follow-up (p < 0.001); the mean VAS score was 6.85 ± 2.2 preoperatively and 0.86 ± 1.60 at final follow-up (p < 0.001). The average Constant-Murley score was 93.38 ± 3.25 at the end of the follow-up. All of the patients had returned to their original occupations. The average time to return to occupation was 16 weeks. Twelve of the patients were recreational sportspersons and all of them had resumed sporting activities at an average duration of about 19 weeks. Thirty-three patients had a full range of motion of the operated side compared to the healthy side (restriction of range of motion in 10.8%). None of the patients reviewed during follow-up visits had any undue prominence of the clavicular button.
Of the 37 patients assessed, 35 had an anatomical reduction and fracture consolidation at the end of 5 years. There were 2 fixation failures (5.4%) with established non-union, despite initial radiographs showing a good reduction. Bony union was found in all other cases at an average period of 8–12 weeks. Three patients developed radiographic AC joint arthritis between 18 and 24 months but only 2 of them were symptomatic and were managed conservatively. No patient had undergone secondary surgery for removal of the implant. Ossification was seen on the inferior surface of the distal clavicle at the site of CC ligament attachment, in 5 patients but these patients had no symptoms. Follow-up radiographs showed mild bone resorption around the clavicular button in 32 patients. The clavicular button was found to be subsided into the clavicle in 4 patients, but none of them had any symptoms and the reduction of the clavicle was maintained. There were 3 patients with bone resorption around the coracoid button, 1 of whom had resorption around the coracoid button as well. No other patient had any bone reaction around the implant. Despite of enlargement of clavicular and coracoid holes, there was no case of refracture in our patients during the follow-up period.
Discussion
The most important finding of this study was that arthroscopically assisted fixation of displaced lateral end clavicle fractures by TightRope leads to improved QuickDASH score, Constant-Murley score and VAS score for pain with a low complication rate.
Neer types 2 and 5 are considered unstable fracture patterns. Neer type 2 fractures are subdivided into 2a and 2b. In type 2a, the fracture line passes medial to the CC ligaments, with the intact ligaments. In type 2b the fracture occurs between the conoid and trapezoid components of the CC ligaments and the conoid ligament is torn, or the fracture occurs lateral to the CC ligaments and both the conoid and trapezoid components of the ligaments are torn. Operative management is the treatment of choice for these displaced lateral end clavicle fractures.6,20 Non-operative management of these fractures is fraught with high chances of non-union and subsequent pain and limitation of shoulder function.21
These fractures have traditionally been treated with open reduction and direct osteosynthesis using hook plates and pre-contoured locking plates. Their outcomes have been satisfactory, although they are associated with problems of hardware prominence and they also necessitate a second surgery for removal.22,23 In their meta-analysis of 425 cases, Oh et al.24 studied cases managed by hook plates, K-wires and tension band wiring, intramedullary fixation and CC stabilization. They found that the non-union rate was not significantly different among the techniques. The complication rate was significantly higher when using the hook plate (40.7%) and K-wire plus tension band wiring (20.0%) than when resorting to either CC stabilization (4.8%). The most frequent complications were restriction of range of motion (18.5%), plate migration (9.3%) and acromion hole widening (4.3%) when using hook plate, and infection (7.5%) and partial loss of reduction (7.5%) when using K-wire plus tension band wiring. In comparison our study showed restriction in range of motion in 10.8% cases, and the rate of loss of reduction due to fixation failure was 5.4%.
Stegeman et al.25 in their meta-analysis demonstrated that all these methods have good rates of fracture union without significant difference in functional outcome. However, these techniques are associated with a high complication rate. Most of the reported complications are due to painful or prominent hardware and the reoperation rate can be as high as 43%.26 Other complications of the hook plate include are infection and a stiff shoulder. They also entail a future surgery for implant removal. Locking plates are better than the hook plate in complication rate but they are also not free from hardware irritation and also may necessitate a future surgery for removal.27
Additionally, methods of direct osteosynthesis rely on adequate bony purchase of the screws in the lateral fragment, which may be small and comminuted, thereby making internal fixation difficult and unsound.28 Unlike locking plate fixation, indirect fixation by CC stabilization with TightRope does not rely on size and bony purchase in the lateral fragment.17 Indirect fixation by CC stabilization can address the problem of hardware prominence and a small comminuted lateral fragment with excellent union rates and good functional outcomes.24
CC stabilization using the TightRope device has been done utilizing both open16,17 and arthroscopic techniques.18,19 The arthroscopic technique has shown good radiological and functional outcomes with low complication rates in short-term follow-ups. Loriaut et al.18 retrospectively analyzed 21 patients with isolated type 2b fractures of the lateral end of the clavicle, who underwent arthroscopically assisted fixation using a double button. They reported mean QuickDASH score, Constant-Murley score and VAS score as 3.2 ± 6, 94.8 ± 9.9 and 0.5 ± 1.2, respectively, at the end of a mean follow-up of 35 months. They reported 1 case of implant failure with non-union and 1 case of AC arthritis. Similarly, good short- to medium-term outcomes of this technique are borne out in the study by Motta et al.19 who reported a 2-year follow-up of 14 patients with type 2a, 2b and 5 fractures treated arthroscopically with TightRope. They reported that all fractures were confirmed to have healed without limitations in range of motion or loss of reduction. They reported delayed healing in only 2 patients. These results are comparable to results obtained in this study. Furthermore, the good outcomes obtained were maintained in the mid-term follow-up. The restriction of range of motion in 4 patients did not affect their function.
To the best of our knowledge, this study has one of the largest series of cases treated with arthroscopic TightRope fixation and the first study to report the mid- to long-term follow-up of isolated TightRope fixation of displaced lateral clavicle fractures. Five-year follow-up of patients showed good functional and radiological outcomes with low complications.
This study had a few limitations. First of all, this was a retrospective descriptive review of cases. Functional scoring was done only at the end of the follow-up period. Fractures included in this study were type 2a, 2b fractures. Only the younger active population was included. A better understanding of the utility of this technique may be obtained by a prospective study. The standard of care regarding the management of these fractures is yet to be established and a randomized study comparing the TightRope to other modalities of surgical treatment may prove useful.
In conclusion, arthroscopic TightRope fixation of displaced lateral end clavicular fractures provides good radiological and functional outcomes at mid- to long-term follow-up. With the low complication rate and high patient satisfaction, this technique can be considered as a primary option in the surgical treatment of these fractures.
Funding
Nil.
Ethical statement
Ethical approval was obtained from the Ethics Committee of the Institution.
Declaration of competing interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Author contributions
Amit Meena: Concepts, design, literature search, data acquisition, data analysis, statistical analysis, manuscript preparation, manuscript editing, manuscript review and responsible for all the correspondence. Akshya Raj A: manuscript preparation, manuscript editing, manuscript review, statistical analysis. Sumon Singphow saikia: Data acquisition, statistical analysis, manuscript preparation, manuscript editing, manuscript review. B P Sharma: Supervisor of the study, performed all the surgeries, manuscript editing and review. All the authors approved the final version of the manuscript.
Acknowledgments
The study group wants to thank all the participants of the study for their efforts.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Edwards D.J., Kavanagh T.G., Flannery M.C. Fractures of the distal clavicle: a case for fixation. Injury. 1992;23:44–46. doi: 10.1016/0020-1383(92)90125-C. [DOI] [PubMed] [Google Scholar]
- 2.van der Meijden O.A., Gaskill T.R., Millett P.J. Treatment of clavicle fractures: current concepts review. J Shoulder Elbow Surg. 2012;21:423–429. doi: 10.1016/j.jse.2011.08.053. [DOI] [PubMed] [Google Scholar]
- 3.Nordqvist A., Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res. 1994;300:127–132. [PubMed] [Google Scholar]
- 4.Robinson C.M. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br. 1998;80:476–484. doi: 10.1302/0301-620X.80B3.0800476. [DOI] [PubMed] [Google Scholar]
- 5.Banerjee R., Waterman B., Padalecki J., et al. Management of distal clavicle fractures. J Am Acad Orthop Surg. 2011;19:392–401. doi: 10.5435/00124635-201107000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Neer C.S., 2nd Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- 7.Deafenbaugh M.K., Dugdale T.W., Staeheli J.W., et al. Nonoperative treatment of Neer type II distal clavicle fractures: a prospective study. Contemp Orthop. 1990;20:405–413. [PubMed] [Google Scholar]
- 8.Craig E.V. In: Rockwood C.A. Jr., Matsen F.A. III, editors. ume 1. WB Saunders; Philadelphia: 1990. Fractures of the clavicle; pp. 367–401. (The Shoulder). [Google Scholar]
- 9.NEER C.S., 2nd Fracture of the distal clavicle with detachment of the coracoclavicular ligaments in adults. J Trauma. 1963;3:99–110. doi: 10.1097/00005373-196303000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Kim D.W., Kim D.H., Kim B.S., et al. Current concepts for classification and treatment of distal clavicle fractures. Clin Orthop Surg. 2020;12:135–144. doi: 10.4055/cios20010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rokito A.S., Zuckerman J.D., Shaari J.M., et al. A comparison of nonoperative and operative treatment of type II distal clavicle fractures. Bull Hosp Jt Dis. 2002-2003;61:32–39. [PubMed] [Google Scholar]
- 12.Kao F.C., Chao E.K., Chen C.H., et al. Treatment of distal clavicle fracture using Kirschner wires and tension-band wires. J Trauma. 2001;51:522–525. doi: 10.1097/00005373-200109000-00016. [DOI] [PubMed] [Google Scholar]
- 13.Jou I.M., Chiang E.P., Lin C.J., et al. Treatment of unstable distal clavicle fractures with Knowles pin. J Shoulder Elbow Surg. 2011;20:414–419. doi: 10.1016/j.jse.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 14.Ballmer F.T., Gerber C. Coracoclavicular screw fixation for unstable fractures of the distal clavicle. A report of five cases. J Bone Joint Surg Br. 1991;73:291–294. doi: 10.1302/0301-620X.73B2.2005158. [DOI] [PubMed] [Google Scholar]
- 15.Haidar S.G., Krishnan K.M., Deshmukh S.C. Hook plate fixation for type II fractures of the lateral end of the clavicle. J Shoulder Elbow Surg. 2006;15:419–423. doi: 10.1016/j.jse.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 16.Yagnik G.P., Porter D.A., Jordan C.J. Distal clavicle fracture repair using cortical button fixation with coracoclavicular ligament reconstruction. Arthrosc Tech. 2018;7:e411–e415. doi: 10.1016/j.eats.2017.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al-Tawil K., Garner M., Antonios T., et al. The use of Tightrope device as the sole method of fixation in treating lateral end clavicle fractures. Shoulder Elbow. 2022;14:60–64. doi: 10.1177/1758573220964807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Loriaut P., Moreau P.E., Dallaudière B., et al. Outcome of arthroscopic treatment for displaced lateral clavicle fractures using a double button device. Knee Surg Sports Traumatol Arthrosc. 2015;23:1429–1433. doi: 10.1007/s00167-013-2772-9. [DOI] [PubMed] [Google Scholar]
- 19.Motta P., Bruno L., Maderni A., et al. Acute lateral dislocated clavicular fractures: arthroscopic stabilization with TightRope. J Shoulder Elbow Surg. 2014;23:e47–e52. doi: 10.1016/j.jse.2013.05.016. [DOI] [PubMed] [Google Scholar]
- 20.Neviaser R.J. Injuries to the clavicle and acromioclavicular joint. Orthop Clin N Am. 1987;18:433–438. doi: 10.1016/S0030-5898(20)30373-4. [DOI] [PubMed] [Google Scholar]
- 21.Kashii M., Inui H., Yamamoto K. Surgical treatment of distal clavicle fractures using the clavicular hook plate. Clin Orthop Relat Res. 2006;447:158–164. doi: 10.1097/01.blo.0000203469.66055.6a. [DOI] [PubMed] [Google Scholar]
- 22.Sajid S., Fawdington R., Sinha M. Locking plates for displaced fractures of the lateral end of clavicle: potential pitfalls. Int J Shoulder Surg. 2012;6:126–129. doi: 10.4103/0973-6042.106226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martetschläger F., Kraus T.M., Schiele C.S., et al. Treatment for unstable distal clavicle fractures (Neer 2) with locking T-plate and additional PDS cerclage. Knee Surg Sports Traumatol Arthrosc. 2013;21:1189–1194. doi: 10.1007/s00167-012-2089-0. [DOI] [PubMed] [Google Scholar]
- 24.Oh J.H., Kim S.H., Lee J.H., et al. Treatment of distal clavicle fracture: a systematic review of treatment modalities in 425 fractures. Arch Orthop Trauma Surg. 2011;131:525–533. doi: 10.1007/s00402-010-1196-y. [DOI] [PubMed] [Google Scholar]
- 25.Stegeman S.A., Nacak H., Huvenaars K.H., et al. Surgical treatment of Neer type-II fractures of the distal clavicle: a meta-analysis. Acta Orthop. 2013;84:184–190. doi: 10.3109/17453674.2013.786637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Böstman O., Manninen M., Pihlajamäki H. Complications of plate fixation in fresh displaced midclavicular fractures. J Trauma. 1997;43:778–783. doi: 10.1097/00005373-199711000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Zhang C., Huang J., Luo Y., et al. Comparison of the efficacy of a distal clavicular locking plate versus a clavicular hook plate in the treatment of unstable distal clavicle fractures and a systematic literature review. Int Orthop. 2014;38:1461–1468. doi: 10.1007/s00264-014-2340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Page R.S., Bhatia D.N. Noncomminuted lateral end clavicle fractures associated with coracoclavicular ligament disruption: technical considerations for optimal anatomic fixation and stability. Int J Shoulder Surg. 2014;8:86–89. doi: 10.4103/0973-6042.140116. [DOI] [PMC free article] [PubMed] [Google Scholar]