Abstract
Study Objectives:
Sleep deficiency can adversely affect the performance of resident physicians, resulting in greater medical errors. However, the impact of sleep deficiency on surgical outcomes, particularly among attending surgeons, is less clear.
Methods:
Sixty attending surgeons from academic and community departments of surgery or obstetrics and gynecology were studied prospectively using direct observation and self-report to explore the effect of sleep deprivation on patient safety, operating room communication, medical errors, and adverse events while operating under 2 conditions, post-call (defined as > 2 hours of nighttime clinical duties) and non-post-call.
Results:
Each surgeon contributed up to 5 surgical procedures post-call and non-post-call, yielding 362 cases total (150 post-call and 210 non-post-call). Most common were caesarian section and herniorrhaphy. Hours of sleep on the night before the operative procedure were significantly less post-call (4.98 ± 1.41) vs non-post-call (6.68 ± 0.88, P < .01). Errors were infrequent and not related to hours of sleep or post-call status. However, Non-Technical Skills for Surgeons ratings demonstrated poorer performance while post-call for situational awareness, decision-making, and communication/teamwork. Fewer hours of sleep also were related to lower ratings for situational awareness and decision-making. Decreased self-reported alertness was observed to be associated with increased procedure time.
Conclusions:
Sleep deficiency in attending surgeons was not associated with greater errors during procedures performed during the next day. However, procedure time was increased, suggesting that surgeons were able to compensate for sleep loss by working more slowly. Ratings on nontechnical surgical skills were adversely affected by sleep deficiency.
Citation:
Quan SF, Landrigan CP, Barger LK, et al. Impact of sleep deficiency on surgical performance: a prospective assessment. J Clin Sleep Med. 2023;19(4):673–683.
Keywords: sleep deficiency, insufficient sleep, surgery, surgical complications, attending surgeon, surgical outcomes
BRIEF SUMMARY
Current Knowledge/Study Rationale: Sleep deficiency can adversely affect the performance of resident physicians, resulting in greater medical errors. However, the impact of sleep deficiency on surgical outcomes, particularly among attending surgeons, is less clear.
Study Impact: Although sleep deficiency in attending surgeons adversely affected ratings on their nontechnical surgical skills, it was not associated with a greater rate of errors during procedures performed on the following day. However, procedure time increased, suggesting that surgeons are able to compensate for sleep loss by working more slowly.
INTRODUCTION
Chronically insufficient sleep is endemic in the United States,1 where nearly one-third of adults regularly sleep less than 6 hours.2 Sleep deficiency is associated with impairments in mood and cognitive and psychomotor function.1 In occupational settings such as the transportation industry where decision-making, attention, and motor skills are critical, sleep deficiency has been found to result in disastrous consequences, including loss of life and substantial property costs.3
Physicians may be similarly affected by sleep deficiency, and impairments in their performance could adversely affect patient care.4 Much of the evidence examining the effect of sleep deficiency on physician performance has focused on resident physicians. Studies of resident physicians document that they frequently work more than 24 consecutive hours and that their sleep deprivation results in increased medical errors.5–7 Surgical residents may be at particular risk for adverse impacts of insufficient sleep because of the requirements for precision motor skills, attention to detail, and rapid decision-making in the operating room. Most, but not all, studies using surgical simulators have demonstrated that sleep deprivation adversely affects residents’ surgical proficiency and increases errors.8 However, greater complication and mortality rates related to resident physician sleep deprivation have not been consistently demonstrated.9–11 It is possible that the impact of fatigue and sleep deficiency among surgical residents is mitigated by the supervision of attending surgeons, who are present during most operative procedures, although this remains unclear.12–14
Unlike resident physicians, who are limited to 80–88 hours maximum per week and shifts of no more than 28 consecutive hours by the Accreditation Council for Graduate Medical Education, attending physicians have no restrictions on their work hours. Moreover, limitation on duty hours imposed on residents may result in greater workloads on attending physicians. In 1 survey, 37.1% of practicing primary care physicians and 60.6% of surgeons worked more than 80 hours per week, which is the maximum amount allowed for resident physicians in most residency programs by the Accreditation Council for Graduate Medical Education.15 However, there are few studies of the effect of sleep deficiency on performance among attending physicians. In a recent cross-sectional survey of over 11,000 US physicians including 7,700 attending physicians, subjective sleep-related impairment was associated with self-reported clinically significant medical errors.4 Another smaller study also confirmed the occurrence of increased errors related to self-perceived sleepiness.16 In both studies, results stratified by specialty and training status were not provided. Most investigations focused exclusively on surgical performance have not demonstrated increased morbidity or mortality,17–19 but few have specifically quantified the amount of sleep experienced.18 In the 2 studies that did assess sleep, Chu et al20 concluded that prior sleep duration did not affect cardiac surgical outcomes, whereas Rothschild et al21 found increased complications in a variety of surgical procedures when surgeons had less than a 6-hour sleep opportunity the night prior to the procedure. Both investigations were retrospective with data obtained through chart review.
In the present study, we performed a prospective evaluation of the impact of sleep deficiency on attending surgeons comparing their operative performance after having had a night of normal sleep opportunity vs a night of diminished sleep opportunity, the latter characterized by having a night on call with at least 2 hours of hospital clinical duties. Our primary goal was to determine whether there would be more medical errors, adverse events, and operating room communication and teamwork issues after a night on call. Performance was assessed prospectively by independent observers in the operating room as well as by self-assessment.
METHODS
Study design
We conducted a prospective within-subjects, repeated measures observational study in which attending surgeons were evaluated to explore the effect of sleep deprivation and extended duration shifts on patient safety through direct observation and self-reporting of operating room communication failures, medical errors, and adverse events. Surgeons were assessed while operating under 2 conditions, post-call and non-post-call, to capture the impact of sleep deficiency on their performance. Post-call cases were defined as surgical cases performed the morning after a surgeon had clinical duties occurring for at least 2 hours between the hours of 12 am and 7 am. Non-post-call cases were performed on mornings where surgeons had not been on clinical duty the prior night.
Participants
Surgeons were recruited from 8 local area hospitals with surgical and/or obstetrical services. In order to provide a heterogeneous sample of surgeons, hospitals considered for inclusion were of varying characteristics based on the American Hospital Association’s definitions, which group hospitals based on size (small, medium, or large), geographical region (urban or rural), and the presence or absence of an academic program (academic or nonacademic “community”). Presentations were made to the administration and surgical department chairs of these hospitals to elicit their collaboration in the study. If a hospital agreed to collaborate, a formal recruitment letter was disseminated among the attending surgeons followed by attempts at personal contact. Sixty surgeons from a variety of specialties agreed to participate and provided informed consent (Table 1). The study protocol was approved by the Institutional Review Board of Partners Healthcare (protocol no.: 2008P002394).
Table 1.
Surgeon characteristics.
| Age, years (mean ± SD) | 47.6 ± 9.5 |
| Sex (% men) | 64.6 |
| Race/ethnicity (%) | |
| Non-Hispanic White | 68.3 |
| Black | 6.1 |
| Hispanic | 6.1 |
| Asian | 11.0 |
| Other/unknown | 8.6 |
| Hospital affiliation (%) | |
| Hospital 1 | 20.7 |
| Hospital 2 | 13.4 |
| Hospital 3 | 4.9 |
| Hospital 4 | 8.5 |
| Hospital 5 | 11.0 |
| Hospital 6 | 13.4 |
| Hospital 7 | 8.5 |
| Hospital 8 | 11.0 |
| Multiple | 3.7 |
| Unknown/not recorded | 4.9 |
| Specialty (%) | |
| General obstetrics/gynecology | 35.4 |
| Obstetrics/gynecology subspecialty | 7.3 |
| General surgery | 26.8 |
| Surgical subspecialty | 25.6 |
| Unknown/not recorded | 4.9 |
| Years postresidency (mean ± SD) | 14.7 ± 9.9 |
| Supervise residents (% yes) | 70.7 |
Procedure
After surgeons agreed to participate, demographic information was collected by questionnaire. Additionally, surgeons completed daily sleep and work logs.
Two methods were used to identify potential post-call cases. First, surgeons were asked to notify the study team in the morning when they had been performing 1 or more overnight operations or deliveries that occupied at least 2 hours of the period between 12 am and 7 am. Second, all operative and delivery records as well as the operating room schedule were examined each morning to identify cases that required participant surgeons to be working overnight for at least 2 hours. The operating room schedule was then reviewed to determine whether the surgeon was scheduled to operate that morning. Non-post-call cases were ascertained by examining the operating and delivery room schedules for cases where the surgeon had not worked on the previous night. After appropriate cases from either post-call or non-post-call surgeons were selected, the study team was notified to be present during the operation but was blinded as to post-call status of the surgeon; surgeons were asked not to discuss their call status or sleep while in the presence of observers.
During each case, the study team consisting of 2 observers, one a person trained in human factors interactions and the other a physician, evaluated surgical performance and operating room environmental conditions using standardized observation tools. Neither individual scrubbed with the operating team but both were in the operating room. In addition, at the end of the operation, surgeons completed self-assessments of their sleep. Surgeons and other members of the operative team (eg, anesthesiologists and nurses) also assessed the level of teamwork and communication among the operating room personnel and reported any errors they believe had occurred during the operation. After the operation, chart review was conducted by the study team to identify any errors not previously noted during the procedure.
Data collection
Questionnaires
A baseline questionnaire collected demographic data as well as descriptive data about each surgeon including hospital affiliation, specialty, teaching/leadership roles, and education/subspecialization. During their period of active participation, surgeons completed daily sleep and work logs that collected sleep and wake times, awakenings, net sleep durations, naps and duration, hospital shift length, and on-call shift length.
At the conclusion of each observed surgical procedure the attending surgeon completed a postoperative questionnaire (Figure S1 (643KB, pdf) in the supplemental material). This questionnaire was designed to collect data on self-reported sleep duration, quality, and number of awakenings for work duties the previous night and general alertness during the procedure. Alertness and sleep quality were assessed using continuous rating scales with sleepy scored as 0 and alert scored as 100. Similarly, sleep quality was scored as awful equal to 0 and excellent equal to 100. Additionally, respondents were given the opportunity to self-report any medical errors that occurred during the procedure, although these were also being collected independently by the physician observer (Figure S2 (643KB, pdf) ).
Observation of the surgical procedure
The physician observer member of the study team was present at all surgical procedures to monitor and record medical errors, adverse events, and other events either directly or indirectly related to the surgical care process. All medical errors and adverse events (eg, unrecognized bleeding or inadvertent transection of a structure) identified by an observer were subsequently adjudicated by 2 independent physician reviewers blinded as to the on-call and sleep status of the surgeon. A physician observer also recorded the time spent in each step of the surgical process (ie, start to site preparation, incision, intubation, time out, incision, extubation, and out of room). Additionally, a human factors observer evaluated the procedure to identify human factor errors (eg, marking the wrong extremity to be operated upon or a contaminated instrument inadvertently left on the instrument tray) and to provide ratings of nontechnical surgical skill using the evaluation system (Non-Technical Skills for Surgeons, NOTSS) developed by the Royal College of Surgeons of Edinburgh.22 Surgeons were rated in 4 categories, situational awareness, decision-making, communication and teamwork, and leadership, using a 4-point scale where 1 = poor, 2 = marginal, 3 = acceptable, and 4 = good. The human factors observer also recorded nonoperative events related to the operating room environment that were thought to be unrelated to sleep deficiency such as equipment issues, anesthesia delays, or pages to surgical team members (Table S1 (643KB, pdf) ). Several other types of nontechnical events that occurred and were potentially related to the performance of the surgeon also were recorded by the observer team (Table 2). These included surgical team members disagreeing about the surgical process or an unexpected patient complication.
Table 2.
Frequency of nonoperative communication and task events.
| No. of Events | |||
|---|---|---|---|
| Overall (n = 360) | Non-Post-Call (n = 210) | Post-Call (n = 150) | |
| Communication events | |||
| Team members disagree about surgery progress or mention an alternative path forward | 14 | 5 | 9 |
| Miscommunication/misinterpretation of information | 22 | 11 | 11 |
| All communication events | 36 | 16 | 20 |
| Task events | |||
| Patient complication | 23 | 13 | 10 |
| Clinical nonstandard intervention | 6 | 2 | 4 |
| Patient status deteriorates | 1 | 1 | 0 |
| Unexpected information regarding patient | 4 | 2 | 2 |
| Unable to find necessary information regarding patient | 0 | 0 | 0 |
| All task events | 34 | 18 | 16 |
Statistical analysis
Differences in sleep outcomes (hours of sleep, number of awakenings, sleep quality, and alertness) based on post-call status were determined with mixed models using post-call status as a predictor, participant ID as a subject variable, and case count per participant as a random repeated-measures variable to control for within-subjects effects. We also directly evaluated the impact of sleep deficiency on processes and outcomes of interest, analogous to the approach we previously took in a retrospective study of surgeons’ sleep deficiency.21 Therefore, both post-call status and hours of sleep were used as predictors of the impact of sleep deficiency. Hours of sleep were determined based on surgeons’ sleep logs.
Operating room environmental events were clustered into 4 categories of items or events related to (1) the difficulty or complexity inherent in each procedure (E-Task), (2) interactions among the surgical team (Organization), (3) status of equipment critical to the procedure (Equipment), and (4) a miscellaneous category (Miscellaneous). The overall frequency of these events was compared according to post-call status by modeling a Poisson or negative binomial distribution as appropriate. These events also were considered as covariates in subsequent analyses.
Ratings for NOTSS were ordinal and preliminary analyses demonstrated a nonnormal distribution for all 4 categories. Therefore, the effect of post-call status was analyzed using ordinal logistic regression. Additionally, NOTSS scores were collapsed into ratings of “Good” vs “All Other” and assessed using binary logistic regression. Participant ID and case count per participant were included in the models to control for within-subjects effects. In addition, the impact of hours of sleep on NOTSS scores for each category was analyzed using repeated measures ordinal logistic regressions using participant ID as a subject variable and case count per participant as a random repeated-measures variable to control for within-subjects effects. Models included adjustment for the involvement of residents in the procedure because of the potential for NOTTS ratings to be influenced by their participation.
The impact of hours of sleep, sleep quality, number of awakenings, and alertness on time spent on the operative procedure was determined using mixed regression models with participant ID as a subject variable and case count per participant as a random repeated-measures variable to control for within-subjects effects. Because operation time varies according to the type of procedure and its complexity, procedures were clustered into related categories and dummy variables were included in the regression models. Adjusted analyses also included resident participation and hospital site as covariates because preliminary analyses suggested differences in operation time as a function of these factors.
Clinical errors defined as having the potential to directly affect the surgical procedure or a patient outcome were adjudicated by 2 physicians independently. The remaining human factor errors were adverse events related to behaviors not related to medical expertise. All errors whether recorded by the observation team or self-reported by the surgeon and other operating room personnel were combined to reflect total errors. The frequency of these events was compared as a function of post-call status using a multinomial logistic regression.
Nonoperative events occurring during the procedure (Table 2) were clustered into 2 categories, Communication and Task. The occurrence of these events was analyzed by modeling a Poisson distribution with surgeon and case count per surgeon included as covariates to control for within-subjects effects. Additionally, the E-Task and Equipment operating environment clusters were included as covariates because they were found to be different post-call compared to non-post-call.
Data are presented as percentages, means, and standard deviations. Alpha was set at 0.05 for all comparisons. IBM SPSS Versions 23 and 28 (IBM, Armonk, New York) were used for all analyses.
RESULTS
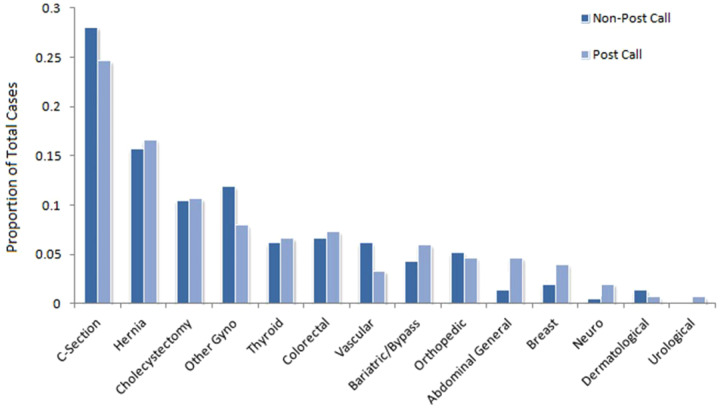
Sixty surgeons agreed to participate. Each participant took part in up to 5 surgical procedures post-call and non-post-call, with the majority of participants contributing 4 surgeries in each condition. This yielded 362 cases total (150 post-call and 210 non-post-call). Demographic and descriptive data regarding the participating surgeons are provided in Table 1. Two-thirds of the surgeons were men, and most were non-Hispanic White. They also were generally middle-aged and were experienced practitioners with an average of approximately 15 years of experience postresidency. General and surgical subspecialty surgeons constituted 52.4% of the cohort and obstetrical/gynecologic surgeons represented most of the remainder. Of the 70.7% of surgeons who indicated that they supervised residents, residents participated in 52.3% of their cases. However, in the cases observed in this study only 17.7% of cases involved a resident. Types of procedures observed stratified by call status are shown in Figure 1. Caesarian section and herniorrhaphy were the most common. Hours of sleep on the night before the operative procedure were significantly less when post-call (4.98 ± 1.41) vs non-post-call (6.68 ± 0.88; P < .01).
Figure 1. Distribution of surgical procedures according to post-call status.
The frequency of environmental events stratified by post-call status is shown in Table S1 (643KB, pdf) . There were few individual differences between post-call and non-post-call status. However, events in the cluster E-Task were more common post-call (incident rate ratio [IRR]: 3.015; 95% confidence interval [CI]: 1.562–5.821; P = .001). In contrast, Equipment events were slightly less frequent post-call (IRR: 0.688; 95% CI: 0.493–0.904; P < .05).
Errors occurred infrequently whether observed by the observer team or self-reported by surgeons, nurses, or anesthesiologists. Their distribution is shown in Table S2 (643KB, pdf) ; there was no association with the type of procedure or specialty of the surgeon (data not shown). Although errors tended to be more frequent post-call, the difference was not significant (IRR: 3.16; 95% CI: 0.623–16.018; P = .165). In addition, there was no association between hours of sleep and incidence of errors (IRR: 0.996; 95% CI: 0.715–1.388; P = .996).
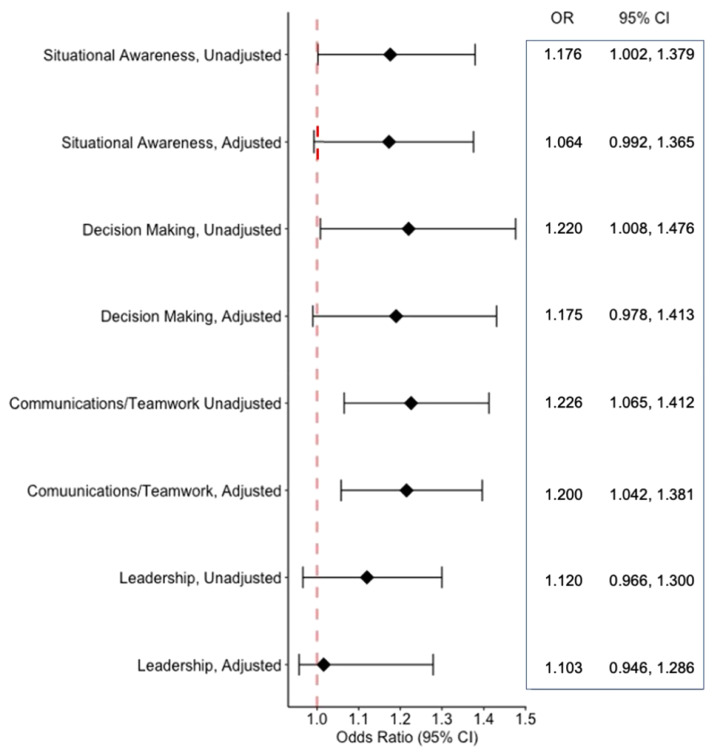
The ratings for NOTSS stratified by post-call status are shown in Table 3. Non-post-call status resulted in higher ratings for situational awareness and decision-making with a borderline effect for communication and teamwork. As shown in Table 4, the frequency of “Good” ratings was related to non-post-call status for situational awareness, decision-making, and communication and teamwork but not leadership. Similarly, more hours of sleep in a fully adjusted model (Figure 2) were associated with higher NOTSS ratings for communication and teamwork, representing an increase in likelihood of a higher NOTSS rating of 20.0% (odds ratio: 1.200; 95% CI 1.065–1.381; P = .011). There was no significant impact on leadership (odds ratio: 1.016; 95% CI: 0.946–1.286; P = .209). However, there were marginal effects observed for situational awareness (odds ratio: 1.064; 95% CI: 0.992–1.365; P = .063) and for decision-making (odds ratio: 1.175; 95% CI: 0.978–1.413; P = .085).
Table 3.
Frequencies and descriptive statistics for NOTSS ratings.
| Post-Call Status* | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No (n = 201) | Yes (n = 142) | |||||||||||
| Mean | SD | 4 | 3 | 2 | 1 | Mean | SD | 4 | 3 | 2 | 1 | |
| SA† | 3.79 | 0.46 | 162 (80.6) | 35 (17.4) | 4 (2.0) | 0 (0) | 3.49 | 0.77 | 90 (63.4) | 34 (23.9) | 15 (10.6) | 3 (2.1) |
| DM‡ | 3.90 | 0.32 | 181 (90.0) | 19 (9.5) | 1 (0.5) | 0 (0) | 3.80 | 0.43 | 116 (81.7) | 24 (16.9) | 2 (1.4) | 0 (0) |
| CT‡ | 3.65 | 0.58 | 140 (69.7) | 52 (25.9) | 8 (4.0) | 1 (0.5) | 3.52 | 0.66 | 87 (61.3) | 42 (29.6) | 13 (9.2) | 0 (0) |
| LD | 3.63 | 0.61 | 138 (68.7) | 53 (26.4) | 8 (4.0) | 2 (1.0) | 3.57 | 0.61 | 90 (63.4) | 43 (30.3) | 9 (6.3) | 0 (0) |
Values presented as n (%) unless otherwise indicated. *Adjusted for resident participation and hospital site. Rating scale: 4 = good; 3 = acceptable; 2 = marginal; 1 = poor. †P < .001 non-post-call vs post-call. ‡P = .05 non-post-call vs post-call. CT = communication and teamwork, DM = decision-making, LD = leadership, NOTSS = Non-Technical Skills for Surgeons, SA = situational awareness, SD = standard deviation.
Table 4.
Frequency of “good” scores for NOTSS ratings.
| NOTSS Category* | Non-Post-Call | Post-Call | P | |||
|---|---|---|---|---|---|---|
| Count | % | Count | % | |||
| SA | 4 (Good) | 162 | 80.6 | 90 | 63.4 | <.001 |
| All Other | 39 | 11.4 | 52 | 15.2 | ||
| DM | 4 (Good) | 181 | 90.1 | 116 | 81.7 | .011 |
| All Other | 20 | 10.0 | 26 | 18.3 | ||
| CT | 4 (Good) | 140 | 69.7 | 87 | 61.3 | .043 |
| All Other | 61 | 30.3 | 55 | 38.7 | ||
| LD | 4 (Good) | 138 | 68.7 | 90 | 63.4 | .158 |
| All Other | 63 | 31.3 | 52 | 36.6 | ||
Rating scale: 4 = good; 3 = acceptable; 2 = marginal; 1 = poor. CT = communication and teamwork, DM = decision-making, LD = leadership, NOTSS = Non-Technical Skills for Surgeons, SA = situational awareness.
Figure 2. Associations between NOTSS ratings and hours of sleep determined by sleep log.
Odds ratios (OR) represent the odds of a change in rating category per hour of sleep. OR values are greater than 1, indicating that increase in sleep was related to higher NOTSS ratings. Adjusted models were adjusted for resident participation, hospital site, and operating room environmental events. CI = confidence interval, NOTSS = Non-Technical Skills for Surgeons.
Mean operative procedure time (time from incision to extubation) was 68.8 ± 48.4 minutes. Resident participation was associated with a nonstatistically significant longer operative time (75.4 ± 47.8 vs 67.3 ± 48.4 minutes; P = .251). As shown in Table 5, there was no impact of hours of sleep, sleep quality, or number of awakenings on operative procedure time. However, decreasing self-reported alertness was associated with an increase in operative time in unadjusted analyses as well as after adjustment for resident participation and hospital site. Secondary analyses indicated that this finding resulted primarily from vascular procedures (n = 19).
Table 5.
Association of self-reported duration and quality of sleep with procedure time.
| Unadjusted | Adjusted* | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimate (b) | SE | 95% CI | P | Estimate (b) | SE | 95% CI | P | |||
| Lower | Upper | Lower | Upper | |||||||
| Hours of sleep | −0.393 | 1.651 | −3.643 | 2.856 | .812 | −1.517 | 1.489 | −4.448 | 1.413 | .309 |
| Sleep in 24 hours | −3.697 | 3.175 | −9.950 | 2.556 | .245 | −2.846 | 2.737 | −8.237 | 2.544 | .299 |
| Awakenings | −0.914 | 1.403 | −3.677 | 1.849 | .515 | −1.518 | 1.436 | −4.354 | 1.317 | .292 |
| Sleep quality | −0.114 | 0.105 | −0.320 | 0.092 | .278 | −0.161 | 0.105 | −0.368 | 0.046 | .127 |
| Alertness | −0.395 | 0.141 | −0.674 | −0.117 | .006 | −0.543 | 0.126 | −0.792 | −0.295 | <.001 |
| Vascular Procedures Excluded | ||||||||||
| Alertness | −0.286 | 0.158 | −0.597 | 0.237 | .070 | −0.078 | 0.137 | −0.349 | 0.248 | .192 |
Adjusted for resident participation, hospital site, and operating room environmental events. CI = confidence interval.
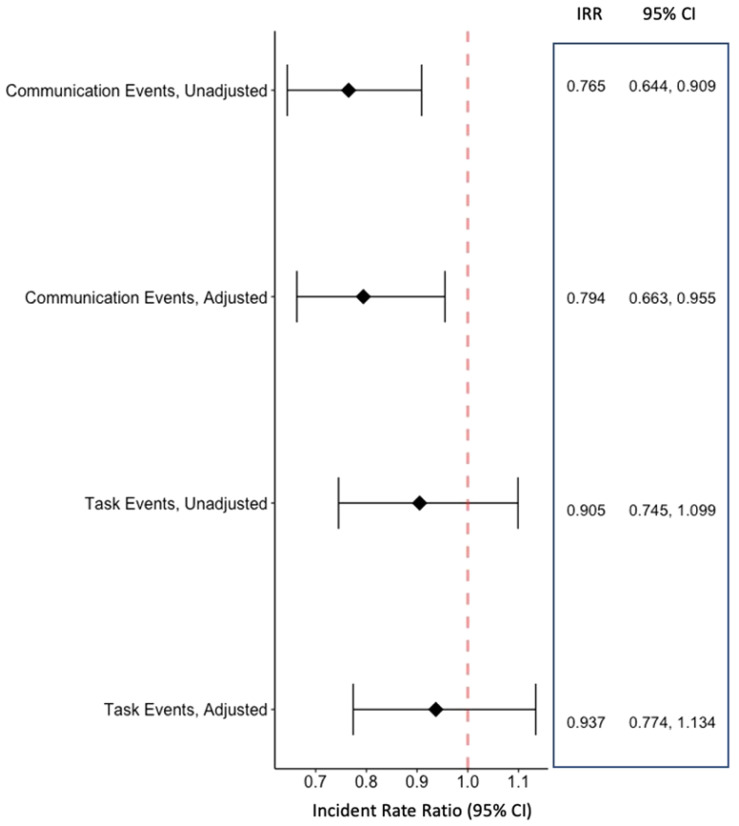
The frequency of events in the Task and Communication nonoperative event clusters stratified by post-call status is provided in Table 2. No significant differences were observed in either the Task or Communication clusters. However, as shown in Figure 3, analyses as a function of hours of sleep demonstrated that events in the Communication cluster declined as hours of sleep increased (adjusted IRR: 0.797; 95% CI: 0.666–0.953). No association with hours of sleep was observed for the Task cluster (adjusted IRR: 0.932; 95% CI: 0.763–1.138).
Figure 3. Associations between nonoperative task and communication events and hours of sleep determined by sleep log.
Incident rate ratios (IRR) represent the incident event rate per hour of sleep. IRR values are less than 1, indicating that an increasing amount of sleep was associated with a reduction in incident events. Adjusted models were adjusted for resident participation, hospital site, and operating room environmental events. CI = confidence interval.
DISCUSSION
In this study we performed a prospective assessment of attending surgeons’ operative performance after having had a night of normal sleep opportunity in comparison to a night of potentially diminished sleep as a result of being on-call. We found that although surgeons who were post-call were on average sleep-deficient, an increase in errors was not observed. However, post-call status was related to lower ratings of nontechnical surgical skills. In addition, fewer hours of sleep on the previous night were associated with an increase in operative procedure time, particularly in vascular surgery cases, and a greater number of communication issues among members of the operating room team.
After a night of being on call and performing at least 2 hours of clinical work, attending surgeons in this study experienced approximately 1.7 hours less sleep than on nights without clinical duties. This amount of sleep deficiency did not lead to a significant change in the number of errors observed during an operative procedure the following day. Several prior systematic reviews,17,18,23 a recent large cross-sectional retrospective study,19 and 2 meta-analyses have likewise found no adverse impact of surgeon fatigue on postoperative mortality or complications17,23 or post-night work percutaneous coronary interventions.24 However, most of the studies included in those reports did not seek to directly calculate sleep or sleep opportunity but instead inferred that fatigue or sleep deficiency was present based on the timing of the operative procedure (ie, day vs night) or the previous workload of the surgeon (ie, number of preceding procedures). In the only 2 studies that provided a direct assessment of sleep opportunity or sleep, 1 found an increased rate of complications in surgeons who had a sleep opportunity of less than 6 hours21 and the other found no association between postoperative complications and hours of sleep.20 In contrast, studies of predominantly nonsurgeons and resident physicians have consistently found increased rates of medical errors in those who were sleep-deficient.4–6,16 In addition, a recent systematic review found that sleep deprivation adversely affected technical skills during simulated surgical procedures, although the impact appeared less striking among attending surgeons.25
There are several explanations that could explain our inability to detect any increase in errors among surgeons who were post-call in our study as well as the absence of increased mortality or complications in prior studies. First, although the attending surgeon is “captain of the ship” and bears ultimate responsibility, in most cases surgery is conducted as a team. Other personnel such as the anesthesiologist, operating room nurses, and in many cases surgical residents also are active participants in the procedure. Their presence could have mitigated against the occurrence of adverse events. Second, it has been suggested that surgeons who are working at night preferentially schedule less complicated cases.26 Third, surgeons who are sleep-deficient may have compensated for detrimental effects of sleep loss by devoting greater attention to detail and working more slowly. If true, this type of behavior runs contrary to previous human laboratory research that has found sleep-deficient participants trade accuracy for speed when performing spatial configuration and search tasks.27,28 However, under conditions where time pressure is generally not severe, such as during most elective surgical procedures, accuracy may not necessarily be sacrificed for speed.29 Although a recent study found a small decrease in the length of operations after overnight work,19 our finding that procedure times increased as alertness decreased supports the contention that surgeons can compensate for the adverse effects of sleep deficiency in part by working more slowly. Last, the amount of sleep deficiency induced by at least 2 hours of clinical duties was approximately 1.7 hours. Nightly sleep deficiency of approximately this extent experienced over 2 weeks is associated with deficits in cognitive performance, but there is little impairment after a single night.30 Thus, if the attending surgeons in this study did not have a significant chronic sleep debt this amount of sleep loss after a night of being on call may have been inadequate to produce significant deterioration in surgical performance.
We did find a positive association between hours of sleep as well as non-post-call status and ratings on nontechnical surgical skills. Situational awareness, decision-making, and communication/teamwork, but not leadership, improved with greater amounts of sleep and non-post-call status as documented by the NOTSS instrument. The positive relationship between the communication/teamwork component of the NOTSS and greater amounts of sleep was corroborated by our observation that the number of disruptive communication events increased as hours of sleep decreased. Collectively, these observations are consistent with the known adverse effects of sleep deficiency on attention, working memory, judgment, and mood.1,8,31
There is increasing recognition that nontechnical surgical skills are an important component of effective surgical performance.8,32–34 Deficiencies in these skills, particularly communication issues, have been implicated as causal factors in retrospective studies of adverse surgical events.35–37 Most prospective studies assessing nontechnical surgical skills have been performed during simulated surgical procedures.33 Observations in the operating room have been more limited.38–43 These studies noting poorer ratings of situational awareness were associated with an increase in errors38,40 and communication issues were related to near-miss events,41 errors,39,43 blood loss, and longer operative time.42 However, none of these previous studies have linked lower ratings of nontechnical surgical skills with less sleep. Our results extend these prior studies by documenting that sleep deficiency is an important causal factor leading to worse behavior related to nontechnical surgical skills.
There are several caveats to our findings. First, our initial power analyses and sample size calculations were predicated on the occurrence of a larger number of errors than were observed in the study. Therefore, our power to detect modest differences in errors rates was limited. It is possible that a larger study would have been more informative. In addition, although the independent observers were present in the operating room they were not “scrubbed in.” They did not always have visual access to the surgical field; consequently, the number of errors detected was partially dependent on the extent to which errors were discussed in the operating room in front of observers. Furthermore, although 1 of the independent observers was a physician, he/she was not a surgeon and therefore subtle clinical errors may have been missed. Consequently, there is the potential that errors were undercounted. Second, although we did not find an increase in the number of errors as a result of sleep deficiency, surgical case heterogeneity may have created negative bias. We observed surgical performance over a broad range of procedures. They ranged from those that were straightforward such as an inguinal hernia repair to those that were more complex such as removal of an abdominal aortic aneurysm. However, we did not find any association between the type of operative procedure and errors, which makes this explanation less tenable. Third, residents were members of the operative team in some cases. Thus, it is possible that our results do not entirely reflect the performance of the surgical attending; errors may be greater in a teaching environment.36 However, adjustment for resident participation in our analyses did not materially affect our findings. Fourth, clinical characteristics of the patient were not recorded. It is possible that residual confounding from factors other than sleep deficiency such as age or the presence of obesity could have affected our findings. Last, some of the outcomes reported in this study were self-reported, which may have resulted in greater data heterogeneity. However, in a recent simulation study of surgical skills after a night of call, objective and self-reported assessments of sleepiness were similar.44 This suggests that our self-reported outcomes were reasonable surrogates for objective measures.
Despite the aforementioned limitations, our study has several strengths. In contrast to most previous studies of sleep deficiency, we performed a prospective assessment of surgical performance using trained independent observers. Importantly, our assessment of sleep used sleep logs, which have been validated against polysomnography in a related type of field study.45 Three hundred sixty-two procedures comprising a broad spectrum of different types were evaluated. To our knowledge, this is the largest prospective study of the impact of sleep deficiency on surgical performance to date. We also used a well-validated method of assessing nonsurgical technical skills, thus minimizing variability in evaluations among the cases and observers.46–48
In summary, sleep deficiency in attending surgeons was not associated with an increase in errors during procedures performed during the next day in this study. However, procedure time was increased, suggesting that surgeons were able to compensate for sleep loss by working more slowly. Ratings on nontechnical surgical skills were adversely affected by sleep deficiency, and communication events were more common with sleep deficiency. Additional studies in larger cohorts are needed to assess the ramifications of this observation.
DISCLOSURE STATEMENT
This study was supported by HL095472 (Dr. Czeisler), 1K01HL150339 (Dr. Robbins), R56HL151637-01 (Dr. Weaver), and R01OH011773 (Dr. Barger). Dr. Landrigan has consulted with and holds equity in the I-PASS Institute, which seeks to train institutions in best handoff practices and aid in their implementation. He has consulted with the Missouri Hospital Association/Executive Speaker’s Bureau regarding I-PASS. In addition, Dr. Landrigan has received monetary awards, honoraria, and travel reimbursement from multiple academic and professional organizations for teaching and consulting on sleep deprivation, physician performance, handoffs, and safety and has served as an expert witness in cases regarding patient safety and sleep deprivation. Dr. Weaver reports consulting fees from the National Sleep Foundation and the University of Pittsburgh. Dr. Barger reports consulting fees from Puget Sound Pilots and Boston Children’s Hospital. Dr. Robbins reports personal fees from SleepCycle AB; Rituals Cosmetics BV; Denihan Hospitality Group, LLC; AdventHealth; and With Deep, LLC. Dr. Quan has served as a consultant for Best Doctors, Bryte Foundation, Jazz Pharmaceuticals, and Whispersom. Dr. Barger reports personal fees from Boston Children’s Hospital, University of Helsinki, and the AAA Foundation. Dr. Czeisler reports grants and contracts to Brigham and Women’s Hospital from Dayzz Live Well, Delta Airlines, Jazz Pharma, Puget Sound Pilots, Regeneron Pharmaceuticals/Sanofi; is/was paid consultant/speaker for Inselspital Bern, Institute of Digital Media and Child Development, Klarman Family Foundation, M. Davis and Co, National Council for Mental Wellbeing, National Sleep Foundation, Physician’s Seal, SRS Foundation, State of Washington Board of Pilotage Commissioners, Tencent, Teva Pharma Australia, With Deep, and Vanda Pharmaceuticals, in which Dr. Czeisler holds an equity interest; received travel support from Aspen Brain Institute, Bloomage International Investment Group, Inc., Dr. Stanley Ho Medical Development Foundation, German National Academy of Sciences, Ludwig-Maximilians-Universität München, National Highway Transportation Safety Administration, National Safety Council, National Sleep Foundation, Salk Institute for Biological Studies/Foundation Ipsen, Society for Research on Biological Rhythms, Stanford Medical School Alumni Association, Tencent Holdings, Ltd, and Vanda Pharmaceuticals; receives research/education gifts through Brigham and Women’s Hospital from Arbor Pharmaceuticals, Avadel Pharmaceuticals, Bryte, Alexandra Drane, Cephalon, DR Capital Ltd, Eisai, Harmony Biosciences, Jazz Pharmaceuticals, Johnson & Johnson, Mary Ann & Stanley Snider via Combined Jewish Philanthropies, NeuroCare, Inc., Optum, Philips Respironics, Regeneron, Regional Home Care, ResMed, Resnick Foundation (The Wonderful Company), San Francisco Bar Pilots, Sanofi SA, Schneider, Simmons, Sleep Cycle AB, Sleep Number, Sysco, Teva Pharmaceuticals, Vanda Pharmaceuticals; is/was an expert witness in legal cases, including those involving Advanced Power Technologies, Aegis Chemical Solutions, Amtrak; Casper Sleep Inc, C&J Energy Services, Catapult Energy Services Group, Covenant Testing Technologies, Dallas Police Association, Enterprise Rent-A-Car, Espinal Trucking/Eagle Transport Group/Steel Warehouse Inc, FedEx, Greyhound, Pomerado Hospital/Palomar Health District, PAR Electrical Contractors, Product & Logistics Services LLC/Schlumberger Technology, Puckett EMS, Puget Sound Pilots, Union Pacific Railroad, UPS, and Vanda Pharmaceuticals; serves as the incumbent of an endowed professorship given to Harvard by Cephalon; and receives royalties from McGraw Hill and Philips Respironics for the Actiwatch-2 and Actiwatch Spectrum devices. Dr. Czeisler’s interests were reviewed and are managed by the Brigham and Women’s Hospital and Mass General Brigham in accordance with their conflict-of-interest policies.
ACKNOWLEDGMENTS
Author contributions: concept and design: C.P.L., C.A.C., C.D., E.L.P.; data collection: J.D.B., A.M., B.H.S., J.T.S.; data analysis and interpretation: S.F.Q., M.D.W.; drafting of manuscript: S.F.Q., C.P.L.; critical feedback and revision of manuscript: L.K.B., C.D., E.L.P., R.R., C.A.C., C.P.L., S.F.Q.
ABBREVIATIONS
- CI
confidence interval
- IRR
incident rate ratio
- NOTSS
Non-Technical Skills for Surgeons
REFERENCES
- 1. Chattu VK , Manzar MD , Kumary S , Burman D , Spence DW , Pandi-Perumal SR . The global problem of insufficient sleep and its serious public health implications . Healthcare (Basel). 2018. ; 7 ( 1 ): 1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sheehan CM , Frochen SE , Walsemann KM , Ailshire JA . Are U.S. adults reporting less sleep?: findings from sleep duration trends in the National Health Interview Survey, 2004-2017 . Sleep. 2019. ; 42 ( 2 ): zsy221 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Quan SF , Barger LK . Brief review: sleep health and safety for transportation workers . Southwest J Pulm Crit Care. 2015. ; 10 ( 3 ): 130 – 139 . [Google Scholar]
- 4. Trockel MT , Menon NK , Rowe SG , et al . Assessment of physician sleep and wellness, burnout, and clinically significant medical errors . JAMA Netw Open. 2020. ; 3 ( 12 ): e2028111 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Barger LK , Ayas NT , Cade BE , et al . Impact of extended-duration shifts on medical errors, adverse events, and attentional failures . PLoS Med. 2006. ; 3 ( 12 ): e487 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. West CP , Tan AD , Habermann TM , Sloan JA , Shanafelt TD . Association of resident fatigue and distress with perceived medical errors . JAMA. 2009. ; 302 ( 12 ): 1294 – 1300 . [DOI] [PubMed] [Google Scholar]
- 7. Basner M , Dinges DF , Shea JA , et al . Sleep and alertness in medical interns and residents: an observational study on the role of extended shifts . Sleep. 2017. ; 40 ( 4 ): zsx027 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sugden C , Athanasiou T , Darzi A . What are the effects of sleep deprivation and fatigue in surgical practice? Semin Thorac Cardiovasc Surg. 2012. ; 24 ( 3 ): 166 – 175 . [DOI] [PubMed] [Google Scholar]
- 9. Ellman PI , Kron IL , Alvis JS , et al . Acute sleep deprivation in the thoracic surgical resident does not affect operative outcomes . Ann Thorac Surg. 2005. ; 80 ( 1 ): 60 – 64, discussion 64–65 . [DOI] [PubMed] [Google Scholar]
- 10. Ellman PI , Law MG , Tache-Leon C , et al . Sleep deprivation does not affect operative results in cardiac surgery . Ann Thorac Surg. 2004. ; 78 ( 3 ): 906 – 911 , discussion 906-911. [DOI] [PubMed] [Google Scholar]
- 11. Simpson AM , Kwok AC , Collier WH , Kim J , Veith J , Agarwal JP . 2011 ACGME duty hour limits had no association with breast reconstruction complications . J Surg Res. 2020. ; 247 : 469 – 478 . [DOI] [PubMed] [Google Scholar]
- 12. Oliver JB , Kunac A , McFarlane JL , Anjaria DJ . Association between operative autonomy of surgical residents and patient outcomes . JAMA Surg. 2022. ; 157 ( 3 ): 211 – 219 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kunac A , Oliver JB , McFarlane JL , Anjaria DJ . General surgical resident operative autonomy vs patient outcomes: are we compromising training without net benefit to hospitals or patients? J Surg Educ. 2021. ; 78 ( 6 ): e174 – e182 . [DOI] [PubMed] [Google Scholar]
- 14. Itani KMF , DePalma RG , Schifftner T , et al . Surgical resident supervision in the operating room and outcomes of care in Veterans Affairs hospitals . Am J Surg. 2005. ; 190 ( 5 ): 725 – 731 . [DOI] [PubMed] [Google Scholar]
- 15. Anim M , Markert RJ , Wood VC , Schuster BL . Physician practice patterns resemble ACGME duty hours . Am J Med. 2009. ; 122 ( 6 ): 587 – 593 . [DOI] [PubMed] [Google Scholar]
- 16. Chen I , Vorona R , Chiu R , Ware JC . A survey of subjective sleepiness and consequences in attending physicians . Behav Sleep Med. 2008. ; 6 ( 1 ): 1 – 15 . [DOI] [PubMed] [Google Scholar]
- 17. Koda N , Oshima Y , Koda K , Shimada H . Surgeon fatigue does not affect surgical outcomes: a systematic review and meta-analysis . Surg Today. 2021. ; 51 ( 5 ): 659 – 668 . [DOI] [PubMed] [Google Scholar]
- 18. Gates M , Wingert A , Featherstone R , Samuels C , Simon C , Dyson MP . Impact of fatigue and insufficient sleep on physician and patient outcomes: a systematic review . BMJ Open. 2018. ; 8 ( 9 ): e021967 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sun EC , Mello MM , Vaughn MT , et al . Assessment of perioperative outcomes among surgeons who operated the night before . JAMA Intern Med. 2022. ; 182 ( 7 ): 720 – 728 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chu MWA , Stitt LW , Fox SA , et al . Prospective evaluation of consultant surgeon sleep deprivation and outcomes in more than 4000 consecutive cardiac surgical procedures . Arch Surg. 2011. ; 146 ( 9 ): 1080 – 1085 . [DOI] [PubMed] [Google Scholar]
- 21. Rothschild JM , Keohane CA , Rogers S , et al . Risks of complications by attending physicians after performing nighttime procedures . JAMA. 2009. ; 302 ( 14 ): 1565 – 1572 . [DOI] [PubMed] [Google Scholar]
- 22. University of Aberdeen . The Non-Technical Skills for Surgeons (NOTSS) System Handbook v1.2 [published online June 2012]. https://research.abdn.ac.uk/wp-content/uploads/sites/14/2019/03/NOTSS-Handbook-2012.pdf ; Accessed on February 24, 2022. .
- 23. Guan G , Cheng Z , Yin J , et al . Daytime versus after-hours surgery outcomes in hip fracture patients: a systematic review and meta-analysis . Aging Clin Exp Res. 2020. ; 32 ( 12 ): 2427 – 2438 . [DOI] [PubMed] [Google Scholar]
- 24. Aronow HD , Gurm HS , Blankenship JC , et al . Middle-of-the-night percutaneous coronary intervention and its association with percutaneous coronary intervention outcomes performed the following day: an analysis from the National Cardiovascular Data Registry . JACC Cardiovasc Interv. 2015. ; 8 ( 1, 1 Pt A ): 49 – 56 . [DOI] [PubMed] [Google Scholar]
- 25. Whelehan DF , McCarrick CA , Ridgway PF . A systematic review of sleep deprivation and technical skill in surgery . Surgeon. 2020. ; 18 ( 6 ): 375 – 384 . [DOI] [PubMed] [Google Scholar]
- 26. Leya GA , Feldman ZM , Chang DC . Are surgeons really more resilient than athletes?: the trade-off between surgeon outcomes and surgeon well-being . JAMA Intern Med. 2022. ; 182 ( 7 ): 728 – 729 . [DOI] [PubMed] [Google Scholar]
- 27. Horowitz TS , Cade BE , Wolfe JM , Czeisler CA . Searching night and day: a dissociation of effects of circadian phase and time awake on visual selective attention and vigilance . Psychol Sci. 2003. ; 14 ( 6 ): 549 – 557 . [DOI] [PubMed] [Google Scholar]
- 28. Santhi N , Horowitz TS , Duffy JF , Czeisler CA . Acute sleep deprivation and circadian misalignment associated with transition onto the first night of work impairs visual selective attention . PLoS One. 2007. ; 2 ( 11 ): e1233 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hudson AN , Hansen DA , Hinson JM , et al . Speed/accuracy trade-off in the effects of acute total sleep deprivation on a sustained attention and response inhibition task . Chronobiol Int. 2020. ; 37 ( 9-10 ): 1441 – 1444 . [DOI] [PubMed] [Google Scholar]
- 30. Van Dongen HPA , Maislin G , Mullington JM , Dinges DF . The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation . Sleep. 2003. ; 26 ( 2 ): 117 – 126 . [DOI] [PubMed] [Google Scholar]
- 31. Banks S , Dinges DF . Behavioral and physiological consequences of sleep restriction . J Clin Sleep Med. 2007. ; 3 ( 5 ): 519 – 528 . [PMC free article] [PubMed] [Google Scholar]
- 32. Agha RA , Fowler AJ , Sevdalis N . The role of non-technical skills in surgery . Ann Med Surg . 2015. ; 4 ( 4 ): 422 – 427 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hull L , Arora S , Aggarwal R , Darzi A , Vincent C , Sevdalis N . The impact of nontechnical skills on technical performance in surgery: a systematic review . J Am Coll Surg. 2012. ; 214 ( 2 ): 214 – 230 . [DOI] [PubMed] [Google Scholar]
- 34. Yule S , Flin R , Paterson-Brown S , Maran N . Non-technical skills for surgeons in the operating room: a review of the literature . Surgery. 2006. ; 139 ( 2 ): 140 – 149 . [DOI] [PubMed] [Google Scholar]
- 35. Greenberg CC , Regenbogen SE , Studdert DM , et al . Patterns of communication breakdowns resulting in injury to surgical patients . J Am Coll Surg. 2007. ; 204 ( 4 ): 533 – 540 . [DOI] [PubMed] [Google Scholar]
- 36. Gawande AA , Zinner MJ , Studdert DM , Brennan TA . Analysis of errors reported by surgeons at three teaching hospitals . Surgery. 2003. ; 133 ( 6 ): 614 – 621 . [DOI] [PubMed] [Google Scholar]
- 37. Rogers SO Jr , Gawande AA , Kwaan M , et al . Analysis of surgical errors in closed malpractice claims at 4 liability insurers . Surgery. 2006. ; 140 ( 1 ): 25 – 33 . [DOI] [PubMed] [Google Scholar]
- 38. Catchpole K , Mishra A , Handa A , McCulloch P . Teamwork and error in the operating room: analysis of skills and roles . Ann Surg. 2008. ; 247 ( 4 ): 699 – 706 . [DOI] [PubMed] [Google Scholar]
- 39. ElBardissi AW , Wiegmann DA , Henrickson S , Wadhera R , Sundt TM 3rd . Identifying methods to improve heart surgery: an operative approach and strategy for implementation on an organizational level . Eur J Cardiothorac Surg. 2008. ; 34 ( 5 ): 1027 – 1033 . [DOI] [PubMed] [Google Scholar]
- 40. Mishra A , Catchpole K , Dale T , McCulloch P . The influence of non-technical performance on technical outcome in laparoscopic cholecystectomy . Surg Endosc. 2008. ; 22 ( 1 ): 68 – 73 . [DOI] [PubMed] [Google Scholar]
- 41. Manuguerra A , Mazeaud C , Hubert N , et al . Non-technical skills in robotic surgery and impact on near-miss events: a multi-center study . Surg Endosc. 2021. ; 35 ( 9 ): 5062 – 5071 . [DOI] [PubMed] [Google Scholar]
- 42. Schiff L , Tsafrir Z , Aoun J , Taylor A , Theoharis E , Eisenstein D . Quality of communication in robotic surgery and surgical outcomes . JSLS. 2016. ; 20 ( 3 ): e2016.00026 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wiegmann DA , ElBardissi AW , Dearani JA , Daly RC , Sundt TM 3rd . Disruptions in surgical flow and their relationship to surgical errors: an exploratory investigation . Surgery. 2007. ; 142 ( 5 ): 658 – 665 . [DOI] [PubMed] [Google Scholar]
- 44. Whelehan DF , Alexander M , Connelly TM , McEvoy C , Ridgway PF . Sleepy surgeons: a multi-method assessment of sleep deprivation and performance in surgery . J Surg Res. 2021. ; 268 : 145 – 157 . [DOI] [PubMed] [Google Scholar]
- 45. Lockley SW , Cronin JW , Evans EE , et al. Harvard Work Hours, Health and Safety Group . Effect of reducing interns’ weekly work hours on sleep and attentional failures . N Engl J Med. 2004. ; 351 ( 18 ): 1829 – 1837 . [DOI] [PubMed] [Google Scholar]
- 46. Crossley J , Marriott J , Purdie H , Beard JD . Prospective observational study to evaluate NOTSS (Non-Technical Skills for Surgeons) for assessing trainees’ non-technical performance in the operating theatre . Br J Surg. 2011. ; 98 ( 7 ): 1010 – 1020 . [DOI] [PubMed] [Google Scholar]
- 47. Yule S , Flin R , Maran N , Rowley D , Youngson G , Paterson-Brown S . Surgeons’ non-technical skills in the operating room: reliability testing of the NOTSS behavior rating system . World J Surg. 2008. ; 32 ( 4 ): 548 – 556 . [DOI] [PubMed] [Google Scholar]
- 48. Yule S , Rowley D , Flin R , et al . Experience matters: comparing novice and expert ratings of non-technical skills using the NOTSS system . ANZ J Surg. 2009. ; 79 ( 3 ): 154 – 160 . [DOI] [PubMed] [Google Scholar]