Abstract
Study Objectives:
The lifestyles change of children and adolescents during the COVID-19 pandemic due to antipandemic measures can affect their sleep health. Existing studies have used convenient samples and focused on the initial months of the pandemic, leaving a knowledge gap on changes in young people’s sleep patterns under the “new normal” under COVID-19.
Methods:
As part of a territory-wide epidemiological study in Hong Kong, this cross-sectional study recruited primary and secondary school students by stratified random sampling. Sleep parameters were collected using the structured diagnostic interview for sleep patterns and disorders. We investigated the pandemic’s effects on sleep parameters by comparing data of participants recruited pre-COVID and those recruited during COVID using multivariate regression, adjusting for age, sex, household income, seasonality, and presence of mental disorders, and the moderators and mediators of the effects.
Results:
Between September 1, 2019 and June 2, 2021, 791 primary and 442 secondary school students were recruited and analyzed. Primary school and secondary school participants assessed before COVID had a longer sleep latency on school days (95% confidence interval [CI] = 1.0–5.2 minutes, adjusted P-value = .010; and 95% CI= 3.9–13.0 minutes, adjusted P-value = .004, respectively) and nonschool days (95% CI = 1.7–7.2 minutes, adjusted P-value = .005; 95% CI = 3.4–13.7 minutes, adjusted P-value = .014, respectively). Low household income was a moderator for later bedtime (adjusted P-value = .032) and later sleep onset (adjusted P-value = .043) during nonschool days among secondary school students.
Conclusions:
Changes associated with COVID have a widespread and enduring effect on the sleep health of school-aged students in Hong Kong. Household income plays a role in adolescent sleep health resilience, and the impact of antiepidemic measures on the health gaps of the youth should be considered.
Citation:
Chau SWH, Hussain S, Chan SSM, et al. A comparison of sleep-wake patterns among school-age children and adolescents in Hong Kong before and during the COVID-19 pandemic. J Clin Sleep Med. 2023;19(4):749–757.
Keywords: sleep health, pandemic, epidemiology, children, adolescents
BRIEF SUMMARY
Current Knowledge/Study Rationale: Existing studies reported a high rate of sleep problems among children and adolescents during the initial few months of the COVID-19 pandemic. However, the methodological limitations of these studies, in particular the convenience sampling method commonly employed, introduced bias and compromised the level of certainty of this evidence.
Study Impact: To the best of our knowledge, this is the first study that used a school-based, stratified random sampling method to study the shift in sleep patterns of school-aged children and adolescents. The moderating effect of household income on circadian disruption among adolescents should alert us to the socioeconomic determinants of health outcomes during the pandemic, even in a population without a high rate of COVID infection.
INTRODUCTION
The world has now lived with the COVID-19 pandemic for over 2 years. While children and adolescents may not be the worst-hit by direct COVID-19 related health problems due to the generally milder disease severity among this population, if infected1 they experience indirect effects on their lifestyles due to widespread school suspensions, home confinement, and reduced accessibility to health care and social resources. In March 2021, UNICEF estimated that 168 million children could not attend school for 1 year.2 A wide range of health problems have been rising among children and adolescents globally due to such disruptions.3,4 Sleep health, an essential aspect of health, is sensitive to lifestyle changes. The sleep-wake patterns of young individuals are highly affected by their daytime activity routines, school schedules, and the lifestyles of their parents.5 Disruptions of sleep and circadian rhythms in the younger population have significant physical and mental health implications.6 For example, insomnia is independently associated with an increased risk of a wide range of emotional and behavioral problems, such as depression, anxiety, daytime sleepiness, and suicidality among adolescents.7,8 Delayed sleep preference is associated with a wide range of physical, psychological, and behavioral problems among young people, such as depression, substance use,9 and adverse endocrine and physical profiles.10,11 Evidence from prospective cohort studies suggests that poor sleep and circadian health could be the precursor for at least some of these adverse outcomes.9,12 Therefore, it is important to examine changes in sleep and circadian parameters during the COVID-19 pandemic and identify biopsychosocial risk factors in order to more precisely formulate preventive public health measures. A meta-analysis of 9 studies estimated that up to 54% of school-aged youths experienced sleep problems during the early stages of the pandemic.13 However, existing studies were limited by methodological concerns such as the use of convenient sampling methods and retrospective recalls, making them prone to biases. Second, these studies only covered the first few months of the pandemic, and an updated investigation would be a more timely reflection of the “new normal” of living with the pandemic as it lingers on. Third, previous studies did not set out to identify factors moderating the effect of the COVID-19 pandemic on young people’s sleep health.
Biological sex is 1 of the factors that potentially moderates the effect of pandemic-associated changes in young people, since it is known that insomnia is more common among females than males after puberty.14 Another potential moderating factor is household income. Low household income is a predictor of poorer health outcomes for young people.15 During the pandemic, socioeconomic status was repeatedly shown to be a key determinant for various infection risks and infection outcomes worldwide, including in Hong Kong.16 For young people specifically, school closures and social restrictions are likely to cause more activity limitations for those with fewer financial resources.17
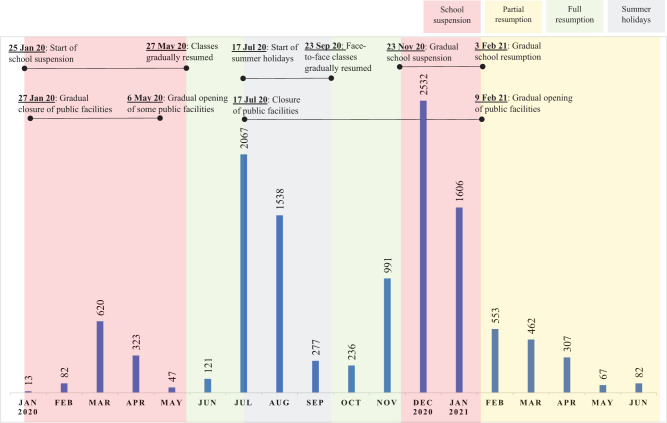
Hong Kong was spared mass casualties from COVID-19 and avoided a hard lockdown (until the recent 2022 surge due to the Omicron variant). However, prolonged and stringent social distancing measures and school suspensions have been in place over the most of the period between early 2020 and mid-2021 (Figure 1). Some of these measures directly affected school-age children and adolescents, in particular the year-long school suspension and the adoption of online home learning. There were concerns that these changes would disrupt the lifestyles of children and adolescents, and consequently threaten their health, including sleep health. These changes may also lead to an increase in digital leisure time, exacerbating sleep problems.18
Figure 1. Timeline of antipandemic measures from January 2020 to June 2021 in Hong Kong.
Bar charts and numbers represent the total number of confirmed COVID-19 cases of the month.
The “Let’s Work Heart” project is a territory-wide epidemiological study of mental, sleep, and behavioral health among primary and secondary school students in Hong Kong. The study began in 2019 (ie, prior to the pandemic) and is ongoing. The study’s timeframe thus provides a natural opportunity to compare the sleep-wake patterns in a representative sample of school-age children and adolescents in Hong Kong between the pre-COVID and COVID periods. In this substudy, we asked 3 questions: (1) Are there differences in sleep-wake patterns among school students during COVID compared to the pre-COVID period; (2) Are the differences in these patterns, if any, different between primary and secondary school students; (3) Do socio-demographics moderate the differences in sleep parameters before and during COVID, if any; and (4) Does change in the amount of digital leisure time mediate the differences in sleep parameters before and during COVID, if any.
METHODS
This was a cross-sectional study.
Participants
The inclusion criteria were students aged 6–17 years from any mainstream primary school and secondary school in Hong Kong where school enrollment in this age group is universal.19 No exclusion criteria were applied. The study adopted a 2-stage random sampling method. Schools were first randomly selected using stratified sampling. Within each participating school, every 1 out of 7 students was then randomly selected. Written parental consent was obtained from all student participants. The study was approved by the Joint Chinese University of Hong Kong–New Territories East Cluster Clinical Research Ethics Committee (Ref. no: 2018.497).
Measures
We recorded demographic and socioeconomic data from participants’ households, including household size and household income. Students’ electronic media use was assessed by the Media Activity Form.20 For primary school student participants, 1 of their parents (or the primary caregiver) was interviewed by trained research staff to determine the presence of lifetime sleep disorders using the Structured Diagnostic Interview for Sleep Patterns and Disorders,21 which was slightly modified to better correlate with the diagnostic criteria from the Third edition of the International Classification of Sleep Disorders. For this study, we used the sleep-wake parameters of the student participant during school days and nonschool days in the past month captured by the Structured Diagnostic Interview for Sleep Patterns and Disorders. The sleep parameters we investigated were bedtime, sleep latency, sleep onset time, wake-up time, sleep duration, and sleep midpoint of school days and nonschool days, and social jetlag (ie, the difference in sleep midpoint between school days and nonschool days). They were also interviewed to determine the presence of psychiatric disorders as defined by the Fifth version of the Diagnostic and Statistical Manual (DSM-5) in the past 12 months using the Diagnostic Interview Schedule for Children, fifth version (DISC-5). For secondary school participants, interviews for sleep patterns were conducted with the students themselves, and a multi-informant approach was used for diagnostic interviews for mental disorders.22 All interviews took place at the participants’ schools in the pre-COVID phase, while video-conferencing was used during the COVID phase.
Statistical analyses
Data from primary and secondary school students were analyzed separately due to significant differences in school-related factors. Participants with missing sleep parameters were excluded from the analysis. Other missing variables were imputed using median values of the whole data pool. We performed univariate analyses for differences in sleep parameters between participants assessed in the pre-COVID and COVID periods using independent t tests to select sleep parameters of interest for multivariate analyses (criteria set as P < .1). We used March 1, 2020 as a boundary for the pre-COVID and COVID periods, as the first school suspension in the city started at the end of January 2020 (no interviews were conducted between February 6, 2020 to March 4, 2020) (Table S1 (1,007.3KB, pdf) in the supplemental material). We then used multivariate general linear models to compute the adjusted regression coefficient of the assessment period as a predictor of the differences in the selected sleep parameters of interest, controlling for the potential confounders of age, sex, seasonality (summer/winter/others), income status (low income/middle-to-high income), and presence of any mental disorder. We also reported the more conservative adjusted P-value using the Holm-Sidak method of multiple hypothesis-testing corrections. To examine the moderating effects of biological sex and household income status, the multivariate general linear models were tested again with interaction terms added. To examine the mediating effect of the amount of digital leisure time, we followed the method described by Baron and Kenny.23 The participants’ amount of digital leisure time was retrieved from the Media Activity Form (excluding educational use of digital media). Since the digital leisure time measure was highly skewed, we performed a log-transformation on this data before proceeding with further analysis.
RESULTS
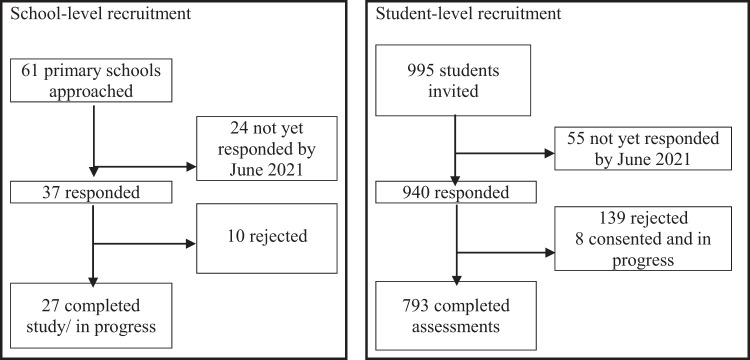
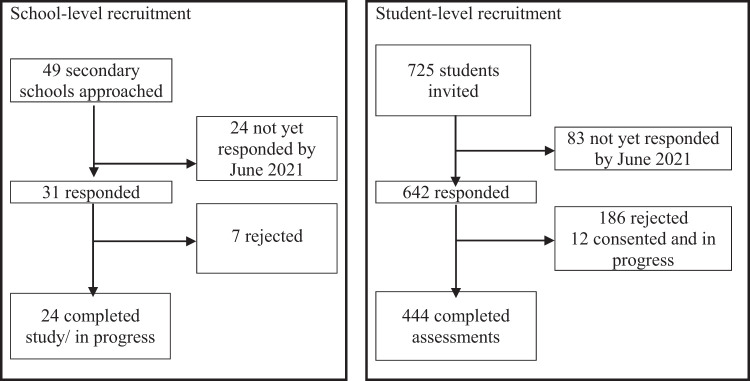
Over the period from September 1, 2019 to June 2, 2021 (ie, over 2 academic years), we recruited and assessed 793 primary school students and 444 secondary school students. The overall school-level response rate in the specified period was 75.0%, and the student-level response rate was 79.5% (recruitment flowcharts in Figure 2 and Figure 3) . Please see Table S1 (1,007.3KB, pdf) for month-by-month recruitment numbers.
Figure 2. Recruitment flowchart of primary school student participants.
Figure 3. Recruitment flowchart of secondary school student participants.
Sample characteristics
Among the primary school students, the mean age was 8.7 years (range = 6–13), and 49.5% were female. The assessments of 247 students were conducted pre-COVID (ie, before March 1, 2020), and 546 were conducted during the COVID period. Two were excluded for invalid data (1 was evaluated in the pre-COVID period and another in the COVID period); hence, the total analyzed sample size was 791. The pre-COVID and COVID period samples were comparable in age, sex, school type, and proportion of low-income households (defined as falling below 50% of the median Hong Kong household income of households of the same size, using data from the fourth quarter of 2020) (Census and Statistics Department, Hong Kong Special Administrative Region), but not in terms of the season at the time of assessment and the presence of any mental disorder as defined by the DSM-5 (Table 1).
Table 1.
Comparison of characteristics of primary school student participants recruited pre- and during COVID.
| Pre-COVID (n = 246) | COVID (n = 545) | P | |
|---|---|---|---|
| Age, years, mean (SD) | 8.5 (1.7) | 8.8 (1.8) | .05 |
| Female, n (%) | 120 (48%) | 272 (50%) | .75 |
| Government-subsidized school, n (%) | 246 (100%) | 545 (100%) | 1 |
| Low-income household, n (%) | 71 (28.9%) | 136 (25.0%) | .25 |
| Season at the time of assessment: | < .001 | ||
| Spring (Mar–Apr), n (%) | 0 (0%) | 79 (14.5%) | |
| Summer (May–Sept), n (%) | 34 (13.8%) | 158 (29.0%) | |
| Autumn (Oct–Nov), n (%) | 31 (12.6%) | 110 (20.2%) | |
| Winter (Dec–Feb), n (%) | 181 (73.6%) | 198 (36.3%) | |
| Any mental disorder, n (%) | 84 (34.1%) | 219 (40.1%) | .027 |
SD = standard deviation.
Among the secondary school students, the mean age was 14.1 years (range = 11–17), and 43.7% were female. We assessed 230 of them pre-COVID, and 214 were evaluated during the COVID period. Two were excluded for invalid data (both were assessed during the COVID period). Thus, the number of analyzed samples was 442. The pre-COVID and COVID period samples matched in school type and frequency of mental disorder, but not in age, sex, proportion of low-income households and season at the time of assessment (see Table 2). Please see Figure S1 (1,007.3KB, pdf) for a summary of the number of missing data of all variables involved in the analysis and Figure S2 (1,007.3KB, pdf) for a detailed breakdown of the frequency of the categories of mental disorders captured in the sample.
Table 2.
Comparison of characteristics of secondary school student participants recruited pre- and during COVID.
| Demographics | Pre-COVID (n = 230) | COVID (n = 212) | P |
|---|---|---|---|
| Age, years, mean (SD) | 13.9 (1.8) | 14.3 (1.7) | .045 |
| Female, n (%) | 111 (48%) | 82 (39%) | .042 |
| Government-subsidized school, n (%) | 230 (100%) | 212 (100%) | 1 |
| Low-income household*, n (%) | 58 (25.2%) | 80 (37.7%) | .005 |
| Season at the time of assessment: | < .001 | ||
| Spring (Mar–Apr), n (%) | 0 (0%) | 40 (18.9%) | |
| Summer (May–Sept), n (%) | 64 (27.8%) | 44 (20.8%) | |
| Autumn (Oct–Nov), n (%) | 88 (41.5%) | 19 (9.0%) | |
| Winter (Dec–Feb), n (%) | 78 (33.9%) | 109 (36.3%) | |
| Any mental disorder, n (%) | 83 (36.1%) | 73 (51.4%) | .72 |
| Digital leisure time, hours per week, median | 64.0 | 71.4 | .043 |
SD = standard deviation.
Comparison of sleep parameters before and during COVID
The univariate analysis showed that, in comparison to those assessed pre-COVID, primary school students assessed during the COVID period had significantly longer sleep latency on school days (P < .001) and nonschool days (P < .001), as well as longer sleep duration on nonschool days (P = .026) (Table 3).
Table 3.
Comparison of sleep parameters among primary school students pre- and during COVID.
| Sleep Parameters | Pre-COVID (n = 246) Mean (SD) | COVID (n = 545) Mean (SD) | P |
|---|---|---|---|
| School days | |||
| Bedtime, hh:mm | 22:08 (±45 min) | 22:09 (±51 min) | .84 |
| Sleep onset time, hh:mm | 22:22 (±47 min) | 22:27 (±51 min) | .25 |
| Sleep midpoint time, hh:mm | 2:42 (±29 min) | 2:42 (±37 min) | .94 |
| Wake up time, hh:mm | 7:01 (±37 min) | 6:57 (±25 min) | .13 |
| Sleep latency, hh:mm | 0:13 (±12 min) | 0:17 (±13 min) | < .001 |
| Sleep duration, hh:mm | 8:39 (±48 min) | 8:30 (±50 min) | .03 |
| Nonschool days | |||
| Bedtime, hh:mm | 22:56 (±53 min) | 22:55 (±61 min) | .91 |
| Sleep onset time, hh:mm | 23:12 (±56 min) | 23:17 (±62 min) | .31 |
| Sleep midpoint time, hh:mm | 3:59 (±56 min) | 4:06 (±60 min) | .17 |
| Wake up time, hh:mm | 8:47 (±70 min) | 8:55 (±74 min) | .17 |
| Sleep latency, hh:mm | 0:16 (±15 min) | 0:21 (±17 min) | < .001 |
| Sleep duration, hh:mm | 9:34 (±59 min) | 9:37 (±65 min) | .53 |
| Social jetlag, hh:mm | 1:17 (±52 min) | 1:23 (±48 min) | .11 |
SD = standard deviation.
Using a multivariate linear regression, assessment period (ie, whether the assessment was conducted in the pre-COVID or COVID period) remained a significant predictor of longer sleep latency on school days (B = 3.1 minutes, 95% confidence interval [CI] = 1.0–5.2, P = .005) and nonschool days (B = 4.4 minutes, 95% CI = 1.7–7.2, P = .002), but not of sleep duration (B = 5.9 minutes, 95% CI = −13.6 to 1.9, P = .13). After applying the Holm-Sidak correction, assessment period remained a significant predictor of longer sleep latency during both school days and nonschool days (adjusted P-values = .010 and .005, respectively).
The univariate analysis showed that secondary school students assessed during the COVID period had longer self-reported sleep latency (P < .001), later sleep onset time (P = .016), and a later sleep midpoint (P = .015) on school days, compared to their peers who were assessed pre-COVID. On nonschool days, students assessed in the COVID period reported a later bedtime (P = .006), longer sleep latency (P = .002), later sleep onset time (P < .001), later wake up time (P = .030), and a later sleep midpoint (P = .005) than their peers who were assessed pre-COVID. Social jetlag was longer among students assessed in the COVID period (P = .049) (Table 4).
Table 4.
Comparison of sleep parameters among secondary school students pre- and during COVID.
| Sleep Parameters | Pre-COVID (n = 230) Mean (SD) | COVID (n = 212) Mean (SD) | P |
|---|---|---|---|
| School days | |||
| Bedtime, hh:mm | 23:13 (±72 min) | 23:24 (±82 min) | .13 |
| Sleep onset time, hh:mm | 23:27 (±73 min) | 23:46 (±91 min) | .016 |
| Sleep midpoint time, hh:mm | 3:03 (±43 min) | 3:15 (±55 min) | .015 |
| Wake up time, hh:mm | 6:39 (±30 min) | 6:43 (±46 min) | .28 |
| Sleep latency, hh:mm | 0:14 (±12 min) | 0:22 (±31 min) | < .001 |
| Sleep duration, hh:mm | 7:11 (±70 min) | 6:56 (±94 min) | .061 |
| Nonschool days | |||
| Bedtime, hh:mm | 00:01 (±84 min) | 00:28 (±85 min) | .006 |
| Sleep onset time, hh:mm | 00:16 (±85 min) | 00:51 (±125 min) | < .001 |
| Sleep midpoint time, hh:mm | 4:41 (±81 min) | 5:05 (±100 min) | .005 |
| Wake up time, hh:mm | 9:20 (±105 min) | 9:43 (±112 min) | .030 |
| Sleep latency, hh:mm | 00:14 (±13 min) | 00:22 (±35 min) | .002 |
| Sleep duration, hh:mm | 9:03 (±102 min) | 8:51 (±105 min) | .23 |
| Social jetlag, hh:mm | 1:37 (±104 min) | 1:50 (±137 min) | .049 |
SD = standard deviation.
Using a multivariate regression model, assessment period was a significant predictor of later bedtime on nonschool days (B = 21.3 minutes, 95% CI = 2.9–39.6, P = .023), longer sleep latency on both school days (B = 8.5 minutes, 95% CI = 3.9–13.0, P < .001) and nonschool days (B = 8.6 minutes, 95% CI = 3.4–13.7, P = .001), later sleep onset on both school days (B = 17.0 minutes, 95% CI = 12.8–21.0, P = .025) and nonschool days (B = 29.8 minutes, 95% CI = 10.1–49.6, P = .0031), a later sleep midpoint on both school days (B = 10.1 minutes, 95% CI = 1.8–19.9, P = .019) and nonschool days (B = 19.5 minutes, 95% CI = 2.4–36.6, P = .025), and shorter sleep duration during school days (B = 19.5 minutes, 95% CI = 2.4–36.6, P = .019). After applying the Holm-Sidak correction, assessment period remained a significant predictor of longer sleep latency during both school days (adjusted P-value = .004) and nonschool days (adjusted P-value = .014) and later sleep onset during nonschool days (adjusted P-value = .025).
Moderators of differences in sleep parameters
For both the primary and secondary school groups, multivariate regression models containing the interaction term “assessment period × sex” did not find that the sex of the participants significantly moderated the COVID period’s predictive effect for any sleep parameters (P > .05).
Among primary school students, multivariate regression models containing the interaction term “assessment period × household income status” showed that low household income was not a significant moderator of the effect of assessment period as a predictive factor of the sleep parameters of interest (P > .05).
Among secondary school students, the same multivariate regression models showed that being assessed during the COVID period was significantly more predictive of a later bedtime (B = 56.7 minutes, 95% CI = 18.2–95.3, P = .004), later sleep onset (B = 56.7 minutes, 95% CI = 15.3–98.2, P = .0071), and later sleep midpoint (B = 37.2 minutes, 95% CI = 1.1–73.2, P = .044) during nonschool days among students from low-income households, compared to their peers from middle- to high-income families. After applying the Holm-Sidak correction, low household income remained a significant moderator for later bedtime (adjusted P-value = .032) and later sleep onset (adjusted P-value = .043) on nonschool days among secondary school students.
Digital leisure time as a mediator of differences in sleep parameters
The median weekly digital leisure time of the pre-COVID and COVID period samples of primary school students were 15.5 hours and 24.2 hours, respectively. The median digital leisure time of the pre-COVID and COVID period samples of secondary school students were 64.0 hours and 71.4 hours, respectively. While the univariate Mann-Whitney U test showed that the median of weekly digital leisure time was significantly different pre- and during COVID for the primary (P < .001) and secondary school students (P = .043), when a multivariate regression model containing age, sex, seasonality, and household income as covariates were used, assessment period did not predict changes in digital leisure time (log-transformed) for primary and secondary school students.
DISCUSSION
To the best of our knowledge, this is the first study comparing sleep-wake patterns before and after the COVID outbreak among children and adolescents using school-based random sampling.
Sleep-wake patterns altered during the COVID period for students in both primary and secondary school
Both primary and secondary school students took longer to fall asleep after the COVID outbreak. Such differences remained robust after adjustment for confounders. In our city, which is characterized by a low infection rate but stringent antipandemic measures, pandemic-related stressors and lifestyle changes have had a widespread effect on the sleep health of young people across ages.
However, the sleep-wake pattern alteration among primary school students are mild (sleep latency lengthened by 3.1–4.4 minutes among those assessed during COVID period), while the alteration among secondary school students was more severe and pervasive. With later bedtime, longer sleep latency, later sleep onset, and later sleep midpoints, this suggests a pattern of a backward shift of sleep period during both school days and nonschool days, even though only an increase in sleep latency survived correction for multiple comparisons. The sleep latency among those assessed during COVID period was 8.5–8.6 minutes longer compared to those assessed pre-COVID, who had a mean sleep latency of 14 minutes. This difference is potentially clinically relevant, especially for those who already had sleep initial difficulties. Our findings extended the current literature that children and adolescents not only had delayed sleep in the first months of the pandemic24,25(p19) by demonstrating enduring changes in sleep-wake patterns over the first 15 months of COVID. It is not surprising that secondary school students are affected more than primary school students, as adolescents are more prone to insomnia and sleep-phase delays than younger children.14 Under COVID, young people in Hong Kong experienced profound lifestyle changes: School attendance was suspended, online learning via video-conferencing platforms became the “new normal,” and activities outside the home were restricted due to social distancing measures and the closing down of venues. As physical activity and light exposure are key inputs of our circadian clock, these lifestyle changes can disturb the circadian rhythm of young people.26 Stress from fear of infection, social isolation and uncertainty are also possible factors contributing to the increase in sleep difficulties.
Secondary school students from low-income households had more delayed sleep on nonschool school days during COVID
Our moderation analysis suggested that the sleep-wake patterns of boys and girls studying in both primary and secondary school were equally altered during the COVID pandemic. Analysis of the moderating effect of household income revealed that secondary school students from low-income households had a consistent pattern of more delayed sleep on nonschool days during the COVID period than their peers from higher-income families, but not on school days. Sleep-wake patterns during nonschool days are a better indicator of one’s “biological clock,” since one is less confined by the “social clock.” However, the increase in sleep latency during both school days and nonschool days was not moderated by household income. Our results thus suggest that secondary school students from low-income households had a more pronounced backward circadian rhythm shift than their wealthier peers without an increase in difficulty in sleep initiation. The magnitude of this shift (close to 1 hour on average) is clinically relevant: A US-based study reported that bedtime delayed for 2 hours or more during nonschool days was associated with increased risk for various mental and behavioral health problems.27 We speculate that this shift in circadian rhythm can be understood within the context of social inequality in Hong Kong, where low-income families were more deprived of social and physical activities during the pandemic. Like many urban areas worldwide, children and adolescents from low-income households in Hong Kong rely heavily on school-based support for activity opportunities. Data from the United States showed that children from low-income households who could not attend school physically during COVID experienced more marked mental health impairment.28 In addition, youths from low-income families were more entrapped at home than their peers from higher-income households due to the closing of public leisure venues over an extended period. This may have widened the gap in accessibility to activities between those from high-income families and low-income families, which may have translated into the differences in their levels of physical activity and light exposure, 2 key zeitgebers of circadian rhythm.29
Socioeconomic status has always been a significant determinant of health in children and adolescent populations, and it undermines one’s resilience against adverse outcomes in times of stress and crisis.23 In line with our findings on the effect of socioeconomic status on sleep health during COVID, a local cross-sectional online survey found that a low-income status and several other socioeconomic adversities increased the risk of psychosocial problems in children during the COVID pandemic.30 Society should pay attention to the possible widening of the health gaps between young people from high-income and low-income families people in the COVID era.
The amount of digital leisure time did not mediate the effect of assessment period on the sleep-wake patterns of children and adolescents
Contrary to our expectations, we did not see a significant increase in digital leisure time after the COVID outbreak. Given that a recent study showed that the rise in use of digital media during the initial lockdown period almost returned to pre-COVID levels afterwards,31 it is possible that during the 15 months of our recruitment during the COVID period, the digital leisure time of our sample increased initially and then subsequently decreased.
Strengths and limitations
The key strength of this study is the use of a territory-wide, random sampling method. Together with a high response rate, we have captured a representative sample of school-aged children and adolescents in Hong Kong. Furthermore, we kept our sampling methodology consistent before and during COVID, making our data from the 2 periods comparable. The study has several limitations: First, this study is cross-sectional by nature and not longitudinal. Second, the sleep parameters were derived only from self-reports or parent-reports, without objective measures such as actigraphy. Third, our data did not capture daytime activities, limiting our interpretation of the mediating factors of the various changes.
CONCLUSIONS
Our results highlighted demonstrable differences in the sleep patterns of children and adolescents of Hong Kong before and during COVID, despite the low COVID infection rate. These changes can, in turn, lead to adverse health consequences. The moderating effect of household income on circadian disruption among adolescents is a source of concern. It should alert us to the widening health gaps between youth from high-income and low-income families under the pressure of COVID. Proactive measures to alleviate the health impact on the younger population during COVID should be part of a holistic pandemic response plan.
DISCLOSURE STATEMENT
All authors have seen and approved the final manuscript. The study was funded by the Government of the Hong Kong Special Administrative Region, Food and Health Bureau, Health and Medical Research Fund (Ref. No.: MHS-P1(Part 1)-CUHK) (Principal investigators: S.F.H. and P.W.L.L.). The funding source played no role in study design, in the collection, analysis, and interpretation of data, in the writing of the report, and in the decision to submit the paper for publication. The authors report no conflict of interest.
ACKNOWLEDGMENTS
The authors thank the participating schools for their facilitation of participant recruitment. We thank Ms. Daisy Cheung for her comments on the manuscript. Data sharing policy: Data available on request.
ABBREVIATIONS
- CI
confidence interval
- COVID/COVID-19
coronavirus disease
REFERENCES
- 1. Bellino S , Punzo O , Rota MC , et al. COVID-19 WORKING GROUP . COVID-19 Disease Severity Risk Factors for Pediatric Patients in Italy . Pediatrics. 2020. ; 146 ( 4 ): e2020009399 . [DOI] [PubMed] [Google Scholar]
- 2. UNICEF . COVID-19: Schools for more than 168 million children globally have been completely closed for almost a full year, says UNICEF. March 2021. https://www.unicef.org/press-releases/schools-more-168-million-children-globally-have-been-completely-closed . Accessed April 29, 2022. .
- 3. Zhang X , Cheung SSL , Chan HN , et al . Myopia incidence and lifestyle changes among school children during the COVID-19 pandemic: a population-based prospective study . Br J Ophthalmol. 2022. ; 106 ( 12 ): 1772 – 1778 . [DOI] [PubMed] [Google Scholar]
- 4. Hu J , Liu J , Wang J , et al . Unfavorable progression of obesity in children and adolescents due to COVID-19 pandemic: A school-based survey in China . Obesity (Silver Spring). 2021. ; 29 ( 11 ): 1907 – 1915 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhang J , Li AM , Fok TF , Wing YK . Roles of parental sleep/wake patterns, socioeconomic status, and daytime activities in the sleep/wake patterns of children . J Pediatr. 2010. ; 156 ( 4 ): 606 – 12.e5 . [DOI] [PubMed] [Google Scholar]
- 6. Matricciani L , Paquet C , Galland B , Short M , Olds T . Children’s sleep and health: A meta-review . Sleep Med Rev. 2019. ; 46 : 136 – 150 . [DOI] [PubMed] [Google Scholar]
- 7. Li SX , Chan NY , Man Yu MW , et al . Eveningness chronotype, insomnia symptoms, and emotional and behavioural problems in adolescents . Sleep Med. 2018. ; 47 : 93 – 99 . [DOI] [PubMed] [Google Scholar]
- 8. Chan NY , Zhang J , Tsang CC , et al . The associations of insomnia symptoms and chronotype with daytime sleepiness, mood symptoms and suicide risk in adolescents . Sleep Med. 2020. ; 74 : 124 – 131 . [DOI] [PubMed] [Google Scholar]
- 9. Haynie DL , Lewin D , Luk JW , et al . Beyond sleep duration: bidirectional associations among chronotype, social jetlag, and drinking behaviors in a longitudinal sample of US high school students . Sleep. 2018. ; 41 ( 2 ): zsx202 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rutters F , Lemmens SG , Adam TC , et al . Is social jetlag associated with an adverse endocrine, behavioral, and cardiovascular risk profile? J Biol Rhythms. 2014. ; 29 ( 5 ): 377 – 383 . [DOI] [PubMed] [Google Scholar]
- 11. Cespedes Feliciano EM , Rifas-Shiman SL , Quante M , Redline S , Oken E , Taveras EM . Chronotype, social jet lag, and cardiometabolic risk factors in early adolescence . JAMA Pediatr. 2019. ; 173 ( 11 ): 1049 – 1057 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Li L , Wu C , Gan Y , Qu X , Lu Z . Insomnia and the risk of depression: a meta-analysis of prospective cohort studies . BMC Psychiatry. 2016. ; 16 ( 1 ): 375 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sharma M , Aggarwal S , Madaan P , Saini L , Bhutani M . Impact of COVID-19 pandemic on sleep in children and adolescents: a systematic review and meta-analysis . Sleep Med. 2021. ; 84 : 259 – 267 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zhang J , Chan NY , Lam SP , et al . Emergence of sex differences in insomnia symptoms in adolescents: a large-scale school-based study . Sleep. 2016. ; 39 ( 8 ): 1563 – 1570 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cooper K , Stewart K . Does household income affect children’s outcomes? A systematic review of the evidence . Child Indic Res. 2021. ; 14 ( 3 ): 981 – 1005 . [Google Scholar]
- 16. Chung GKK , Chan SM , Chan YH , et al . Socioeconomic patterns of COVID-19 clusters in low-incidence city, Hong Kong . Emerg Infect Dis. 2021. ; 27 ( 11 ): 2874 – 2877 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Perez D , Thalken JK , Ughelu NE , Knight CJ , Massey WV . Nowhere to go: parents’ descriptions of children’s physical activity during a global pandemic . Front Public Health. 2021. ; 9 : 642932 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hysing M , Pallesen S , Stormark KM , Jakobsen R , Lundervold AJ , Sivertsen B . Sleep and use of electronic devices in adolescence: results from a large population-based study . BMJ Open. 2015. ; 5 ( 1 ): e006748 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. The Hong Kong Council of Social Service . Combined Primary & Secondary School Enrolment Ratio | Social Indicators of Hong Kong. https://www.socialindicators.org.hk/en/indicators/children/29.4 . Accessed May 2, 2022. .
- 20. Campos L , Veríssimo L , Nobre B , Morais C , Dias P . Protective factors in the use of electronic media according to youth and their parents: an exploratory study . Int J Environ Res Public Health. 2021. ; 18 ( 7 ): 3573 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Merikangas KR , Zhang J , Emsellem H , et al . The structured diagnostic interview for sleep patterns and disorders: rationale and initial evaluation . Sleep Med. 2014. ; 15 ( 5 ): 530 – 535 . [DOI] [PubMed] [Google Scholar]
- 22. Gray EJ , Scott JG , Lawrence DM , Thomas HJ . Concordance between adolescents and parents on the Strengths and Difficulties Questionnaire: Analysis of an Australian nationally representative sample . Aust N Z J Psychiatry. 2021. ; 55 ( 11 ): 1058 – 1070 . [DOI] [PubMed] [Google Scholar]
- 23. Baron RM , Kenny , DA . The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations . J Pers Soc Psychol. 51 ( 6 ): 1173 – 1182 . [DOI] [PubMed] [Google Scholar]
- 24. Maximova K , Khan MKA , Dabravolskaj J , Maunula L , Ohinmaa A , Veugelers PJ . Perceived changes in lifestyle behaviours and in mental health and wellbeing of elementary school children during the first COVID-19 lockdown in Canada . Public Health. 2022. ; 202 : 35 – 42 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Giuntella O , Hyde K , Saccardo S , Sadoff S . Lifestyle and mental health disruptions during COVID-19 . Proc Natl Acad Sci U S A. 2021. ; 118 ( 9 ): e2016632118 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Quante M , Mariani S , Weng J , et al . Zeitgebers and their association with rest-activity patterns . Chronobiol Int. 2019. ; 36 ( 2 ): 203 – 213 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Zhang J , Paksarian D , Lamers F , Hickie IB , He J , Merikangas KR . Sleep patterns and mental health correlates in US adolescents . J Pediatr. 2017. ; 182 : 137 – 143 . [DOI] [PubMed] [Google Scholar]
- 28. Hawrilenko M , Kroshus E , Tandon P , Christakis D . The association between school closures and child mental health during COVID-19 . JAMA Netw Open. 2021. ; 4 ( 9 ): e2124092 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Yamanaka Y , Honma K , Hashimoto S , Takasu N , Miyazaki T , Honma S . Effects of physical exercise on human circadian rhythms . Sleep Biol Rhythms. 2006. ; 4 ( 3 ): 199 – 206 . [Google Scholar]
- 30. Tso WWY , Wong RS , Tung KTS , et al . Vulnerability and resilience in children during the COVID-19 pandemic . Eur Child Adolesc Psychiatry. 2022. ; 31 ( 1 ): 161 – 176 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Werling AM , Walitza S , Grünblatt E , Drechsler R . Media use before, during and after COVID-19 lockdown according to parents in a clinically referred sample in child and adolescent psychiatry: Results of an online survey in Switzerland . Compr Psychiatry. 2021. ; 109 : 152260 . [DOI] [PubMed] [Google Scholar]