In an analysis of Medicaid administrative data, children who received permanent supportive housing saw greater increases in preventive dental care.
Abstract
BACKGROUND AND OBJECTIVES
Permanent supportive housing (PSH) integrates long-term housing and supports for families and individuals experiencing homelessness. Although PSH is frequently provided to families with children, little is known about the impacts of PSH among children. We examined changes in health care visits among children receiving PSH compared with similar children who did not receive PSH.
METHODS
We analyzed Pennsylvania Medicaid administrative data for children entering PSH between 2011 and 2016, matching to a comparison cohort with similar demographic and clinical characteristics who received non-PSH housing services. We conducted propensity score-weighted difference-in-differences (DID) analyses to compare changes in health care visits 3 years before and after children entered PSH versus changes in the comparison cohort.
RESULTS
We matched 705 children receiving PSH to 3141 in the comparison cohort. Over 3 years following PSH entry, dental visits among children entering PSH increased differentially relative to the comparison cohort (DID: 12.70 visits per 1000 person-months, 95% confidence interval: 3.72 to 21.67). We did not find differential changes in preventive medicine visits, hospitalizations, or emergency department (ED) visits overall. When stratified by age, children ≤5 years old at PSH entry experienced a greater decrease in ED visits relative to the comparison cohort (DID: −13.16 visits per 1000 person-months, 95% confidence interval: −26.23 to −0.10). However, emergency visit trends before PSH entry differed between the cohorts.
CONCLUSIONS
Children in PSH had relatively greater increases in dental visits, and younger children entering PSH may have experienced relative reductions in ED visits. Policymakers should consider benefits to children when evaluating the overall value of PSH.
What’s Known on This Subject:
Permanent supportive housing (PSH) reduces homelessness and is associated with changes in healthcare utilization in adults. Approximately one-third of PSH beds in the United States are designated for families with children, however little is known regarding how PSH impacts these children’s healthcare utilization.
What This Study Adds:
Compared with a matched cohort receiving other housing supports, children in PSH had greater increases in dental visits, and relative reductions in emergency department visits in the youngest children. Benefits to children should contribute to the valuation of PSH programs.
Homelessness is a substantial problem for children in the United States, with over 100 000 children under age 18 estimated to have experienced homelessness in 2020.1 Homelessness may affect health through multiple mechanisms, including its impacts on a child’s physical living environment, exposure to stress, and access to health care.2 Homelessness among children is associated with worse self-reported health,3,4 increased severity of asthma exacerbations,5 and poorer vision, dental, and mental health.6 The adverse effects of homelessness may persist several years after exposure to homelessness7 and are likely to be more severe among children in poorer baseline health.8,9
Permanent supportive housing (PSH) aims to address chronic homelessness and its adverse effects on wellbeing by integrating long-term housing—without a time limit on residency—with supportive services, such as case management, substance use disorder treatment, and employment assistance.10,11 PSH has been shown to be effective in reducing homelessness compared with other housing supports.12 Emerging evidence suggests that PSH is also associated with reductions in Medicaid spending13— of importance to states considering whether to pay for PSH services with limited Medicaid funds.14 Furthermore, prior studies of PSH and healthcare utilization, nearly all of which focused on adults, found that receiving PSH is associated with increases in outpatient behavioral health care and reductions in emergency department (ED) visits15 and hospitalizations,16,17 suggesting that PSH improves management of health conditions.13,18,19
PSH programs do not exclusively serve adults. In 2020, approximately one-third of PSH beds in the United States were designated for families with children.1 Several features of PSH may improve children’s health and access to health care. First, PSH programs may directly provide or facilitate referrals to healthcare.20 Second, PSH may promote health and safety by improving a child’s living environment or through complementary provision of services such as childcare.20,21 Third, children may benefit from PSH if increased family stability and parental connection to supportive services leads to improvements in family connection, school attendance, and children’s access to health care.22,23 However, no studies have examined whether family receipt of PSH is associated with changes in health care utilization among children.
In this study, we used linked administrative data from Medicaid and housing programs in Pennsylvania to examine changes in health care utilization among children before and after they and their families received PSH. Using a difference-in-differences design, we compared changes in utilization among children receiving PSH to a comparison cohort of children at risk for homelessness but without PSH enrollment. We examined ED and inpatient hospital utilization (as markers of illness) and dental and preventive medicine visits (which might facilitate health through disease prevention and management). We hypothesized that receiving PSH would be associated with increased preventive health utilization and decreased ED visits and hospital utilization.
Methods
This study was reviewed by the University of Pittsburgh Institutional Review Board and deemed exempt because it is a secondary analysis of deidentified data.
Context
More than 1 in 3 children in Pennsylvania are covered by Medicaid or the Children’s Health Insurance Program.24 Since 2006, the Pennsylvania Department of Human Services has supported PSH programs targeted toward households in which the head of household is experiencing mental illness, substance abuse or other chronic conditions, or other significant “barriers to employment or housing stability.”25 Although federal law prohibits using Medicaid funds directly for housing, Pennsylvania Medicaid funds are used for some PSH-associated services, such as case management, therapy, and medical transportation.26,27
Data
We analyzed Pennsylvania Homeless Management Information System (HMIS) data from 2011 to 2016 and Pennsylvania Medicaid enrollment and claims data from 2008 to 2018. HMIS data capture federally-financed housing services received by individuals who are homeless or at risk for homelessness, and include information about the types of housing services provided (eg, PSH, emergency shelters) and dates of residence associated with these services.28 When we conducted this analysis, HMIS data were available from 54 of Pennsylvania’s 67 counties, including counties in the Pittsburgh but not the Philadelphia metropolitan area. Medicaid and HMIS data were linked by the Pennsylvania Department of Human Services using individual-level identifiers and provided to the University of Pittsburgh on a deidentified basis. Further details on our data sources have been published elsewhere.13
Intervention Cohort
Our intervention cohort consisted of children enrolled in the Pennsylvania Medicaid program who received at least 1 PSH service for ≥180 days during 2011 to 2016 and were under age 18 at the time of PSH entry. The median duration in PSH among all children linked across our HMIS and Medicaid data were 650 days. We limited the sample to children with at least 1 parent or guardian who had a contemporaneous record of PSH entry (Supplemental Information 1). Because we wanted to examine changes in care patterns before and after children entered PSH, we further restricted the sample to children who were enrolled in Pennsylvania Medicaid for at least 12 of the 15 months before and 24 of the 36 months after PSH entry. The first criterion ensures a minimum of 12 months of baseline data in all children, while allowing for the analysis of children as young as 12 months at the time of PSH receipt. Both criteria purposefully allow for some noncontinuous Medicaid enrollment, given well-documented patterns of churn into and out of Medicaid.29 For a given individual, analysis focused on only the first episode of PSH enrollment.
Comparison Cohort
We compared changes in health care visits in our intervention cohort to changes in a matched cohort of children who experienced homelessness or were at risk for homelessness but did not receive PSH. We selected this comparison cohort among children and linked parents in the HMIS dataset who, during our study period, received only non-PSH housing services (eg, emergency shelter stays) indicative of periodic or chronic homelessness. We matched these children many-to-1, without replacement, to the intervention cohort based on the following criteria: date of birth (within 12 months); gender; region; a parent or guardian’s diagnosis of mental illness and substance use disorder; and having at least 1 parent who qualified for Medicaid based on disability. (Additional details about the matching criteria are in Supplemental Table 3.) We matched on age so that our comparison cohort controlled for age-related trends in health care use (eg, decreasing frequency of recommended preventive visits by age, as well as known decreases in acute visits and increases in dental visits as children age),30–32 which we wanted to distinguish from changes in utilization associated with receiving PSH. We assigned each child from this candidate comparison cohort an index date, defined as the date that their matched counterpart from the intervention cohort entered PSH. We retained children who (1) received a non-PSH housing service (in the HMIS) within 6 months of the index date and (2) were also enrolled in Medicaid for at least 12 of the 15 months before and 24 of the 36 months after the index date.
Finally, we used propensity score methods to weight children in the comparison cohort to resemble children in the intervention cohort. The propensity score model used to construct these weights included all variables from the matching procedure, as well as race and ethnicity, urbanicity, and a 3-level variable representing the presence and complexity of chronic conditions according to the Pediatric Medical Complexity Algorithm (PMCA), in the year before the PSH entry date or index date (details of the propensity score model are in Supplemental Information 1).33 These variables were included to account for differences in regional housing programs, factors such as age that influence health utilization, and historic and ongoing effects of racism on housing and access to health care.34,35
Differential disenrollment from Medicaid between the intervention and comparison cohorts might bias estimates of differential changes in utilization. Additionally, since health utilization is linked to age, differential changes in the age composition of our 2 cohorts over the study period (eg, because of different age-dependent patterns of disenrollment) could bias our estimates. To assess these sources of bias, we compared trends in the number of children and the ages of Medicaid-enrolled children in each cohort over time.
Outcome Variables
We assessed hospitalizations and ED visits, both of which have been found to decrease when adults receive PSH.13,17 We also examined dental and preventive medicine visits, whose rates of completion are affected by homelessness.2 Moreover, increasing access to dental and preventive care are Healthy People 2030 goals.36 Similar to other analyses of dental care use, we separately analyzed preventive dental visits (eg, visits including application of prophylactic fluoride varnish) and treatment dental visits (eg, visits including fillings).37 We measured all outcomes at the person-month level for months in which children were enrolled in Medicaid. To facilitate interpretation, we report estimates as rates per 1000 person-months. Technical definitions for each measure are in Supplemental Information 2.
Statistical Analysis
To estimate changes in study outcomes associated with receiving PSH, we performed a difference-in-differences analysis. The analysis compared changes in outcomes (1) in the intervention cohort from the baseline period (up to 3 years before PSH entry) to a postintervention period (spanning up to 3 years after PSH entry), to (2) changes in the comparison cohort (up to 3 years before and after the index date). The difference-in-differences design holds all fixed (eg, baseline) differences between the intervention and comparison cohorts constant, giving an estimate of relative changes between the cohorts attributable to receiving PSH.
We estimated these changes using linear difference-in-differences models. We specified the models with an indicator for the period following PSH entry, an indicator for membership in the intervention cohort, and an interaction between these indicators. Estimates for this interaction term represent the average change in each outcome from baseline to the postintervention period in the intervention cohort, relative to changes in the comparison cohort. Hereafter, we refer to these estimates as differential changes in utilization in the intervention versus comparison cohorts. We adjusted all models for the same characteristics of children and parents used for matching and the construction of propensity score weights, as well as year and quarter fixed effects to adjust for secular trends in utilization. Statistical inferences were conducted using cluster-robust standard errors (each child in the intervention cohort and their set of matched comparators was defined as 1 cluster).
Sensitivity Analyses
We conducted 2 sensitivity analyses. First, because changes in health care use associated with PSH may differ by age and baseline level of health needs,38 we ran separate difference-in-differences models for 3 age groups (defined based on age at PSH entry: children ages ≤5 years, 6–11 years, and 12–17 years) and for children with versus without chronic conditions based on the PMCA. Second, to assess whether our difference-in-differences design isolated changes in utilization associated with receiving PSH from baseline trends, we visually compared utilization trends between the 2 cohorts during the baseline period. Evidence of parallel baseline trends provides support for the assumption that the difference-in-differences design isolated changes in utilization specifically associated with PSH entry.39
Results
Cohort Demographics
Our analysis sample included 705 children who received PSH and 3141 children in the matched comparison cohort. Children resided in 48 of the 54 Pennsylvania counties included in the HMIS dataset. Before weighting, 51.6% of children in the intervention cohort were female, 51.5% were non-Hispanic white, and 31.3% were 6 to 11 years old when they entered PSH. In the comparison cohort, 51.6% of children were female, 47.2% were non-Hispanic white, and 34.9% were 6 to 11 when they entered PSH (Table 1). After weighting, standardized mean differences for measured baseline characteristics were all ≤0.072 in absolute value. The mean age and the number of children enrolled in Medicaid showed similar trends across study years in the 2 cohorts, indicating no compositional changes between the cohorts because of differential disenrollment from Medicaid over time (Supplemental Table 4).
TABLE 1.
Baseline Characteristics of Children Receiving PSH and Matched Comparison Cohort
| Matched Cohorts, Before Weighting N (%) | Matched Cohort, After Propensity Score Weighting % | ||||||
|---|---|---|---|---|---|---|---|
| Characteristic | Intervention Cohort (Received PSH), N = 705, n (%) | Comparison Cohort, N = 3141, n (%) | P a | SMD b | Intervention Cohort (Received PSH), N = 701, n (%) | Comparison Cohort, N = 3120, n (%) | SMD b |
| Female | 364 (51.6) | 1621 (51.6) | .991 | −0.000 | 51.5 | 51.4 | 0.001 |
| Age at time of PSH entry | .609 | ||||||
| ≤2 y old | 140 (19.9) | 609 (19.4) | 0.012 | 19.8 | 19.1 | 0.018 | |
| 3–5 y old | 169 (24.0) | 687 (21.9) | 0.049 | 24.0 | 21.0 | 0.070 | |
| 6–11 y old | 221 (31.3) | 1095 (34.9) | −0.076 | 31.2 | 34.6 | −0.072 | |
| 12–18 y old | 175 (24.8) | 750 (23.9) | 0.022 | 25.0 | 25.3 | −0.009 | |
| Race and Ethnicity | .051 | ||||||
| Non-Hispanic white | 363 (51.5) | 1481 (47.2) | 0.087 | 51.4 | 51.5 | −0.002 | |
| Non-Hispanic black | 300 (42.6) | 1497 (47.7) | −0.103 | 42.7 | 42.7 | −0.000 | |
| Hispanic | 22 (3.1) | 68 (2.2) | 0.055 | 3.1 | 3.0 | 0.007 | |
| Others | 20 (2.8) | 95 (3.0) | −0.011 | 2.9 | 2.9 | −0.000 | |
| Urban c | 613 (87.0) | 2749 (87.5) | .626 | −0.020 | 87.4 | 86.5 | 0.028 |
| Within Southwest Managed Care Region | 624 (88.5) | 2930 (93.3) | <.001 | −0.150 | 88.4 | 87.6 | 0.025 |
| Resides in Pittsburgh or surrounding county | 512 (72.6) | 1755 (55.9) | <.001 | 0.376 | 73.0 | 72.3 | 0.016 |
| Medical complexity d | .009 | ||||||
| Complex chronic disease | 62 (8.8) | 226 (7.2) | 0.056 | 8.8 | 8.6 | 0.007 | |
| Noncomplex chronic disease | 209 (29.6) | 793 (25.2) | 0.096 | 29.5 | 29.2 | 0.007 | |
| No chronic disease | 434 (61.6) | 2122 (67.6) | −0.123 | 61.6 | 62.1 | −0.011 | |
| Parental diagnosis | |||||||
| Mental illness | 683 (96.9) | 3043 (96.9) | .999 | 0.000 | 96.9 | 96.8 | 0.002 |
| Substance use disorder | 505 (71.6) | 1959 (62.4) | <.001 | 0.205 | 71.5 | 71.6 | −0.004 |
| Parent enrolled in Medicaid and Medicare e | 128 (18.2) | 368 (11.7) | <.001 | 0.167 | 18.1 | 18.5 | −0.009 |
| Parent with disability | 205 (29.1) | 969 (30.9) | 0.356 | −0.039 | 29.1 | 29.1 | 0.000 |
P value for differences in means or proportions between children in the intervention and comparison cohorts before propensity score weighting.
SMD: standardized mean difference, calculated as the mean difference between the intervention and comparison cohorts, divided by the SD of the characteristic in the pooled intervention and comparison samples. Small SMD (less than 0.2) indicate similar intervention and control groups.48
Four children (0.6%) in the intervention cohort and 21 children (0.7%) in the comparison cohort lived in ZIP codes without urban or rural classification in Medicaid records.
Medical complexity determined using the Pediatric Medical Complexity Algorithm (PMCA).33 PMCA classifications are described in detail in Supplemental Information 1.
Parental enrollment was defined as any Medicare enrollment during from 2011 to 2018.
Baseline Trends
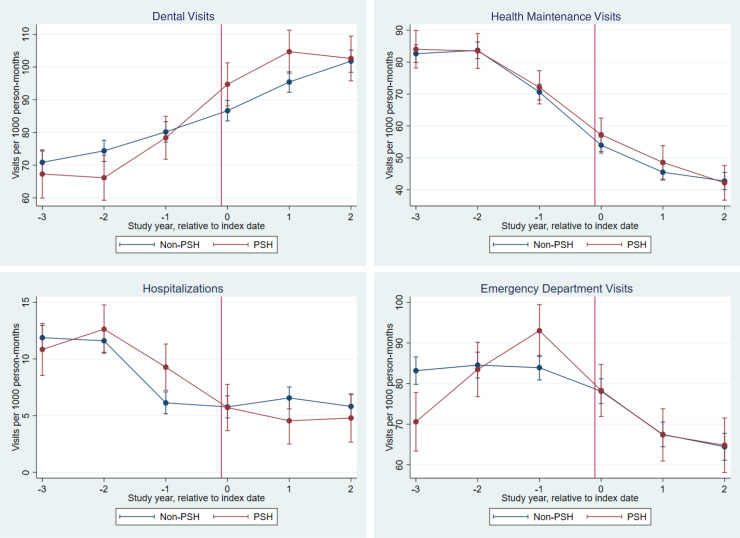
Unadjusted trends in utilization before and after PSH enrollment in the intervention and comparison cohorts are shown in Fig 1. Baseline utilization trends (during the 36 months before PSH entry or index dates) were comparable between the intervention and comparison cohorts for all outcomes except for ED visits, for which the intervention cohort showed a greater increase in visits relative to the comparison cohort in the year before PSH entry (Fig 1). The similar baseline trends in dental, preventive medicine, and inpatient visits satisfied the key difference-in-differences assumption of parallel preintervention trends for these outcomes. Baseline utilization levels did not vary significantly between the intervention and comparison cohorts (Table 2).
FIGURE 1.
Unadjusted utilization by year. Figures show unadjusted trends in our main utilization outcomes before and after entry into PSH (intervention cohort) and before and after the index date (comparison cohort), with entry or index date represented as a red, vertical line. Negative numbers on the horizontal indicate years before PSH entry or the index date, positive numbers indicate years following PSH entry or the index date, and 0 indicates the year beginning on the day of PSH entry or index date. Estimates plotted on the vertical axis represent unadjusted mean rates of utilization per 1000 person-months. The error bars represent 95% confidence intervals which account for clustering (each child in the intervention cohort and their set of matched comparators was defined as 1 cluster).
TABLE 2.
Difference-in-Differences Estimates of Changes in Utilization Associated With PSH Entry Among Children
| Intervention Cohort (Received PSH) | Comparison Cohort (Received Non-PSH Housing Services) | Difference-in-Differences (95% CI) | P | |||||
|---|---|---|---|---|---|---|---|---|
| Outcome (Visits per 1000 Person-Months) | Baseline | Years 1–3 After Baseline | Difference (95% CI) | Baseline | Years 1–3 After Baseline | Difference (95%CI) | ||
| Dental visits | 71.01 | 100.62 | 22.80 * (14.35 to 31.17) | 75.48 | 94.25 | 10.10 * (3.13 to 17.08) | 12.70 * (3.72 to 21.67) | .006 |
| Preventive medicine visits | 79.42 | 49.54 | −27.74 * (−33.54 to −21.93) | 78.55 | 47.66 | −30.23 * (−34.00 to −26.46) | 2.49 (−4.03 to 9.00) | .454 |
| Hospitalizations | 10.87 | 5.02 | −4.85 * (−7.40 to −2.31) | 9.67 | 6.06 | −2.84 (−6.55 to 0.88) | −2.02 (−6.36 to 2.31) | .361 |
| Emergency department visits | 83.25 | 70.32 | −12.85 * (−21.42 to −4.28) | 83.92 | 70.32 | −8.30 * (−14.59 to −2.02) | −4.55 (−13.35 to 4.25) | .311 |
Model adjusted for age, race and ethnicity, gender, rural or urban dwelling status, residence in Pittsburgh and the surrounding county, indicators for Pennsylvania managed care region, medical complexity (PMCA categories of complex chronic condition and noncomplex chronic condition status), parental health conditions including mental health, substance use disorder, and disability status, parental enrollment in Medicaid and Medicare, calendar year fixed effects, and calendar quarter fixed effects. 95% confidence intervals and P values calculated using robust standard errors that account for clustering (each child in the intervention cohort and their set of matched comparators was defined as 1 cluster). Full regression model estimates are in Supplemental Information 4.
P < .05.
Difference-in-differences Estimates
Adjusted difference-in-differences estimates, which reflect differential changes in study outcomes between the intervention and comparison cohorts, are reported in Table 2 (full regression estimates are in Supplemental Table 5). Among children receiving PSH, dental visits increased by 22.80 visits per 1000 person-months between the baseline period and the 36 months after PSH entry. Among children in the comparison cohort, dental visits increased by 10.10 visits per 1000 person-months from the baseline to the 36 months after index date. The resulting differential change of 12.70 visits per 1000 person-months (95% confidence interval [CI] 3.72 to 21.67) indicates a greater increase in dental visits among children after entering PSH. When separate regressions were performed for preventive and treatment dental visits, a significant difference-in-differences was found in preventive dental visits only (differential increase of 7.65 visits per 1000 person-months; 95% CI: 2.02 to 13.28, Supplemental Table 6). We found no differential change in preventive medicine visits, inpatient admissions, or ED visits.
Subgroup Analysis by Age and Presence of Chronic Conditions
In subgroup analyses by age and baseline presence of chronic conditions, children 0 to 5 years on PSH entry showed a significantly greater decrease in ED visits versus the comparison cohort (a differential change of −13.16 visits per 1000 person-months, 95% CI: −26.23 to −0.10). PSH receipt was also associated with significantly greater increases in dental visits among children aged 12 to 17 years (34.13 more visits per 1000 person-months, 95% CI 9.30 to 58.97, Supplemental Information 6; Supplemental Table 7). Subgroups of children with and without chronic conditions showed similar increases in dental visits (12.33 visits per 1000 person-months, 95% CI −2.02 to 26.68 and 12.90 visits per 1000 person-months, 95% CI 1.39 to 24.41, respectively), although this difference only reached significance among children without chronic conditions.
Discussion
In this analysis of health care utilization among children receiving PSH, we found increases in overall and preventive dental visits and some evidence of decreases in illness-related care (ED visits among the youngest children) in the 3 years after children entered PSH, relative to changes in a matched cohort of children who did not receive PSH. Differential increases in overall dental visits were driven by preventive dental visits, particularly among adolescents. Because the cohorts showed similar baseline trends in dental visits, the subsequent differences we found may be attributable to PSH. In contrast, because there were differences in ED visits between cohorts even preceding PSH entry, we have less confidence in attributing the subsequent differential reduction in ED visits specifically to receiving PSH.
This study adds to current understanding of the impact of PSH on families by examining how PSH entry is associated with changes in children’s health care use. To our knowledge, the only prior study examining health care use among children in PSH did not examine changes before and after PSH entry and did not include a comparison cohort.22 Multiple studies, however, have examined health care use among adults in PSH. Two studies using a similar approach to ours (difference-in-differences with a matched comparison cohort) found that entering PSH was associated with a differential reduction in ED visits, and one also found that PSH was associated with overall cost savings because of reductions in inpatient spending.13,40 Both studies also found increases in prescription drug and behavioral health care spending, suggesting that reductions in hospital use associated with PSH were mediated by improvements in disease management.
Our study was designed to examine key markers of pediatric health care use and health outcomes (eg, hospitalizations) that we could measure for all children. Although other outcomes, such as the receipt of guideline-concordant asthma management, behavioral health care, and immunizations, are also critical to examine, these outcomes apply to specific subpopulations of children, ages, or times of year, increasing the sample size which would be necessary to detect differential changes between cohorts. Future research examining changes in additional outcomes among larger cohorts of children could add to evidence about how PSH is associated with changes in care for children.
Our results underscore that children, like their adult guardians, may derive important benefits from receiving PSH, particularly with regard to increased access to preventive dental care. Although Medicaid covers comprehensive dental care in every state,41 dental problems remain common among children experiencing homelessness, with approximately one-third of homeless youth experiencing “very bad” or “bad” dental health.42 Poor dental health is associated with decreased school attendance43 and performance,44,45 which have long-term implications for wellbeing. Thus, the increases in dental care we found to be associated with PSH may facilitate long-term improvements in oral health and overall wellbeing.42,46,47 However, observing long-term benefits linked to these changes in dental visits, such as improved oral health status and reductions in emergency dental care, would likely require longer follow-up.
We did not find greater increases in preventive medical care among children receiving PSH. This negative finding stands in contrast to prior research on PSH, including a study in the Minneapolis-St. Paul metropolitan area, which found high rates of well-child visits among children living in PSH.22 Numerous factors, including the characteristics of families receiving PSH, the availability of local providers, and the components of individual PSH programs, could have contributed to this difference. The role of heterogeneity across PSH programs, which can differ in the services and housing offered, remains an understudied but potentially salient contributor to differences in outcomes associated with receiving PSH. Unfortunately, HMIS data did not allow us to observe programmatic differences among individual PSH programs. Further research characterizing these differences, using detailed program data, may help to illuminate what aspects of supportive housing (eg child-targeted services) may be most beneficial for children’s outcomes, which could be disseminated across programs.
Our study had several additional limitations. First, unmeasured time-varying confounders may have limited our ability to establish true causal relationship between PSH and in health care use. Although we used matching to select a comparison cohort with similar baseline characteristics that were plausibly linked to baseline utilization, and our intervention and comparison cohorts were similar in all measured baseline variables, their preintervention health care utilization showed some differences, visible especially in ED utilization (Fig 1). Because of these baseline trend differences, we cannot confidently attribute subsequent reductions in ED visits to PSH receipt. Second, our data only include administrative records of health care use. Future studies of changes in health status, unmet needs, or other, nonmedical outcomes such as family reunification or school performance, could further characterize the impacts of PSH, but would require alternative data sources.
Conclusion
In this cohort study comparing children receiving PSH to a matched cohort of children at risk for homelessness, we found that receiving PSH was associated with increases in dental visits over a 3-year period. Our data also suggest that PSH may be associated with ED visits in young children. Although eligibility for PSH is evaluated on the basis of adults’ disabilities, benefits of PSH also accrue to children. To fully measure these benefits, future studies should examine changes in health care use and health status, beyond a period of 3 years, among individuals who received PSH as children.
Supplementary Material
Glossary
- DID
difference-in-differences
- ED
emergency department
- HMIS
Homeless Management Information System
- PMCA
Pediatric Medical Complexity Algorithm
- PSH
permanent supportive housing
Footnotes
Dr Bohnhoff conceptualized and designed the study, interpreted the data, drafted the initial manuscript, and reviewed and revised the manuscript; Dr Xue analyzed the data and critically revised the manuscript; Dr Burgette contributed to study design and data interpretation and critically revised the manuscript; Drs Hollander, Cole, Ray and Donohue contributed to study design and critically revised the manuscript; Dr Roberts supervised study conceptualization and design, supervised analysis, interpreted results, and critically revised the manuscript; and all authors have approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Dr Bohnhoff’s current affiliations are Department of Pediatrics, Maine Health, Portland, ME, and Center for Interdisciplinary Population and Health Research, Maine Health Institute for Research, Portland, ME.
FUNDING: This study was supported by an intergovernmental agreement between the Pennsylvania Department of Human Services (PA DHS) and the University of Pittsburgh. Dr Bohnhoff was supported by a Health Resources and Services Administration Training Grant (T32 HP22240). Dr Hollander was supported by a National Institute of Mental Health Training Grant (T32 MH 109436). Drs Cole, Donohue, and Roberts were supported in part by R01MD015261. The other authors received no additional funding.
CONFLICT OF INTEREST DISCLOSURES: The authors have indicated they have no conflicts of interest relevant to this article to disclose.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2022-059885.
References
- 1. Henry M, de Sousa T, Roddey C, et al. The 2020 Annual Homeless Assessment Report (AHAR) to Congress Part 1: Point-in-Time Estimates of Homelessness. Washington, DC: US Department of Housing and Urban Development; 2021 [Google Scholar]
- 2. Karr C, Kline S. Homeless children: what every clinician should know. Pediatr Rev. 2004;25(7):235–241 [DOI] [PubMed] [Google Scholar]
- 3. Sandel M, Sheward R, Ettinger de Cuba S, et al. Unstable housing and caregiver and child health in renter families. Pediatrics. 2018;141(2):e20172199. [DOI] [PubMed] [Google Scholar]
- 4. Cutts DB, Meyers AF, Black MM, et al. US Housing insecurity and the health of very young children. Am J Public Health. 2011;101(8):1508–1514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sakai-Bizmark R, Chang RR, Mena LA, Webber EJ, Marr EH, Kwong KY. Asthma hospitalizations among homeless children in New York State. Pediatrics. 2019;144(2):e20182769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Beharry MS, Christensen R. Homelessness in pediatric populations: strategies for prevention, assistance, and advocacy. Pediatr Clin North Am. 2020;67(2):357–372 [DOI] [PubMed] [Google Scholar]
- 7. Clark RE, Weinreb L, Flahive JM, Seifert RW. Infants exposed to homelessness: health, health care use, and health spending from birth to age six. Health Aff (Millwood). 2019;38(5):721–728 [DOI] [PubMed] [Google Scholar]
- 8. Seltzer RR, Thompson BS, Feudtner C. The daunting problem of medical complexity and housing instability. Pediatrics. 2020;146(1):e20193284. [DOI] [PubMed] [Google Scholar]
- 9. Baker E, Pham NTA, Daniel L, Bentley R. How does household residential instability influence child health outcomes? a quantile analysis. Int J Environ Res Public Health. 2019;16(21):4189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Quinn K, Dickson-Gomez J, Nowicki K, Johnson AK, Bendixen AV. Supportive housing for chronically homeless individuals: challenges and opportunities for providers in Chicago, USA. Health Soc Care Community. 2018;26(1):e31–e38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Henry M, Watt R, Matathey A, et al. The 2019 Annual Homeless Assessment Report (AHAR) to Congress Part 1: Point-in-Time Estimates of Homelessness. Washington, DC: US Department of Housing and Urban Development; 2020 [Google Scholar]
- 12. Kertesz SG, Baggett TP, O’Connell JJ, Buck DS, Kushel MB. Permanent supportive housing for homeless people - reframing the debate. N Engl J Med. 2016;375(22):2115–2117 [DOI] [PubMed] [Google Scholar]
- 13. Hollander MAG, Cole ES, Donohue JM, Roberts ET. Changes in Medicaid utilization and spending associated with homeless adults’ entry into permanent supportive housing. J Gen Intern Med. 2021;36(8):2353–2360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Committee on an Evaluation of Permanent Supportive Housing Programs for Homeless Individuals . Permanent Supportive Housing: Evaluating the Evidence for Improving Health Outcomes Among People Experiencing Chronic Homelessness. Washington, DC: The National Academies Press; 2018 [PubMed] [Google Scholar]
- 15. Lim S, Singh TP, Hall G, Walters S, Gould LH. Impact of a New York City supportive housing program on housing stability and preventable health care among homeless families. Health Serv Res. 2018;53(5):3437–3454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Baxter AJ, Tweed EJ, Katikireddi SV, Thomson H. Effects of Housing First approaches on health and well-being of adults who are homeless or at risk of homelessness: systematic review and meta-analysis of randomised controlled trials. J Epidemiol Community Health. 2019;73(5):379–387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dobbins K, Addison C, Roque A, El-Mallakh PL, El-Mallakh RS. Cost-savings associated with reductions in public service utilization with provision of permanent supported housing in midsized city in the United States. Psychiatr Q. 2021;92(2):833–841 [DOI] [PubMed] [Google Scholar]
- 18. Wright BJ, Vartanian KB, Li HF, Royal N, Matson JK. Formerly homeless people had lower overall health care expenditures after moving into supportive housing. Health Aff (Millwood). 2016;35(1):20–27 [DOI] [PubMed] [Google Scholar]
- 19. Lim S, Gao Q, Stazesky E, Singh TP, Harris TG, Levanon Seligson A. Impact of a New York City supportive housing program on Medicaid expenditure patterns among people with serious mental illness and chronic homelessness. BMC Health Serv Res. 2018;18(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bassuk EL, Huntington N, Amey C, Lampereur K. Family Permanent Supportive Housing: Preliminary Research on Family Characteristics, Program Models, and Outcomes. New York, NY: National Center on Family Homelessness; 2006 [Google Scholar]
- 21. Tiderington E, Bosk E, Mendez A. Negotiating child protection mandates in Housing First for families. Child Abuse Negl. 2021;115:105014. [DOI] [PubMed] [Google Scholar]
- 22. Gewirtz A, Hart-Shegos E, Medhanie A. Psychosocial status of homeless children and youth in family supportive housing. Am Behav Sci. 2008;51(6): 810–823 [Google Scholar]
- 23. Atkins M, Castro I, Sharifi M, et al. Unmet social needs and adherence to pediatric weight management interventions: Massachusetts, 2017-2019. Am J Public Health. 2020;110(S2):S251–S257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kaiser Family Foundation . Medicaid enrollees by enrollment group. Available at: https://www.kff.org/medicaid/state-indicator/distribution-of-medicaid-enrollees-by-enrollment-group/?dataView=0¤tTimeframe=0&selectedRows=%7B%22states%22:%7B%22pennsylvania%22:%7B%7D%7D%7D&sortModel=%7B%22colId%22:%22Children%22,%22sort%22:%22asc%22%7D. Accessed March 10, 2022
- 25. Pennsylvania Department of Human Services . Supportive housing. Available at: https://www.dhs.pa.gov/Services/Mental-Health-In-PA/Pages/Supportive-Housing.aspx. Accessed March 11, 2022
- 26. Medicaid and CHIP Payment and Access Commission . Issue Brief: Medicaid’s Role in Housing. Washington, DC: Medicaid and CHIP Payment Access Commission; 2018. [Google Scholar]
- 27. Corporation for Supportive Housing . Medicaid supportive housing services crosswalk. Available at: https://cshorg.wpengine.com/wp-content/uploads/2016/07/Pennsylvania-Supportive-Housing-Services-Medicaid-Crosswalk.pdf. Accessed November 23, 2022
- 28. US Department of Housing and Urban Development . Homeless management information system. Available at: https://www.hudexchange.info/programs/hmis/. Published 2021. Accessed November 29, 2021
- 29. Solomon J. Continuous Coverage Protections in Families First Act Prevent Coverage Gaps by Reducing “Churn”. Washington, DC: Center on Budget and Policy Priorities; 2020 [Google Scholar]
- 30. Center for Disease Control and Prevention . Dental care utilization among children aged 1–17 years: United States, 2019 and 2020. Available at: https://www.cdc.gov/nchs/products/databriefs/db424.htm. Accessed Nov 11, 2022 [PubMed]
- 31. Witt WP, Weiss AJ, Elixhauser A. Overview of hospital stays for children in the United States, 2012. HCUP Statistical Brief #187. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD: ;2014. [Google Scholar]
- 32. McDermott KW, Stocks C, Freeman WJ. Overview of pediatric emergency department visits, 2015: Statistical brief #242. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD: ;2016 [Google Scholar]
- 33. Simon TD, Haaland W, Hawley K, Lambka K, Mangione-Smith R. Development and validation of the pediatric medical complexity algorithm (PMCA) version 3.0. Acad Pediatr. 2018;18(5): 577–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Milburn NG, Edwards E, Obermark D, Roundtree J. Inequity in the Permanent Supportive Housing System in Los Angeles: Scale, Scope and Reasons for Black Residents’ Returns to Homelessness. Los Angeles, CA: California Policy Lab; 2021 [Google Scholar]
- 35. Artiga S, Young K, Garfield R, Majerol M. Racial and Ethnic Disparities in Access to and Utilization of Care Among Insured Adults. San Francisco, CA: Kaiser Fund Foundation; 2015 [Google Scholar]
- 36. US.Department of Health and Human Services, Office of Disease Prevention and Health Promotion . Healthy people 2030. Available at: https://health.gov/healthypeople/objectives-and-data/browse-objectives/children. Accessed Sept 27, 2021 [PubMed]
- 37. Abdus S, Decker SL. Association between Medicaid adult nonemergency dental benefits and dental services use and expenditures. J Am Dent Assoc. 2019;150(1):24–33 [DOI] [PubMed] [Google Scholar]
- 38. National Committee for Quality Assurance . Child and adolescent well-care visits. Available at: https://www.ncqa.org/hedis/measures/child-and-adolescent-well-care-visits/. Accessed November 11, 2022
- 39. Daw JR, Hatfield LA. Matching and regression to the mean in difference-in-differences analysis. Health Serv Res. 2018;53(6):4138–4156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. DeLia D, Nova J, Chakravarty S, %Tiderington E, Kelly T, Cantor JC. Effects of permanent supportive housing on health care utilization and spending among New Jersey Medicaid enrollees experiencing homelessness. Med Care. 2021;59 (Suppl 2):S199–S205 [DOI] [PubMed] [Google Scholar]
- 41. U.S. Department of Health and Human Services . Does Medicaid cover dental care? Available at: https://www.hhs.gov/answers/medicare-and-medicaid/does-medicaid-cover-dental-care/index.html. Accessed April 14, 2022
- 42. Chi D, Milgrom P. The oral health of homeless adolescents and young adults and determinants of oral health: preliminary findings. Spec Care Dentist. 2008;28(6):237–242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Jackson SL, Vann WF Jr, Kotch JB, Pahel BT, Lee JY. Impact of poor oral health on children’s school attendance and performance. Am J Public Health. 2011;101(10):1900–1906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Seirawan H, Faust S, Mulligan R. The impact of oral health on the academic performance of disadvantaged children. Am J Public Health. 2012; 102(9):1729–1734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Guarnizo-Herreño CC, Wehby GL. Children’s dental health, school performance, and psychosocial well-being. J Pediatr. 2012;161(6): 1153–1159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Savage MF, Lee JY, Kotch JB, Vann WF Jr. Early preventive dental visits: effects on subsequent utilization and costs. Pediatrics. 2004;114(4): e418–e423 [DOI] [PubMed] [Google Scholar]
- 47. Griffin S, Naavaal S, Scherrer C, %Griffin PM, Harris K, Chattopadhyay S. School-based dental sealant programs prevent cavities and are cost-effective. Health Aff (Millwood). 2016;35(12):2233–2240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Andrade C. Mean difference, standardized mean difference (SMD), and their use in meta-analysis: as simple as it gets. J Clin Psychiatry. 2020;81(5):20f13681. [DOI] [PubMed] [Google Scholar]
- 49. Mangione-Smith R. Measurement tools from research by Dr. Rita Mangione-Smith. Available at: https://www.kpwashingtonresearch.org/our-research/our-scientists/rita-mangione-smith-md-mph/measurement-tools-research-dr-rita-mangione-smith. Accessed March 10, 2022
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.