Abstract
OBJECTIVES:
When the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic began, experts raised concerns about in-person instruction in the setting of high levels of community transmission. We describe secondary transmission of SARS-CoV-2 within North Carolina (NC) K-12 school districts during a winter surge to determine if mitigation strategies can hinder within-school transmission.
METHODS:
From 10/26/2020–02/28/2021, 13 NC school districts participating in the ABC Science Collaborative were open for in-person instruction, adhered to basic mitigation strategies, and tracked community- and school-acquired SARS-CoV-2 cases. Public health officials adjudicated each case. We combined these data with that from August 2020 to evaluate the effect of the SARS-CoV-2 winter surge on infection rates, as well as weekly community- and school-acquired cases. We evaluated the number of secondary cases generated by each primary case, as well as the role of athletic activities in school-acquired cases.
RESULTS:
More than 100,000 students and staff from 13 school districts attended school in-person; of these, 4,969 community-acquired SARS-CoV-2 infections were documented by molecular testing. Through contact tracing, NC local health department staff identified an additional 209 infections among >26,000 school close contacts (secondary attack rate <1%). Most within-school transmissions in high schools (75%) were linked to school-sponsored sports. School-acquired cases slightly increased during the surge; however, within-school transmission rates remained constant, from pre-surge to surge, with approximately 1 school-acquired case for every 20 primary cases.
CONCLUSIONS:
With adherence to basic mitigation strategies, within-school transmission of SARS-CoV-2 can be interrupted, even during a surge of community infections.
Article summary
During the 2020–2021 winter surge of SARS-CoV-2 in North Carolina, K–12 within-school transmission remained extremely low among districts implementing basic mitigation strategies.
In March 2020, the World Health Organization declared that coronavirus disease 2019 (COVID-19), which causes severe acute respiratory coronavirus-2 (SARS-CoV-2), had officially become an international pandemic. Kindergarten through grade 12 (K–12) schools across the world preemptively closed their doors to in-person education in hopes of preventing disease spread. Early data from Europe,1 North Carolina (NC),2 and Wisconsin3 demonstrated that within-school transmission was uncommon with a few key mitigation strategies in place (i.e., masking, hand hygiene, physical distancing). Furthermore, early data also suggested that within-school transmission was independent of community transmission. Nonetheless, as community cases of SARS-CoV-2 soared in the late fall of 2020, major policy organizations, including the United States (U.S.) Centers for Disease Control and Prevention (CDC), recommended that community rates be used to make decisions related to in-person K–12 education.4
A year after initial school closures, many public K-12 schools remain closed or only partially open, with proponents of school closures often citing concerns about high levels of community spread, within-school crowding, and inability to improve classroom ventilation. The severe and negative impact of prolonged school closures on children’s physical, emotional, developmental, and academic health has been extensively documented, with increasing evidence of worsening behavioral health5; suicidality; physical abuse6,7; obesity and disordered eating8–11; and racial and ethnic disparities in digital access, food insecurity, school absenteeism, and failing grades.12–14 To further investigate the impact of community transmission on the risk of in-person, K–12 education, the ABC Science Collaborative (ABCs) evaluated within-school transmission of SARS-CoV-2 during a community SARS-CoV-2 surge in NC.
METHODS
Study Population
During the SARS-CoV-2 pandemic, the ABCs partnered with >50 K–12 public school districts in NC, including 13 districts that provided in-person instruction from 10/26/20–2/28/21. The ABCs developed in Summer 2020, when local NC school districts requested scientific input to help guide return-to-school policies during the COVID-19 pandemic. ABCs paired scientists with school communities to ensure leaders had the most relevant and up-to-date information on COVID-19 to guide decisions on school policies. The 13 districts also participated in biweekly educational and quality improvement sessions with ABCs faculty and agreed to prospectively track community- and school-acquired SARS-CoV-2 cases by school and week; these data were provided to the ABCs for analysis. The start of the study period was determined based on the start of the second quarter of K–12 instruction for most of the study districts. After this start date, communities across NC (and much of the U.S.) identified substantial increase in COVID-19 cases (i.e., “the surge”). The districts in this study had >100 cases/100,000 population/7 days, meeting the CDCs “red zone” in their school guidance from 2020 and first quarter 2021.
During the study period, NC law permitted minimal physical distancing (<6 feet) and hybrid education for pre-kindergarten (PreK) through 5th grade (PreK–5) students, and hybrid education with 6 feet of physical distancing for students in grades 6–12. Additionally, NC law required masking, including on school property. Masking during and outside of play for school sports was also required, and in most cases, teams were not permitted to use the locker rooms before, during, or after games. Districts varied in their implementation of minimal physical distancing and hybrid education with reduced capacity for PreK–5 students. NC did not have specific requirements for children with special educational needs to attend in-person classes.
Outcome Measures
The primary outcome was the number of school-acquired SARS-CoV-2 cases as confirmed by molecular diagnostic tests in participating public schools during the study period. Contact tracers from the participating school districts and the local health departments adjudicated each case as community- or school-acquired according to standard criteria15 and as part of standard contact tracing, to determine epidemiologic linkage and source of SARS-CoV-2 infection. Schools also noted whether school-acquired cases were associated with involvement in school-sponsored sports. In most cases, districts and the public health department were conservative in denoting within-school transmission versus community-acquired cases. For example, if cases were identified within classmates who were also known to be friends and gathered outside of school, infection was most often attributed to within-school transmission, although transmission more likely occurred in the unsupervised environment. The determination of epidemiologic linkage due to sports was made in the same manner as all other secondary infections, with timing of secondary infection (e.g., practice), and close contact (e.g., teammate) considered as part of standard contact tracing. Testing of close contacts was encouraged, but not required.
Data Sources
Superintendents or other leaders from participating school districts provided data on the number of students and staff participating in in-person instruction and the number of community- and school-acquired cases for each week during the study period. For some analyses, we used SARS-CoV-2 data from August 2020 for 11 of the participating school districts, as previously described.2 We obtained publicly available data from the NC Department of Public Instruction on district enrollment, as well as racial and ethnic distribution, for the 2020–2021 school year. We used data from the Johns Hopkins COVID-19 data repository16 for community SARS-CoV-2 rates in terms of new cases/1,000 persons/7 days for the county in which the school district was located.
Analyses
We used descriptive statistics to characterize the study population, as well as community- and school-acquired cases of SARS-CoV-2 in participating school districts. We combined data from this study period (October 2020–February 2021) and the prior reporting period (August 2020–October 2020)2 to evaluate the effect of the surge in weekly community SARS-CoV-2 rates on weekly community- and school-acquired cases in the study cohort. We also estimated the effect of the surge on the expected number of secondary cases generated within the school system for each primary case. This number was computed by dividing the total number of school-acquired cases each week by the total number of community-acquired cases. To understand the role of athletic activities on school-acquired cases, we also considered secondary transmission metrics after subtracting out the school-acquired cases that were due to sports. To estimate the effect of the surge on school-acquired cases (with and without cases resulting from sports), we conducted an interrupted time series analysis using an over-dispersed Poisson regression model for the transmission rates in the different periods. Post-hoc, we also conducted exploratory analyses to characterize the expected number of secondary cases for each primary case in elementary, middle, and high school. For these exploratory analyses, we excluded schools that were combined high and middle, or combined elementary and middle schools. We also excluded the largest district because of its size relative to the other districts and its primary focus on elementary schools in the face-to-face environment, which greatly skewed the available data, making it inappropriate for the analysis methods. We used R version 4.0.2 to conduct all statistical analyses.
Data collection and analyses were performed as part of the ABCs research program under a waiver of written consent (Duke University Institutional Review Board Pro00107036).
RESULTS
Study Cohort
The 13 districts participating in this study were diverse in terms of district sizes, racial and ethnic background of students, and rural or urban locations (Table 1). In total, the districts had >100,000 students and staff participating in in-person education during the study period. Overall, 12/13 (92%) participating districts systematically implemented minimal physical distancing (<6 feet) in PreK–5 for at least part of the study period, and all districts offered in-person education for at least some middle and high school students, in addition to their elementary school students. All districts permitted activities such as band, chorus, and high school sports (i.e., basketball and indoor track during the study period).
Table 1.
District Characteristics
| Unique ID | Enrolled Students1 | County Designation2 | %White1 | %Black1 | % Hispanic1 | %Economically Disadvantaged3 |
|---|---|---|---|---|---|---|
| 1 | 963 | Small metro | 47 | 34 | 12 | ≥90 |
| 2 | 1642 | Micropolitan | 45 | 8 | 22 | 54 |
| 3 | 2828 | Noncore | 84 | 1 | 13 | 57 |
| 4 | 3830 | Medium metro | 38 | 20 | 26 | 62 |
| 5 | 4963 | Medium metro | 66 | 3 | 27 | 57 |
| 6 | 4499 | Medium metro | 79 | 4 | 11 | 44 |
| 7 | 5766 | Medium metro | 72 | 7 | 16 | 44 |
| 8 | 7133 | Micropolitan | 70 | 2 | 25 | 60 |
| 9 | 12376 | Micropolitan | 62 | 15 | 15 | 39 |
| 10 | 20,038 | Large fringe metro | 63 | 14 | 15 | 40 |
| 11 | 22,971 | Small metro | 35 | 46 | 12 | 67 |
| 12 | 29,490 | Large fringe metro | 54 | 23 | 16 | 62 |
| 13 | 68,978 | Medium metro | 29 | 42 | 17 | 66 |
All of the districts were required to enforce masking, to adhere to 6-foot distancing for middle and high school, and to follow the NC Department of Health and Human Services StrongSchoolsNC Public Health Toolkit as their guide for mitigation strategies.15 The central tenants of the toolkit are masking, handwashing, and distancing in classrooms, where possible. Only one student was allowed per bus seat, and traffic flow was directed in school hallways. Additionally, the toolkit initially required health screening questions and temperature checks prior to entering school buildings, but due to lack of efficacy, this screening requirement was no longer required towards the end of the study period. Student cohorts were employed when possible to minimize spread and facilitate contact tracing. Additional caution (e.g., increased distancing, outdoor seating, instrument covers) was taken in circumstances where masking was not possible (e.g., meals, band).
Each district had specific procedures in place (e.g., daily walkthroughs) to evaluate and encourage the fidelity and adherence to masking of >90% of staff and students, >90% of the time, in the mainstream curriculum. Within the special needs curriculum, masking adherence for students was approximately 50%, with efforts made to ensure that students remained in small cohorts, practiced additional distancing when able, and that teachers and staff used supplemental personal protective equipment (i.e., face shields). None of the districts implemented large scale overhauls of their ventilation systems; districts had no choice but to continue to operate in classrooms and old buildings (and often times in schools where the windows did not open); no districts installed HEPA filters; and only one district upgraded filters to MERV 13, where possible (<30 classrooms). Each district made efforts to have students eat outside or ≥6 feet apart in their classrooms during breakfast and lunch. Students remained in classroom cohorts (11–25 students/cohort) in elementary school, grade A/B cohorts during middle school (e.g., 100 students/cohort), and A/B cohorts during high school (e.g., ~300–500 students/cohort). None of the districts implemented surveillance or screening testing of students or staff members. SARS-CoV-2 diagnostic testing was widely available free of charge in NC. All students and staff from each district were given explicit directions for how and when to get tested after exposure.
Community Rates and Community-acquired Infections in School Buildings
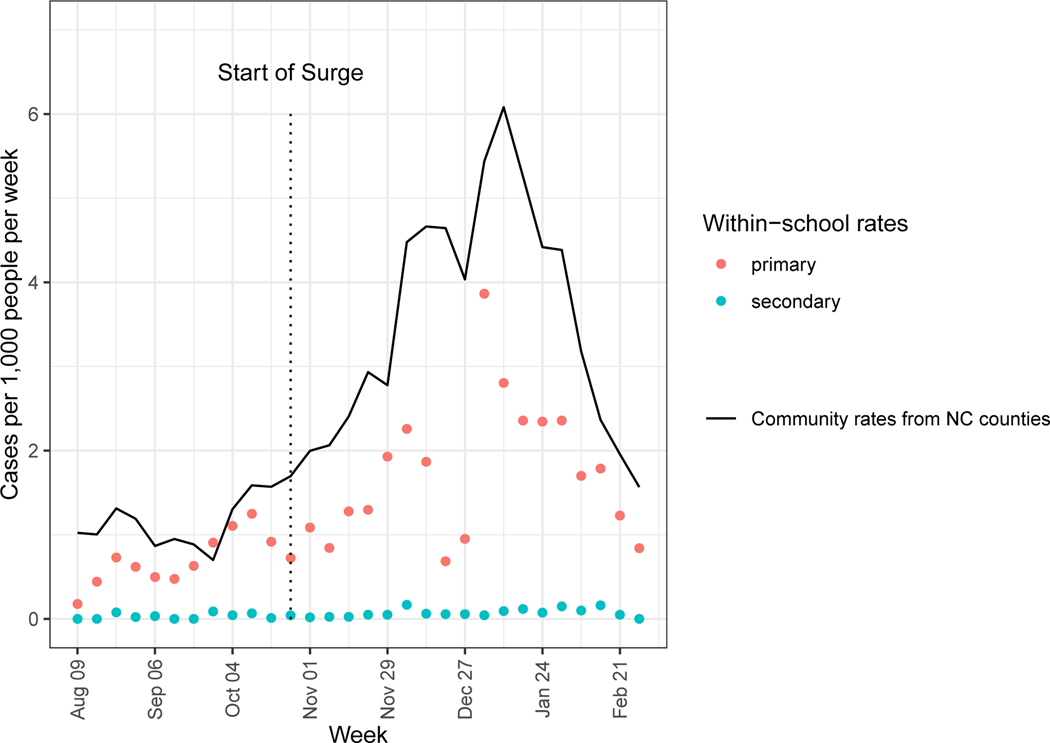
During the pre-surge period, the average weekly incidence of community-acquired infection was 1.17 cases/1,000 people, increasing to 3.6 during the surge. Across the 13 school districts, 4,969 students and staff with documented community-acquired SARS-CoV-2 infections, were present on school campuses. The rate of primary infections reported in the schools during the pre-surge and surge periods tracked closely with community rates (Figure 1).
Figure 1. Community Rates vs. Community- and School-acquired Infections.
Community rates of infection vs. community-acquired (primary) and school-acquired (secondary) infections in school buildings.
School-acquired Cases and their Relationship to Community Rates
Community-acquired infections within school buildings resulted in only 209 school-acquired infections, including 93 in students and staff in elementary, 26 in middle, and 87 in high school buildings (Table 2). These 209 infections occurred among >26,000 close contacts, resulting in a secondary attack rate of <1%. School-sponsored athletics were the setting of transmission for 75% of school-acquired infections among high school students and staff, with indoor basketball accounting for the majority of cases.
Table 2.
Community and School-acquired SARS-CoV-2 Infections
| Unique ID | Students Face-to-Face | Community -acquired | School-acquired | School-acquired by School Level | Quarantine | ||||
|---|---|---|---|---|---|---|---|---|---|
| Staff | Elementary | Middle | High | High Sports | |||||
| 1 | 760 | 169 | 44 | 4 | 1 | 0 | 3 | 1 | 21 |
| 2 | 1,024 | 230 | 101 | 0 | 0 | 0 | 0 | 0 | 119 |
| 3 | 2,320 | 404 | 116 | 6 | 3 | 1 | 2 | 2 | 626 |
| 4 | 3,055 | 457 | 229 | 1 | 0 | 0 | 1 | 1 | 1,243 |
| 5 | 4,284 | 658 | 131 | 37 | 11 | 4 | 22 | 22 | 1,652 |
| 6 | 4,338 | 648 | 315 | 11 | 3 | 2 | 6 | 3 | 2,243 |
| 7 | 5,068 | 665 | 293 | 11 | 5 | 3 | 3 | 0 | 1,995 |
| 8 | 5,467 | 928 | 479 | 12 | 0 | 0 | 12 | 10 | 5,000 |
| 9 | 10,249 | 1,536 | 405 | 27 | 17 | 4 | 6 | 2 | 2,762 |
| 10 | 16,523 | 2,316 | 427 | 53 | 32 | 10 | 11 | 11 | 2,182 |
| 11 | 17,000 | 2,712 | 306 | 26 | 12 | 2 | 12 | 9 | 2,277 |
| 12 | 19,434 | 3,231 | 1,149 | 21 | 0 | 0 | 0 | 0 | 5,202 |
| 13 | 48,549 | 9,180 | 974 | 19 | 9 | 0 | 9 | 5 | 1,297 |
| Total | 138,071 | 23,134 | 4,969 | 209 | 93 | 26 | 87 | 66 | 26,6192 |
Occurred in the central office.
Approimately 17% of the face-to-face population.
In the interrupted time-series analysis, we observed an increase in the rate of school-acquired cases during the surge period relative to pre-surge (relative rate = 2.3; 95% confidence interval [CI] 1.2–4.7), but the rate remained low through the time period studied, averaging slightly less than 0.08 school-acquired cases per 1,000 people. After subtracting out the cases due to sports, the relative increase in the rate of school-acquired cases decreased to 1.5 (95% CI 0.7–3.4). The within-school reproductive rate remained relatively constant from the pre-surge to surge period, with approximately 1 school-acquired case for every 24 primary cases during the surge. The within-school reproductive rate decreased slightly during the surge period after subtracting out the cases due to sports, with approximately 1 school-acquired case for every 35 primary cases.
Exploratory analyses evaluating the expected number of secondary cases for each primary case by elementary, middle, or high school were under powered to resolve differences between grade levels between the surge and pre-surge periods (Table 3).
Table 3.
Rate of Expected Secondary Infections per 100 Primary Cases (95% CI), by Grade Level
| Grade Level | Pre-surge Secondary Infections/100 Primary Cases (95% CI) | Post-surge | Post-surge without Sports |
|---|---|---|---|
| Elementary | 6.51 (3.70, 11.5) | 4.43 (2.82, 6.96) | 4.43 (2.91, 6.75) |
| Middle | 4.48 (1.73, 11.6) | 2.68 (1.25, 5.75) | 2.68 (1.31, 5.47) |
| High | 1.57 (0.49, 5.06) | 3.92 (2.36, 6.51) | 1.05 (0.42, 2.63) |
| CI, confidence interval | |||
DISCUSSION
In a racially and ethnically diverse real-world setting, with participants strictly adhering to masking and variable distancing, school-acquired SARS-CoV-2 infection was uncommon. As demonstrated by the low number of school-acquired cases compared to the number of community-acquired cases entering school buildings, along with the transmission observed when masking is more difficult (e.g., sports), we found that within-school transmission of SARS-CoV-2 can be prevented by simple mitigation strategies. These data also underscore how within-school transmission should be the key metric for evaluating whether schools and districts can and should be open to in-person instruction, rather than relying on community-acquired rates.
Our findings are notable, particularly since substantial credence has been given to the importance of community transmission in the debate to reopen schools, perhaps with the intent of encouraging communities to control transmission and help end the pandemic. Nevertheless, children were clearly not the priority in this public health recommendation; bars and sporting events were allowed to open even as schools remained closed. Moreover, based on the February 2021 CDC guidance for school reopening,4 94% of schools in the U.S. would not have qualified for reopening.17 Local control of school reopening resulted in differential application of “community transmission standards” and other guidelines, largely based on wealth, race, and ethnicity; private schools quickly opened in fall 2020, as did public schools in more rural locations. Meanwhile, public schools in urban locations, particularly those with substantial proportions of Black and Latino populations, remained shuttered.18,19 Uncoupling of community transmission and school reopening is not only supported by science, but promotes equity.
Although these data come from a large and diverse sample size, the results are not particularly surprising. Few public schools across the country that opened early in fall 2020 implemented overhauls of ventilation systems or had large-scale screening or surveillance testing. Yet where masking mandates were present and adhered to, there were no reports of substantial spread within the school environment, or of increased community spread; this is in contrast to the outbreaks observed in Tel Aviv, when schools opened without masking mandates in place.20 Data from NC in the first quarter of the school year demonstrated only 32 cases of school-acquired infection from 773 community-acquired cases within school buildings, at a time when community transmission was >4 times the “high level” of community transmission in CDC guidelines.2 Among 11 schools in Wisconsin, within-school transmission was limited despite diagnostic test positivity up to 40% in the surrounding communities.3 Similar findings were reported in schools in Utah and St. Louis, Missouri.21,22 Masking is known to be effective; there is no reason to believe that this central tenet of public health mitigation strategies would not also reduce transmission within school buildings, where adherence to policies and procedures is typically routine. Importantly, data collection required to monitor within-school transmission, the most important metric for identifying the safety of schools, is not dependent on collaboration with an entity such as the ABCs. Rather, data relies on collaboration between schools and public health officials. Data should be widely replicable, particularly as mitigation strategies (e.g., mask mandates) change over the coming year.
We also did not observe substantial differences in school-acquired cases between elementary, middle, and high school, despite minimal physical distancing implemented in elementary school or concerns that older students may be more likely to spread disease. Moreover, transmission in high schools largely resulted from participation in sports. While preliminary, these data are supportive of reduced distancing between children at schools, consistent with recent data from Massachusetts, which identified no significant differences in infections in schools with 3- vs. 6-foot distancing, and from other states (e.g., Utah) that never implemented a 6-foot distancing rule. Reduced distancing will also allow more children in school buildings at one time, effectively increasing their participation in in-person education. The findings of transmission through participation in athletics are also consistent with prior findings.23,24 Although NC has a mask mandate for athletics, these rules are inconsistently followed and enforced on athletic fields and courts. These data highlight the need for alternative strategies to prevent transmission (e.g., vaccination), provide early detection and mitigation of infection (e.g., testing), and added vigilance in enforcing masking in athletics and during sports team activities, similar to how these strategies are enforced in the classroom.
Limitations
Our study has some limitations. First, submission of data to the ABCs was voluntary and may have selected for school districts that were particularly adherent to preventive measures and value transparency. Second, these data relied on existing contact tracing practices, including adjudication of cases by the local health department, which can be imperfect and hampered by limitations in resources and personnel; however, contact tracing is the existing standard to identify infections and the sources of infections within the community, where community spread was consistently greater than that in schools. Moreover, in school buildings, attendance records are kept and shared with the public health department, increasing the likelihood that all contacts within a school are identified, compared to within the community, where refusal to reveal contacts is not infrequent. When compared to genotyping of SARS-CoV-2 specimens, the gold standard in identifying source of infection, contact tracing is an accurate method to identify the source of SARS-CoV-2 transmission.21 Third, no surveillance or screening testing was implemented in these districts, potentially underestimating the number of community-acquired infections entering school building; however, this analysis focuses on secondary infections arising from known primary cases. Fourth, testing of all students and staff after exposure to a community-acquired case could not be enforced given current policies in NC; however, testing was widely available at no cost within the state. Many of the included counties allowed testing out of quarantine according to CDC guidance, and uptake of testing among exposed teachers is known to be near universal. Fifth, to protect privacy of students and staff, most school districts did not track or report primary cases by staff compared to students, nor was data collected specific to extracurricular activities other than sports. Finally, it is unknown whether transmission among athletic teams (including players and coaches) occurred during play or other team events, such as travel to and from games.
CONCLUSIONS
With strict adherence to masking and some distancing, school-acquired SARS-CoV-2 infection is uncommon, even in the setting of high community infection rates. Consistent with prior data, schools can and should reopen safely.
What’s known on this subject
In Spring 2020, concerns about high levels of community transmission continued to be substantial barriers to in-person education for many school districts across the United States. The impact of higher levels of SARS-CoV-2 community transmission on within-school transmission remains unknown.
What this study adds
We examined >100,000 students and staff in 13 school districts implementing mitigation strategies and tracking within-school transmission of SARS-CoV-2 during a surge of infections in North Carolina. Community-acquired infections among school-aged children increased, but school-acquired infections remained uncommon.
CONTRIBUTORS’ STATEMENT
Drs. Zimmerman and Benjamin conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript.
Drs. Zimmerman, Brookhart, and Benjamin designed the data collection instruments, collected data, carried out the initial analyses, and reviewed and revised the manuscript.
Drs. Zimmerman, Akinboyo, Boutzoukas, McGann, Maradiaga Panayotti, Smith, Armstrong, Weber, Brookhart, Moorthy, and Benjamin reviewed and revised the manuscript.
Drs. Zimmerman and Benjamin conceptualized and designed the study, coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Acknowledgments:
Erin Campbell, MS, provided editorial review and submission; Liliana Suarez, BS, Emily D’Agostino, PhD, and Cody Neshteruk, PhD conducted partial literature review.
Funding/support:
This work was funded by the Trial Innovation Network, which is an innovative collaboration addressing critical roadblocks in clinical research and accelerating the translation of novel interventions into life-saving therapies. This work was also funded by the National Institute of Child Health and Human Development (NICHD) contract (HHSN275201000003I) for the Pediatric Trials Network (PI, Daniel Benjamin) and RADx-UP project: SARS-CoV-2 Screening and Diagnostic Testing for Return to K-12 Schools OTA (number: 1OT2HD107559-01; PI, Kanecia Zimmerman). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Role of the funder/sponsor:
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations:
- ABCs
ABC Science Collaborative
- CDC
Centers for Disease Control and Prevention
- CI
confidence interval
- COVID-19
coronavirus 2019
- K–12
kindergarten through 12th grade
- PreK
pre-kindergarten
- PreK–5
pre-kindergarten through 5th grade
- NC
North Carolina
- SARS-CoV-2
severe acute respiratory syndrome coronavirus 2
- U.S.
United States
Footnotes
Clinical trial registration: N/A
Conflict of interest disclosures: None
REFERENCES
- 1.European Centre for Disease Prevention and Control (ECDC). COVID-19 in children and the role of school settings in COVID-19 transmission. Available at: https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-schools-transmission-August%202020.pdf. Published August 6, 2020. Accessed May 27, 2021.
- 2.Zimmerman KO, Akinboyo IC, Brookhart MA, et al. Incidence and secondary transmission of SARs-CoV-2 infections in schools. Pediatrics. 2021;14(4):e2020048090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Falk A, Benda A, Falk P, Steffen S, Wallace Z, Høeg TB. COVID-19 cases and transmission in 17 K-12 schools - Wood County, Wisconsin, August 31-November 29, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(4):136–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC). Operational strategy for K-12 schools through phased prevention. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/operation-strategy.html. Updated May 15, 2021. Accessed May 27, 2021.
- 5.Patrick SW, Henkhaus LE, Zickafoose JS, et al. Well-being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics. 2020;146(4):e2020016824. [DOI] [PubMed] [Google Scholar]
- 6.Hill RM, Rufino K, Kurian S, Saxena J, Saxena K, Williams L. Suicide ideation and attempts in a pediatric emergency department before and during COVID-19. Pediatrics. 2021;147(3):e2020029280. [DOI] [PubMed] [Google Scholar]
- 7.Sidpra J, Abomeli D, Hameed B, Baker J, Mankad K. Rise in the incidence of abusive head trauma during the COVID-19 pandemic. Arch Dis Child. 2021;106(3):e14. [DOI] [PubMed] [Google Scholar]
- 8.Gassman-Pines A, Oltmans Ananat E, Fitz-Henley J. COVID-19 and parent-child psychological well-being. Pediatrics. 2020;146(4):e2020007294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jenssen BP, Kelly MK, Powell M, Bouchelle Z, Mayne SL, Fiks AG. COVID-19 and changes in child obesity. Pediatrics. 2021;147(5):e2021050123. [DOI] [PubMed] [Google Scholar]
- 10.Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID-19 related school closings and risk of weight gain among children. Obesity (Silver Spring). 2020;28(6):1008–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stockwell S, Trott M, Tully M, et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med. 2021;7:3000960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pew Research Center. The numbers behind the broadband ‘homework gap.’ Available at: https://www.pewresearch.org/fact-tank/2015/04/20/the-numbers-behind-the-broadband-homework-gap/. Published April 20, 2015. Accessed May 27, 2021.
- 13.Northwest Evaluation Association (NWEA). Learning during COVID-19: Initial findings on students’ reading and math achievement and growth. Published November 2020. Accessed May 27, 2021. [Google Scholar]
- 14.The News & Observer. Durham students failing, leaving district during COVID pandemic. Available at: https://www.newsobserver.com/news/local/counties/durham-county/article249159400.html. Updated February 12, 2021. Accessed May 27, 2021.
- 15.NCDHHS COVID-19 Response. StrongSchoolsNC Public Health Toolkit (K-12): Interim Guidance. Available at: https://covid19.ncdhhs.gov/media/164/open. Published June 30, 2020. Updated May 14, 2021. Accessed May 27, 2021. [Google Scholar]
- 16.Johns Hopkins Coronavirus Resource Center. Available at: https://coronavirus.jhu.edu/data. Accessed May 27, 2021.
- 17.Institute of Education Sciences (IES). Monthly school survey dashboard. Available at: https://ies.ed.gov/schoolsurvey/. Accessed May 27, 2021.
- 18.Parolin Z, Lee EK. Large socio-economic, geographic and demographic disparities exist in exposure to school closures. Nat Hum Behav. 2021;5(4):522–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaufman BG, Mahendraratnam N, Nguyen T, et al. Factors associated with initial public school reopening plans during the US COVID-19 pandemic: a retrospective study. J Gen Inter Med. 36(3):852–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stein-Zamir C, Abramson N, Shoob H, et al. A large COVID-19 outbreak in a high school 10 days after schools’ reopening, Israel, May 2020. Euro Surveill. 2020;25(29):2001352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hershow RB, Wu K, Lewis NM, et al. Low SARS-CoV-2 transmission in elementary schools — Salt Lake County, Utah, December 3, 2020–January 31, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(12):442–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dawson P, Worrell MC, Malone S, et al. Pilot investigation of SARS-CoV-2 secondary transmission in kindergarten through grade 12 schools implementing mitigation strategies — St. Louis County and City of Springfield, Missouri, December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(12):449–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Atherstone C, Siegel M, Schmitt-Matzen E, et al. SARS-CoV-2 Transmission Associated with High School Wrestling Tournaments — Florida, December 2020–January 2021. MMWR Morb Mortal Wkly Rep. 2021;70(4):141–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Siegel M, Kloppenburg B, Woerle S, Sjoblom S, Danyluk G. Notes from the Field: SARS-CoV-2 Transmission Associated with High School Football Team Members — Florida, September–October 2020. MMWR Morb Mortal Wkly Rep. 2021;70(11);402–404. [DOI] [PMC free article] [PubMed] [Google Scholar]