Abstract
Objective
Limited staffing and initial transmission concerns have limited rehabilitation services during the COVID-19 pandemic. The purpose of this analysis was to determine the associations between Activity Measure for Post-Acute Care (AM-PAC) mobility categories and allocation of rehabilitation, and in-hospital AM-PAC score change and receipt of rehabilitation services for patients with COVID-19.
Methods
This was a retrospective cohort study of electronic health record data from 1 urban hospital, including adults with a COVID-19 diagnosis, admitted August 2020 to April 2021. Patients were stratified by level of medical care (intensive care unit [ICU] and floor). Therapy allocation (referral for rehabilitation, receipt of rehabilitation, and visit frequency) was the primary outcome; change in AM-PAC score was secondary. AM-PAC Basic Mobility categories (None [21–24], Minimum [18–21], Moderate [10–17], and Maximum [6–9]) were the main predictor variable. Primary analysis included logistic and linear regression, adjusted for covariates.
Results
A total of 1397 patients (ICU: n = 360; floor: n = 1037) were included. AM-PAC mobility category was associated with therapy allocation outcomes for floor but not patients in the ICU: the Moderate category had greater adjusted odds of referral (adjusted odds ratio [aOR] = 10.88; 95% CI = 5.71–21.91), receipt of at least 1 visit (aOR = 3.45; 95% CI = 1.51–8.55), and visit frequency (percentage mean difference) (aOR = 42.14; 95% CI = 12.45–79.67). The secondary outcome of AM-PAC score improvement was highest for patients in the ICU who were given at least 1 rehabilitation therapy visit (aOR = 5.31; 95% CI = 1.90–15.52).
Conclusion
AM-PAC mobility categories were associated with rehabilitation allocation outcomes for floor patients. AM-PAC score improvement was highest among patients requiring ICU-level care with at least 1 rehabilitation therapy visit.
Impact
Use of AM-PAC Basic Mobility categories may help improve decisions for rehabilitation therapy allocation among patients who do not require critical care, particularly during times of limited resources.
Keywords: Acute Care, Hospitalization, Mobility, Rehabilitation
Introduction
As of September 2021, more than 3 million patients were hospitalized in the United States with disease due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection (ie, COVID-19).1 Although any hospitalization is associated with substantial rates of both immobility and deterioration of physical function,2–6 these consequences may be exacerbated among patients hospitalized due to COVID-19.7 Early in the pandemic, protocols aimed to conserve personal protective equipment (PPE) and limit health care providers’ (eg, rehabilitation therapists) direct contact with patients diagnosed with COVID-19.8,9 This focus on containing viral spread, conserving PPE, and decreasing clinician exposure may have resulted in deviations from recommended practices in some hospitals (eg, ABCDEF bundle for critically ill patients).10,11
Even prior to the COVID-19 pandemic, improved targeting of in-hospital rehabilitation services was a focus for optimizing care.12–15 The need to appropriately allocate rehabilitation therapy services became an even greater priority during the COVID-19 pandemic given that many hospitals experienced high patient volumes, capacity challenges, staffing shortages and turnover, crisis standards of care implementation, and unpredictable availability of postacute care resources including rehabilitation.16–18 These factors created additional challenges to efficiently identify patients who may benefit from therapy during hospitalization.
One strategy to improve the identification of patients who may benefit from in-hospital rehabilitation therapy is to implement a systematic, interdisciplinary measurement of physical function. The Activity Measure for Post-Acute Care Inpatient Short Form for Basic Mobility (AM-PAC Basic Mobility) is an assessment that quantifies a patient’s need for assistance during mobility tasks and can improve communication amongst an interdisciplinary team.14,15,19 The AM-PAC Basic Mobility was developed from an item pool consisting of 101 different items20; the shorter 6-item measure was validated in the acute care setting.21 The AM-PAC Basic Mobility can predict discharge disposition22,23 and identify possibly unnecessary referrals for rehabilitation services.12,14 Previous studies often used a single cut-point (≤16–17) to identify patients in need of acute care rehabilitation services and/or discharge to a postacute rehabilitation facility.23–25 Others used higher scores (22–24) to identify patients likely to discharge home and thus unlikely to require rehabilitation therapy while hospitalized,17 or used multiple categories to guide patient mobility goals during hospitalization.15 However, to our knowledge, no study has examined the relationship between AM-PAC Basic Mobility-derived functional categories and rehabilitation service allocation, especially during a global pandemic.
We sought to determine the association between limited mobility among patients hospitalized with COVID-19, as measured by the AM-PAC Basic Mobility assessment, and outcomes of rehabilitation therapy allocation. Secondarily, we sought to determine the relationship between receipt of rehabilitation therapy services and the change in AM-PAC Basic Mobility scores.
Methods
Study Design and Data Sources
We performed a retrospective cohort study using data collected from the University of Colorado Health Data Compass database following approval from the Colorado Multiple Institutional Review Board. The Health Data Compass comprises electronic health record (EHR) data from 12 hospitals within the University of Colorado health system. Due to limited availability of data on therapy visits, only University of Colorado Anschutz Medical Center patients were included in this analysis.
Study Population
All patients aged 18 years and older with a COVID-19 diagnosis who were admitted between August 2020 and April 2021 and had a complete hospital course were included in the analysis. COVID-19 diagnosis was defined by the presence of a positive polymerase chain reaction test or a COVID-19-associated diagnosis code documented in the EHR.26 Patients were excluded if they were hospitalized for obstetrics-related reasons.
To reflect important differences for determining rehabilitation therapy needs, analyses were stratified by level of medical acuity: (1) intensive care unit (ICU)-level care indicating any critical care received during hospitalization, and (2) no ICU-level care (floor). See Supplementary Appendix S1 for details of local guidelines for rehabilitation therapy referral and therapist management of patients with COVID-19.
Outcome Variables
Our primary outcome was therapy allocation as measured by 3 variables: (1) a binary variable indicating the presence/absence of a referral in the EHR for rehabilitation therapy services, (2) a binary variable indicating receipt of at least 1 rehabilitation visit (conditional on presence of referral), and (3) a continuous variable measuring visit frequency (conditional on presence of at least 1 visit). A rehabilitation therapy visit was identified through procedural codes that indicated a physical or occupational therapy visit occurred. Each charge code represented 1 visit, and it was possible for patients to receive more than 1 visit per day. Visit frequency was defined as the number of visits (including initial evaluation) per span of days between the therapy visit and hospital discharge.
Our secondary outcome was change in physical function as measured by AM-PAC Basic Mobility score. Beginning in August 2020, the AM-PAC Basic Mobility was implemented hospital-wide as standard documentation for nursing staff (daily) and physical therapy (each visit). The AM-PAC Basic Mobility has excellent interrater reliability (intraclass correlation coefficient = 0.96) between nurses and physical therapists19; it assesses 6 mobility tasks ranging from bed mobility to ascending 4 steps. Each task is scored using a 4-point ordinal scale reflecting level of assistance needed to complete the task (1 = total, 2 = a lot, 3 = a little, 4 = none).19 Raw scores range from 6 to 24, and higher scores indicate less assistance and higher potential mobility performance.27 For AM-PAC change score, raw scores were transformed to t-scores (range 0–100)28,29; change in AM-PAC t-score was calculated as the final recorded score minus the lowest recorded score. The minimal detectable change of the AM-PAC t-score is 4.5 points19 consistent with research that demonstrated the minimal detectable difference of health-related measures is usually 0.5 of an SD30; with an SD of 10, the minimal detectable difference is estimated to be 5 points on the t-scale. Thus, models evaluated the odds of improvement of at least 5 points (vs <5 points) in patients with at least 2 scores to provide a more conservative estimate. Individuals were excluded if their lowest recorded AM-PAC Basic Mobility raw score was 24.
Predictor Variables
First recorded AM-PAC Basic Mobility score was the primary predictor for therapy allocation (primary outcome). The first recorded AM-PAC Basic Mobility score was used to categorize patients because most referrals were placed within 48 hours of admission. The mobility categories were defined as follows using the Johns Hopkins Mobility Goal Calculator27: (1) “None” for raw scores 22 to 24; (2) “Minimum” 18 to 21; (3) “Moderate” 10 to 17; and (4) “Maximum” 6 to 9 (Tab. 1). The 2 indicators of therapy dose—(1) presence of at least 1 rehabilitation therapy visit, and (2) visit frequency—were the primary predictors to evaluate the change in AM-PAC score (secondary outcome).
Table 1.
Description of Mobility Categories Defined by AM-PAC Short Form for Basic Mobilitya
|
Short Mobility Category Name (Raw AM-PAC Score Range) |
Average Human Assistance | Potential In-Hospital Mobility Performance and/or Goal 28 and Functional Implications |
|---|---|---|
| None (22–24) | None to a little assistance for most tasks | Walk >25 feet May be able to ambulate in the household and community |
| Minimum (18–21) | A little assistance for most tasks | Walk >10 steps May need wheelchair for community navigation; may demonstrate limited household ambulation |
| Moderate (10–17) | A little to a lot of assistance for most tasks | May demonstrate ability to perform standing transfer to chair; may be confined to a single room in the home and need wheelchair for home and/or community ambulation |
| Maximum (6–9) | Unable to perform; a lot to total assistance for most tasks | May demonstrate ability to perform bed activities and tolerate sitting at edge of bed; may require dependent lift (mechanical or manual) to transfer out of bed |
AM-PAC = Activity Measure for Post-Acute Care.
Additional covariates were identified a priori based on prior literature23,31,32 and knowledge of local pandemic factors that may have influenced therapy allocation; these variables included age, sex (male, female), race/ethnicity (non-Hispanic, White [reference]; non-Hispanic African American or Black; Hispanic; or other), body mass index (BMI), mechanical ventilation (yes or no; ICU group only), length of stay in days, in-hospital mortality, and time period during the pandemic (categorical). Time period was categorized around the peak admission months to adjust for the possibility of higher demand for therapy services: August to October 2020 (reference), November 2020 to January 2021 (peak admissions), and February 2021 to April 2021. We did not adjust for in-hospital mortality for the outcomes of referral to rehabilitation services and receipt of at least 1 rehabilitation visit because of the unpredictable nature of COVID-19. We did adjust for mortality for visit frequency and AM-PAC score improvement because individuals who died were rarely seen for more than 1 visit, and there would be no AM-PAC score improvement. Because BMI was missing for many patients but weight was present, we imputed height based on sex and race/ethnicity to calculate BMI; the imputed BMI was used for analysis to reduce the number of observations dropped from analysis.
Statistical Analysis
We performed descriptive statistics to describe the population characteristics and outcomes stratified by ICU versus floor. Comparisons of characteristics across AM-PAC mobility categories within each care level (ICU and floor) were performed using analysis of variance or chi-square tests (or nonparametric or exact equivalents where appropriate); pairwise testing was not performed. For the primary outcomes, unadjusted logistic regression was used to estimate the odds of referral as a function of mobility category (None, reference category) and to estimate the odds for receipt of at least 1 therapy visit in the subset of patients who received a referral. Average visit frequency was log-transformed due to distributional right skew; then, linear regression was used to estimate the geometric mean visit frequency by mobility category among individuals who received at least 1 therapy visit (results reported as geometric means and percentage mean difference). We then performed adjusted analyses for each outcome in the same manner. For the secondary outcome, unadjusted and adjusted logistic regression was used to estimate the odds of AM-PAC score improvement as a function of (1) receipt of at least 1 visit (binary), and (2) visit frequency (continuous). We performed sensitivity analyses for imputed BMI for all models. All analyses were conducted via R statistical software (version 3.6.0; R Core Team, Vienna, Austria). All tests of association were 2-sided with a P value <.05 considered statistically significant.
Role of the Funding Source
The funders played no role in the design, conduct, or reporting of this study.
Results
Of 2331 individuals admitted with a diagnosis of COVID-19 by April 2021, obstetrics-related admissions (n = 114) and admissions prior to August 1, 2020 (n = 820) were excluded, resulting in 1397 individuals. Of these, 360 (26%) were in the ICU and 1037 (74%) on the floor. More than half of patients in the ICU (54.9%) and nearly all floor patients (93.0%) were discharged home. Of 360 patients in the ICU, 276 (76.7%) had a rehabilitation referral, and 222 (61.7%) had at least 1 visit. Of 1037 floor patients, 378 (36.5%) had a rehabilitation referral and 295 (28.4%) had at least 1 visit. Additional characteristics by level of care and mobility category are described in Table 2.
Table 2.
Patient and Hospital Course Characteristicsa
|
Intensive Care Unit (n = 357b) |
Floor (n = 1017c) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Individual and Hospital Variable |
None (22–24) n = 94 |
Minimum (18–21) n = 88 |
Moderate (10–17) n = 73 |
Maximum (6–9) n = 102 |
P |
None (22–24) n = 650 |
Minimum (18–21) n = 238 |
Moderate and Maximum (6–17) n = 129 |
P | |
| Age, y, mean (SD) | 57.05 (13.14) | 63.50 (17.54) | 69.77 (12.23) | 58.42 (14.34) | <.001 | 52.49 (15.28) | 62.36 (16.89) | 71.29 (16.99) | <.001 | |
| Sex: male, n (%) | 61 (64.9) |
59 (67.0) | 36 (49.3) |
66 (64.7) |
.09 | 354 (54.5) | 125 (52.5) | 55 (42.6) |
.05 | |
| Race/ethnicity, n (%) | .81 | <.001 | ||||||||
| White, non-Hispanic | 35 (37.2) |
30 (34.1) | 24 (32.9) |
33 (32.4) |
199 (30.6) | 89 (37.4) | 54 (41.9) |
|||
| Black or African American, non-Hispanic | <20 | <20 | <20 | <20 | 89 (13.7) | 25 (10.5) | 28 (21.7) |
|||
| Hispanic | 40 (42.6) |
36 (40.9) | 26 (35.6) |
45 (44.1) |
291 (44.8) | 88 (37.0) | 32 (24.8) |
|||
| Other | <20 | <20 | <20 | <20 | 71 (10.9) | 36 (15.1) | <20 | |||
| Interpreter needed: yes, n (%) | 26 (27.7) |
27 (30.7) | 22 (30.1) |
31 (30.4) |
.97 | 183 (28.2) | 73 (30.7) | 36 (27.9) |
.75 | |
| BMI, kg/m2, mean (SD) | 30.85 (7.23) | 29.38 (6.84) | 31.49 (10.06) | 32.22 (8.48) | .11 | 30.98 (8.00) | 31.13 (9.60) | 27.75 (8.11) | <.001 | |
| Insurer, n (%) | .01 | <.001 | ||||||||
| Commercial | 30 (31.9) |
<20 | <20 | 25 (24.5) |
193 (29.7) | 41 (17.2) | <20 | |||
| Medicaid | 21 (22.3) |
<20 | <20 | 28 (27.5) |
165 (25.4) | 54 (22.7) | 28 (21.7) |
|||
| Medicare | 30 (31.9) |
43 (48.9) | 41 (56.2) |
31 (30.4) |
174 (26.8) | 116 (48.7) | 80 (62.0) |
|||
| Other/unknown | <20 | <20 | <20 | <20 | 118 (18.2) | 27 (11.3) | <20 | |||
| LOS, d, median [IQR] | 11.00 [6.25–17.00] | 15.00 [8.75–23.25] | 14.00 [8.00–22.00] | 17.50 [12.00–26.00] | <.001 | 5.00 [3.00–7.00] | 5.00 [4.00–8.75] | 7.00 [5.00–12.00] |
<.001 | |
| Intubated: yes, n (%) | 32 (34.0) |
39 (44.3) | 33 (45.2) |
87 (85.3) |
<.001 | N/A | N/A | N/A | ||
| Consultation for rehabilitation services: yes, n (%) | 62 (66.0) |
68 (77.3) | 59 (80.8) |
86 (84.3) |
.02 | 134 (20.6) | 132 (55.5) | 109 (84.5) |
<.001 | |
| Days from admission to consultation: median [IQR] | 4.00 [0.00–6.25] | 2.50 [1.00–6.00] | 2.00 [1.00–5.00] | 2.00 [0.00–8.00] | .66 | 2.00 [0.00–3.00] | 1.00 [0.00–3.00] | 1.00 [0.00–1.00] |
.001 | |
| Rehabilitation therapy visit: yes, n (%) | 48 (51.1) |
54 (61.4) | 50 (68.5) |
70 (68.6) |
.05 | 89 (13.7) | 109 (45.8) | 97 (75.2) |
<.001 | |
| Days from consultation to first visit: median [IQR] | 1.00 [1.00–4.00] | 2.00 [1.00–3.00] | 1.00 [1.00–3.00] | 4.00 [1.00–7.00] | .04 | 1.00 [1.00–2.00] | 1.00 [1.00–2.00] | 1.00 [1.00–2.00] |
0.73 | |
| Number of visits: median [IQR] | 4.00 [2.75–10.00] | 5.00 [2.00–10.75] | 5.00 [2.250.00] | 9.00 [5.00–17.75] | .007 | 2.00 [1.00–4.00] | 2.00 [1.00–4.00] | 4.00 [2.00–7.00] |
<0.001 | |
| Visit frequency: median [IQR] | 0.50 [0.29–1.00] | 0.54 [0.32–1.00] | 0.79 [0.34–1.00] | 0.83 [0.54–1.20] | .02 | 0.50 [0.33–1.00] | 0.67 [0.43–1.00] | 0.75 [0.50–1.00] |
0.01 | |
| Discharge disposition, n (%) | .001 | <0.001 | ||||||||
| Home | 69 (74.2) |
46 (52.3) | 37 (50.7) |
44 (43.1) |
639 (98.6) | 212 (89.1) | 94 (72.9) |
|||
| Facility | <20 | <20 | <20 | 24 (23.5) |
<20 | 24 (10.1) | 33 (25.6) |
|||
| Expired in hospital | <20 | 28 (31.8) | 24 (32.9) |
34 (33.3) |
<20 | <20 | <20 | |||
Uses first recorded AM-PAC score; all scores are raw scores (range 6–24). Not all variables total the number of patients in each stratum due to missing data. <20 is used to censor the data. AM-PAC = Activity Measure for Post-Acute Care; BMI = body mass index; LOS = length of stay.
b Missing 3 due to missing AM-PAC scores.
c Missing 20 due to missing AM-PAC scores.
Characteristics Among Those Referred for and/or Receiving Rehabilitative Services
A higher proportion of patients in the ICU received a referral for rehabilitation therapy (76.7%) than floor patients (36.5%). Among patients in the ICU who received at least 1 therapy visit, median (interquartile range [IQR]) time to first visit was 2 (1–5) days from date of referral, and median (IQR) visit frequency was 0.72 (0.35–1.0) visits per day. Among 54 individuals who received a referral but were not seen, approximately two-thirds died in the hospital. Among 84 individuals without a referral, mean (SD) age was 55.9 (15.9) years, and all were either discharged home (60.7%) or died in the hospital (38.1%). Of all patients in the ICU, 193 were intubated, of whom 82 (42.3%) died while hospitalized. Additional characteristics of patients in the ICU by referral and treatment status are in Supplementary Table S1.
Among floor patients, the mean (SD) age was 57.1 (17.2) (Tab. 2). Of floor patients with a referral, 295 (78.0%) received at least 1 therapy visit. Median (IQR) time to receipt of first visit was 1 (1–2) day, and median (IQR) visit frequency was 0.67 (0.4–1.0) visits per day. Among patients with a referral but no treatment, most required little to no assistance with basic mobility tasks (raw score ≥18; 81.9%) and were discharged home (94.0%). Individuals without a referral (n = 659) tended to be younger (mean [SD] = 51.1 [14.9] years) and Hispanic (47.3%) and most were discharged home (97.4%). Additional characteristics of floor patients by referral and treatment status are in Supplementary Table S2.
Rehabilitation Allocation: Referral for Services, Receipt of Rehabilitation Services, Visit Frequency by AM-PAC Mobility Category
Among patients in the ICU, the distribution across mobility categories by referral and treatment status is depicted in Supplementary Figure S1. The odds of receiving a referral were highest for the Maximum category (P = .003) followed by the Moderate category (P = .04); however, these findings were not significant in adjusted analysis (Tab. 3; Suppl. Tab. S3 [full model results]). Mobility category was not associated with odds of receiving at least 1 rehabilitation visit in unadjusted and adjusted analyses (Suppl. Tab. S5 [full model results]); length of stay was associated with 8% (95% CI = 4%–14%; P < .001) higher odds per day of receiving a visit, and intubation was associated with 65% (95% CI = 18%–85%; P = .02) lower odds of receiving a visit (vs no intubation). Geometric mean visit frequency was highest in the Maximum category (0.81 visits/day; P = .01), but these differences were not statistically significant in adjusted analyses (Tab. 4; Suppl. Tab. S6 [full model results]). Visit frequency was 30.9% (95% CI = 1.9%–68.0%; P = .04) higher among patients who required intubation (vs no intubation) and 72.7% (95% CI = 19.6%–149.4%; P = .004) higher for unknown insurance status (vs commercial insurance).
Table 3.
Unadjusted and Adjusted Odds of Referral for and Receipt of Rehabilitation Therapy Visit Among All Eligible Patientsa
| Odds of Receiving a Referral for Rehabilitation | |||||||
|---|---|---|---|---|---|---|---|
| AM-PAC Mobility Category | OR | 95% CI | P | aORb | 95% CI | P | |
| Unadjusted: n = 357c | Adjusted: n = 352d | ||||||
| ICU | Minimum (18–21) | 1.75 | 0.92–3.42 | .09 | 1.15 | 0.52–2.51 | .73 |
| Moderate (10–17) | 2.18 | 1.07–4.59 | .04 | 1.32 | 0.56–3.19 | .54 | |
| Maximum (6–9) | 2.77 | 1.42–5.60 | .003 | 2.36 | 0.97–5.86 | .06 | |
| Unadjusted: n = 1017e | Adjusted: n = 960f | ||||||
| Floor | Minimum (18–21) | 4.80 | 3.49–6.61 | <.001 | 3.02 | 2.06–4.43 | <.001 |
| Moderate (10–17) | 21.29 | 12.59–38.08 | <.001 | 10.88 | 5.71–21.91 | <.001 | |
| Maximum (6–9) | 19.25 | 6.24–84.00 | <.001 | 4.03 | 1.12–19.50 | .05 | |
| Odds of Receiving ≥1 Rehabilitation Therapy Visit | |||||||
| AM-PAC Mobility Category | OR | 95% CI | P | aORb | 95% CI | P | |
| Unadjusted: n = 275g | Adjusted: n = 271h | ||||||
| ICU | Minimum (18–21) | 1.13 | 0.48–2.61 | .78 | 1.42 | 0.55–3.69 | .47 |
| Moderate (10–17) | 1.62 | 0.65–4.22 | .31 | 2.15 | 0.75–6.39 | .16 | |
| Maximum (6–9) | 1.28 | 0.56–2.86 | .55 | 1.76 | 0.66–4.75 | .26 | |
| Unadjusted: n = 375i | Adjusted: n = 354j | ||||||
| Floor | Minimum (18–21) | 2.40 | 1.36–4.31 | .003 | 2.21 | 1.18–4.22 | .01 |
| Moderate (10–17) | 4.25 | 2.08–9.42 | <.001 | 3.45 | 1.51–8.55 | .005 | |
| Maximum (6–9) | 3.29 | 0.86–21.60 | .13 | 2.36 | 0.52–16.93 | .31 | |
None (22–24) is the reference category. AM-PAC = Activity Measure for Post-Acute Care; aOR = adjusted odds ratio; ICU = intensive care unit; OR = odds ratio.
b ICU: adjusted for sex, race/ethnicity, age, body mass index (BMI), length of stay, intubation status, insurance payer, and categorical time. Floor: adjusted for sex, race/ethnicity, age, BMI, length of stay, insurance payer, and categorical time.
c Includes all patients in the ICU; 3 removed due to missing AM-PAC scores.
d Five additional removed from adjusted analysis due to missing BMI and weight for imputation.
e Includes all patients on the floor; 20 removed due to missing AM-PAC scores.
f Fifty-two additional removed from adjusted analysis due to missing BMI and weight for imputation.
g Patients included conditional on the presence of a referral; 1 removed due to missing AM-PAC score.
h Four additional removed from adjusted analysis due to missing BMI and weight for imputation.
i Patients included conditional on presence of a referral; 3 removed due to missing AM-PAC score.
j Twenty-one additional removed from adjusted analysis due to missing BMI and weight for imputation.
Table 4.
Unadjusted Geometric Mean and Adjusted Percentage Mean Difference for Visit Frequency Among Patients Receiving Any Rehabilitation Servicesa
| Visit Frequency | ||||||
|---|---|---|---|---|---|---|
| AM-PAC Mobility Category |
Geometric Mean (95% CI) |
% Mean Difference (95% CI) |
P |
% Mean Difference (95% CI) |
P | |
| Unadjusted: n = 222b | Adjustedc: n = 219d | |||||
| ICU | None (22–24) (reference) | 0.53 (0.41 to 0.69) | ||||
| Minimum (18–21) | 0.54 (0.42 to 0.68) | 1.1 (−28.6 to 43.2) | .95 | 13.91 (−16.15 to 54.76) | .40 | |
| Moderate (10–17) | 0.61 (0.47 to 0.78) | 13.7 (−20.2 to 62.0) | .48 | 17.52 (−14.83 to 62.15) | .32 | |
| Maximum (6–9) | 0.81 (0.65 to 0.99) | 51.2 (8.9 to 110.0) | .01 | 26.66 (−6.35 to 71.29) | .12 | |
| Unadjusted: n = 295e | Adjustedc: n = 277f | |||||
| Floor | None (22–24) (reference) | 0.56 (0.47 to 0.65) | ||||
| Minimum (18–21) | 0.63 (0.55 to 0.73) | 14.0 (−8.0 to 41.3) | .23 | 18.47 (−4.02 to 46.24) | .11 | |
| Moderate (10–17) | 0.79 (0.67 to 0.93) | 41.9 (13.0 to 78.3) | .003 | 42.14 (12.45 to 79.67) | .003 | |
| Maximum (6–9) | 0.59 (0.39 to 0.89) | 5.8 (−32.2 to 65.2) | .80 | 2.98 (−34.21 to 61.20) | .90 | |
AM-PAC = Activity Measure for Post-Acute Care; ICU = intensive care unit.
b Patients included conditional on receipt of ≥1 rehabilitation visits (53 excluded for this reason).
c ICU: adjusted for sex, race/ethnicity, age, body mass index (BMI), intubation status, insurance payer, in-hospital death, and categorical time. Floor: adjusted for sex, race/ethnicity, age, BMI, insurance payer, and categorical time.
d Three additional removed from adjusted analysis due to missing BMI and weight for imputation.
e Patients included conditional on receipt of ≥1 rehabilitation visits (80 excluded for this reason).
f Eighteen additional removed from adjusted analysis due to missing BMI and weight for imputation.
Among floor patients, the distribution across mobility categories by referral and treatment status is depicted in Supplementary Figure S1. Maximum, Moderate, and Minimum categories had significantly greater odds of receiving a referral than the None category (Tab. 3; Suppl. Tab. S4 [full model results]). Minimum and Moderate categories had significantly increased odds for receiving at least 1 therapy visit in unadjusted analyses. Similar but attenuated results were seen in adjusted analyses (Tab. 3; Suppl. Tab. S5 [full model results]). Geometric mean visit frequency was highest in the Moderate category (0.79 visits/day; P = .003), and this difference was maintained in adjusted analysis (Tab. 4; Suppl. Tab. S6 [full model results]). Visit frequency was 40.2% (95% CI = 6.7%–84.2%; P = .02) higher for people identifying as Black (vs White) and 152.3% (95% CI = 66.5%–282.2%; P < .001) higher for patients with unknown insurance status (vs commercial insurance).
Change in AM-PAC Scores by Receipt of Rehabilitation Therapy and Visit Frequency
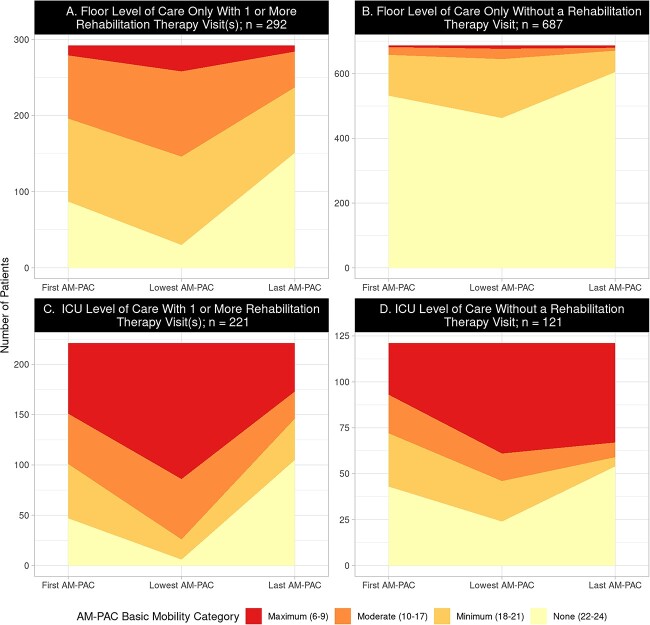
Of 1397 individuals, 256 were excluded for lowest recorded AM-PAC score = 24; a further 76 were excluded for less than 2 documented scores, and 46 for missing BMI and weight, resulting in 1019 included in secondary analyses (ICU: n = 327; floor: n = 692). Changes in AM-PAC mobility categories during hospitalization are shown in the Figure.
Figure.
Change in AM-PAC mobility categories during hospitalization stratified by intensive care unit (ICU) and floor. Change in the number of people by AM-PAC category for 3 different measurements (first recorded, lowest recorded at any time during length of stay, and last recorded). For example, in Panel A, the number of people who scored within the None category decreased from the first recorded AM-PAC score to the lowest recorded AM-PAC score but then increased from the lowest recorded AM-PAC score to the last recorded AM-PAC score. AM-PAC = Activity Measure for Post-Acute Care.
Among 327 patients in the ICU, those with a rehabilitation therapy visit had 5.35 (95% CI = 3.29–8.83; P < .001) greater odds of AM-PAC score improvement compared with patients without a visit; findings persisted in adjusted analysis (Tab. 5; Suppl. Tab. S7 [full model results]). Medicare insurance (vs commercial insurance) and 2 time periods (October 2020–January 2021 [peak admissions] and February 2021–April 2021 vs August 2020–October 2020) were associated with reduced odds of AM-PAC score improvement in adjusted analyses. An increase in visit frequency by 0.5 (ie, 1 visit every 2 days) was associated with greater odds of improvement in unadjusted (odds ratio [OR] = 2.89; 95% CI = 2.12–4.10; P < .001) but not adjusted analyses (adjusted odds ratio [aOR] = 1.52; 95% CI = 1.03–2.47; P = .06) (Tab. 5; Suppl. Tab. S8 [full model results]).
Table 5.
Unadjusted and Adjusted Odds of AM-PAC Score Improvementa
| Therapy Allocation Variable | AM-PAC Score Improvement (t-score ≥ 5 Points) | ||||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | aOR | 95% CI | P | ||
| ICU (n = 327b) | No rehabilitation visit (reference) | 1.0 | |||||
| ≥1 rehabilitation visitsc | 5.35 | 3.29–8.83 | <.001 | 4.17 | 1.58–11.32 | .004 | |
| Visit frequency (0.5)d | 2.89 | 2.12–4.10 | <.001 | 1.52 | 1.03–2.47 | .06 | |
| Floor (n = 692e) | No rehabilitation visit (reference) | 1.0 | |||||
| ≥1 rehabilitation visitsf | 1.56 | 1.14–2.14 | .006 | 1.56 | 1.02–2.41 | .04 | |
| Visit frequency (0.5)g | 1.11 | 0.97–1.27 | .13 | 1.13 | 0.97–1.32 | .13 | |
AM-PAC = Activity Measure for Post-Acute Care; aOR = adjusted odds ratio; BMI = body mass index; ICU = intensive care unit; LOS = length of stay.
b ICU—excluded: <2 AM-PAC scores (n = 18); lowest AM-PAC score = 24 (n = 11); missing BMI and weight (n = 4).
c Adjusted for AM-PAC mobility category (using lowest AM-PAC score), sex, race/ethnicity, age, BMI, length of stay, intubation status, insurance payer, in-hospital mortality, and categorical time.
d Adjusted for AM-PAC mobility category (using lowest AM-PAC score), sex, race/ethnicity, age, BMI, intubation status, insurance payer, in-hospital mortality, and categorical time.
e Floor—excluded: <2 AM-PAC scores (n = 58); lowest AM-PAC score = 24 (n = 245); missing BMI and weight (n = 42).
f Adjusted for AM-PAC mobility category (using lowest AM-PAC score), sex, race/ethnicity, age, BMI, length of stay, insurance payer, and categorical time.
g Adjusted for AM-PAC mobility category (using lowest AM-PAC score), sex, race/ethnicity, age, BMI, insurance payer, and categorical time.
Among 692 patients receiving floor-level care only, those with a rehabilitation therapy visit had 1.56 (95% CI = 1.14–2.14; P = .006) greater odds of AM-PAC score improvement compared with patients without a visit, and this association was similar in adjusted analysis (Tab. 5; Suppl. Tab. S7 [full model results]). An increase in visit frequency by 0.5 was not associated with change in AM-PAC score during hospitalization in unadjusted or adjusted analyses [Tab. 5; Suppl. Tab. S8 [full model results]).
Results from sensitivity analyses excluding patients without an available BMI showed these same trends, though the magnitude and significance of AM-PAC mobility category estimates were mildly attenuated in most models.
Discussion
During the COVID-19 pandemic, we found a higher proportion of ICU than floor patients received rehabilitation therapy. In adjusted analyses, AM-PAC mobility categories were not associated with rehabilitation allocation outcomes among patients in the ICU but were significantly associated with rehabilitation allocation among floor patients. The Moderate AM-PAC category was associated with all allocation outcomes, and the Minimum category was associated with both receipt of referral and receipt of at least 1 visit. Lastly, odds of AM-PAC Basic Mobility score improvement were highest among patients in the ICU, and score change was strongly associated with receipt of therapy in both groups.
The high proportion of referral and receipt of rehabilitative services among patients in the ICU is likely reflective of the bundled, team-based treatment recommended for critically ill patients.33–36 These standards of care, combined with ongoing integration of rehabilitation therapists into our ICU care teams, may explain the lack of an association between AM-PAC mobility category and therapy allocation in patients in the ICU. An important component of these standards (eg, ABCDEF bundle) is “E” early mobilization, especially for those requiring mechanical ventilation, as it supports weaning from ventilation.35 Our results showed mechanical ventilation was associated with higher visit frequency—conditional upon receipt of at least 1 rehabilitation visit and when adjusting for in-hospital mortality—suggesting our rehabilitation staff were able to maintain ICU standards of care during the pandemic. Further, these ventilated patients had the greatest odds for AM-PAC score improvement, and receipt of therapy was an independent factor in that improvement.
Approximately 40% of patients in the ICU never received either a referral or a rehabilitation session. We suspect that this reflects: (1) lack of functional impairment or rapid improvement of functional deficits, or (2) medical instability/death. Supporting the first possibility, most patients without a referral (61.9%) had the potential for at least in-room ambulation per first recorded AM-PAC Basic Mobility score (≥18). These patients probably required little to no assistance for bed mobility, transfers, and standing, suggesting the potential to mobilize successfully with nonrehabilitation staff (eg, nursing) and hence clinicians likely recognized these patients did not require in-hospital rehabilitation therapy services for mobility progression. A similar approach implemented by Klein et al.27 prepandemic empowered nursing staff to mobilize patients rather than refer to rehabilitation therapy. Supporting the second possibility—medical instability or death—38.1% of patients without a referral and 64.8% of patients with a referral but no therapy visit died while hospitalized, and we did not adjust for mortality in these analyses. It is reasonable to assume many of these patients were unstable throughout their hospitalization, precluding rehabilitation therapy services (Suppl. Appendix S1). Further, mechanical ventilation was associated with reduced odds of receiving both a referral and at least 1 rehabilitation therapy visit; this is not surprising because 43% of patients who received mechanical ventilation died during hospitalization.
Receipt of rehabilitation therapy was associated with greater odds of AM-PAC Basic Mobility score improvement; however, there was no relationship between visit frequency and AM-PAC Basic Mobility score improvement. This finding differs from a study by Johnson et al.31 that identified a significant relationship between visit frequency and AM-PAC Basic Mobility score at discharge for a cohort of patients with COVID-19; their cohort exhibited lower mean AM-PAC Basic Mobility scores at admission, and a higher proportion required intensive care. If considering only our patients in the ICU, patients in both studies were similar, and visit frequency was significantly associated with AM-PAC score improvement in our unadjusted analyses.
Most patients admitted to the hospital due to COVID-19 never required intensive care; guidelines may help clinicians better identify noncritical patients most likely to benefit from in-hospital rehabilitation therapy. Locally, rehabilitation guidelines were focused on patients with physical function impairment that would require therapist intervention for improvement (Suppl. Appendix S1). Such patients often required ongoing rehabilitation therapy to progress to community discharge, facilitate efficient physical function recovery, mitigate immobility harms, and/or elucidate postacute care discharge location. In our cohort, rehabilitation therapy resources were allocated to patients with more physical impairment, and those with greater impairment (Moderate category) had the highest mean visit frequency. Prior research supports that patients with an AM-PAC score of 17 or less are more likely to discharge to a rehabilitation facility versus home22–25 and thus may benefit from in-hospital rehabilitation services. However, those with little impairment (Minimum category) may also benefit from in-hospital rehabilitation to reduce length of stay, mitigate hospital-acquired functional decline, and facilitate safe and efficient discharge to the community.17 Among floor patients, those who identified as Black, non-Hispanic had higher visit frequency (vs White); this finding may have emerged because individuals of Black race/ethnicity tend to have higher comorbidity burden, which is associated with impaired physical function37 and greater likelihood of hospitalization due to severe COVID-19 illness.38,39
An additional area for improving referral and treatment practices among floor-only patients is to understand who receives a referral but no rehabilitation therapy. These referrals could represent missed therapy needs or, contrarily, could create additional work that can further strain limited rehabilitation therapy resources if these patients do not require in-hospital rehabilitation.12–14 Martinez et al.12 evaluated possible overuse of in-hospital physical therapy and found that 38% of referrals were for patients with an admission AM-PAC score greater than 18 who were discharged to home and were considered “potentially inappropriate.” Fifty-five percent of our floor patients met this definition for “potentially inappropriate” referral, representing a higher rate compared with Martinez et al. However, a portion of these referrals may have been to elucidate postacute rehabilitation needs because patients hospitalized with COVID-19 who were high functioning may still have required postacute rehabilitation to manage sequelae of the infection.40 The need for and benefit of rehabilitation following COVID-19 is increasingly recognized41 because long-term, multisystem deficits are identified even among those who were not hospitalized.42,43 Other patients may have received both a referral and therapy sessions while hospitalized due to anticipated lack of access to postacute rehabilitation therapy, as suggested by the higher frequency of therapy among those in our cohort with unknown insurance status.
Study Limitations
There are some limitations to the present study. First, we used the first recorded AM-PAC Basic Mobility score to group patients into functional categories. This score may not have been reflective of a patient’s actual function at the time of referral or therapy intervention but provided a conservative estimate because patients tended to decline following admission. AM-PAC Basic Mobility is a judgement as to how much, if any, assistance a patient would need for mobility. Although this lends itself to successful integration into EHRs via rapid assessment and ease of documentation, it does not provide data on actual mobility performance. Therefore, an AM-PAC score of 18 or more does not guarantee that the patient ambulated during hospitalization but rather implies the potential to do so. Despite this limitation, the AM-PAC Basic Mobility is moderately correlated with tests of lower extremity strength and walking ability.19 Furthermore, AM-PAC score improvements may have been due, in part, to spontaneous functional recovery following medical stabilization. Few patients scored in the Maximum category (n < 20) among our floor cohort making interpretation limited for this group. As an EHR-based study, we had limited data on other factors that contribute to decisions about rehabilitation therapy allocation including prior level of function and the potential for physical function improvement via alternate modes (eg, time, medical treatment). We had a large amount of missing data for comorbidities and were unable to adjust for those conditions likely to influence recovery (eg, cardiovascular disease, diabetes, total comorbidity burden).44–46 Finally, this analysis was limited to patients hospitalized with COVID-19 during a global pandemic. Although this was a heterogeneous group of patients, our analysis may not be representative of other patient populations or hospital systems, and our results may not be generalizable to patients hospitalized during nonpandemic times.
Conclusions
We found a high rate of rehabilitation referral and receipt among patients in the ICU. Lower AM-PAC Basic Mobility scores were associated with rehabilitation allocation among floor patients, and visit frequency was the highest for Moderate category (floor patients only). AM-PAC Basic Mobility score improvement was greatest among patients requiring ICU-level care who received at least 1 rehabilitation therapy visit. Overall, these results align with the proposals, guidelines, and experiences of other academic institutions that judiciously constructed rehabilitation therapy approaches to address the rehabilitation needs of patients hospitalized with COVID-19.17,18 Use of AM-PAC Basic Mobility categories may help improve decisions regarding rehabilitation therapy allocation among non-critically ill hospitalized patients, particularly during times of limited resources. Future studies should aim to improve identification of patients who may benefit most from in-hospital rehabilitation therapy, test optimal dosing of therapy (frequency, therapy minutes, content, etc), and identify strategies to efficiently allocate rehabilitation resources while reducing unnecessary referrals and visits. Future studies should evaluate the impact of in-hospital rehabilitation services on longer-term function.
Supplementary Material
Contributor Information
Michelle R Rauzi, Physical Therapy Program, Department of Physical Medicine and Rehabilitation, University of Colorado, Aurora, Colorado USA.
Kyle J Ridgeway, Physical Therapy Program, Department of Physical Medicine and Rehabilitation, University of Colorado, Aurora, Colorado USA; Inpatient Rehabilitation Therapy Department, University of Colorado Hospital, University of Colorado Health, Aurora, Colorado, USA.
Melissa P Wilson, Department of Biomedical Informatics, University of Colorado, Aurora, Colorado, USA.
Sarah E Jolley, Division of Pulmonary and Critical Care Medicine, Department of Medicine, University of Colorado, Aurora, Colorado, USA.
Amy Nordon-Craft, Physical Therapy Program, Department of Physical Medicine and Rehabilitation, University of Colorado, Aurora, Colorado USA.
Jennifer E Stevens-Lapsley, Physical Therapy Program, Department of Physical Medicine and Rehabilitation, University of Colorado, Aurora, Colorado USA; VA Eastern Colorado Geriatric Research, Education, and Clinical Center (GRECC), VA Eastern Colorado Health Care System, Aurora, Colorado, USA.
Kristine M Erlandson, Division of Infectious Diseases, Department of Medicine, University of Colorado-Anschutz Medical Campus, Aurora, Colorado, USA.
Author Contributions
Concept/idea/research design: M.R. Rauzi, K.J. Ridgeway, S.E. Jolley, A. Nordon-Craft, J.E. Stevens-Lapsley, K.M. Erlandson
Writing: M.R. Rauzi, K.J. Ridgeway, S.E. Jolley, A. Nordon-Craft, K.M. Erlandson
Data analysis: M.R. Rauzi, M.P. Wilson
Project management: M.R. Rauzi
Fund procurement: M.R. Rauzi, J.E. Stevens-Lapsley, K.M. Erlandson
Providing facilities/equipment: K.M. Erlandson
Providing institutional liaisons: S.E. Jolley, K.M. Erlandson
Consultation (including review of manuscript before submitting): M.P. Wilson, J.E. Stevens-Lapsley, K.M. Erlandson
Funding
This study was supported by the National Institutes of Health and the Health Data Compass Data Warehouse (healthdatacompass.org). K.M. Erlandson and J.E. Stevens-Lapsley were supported by National Institutes of Health/National Institute on Aging grant (R01 AG 054366-05S1). M.R. Rauzi was supported in part by a Promotion of Doctoral Studies I Scholarship from the Foundation for Physical Therapy Research and National Institutes of Health Research Training grant (T32AG000279), funded by the National Institute on Aging. S.E. Jolley was supported by a grant from the National Institutes of Health/National Institute on Alcohol Abuse and Alcoholism (K23 AA 026315–05).
Ethics Approval
This study was approved by the Colorado Multiple Institutional Review Board.
Data Availability
Due to the identifiable nature of the EHR data, the dataset is not available.
Disclosures
The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and reported no conflicts of interest.
References
- 1. Centers for Disease Control and Prevention . COVID data tracker: new admissions of patients with confirmed COVID-19 per 100,000 population by age group, United States. Atlanta, GA: US Department of Health and Human Services, CDC. Updated September 25, 2021. Accessed September 27, 2021. https://covid.cdc.gov/covid-data-tracker/#new-hospital-admissions [Google Scholar]
- 2. Falvey JR, Mangione KK, Stevens-Lapsley JE. Rethinking hospital-associated deconditioning: proposed paradigm shift. Phys Ther. 2015;95:1307–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: "she was probably able to ambulate, but I'm not sure". JAMA. 2011;306:1782–1793. [DOI] [PubMed] [Google Scholar]
- 4. Brown CJ, Friedkin RJ, Inouye SK. Prevalence and outcomes of low mobility in hospitalized older patients. J Am Geriatr Soc. 2004;52:1263–1270. [DOI] [PubMed] [Google Scholar]
- 5. Brown CJ, Redden DT, Flood KL, Allman RM. The underrecognized epidemic of low mobility during hospitalization of older adults. J Am Geriatr Soc. 2009;57:1660–1665. [DOI] [PubMed] [Google Scholar]
- 6. Mudge AM, McRae P, McHugh K, et al. Poor mobility in hospitalized adults of all ages. J Hosp Med. 2016;11:289–291. [DOI] [PubMed] [Google Scholar]
- 7. Daunter AK, Bowman A, Danko J, Claflin ES, Kratz AL. Functional decline in hospitalized patients with COVID-19 in the early months of the pandemic. PM R. 2022;14:198–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.US Department of Health and Human Services. Hospital experiences responding to the COVID-19 pandemic: results of a national pulse survey March 23–27, 2020. Accessed March 2, 2023. https://oig.hhs.gov/oei/reports/oei-06-20-00300.pdf.
- 9. Garcia-Houchins S, Cullen D, Belton BM. Preparing hospitals for COVID-19. The Joint Commission; 2019 [webinar]. https://www.jointcommission.org/-/media/tjc/documents/resources/webinar-replays/hap-coronavirus-webinar-final.pdf. [Google Scholar]
- 10. Devlin JW, O'Neal HR Jr, Thomas C, et al. Strategies to optimize ICU liberation (A to F) bundle performance in critically ill adults with coronavirus disease 2019. Crit Care Explor. 2020;2:e0139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liu K, Nakamura K, Katsukawa H, et al. Implementation of the ABCDEF bundle for critically ill ICU patients during the COVID-19 pandemic: a multi-national 1-day point prevalence study. Front Med (Lausanne). 2021;8:735860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Martinez M, Cerasale M, Baig M, et al. Defining potential overutilization of physical therapy consults on hospital medicine services. J Hosp Med. 2021;16:553–555. [DOI] [PubMed] [Google Scholar]
- 13. Hobbs JA, Boysen JF, McGarry KA, Thompson JM, Nordrum JT. Development of a unique triage system for acute care physical therapy and occupational therapy services: an administrative case report. Phys Ther. 2010;90:1519–1529. [DOI] [PubMed] [Google Scholar]
- 14. Probasco JC, Lavezza A, Cassell A, et al. Choosing wisely together: physical and occupational therapy consultation for acute neurology inpatients. Neurohospitalist. 2018;8:53–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Young D, Kudchadkar SR, Friedman M, et al. Using systematic functional measurements in the acute hospital setting to combat the immobility harm. Arch Phys Med Rehabil. 2022;103:S162–S167. [DOI] [PubMed] [Google Scholar]
- 16.US Department of Health and Human Services. Hospitals reported that the COVID-19 pandemic has significantly strained health care delivery. Results of a national pulse survey February 22–26, 2021. 2021 Accessed March 2, 2023. 10.1038/s41526-020-0103-2. [DOI]
- 17. Kim SY, Kumble S, Patel B, et al. Managing the rehabilitation wave: rehabilitation services for COVID-19 survivors. Arch Phys Med Rehabil. 2020;101:2243–2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. McLaughlin KH, Simon L, Friedman M, Siddiqui ZK, Ficke JR, Kantsiper ME. Lessons learned from implementing rehabilitation at a COVID-19 field hospital. Am J Phys Med Rehabil. 2021;100:1027–1030. [DOI] [PubMed] [Google Scholar]
- 19. Hoyer EH, Young DL, Klein LM, et al. Toward a common language for measuring patient mobility in the hospital: reliability and construct validity of interprofessional mobility measures. Phys Ther. 2018;98:133–142. [DOI] [PubMed] [Google Scholar]
- 20. Haley SM, Andres PL, Coster WJ, Kosinski M, Ni P, Jette AM. Short-form activity measure for post-acute care. Arch Phys Med Rehabil. 2004;85:649–660. [DOI] [PubMed] [Google Scholar]
- 21. Jette DU, Stilphen M, Ranganathan VK, Passek SD, Frost FS, Jette AM. Validity of the AM-PAC "6-clicks" inpatient daily activity and basic mobility short forms. Phys Ther. 2014;94:379–391. [DOI] [PubMed] [Google Scholar]
- 22. Hoyer EH, Young DL, Friedman LA, et al. Routine inpatient mobility assessment and hospital discharge planning. JAMA. Intern Med. 2019;179:118–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Young DL, Colantuoni E, Friedman LA, et al. Prediction of disposition within 48 hours of hospital admission using patient mobility scores. J Hosp Med. 2020;15:540–543. [DOI] [PubMed] [Google Scholar]
- 24. Jette DU, Stilphen M, Ranganathan VK, Passek SD, Frost FS, Jette AM. AM-PAC "6-clicks" functional assessment scores predict acute care hospital discharge destination. Phys Ther. 2014;94:1252–1261. [DOI] [PubMed] [Google Scholar]
- 25. Warren M, Knecht J, Verheijde J, Tompkins J. Association of AM-PAC "6-clicks" basic mobility and daily activity scores with discharge destination. Phys Ther. 2021;101:pzab043. [DOI] [PubMed] [Google Scholar]
- 26. Kim J, Neumann L, Paul P, et al. Privacy-protecting, reliable response data discovery using COVID-19 patient observations. J Am Med Inform Assoc. 2021;28:1765–1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Klein LM, Young D, Feng D, et al. Increasing patient mobility through an individualized goal-centered hospital mobility program: a quasi-experimental quality improvement project. Nurs Outlook. 2018;66:254–262. [DOI] [PubMed] [Google Scholar]
- 28. Thissen D, Pommerich M, Billeaud K, Williams VSL. Item response theory for scores on tests including polytomous items with ordered responses. Appl Psychol Meas. 1995;19:39–49. [Google Scholar]
- 29. Lord FM, Wingersky MS. Comparison of IRT true-score and equipercentile observed-score "Equatings". Appl Psychol Meas. 1984;8:453–461. [Google Scholar]
- 30. Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41:582–592. [DOI] [PubMed] [Google Scholar]
- 31. Johnson JK, Lapin B, Green K, Stilphen M. Frequency of physical therapist intervention is associated with mobility status and disposition at hospital discharge for patients with COVID-19. Phys Ther. 2021;101:pzaa181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Freburger JK, Chou A, Euloth T, Matcho B. Variation in acute care rehabilitation and 30-day hospital readmission or mortality in adult patients with pneumonia. JAMA Netw Open. 2020;3:e2012979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pun BT, Balas MC, Barnes-Daly MA, et al. Caring for critically ill patients with the ABCDEF bundle: results of the ICU liberation collaborative in over 15,000 adults. Crit Care Med. 2019;47:3–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Barnes-Daly MA, Phillips G, Ely EW. Improving hospital survival and reducing brain dysfunction at seven California community hospitals: implementing PAD guidelines via the ABCDEF bundle in 6,064 patients. Crit Care Med. 2017;45:171–178. [DOI] [PubMed] [Google Scholar]
- 35. Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373:1874–1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Devlin JW, Skrobik Y, Gélinas C, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46:e825–e873. [DOI] [PubMed] [Google Scholar]
- 37. Groll DL, To T, Bombardier C, Wright JG. The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol. 2005;58:595–602. [DOI] [PubMed] [Google Scholar]
- 38. Gupta R, Agrawal R, Bukhari Z, et al. Higher comorbidities and early death in hospitalized African-American patients with Covid-19. BMC Infect Dis. 2021;21:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sze S, Pan D, Nevill CR, et al. Ethnicity and clinical outcomes in COVID-19: a systematic review and meta-analysis. EClinicalMedicine. 2020;29:100630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tleyjeh IM, Saddik B, Ramakrishnan RK, et al. Long term predictors of breathlessness, exercise intolerance, chronic fatigue and well-being in hospitalized patients with COVID-19: a cohort study with 4 months median follow-up. J Infect Public Health. 2022;15:21–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Debeuf R, Swinnen E, Plattiau T, et al. The effect of physical therapy on impairments in COVID-19 patients from intensive care to home rehabilitation: a rapid review. J Rehabil Med. 2022;54:jrm00242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. van Kessel SAM, Olde Hartman TC, Lucassen P, van Jaarsveld CHM. Post-acute and long-COVID-19 symptoms in patients with mild diseases: a systematic review. Fam Pract. 2022;39:159–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Crook H, Raza S, Nowell J, Young M, Edison P. Long COVID-mechanisms, risk factors, and management. BMJ. 2021;374:n1648. [DOI] [PubMed] [Google Scholar]
- 44. Huang I, Lim MA, Pranata R. Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia—a systematic review, meta-analysis, and meta-regression. Diabetes Metab Syndr. 2020;14:395–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Brojakowska A, Eskandari A, Bisserier M, et al. Comorbidities, sequelae, blood biomarkers and their associated clinical outcomes in the Mount Sinai health system COVID-19 patients. PLoS One. 2021;16:e0253660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ge E, Li Y, Wu S, Candido E, Wei X. Association of pre-existing comorbidities with mortality and disease severity among 167,500 individuals with COVID-19 in Canada: a population-based cohort study. PLoS One. 2021;16:e0258154. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Due to the identifiable nature of the EHR data, the dataset is not available.