Abstract
Background
Few studies have investigated disparities in disordered eating between new immigrant and native adolescents in Taiwan. This study examines the differential pathways to disordered eating in these two populations.
Methods
This cross-sectional study analyzed data collected from March to June 2019. In total, 729 adolescents aged between 13 and 16 years recruited from 37 classes in 3 middle schools in New Taipei City were included in the final analysis. Standardized assessment tools measured disordered eating (EAT-26) and psychological distress (BSRS-5). Generalized structural equation modeling was used to conduct the path analysis.
Results
The prevalence of disordered eating was significantly higher in immigrant adolescents than in their native counterparts. Multipath models indicated that weight-teasing driven by overweight and obese status and weight overestimation could lead to disordered eating through psychological distress; however, the pathways differed for the two groups studied. Family weigh-teasing indirectly leads to disordered eating through psychological distress for native adolescents; by contrast, for immigrant adolescents, friend weigh-teasing indirectly leads to disordered eating through psychological distress. Additionally, weight overestimation directly leads to disordered eating and indirectly through psychological distress to disordered eating for immigrant adolescents.
Conclusion
This study offers a plausible explanation of the differences in the paths to disordered eating between immigrant and native adolescents in Taiwan, which was not reported previously. The study urges the need for school-based prevention programs to improve immigrant students’ mental health.
Keywords: Disordered eating, Psychological distress, Weight overestimation, Immigrant adolescents, Weight-teasing
This study fills the gap in the literature on disparities in disordered eating and factors associated with disordered eating among immigrant adolescents in Taiwan. To our knowledge, this is the first study focusing on disordered eating among immigrant adolescents in Taiwan. The unique contribution of this research is to elucidate the different pathways leading to disordered eating for native and immigrant adolescents. In native adolescents, weight-teasing by family members but not by friends was indirectly related to disordered eating through psychological distress. In adolescents with an immigrant background, weight-teasing by friends was indirectly associated with disordering eating through psychological distress. Additionally, weight overestimation is a unique risk factor directly and indirectly through psychological distress related to disordered eating for immigrant adolescents. As a highly Westernized country, the Taiwanese’s mainstream ideal body shape is “thinness.” Substantial social discrimination against obese adolescents regarding peer acceptance and sexual attraction may put immigrant adolescents at an increased risk of experiencing body dissatisfaction, psychological stress, and eating disorder symptoms due to their minority status, struggling to adapt to a social environment different from their parents, and wanting peer acceptance. The study urges the need for school-based prevention programs to improve immigrant students’ mental health.
Background
Disordered eating is irregular, including restrained and binge eating [1]. Frequent dieting, compulsive eating behaviors, and chronic weight fluctuations are common characteristics of problematic eating behavior that may progress to eating disorders if left untreated [1]. Disordered eating concerns and behaviors have been documented in various cultures and ethnic groups in the United States and Europe [2–4]. Disordered eating has also increased in several Asian countries [5]. Several studies adopting the EAT-26 revealed that approximately 10.4% and 17.1% of adolescent Taiwanese girls presented with disordered eating behaviors [6, 7]. These prevalence rates are similar to those of teenage girls in South Korea (14.8%) [8] and those of students aged 12–25 years in China [9].
Since 1994, Taiwan’s Southbound Policy concerning China and countries in the Association of Southeast Asian Nations contributed to a substantial increase in transnational marriages in Taiwan [10]. In 2016, the government initiated a new Southbound Policy to promote further international investments and business/trade activities between Taiwan and Southeastern countries, including Vietnam, Thailand, and others [11]. According to the 2019 Ministry of the Interior report, 15.8% of marriages were transnational. Of those transnational marriages, about 74.1% came from Mainland China and Southeast Asian countries, and foreign brides accounted for 72% of transnational marriages [12].
Most new immigrant families are relatively disadvantaged and have lower economic and educational levels. They are often stigmatized as “Problematic minorities” and experience discrimination [13]. Transnational marriage is usually considered unfavorable, a way to escape poverty. Taiwanese men who marry foreign-born women from Southeastern countries often have low socioeconomic status and education levels, most of whom are low-level farmers, workers, or fishermen residing in rural areas [14]. Immigrant mothers usually have high rates of psychological distress (70%) and depression (24%). Their children (sometimes called second-generation immigrants) suffer from physiological or psychological problems [15, 16], compared with children those whose parents are Taiwanese [17, 18]. Immigrant mothers also experience more discrimination than Taiwanese mothers [15, 19].
Acculturation may be defined as social interaction and coping styles that individuals adopt when interacting with individuals and groups from another culture [20]. The acculturation process is often accompanied by psychological stress, known as acculturation stress resulting in adapting from one culture to another [20, 21]. Acculturative tension derives from participating in activities, values, beliefs, and practices of the dominant culture versus the culture of origin [22] and is associated with a host of mental health symptoms such as general psychological distress [23], depression, and suicide [24] and eating disorder symptoms [25]. While several studies indicate the association between the extent of acculturation into the dominant culture and eating disorders in ethnic minority women in the United States [21, 22], few concerns were directed to disordered eating among adolescent immigrants in East Asian countries, including Taiwan. As a highly Westernized society, Taiwan may have an increased risk of body dissatisfaction and disordered eating for adolescents because the ideal body image purported by Western sculpture is much thinner than the actual body size [26]. Minority adolescents who acculturate to Taiwanese culture with a cultural value of thinness may be at a greater risk for experiencing body dissatisfaction and eating disorder symptoms because of their minority status and psychological anxiety from adapting to the dominant culture [27]. However, no research so far has explored this issue. We hypothesize that native and immigrant adolescents might present different pathways to disordered eating because immigrant adolescents may experience additional stress from the acculturation process. Previous studies have indicated that children of immigrant mothers have a higher risk of poor mental health and exhibit more somatic and internalized symptoms than children whose parents are Taiwanese [18, 19].
Pathways to disordered eating in adolescents
Models of disordered eating have indicated that the pathways to disordered eating are complex and multifaceted [28]. Overweight status and related weight teasing are often the primary factors for disordered eating [29–33]. Numerous studies provided strong evidence indicating peer and family weight-related teasing is associated with disordered eating in adolescents [29–39]; psychological dysfunction resulting from weight-teasing is often considered the pathway leading to disordered eating behaviors [20, 40–47]. For example, a study conducted in China supported the pathway of weight teasing to depression to disordered eating [30]. A Malaysian university student survey also identified that eating disorders could lead to depression through weight teasing [48].
Additionally, the impact of the ideal Western body image on Asian countries is considered a contributing factor to the increasing prevalence of disordered eating in these countries [20, 41]. Bodyweight misperception is a discrepancy between an individual’s actual and self-perceived body weight, including weight underestimation and overestimation [49]. Extensive studies from various cultural contexts, including Taiwan, supports body dissatisfaction as a risk factor for disordered eating [6, 26, 30, 37, 39, 45, 50–52], and body dissatisfaction is closely linked to weight misperception [49, 53, 54]. In particular, evidence supports that weight overestimation, rather than weight underestimation, leads to disordered eating, such as restricted eating [54, 55].
Weight overestimation is related to psychological distress. Studies conducted with American adolescents have reported a significant association between depression and misperception about being overweight or obese [56, 57]. However, longitudinal studies have revealed mixed findings. A survey among American adolescents revealed that depression increased weight overestimation [56]. In contrast, another study conducted among Chinese adolescents indicated that weight overestimation caused an increased risk of depression [53].
Control variables
Most studies on adolescent eating disorders have involved only women[2, 6, 58–61]. However, recent studies have revealed the existence of eating disorders among men as well [62–64], showing that men have similar prevalence as women in terms of concern about diet, exercise (i.e., exercising compulsively as a means of controlling one’s weight or body shape) and binge eating habits [62–64]. Therefore, sex is controlled in the models.
In addition, as indicated above, most new immigrant families are of lower economic and educational levels [13, 65]. Father’s education is usually used as the family’s socioeconomic index [66], however, The mothers of children from immigrant families were significantly less likely to attain high education than mothers born in Taiwan [28]. Therefore, the models controlled the father’s and mother’s high education. Lastly, the study sample concerns adolescents aged 13–15, and age plays a vital role in everyday life [67]. Therefore, the models also controlled for age.
The present study
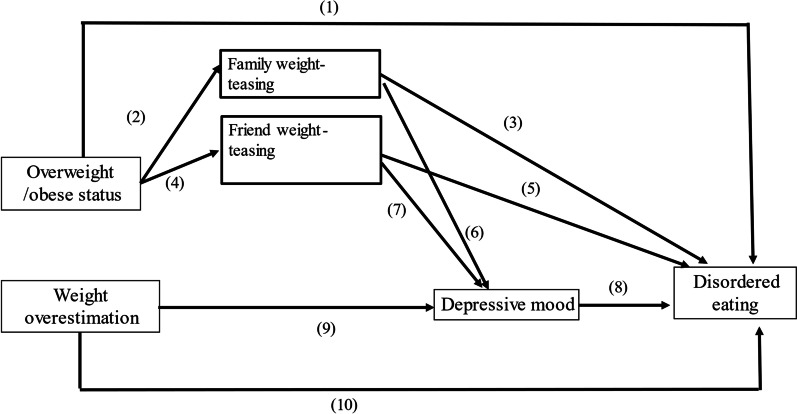
Based on previous studies, we hypothesized a multipath model of disordered eating (Fig. 1) and identified ten direct and indirect paths to disordered eating in adolescents, as shown in Fig. 1. However, due to the scarcity of studies on the associations between immigrant adolescents and disordered eating, we first specified the same hypothetical pathways to disordered eating for native and immigrant adolescents. Then, we examined the multipath pathway model for the entire study sample and investigated if being an immigrant adolescent was significantly associated with a high chance of eating disorders. Second, we stratified the study sample into two groups, native and immigrant adolescents, to examine the differences in the pathways to disordered eating for each group.
Fig. 1.
Hypothesized multipath model for disordered eating
Path 1 is from overweight/obese status directly to disordered eating. Path 2 is from overweight/obese status to family weight-teasing and disordered eating (path 3). Path 4 is from overweight/obese status to friend weight-teasing and then to disordered eating (path 5). Path 6 is from family weight-teasing to psychological distress, and path 7 is from friend weight-teasing to psychological distress. Path 8 is from psychological distress to disordered eating. Path 9 is from weight overestimation to psychological distress. Path 10 is from weight overestimation directly to disordered eating. The multipath models were controlled for sex, age, and family socioeconomic status (represented by fathers’ education level).
Methods
Study participants
This study used a cross-sectional design conducted from March to June 2019 in New Taipei City, Taiwan. The participants were recruited by convenience sampling from 23 classes at three junior high schools in New Taipei City. Three junior high schools were selected through the researchers’ personal contacts, and verbal approvals by the schools’ superintendents and teachers were obtained. Written informed consent forms were collected from the participants and their legal guardians before they participated in this study. Each student completed a 20–25 min questionnaire in a classroom setting.
One hundred fifty-seven participants (15.4%, 157 out of 1020 total participants) were excluded because of incomplete information regarding their parents’ informed consent. Among the 863 valid participants, 134 participants (15.5%) were also excluded from the analysis due to insufficient data on variables of interest. Comparisons between the participants excluded (n = 134) and included (n = 729) in the study indicated no significant difference in demographic characteristics, such as gender, family and friend teasing, family and friend support, and psychological distress state, and EAT-26 scores [29]. A total of 729 participants from 37 classes in 3 middle schools were included for data analysis. The study participants were between 13 and 16 years old, with a mean age of 13.83 years (standard deviation [SD] = 0.98). The study was approved by Taiwan’s Research Ethics Committee (NTU NO. 201901HS030).
Survey development and measures
A structured self-administered questionnaire was developed for data collection. A prior qualitative study (unpublished work) was conducted in 2018 by interviewing 30 junior high school students in New Taipei City to draft the initial questionnaire. Expert validity was conducted to evaluate the initial questionnaire. Subsequently, the questionnaire was modified based on the suggestions from the three experts. A pretest was then performed among 38 junior high school students to improve the questionnaire further. Finally, the pilot study was conducted among 196 junior high school students to ensure reliability and validity of the final questionnaire [29, 68].
Eating attitudes test-26 (EAT-26)
We used the EAT-26 to measure symptoms and characteristics of disordered eating. The EAT-26 comprises 26 questions on disordered eating attitudes and behaviors, and questions are answered using a Likert-type scale, where 0 = never, rarely, or sometimes; 1 = often; 2 = usually; and 3 = always [69]. Disordered eating is indicated by a score of ≥ 20 [69]. Because EAT-26 is an assessment tool widely used to screen for disordered eating among adolescents from various cultural contexts, it was chosen to measure disordered eating in our study participants [6, 20, 37, 41, 52, 70–73].
Psychological distress was measured by the Five-item Brief Symptom Rating Scale (BSRS-5). BSRS-5 is a short assessment tool to screen patients and community members for psychological disorders, especially depression and anxiety [74]. The BSRS-5 has been widely used in research on mental health among Chinese and Southeast Asian immigrants in Taiwan [75] and to assess psychopathological symptoms in adolescents [76, 77]. Therefore, we adopted the BSRS-5 to assess adolescents’ psychological distress in our study. The internal consistency of BSRS-5 in this study was satisfactory (Cronbach’s alpha = 0.89). The BSRS-5 contains items measuring “difficulty sleeping,” “feeling nervous,” “feeling easily distressed or angry,” “feeling depressed or in a low mood,” and “feeling inferior.” The BSRS-5 uses a Likert-type scale, where 0 = not at all, 1 = mild, 2 = moderate, 3 = severe, and 4 = extremely severe. Scores ≥ 10 indicate moderate to severe psychological distress.
Friend weight-teasing was measured by asking participants whether their friends had made fun of or mocked them about their weight or body shape. Respondents replied with a Yes or No.
Family weight-teasing was measured by asking participants whether their family members made fun of or mocked them about their weight or body shape. Respondents replied with a Yes or No.
Weight overestimation is measured by the difference between respondents’ self-reported weight and height (for calculating BMI) and their perceived body size. Perceived body size was measured by asking respondents, “what do you think of your body size” and respondents replied as underweight, normal, overweight, or obese. BMI was categorized into underweight, normal, overweight, and obese using official sex and gender-specific cutoffs of BMI from Taiwan Health Promotion, Ministry of Health and Welfare [78]. Respondents whose BMI-based body size is normal or underweighted but perceived themselves as overweight and obese were classified as having weight overestimation.
Controls
Immigrant status Respondents with one or two of their parents who are foreign were classified as immigrant adolescents. This survey question did not specifically ask whether the mother or the father has a foreign nationality. The immigrant adolescents in this study were assumed to be the second-generation immigrant adolescents.
Father with high education
Respondents who reported their father’s education as college or above was coded as having a father with high education.
Mother with high education
Respondents who reported their mother’s education as college or above was coded as having a mother with high education.
Age was considered a continuous variable.
Sex referred to the biological distinction between male and female, and coded as 1 for male, 0 for female.
Statistical analysis
We conducted the univariate analysis to describe the frequencies and means of basic demographic information and factors associated with disordered eating. Moreover, we measured the prevalence rates of disordered eating in all participants and stratified these rates by immigrant status. A chi-square test was used to compare factors associated with disordered eating, and individual items from the EAT-26 were compared between the immigrant and native adolescents. Because the dependent and mediating variables are categorical, we conducted a path analysis using generalized structural equation modeling (GSEM) to test our hypotheses. Indirect and total effects were unavailable because the dependent variable is categorical [79]. The Goodness fit index was also not reported in GSEM models. Therefore, we documented 2000 bootstrapping adjusted odds ratios (AOR) and 95% confidence interval for each path [79].
We created a multipath model separately for immigrant and native adolescents. All statistical analyses were performed using Stata. STATA is a general-purpose statistical software package developed by Stata Corp for data manipulation, visualization, statistics, and automated reporting. The current version is Stata 17, released in April 2021.
Results
Univariate and bivariate analysis
The mean age of the study participants was 13.83 years (SD ± 0.98), with girls and boys constituting 51.03% (n = 372) and 48.97% (n = 357) of the sample, respectively (Table 2). Of the participants, 24.42% (n = 178) were immigrants, whereas 75.58% (n = 551) were Taiwanese. A disordered eating prevalence rate of 11.39% was observed among the participants, with disordered eating being defined by a score of ≥ 20 on the EAT-26 (mean = 11.68, SD ± 8.38). The prevalence of disordered eating was 16.85% (mean EAT-26 score = 12.56, SD ± 8.85) among immigrant adolescents and 9.62% (mean EAT-26 score = 11.40, SD ± 8.21) among native Taiwanese adolescents. The immigrant adolescents had a significantly higher prevalence of disordered eating (X2 = 6.98, p = 0.01) and mean EAT-26 score (X2 = 70.09, p = 0.01) than their Taiwanese counterparts. Approximately 16.32% (n = 119) and 8.02% (n = 58) of our study participants exhibited moderate to severe psychological distress and bodyweight misperceptions, respectively. Furthermore, relative to Taiwanese adolescents, a significantly lower percentage of immigrant adolescents had mothers who received higher education (30.85% vs. 19.66%; X2 = 8.33, p = 0.00). Details are presented in Table 1.
Table 2.
The eating attitudes test-26 (N = 729)
| All | Immigrant adolescents | Native adolescents | X2 (df) | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| Items | N1 | % | N | % | N | % | ||
| 1. I am terrified about being overweight | 261 | 35.80 | 69 | 38.76 | 192 | 34.85 | 0.90 (1) | 0.34 |
| 2. I avoid eating when I am hungry | 139 | 19.07 | 36 | 20.22 | 103 | 18.69 | 0.20 (1) | 0.65 |
| 3. I find myself preoccupied with food | 121 | 16.60 | 28 | 15.73 | 93 | 16.88 | 0.13 (1) | 0.72 |
| 4. I have gone on eating binges where I feel that I may not be able to stop | 65 | 8.92 | 16 | 8.99 | 49 | 8.89 | 0.00 (1) | 0.97 |
| 5. I cut my food into small pieces | 170 | 23.32 | 39 | 21.91 | 131 | 23.77 | 0.26 (1) | 0.61 |
| 6. I aware of the calorie content of foods that I eat | 97 | 13.31 | 33 | 18.54 | 64 | 11.62 | 5.81 (1) | 0.12 |
| 7. I particularly avoid food with a high carbohydrate content (i.e. bread, rice, potatoes, etc.) | 71 | 9.74 | 20 | 11.24 | 51 | 9.26 | 0.60 (1) | 0.44 |
| 8. I feel that others would prefer if I ate more | 207 | 28.40 | 56 | 31.46 | 151 | 27.40 | 1.09 (1) | 0.30 |
| 9. I vomit after I have eaten | 11 | 1.51 | 3 | 1.69 | 8 | 1.45 | 0.05 (1) | 0.82 |
| 10. I feel extremely guilty after eating | 47 | 6.45 | 16 | 8.99 | 31 | 5.63 | 2.52 (1) | 0.11 |
| 11. I am occupied with a desire to be thinner | 301 | 41.29 | 80 | 44.94 | 221 | 40.11 | 1.30 (1) | 0.26 |
| 12. I think about burning up calories when I exercise | 232 | 31.82 | 59 | 33.15 | 173 | 31.40 | 0.19 (1) | 0.66 |
| 13. I other people think that I am too thin | 210 | 28.81 | 49 | 27.53 | 161 | 29.22 | 0.19 (1) | 0.67 |
| 14. I am preoccupied with the thought of having fat on my body | 267 | 36.63 | 73 | 41.01 | 194 | 35.21 | 1.95 (1) | 0.16 |
| 15. I take longer than others to eat my meals | 126 | 17.28 | 31 | 17.42 | 95 | 17.24 | 0.00 (1) | 0.96 |
| 16. I avoid foods with sugar in them | 101 | 13.85 | 26 | 14.61 | 75 | 13.61 | 0.11 (1) | 0.74 |
| 17. I eat diet foods | 28 | 3.84 | 6 | 3.37 | 22 | 3.99 | 0.14 (1) | 0.71 |
| 18. I feel that food controls my life | 77 | 10.56 | 18 | 10.11 | 59 | 10.71 | 0.05 (1) | 0.82 |
| 19. I display self-control around food | 292 | 40.05 | 73 | 41.01 | 219 | 39.75 | 0.09 (1) | 0.77 |
| 20. I feel that others pressure me to eat | 95 | 13.03 | 25 | 14.04 | 70 | 12.70 | 0.21 (1) | 0.64 |
| 21. I give too much time and thought to food | 80 | 10.97 | 19 | 10.67 | 61 | 11.07 | 0.02 (1) | 0.88 |
| 22. I feel uncomfortable after eating sweets | 54 | 7.41 | 19 | 10.67 | 35 | 6.35 | 3.66 (1) | 0.06 |
| 23. I engage in dieting behavior | 62 | 8.50 | 15 | 8.43 | 47 | 8.53 | 0.00 (1) | 0.97 |
| 24. I like my stomach to be empty | 59 | 8.09 | 17 | 9.55 | 42 | 7.62 | 0.67 (1) | 0.41 |
| 25. I have the impulse to vomit after meals | 31 | 4.25 | 8 | 4.49 | 23 | 4.17 | 0.03 (1) | 0.85 |
| 26. I enjoy trying new rich foods | 549 | 95.75 | 133 | 95.51 | 416 | 95.85 | 0.04 (1) | 0.83 |
N is the number of participants who reported they have this attitude or behaviors often, most of the time, and always to the questions of EAT26
Column percentages were reported
Table 1.
Sample descriptives (N = 729)
| All adolescents | Native adolescents | Immigrant adolescents | X2 (df) | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| Variables | N/Means | %/SD | N/Means | %/SD | N/Means | %/SD | ||
| Age | 13.83 | 0.98 | 13.82 | 0.98 | 13.86 | 1.00 | 0.20 (3) | 0.98 |
| Sex | ||||||||
| Male | 357 | 48.97 | 271 | 49.18 | 86 | 48.31 | 0.04 (1) | 0.84 |
| Female | 372 | 51.03 | 280 | 50.82 | 92 | 51.69 | ||
| Parents of a foreign nationality | ||||||||
| Yes | 178 | 24.42 | – | – | – | – | ||
| No | 551 | 75.58 | ||||||
| Disordered eating (EAT-26) | ||||||||
| Yes | 83 | 11.39 | 53 | 9.62 | 30 | 16.85 | 6.98 (1) | 0.01 |
| Mean EAT-26 score | 11.68 | 8.38 | 11.4 | 8.21 | 12.56 | 8.85 | 70.09 (43) | 0.01 |
| Moderate to severepsychological distress (BSRS-5) | ||||||||
| Yes | 119 | 16.32 | 84 | 15.25 | 35 | 19.66 | 1.92 (1) | 0.17 |
| Body overestimation | ||||||||
| Yes | 58 | 8.02 | 43 | 7.88 | 15 | 8.47 | 0.07 (1) | 0.80 |
| Friend weight-teasing | ||||||||
| Yes | 184 | 25.24 | 134 | 24.32 | 50 | 28.09 | 1.01 (1) | 0.31 |
| Family weight-teasing | ||||||||
| Yes | 173 | 23.73 | 129 | 23.41 | 44 | 24.72 | 0.13 (1) | 0.72 |
| Mother with college degree or above | ||||||||
| Yes | 205 | 28.1 | 170 | 30.9 | 35 | 19.7 | 8.33 (1) | 0.004 |
| Father with college degree or above | ||||||||
| Yes | 229 | 32.62 | 172 | 32.39 | 57 | 33.33 | 0.05 (1) | 0.82 |
As indicated in Table 2, no significant difference was observed in most of the items in the EAT-26 between immigrant and native adolescents. However, a considerably higher percentage of immigrants than native adolescents (18.54% vs. 11.62%) reported being aware of the calories consumed in food (X2 = 5.59, p = 0.02).
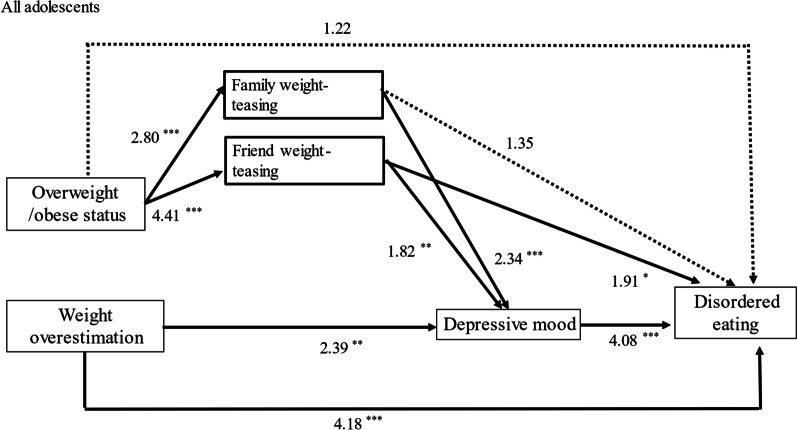
Generalized path model for all adolescents
The results revealed that overweight or obese status was significantly associated with negative social interactions, including family teasing and friend teasing (adjusted odds ratio [AOR] = 2.80, p < 0.001; AOR = 4.41, p < 0.001, respectively). Friend teasing is significantly associated with the likelihood of disordered eating (path 5). Family and friend teasing were significantly related to the likelihood of psychological distress (AOR = 2.34, p < 0.001; AOR = 1.91, p < 0.001, respectively). Psychological distress was significantly related to the likelihood of disordered eating (AOR = 4.08, p < 0.001). As indicated, the pathway from overweight or obesity to disordered eating mainly proceeded through experiencing family and friend teasing, resulting in psychological distress and increasing the likelihood of disordered eating (path 2 → 6 → 8; path 4 → 7 → 8). Another pathway from overweight or obesity led to friend teasing, increasing the likelihood of disordered eating (path 4 → 5). However, the direct pathway from overweight or obesity to disordered eating was not statistically significant (path 1), as shown in Table 3 and Fig. 2.
Table 3.
Generalized path analysis results
| All adolescents | Native adolescents | Immigrant adolescents | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pathways | Coef | AOR | 95% CI | p-value | Coef | AOR | 95% CI | p-value | Coef | AOR | 95% CI | p-value |
| Overweight/Obese status → Disordered eating (1) | 0.20 | 1.22 | (0.66, 2.31) | 0.54 | 0.41 | 1.51 | (0.69, 3.31) | 0.31 | − 0.45 | 0.64 | (0.18, 2.19) | 0.47 |
| Overweight/Obese status → Family teasing (2) | 1.03 | 2.80 | (1.96, 4.01) | 0.00*** | 1.09 | 2.97 | (1.96, 4.51) | 0.00*** | 0.86 | 2.36 | (1.16, 4.79) | 0.02* |
| Family weight-teasing → Disordered eating (3) | 0.30 | 1.35 | (0.74, 2.48) | 0.33 | 0.56 | 1.76 | (0.85, 3.63) | 0.13 | − 0.24 | 0.79 | (0.24, 2.58) | 0.69 |
| Overweight/Obese status → Friend weight-teasing (4) | 1.48 | 4.41 | (3.09, 6.31) | 0.00*** | 1.45 | 4.27 | (2.82, 6.49) | 0.00*** | 1.56 | 4.76 | (2.36, 9.62) | 0.00*** |
| Friend weight-teasing → Disordered eating (5) | 0.64 | 1.91 | (1.03, 3.54) | 0.04* | 0.49 | 1.64 | (0.76, 3.51) | 0.21 | 1.06 | 2.88 | (0.92, 9.09) | 0.07 |
| Family weight teasing → Depressive mood (6) | 0.85 | 2.34 | (1.46, 3.76) | 0.00*** | 0.86 | 2.36 | (1.37, 4.08) | 0.00*** | 0.88 | 2.40 | (0.89, 6.48) | 0.08 |
| Friend weight-teasing → Depressive mood (7) | 0.60 | 1.82 | (1.14, 2.92) | 0.01** | 0.40 | 1.50 | (0.87, 2.59) | 0.15 | 1.09 | 2.98 | (1.12, 7.92) | 0.03* |
| Depressive mood → Disordered eating (8) | 1.41 | 4.08 | (2.30, 7.22) | 0.00*** | 1.24 | 3.46 | (1.75, 6.87) | 0.00*** | 1.74 | 5.72 | (1.77, 18.47) | 0.00*** |
| Weight overestimation → Depressive mood (9) | 0.87 | 2.39 | (1.27, 4.48) | 0.01** | 0.68 | 1.98 | (0.92, 4.27) | 0.08 | 1.48 | 4.40 | (1.48, 13.08) | 0.01** |
| Weight overestimation → Disordered eating (10) | 1.43 | 4.18 | (1.91, 9.18) | 0.00*** | 0.98 | 2.67 | (0.93, 7.71) | 0.07 | 2.39 | 10.91 | (2.80, 42.53) | 0.00*** |
| Controls | ||||||||||||
| Parents of a foreign nationality → Disordered Eating | 0.56 | 1.75 | (1.02, 3.02) | 0.04* | ||||||||
| Sex (female) → Disordered Eating | − 0.20 | 0.82 | (0.50, 1.34) | 0.43 | − 0.03 | 0.97 | (0.52, 1.79) | 0.91 | − 0.71 | 0.49 | (0.19, 1.29) | 0.15 |
| Age → Disordered eating | − 0.30 | 0.74 | (0.57, 0.97) | 0.03* | − 0.39 | 0.68 | (0.47, 0.97) | 0.03* | − 0.21 | 0.81 | (0.50, 1.34) | 0.42 |
| Mather's high education → Disordered eating | 0.48 | 1.61 | (0.82, 3.15) | 0.16 | 0.63 | 1.88 | (0.86, 4.09) | 0.11 | 0.13 | 1.14 | (0.29, 4.49) | 0.85 |
| Father's high education → Disordered eating | 0.20 | 1.23 | (0.64, 2.36) | 0.54 | − 0.04 | 0.96 | (0.43, 2.12) | 0.92 | 0.63 | 1.88 | (0.56, 6.31) | 0.31 |
2000 Bootstrap samples
*p < 0.05, **p < 0.01, ***p < 0.001
Fig. 2.
Path analysis results for all adolescents. Adjusted odds ratios (AOR) are presented. *p < 0.05, **p < 0.01, ***p < 0.001. Solid lines represent statistically significant associations. Dotted lines represent statistically insignificant associations
Weight overestimation was significantly associated with the likelihood of psychological distress (AOR = 2.39, p < 0.01), and psychological distress was associated with an increased chance of disordered eating (AOR = 4.08, p < 0.001) (path 9 → 8). Furthermore, weight overestimation was directly associated with an increased likelihood of disordered eating (AOR = 4.18, p < 0.0001)(path 10). Finally, being an immigrant adolescent (AOR = 1.75, p < 0.04) was significantly associated with an increased likelihood of disordered eating. Details are presented in Table 3 and Fig. 2. We further stratified the study participants by their immigrant status.
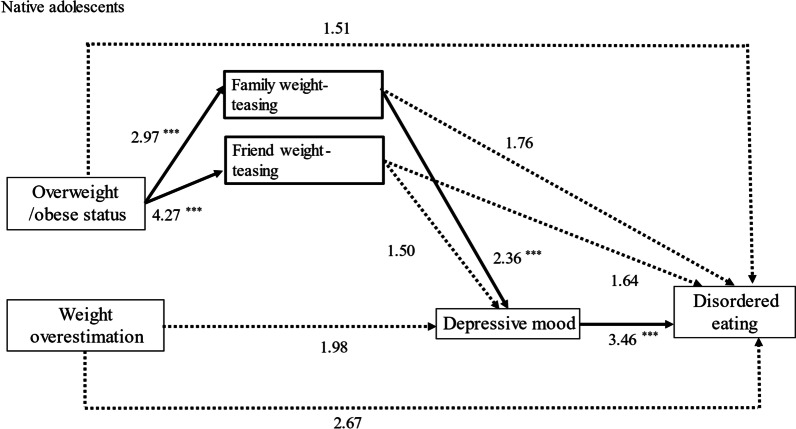
Native adolescents
The results indicate that overweight or obese status was significantly associated with family and friend weight-teasing (AOR = 2.97, p < 0.001; AOR = 4.27, p < 0.001). However, only family weight teasing was significantly associated with an increased likelihood of psychological distress (AOR = 2.36, p < 0.001). Psychological distress was significantly related to an increased chance of disordered eating (AOR = 3.46, p < 0.001). Consequently, the pathways from overweight or obese status to disordered eating mainly proceeded from experiencing family weight-teasing, which led to psychological distress, increasing the likelihood of disordered eating (path 2 → 6 → 8). The direct pathway from overweight or obese status to disordered eating was nonsignificant for native adolescents (path 1).
Notably, weight overestimation was unrelated to the likelihood of psychological distress or disordered eating for native adolescents. Details are presented in Table 3 and Fig. 3.
Fig. 3.
Path analysis results for native adolescents. Adjusted odds ratios (AOR) are presented. *p < 0.05, **p < 0.01, ***p < 0.001. Solid lines represent statistically significant associations. Dotted lines represent statistically insignificant associations
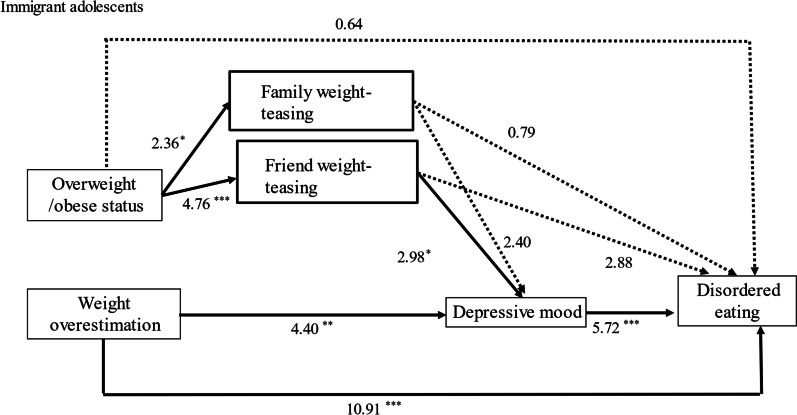
Immigrant adolescents
Unlike Taiwanese native adolescents, for immigrant adolescents, being overweight or obese was significantly associated with friend weight-teasing (AOR = 4.76, p < 0.001). Friend weight-teasing was significantly associated with an increased chance of psychological distress (path 6) (AOR = 2.98, p < 0.001). The psychological distress then contributed to an increased likelihood of disordered eating (path 8) (AOR = 5.72, p < 0.001). In summary, the pathways from being overweight or obese to disordered eating mainly proceeded indirectly through experiencing friend teasing, not family weight-teasing, which resulted in psychological distress, increasing the likelihood of disordered eating (path 4 → 7 → 8). Like native adolescents, the path from overweight or obese status to disordered eating (path 1) was not statistically significant.
In addition, weight overestimation was directly associated with disordered eating (path 10) (AOR = 10.91, p < 0.001) and indirectly proceeded through psychological distress to disordered eating among immigrant adolescents (path 9 → 8). Details are presented in Table 3 and Fig. 4.
Fig. 4.
Path analysis results for immigrant adolescents. Adjusted odds ratios (AOR) are presented. *p < 0.05, **p < 0.01, ***p < 0.001. Solid lines represent statistically significant associations. Dotted lines represent statistically insignificant associations
Discussion
This study revealed a significantly higher frequency of disordered eating among immigrant adolescents than their native peers. Studies comparing the prevalence of disordered eating between immigrant and native adolescents in Western countries have reported mixed results on whether immigrant adolescents are at a higher risk for disordered eating [52, 72, 73]. Our study observed that immigrant adolescents in Taiwan have a higher risk of disordered eating compared to their native counterparts.
The unique finding of this research is that, for most adolescents, the path from overweight or obese status to disordered eating is mainly through indirect pathways; however, the pathways are different between these two native and immigrant groups. As for native adolescents, the pathways from overweight or obese led to family teasing, which led to psychological distress, resulting in an increased chance of disordered eating. By contrast, for immigrant adolescents, the indirect pathway was from overweight or obese led to friend weight-teasing, which led to psychological distress, yielding an increased likelihood of disordered eating. Our study helps fill the literature gap regarding the potential risk factors of disordered eating among immigrant adolescents in East Asia.
For native and immigrant adolescents, being overweight or obese is not directly associated with the risk of disordered eating. However, it can significantly increase the risk of weight teasing and, at worst, discrimination [80]. Adolescents who are overweight or obese often experience weight teasing from multiple sources such as schools, healthcare organizations, media, and, most importantly, peers and family members [81]. Independent from weight status, in a school and population-based study, about 28.7% of adolescent girls and 16.1% of teenage boys reported being teased about weight by someone in their families [82].
Our findings were consistent with the vast body of literature in which weight-based teasing has been identified as a critical risk factor for disordered eating among adolescents in both Western and Asian countries [30, 31, 33, 35–37, 39]. In general, there are two types of teasing: weight/shape related teasing vs. overall appearance/non-weight related, and the source of negative comments is often received from parents or peers [83]. The impact of teasing from parents, family members, and peers on body dissatisfaction and disordered eating has been confirmed previously. A study of middle school girls indicated that parental weight-based teasing was a significant predictor of body dissatisfaction and disordered eating behaviors [84]. These negative experiences with body size judging can indirectly increase the likelihood of disordered eating through psychological distress.
Our study discovers a unique perspective where the association between disordered eating and weight teasing differs for native and immigrant adolescents. Our findings found that family teasing can lead to psychological distress, resulting in a high chance of disordered eating for most native Taiwanese adolescents. Similarly, Yu and Perez’s study [39] showed that weight-teasing from mothers was strongly associated with disordered eating in Asian Americans [39]. Chen et al. [68] reported that family members’ weight-teasing was associated with eating disordered among Taiwanese girls. A longitudinal study indicated a significant association between family weight teasing and appearance anxiety [63]. A prospective cohort study conducted on adolescents residing throughout the US found a significant association between parental weight-related teasing and binge eating [85]. These findings suggest the importance of the family environment in developing disordered eating among adolescents. Health promotion programs targeting adolescents’ health should, thus, further examine the family dynamics while designing and implementing family-based interventions for native adolescents.
On the other hand, friend weight teasing was indirectly related to disordered eating through experiencing depression for immigrant adolescents. Friend weight-teasing may result from the social norms regarding ideal body size and exert additional psychological stress on immigrant adolescents while they try to adapt to mainstream society [20, 21]. Further, one study on 80 obese children found that overweight children who experience peer teasing have higher levels of depression and disordered eating than those who are not teased by peers [86]. Acculturative stress is a unique stress often experienced by immigrants navigating and negotiating through different cultures and environments [87]. The stressors resulting from the acculturation process often impair one’s physical, social, and mental health [21, 88]. Furthermore, the cultural body idealization of being thin becomes a critical influencing factor on immigrant adolescents’ body weight perception in most Westernized countries [89]. A literature review on Chinese American women’s experiences with body weight teasing revealed that social acceptance is a crucial factor affecting body weight misperception for Asian immigrants [49]. Studies across cultures found that peer acceptance provides adolescents with better adjustment in school. In contrast, negative peer interactions, specifically peer rejection or isolation, may represent risk factors for poorer psychological functioning, such as depression and maladjustment [90]. Therefore, school-based intervention programs should reduce weight-related teasing and peer criticism.
Notably, no significant association was observed between body weight overestimation, psychological distress, and disordered eating for most native adolescents. However, for immigrant adolescents, weight overestimation significantly increases the risk of disordered eating directly and indirectly through psychological distress. This finding suggests that as a highly Westernized country, Taiwanese’s notion of the ideal body shape is to be “thin” [26, 52]. Evidence revealed that the Taiwanese present substantial social discrimination against obese adolescents in terms of peer acceptance [91], wage differentials [92], and sexual attraction [93]. Many adolescents, in particular those who are overweight or obese, report being teased about their weight and being bothered by the teasing [32]. The perception of being overweight during adolescence is a significant risk factor for depression, and these weight-related discriminatory experience among adolescents is often associated with disordered eating behaviors [80].
Considering being the minority, the parents of immigrant adolescents who moved to Taiwan, where being thin is mainstream, may be at an increased risk for experiencing body dissatisfaction, psychological stress, and eating disorder symptoms due to their minority status and wanting peer acceptance [27]. Racial discrimination against immigrant adolescents in Taiwan may contribute to our study’s main finding. A survey conducted among Southeast Asian and Chinese immigrant women living in Taiwan revealed that racial discrimination was associated with depression [15]. Poor socioeconomic status and the stress related to immigration and acculturation often negatively impact adolescents’ mental health [94]. However, limited research has been conducted on the effect of immigration and acculturation on stress-externalizing behaviors, such as disordered eating. Additionally, in our sample of predominantly Taiwanese individuals of Han Chinese descent, most immigrant families consisted of a mother from China, Vietnam, or Indonesia married to a Taiwanese man of Han Chinese ethnicity. In our data, the disparity between the educational levels of fathers and mothers in immigrant families was significant (p < 0.005). Whether the high prevalence of disordered eating is related to stress from the immigrant family environment or simply during the acculturation process is an interesting question for further investigation.
There appears to be a notable association between acculturation and disordered eating psychopathology among immigrant adolescents. Adolescence is a unique period in one’s lifetime where an individual transitions from puberty to adulthood, characterized by marked psychological changes, development of sexual attraction, and efforts toward constructing identity [95]. At the same time, immigrant adolescents in this study struggling to adapt to a social environment different from their parents may be at a higher risk of developing depressive symptoms [96]. Furthermore, the relationship between depression and eating disorders is rather complex because depression can cause a person to struggle with unhealthy eating patterns. In contrast, eating disorders can also lead to feelings of depression [97]. Consequently, these findings emphasize the urgent need for school-based prevention programs to improve immigrant students’ mental health.
This is the first quantitative study assessing the complex relationships between overweight or obese status, weight-based teasing, weight misperception, and disordered eating among immigrant and native adolescents. Public health practitioners should consider the unique characteristics of native and immigrant adolescents when designing specific prevention strategies for disordered eating behaviors for these two populations. Specifically, school-based prevention programs for immigrant adolescents should address body size misconceptions, racial discrimination, and depression associated with weight-based teasing at school. Future research is needed to understand immigration-related risk and protective factors at individual and school levels. As for native adolescents, disordered eating prevention campaigns may focus on understating family dynamics and educating parents on child health rather than weight to reduce peer weight teasing and its harmful consequences, such as disordered eating, depression, substance use, and stress. In addition, we suggest that healthcare providers working with families be aware that parental weight concerns might contribute to family weight teasing and try to use sensitive and non-stigmatizing language when communicating about weight with adolescents and their families.
Our study has several strengths. This study fills the gap in the literature on disparities in disordered eating and factors associated with disordered eating among immigrant adolescents in Taiwan. To our knowledge, this is the first study focusing on disordered eating among immigrant adolescents in Taiwan. We used standardized measures for disordered eating and psychological distress, which allows for international comparisons regarding the potential risks associated with adolescent disordered eating. Lastly, our study offers a plausible explanation of the differences in the paths to disordered eating between immigrant and native adolescents in Taiwan, which was not reported previously.
Some limitations need to be mentioned. First, cross-sectional research cannot be used to infer causality; thus, further research on this topic in Taiwan should be conducted using a study design suitable for determining the basis. Second, we applied convenience sampling in this study, and only adolescents in New Taipei City were recruited. Furthermore, the percentage of immigrant adolescents in the study sample (24.4%) is higher than that of the entire New Taipei City (2017–2019, 11%) [98]. Therefore, the results cannot be generalized to all immigrant and native adolescents in New Taipei City or Taiwan. Future research should investigate social and individual factors associated with disordered eating in these two populations in Taiwan. Lastly, detailed immigration information, including the country where respondent’s parents immigrated from and whether their grandparents also immigrated to Taiwan, is unclear. It may limit our understanding of the family dynamics related to the cause of disordered eating. To expand on the present quantitative results, qualitative studies on disordered eating among immigrant adolescents can be suggested to examine other factors associated with disordered eating within this unique population.
Conclusion
This study reveals a higher frequency of disordered eating and a higher mean EAT-26 score among immigrant adolescents compared to native adolescents in Taiwan. The proposed pathways to disordered eating appear different for immigrant and native adolescents. Our findings highlight the importance of further research to investigate multi-level factors, such as family, school, and societal factors, associated with disordered eating among immigrant adolescents to prevent disordered eating in this high-risk population. Since health inequality may exist in this case, healthcare providers should carefully consider the differential factors for native and immigrant adolescents separately when designing and implementing disordered eating prevention programs in Taiwan.
Acknowledgements
The authors appreciate the contributions and cooperation of this study's participants and school teachers. We thank Ms. Ya-Chuan Yang for her help in the data collection.
Abbreviations
- EAT-26
The eating attitudes test-26
- BSRS-5
Five-item brief symptom rating scale
- AOR
Adjusted odds ratio
- GSEM
Generalized structural equation modeling
Author contributions
DRC conceived, planned, and implemented the study. DRC drafted the manuscript. LYL revised the manuscript, and B. Levin prepared the literature review. All authors reviewed and approved the final manuscript.
Funding
This study was financially supported by the Ministry of Science and Technology (grant number MOST 109-2410H-002-054-SS2).
Availability of data and materials
Data is available upon reasonable request.
Declarations
Ethics approval and consent to participate
Informal consent was obtained from the participants and their parents. Subsequently, each student completed a 20–25-min questionnaire in the classroom. The study followed the Declaration of Helsinki and was approved by Taiwan’s Research Ethics Committee (NTU NO. 201901HS030).
Consent for publication
All the authors have provided their consent for publication.
Competing interests
The authors have no Competing interests to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.National Eating Disorders Collaboration. Disordered Eating & Dieting [Internet]. 2021. https://nedc.com.au/eating-disorders/eating-disorders-explained/disordered-eating-and-dieting/. Accessed 8 Feb 2022.
- 2.Haines J, Ziyadeh NJ, Franko DL, McDonald J, Mond JM, Austin SB. Screening high school students for eating disorders: validity of brief behavioral and attitudinal measures. J Sch Health. 2011;81:530–535. doi: 10.1111/j.1746-1561.2011.00623.x. [DOI] [PubMed] [Google Scholar]
- 3.Yanez AA, Peix MA, Atserias N, Arnau A, Brug J, Yanez AA, et al. Association of eating attitudes between teenage girls and their parents. Int J Soc Psychiatry. 2007;53:507–513. doi: 10.1177/0020764007078350. [DOI] [PubMed] [Google Scholar]
- 4.Zervaki K, Yiannakouris N, Sdrali D, Costarelli V. Diet quality, disordered eating and health-related quality of life in greek adolescents. Nutr Food Sci. 2017;47(4):511–521. doi: 10.1108/NFS-12-2016-0189. [DOI] [Google Scholar]
- 5.Pike KM, Dunne PE. The rise of eating disorders in Asia: a review. J Eat Disord. 2015;3:1–14. doi: 10.1186/s40337-015-0070-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong Y, Lin J-S, Chang Y-J. Body satisfaction, emotional intelligence, and the development of disturbed eating: a survey of Taiwanese students. Asia Pac J Clin Nutr. 2014;23:651–659. doi: 10.6133/apjcn.2014.23.4.02. [DOI] [PubMed] [Google Scholar]
- 7.Chang YJ, Lin W, Wong Y. Survey on eating disorder–related thoughts, behaviors, and their relationship with food intake and nutritional status in female high school students in Taiwan. J Am Coll Nutr. 2011;30:39–48. doi: 10.1080/07315724.2011.10719942. [DOI] [PubMed] [Google Scholar]
- 8.Lee HJ, Park S, Kim CI, Choi DW, Lee JS, Oh SM, et al. The association between disturbed eating behavior and socioeconomic status: the online Korean adolescent panel survey (OnKAPS) PLoS ONE. 2013;8:57880. doi: 10.1371/journal.pone.0057880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tao ZL. Epidemiological risk factor study concerning abnormal attitudes toward eating and adverse dieting behaviours among 12–25-years-old Chinese students. Eur Eat Disord Rev. 2010;18:507–514. doi: 10.1002/erv.1032. [DOI] [PubMed] [Google Scholar]
- 10.Lin J-P. Tradition and Progress: Taiwan’s Evolving Migration Reality [Internet]. 2012. https://www.migrationpolicy.org/article/tradition-and-progress-taiwans-evolving-migration-reality. Accessed 8 Feb 2022.
- 11.2.16.886.101.20003. 2.16.886.101.20003. 2.16.886.101.20003; 2011. https://www.ey.gov.tw/otnen/. Accessed 13 Mar 2023.
- 12.Ministry of the Interior [Internet]. Minist. Inter. http://www.moi.gov.tw/english/Default.aspx. Accessed 13 Mar 2023.
- 13.Hsia H-C. Imaged and imagined threat to the nation: the media construction of the ‘foreign brides’ phenomenon’as social problems in Taiwan. Inter-Asia Cult Stud. 2007;8:55–85. doi: 10.1080/14649370601119006. [DOI] [Google Scholar]
- 14.Hsia H. Transnational marriage and internationalization of capital-the case of the “foreign bride” phenomenon in Taiwan. Taiwan Radic Q Soc Stud. 2000;39:45–92. [Google Scholar]
- 15.Yang H-J, Wu J-Y, Huang S-S, Lien M-H, Lee TS-H. Perceived discrimination, family functioning, and depressive symptoms among immigrant women in Taiwan. Arch Womens Ment Health. 2014;17:359–366. doi: 10.1007/s00737-013-0401-8. [DOI] [PubMed] [Google Scholar]
- 16.Lin L-H, Hung C-H. Vietnamese women immigrants’ life adaptation, social support, and depression. J Nurs Res LWW. 2007;15:243–254. doi: 10.1097/01.JNR.0000387621.95306.98. [DOI] [PubMed] [Google Scholar]
- 17.Chang J-C, Huang W-L, Chen Y-L, Gau SS-F. The mental health of immigrant mother’s offspring in Taiwan: a national epidemiological study. J Formos Med Assoc. 2020;119:601–609. doi: 10.1016/j.jfma.2019.08.033. [DOI] [PubMed] [Google Scholar]
- 18.Yang H-J, Kuo Y-J, Wang L, Yang C-Y. Culture, parenting, and child behavioral problems: a comparative study of cross-cultural immigrant families and native-born families in Taiwan. Transcult Psychiatry. 2014;51:526–544. doi: 10.1177/1363461514532306. [DOI] [PubMed] [Google Scholar]
- 19.Wu W, Wu JC-L, Chiang T. Variation in the association between socioeconomic status and breastfeeding practices by immigration status in Taiwan: a population based birth cohort study. BMC pregnancy childbirth. BioMed Cent. 2015;15:1–11. doi: 10.1186/s12884-015-0732-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barry DT, Garner DM. Eating concerns in East Asian immigrants: relationships between acculturation, self-construal, ethnic identity, gender, psychological functioning and eating concerns. Eat Weight Disord: Stud Anorex Bulim Obes. 2001;6:90–98. doi: 10.1007/BF03339757. [DOI] [PubMed] [Google Scholar]
- 21.Berry JW, Kim U, Minde T, Mok D. Comparative studies of acculturative stress. Int Migr Rev. 1987;21:491–511. doi: 10.1177/019791838702100303. [DOI] [Google Scholar]
- 22.Landrine H, Klonoff EA. African American acculturation: deconstructing race and reviving culture. Sage Publications Inc; 1996. [Google Scholar]
- 23.Neff JA, Hoppe SK. Race/ethnicity, acculturation, and psychological distress: fatalism and religiosity as cultural resources. J Commun Psychol. 1993;21:3–20. doi: 10.1002/1520-6629(199301)21:1<3::AID-JCOP2290210102>3.0.CO;2-9. [DOI] [Google Scholar]
- 24.Walker RL, Wingate LR, Obasi EM, Joiner TE., Jr An empirical investigation of acculturative stress and ethnic identity as moderators for depression and suicidal ideation in college students. Cultur Divers Ethnic Minor Psychol. 2008;14:75. doi: 10.1037/1099-9809.14.1.75. [DOI] [PubMed] [Google Scholar]
- 25.Kalantzis MA, Lim S, Dauber AK, Studer-Perez EI, Silverman ZJ, O’Brien WH. Acculturative stress and eating disorder psychopathology: a meta-analysis. Eat Behav. 2022;48:101694. doi: 10.1016/j.eatbeh.2022.101694. [DOI] [PubMed] [Google Scholar]
- 26.Chang F-C, Lee C-M, Chen P-H, Chiu C-H, Pan Y-C, Huang T-F. Association of thin-ideal media exposure, body dissatisfaction and disordered eating behaviors among adolescents in Taiwan. Eat Behav. 2013;14:382–385. doi: 10.1016/j.eatbeh.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 27.Akoury LM, Warren CS, Culbert KM. Disordered eating in Asian American women: sociocultural and culture-specific predictors. Front Psychol. 2019;10:1950. doi: 10.3389/fpsyg.2019.01950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Field AE, Javaras KM, Aneja P, Kitos N, Camargo CA, Taylor CB, et al. Family, peer, and media predictors of becoming eating disordered. Arch Pediatr Adolesc Med. 2008;162:574–579. doi: 10.1001/archpedi.162.6.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen D-R, Sun G, Levin B. Gender-specific responses to multifaceted factors associated with disordered eating among adolescents of 7–9th grade. J Eat Disord BioMed Central. 2022;10:1–15. doi: 10.1186/s40337-021-00524-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen X, Luo Y, Chen H. Body image victimization experiences and disordered eating behaviors among Chinese female adolescents: the role of body dissatisfaction and depression. Sex Roles. 2020;83:442–452. doi: 10.1007/s11199-020-01122-4. [DOI] [Google Scholar]
- 31.Kluck AS. Family factors in the development of disordered eating: integrating dynamic and behavioral explanations. Eat Behav. 2008;9:471–483. doi: 10.1016/j.eatbeh.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 32.Neumark-Sztainer D, Falkner N, Story M, Perry C, Hannan PJ, Mulert S. Weight-teasing among adolescents: correlations with weight status and disordered eating behaviors. Int J Obes. 2002;26:123–131. doi: 10.1038/sj.ijo.0801853. [DOI] [PubMed] [Google Scholar]
- 33.Xu X, Mellor D, Kiehne M, Ricciardelli LA, McCabe MP, Xu Y. Body dissatisfaction, engagement in body change behaviors and sociocultural influences on body image among Chinese adolescents. Body Image. 2010;7:156–164. doi: 10.1016/j.bodyim.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 34.Eisenberg ME, Puhl R, Areba EM, Neumark-Sztainer D. Family weight teasing, ethnicity and acculturation: associations with well-being among Latinx, Hmong, and Somali Adolescents. J Psychosom Res. 2019;122:88–93. doi: 10.1016/j.jpsychores.2019.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lieberman M, Gauvin L, Bukowski WM, White DR. Interpersonal influence and disordered eating behaviors in adolescent girls: the role of peer modeling, social reinforcement, and body-related teasing. Eat Behav. 2001;2:215–236. doi: 10.1016/S1471-0153(01)00030-7. [DOI] [PubMed] [Google Scholar]
- 36.Shagar PS, Donovan CL, Loxton N, Boddy J, Harris N. Is thin in everywhere?: A cross-cultural comparison of a subsection of tripartite influence model in Australia and Malaysia. Appetite. 2019;134:59–68. doi: 10.1016/j.appet.2018.12.025. [DOI] [PubMed] [Google Scholar]
- 37.Tsai M-R, Chang Y-J, Lien P-J, Wong Y. Survey on eating disorders related thoughts, behaviors and dietary intake in female junior high school students in Taiwan. Asia Pac J Clin Nutr. 2011;20:196–205. [PubMed] [Google Scholar]
- 38.Webb HJ, Kerin JL, Zimmer-Gembeck MJ. Increases in emotional eating during early adolescence and associations with appearance teasing by parents and peers, rejection, victimization, depression, and social anxiety. J Early Adolesc. 2021;41:754–777. doi: 10.1177/0272431620950469. [DOI] [Google Scholar]
- 39.Yu K, Perez M. The association between maternal criticism and body dissatisfaction on disordered eating pathology across racial and ethnic groups. Cultur Divers Ethnic Minor Psychol. 2020;26:61. doi: 10.1037/cdp0000277. [DOI] [PubMed] [Google Scholar]
- 40.Cance JD, Loukas A, Talley AE. The differential associations of internalizing symptoms and family and school relationships with disordered eating attitudes among early adolescents. J Soc Pers Relatsh. 2015;32:41–56. doi: 10.1177/0265407514523551. [DOI] [Google Scholar]
- 41.Chen J, Wang Z, Guo B, Arcelus J, Zhang H, Jia X, et al. Negative affect mediates effects of psychological stress on disordered eating in young Chinese women. San Francisco: Public Library of Science; 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Duarte C, Pinto-Gouveia J, Stubbs RJ. The prospective associations between bullying experiences, body image shame and disordered eating in a sample of adolescent girls. Personal Individ Differ. 2017;116:319–325. doi: 10.1016/j.paid.2017.05.003. [DOI] [Google Scholar]
- 43.Ferreiro F, Seoane G, Senra C. Gender-related risk and protective factors for depressive symptoms and disordered eating in adolescence: a 4-year longitudinal study. J Youth Adolesc. 2012;41:607–622. doi: 10.1007/s10964-011-9718-7. [DOI] [PubMed] [Google Scholar]
- 44.Lee KS, Vaillancourt T. A 4-year prospective study of bullying, anxiety, and disordered eating behavior across early adolescence. Child Psychiatry Hum Dev. 2019;50:815–825. doi: 10.1007/s10578-019-00884-7. [DOI] [PubMed] [Google Scholar]
- 45.Lin Y-W, Lin C-Y, Strong C, Liu C-H, Hsieh Y-P, Lin Y-C, et al. Psychological correlates of eating behavior in overweight/obese adolescents in Taiwan: psychometric and correlation analysis of the three-factor eating questionnaire (TFEQ)-R21. Pediatr Neonatol. 2021;62:41–48. doi: 10.1016/j.pedneo.2020.08.006. [DOI] [PubMed] [Google Scholar]
- 46.Puccio F, Fuller-Tyszkiewicz M, Youssef G, Mitchell S, Byrne M, Allen N, et al. Longitudinal bi-directional effects of disordered eating, depression and anxiety. Eur Eat Disord Rev. 2017;25:351–358. doi: 10.1002/erv.2525. [DOI] [PubMed] [Google Scholar]
- 47.Tsai M-C, Gan S-T, Lee C-T, Liang Y-L, Lee L-T, Lin S-H. National population-based data on the incidence, prevalence, and psychiatric comorbidity of eating disorders in Taiwanese adolescents and young adults. Int J Eat Disord. 2018;51:1277–1284. doi: 10.1002/eat.22970. [DOI] [PubMed] [Google Scholar]
- 48.Gan WY, Nasir MTM, Zalilah MS, Hazizi AS. Direct and indirect effects of sociocultural influences on disordered eating among Malaysian male and female university students. A mediation analysis of psychological distress. Appetite. 2011;56:778–783. doi: 10.1016/j.appet.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 49.Tock WL, Tung W-C, Holston EC, Hsu Y-W. Bodyweight misperception by Chinese American females influenced by cultural and social ideals: implication for home health care. Home Health Care Manag Pract. 2020;32:172–178. doi: 10.1177/1084822319893993. [DOI] [Google Scholar]
- 50.Blodgett Salafia EH, Lemer JL. Associations between multiple types of stress and disordered eating among girls and boys in middle school. J Child Fam Stud. 2012;21:148–157. doi: 10.1007/s10826-011-9458-z. [DOI] [Google Scholar]
- 51.Bucchianeri MM, Fernandes N, Loth K, Hannan PJ, Eisenberg ME, Neumark-Sztainer D. Body dissatisfaction: do associations with disordered eating and psychological well-being differ across race/ethnicity in adolescent girls and boys? Cultur Divers Ethnic Minor Psychol. 2016;22:137. doi: 10.1037/cdp0000036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tsai G, Curbow B, Heinberg L. Sociocultural and developmental influences on body dissatisfaction and disordered eating attitudes and behavious of Asian women. J Nerv Ment Dis. 2003;191:309–318. doi: 10.1097/01.NMD.0000066153.64331.10. [DOI] [PubMed] [Google Scholar]
- 53.Xie B, Chou C-P, Spruijt-Metz D, Reynolds K, Palmer PH, Wu Q, et al. Longitudinal analysis of weight perception and psychological factors in Chinese adolescents. Am J Health Behav. 2011;35:92–104. doi: 10.5993/AJHB.35.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yan H, Wu Y, Oniffrey T, Brinkley J, Zhang R, Zhang X, et al. Body weight misperception and its association with unhealthy eating behaviors among adolescents in China. Int J Environ Res Public Health. 2018;15:936. doi: 10.3390/ijerph15050936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Talamayan KS, Springer AE, Kelder SH, Gorospe EC, Joye KA. Prevalence of overweight misperception and weight control behaviors among normal weight adolescents in the United States. ScientificWorldJournal. 2006;6:365–373. doi: 10.1100/tsw.2006.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pasch KE, Klein EG, Laska MN, Velazquez CE, Moe SG, Lytle LA. Weight misperception and health risk behaviors among early adolescents. Am J Health Behav. 2011;35:797–806. doi: 10.5993/AJHB.35.6.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Roberts RE, Duong HT. Perceived weight, not obesity, increases risk for major depression among adolescents. J Psychiatr Res. 2013;47:1110–1117. doi: 10.1016/j.jpsychires.2013.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lee H-J, Park S, Kim C, Choi D, Lee JS, Oh SM, et al. The association between disturbed eating behavior and socioeconomic status: the online Korean adolescent panel survey (OnKAPS) PLoS ONE. 2013;8:e57880. doi: 10.1371/journal.pone.0057880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Farah Wahida Z, Mohd Nasir MT, Hazizi AS. Physical activity, eating behaviour and body image perception among young adolescents in Kuantan, Pahang, Malaysia. Malays J Nutr. 2011;17. [PubMed]
- 60.Neumark-Sztainer D, Bauer KW, Friend S, Hannan PJ, Story M, Berge JM. Family weight talk and dieting: how much do they matter for body dissatisfaction and disordered eating behaviors in adolescent girls? J Adolesc Health. 2010;47:270–276. doi: 10.1016/j.jadohealth.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lee AM, Lee S. Disordered eating and its psychosocial correlates among Chinese adolescent females in Hong Kong. Int J Eat Disord. 1996;20:177–183. doi: 10.1002/(SICI)1098-108X(199609)20:2<177::AID-EAT8>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 62.Dominé F, Berchtold A, Akré C, Michaud P-A, Suris J-C. Disordered eating behaviors: what about boys? J Adolesc Health. 2009;44:111–117. doi: 10.1016/j.jadohealth.2008.07.019. [DOI] [PubMed] [Google Scholar]
- 63.Zimmer-Gembeck MJ, Webb HJ, Kerin J, Waters AM, Farrell LJ. Risk factors and temporal patterns of disordered eating differ in adolescent boys and girls: testing gender-specific appearance anxiety models. Dev Psychopathol. 2020;33(3):856–867. doi: 10.1017/S0954579420000188. [DOI] [PubMed] [Google Scholar]
- 64.Striegel-Moore RH, Rosselli F, Perrin N, DeBar L, Wilson GT, May A, et al. Gender difference in the prevalence of eating disorder symptoms. Int J Eat Disord. 2009;42:471–474. doi: 10.1002/eat.20625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hsia H-C. Foreign brides, multiple citizenship and the immigrant movement in Taiwan. Asian Pac Migr J. 2009;18:17–46. doi: 10.1177/011719680901800102. [DOI] [Google Scholar]
- 66.Blau PM, Duncan OD. The American occupational structure. ERIC; 1967. [Google Scholar]
- 67.Titzmann PF, Juang PL. Immigrant adolescents: opportunities and challenges. Emerg Trends Soc Behav Sci Interdiscip Searchable Linkable Resour. 2015 doi: 10.1002/9781118900772.etrds0438. [DOI] [Google Scholar]
- 68.Wang C-W, Chen D-R. Associations of sugar-sweetened beverage knowledge, self-efficacy, and perceived benefits and barriers with sugar-sweetened beverage consumption in adolescents: a structural equation modeling approach. Appetite. 2022;168:105663. doi: 10.1016/j.appet.2021.105663. [DOI] [PubMed] [Google Scholar]
- 69.Garner DM, Olmsted MP, Bohr Y, Garfinkel PE. The eating attitudes test: psychometric features and clinical correlates. Psychol Med. 1982;12:871–878. doi: 10.1017/S0033291700049163. [DOI] [PubMed] [Google Scholar]
- 70.Cheng H-L, Tran AG, Miyake ER, Kim HY. Disordered eating among Asian American college women: a racially expanded model of objectification theory. J Couns Psychol. 2017;64:179. doi: 10.1037/cou0000195. [DOI] [PubMed] [Google Scholar]
- 71.Hsu Y-Y, Chen B-H, Huang M-C, Lin SJ, Lin M-F. Disturbed eating behaviors in Taiwanese adolescents with type 1 diabetes mellitus: a comparative study. Pediatr Diabetes. 2009;10:74–81. doi: 10.1111/j.1399-5448.2008.00422.x. [DOI] [PubMed] [Google Scholar]
- 72.Jennings PS, Forbes D, McDermott B, Juniper S, Hulse G. Acculturation and eating disorders in Asian and Caucasian Australian adolescent girls. Psychiatry Clin Neurosci. 2005;59:56–61. doi: 10.1111/j.1440-1819.2005.01332.x. [DOI] [PubMed] [Google Scholar]
- 73.Jennings PS, Forbes D, McDermott B, Hulse G, Juniper S. Eating disorder attitudes and psychopathology in Caucasian Australian, Asian Australian and Thai university students. Aust N Z J Psychiatry. 2006;40:143–149. doi: 10.1080/j.1440-1614.2006.01761.x. [DOI] [PubMed] [Google Scholar]
- 74.Lee M-B, Liao S-C, Lee Y-J, Wu C-H, Tseng M-C, Gau S-F, et al. Development and verification of validity and reliability of a short screening instrument to identify psychiatric morbidity. J Formos Med Assoc. 2003;102:687–694. [PubMed] [Google Scholar]
- 75.Chen W, Shiao W-B, Lin BY-J, Lin C-C. Rural and urban married Asian immigrants in Taiwan: determinants of their physical and mental health. J Immigr Minor Health. 2013;15:1038–1047. doi: 10.1007/s10903-012-9750-z. [DOI] [PubMed] [Google Scholar]
- 76.Lyu S-Y, Chi Y-C, Farabee D, Tsai L-T, Lee M-B, Lo F-E, et al. Psychological distress in an incarcerated juvenile population. J Formos Med Assoc. 2015;114:1076–1081. doi: 10.1016/j.jfma.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 77.Pan C-H, Lee M-B, Wu C-Y, Liao S-C, Chan C-T, Chen C-Y. Suicidal ideation, psychopathology, and help-seeking in 15–19-year-old adolescents in Taiwan: a population-based study 2015–2019. J Affect Disord. 2021;282:846–851. doi: 10.1016/j.jad.2020.12.139. [DOI] [PubMed] [Google Scholar]
- 78.Health Promotion Administration (HPA) [Internet]. https://www.hpa.gov.tw/EngPages/Index.aspx. Accessed 2 Jan 2023.
- 79.Huber C. Generalized structural equation modeling using stata. Ital Stata Users Group Meet Novemb. 2013. p. 14–5.
- 80.Puhl RM, Latner JD. Stigma, obesity, and the health of the nation’s children. Psychol Bull. 2007;133:557. doi: 10.1037/0033-2909.133.4.557. [DOI] [PubMed] [Google Scholar]
- 81.Pötzsch A, Rudolph A, Schmidt R, Hilbert A. Two sides of weight bias in adolescent binge-eating disorder: adolescents’ perceptions and maternal attitudes. Int J Eat Disord. 2018;51:1339–1345. doi: 10.1002/eat.22982. [DOI] [PubMed] [Google Scholar]
- 82.Eisenberg ME, Neumark-Sztainer D, Story M. Associations of weight-based teasing and emotional well-being among adolescents. Arch Pediatr Adolesc Med. 2003;157:733–738. doi: 10.1001/archpedi.157.8.733. [DOI] [PubMed] [Google Scholar]
- 83.Menzel JE, Schaefer LM, Burke NL, Mayhew LL, Brannick MT, Thompson JK. Appearance-related teasing, body dissatisfaction, and disordered eating: a meta-analysis. Body Image. 2010;7:261–270. doi: 10.1016/j.bodyim.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 84.Keery H, Boutelle K, Van Den Berg P, Thompson JK. The impact of appearance-related teasing by family members. J Adolesc Health. 2005;37:120–127. doi: 10.1016/j.jadohealth.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 85.Haines J, Kleinman KP, Rifas-Shiman SL, Field AE, Austin SB. Examination of Shared Risk and Protective Factors for Overweight and Disordered Eating Among Adolescents. Arch Pediatr Adolesc Med [Internet]. 2010. 10.1001/archpediatrics.2010.19. Accessed 23 Apr 2021. [DOI] [PMC free article] [PubMed]
- 86.Madowitz J, Knatz S, Maginot T, Crow SJ, Boutelle KN. Teasing, depression and unhealthy weight control behaviour in obese children. Pediatr Obes. 2012;7:446–452. doi: 10.1111/j.2047-6310.2012.00078.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Staudenmeyer A, Macciomei E, Del Cid M, Patel SG. Immigrant youth life stressors. Psychother Immigr Youth. Springer; 2016. pp. 3–24. [Google Scholar]
- 88.Chun H, Mobley M. The, “Immigrant Paradox” phenomenon: assessing problem behaviors and risk factors among immigrant and native adolescents. J Prim Prev. 2014;35:339–356. doi: 10.1007/s10935-014-0359-y. [DOI] [PubMed] [Google Scholar]
- 89.Kern MR, Heinz A, Stevens GW, Walsh SD, Willems H. “What’s a normal weight?”–Origin and receiving country influences on weight-status assessment among 1.5 and 2nd generation immigrant adolescents in Europe. Soc Sci Med. 2020;264:113306. doi: 10.1016/j.socscimed.2020.113306. [DOI] [PubMed] [Google Scholar]
- 90.Rubin KH, Coplan R, Chen X, Bowker J, McDonald KL. Peer relationships in childhood. Soc Personal Dev 2013;317–68
- 91.Chen D-R, Lu H-H. Social alienation of adolescents with obesity in classrooms: a multilevel approach. J Adolesc. 2022;94:81–91. doi: 10.1002/jad.12001. [DOI] [PubMed] [Google Scholar]
- 92.Huang C-Y, Chen D-R. Association of weight change patterns in late adolescence with young adult wage differentials: a multilevel longitudinal study. PLoS ONE. 2019;14:e0219123. doi: 10.1371/journal.pone.0219123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Yeh J-C, Chen D-R. Delayed romantic experience: association of romantic relationship and weight change patterns over 7 years among taiwanese adolescents. Youth Soc. 2021;54(8):1330–1351. doi: 10.1177/0044118X211023517. [DOI] [Google Scholar]
- 94.Perreira KM, Ornelas IJ. The physical and psychological well-being of immigrant children. Fut Child. 2011;21:195–218. doi: 10.1353/foc.2011.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Shlafer R, Hergenroeder AC, Jean Emans S, Rickert VI, Adger H, Spear B, et al. Adolescence as a critical stage in the MCH life course model: commentary for the leadership education in adolescent health (LEAH) interdisciplinary training program projects. Matern Child Health J. 2014;18:462–466. doi: 10.1007/s10995-013-1243-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Shi L, Chen W, Bouey JH, Lin Y, Ling L. Impact of acculturation and psychological adjustment on mental health among migrant adolescents in Guangzhou, China: a cross-sectional questionnaire study. BMJ Open. 2019;9:e022712. doi: 10.1136/bmjopen-2018-022712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Cattarin JA, Thompson JK. A 3-year longitudinal study of body image, eating disturbance, and general psychological functioning in adolescent females. Eat Disord. 1994;2:114–125. doi: 10.1080/10640269408249107. [DOI] [Google Scholar]
- 98.Statistical Indicators [Internet]. Stat. Indic. 2019. https://english.moe.gov.tw/cp-86-18943-e698b-1.html. Accessed 13 Mar 2023.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is available upon reasonable request.