Abstract
Rates of pre-exposure prophylaxis (PrEP) uptake for HIV prevention continue to increase rapidly among men who have sex with men (MSM) in the United States (U.S.); however, these increases have been slower among young MSM. Emerging adulthood (ages 18–25) is a time of transitions and social development, resulting in increased vulnerability to HIV. Analyzing data from a cross-sectional survey of emerging adult MSM (ages 18–25 years; n=281) in the Mid-Atlantic urban metropolitan region of the U.S., we examined how social identity support, descriptive PrEP norms, and economic instability were related to PrEP engagement. In structural equation models, PrEP norms were directly associated with PrEP engagement (β = 0.29, 95% CI = [0.12,0.46]) and social identity support was indirectly associated with PrEP engagement through its association with descriptive PrEP norms (β = 0.18, 95% CI = [0.09,0.28]). Economic instability was not significantly associated with PrEP engagement, although a negative trend was present (β = −0.19, 95% CI = [−0.39,0.02]). Our results suggest that an integrative socioecological model is appropriate for the study of PrEP engagement among emerging adult MSM. Efforts to increase PrEP engagement should support community capacity building, amplify positive descriptive PrEP norms, and address unmet economic needs.
Keywords: HIV, pre-exposure prophylaxis, emerging adults, MSM
Introduction
Emerging adult men who have sex with men (EAMSM; ages 18–25 years) are disproportionately affected by the HIV epidemic in the United States (CDC, 2018b). The significant social and economic transitions (e.g., increased independence and economic responsibility) that characterize emerging adulthood (Arnett, 2000) may affect HIV-related behaviors. Daily oral pre-exposure prophylaxis (PrEP) medications have the potential to reduce new HIV infections, yielding a 99% reduction in transmission if taken with high adherence (Anderson et al., 2012). In the United States, PrEP is recommended for adolescents and adults at increased risk for HIV, including those who use condoms inconsistently and those with a recently diagnosed bacterial sexually transmitted infection (CDC, 2021a). Despite experiencing a disproportionate burden of HIV infections, emerging adults are the age group with the lowest PrEP uptake rate among those indicated for the medication (CDC, 2021b). PrEP engagement is commonly measured using the PrEP care continuum, a framework that describes the four key motivational and behavioral stages in the process of adopting PrEP for HIV prevention: 1) awareness of PrEP, 2) willingness to use PrEP, 3) intention to use PrEP, and 4) current use of PrEP (Parsons et al., 2017). Low uptake among EAMSM in emerging adulthood suggest that PrEP is being inadequately rolled out for this community (CDC, 2018a; Finlayson et al., 2019; Siegler et al., 2018) and that efforts are needed to identify, contextualize, and attend to multilevel social factors that facilitate EAMSM’s PrEP engagement.
Social identity support may inform PrEP engagement in EAMSM given prior evidence of its role in other sexual health behaviors. Sexual orientation disclosure, or “coming out”, is a common milestone toward self-acceptance that often occurs during adolescence or emerging adulthood (Martos et al., 2015). Sexual orientation disclosure may facilitate new resources for social support (Chaudoir & Fisher, 2010), boost the effects of existing supportive relationships (Weisz et al., 2016), and has been shown to associated with better mental health outcomes (Juster et al., 2013). Social environments that nurture self-acceptance may have implications for how EAMSM seek and utilize resources that support their sexual health.
How EAMSM connect with the gay community can have important implications for HIV prevention (Ramirez-Valles, 2002). Gay community attachments may serve as a natural connection to peers who have a history of PrEP use and who can provide information on how to navigate PrEP access, including referring their peers to sexuality-affirming providers (Meanley et al., 2020). Furthermore, the broader gay community may elicit descriptive norms about socially-acceptable sexual health behaviors. Descriptive norms are individuals’ perceptions about common and accepted behaviors within their networks and provide a point of reference in personal behavioral decision-making (Van de Bongardt et al., 2015). Recent findings exhibited that MSM who perceive PrEP use in their social network are more likely to access PrEP medications (Parent et al., 2020).
Economic transitions in housing, income, and access to healthcare during emerging adulthood may also be pertinent to MSM’s sexual health. EAMSM are at increased risk of homelessness compared to their heterosexual counterparts (Shelton et al., 2009), and housing instability can present multiple barriers to accessing PrEP (Santa Maria et al., 2019). Economic transitions may also create conditions where emerging adults use informal sexual economies to earn income or obtain other resources necessary for survival (Stevens et al., 2017). Transactional sex, defined as the exchange of sex for basic, socioeconomic needs may elevate individuals’ risk for HIV, compromising individuals’ autonomy in sexual health decision-making, and thereby shaping how EAMSM engage with HIV prevention (Oldenburg et al., 2015).
Regarding access to care, emerging adults have greater control of healthcare decision-making compared to adolescence. This transition may facilitate access to PrEP by removing the need for parental consent to use medical services. However, many EAMSM experience challenges with healthcare insurance coverage (Kipke et al., 2007; Patel et al., 2017). Even those who are covered by a parent’s insurance plan may still face barriers to PrEP access, especially if they have not disclosed their sexual orientation to their parents (Moore Jr et al., 2019).
The profound social transitions MSM experience during emerging adulthood may be informative as local health systems seek to scale up PrEP implementation efforts for these communities. Given these transitions, we sought to examine how social identity support, descriptive PrEP norms, and economic instability are associated with PrEP engagement among EAMSM.
Materials and Methods
Procedures
Our data came from the Mid-Atlantic PrEP study, a web-based cross-sectional study exploring PrEP engagement among EAMSM. Recruitment took place through Grindr and Facebook (October 2018-February 2019) using ads on these platforms inviting users to participate in a survey about their community’s attitudes around sex. Participants were eligible if they were 18 to 25 years old, identified as cis-gender men, self-reported being HIV-negative or status unaware, had sex with a man in the past six months, and lived along the Philadelphia (PA), Baltimore (MD), and Washington, DC metropolitan corridor (i.e., reported residing in one of 1463 eligible zip codes). Eligible participants completed online informed consent followed by a 20–30-minute web survey and were compensated a $10 Amazon e-gift card. Surveys were verified by cross-checking for duplicate and legitimate email addresses and IP addresses (Bauermeister et al., 2012). The sample size was N = 290 EAMSM. Nine participants had missing data for at least one of our variables of interest. Listwise deletion was used to exclude these missing cases, yielding a final analytic sample of N = 281 EAMSM. All data were stored on a secure, university firewalled server. Study procedures were approved by our Institutional Review Board.
Measures
PrEP Continuum
The PrEP continuum (Parsons et al., 2017) was measured across five mutually-exclusive, ordered categories: (1) PrEP unaware, (2) aware but unwilling to use PrEP, (3) aware, willing, but no intention to use PrEP, (4) aware, willing, and intending to seek PrEP within three months, and (5) current PrEP users. EAMSM who had discontinued PrEP use were asked about their willingness and intention to begin PrEP again and were classified along the PrEP continuum according to these responses.
Social Identity Support
We constructed a social identity support latent variable indicated by gay community attachment, sexual orientation disclosure, and emotional support. To assess gay community attachment, we used four items adapted from a previously validated scale for racially and ethnically diverse populations (e.g., “I feel that I am part of my area’s LGBT community;” Frost & Meyer, 2012). A four-point scale was used to measure each of these items (0: Strongly disagree, 3: Strongly agree”), and the items had high internal consistency (Cronbach’s alpha = 0.86). Mean scores were calculated, resulting in a one-number estimate of gay community attachment, with higher numbers indicating higher gay community attachment.
For sexual orientation disclosure, participants were asked to indicate how many people (0: No one, 3: All) from each of the following groups who were aware of their sexual orientation: immediate family members, extended family members, friends in the LGBTQ community, and heterosexual friends (Aranda et al., 2015). These items had high internal consistency (Cronbach’s alpha=0.82) and were averaged to give a one-number estimate of sexual orientation disclosure, with higher numbers indicating greater disclosure.
Participants reported the extent (0: Not at all, 3: A lot) that they received social/emotional support from their friends, family, and the LGBTQ community, respectively. These items had moderate internal consistency (Cronbach’s alpha = 0.53) and were averaged, resulting in a one number estimate of social support, with higher numbers indicating greater social support.
Economic Instability
We constructed an economic instability latent variable indicated by housing instability, engagement in transactional sex, and health insurance status. For housing instability, participants reported if they had spent at least one night in the past 30 days in one of many provided non-permanent housing locations (e.g., a homeless shelter, a public place not intended for sleeping, on the street or anywhere outside). Housing instability was a binary variable that indicates an affirmative response to any of these options. Transactional sex was assessed by asking participants if they had exchanged anal or oral sexual intercourse with someone in the past 6 months because they needed money, food/groceries, drugs or alcohol, clothes or other material goods, college tuition or other education-related expenses, support for other family members/dependents, travel/transportation expenses, or housing/place to sleep (0: No; 1: Yes). Health insurance status was measured by self-reported health insurance coverage and dichotomized into private insurance (0) and uninsured or government assistance (1).
Descriptive PrEP Norms
We measured descriptive PrEP norms by asking EAMSM how many of their MSM friends they believed were using PrEP (0: None of them, 1: A few or very few of them, 2: Some of them, 3: Many of them, 4: Most of them or all of them).
Sociodemographic Characteristics
Participants self-reported their age, sexual orientation (i.e. Gay, Queer, Same Gender Loving, Homosexual, Bisexual or Pansexual), and racial/ethnic identity (i.e. Non-Hispanic White, Latino/Hispanic, Non-Hispanic Black, or Other/Multiracial). For multivariable analysis, race/ethnicity was collapsed into two groups due to low cell sizes (Non-Hispanic White and racial/ethnic minority).
Statistical Analysis
After generating descriptive statistics to characterize our study sample, we fit a structural equation model (SEM) to assess the relationships linking social identity support, descriptive PrEP norms and economic instability to progression along the PrEP continuum. SEMs allows for the estimation of unmeasured latent variables, which represent an underlying construct which is of interest to the researcher, while also modeling direct and indirect effects of both latent and measured variables. Using latent variables in this way both reduces the number of predictor variables that need to be estimated and allows for a more intuitive interpretation of the estimated relationships.
To evaluate the appropriateness of our latent variables, we used confirmatory factor analysis to estimate the factor loadings of each indicator variable on our proposed latent variables and assess the overall fit of this model. We used the comparative fit index (CFI), the Tucker-Lewis index (TLI), and the root mean squared error of approximation (RMSEA) to evaluate model fit, and Cronbach’s alpha to evaluate the internal consistency of our proposed latent factors. We then fit a full SEM to assess the various hypothesized relationships between the variables in the model. Given that we conceptualize the PrEP continuum as an ordered categorical variable, we used a diagonally weighted least squares estimator with robust standard errors to model ordinal regression of PrEP continuum progression on our predictor variables.
Analyses were performed in R 3.5.1(R Core Team) using the lavaan package (Rosseel, 2012) sem and cfa functions for SEMs and the psych package (Revelle, 2017) omega function to estimate factor saturation.
Results
Participant Characteristics
Participant characteristics are presented in Table 1. Most participants identified as Non-Hispanic White (n = 181, 64%), with a median age of 23 years (interquartile range [IQR] = [20,24]). On average, participants reported moderate levels of gay community attachment (median = 2.75, IQR = [2.25,3.25]), moderate levels of sexual orientation disclosure (median= 3.00, IQR = [2.25, 3.75]), and moderate to high levels of emotional support (median= 3.33, IQR = [3.00, 3.67]). Most participants believed that few or no members of their social network were taking PrEP (n = 185, 66%).
Table 1:
Summary of participant characteristics and PrEP continuum stage among emerging adult men who have sex with men (n = 281) from Mid-Atlantic PrEP Study (MAPS)
| Overall (n=281) |
|
|---|---|
|
| |
| Age, years (median, [IQR]) | 23 [20,24] |
| Race/Ethnicity | -- |
| Non-Hispanic White (n,%) | 181 (64) |
| Latino/Hispanic (n,%) | 37 (13) |
| Non-Hispanic Black (n,%) | 25 (9) |
| Other/Multiracial (n,%) | 38 (14) |
| Sexual Orientation | -- |
| Gay, Queer, Same Gender Loving, or Homosexual (n,%) | 229 (81) |
| Bisexual or Pansexual (n,%) | 52 (19) |
| Metropolitan Area | -- |
| Philadelphia (n,%) | 108 (38) |
| Baltimore (n,%) | 50 (18) |
| Washington D.C (n,%). | 123(44) |
| PrEP use in network, 1–5 (median, [IQR]) | 2 [1,3] |
| Gay community attachment, 1–4 (median, [IQR]) | 2.75 [2.25,3.25] |
| Sexual orientation disclosure, 1–4 (median, [IQR]) | 3.00 [2.25, 3.75] |
| Emotional support, 1–4 (median, [IQR]) | 3.33 [3.00, 3.67] |
| Housing instability (n, %) | 26 (9) |
| Transactional sex (n, %) | 29 (10) |
| Uninsured or government insurance (n, %) | 33 (12) |
| PrEP Continuum Stage | -- |
| PrEP Unaware (n, %) | 16 (6) |
| PrEP Aware (Unwilling) (n, %) | 33 (12) |
| PrEP Willing (Not Intending) (n, %) | 99 (35) |
| PrEP Intending (Not Using) (n, %) | 53 (19) |
| Current PrEP Use (n,%) | 80 (28) |
Figure 1 shows participants’ positions along the PrEP continuum. We found that 94% of participants were aware of PrEP (n = 265), 82% were willing to start using PrEP (n = 232), 47% intended to start using PrEP (n = 133), and 28% were currently using PrEP (n = 80).
Figure 1.
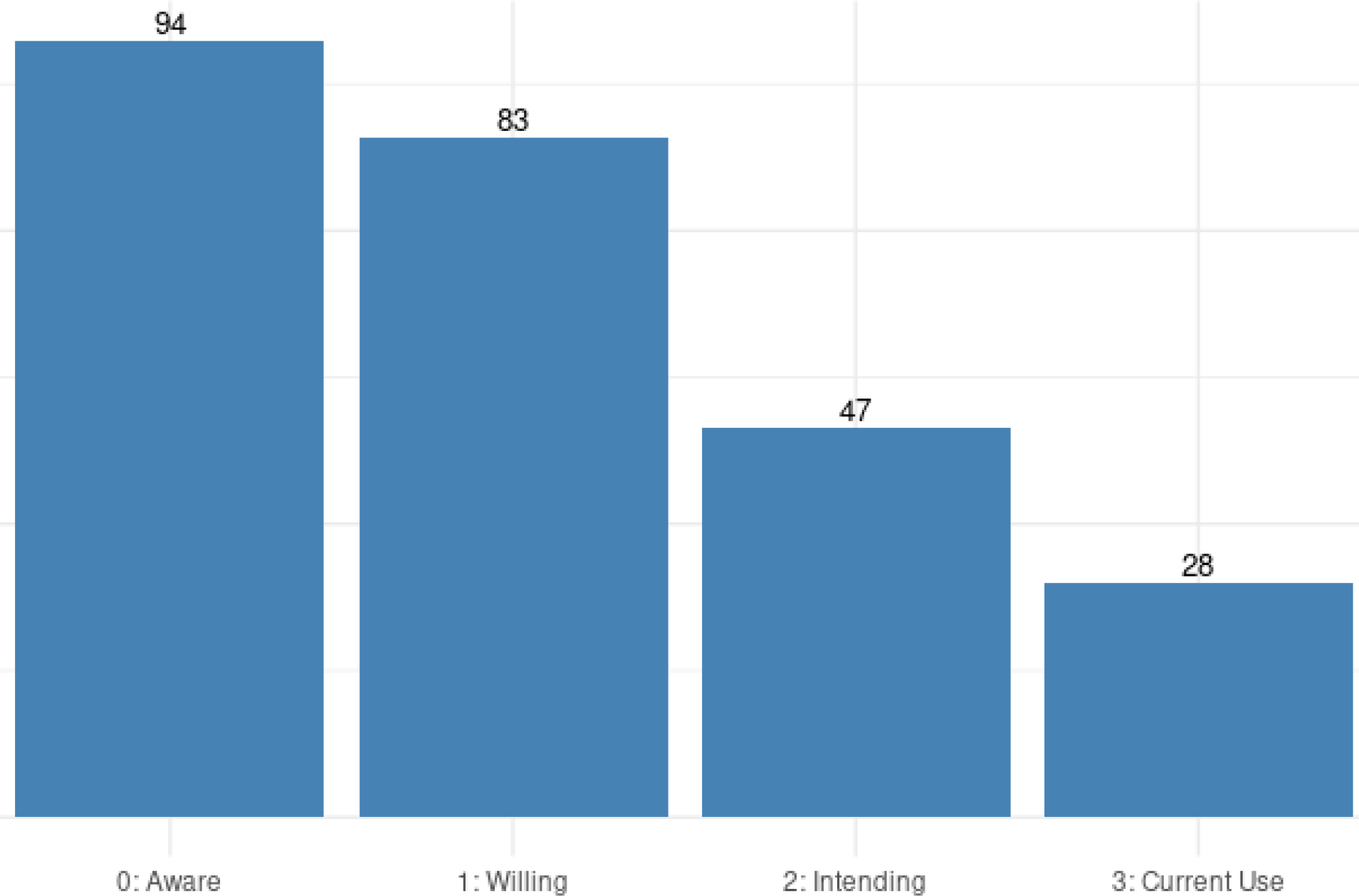
Position of study sample on PrEP continuum. Numbers on bars denote percentage of total sample that is at or beyond each level of the continuum.
Structural Equations Model
We first fit a measurement model to examine how our indicators loaded onto the proposed latent factors. The measurement model had good fit statistics (CFI = 0.97, TLI = 0.95, SRMR = 0.061, RMSEA = 0.034 [90% CI = {0.000,0.083}]). The three measures of social identity support had positive loadings onto a latent construct (see Table 2) and showed moderately high internal consistency (Cronbach’s alpha = 0.65), and the three measures of economic instability had positive loadings onto a latent construct with moderately high internal consistency (Cronbach’s alpha = 0.69).
Table 2:
Standardized factor loadings from measurement model and standardized regression coefficients from full structural model for structural pathways
| Path | Estimate (95% CI) |
|---|---|
|
| |
| Factor loadings for latent variables: | |
| Social Identity Support | |
| Gay community attachment | 0.53 (0.42, 0.64) |
| Sexual orientation disclosure | 0.52 (0.39, 0.64) |
| Emotional support | 0.83 (0.69, 0.96) |
| Economic Instability | |
| Housing instability | 0.63 (0.34, 0.93) |
| Transactional sex | 0.85 (0.52, 1.19) |
| Uninsured or government insurance | 0.50 (0.21, 0.78) |
| Direct effects: | |
| Social identity support → PrEP engagement | 0.10 (−0.12, 0.32) |
| Economic instability → PrEP engagement | −0.19 (−0.39, 0.02) |
| PrEP use in network → PrEP engagement | 0.29 (0.12, 0.46) |
| Social identity support → PrEP use in network | 0.63 (0.50, 0.76) |
| Economic instability → PrEP use in network | 0.16 (−0.04, 0.36) |
| Economic instability → Social identity support | −0.26 (−0.51, 0.01) |
| Age→ PrEP engagement | 0.17 (0.04,0.30) |
| Race→ PrEP engagement | 0.14 (−0.04,0.31) |
| Indirect effects: | |
| Social identity support → PrEP use in network → PrEP engagement | 0.18 (0.09, 0.28) |
| Economic instability → PrEP use in network → PrEP engagement | 0.05 (−0.02, 0.11) |
| Economic instability → Social identity support → PrEP use in network | −0.16 (−0.34, 0.02) |
| Economic instability → Social identity support → PrEP use in network → PrEP engagement | −0.05 (−0.10, 0.01) |
We then fit a full SEM that included direct and indirect pathways for the measured and latent variables (see Figure 2). This model showed adequate fit (CFI = 0.95, TLI = 0.91, SRMR = 0.075, RMSEA = 0.050 [90% CI = {0.021,0.076}]). Standardized path coefficients are presented in Table 2 for all hypothesized pathways. We found a positive, direct association between perceived PrEP use in network and PrEP engagement (β = 0.29, 95% CI = [0.12,0.46]) and a positive, direct association between social identity support and descriptive PrEP norms (β = 0.63, 95% CI = [0.50,0.76]). There were no other statistically significant direct associations, however there was a trend towards a negative association between economic instability and PrEP engagement (β = −0.19, 95% CI = [−0.39,0.02]). We found a significant, indirect association between social identity support and PrEP engagement through descriptive PrEP norms (β = 0.18, 95% CI = [0.09,0.28]). There were no other statistically significant indirect associations. See Supplementary File 1 for full model output.
Figure 2.
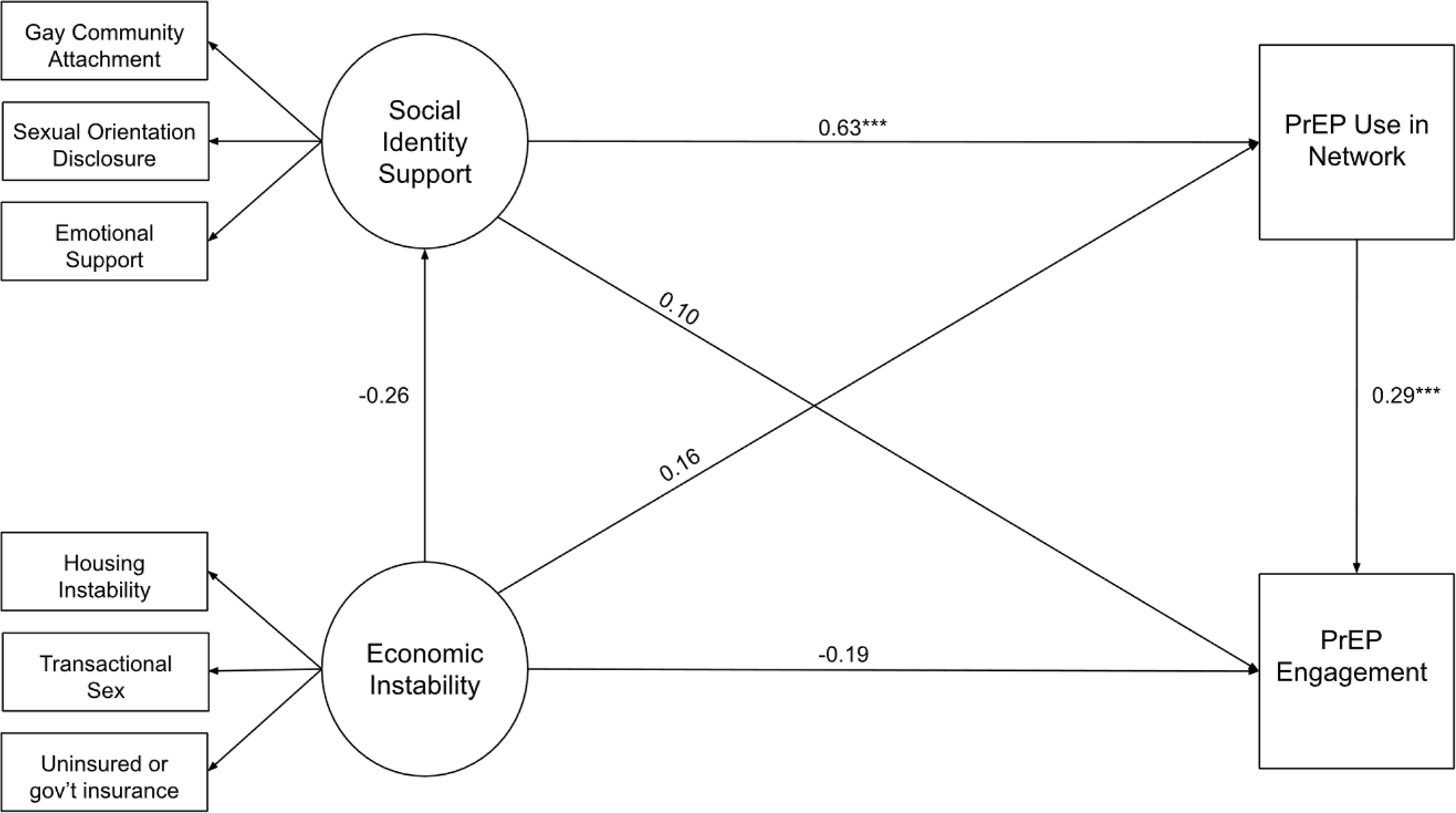
Diagram of full structural equation model, adjusted for age and race. Latent variables are represented by circles and observed variables are represented by squares. Only direct effects are shown. *** p<=.001, ** p<=.01, * p<=.05
Discussion
In this study, we propose a measurement model for social identity support and economic instability, and then use a structural model to test a series of hypotheses about these latent variables and their relationship to engagement with the PrEP continuum. Previous studies have found that the various components of our two latent variables (social identity support and economic instability) are associated with sexual health outcomes (Oldenburg et al., 2015; Ramirez-Valles, 2002; Santa Maria et al., 2019). In our measurement models we see evidence that our proposed latent variables can be measured by our proposed indicators (i.e., good fit statistics, positive loadings, and moderately high Cronbach’s alpha). Thus, our study provides some preliminary evidence for the conceptualization of these constructs.
We did not observe a direct association of social identity support on PrEP engagement; however, descriptive PrEP norms was directly linked and mediated the association of social identity support on PrEP engagement. These findings are supported by another recent study that found positive descriptive PrEP norms to be associated with greater intention to use PrEP (Walsh, 2019) and suggests that HIV prevention experts should consider how to increase and facilitate sex-positive, peer-based discussions about PrEP within MSM networks.
For EAMSM, social identity support may shape decisions in HIV prevention that involves the dynamics of self-acceptance, community attachments, and social support systems. Aspects of social identity support, specifically community attachment and social support, have been previously linked to PrEP engagement (Lelutiu-Weinberger et al., 2020; Schueler et al., 2019). Participation in gay community groups has been linked to increased awareness, knowledge, and PrEP uptake (Hotton et al., 2018; Mehrotra et al., 2018). Rather than directly influencing PrEP engagement, participating in LGBTQ-centered community organizations may connect young people to social networks where PrEP use is more common, discussed, and accepted, thereby motivating personal PrEP decision-making. Similarly, having supportive relationships with peers could facilitate opportunities to talk about sexual health in ways that are supportive and could foster positive perceptions about PrEP.
Though social identity support may facilitate exposure to network PrEP norms, this kind of support may be insufficient to catalyze PrEP engagement. Emerging adults who navigate new social communities and forge new connections might still lack critical elements necessary to adopt PrEP (e.g., trust). Furthermore, the influence of social identity support may be dependent on economic contexts. Economic barriers may preclude young people from accessing PrEP, even if they have high levels of community attachments. Future research should refine and validate the measurement of social identity support and continue to explore the connection between EAMSM’s social networks and psychosocial motivations to use PrEP.
The economic transitions that characterize emerging adulthood can create conditions of heightened HIV vulnerability for EAMSM with implications for PrEP engagement (Biello et al., 2018; Okafor et al., 2017). Our model supports measuring economic instability as a latent factor including transactional sex, housing instability, and insurance status. Our SEM exhibited a negative trend between economic instability and PrEP engagement, but this trend did not reach statistical significance. Given that few participants reported these economic instability indicators, it is possible that this trend would be more pronounced in a sample with greater variance in economic barriers. Measuring economic instability as a unified construct comprised of disparate but linked structural conditions may help illuminate the impact of economic vulnerability on PrEP engagement for EAMSM and may inform efforts to improve PrEP rollout for this community.
Our study provided key insights into EAMSM’s PrEP engagement; however, this study has several limitations. First, although our study design allowed us to fit a complex SEM, we did not have adequate statistical power to explore differences by racial/ethnic groups. Future studies should recruit larger samples of Black and Latinx EAMSM to better understand how social and structural factors shape their PrEP engagement. Second, our sample evinced high engagement with the PrEP continuum compared to national estimates. This allowed for granular investigation of the PrEP continuum, but also suggests that our sample may represent a subset of EAMSM who have more information, motivation, and access to PrEP than many of their peers. Third, our measurement of health insurance status did not distinguish between those who had coverage under a parent’s health insurance plan or their own. This distinction could illuminate potential challenges to autonomy in seeking PrEP among EAMSM who are dependent on their parent’s insurance plans. Lastly, we cannot assume causal relationships given our study design’s cross-sectional nature. Longitudinal research may better inform how changes in social and structural factors impact movement along the PrEP continuum.
Our study has implications for health policy and practice. Clinicians should consider the impact of social and economic transitions on sexual health decision-making when working with EAMSM. Social environments that support self-acceptance among EAMSM may create conditions that promote PrEP engagement (Flores et al., 2020). Those who live in households without support systems or who have recently transitioned to new social environments, like a new school or new city, may benefit from referrals to PrEP navigation resources. Clinicians and policy makers should also be aware of the potential impact of economic instability on how emerging adults engage with PrEP-related medical care. Discussing insurance options for accessing PrEP at minimal cost will be critical to connecting EAMSM facing economic barriers to PrEP. Institutional and government programs are needed to expand low-cost avenues for PrEP, with prioritized marketing strategies for EAMSM. Additionally, public health efforts to increase EAMSM’s PrEP engagement should support peer-led interventions to promote PrEP use within social networks (Patel et al., 2018; Young et al., 2018) and leverage social networks to promote sex-positive conversations about sexual health and PrEP use.
Conclusion
The addition of PrEP to the HIV prevention toolkit has helped mitigate new HIV infections for EAMSM. HIV researchers must continue to build upon the current understanding of multilevel factors linked to MSM’s PrEP engagement as they transition from adolescence to emerging adulthood. During this transition, social and economic forces can play a prominent role in decisions about sexual health with important implications for how young people engage with PrEP. For EAMSM, the interactions between social networks, identity support, and structural factors create a complex landscape that shapes awareness, interest, and access to PrEP. Understanding these connections will be critical to creating programs that facilitate young people’s access to PrEP during a stage of heightened social vulnerability to HIV.
Supplementary Material
Funding
This manuscript resulted (in part) from research supported by the Centers for AIDS Research at the University of Pennsylvania (P30 AI 045008; PI Ronald Collman), Johns Hopkins University (P30 AI 094189; PI: Richard Chaisson), and the District of Columbia (P30 AI 117970; PI: Alan E. Greenberg). This collaboration is supported by the following NIH Co-Funding and Participating Institutes and Centers: NIAID, NCI, NICHD, NHLBI, NIDA, NIMH, NIA, FIC, NIGMS, NIDDK, and OAR. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflicts of Interest Statement
The authors have no relevant financial or non-financial interests to disclose.
Data Availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
References
- Anderson PL, Glidden DV, Liu A, Buchbinder S, Lama JR, Guanira JV, McMahan V, Bushman LR, Casapía M, Montoya-Herrera O, & others. (2012). Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Science Translational Medicine, 4(151), 151ra125–151ra125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnett JJ (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55(5), 469. [PubMed] [Google Scholar]
- Bauermeister JA, Pingel E, Zimmerman M, Couper M, Carballo-Dieguez A, & Strecher VJ (2012). Data quality in HIV/AIDS web-based surveys: Handling invalid and suspicious data. Field Methods, 24(3), 272–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biello K, Bazzi A, Mimiaga M, Biancarelli D, Edeza A, Salhaney P, Childs E, & Drainoni M (2018). Perspectives on HIV pre-exposure prophylaxis (PrEP) utilization and related intervention needs among people who inject drugs. Harm Reduction Journal, 15(1), 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2018a). HIV prevention pill not reaching most Americans who could benefit – especially people of color. [Press release]. Atlanta: CDC. https://www.cdc.gov/nchhstp/newsroom/2018/croi-2018-PrEP-press-release.html
- Centers for Disease Control and Prevention. (2018b). HIV Surveillance Report, 2017. Vol 29. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html
- Centers for Disease Control and Prevention. (2021). Core indicators for monitoring the Ending the HIV Epidemic initiative (preliminary data): National HIV Surveillance System data reported through September 2021; and preexposure prophylaxis (PrEP) data reported through June 2021. HIV Surveillance Data Tables 2021;2(No. 5). Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/library/reports/surveillance-data-tables/index.html. [Google Scholar]
- Centers for Disease Control and Prevention: US Public Health Service. (2021). Preexposure prophylaxis for the prevention of HIV infection in the United States—2021 Update: A clinical practice guideline. Centers for Disease Control and Prevention: US Public Health Service. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf. [Google Scholar]
- Chaudoir SR, & Fisher JD (2010). The disclosure processes model: Understanding disclosure decision making and postdisclosure outcomes among people living with a concealable stigmatized identity. Psychological Bulletin, 136(2), 236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlayson T, Cha S, Xia M, Trujillo L, Denson D, Prejean J, Kanny D, Wejnert C, Abrego M, Al-Tayyib A, & others. (2019). Changes in HIV preexposure prophylaxis awareness and use among men who have sex with men—20 urban areas, 2014 and 2017. Morbidity and Mortality Weekly Report, 68(27), 597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores DD, Meanley SP, Wood SM, & Bauermeister JA (2020). Family characteristics in sex communication and social support: Implications for emerging adult men who have sex with men’s PrEP engagement. Archives of Sexual Behavior, 49(6), 2145–2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost DM, & Meyer IH (2012). Measuring community connectedness among diverse sexual minority populations. Journal of Sex Research, 49(1), 36–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hotton AL, Keene L, Corbin DE, Schneider J, & Voisin DR (2018). The relationship between Black and gay community involvement and HIV-related risk behaviors among Black men who have sex with men. Journal of Gay & Lesbian Social Services, 30(1), 64–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juster R-P, Smith NG, Ouellet É, Sindi S, & Lupien SJ (2013). Sexual orientation and disclosure in relation to psychiatric symptoms, diurnal cortisol, and allostatic load. Psychosomatic Medicine, 75(2), 103–116. [DOI] [PubMed] [Google Scholar]
- Kelley CF, Kahle E, Siegler A, Sanchez T, del Rio C, Sullivan PS, & Rosenberg ES (2015). Applying a PrEP continuum of care for men who have sex with men in Atlanta, Georgia. Clinical Infectious Diseases, 61(10), 1590–1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kipke MD, Kubicek K, Weiss G, Wong C, Lopez D, Iverson E, & Ford W (2007). The health and health behaviors of young men who have sex with men. Journal of Adolescent Health, 40(4), 342–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lelutiu-Weinberger C, Wilton L, Koblin BA, Hoover DR, Hirshfield S, Chiasson MA, Nandi V, Usher D, & Frye V (2020). The Role of Social Support in HIV Testing and PrEP Awareness among Young Black Men and Transgender Women Who Have Sex with Men or Transgender Women. Journal of Urban Health, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martos AJ, Nezhad S, & Meyer IH (2015). Variations in sexual identity milestones among lesbians, gay men, and bisexuals. Sexuality Research and Social Policy, 12(1), 24–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meanley S, Connochie D, Choi SK, Bonett S, Flores DD, & Bauermeister JA (2020). Assessing the Role of Gay Community Attachment, Stigma, and PrEP Stereotypes on Young Men Who Have Sex with Men’s PrEP Uptake. AIDS and Behavior, 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehrotra ML, Amico KR, McMahan V, Glidden DV, Defechereux P, Guanira JV, & Grant RM (2018). The role of social relationships in PrEP uptake and use among transgender women and men who have sex with men. AIDS and Behavior, 22(11), 3673–3680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore KL Jr, Dell S, Oliva M, Hsieh Y-H, Rothman RE, & Arrington-Sanders R (2019). Do confidentiality concerns impact pre-exposure prophylaxis willingness in emergency department adolescents and young adults? The American Journal of Emergency Medicine, 37(6), 1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okafor CN, Gorbach PM, Ragsdale A, Quinn B, & Shoptaw S (2017). Correlates of preexposure prophylaxis (PrEP) use among men who have sex with men (MSM) in Los Angeles, California. Journal of Urban Health, 94(5), 710–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldenburg CE, Perez-Brumer AG, Reisner SL, & Mimiaga MJ (2015). Transactional sex and the HIV epidemic among men who have sex with men (MSM): Results from a systematic review and meta-analysis. AIDS and Behavior, 19(12), 2177–2183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parent MC, Woznicki N, Dillon FR, & Pituch KA (2020). Psychosocial barriers to pre-exposure prophylaxis (PrEP) uptake: The roles of heterosexual self-presentation, sexual risk, and perceived peer prep use. Psychology of Men & Masculinities. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Rendina HJ, Lassiter JM, Whitfield TH, Starks TJ, & Grov C (2017). Uptake of HIV pre-exposure prophylaxis (PrEP) in a national cohort of gay and bisexual men in the United States: The motivational PrEP cascade. Journal of Acquired Immune Deficiency Syndromes (1999), 74(3), 285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel RR, Mena L, Nunn A, McBride T, Harrison LC, Oldenburg CE, Liu J, Mayer KH, & Chan PA (2017). Impact of insurance coverage on utilization of pre-exposure prophylaxis for HIV prevention. PLoS One, 12(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel VV, Ginsburg Z, Golub SA, Horvath KJ, Rios N, Mayer KH, Kim RS, & Arnsten JH (2018). Empowering with PrEP (E-PrEP), a peer-led social media–based intervention to facilitate HIV preexposure prophylaxis adoption among young Black and Latinx gay and bisexual men: Protocol for a cluster randomized controlled trial. JMIR Research Protocols, 7(8), e11375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. (n.d.). R: A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.R-project.org/ [Google Scholar]
- Ramirez-Valles J (2002). The protective effects of community involvement for HIV risk behavior: A conceptual framework. Health Education Research, 17(4), 389–403. [DOI] [PubMed] [Google Scholar]
- Revelle WR (2017). psych: Procedures for personality and psychological research. [Google Scholar]
- Rosseel Y (2012). Lavaan: An R package for structural equation modeling and more. Version 0.5–12 (BETA). Journal of Statistical Software, 48(2), 1–36. [Google Scholar]
- Santa Maria D, Gallardo KR, Narendorf S, Petering R, Barman-Adhikari A, Flash C, Hsu H-T, Shelton J, Ferguson K, & Bender K (2019). Implications for PrEP Uptake in Young Adults Experiencing Homelessness: A Mixed Methods Study. AIDS Education and Prevention, 31(1), 63–81. 10.1521/aeap.2019.31.1.63 [DOI] [PubMed] [Google Scholar]
- Schueler K, Ferreira M, Nikolopoulos G, Skaathun B, Paraskevis D, Hatzakis A, Friedman SR, & Schneider JA (2019). Pre-exposure prophylaxis (PrEP) awareness and use within high HIV transmission networks. AIDS and Behavior, 23(7), 1893–1903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelton KH, Taylor PJ, Bonner A, & van den Bree M (2009). Risk factors for homelessness: Evidence from a population-based study. Psychiatric Services, 60(4), 465–472. [DOI] [PubMed] [Google Scholar]
- Siegler AJ, Mouhanna F, Giler RM, Weiss K, Pembleton E, Guest J, Jones J, Castel A, Yeung H, Kramer M, & others. (2018). The prevalence of pre-exposure prophylaxis use and the pre-exposure prophylaxis–to-need ratio in the fourth quarter of 2017, United States. Annals of Epidemiology, 28(12), 841–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens R, Icard L, Jemmott JB, O’leary A, Rutledge S, Hsu J, & Stephens-Shields A (2017). Risky trade: Individual and neighborhood-level socio-demographics associated with transactional sex among urban African American MSM. Journal of Urban Health, 94(5), 676–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van de Bongardt D, Reitz E, Sandfort T, & Deković M (2015). A meta-analysis of the relations between three types of peer norms and adolescent sexual behavior. Personality and Social Psychology Review, 19(3), 203–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh JL (2019). Applying the information–motivation–behavioral skills model to understand PrEP intentions and use among men who have sex with men. AIDS and Behavior, 23(7), 1904–1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz BM, Quinn DM, & Williams MK (2016). Out and healthy: Being more “out” about a concealable stigmatized identity may boost the health benefits of social support. Journal of Health Psychology, 21(12), 2934–2943. [DOI] [PubMed] [Google Scholar]
- Young LE, Schumm P, Alon L, Bouris A, Ferreira M, Hill B, Khanna AS, Valente TW, & Schneider JA (2018). PrEP Chicago: A randomized controlled peer change agent intervention to promote the adoption of pre-exposure prophylaxis for HIV prevention among young Black men who have sex with men. Clinical Trials, 15(1), 44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to their containing information that could compromise the privacy of research participants.


