Abstract
Objective:
Although Goldilocks mastectomy offers good aesthetic outcomes. Removal of the nipple-areolar complex (NAC) often has a negative psychological impact. The objective of this study was to assess the feasibility and esthetic outcome of this technique with salvage of the NAC using a dermal pedicle.
Materials and Methods:
The study included female patients suffering from breast carcinoma with large and or ptotic breast. Patients were offered Goldilocks mastectomy. Those who were unfit for anesthesia, those with locally advanced or metastatic disease or those refusing the procedure were excluded.
Results:
Fifteen female patients (18 breasts) with a mean age of 51.6 years underwent Goldilocks breast reconstruction with a trial of NAC preservation. The mean body mass index was 39.1 kg/m2. More than half (56%) were cup C, while 44% were cup D. Seven cases (46.7%) showed grade II ptosis and 8 (53.3%) were grade III. The mean operative time was 168 minutes (range 130–240 minutes). NAC ischemic changes were noted in five cases; two (11%) were partial while three (17%) were total. Two cases (11%) suffered from flap loss and one of them was total. No locoregional recurrence or distant metastases were observed.
Conclusion:
The Goldilocks mastectomy with nipple preservation is an appealing and feasible option for a certain group of patients who have large-sized and/or ptotic breasts. Nevertheless, it is a time-consuming technique with relatively higher rates of flap and NAC complications. Further, studies are required with a larger number of cases and longer follow-up.
Keywords: Goldilocks mastectomy, breast reconstruction, nipple areola complex
Key Points
• Goldilocks mastectomy
• Breast reconstruction
• Nipple areola complex
Introduction
Skin- and nipple-sparing mastectomies are challenging procedures, especially in large and ptotic breasted-women due to the resulting redundant skin flaps (1). The Goldilocks mastectomy was designed to make use of the redundant lower pole skin and subcutaneous fat to recreate a breast mound without a prosthetic implant or autologous tissue transfer. The main challenge for this technique was preservation of the nipple areolar complex (NAC) due to the relocated upper areolar border to the newly created inframammary crease and the placement of the lower areolar border under the upper pole which interferes with blood supply of the NAC (2). Although NAC preservation was described with Goldilocks mastectomy in the form of skin graft with success (3, 4), NAC sparing is still questionable. To the best of our knowledge, there are few studies investigating the possibility of NAC preservation with Goldilocks mastectomy (5). This work was designed to evaluate the feasibility of NAC sparing during the Goldilocks mastectomy.
Materials and Methods
Patients
The study was conducted in the period from February 2019 to February 2022. Fifteen consecutive patients with breast carcinoma who were offered Goldilocks mastectomy were included in the study. Patients with large-sized and or ptotic breasts who were not candidates for breast conserving surgery (BCS) were included. Patients who refused the procedure or those with history of breast surgery that might interfere with vascularity of the skin flaps were excluded. All patients were diagnosed through the symptomatic and screening service in the oncology institute. All patients were informed about the expected advantages and risks of the procedure, with the possibility of nipple necrosis and written consents were obtained. The study obtained the required approval from the local ethical committee.
Surgical technique
Preoperative marking was performed in the standing position using a Wise pattern (Figure 1A). The NAC was reduced to a 42-mm diameter and left intact as the keyhole pattern is de-epithelialized (Figure 1A). When creating the circum-areolar incision, we took great care in order not to divide the thicker fibrous dermal layer with a full-thickness incision to protect the subdermal vascular plexus. De-epithelization and tissue dissection was done using tumescent infiltration and scissor dissection (Figure 1B). The tumescent fluid was a mixture of lidocaine 2% in a total maximum dose of 20 mg/kg, adrenaline in a dose of 2 mg 1/1.000, sodium bicarbonate which is diluted in saline then injected at the subdermal and subcutaneous tissue till it becomes tense, edematous, and swollen to facilitate the de-epithelialization process. The standard mastectomy flap was created via the lateral pillar of the keyhole pattern (Figure 2A). The plane was created at the gross interface of the parenchyma and subdermal fat by infiltration of tumescent fluid with delicate scissor dissection, avoiding injury of the subdermal vascular plexus (Figure 2B). The breast was elevated from the chest wall and sent for pathological evaluation. The skin flaps represent the entire skin envelop of the breast with the de-epithelialized keyhole portion containing the NAC. When necessary, sentinel lymph node biopsy and/or axillary dissection was carried out through the same incisions. Once the supply of the most distal portion of the flaps and NAC was adequate (Figure 3A). The NAC was transposed to the previously marked position with tailoring sutures while the medial and lateral vertical limbs of the keyhole were approximated (Figure 3B). The de-epithelialized fasciocutaneous flaps were folded to provide volume. Adjustments were made with the patient in the sitting position. When the configuration was satisfactory, the tailoring sutures were removed, drains were placed, and the dermal closure was accomplished (Figure 4).
Figure 1.
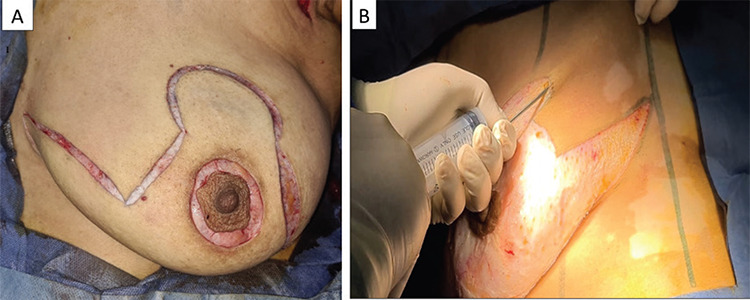
A. Intraoperative: marking the wise pattern + circum-areolar incision. B. Subcutaneous tumescent fluid infiltration
Figure 2.
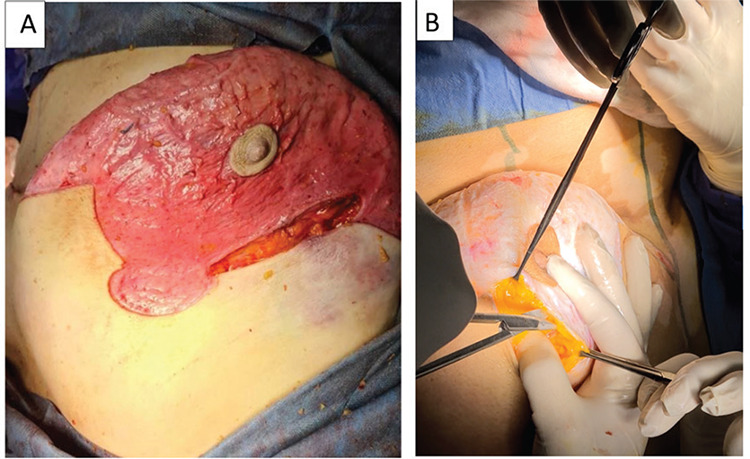
A. Mastectomy via lateral pillar of keyhole pattern. B. Scissor dissection through mastectomy flap plane
Figure 3.
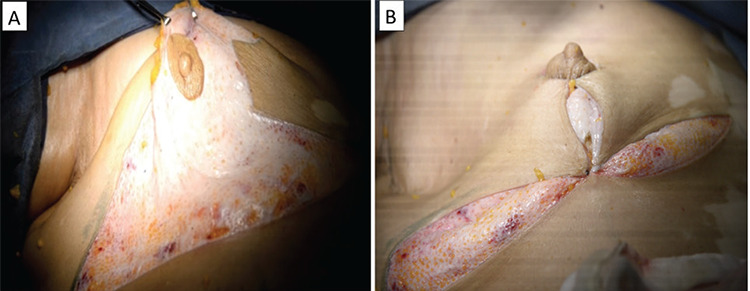
A. The de-epithelialized keyhole containing NAC. B. Closure of the upper envelope over the lower de-epithelialized dermal flap
Figure 4.

Inverted T shape closure with the patient in sitting position
Follow-up
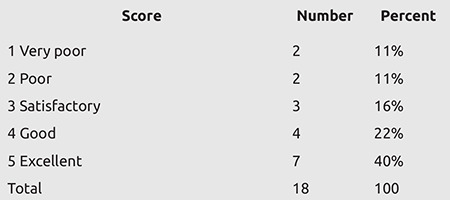
The follow-up schedule was weekly in the first month, then every three months after that for 15 months. Patients were assessed physically to detect early postoperative complications, including infection, hematoma, seroma, wound problems, flap loss and NAC congestion or ischemia. The aesthetic outcome was assessed by independent surgeons during the postoperative follow-up and images were judged by a panel of three surgeons. The aesthetic results were estimated on a 5-points scale (excellent: 5, good: 4, fair: 3, poor: 2, bad: 1) depending on multiple parameters, including volume symmetry, shape of breast mound, symmetry of NAC and post-irradiation changes. Delay in adjuvant therapy, local recurrence or distant metastasis were recorded.
Results
Between February 2020 and February 2022, a total of 15 female patients (18 breasts) with breast cancer with large sized and or ptosed breasts were offered Goldilocks mastectomy with nipple preservation. Three cases went for bilateral nipple sparing goldilocks mastectomy. Median follow-up was 15 months (range 3–24 months). Table 1 shows patient and tumor characteristics. The mean age was 51.6 years old (range 33 to 70 years; Table 1). The mean body mass index (BMI) was 39.1 kg/m2. Five patients were recorded with medical co-morbidities (three were diabetic and hypertensive). Four patients had a history of neoadjuvant therapy and 11 patients proceeded for upfront surgery. Eight patients received adjuvant radiotherapy. Table 2 shows the operative details. The mean operative time was 168 minutes (ranging from 130 to 240 minutes). The mean estimated blood loss was 110 cc (50–250 cc) with no intraoperative blood transfusion. Regarding complications (Table 3), two cases (11%) suffered from wound gaping, neither of whom was diabetic. Both were managed by refashioning and closure under local anesthesia. NAC ischemic changes occurred in five cases; two (11%) were managed by medical treatment and frequent dressing using heparin-soaked gauze, and they completely recovered. However, three cases (17%) suffered from total NAC loss and underwent NAC amputation. Two cases (11%) suffered from flap loss. One of them exhibited total flap loss, and it was managed by flap amputation and immediate closure under general anesthesia. The other case showed partial flap loss and underwent debridement and closure (Figure 5). Seroma developed in one case (5.5%), and this was managed by tube drain insertion under local anesthesia, as aspiration by wide pore needle failed to control the condition. One case (5.5%) suffered from superficial skin necrosis, and this was managed by topical ointments, dressing and medications until complete resolution. No cases suffered from fat necrosis during the follow-up period.
Table 1. Patients and tumor characteristics.
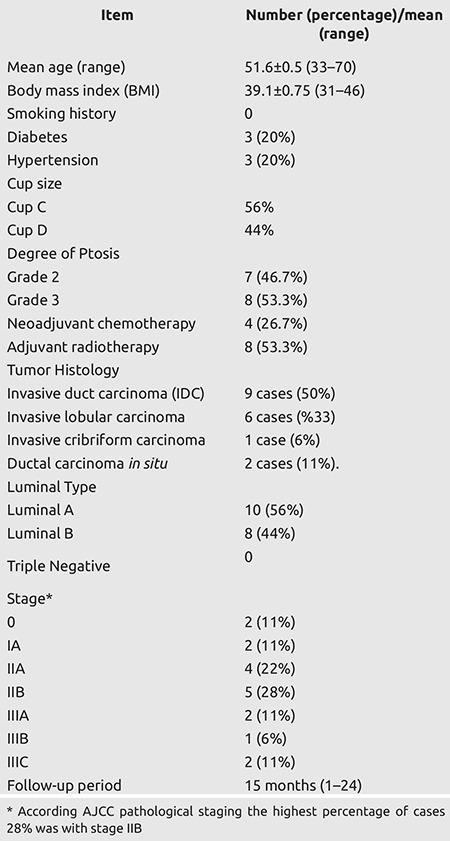
Table 2. Operative details.
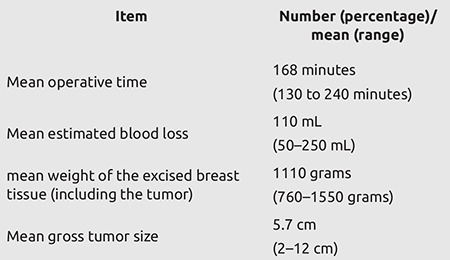
Table 3. Post-operative complications.
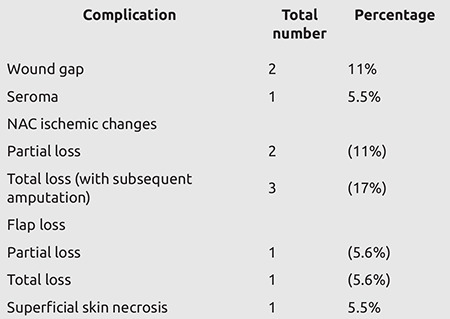
Figure 5.

NAC necrosis; A partial, B: complete
Esthetic Outcome
Seven (40%) patients were scored as excellent, four (22%) as good, and three (16%) as satisfactory. Two patients (11%) were scored as poor and other two (11%) as very poor (Table 4).
Table 4. Cosmetic outcome evaluation.
Oncologic Outcome
There was a median follow-up period of 15 (1–24) months, during which no loco-regional recurrences or distant metastasis were recorded.
Discussion and Conclusion
The Goldilocks procedure has increased in popularity since its original description in 2012 as an alternative for immediate breast reconstruction, particularly for obese women who are not candidates for traditional prosthetic or autologous reconstruction (1, 4). The aim of this technique was to reconstruct a breast mound exclusively from the cutaneous mastectomy flap tissue. To achieve a more aesthetically acceptable result, certain modifications have been made, such as free nipple grafting, simultaneous addition of the LICAP perforator flap, usage of this technique as a bridge for implant-based breast reconstruction or fat grafting (5, 6). In 2018, Richardson and Aronowitz (5) published a case report for bilateral Goldilocks mastectomy with in situ NAC preservation using a dermal pedicled flap. To our knowledge, this is the first case series in which the Goldilocks technique has been utilized for autologous reconstruction with in situ NAC preservation. Fifteen patients (18 breasts) with large-sized (CUP C and D) ptotic breasts who were not eligible for or refused BCS and other oncoplastic techniques. Counselling about a contralateral procedure to improve the overall symmetry was performed. Three cases underwent contralateral inferior pedicled reduction. One case underwent a modified radical mastectomy 15 years previously without reconstruction. Three cases went for bilateral, nipple-sparing Goldilocks mastectomy and eight cases refused contralateral symmetrization (7). Our BMI is relatively higher than the study of Heather Richardson in 2012 (sample of 32 women with a mean BMI 30.3 kg/m2 and range 18–51.9 kg/m2 (4). The mean age was 51.6 years with a range of 33–70 years. The older patients had greater appreciation for this technique, and they were satisfied with the outcome (8). One third of our patients had comorbidities, like hypertension and diabetes. In other studies, this ratio was 50% (9). The mean operative time was 168 minutes ranging for 120–240 minutes, which is longer than the initial technique of Goldilocks (its mean operative time was 120 minutes). This may be due to the time taken for NAC preservation. Regarding complications, two cases (11%) suffered from wound gaping, and they were managed by refashioning and suturing under local anesthesia. There was one case of seroma, which was managed by insertion of a tube drain under local anesthesia when frequent aspiration failed to resolve the condition. There were no cases of hematoma. One of the most important advantages of this technique is preservation and maintenance of nipple protrusion, which is lost in most cases with nipple grafting which may also suffer from hypopigmentation (9). NAC ischemic changes was noted in five cases; two (11%) were managed by medical treatment and frequent dressing using heparin-soaked gauze, and both totally improved. In three cases (17%), there was a NAC loss, and they underwent NAC amputation. Two cases (11%) suffered from flap loss, one of them was total, and it was managed by flap amputation and primary closure while the other was partial, and it underwent debridement and refashioning. One case (5.5%) suffered from superficial skin necrosis and infection, and it was managed by local ointments, dressing and medical treatment till complete resolution. No cases suffered from fat necrosis during the follow-up period. This matches with most of the complication rates in the literature; Davies et al. (10) reported a rate of 17.2% major complications, 23%minor and 61% of patients who had no complications. In our study, we faced the primary disadvantage of Goldilocks procedure, which was the limited window for glandular resection. This problem was solved by glandular resection from both pillars of the skin flaps.
The Goldilocks mastectomy with nipple preservation is an appealing and feasible option for a certain group of patients who have large-sized and/or ptotic breasts. Nevertheless, it is a time-consuming technique with relatively higher rates of flap and NAC complications. Further, studies are required with a larger number of cases and longer follow-up.
Footnotes
Ethics Committee Approval: The study obtained the required approval from the local ethical committee (Medical Research Ethics Committee Institutional Review Board – approval number: MS.20.10.11, date: 05.01.2021).
Informed Consent: Written consents were obtained.
Peer-review: Internally and externally peer-reviewed.
Authorship Contributions
Surgical and Medical Practices: A.S., K.B., A.K., I.E., A.H., E.H.; Concept: A.S., K.B.; Design: A.S., A.K.; Data Collection or Processing: A.S., K.B., A.K.; Analysis or Interpretation: A.S., K.B., A.K.; Literature Search: A.S., K.B., A.K., A.H.; Writing: A.S., K.B., A.K., I.E., A.H., E.H.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study received no financial support.
References
- 1.Zavala KJ, Kwon JG, Han HH, Kim EK, Eom JS. The Goldilocks technique: An alternative method to construct a breast mound after prosthetic breast reconstruction failure. Arch Plast Surg. 2019;46:475–479. doi: 10.5999/aps.2018.00808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oliver JD, Chaudhry A, Vyas KS, Manrique OJ, Martinez-Jorge J. Aesthetic Goldilocks mastectomy and breast reconstruction: promoting its use in the ideal candidate. Gland Surg. 2018;7:493–495. doi: 10.21037/gs.2018.07.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chaudhry A, Oliver JD, Vyas KS, Alsubaie SA, Manrique OJ, Martinez-Jorge J. Outcomes analysis of Goldilocks mastectomy and breast reconstruction: A single institution experience of 96 cases. J Surg Oncol. 2019;119:1047–1052. doi: 10.1002/jso.25465. [DOI] [PubMed] [Google Scholar]
- 4.Richardson H, Ma G. The Goldilocks mastectomy. Int J Surg. 2012;10:522–526. doi: 10.1016/j.ijsu.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Richardson H, Aronowitz JA. Goldilocks Mastectomy with Bilateral In Situ Nipple Preservation Via Dermal Pedicle. Plast Reconstr Surg Glob Open. 2018;6:e1748. doi: 10.1097/GOX.0000000000001748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Biasio F, Zingaretti N, Mura S, Fin A, Riccio M, Parodi PC. A new method of salvaging nipple projection after secondary nipple reconstruction using locoregional flap. Indian J Plast Surg. 2017;50:107–108. doi: 10.4103/ijps.IJPS_47_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schwartz Jean-Claude D, Skowronski Piotr P. Total single-stage autologous breast reconstruction with free nipple grafts. Plast Reconstr Surg. 2015;3:e587. doi: 10.1097/GOX.0000000000000563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zeeneldin AA, Ramadan M, Gaber AA, Taha FM. Clinico-pathological features of breast carcinoma in elderly Egyptian patients: a comparison with the non-elderly using population-based data. J Egypt Natl Canc Inst. 2013;25:5–11. doi: 10.1016/j.jnci.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 9.Manrique OJ, Kuruoglu D, Yan M, Bustos SS, Boughey JC, Harless CA, et al. Immediate Breast Reconstruction Using the Goldilocks Procedure: A Balance between More Surgery and Patient Satisfaction. Plast Reconstr Surg. 2022;149:801–809. doi: 10.1097/PRS.0000000000008895. [DOI] [PubMed] [Google Scholar]
- 10.Davies K, Allan L, Roblin P, Ross D, Farhadi J. Factors affecting post-operative complications following skin sparing mastectomy with immediate breast reconstruction. Breast. 2011;20:21–25. doi: 10.1016/j.breast.2010.06.006. [DOI] [PubMed] [Google Scholar]


