Abstract
Objective:
The role of baseline and post-treatment standardized uptake value (SUVmax) values in predicting pathological response in patients with breast cancer after neoadjuvant chemotherapy (NAC).
Materials and Methods:
Thirty patients with invasive ductal breast cancer were included in this retrospective study. F-18 fluorodeoxyglucose (FDG) positron emission tomography/computerized tomography (PET/CT) examinations were performed before and after NAC. Pretreatment SUVmax (SUVmax I), post-treatment SUVmax (SUVmax II) and ΔSUVmax values of primary breast cancer were obtained. Breast tumor pathology preparations were examined for the evaluation of tumor response according to the Miller and Payne classification. Patients were grouped as responding to treatment (pCR) and unresponsive to treatment (nonpCR). In all analyses, p<0.05 was considered statistically significant.
Results:
The mean age of the 30 patients included in the study was 51.2±11.98 years. In the study-defined grouping, 13 patients (43.3%) were nonresponders and 17 patients (56.7%) were responders. ΔSUVmax was significantly greater in the responders group compared to the nonresponders group, while SUVmax II was lower (p = 0.001 and p = 0.004, respectively). There was no significant difference between the responders and nonresponders in terms of age, tumor diameter, and SUVmax I values. Multivariate logistic regression analysis showed ΔSUVmax to be the only independent predictive factor for pCR.
Conclusion:
F-18 FDG PET/CT was an effective method in evaluating the treatment response after NAC in breast cancer, and ΔSUVmax and post-treatment SUVmax can be used to predict the response of the primary tumor to treatment.
Keywords: Breast cancer, F-18 FDG, SUVmax, neoadjuvant chemotherapy
Key Points
• F-18 FDG PET/CT is an effective method in evaluating the treatment response after NAC in breast cancer.
• ΔSUVmax and post-treatment SUVmax values correlate with pathological evaluation in predicting pCR.
• Multivariate logistic regression analysis showed ΔSUVmax to be the only independent predictive factor for pCR.
Introduction
Breast cancer is the most common type of cancer among women and its incidence has been increasing over the years (1). In the treatment of breast cancer, neoadjuvant chemotherapy (NAC) has recently become more frequently used. NAC is preferred, especially in locally advanced breast cancer, to reduce tumor volume and to allow breast-conserving surgery (2). In addition, it is stated that NAC has advantages, such as early detection of possible resistance to chemotherapy and predicting prognosis (3). Patients with pathological complete response (pCR) after NAC had better disease-free survival and overall survival rates than patients without a complete response (4). Although anatomical imaging methods are primarily used in the evaluation of response after NAC, there are some limitations. Conventional methods may not be able to clearly distinguish between viable tumor tissue and fibrotic scar tissue in patients with residual tissue after treatment.
2-deoxy-2-[18F]-fluoro-D-glucose positron emission tomography/computed tomography (F-18 FDG PET/CT) is a molecular imaging method frequently used in oncology practice to evaluate response to treatment. Glucose metabolism is increased in cancer tissue and this a decrease in the metabolic activity of the residual tumor tissue after NAC is indicative of the response to treatment. In the literature, there are several studies investigating the accuracy of F-18 FDG PET/CT in evaluating response to treatment after NAC, with the pathological response criteria as reference (5, 6, 7, 8, 9). Due to the cytotoxic effect of chemotherapy, a decrease in cellular glycolysis is observed before tumor shrinkage. Therefore, standardized uptake value (SUVmax), which is a semi-quantitative parameter, is used to show the metabolic activity change more accurately.
In this study, the role of baseline and post-treatment SUVmax values and SUVmax change in predicting pathological response in patients with breast cancer after NAC was investigated.
Materials and Methods
Patients
Thirty patients with newly diagnosed, non-inflammatory, non-metastatic, invasive breast cancer were included in this retrospective study. In all patients, the diagnosis of invasive breast cancer was made with tru-cut biopsy and NAC treatment was given. F-18 FDG PET/CT examinations were performed on the patients before and after NAC. F-18 FDG PET/CT examination after NAC was performed at least 15 days after the end of the treatment. All patients underwent mastectomy/breast-conserving surgery 4-6 weeks after post-treatment F-18 FDG PET/CT. Exclusion criteria of the patients in the study were: patients who were diagnosed with inflammatory breast cancer; whose F-18 FDG PET/CT examination was contraindicated (for example with pregnancy or high blood sugar); who had a chronic disease; and who had previously received surgery or radiotherapy as treatment were excluded from the study.
Different NAC regimens were administered to the patients as follows: Six patients received cyclophosphamide and doxorubicin; 17 patients received cyclophosphamide and adriamycin; three patients received cyclophosphamide, doxorubicin and docetaxel; one patient received pertuzumab, herceptin and docetaxel; one patient received herceptin, paclitaxel and carboplatin; and two patients received herceptin and paclitaxel. The patients were administered 4-6 cycles of NAC.
This study was approved by the Faculty Ethics Committee of Pamukkale University (60116787-020/71416).
F-18 FDG PET/CT Imaging
After fasting and resting for six hours, the patients received 259–407 MBq (7–11 mCi) of F-18 FDG intravenously when their fasting bloodglucose level was <200 mg/dL. The patients were examined using a dedicated PET/CT scanner (Gemini TF TOF PET-CT; Philips, Cleveland, OH, USA). Emission scans were acquired from the calvaria base to the middle of the thigh for 1.5 minutes per position without intravenous contrast medium injection. Transmission images were obtained by low-dose CT (50–120 mA s, 90–140 kVp, 16 sections of 5 mm thickness).
Attenuation correction was performed for PET images using CT findings and the ordered subsets-expectation maximization (OSEM) algorithm (33 subsets, 3 iterations). PET images were reconstructed by the iterative method. Transverse, sagittal and coronal sections (5 mm thickness) were created from PET/CT fusion images and evaluated using Philips Fusion Viewer software (ver.2.1; Philips Healthcare, Best, The Netherlands).
In this study, patients underwent two F-18 FDG PET/CT scans; basal scan for staging before NAC and post-treatment scan for response to treatment after NAC. Both examinations were performed on the patients under the same conditions and the same acquisition parameters.
Image Analysis
F-18 FDG PET/CT images were evaluated by two nuclear medicine physicians and consensus was reached in all patients. The isocontour method was used to create volume of interest (VOI) around the tumor. A 40% SUVmax threshold was used for the isocontour. SUVmax was defined as the maximum SUV from a single voxel anywhere within the VOI. Tumor size was obtained by carefully measuring the longest diameter of the tumor from PET/CT images.
Metabolic response assessment with F-18 FDG PET/CT was performed by looking at the relative change in tumoral F-18 FDG uptake before and after treatment, and the following formula was used:
ΔSUVmax=100 x (post-treatment SUVmax – baseline SUVmax)/baseline SUVmax
Pathological Evaluation
Pathological responses of primary tumors were evaluated by the pathologist according to the Miller and Payne grading system (10). Breast tumor pathology preparations were re-evaluated for the evaluation of tumor response according to Miller and Payne classification. This was divided into five grades based on the comparison of tumor cellularity between the pre-neoadjuvant core biopsy and the post-surgical sample. The Miller and Payne grading system rates the postoperative curative effect from levels 1 to 5 according to the reduction in tumor cells.
The grades were determined as follows:
Grade 1 (G1): No or some change in individual malignant cells, but no reduction in overall cellularity;
Grade 2 (G2): Minimal tumor cell loss (up to 30% loss), but overall cellularity still high;
Grade 3 (G3): 30% to 90% reduction in tumor cells;
Grade 4 (G4): Marked disappearance of tumor cells, leaving only small clumps or widely scattered individual cells; more than 90% loss of tumor cells;
Grade 5 (G5): No identifiable malignant cells in sections from tumor site, only vascular fibroelastotic stroma remaining, usually containing macrophages. Ductal carcinoma in situ (DCIS) may be present (11).
G1, G2 and G3 were included in the nonresponder group (nonpCR), and G4 and G5 were included in the responder group (pCR).
Statistical Analysis
Data were analyzed with SPSS, version 25.0 (IBM Inc., Armonk, NY, USA). Continuous variables were expressed as mean ± standard deviation, median (minimum-maximum values), and categorical variables as number and percentage. The compatibility of the data with the normal distribution was examined by the Kolmogorov-Smirnov test, and the homogeneity was examined by the Levene's test. Student’s t-test was used to compare independent group differences with normal distribution. The Mann-Whitney U test was used to compare the independent group differences that did not fit the normal distribution. A logistic regression model was created using ΔSUVmax and SUVmax II parameters, which were found to be independent statistically significant, to predict response to treatment.
A receiver-operating characteristics (ROC) analysis was performed, and cut-off values of the quantitative parameters of F-18 FDG PET/CT were obtained to evaluate the response to treatment. Sensitivity and specificity were calculated at 95% CI to measure the validity. In all analyses, p<0.05 was considered statistically significant.
Results
The mean age of the 30 patients included in the study was 51.2±11.98 (28–75) years. According to their pathological response scores, the patients were distributed as follows: One patient (3.3%) was G1, four patients (13.3%) G2, 8 patients (26.7%) G3, nine patients (30%) G4, and eight patients (26.7%) G5. Thus, for study purposes, 13 patients (43.3%) were nonresponders and 17 patients (56.7%) were responders. Ten (33.3%) of the patients were premenopausal and 20 (66.7%) were postmenopausal. Patient characteristics are listed in Table 1.
Table 1. Patient and tumor characteristics.
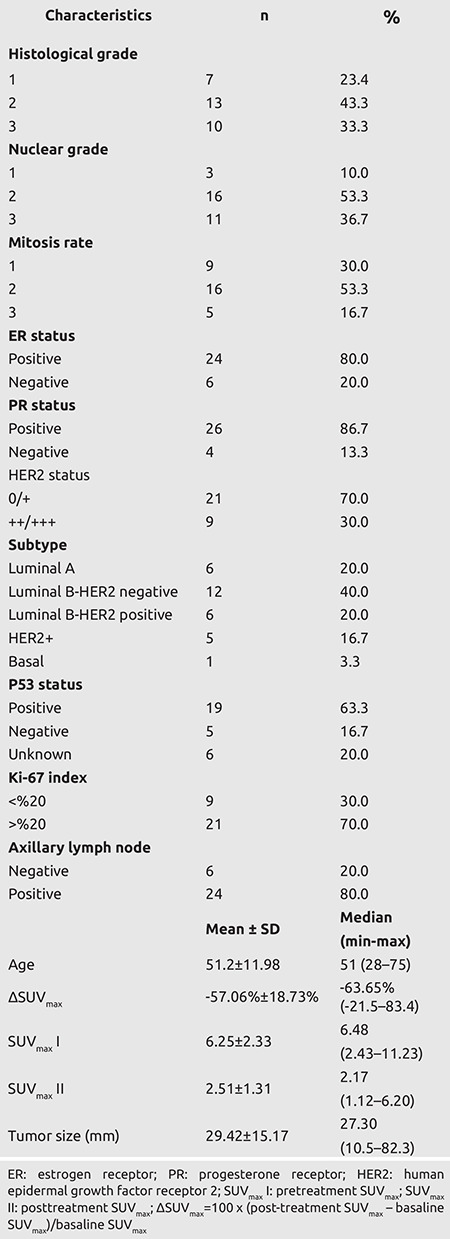
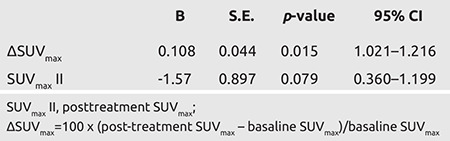
ΔSUVmax was statistically significantly higher in the responders group compared to the nonresponders group, while SUVmax II was lower (p = 0.001 and p = 0.004, respectively). There was no statistically significant difference between the responders and nonresponders groups in terms of age, tumor diameter, and SUVmax I values (Table 2).
Table 2. Relationship between primary tumor characteristics and response to treatment.
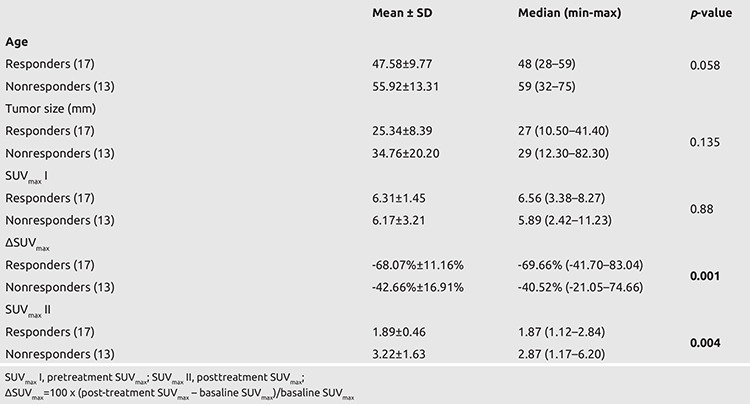
With multivariate logistic regression analysis, ΔSUVmax was found to be the only independent predictive factor for pCR (Table 3).
Table 3. Logistic regression.
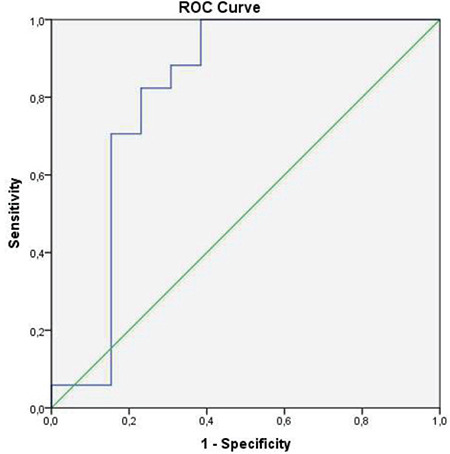
In the ROC curve analysis performed to determine the cut-off values of PET/CT parameters in the differentiation of pCR and non-pCR after neoadjuvant chemotherapy, the cut-off value for ΔSUVmax was found to be -59.69%, and the sensitivity and specificity values for this value were 82% and 85%, respectively [area under the ROC curve (AUC): 0.878, p = 0.001, 95% confidence interval (CI) (0.74–1); see Figure 1], while the cut-off value for SUVmax II was found to be 2.14, and the sensitivity and specificity values for this value were 70% and 85%, respectively [AUC: 0.810, p = 0.004, 95% CI (0.62-0.99); see Figure 2].
Figure 1.
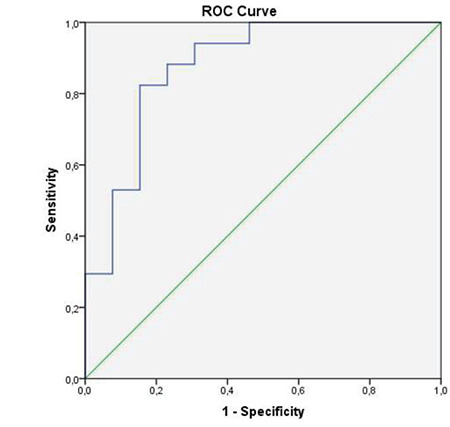
Receiver operating characteristic (ROC) curve for the prediction of pathological complete response (pCR) using ΔSUVmax in F-18 FDG PET/CT [Area under ROC curve (AUC)=0.878]
FDG: fluorodeoxyglucose; PET: positron emission tomography; CT: computerized tomography
Figure 2.
Receiver operating characteristic (ROC) curve for the prediction of pathological complete response (pCR) using posttreatment SUVmax (SUVmax II) in F-18 FDG PET/CT [Area under ROC curve (AUC)=0.810]
FDG: fluorodeoxyglucose; PET: positron emission tomography; CT: computerized tomography
Discussion and Conclusion
While NAC allows breast-conserving surgery by reducing tumor size in breast cancer, it also makes a significant contribution to survival. It has been reported that patients with pCR after NAC had better disease-free survival and overall survival rates than patients whose response was evaluated by other methods (4). For this reason, in the present study, pCR was chosen as the reference standard for evaluating tumor response after NAC. In the present study, patients in the G4 and G5 groups were included in the pCR group according to the Miller and Payne classification system. In the literature, no difference was found in terms of prognosis between minimal residual disease and complete response (12), and in previous studies, pCR (G4, G5) and non-pCR (G1, G2, G3) groups were formed in this way (13, 14). In the present study, the pCR rate was 56.7%. In different studies, response rates after NAC have been reported to vary between 16.3% and 55.6% (15, 16, 17). This variation was thought to be due to the use of different pathological assessment and scoring methods.
In the present study, ΔSUVmax was found to be a highly effective parameter for predicting pCR after NAC in breast cancer patients. The cut-off value for ΔSUVmax was found to be -59.69%, and the sensitivity and specificity values for this value were 82% and 85%, respectively (Figures 3 and 4). In a meta-analysis evaluating 19 studies, to predict histopathological response in primary breast lesions by PET, the pooled sensitivity and specificity were 84% (95% CI, 78–88%) and 66% (95% CI, 62–70%), respectively (18). Our specificity value was found to be higher than the specificity value determined in the meta-analysis. Studies in the meta-analysis used very different NAC regimens, and the timing of the F-18 FDG PET/CT scan was different from each other. In our study, PET/CT examination times were the same, and the same device and the same examination protocol were used. In the 43-patient study of García-Esquinas et al. (9), the sensitivity and specificity were found to be 90.9% and 90.6% when the ΔSUVmax cut-off was taken at -90.4%. In that study, the same NAC regimen was used in each patient, unlike ours, and the high ΔSUVmax cut-off value may have increased the sensitivity and specificity. This may explain the higher sensitivity and specificity than we found. The values obtained for ΔSUVmax in several studies in the literature were similar to or lower than our results (5, 8, 19, 20, 21). In the study of Berrido-Rieninger et al. (20), specificity was found to be 86% when ΔSUVmax was -60% (20). This finding is consistent with our result. In the 50-patient study of Park et al. (22), the sensitivity was 100% while the specificity was 62%. About half of the primary tumors in this study were <1 cm. In our study, the primary tumor size was greater than 1 cm in all patients. The low specificity can be attributed to the small tumor size. In another study, sensitivity was 82.3% and specificity 82.4% when ΔSUVmax was -87.9% (5). Although the ΔSUVmax cut-off value of this study was higher than ours, we obtained similar sensitivity and specificity values.
Figure 3.
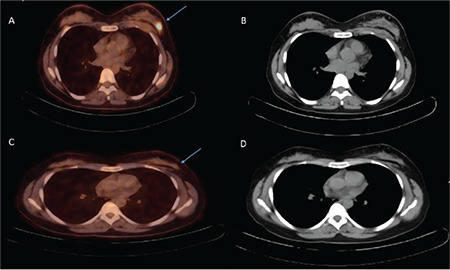
Forty-six years old woman. Left breast localized invasive ductal carcinoma (primary tumor axial diameter 14.6 mm, primary tumor SUVmax: 8.02) is seen in pretreatment CT and fusion PET/ CT transaxial images (blue arrow) (A, B). There is a significant decrease in F-18 FDG uptake (SUVmax:1.36; ΔSUVmax:-83.04%) in posttreatment CT and fusion PET/CT transaxial images (blue arrow) after four cycles of cyclophosphamide/adriamycin chemotherapy (C, D). Histopathological features of the primary tumor: histological grade 3, nuclear grade 3, mitosis rate 2, ER and PR negative, HER2 +3 positive, K-67 40%, p53 positive, and subtype HER2 positive. Miller and Payne grading system pathological score 4
FDG: fluorodeoxyglucose; PET: positron emission tomography; CT: computerized tomography; SUV: standardized uptake value; HER2: human epidermal growth factor receptor 2; ER: estrogen receptor; PR: progesterone receptor
Figure 4.
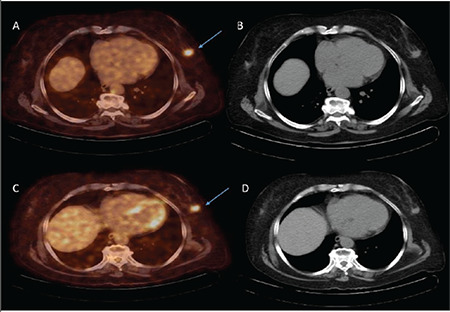
Seventy-eight years old woman. Left breast localized invasive ductal carcinoma (primary tumor axial diameter 18.7 mm, primary tumor SUVmax:6.55) is seen in pretreatment CT and fusion PET/CT transaxial images (blue arrow) (A, B). There is a slight decrease in F-18 FDG uptake (SUVmax:4.51; ΔSUVmax:-44.25%) in posttreatment CT and fusion PET/CT transaxial images (blue arrow) after four cycles of cyclophosphamide/adriamycin chemotherapy (C, D). Histopathological features of the primary tumor: histological grade 2, nuclear grade 2, mitosis rate 2, ER 90% positive, PR 90% positive, HER2 negative, Ki-67 30%, p53 positive, and subtype luminal B/HER2 negative. Miller and Payne grading system pathological score 3
FDG: fluorodeoxyglucose; PET: positron emission tomography; CT: computerized tomography; SUV: standardized uptake value; HER2: human epidermal growth factor receptor 2; ER: estrogen receptor; PR: progesterone receptor
SUVmax was used as a semi-quantitative parameter in most of the studies on the value of F-18 FDG PET/CT in response assessment after NAC. In the study of Berriolo-Riedinger et al. (20), except SUVmax, SUV parameters corrected for total body weight, body surface area and blood glucose were used (8). However, no significant difference was found between SUV parameters in estimating pCR. Therefore, in our study, we used SUVmax parameters (SUVmax I, SUVmax II and ΔSUVmax) in accordance with the literature.
In the present study, we evaluated the potential of pretreatment SUVmax (SUVmax I) and post-treatment SUVmax (SUVmax II) to predict pCR, as well as ΔSUVmax. The cut-off value for SUVmax II was found to be 2.14, and the sensitivity and specificity values for this value were 70% and 85%, respectively. In the literature, there are few studies evaluating the efficacy of post-treatment SUVmax in predicting the response to treatment after NAC in breast cancer. In the study of Yıldırım et al. (21), consisting of 51 patients, no significant difference was observed between pCR and nonpCR in terms of pretreatment SUVmax, but a significant difference was found between post-treatment SUVmax values. Our findings are consistent with this study. In the present study, it was revealed that, like ΔSUVmax, the value of post-treatment SUVmax was an effective parameter in predicting the response to treatment after NAC in breast cancer. However, this finding needs to be supported by new studies. There are different results in the literature regarding the value of pretreatment SUVmax in predicting the response to treatment after NAC in breast cancer. In some studies, basal SUVmax was found to be higher in the pCR group (23, 24, 25), while in some studies, higher SUVmax values were found in unresponsive patients (26, 27). In addition, and in contrast to these studies, there are also publications that argue that there is no difference in basal SUVmax between pCR and nonpCR (15, 20, 28). Therefore, the findings in the literature suggest that there is no consensus regarding the value of pretreatment SUVmax in predicting the response to treatment after NAC.
The present study has some limitations. It was designed retrospectively and the number of patients was low. Due to the low number of patients, subgroup-related to prognostic factors (receptor status, grade, subtype, Ki-67 ratio, etc.) of breast cancer could not be formed and their relationship with PET parameters could not be evaluated. Different NAC regimens were administered to the patients and the relationship between the different NAC regimens could not be evaluated due to the small number of patients.
F-18 FDG PET/CT was an effective method in predicting the response to treatment after NAC in breast cancer. ΔSUVmax and post-treatment SUVmax values correlate with pathological evaluation in predicting pCR. We did not find that pretreatment SUVmax was effective in predicting response to treatment.
Footnotes
Ethics Committee Approval: This study was approved by the Faculty Ethics Committee of our institution (60116787-020/71416) (Pamukkale University Non-Invasive Clinical Research Ethics Committee).
Informed Consent: Retrospective study.
Peer-review: Externally peer-reviewed.
Authorship Contributions
Surgical and Medical Practices: Y.A.K., A.G., S.Y., E.E., B.Y.T.; Concept: T.S.; Design: T.S., B.Y.T.; Data Collection or Processing: Y.A.K., A.G., B.Y.T., O.Y.; Analysis or Interpretation: T.S., A.G., D.Y.; Literature Search: T.S., S.Y., E.E., D.Y.; Writing: T.S.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study received no financial support.
References
- 1.Taghipour M, Wray R, Sheikhbahaei S, Wright JL, Subramaniam RM. FDG avidity and tumor burden: survival outcomes for patients with recurrent breast cancer. AJR Am J Roentgenol. 2016;4:846–855. doi: 10.2214/AJR.15.15106. [DOI] [PubMed] [Google Scholar]
- 2.Honkoop AH, van Diest PJ, de Jong JS, Linn SC, Giaccone G, Hoekman K, et al. Prognostic role of clinical, pathological and biological characteristics in patients with locally advanced breast cancer. Br J Cancer. 1998;77:621–626. doi: 10.1038/bjc.1998.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Esserman LJ, Berry DA, DeMichele A, Carey L, Davis SE, Buxton M, et al. Pathologic complete response predicts recurrence-free survival more effectively by cancer subset: results from the I-SPY 1 TRIAL–CALGB 150007/150012, ACRIN 6657. J Clin Oncol. 2012;30:3242–3249. doi: 10.1200/JCO.2011.39.2779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–172. doi: 10.1016/S0140-6736(13)62422-8. [DOI] [PubMed] [Google Scholar]
- 5.Akdeniz N, Kömek H, Küçüköner M, Kaplan MA, Urakçı Z, Oruç Z, et al. The role of basal 18F-FDG PET/CT maximum standard uptake value and maximum standard uptake change in predicting pathological response in breast cancer patients receiving neoadjuvant chemotherapy. Nucl Med Commun. 2021;42:315–324. doi: 10.1097/MNM.0000000000001332. [DOI] [PubMed] [Google Scholar]
- 6.Vicente AMG, Mora MAC, Martín AAL, Sánchez MMM, Calatayud FR, López OVG, et al. Glycolytic activity with 18F-FDG PET/CT predicts final neoadjuvant chemotherapy response in breast cancer. Tumor Biol. 2014;35:11613–11620. doi: 10.1007/s13277-014-2495-7. [DOI] [PubMed] [Google Scholar]
- 7.Sarhan EAS, El Gohary MI, El Moneim LA, Ali SA. Role of 18 fluorine-fluorodeoxyglucose positron emission tomography/computed tomography in assessment of neoadjuvant chemotherapy response in breast cancer patients. Egypt J Radiol Nucl Med. 2020;51:116. [Google Scholar]
- 8.Erdi YE, Macapinlac H, Rosenzweig KE, Humm JL, Larson SM, Erdi AK, et al. Use of PET to monitor the response of lung cancer to radiation treatment. Eur J Nucl Med. 2000;27:861–866. doi: 10.1007/s002590000258. [DOI] [PubMed] [Google Scholar]
- 9.García-Esquinas MAG, García JA, García-Sáenz JA, Furió-Bacete V, Ferrer MEF, Candil AO, et al. Predictive value of PET-CT for pathological response in stages II and III breast cancer patients following neoadjuvant chemotherapy with docetaxel. Rev Esp Med Nucl Imagen Mol. 2014;33:14–21. doi: 10.1016/j.remn.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 10.Song D, Man X, Jin M, Li Q, Wang H, Du Y. A Decision-Making Supporting Prediction Method for Breast Cancer Neoadjuvant Chemotherapy. Front Oncol. 2021;10:592556. doi: 10.3389/fonc.2020.592556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ying M, He Y, Qi M, Dong B, Lu A, Li J, et al. Value of pre-treatment biomarkers in prediction of response to neoadjuvant endocrine therapy for hormone receptor-positive postmenopausal breast cancer. Chin J Cancer Res. 2013;25:397–404. doi: 10.3978/j.issn.1000-9604.2013.08.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ueda S, Tsuda H, Asakawa H, Shigekawa T, Fukatsu K, Kondo N, et al. Clinicopathological and prognostic relevance of uptake level using 18F-fluorodeoxyglucose positron emission tomography/computed tomography fusion imaging (18F-FDG PET/CT) in primary breast cancer. Jpn J Clin Oncol. 2008;38:250–258. doi: 10.1093/jjco/hyn019. [DOI] [PubMed] [Google Scholar]
- 13.Duch J, Fuster D, Muñoz M, Fernández PL, Paredes P, Fontanillas M, et al. 18F-FDG PET/CT for early prediction of response to neoadjuvant chemotherapy in breast cancer. Eur J Nucl Med Mol Imaging. 2009;36:1551–1557. doi: 10.1007/s00259-009-1116-y. [DOI] [PubMed] [Google Scholar]
- 14.Kiyoto S, Sugawara Y, Hosokawa K, Nishimura R, Yamashita N, Ohsumi S, et al. Predictive ability of 18F-fluorodeoxyglucose positron emission tomography/computed tomography for pathological complete response and prognosis after neoadjuvant chemotherapy in triple-negative breast cancer patients. Asia Ocean J Nucl Med Biol. 2016;4:3–11. doi: 10.7508/aojnmb.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koolen BB, Pengel KE, Wesseling J, Vogel WV, Peeters MJV, Vincent AD, et al. FDG PET/CT during neoadjuvant chemotherapy may predict response in ER-positive/HER2-negative and triple negative, but not in HER2-positive breast cancer. Breast. 2013;22:691–697. doi: 10.1016/j.breast.2012.12.020. [DOI] [PubMed] [Google Scholar]
- 16.Zucchini G, Quercia S, Zamagni C, Santini D, Taffurelli M, Fanti S, et al. Potential utility of early metabolic response by 18F-2- fluoro-2-deoxy-D-glucose-positron emission tomography/computed tomography in a selected group of breast cancer patients receiving preoperative chemotherapy. Eur J Cancer. 2013;49:1539–1545. doi: 10.1016/j.ejca.2012.12.024. [DOI] [PubMed] [Google Scholar]
- 17.Rousseau C, Devillers A, Sagan C, Ferrer L, Bridji B, Campion L, et al. Monitoring of early response to neoadjuvant chemotherapy in stage II and III breast cancer by [18F]fluorodeoxyglucose positron emission tomography. J Clin Oncol. 2006;24:5366–5372. doi: 10.1200/JCO.2006.05.7406. [DOI] [PubMed] [Google Scholar]
- 18.Wang Y, Zhang C, Liu J, Huang G. Is 18F-FDG PET accurate to predict neoadjuvant therapy response in breast cancer? A meta-analysis. Breast Cancer Res Treat. 2012;131:357–369. doi: 10.1007/s10549-011-1780-z. [DOI] [PubMed] [Google Scholar]
- 19.Jung S-Y, Kim S-K, Nam B-H, Min SY, Lee SJ, Park C, et al. Prognostic impact of [18F] FDG-PET in operable breast cancer treated with neoadjuvant chemotherapy. Ann Surg Oncol. 2009;17:247–253. doi: 10.1245/s10434-009-0710-3. [DOI] [PubMed] [Google Scholar]
- 20.Berriolo-Riedinger A, Touzery C, Riedinger J-M, Toubeau M, Coudert B, Arnould L, et al. [18F]FDG-PET predicts complete pathological response of breast cancer to neoadjuvant chemotherapy. Eur J Nucl Med Mol Imaging. 2007;34:1915–1924. doi: 10.1007/s00259-007-0459-5. [DOI] [PubMed] [Google Scholar]
- 21.Yildirim N, Simsek M, Aldemin MN, Bilici M, Tekin SB. The relationship between 18-FDG-PET/CT and clinicopathologic features, pathologic response in patients with locally advanced breast cancer. Eurasian J Med. 2019;51:154–159. doi: 10.5152/eurasianjmed.2018.18036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park JS, Moon WK, Lyou CY, Cho N, Kang KW, Chung J-K. The assessment of breast cancer response to neoadjuvant chemotherapy: comparison of magnetic resonance imaging and 18F-fluorodeoxyglucose positron emission tomography. Acta Radiol. 2011;52:21–28. doi: 10.1258/ar.2010.100142. [DOI] [PubMed] [Google Scholar]
- 23.Schwarz-Dose J, Untch M, Tiling R, Sassen S, Mahner S, Kahlert S, et al. Monitoring primary systemic therapy of large and locally advanced breast cancer by using sequential positron emission tomography imaging with [18F]fluorodeoxyglucose. J Clin Oncol. 2009;27:535–541. doi: 10.1200/JCO.2008.17.2650. [DOI] [PubMed] [Google Scholar]
- 24.Buchbender C, Kuemmel S, Hoffmann O, Stahl AR, Kimming R, Otterbach F, et al. FDG-PET/CT for the early prediction of histopathological complete response to neoadjuvant chemotherapy in breast cancer patients: initial results. Acta Radiol. 2012;53:628–636. doi: 10.1258/ar.2012.110699. [DOI] [PubMed] [Google Scholar]
- 25.Ueda S, Saeki T, Shigekawa T, Omata J, Moriya T, Yamamoto J, et al. 18F-Fluorodeoxyglucose positron emission tomography optimizes neoadjuvant chemotherapy for primary breast cancer to achieve pathological complete response. Int J Clin Oncol. 2012;17:276–282. doi: 10.1007/s10147-011-0287-2. [DOI] [PubMed] [Google Scholar]
- 26.Mankoff DA, Dunnwald LK, Gralow JR, Ellis GK, Charlop A, Lawton TJ, et al. Blood flow and metabolism in locally advanced breast cancer: relationship to response to therapy. J Nucl Med. 2002;43:500–509. [PubMed] [Google Scholar]
- 27.Mankoff DA, Dunnwald LK, Gralow JR, Ellis GK, Schubert EK, Tseng J, et al. Changes in blood flow and metabolism in locally advanced breast cancer treated with neoadjuvant chemotherapy. J Nucl Med. 2003;44:1806–1814. [PubMed] [Google Scholar]
- 28.Kolesnikov-Gauthier H, Vanlemmens L, Baranzelli M-C, Vennin P, Servent V, Fournier C, et al. Predictive value of neoadjuvant chemotherapy failure in breast cancer using FDG-PET after the first course. Breast Cancer Res Treat. 2012;131:517–525. doi: 10.1007/s10549-011-1832-4. [DOI] [PubMed] [Google Scholar]


