ABSTRACT
Background:
Mothers who attend antenatal care (ANC) late miss the opportunity to receive health information, early interventions, and timely referrals, which leads to problems complicating pregnancy and contributes to maternal mortality.
Objective:
This study was conducted to assess early initiation of ANC visit and its associated factors in public health facilities at Ambo town administration, Oromiya regional state, Central Ethiopia, 2018.
Methods:
A total sample of 344 pregnant women who attended their first natal care visit were chosen using a systematic random selection procedure for facility-based cross-sectional research. Data were entered into EpiData Version 3.1. “The EpiData Association” Odense, Denmark (In Danish: EpiData foreningen) and analyzed using IBM SPSS Version 21 - International Business Machines Corporation, (Armonk, New York). Descriptive statistics were applied to describe the magnitude of the variable, and binary and multivariable logistic regression analyses were employed to identify factors associated with the early initiation of ANC visits. Statistically significant association was declared at a 95% confidence interval and P value (<0.05).
Results:
The study revealed that only 30.5% of the study respondents started their first ANC timely. Initiation of early ANC booking was affected by factors like having good knowledge of ANC follow-up (Adjusted odd ratio (AOR) = 2.25, 95% CI: 1.06, 4.78), primigravida (AOR = 2.52, 95% CI: 1.20,5.32), planned pregnancy (AOR = 2.86, 95% CI: 1.05, 7.81), partners whose occupation were merchant (AOR = 3.47, 95% CI: 1.15, 10.46), know the available service on ANC service (AOR = 3.00, 95% CI: 1.31, 6.88), and having advice from health professionals (AOR = 2.27, 95% CI: 1.05, 4.89); all these factors had shown significant association with timing of first ANC.
Conclusion:
Early initiation of first ANC was relatively low in the study area. Planned pregnancy, number of pregnancies, knowledge of ANC follow-up, partner’s occupation, knowing the available service on ANC service, and having advice from health professionals were factors associated with it. To improve the situation, it is important to provide continuous public health education on the importance of early initiation of ANC at public health facilities.
Keywords: Associated factor, Central Ethiopia, early initiation of antenatal care, pregnant mother
Background
Antenatal care (ANC) is the care provided by skilled healthcare professionals to pregnant women and adolescent girls to ensure the best health conditions for both mother and baby during pregnancy.[1] When ANC is started early in the pregnancy and continues through delivery, it is more effective in reducing negative pregnancy outcomes. Early pregnancy issue detection results in more timely referrals for women with difficulties or high-risk groups.[2,3,4]
The potential to acquire health information and interventions, such as early identification of human immunodeficiency virus (HIV), sexually transmitted infections (STIs), tuberculosis (TB), anemia, malaria prophylaxis, and prevention or treatment of complications, is lost by mothers who attend ANC late than necessary.[2,5,6]
Every pregnant woman is at risk of pregnancy complications, according to the new World Health Organization (WHO) ANC model, which urges early ANC visits, the first of which should occur before the first trimester. During the appointment, pregnant women are divided into two groups according to their current pregnancy status, prior pregnancies, and general medical concerns. About 75% of pregnant women are classified as being eligible for regular prenatal care (the basic component), and 25% of pregnant women who start ANC have particular medical issues or risk factors that need extra attention. WHO advises expecting women, especially those in poor nations, to begin scheduling ANC in the first four months of pregnancy.[7,8] According to the Ethiopian Ministry of Health, pregnant women who began ANC follow-up early (before 16 weeks of pregnancy) had a potential for early diagnosis of issues that might impact the outcome of the pregnancy.[9]
WHO estimates that every year approximately 8 million women suffer pregnancy-related complications and around half a million die as a result.[5] From the total maternal death, developing countries count for 99% of the global deaths, the majority of which are in sub-Saharan Africa including Ethiopia.[10] Although maternal mortality has been declining in wealthy nations since the 1990s, it has remained steady or even increased in developing nations, indicating that attempts to address this issue are either insufficient or improperly carried out.[11] In sub-Saharan African countries, the leading causes of maternal death were obstetric hemorrhage, hypertensive disorders in pregnancy, and pregnancy-related infections which account for 28.8%, 22.1%, and 11.5%, respectively, that could be identified and entertained during ANC.[12] Moreover, the complications in pregnancy, childbirth, or the postpartum period develop because of pregnant status, and some pregnancy aggravated diseases such as malaria, anemia, and heart disease which account for 20% of indirect causes of maternal death.[13] In Ethiopia, the mini ethiopian demographic and health survey (EDHS) 2019 identified that three-fourths of the mother received ANC for their recent pregnancy.[14] However, the maternal mortality ratio was 412 per 100,000 live births.[10]
In the world from 2007 to 2014, just 64% of pregnant women obtained the required minimum of four ANC visits or more, compared to 83% who did so.[13] One of the many likely causes for the maternal death rate decreasing by 47% between 1990 and 2010 was the increase in ANC provided by trained healthcare professionals from 64% to 81%.[15]
The usage of ANC among young women in sub-Saharan African nations was 55%, with regional differences.[16] Most women wait for ANC until the second or even the third trimester before making the first visit. Out of 91% of women who make at least one ANC visit, 43% of them wait until the third trimester to start ANC.[17] Most pregnant women in sub-Saharan Africa make their first ANC visits very late ranging from 54% in South Africa[16] to 81% in Zambia.[18]
Ethiopian demographic and health survey results showed that 37% of both urban and rural women did not receive ANC service during their last pregnancy and 48.6% of women had no ANC service in the Oromiya region. About 9.7% of urban pregnant women did not receive ANC services and only 44.1% of them had ANC services before four months of gestation.[10] Surveys and research in Ethiopia also show that about 79.6% of pregnant women nationally,[10] 42% of pregnant women in Addis Ababa,[19] 59% in Tigray central zone,[20] 82.6% in Arba Minch,[21] and 64.6% in Dilla town[22] initiate their first ANC visits late.
Early initiation of first ANC has been associated with place of residence, educational status, maternal age, occupation, average household income, information received on accurate time, previous birth experiences, not living with a husband/partner, previous early ANC visit, unplanned pregnancy, late recognition of pregnancy, and decision making ability.[19,22,23,24]
There were limited studies on the timing of first ANC booking in Ethiopia. Thus, this study aims to find out the prevalence of early initiation of focused ANC based on Ethiopian implementation guidelines and factors associated with early booking in Ambo town administration, Oromiya region, Ethiopia.
Conceptual framework
After I reviewed different literatures on factors that are related to early initiation of first antenatal care attendance, I have adapted the following conceptual framework [Figure 1].
Figure 1.
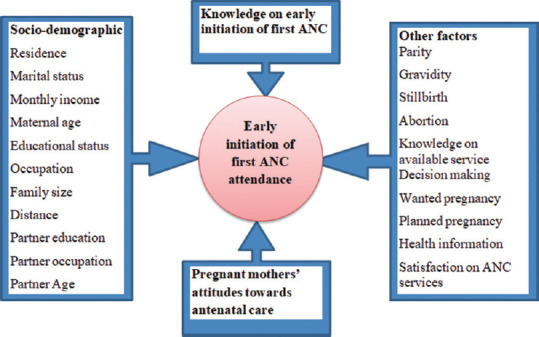
Conceptual framework for early initiation of first ANC and its associated factors among pregnant women attending public health facilities in Ambo town, Western Ethiopia, 2018
Methods
The study was conducted from August to September 2018 in Ambo town administration, Oromiya Regional State with an estimated total population of 83,053.[25] Ambo town administration has two public hospitals (one referral and one general), two health centers, 27 private clinics, one NGO clinic, and three public rural health posts. The study was conducted on public health facilities those supposed to implement ANC services according to the Ethiopian basic national guidelines.[9,26]
Study design, population and sample size
Institutional based crosssectional study design was applied on a total of 345 pregnant women attending antenatal care. Sample was determined using a single population proportion formula with the assumption of 5% of marginal error and 95% confidence interval (α = 0.05) and prevalence of pregnant mothers who came before 16 weeks of gestation 35.4%[22] and by adding 10% of nonresponse rate. Systematic random sampling was applied to recruit the study subjects. Since the study was assumed to be conducted for two months’ duration, the average of last year two months’ report was taken as a sampling frame, and skip interval (K) was calculated by dividing the two months’ load of clients presented for the first ANC booking for the sample size which was 714/345 ≈ 2. The first client to be exit interviewed was selected randomly.
Data collection tool and techniques
Data were collected using a structured questionnaire through the exit interviewer administered method. The questionnaire was developed by reviewing different related literatures.[3,10,19,27] The questionnaire was developed in English and later translated into Afan Oromo and retranslated back to English to ensure consistency.
Data quality control and management
Training was given to data collectors and supervisors for one day on the aim of the study, data collection tool, the confidentiality of information, participant’s rights, informed consent, and techniques of the interview to control data quality. A pretest was done on 5% of the sample size outside of the study area on mothers who come for their first ANC service. The collected data were checked for completeness on daily basis and took corrective measures accordingly by the principal investigator and supervisor.
Data analysis
The collected data were checked for their completeness, entered into EpiData Version 3.1. “The EpiData Association” Odense, Denmark (In Danish: EpiData foreningen), and exported to IBM SPSS Version 21 - International Business Machines Corporation, (Armonk, New York) statistical software for analysis. First univariate analysis was done to explore frequency distribution, central tendency, and variability (dispersion) of the overall distribution of the independent variables. Binary logistic regression was used to determine the association between explanatory variables and early initiation of ANC. Explanatory variables with P values <0.25 were identified through bivariable logistic regression and entered into a multivariable binary logistic regression model to control the confounding effect and to determine independent predictors of first ANC timing. A P value of less than 0.05 was considered as the cutoff point for statistical significance in the final model.
Ethical consideration
Ethical clearance and official letter were obtained from Ambo University, Medicine and Health Sciences College Research and Ethical Review Committee with Ref. No. of: CMHS-ERC: 101/2018 and project number: CMHS: 018/18. Ambo town administrative health office had written a formal letter to public health facilities based on letters from Ambo University Medicine and Health Sciences College. Study participants were informed about the purpose and objective of the study. They were also told that they had every right to discontinue or refuse to participate. Privacy of the participant was maintained by using a separate and quiet environment, and for the confidentiality of the information, the questionnaire did not contain the name of the study participants. For a pregnant woman who was verbally consented to participate in the study, the interview was conducted by pretested interviewer-administered questionnaire.
Results
Socio-demographic characteristics of respondents
A total of 344 pregnant mothers participated in the study giving a response rate of 99.7%. The majority (84.0%) of participants were urban residents. The ethnic composition of study participants showed that 95.9% of them were Oromo. Regarding the age of the respondents, the majority (68%) of respondents aged between 20 and 34 years with a mean age of 24.28 (SD ± 4.25). Three hundred thirty-two (95.9%) of respondents were in marriage and 184 (53.5%) of mothers were housewives by occupation. The two dominant religions of the respondents were Protestant (65.7%) and Orthodox (30.8%). Regarding the educational status of the respondents, a majority (85.5%) of them attended formal education. More than half (53.5%) of respondents had an average monthly family income of above 2001 ETB [Table 1].
Table 1.
Socio-demographic characteristics of pregnant women attending first antenatal care at public health facilities in Ambo town administration, August to September 2018
| Socio-demographic variables | Frequency | Early (before 16 wks)# (%) | Late (at or after 16 weeks)# (%) |
|---|---|---|---|
| Residence | |||
| Urban | 289 | 89 (30.8) | 200 (69.2) |
| Rural | 55 | 16 (29.1) | 39 (70.9) |
| Ethnicity | |||
| Oromo | 330 | 96 (29.1) | 234 (70.9) |
| Others+ | 14 | 9 (64.3) | 5 (35.7) |
| Religion of respondents | |||
| Protestant | 226 | 69 (30.5) | 157 (69.5) |
| Orthodox | 101 | 30 (29.7) | 71 (70.3) |
| Others++ | 17 | 6 (35.3) | 11 (64.7) |
| Age of respondents | |||
| <20 | 93 | 28 (30.1) | 65 (69.9) |
| 20-34 | 234 | 68 (29.1) | 166 (70.9) |
| >=35 | 17 | 9 (52.9) | 8 (47.1) |
| Age of partner | |||
| <20 | 13 | 5 (38.5) | 8 (61.5) |
| (n=332) | |||
| 20-34 | 248 | 83 (33.5) | 165 (66.5) |
| >=35 | 71 | 14 (19.7) | 57 (80.3) |
| Marital status | |||
| In marriage | 330 | 100 (30.3) | 230 (69.7) |
| Out of marriage | 14 | 5 (35.7) | 9 (64.3) |
| Education of respondents | |||
| Has no formal education | 50 | 13 (26) | 37 (74) |
| Primary education | 119 | 39 (32.8) | 80 (67.2) |
| Secondary education | 86 | 23 (26.7) | 63 (73.3) |
| Tertiary education | 89 | 30 (33.7) | 59 (66.3) |
| Partner education | |||
| Has no formal education | 25 | 7 (28) | 18 (72) |
| Primary education | 91 | 24 (26.4) | 67 (73.6) |
| Secondary education | 96 | 30 (31.3) | 66 (68.8) |
| Tertiary education | 118 | 39 (33.1) | 79 (66.9) |
| Occupation of respondents | |||
| Housewife | 184 | 54 (29.3) | 130 (70.1) |
| Government employee | 60 | 19 (31.7) | 41 (68.3) |
| Daily laborer | 34 | 11 (32.4) | 23 (67.6) |
| Merchant | 18 | 9 (50) | 9 (50) |
| Private employed | 37 | 7 (18.9) | 30 (81.1) |
| Others+++ | 11 | 5 (45.5) | 6 (54.5) |
| Average monthly income | |||
| <=500 | 30 | 8 (26.7) | 22 (73.3) |
| 501-1000 | 54 | 18 (33.3) | 36 (66.7) |
| >=1000 | 260 | 79 (30.4) | 181 (69.6) |
Note (+: Amhara, Tigre ++: Muslim, Wakefata, +++: Student, NGO)
Knowledge on the timing of first ANC attendance
Out of the total respondents, 326 (94.8%) of them knew the importance of ANC services for the mother. A majority (96.5%) of respondents reported that ANC services decrease maternal mortality rates. Three hundred thirty-one (96.2%) and 337 (98%) respondents knew that early booking of the first ANC improves pregnancy outcomes for both the fetus and mother.
Concerning knowledge of the appropriate time to begin first ANC, 329 (95.6%) mothers reported that it should be within the first four months (before four months) of pregnancy. Of the total study respondents, 136 (39.5%) mothers reported that all pregnant mothers are at risk of pregnancy complications while 208 (60.5%) reported not being at risk. However, 311 (90.4%) of mothers believed that pregnant women should visit the doctor for ANC service.
Based on mean scores of knowledge, a majority (72.4%) of the pregnant mothers had poor knowledge of ANC follow-up and 27.6% had good knowledge [Table 2].
Table 2.
Knowledge of pregnant women attending first antenatal care at public health facilities in Ambo town administration, August to September 2018
| Variables | Frequency | Early (before 16 weeks) # (%) | Late (at or after 16 weeks) # (%) |
|---|---|---|---|
| ANC service important for a mother’s health | |||
| Yes | 326 | 95 (29.1) | 231 (70.9) |
| No | 18 | 10 (55.6) | 8 (44.4) |
| ANC visits decrease maternal mortality rates | |||
| Yes | 332 | 100 (30.1) | 232 (69.9) |
| No | 12 | 5 (41.7) | 7 (58.3) |
| First ANC check-up be done in the first 4 months | |||
| Yes | 329 | 99 (30.1) | 230 (69.9) |
| No | 15 | 6 (40) | 9 (60) |
| Early ANC visits improve the pregnancy outcome of the fetus | |||
| Yes | 337 | 104 (30.9) | 233 (69.1) |
| No | 7 | 1 (14.3) | 6 (85.7) |
| Early ANC visits improve the pregnancy outcome of the mother | |||
| Yes | 331 | 102 (30.8) | 229 (69.2) |
| No | 13 | 3 (23.1) | 10 (76.9) |
| Pregnant woman see the doctor for ANC if she has pregnancy complication | |||
| Yes | 33 | 14 (42.4) | 19 (57.6) |
| No | 311 | 91 (29.3) | 220 (70.7) |
| All pregnant women are at risk of pregnancy complication | |||
| Yes | 136 | 62 (45.6) | 74 (54.4) |
| No | 208 | 43 (20.7) | 165 (79.3) |
| Knowledge of ANC follow-up | |||
| Poor knowledge | 249 | 63 (25.3) | 186 (74.7) |
| Good knowledge | 95 | 42 (44.2) | 53 (55.8) |
A majority (97.1%) of respondents agreed on early ANC booking is good for their pregnancy and to monitor mothers’ health. Two hundred and eight (60.5%) of pregnant mothers had favorable (positive) and 136 (39.5%) unfavorable (negative) attitudes towards ANC service. Concerning their satisfaction with the service, 180 (52.3%) of them were satisfied whereas 164 (47.7%) of the mothers were unsatisfied with ANC services provided.
Obstetric history and service utilization
One hundred seventy-eight (51.7%) of participants were multigravida and 48.3% were primigravida. Out of 178 multigravida participants, 143 (80.34%) had a history of ANC follow-up from a health facility for their recent birth. One hundred fifty-five (92.3%) were parity one and above, and 73.7% of participants had one to two children. Fifteen women (8.4%) had a history of stillbirth and 35 (15.7%) had a history of abortion. Of the total mothers who gave birth in the previous time, 147 (80.3%) had a history of ANC follow-up [Table 3]. Among 344 respondents who came for ANC booking, 105 (30.5%; 95% CI of 25.63%, 35.41%) of them initiated their first ANC early (before 16 weeks of gestation) [Figure 2]. The mean time for the first visit was 18.0 weeks with a standard deviation of 4.6 weeks and the timing of the first ANC booking ranged from seven weeks to thirty-six weeks [Figure 3].
Table 3.
Obstetric history of pregnant mothers attending first antenatal care booking in Ambo town administration, August to September 2018
| Variables | Frequency | Early (before 16 weeks)# (%) | Late (at or after 16 weeks)# (%) |
|---|---|---|---|
| Number of pregnancies (n=344) | |||
| Primigravida | 166 | 56 (33.7) | 110 (66.3) |
| Multigravida | 178 | 49 (27.5) | 129 (72.5) |
| Parity (n=268) | |||
| Parity zero | 13 | 7 (53.8) | 6 (46.2) |
| Parity one and above | 155 | 36 (23.2) | 119 (76.8) |
| Number of alive children | |||
| 1-2 | 112 | 22 (19.6) | 90 (80.4) |
| >2 | 40 | 12 (30) | 28 (70) |
| ANC visit for last pregnancy (n=178) | |||
| Yes | 143 | 42 (29.4) | 101 (70.6) |
| No | 35 | 7 (20) | 28 (80) |
| History of stillbirth (n=178) | |||
| Yes | 15 | 4 (26.7) | 11 (73.3) |
| No | 163 | 45 (27.6) | 118 (72.4) |
| History of abortion (n=178) | |||
| Yes | 35 | 16 (45.7) | 19 (54.3) |
| No | 143 | 33 (23.1) | 110 (76.9) |
Figure 2.
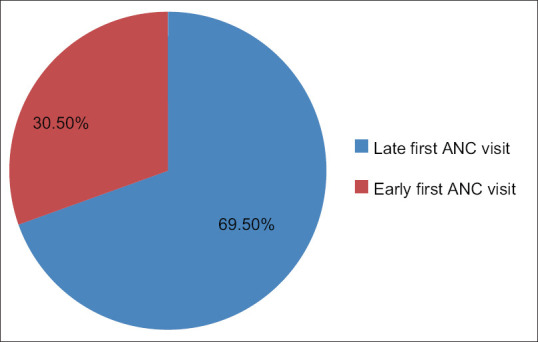
Timing of first ANC booking among pregnant mothers attending health facility in Ambo town administration, August to September 2018
Figure 3.
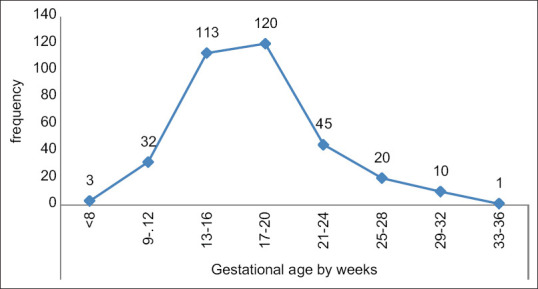
Frequency of pregnant mothers attending public health facility for first ANC booking by gestational age in Ambo town administration, August to September 2018
A majority (83.1%) of the respondents initiated their first ANC later in the second trimester. Only 12.2% of respondents initiated first ANC in the first trimesters [Figure 4].
Figure 4.
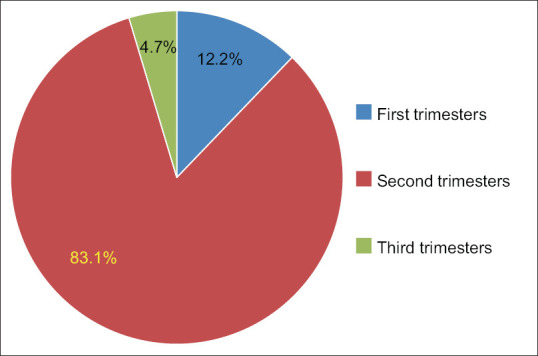
Initiation time of pregnant mothers attending health facility for first antenatal care booking by trimesters in Ambo town administration, August to September 2018
A majority (82.3%) of the respondents’ pregnancy was planned and 282 (82%) of pregnancy was wanted. The reasons given by respondents for coming early were to receive recommended prenatal care services for their unborn child (82.9%), for themselves (62.9%), to learn their health status and avoid pregnancy-related issues (83.8%), and because they had a history of obstetric complications (12.4%). Contrarily, the reasons given by pregnant mothers for coming late for ANC services were as follows: lack of knowledge about the timing of initial ANC services (22.4%); no problems with their pregnancy (30.2%); failure to recognize pregnancy early (46.1%); lack of attention from service providers if they arrived early (10.6%); busyness (30.2%); and 5.7% reporting that they were instructed to arrive after 16 weeks by service.
Factors associated with early initiation of ANC attendants
Binary logistic regression was carried out to identify factors independently associated with early ANC initiation. Multivariable logistic regression revealed that the following factors have an association with early ANC initiation: the occupation of a partner, knowledge of ANC program, number of pregnancies, planned pregnancy, and having advice from the health profession on ANC.
Respondents whose partners’ occupation was merchant had 3.47 times more likelihood (AOR = 3.47, 95% CI: 1.15, 10.46) to initiate first ANC early compared to those partners whose occupation was a government employee. Respondents who had good knowledge of ANC follow-up are 2.25 times more likely (AOR = 2.25, 95% CI: 1.06, 4.78) to book their first ANC early than those who had poor knowledge. Primigravida mothers were 2.52 times more likely (AOR = 2.52, 95% CI: 1.20, 5.32) to initiate first ANC early than those who had multigravida. Participants who had planned pregnancy were 2.86 times more likely (AOR = 2.86, 95% CI: 1.05, 7.81) to initiate first ANC than those mothers who had an unplanned pregnancy. Respondents who know the available service of ANC were three times more likely (AOR = 3.00, 95% CI: 1.31, 6.88) to initiate their first ANC early than those who did not know about the available service of ANC. Similarly, respondents who had ANC advice from health professionals were 2.27 times more likely (AOR = 2.27, 95% CI: 1.05, 4.89) to visit a health facility early for ANC than those who did not get the advice [Table 4].
Table 4.
Multivariate logistic regression analysis result for variables associated with early initiation of first ANC visit among pregnant mothers attending ANC service in Ambo town, August to September 2018
| Variable | Early (before 16 weeks)# (%) | Late (at or after 16 weeks)# (%) | COR 95% CI | AOR 95% CI | P |
|---|---|---|---|---|---|
| Age of respondents | |||||
| <20 | 28 (30.1) | 65 (69.9) | 1 | 1 | |
| 20-34 | 68 (29.1) | 166 (70.9) | 0.95 (0.56,1.61) | 0.68 (0.26,1.77) | 0.120 |
| ≥35 | 9 (52.9) | 8 (47.1) | 2.61 (0.91,7.47) | 4.09 (0.69,24.13) | 0.160 |
| Total family size | |||||
| <3 | 83 (32.7%) | 171 (67.3%) | 1.50 (0.87,2.60) | 1.76 (0.72,4.28) | 0.216 |
| ≥3 | 22 (24.4%) | 68 (75.6%) | 1 | 1 | |
| Distance from nearest health facility | |||||
| ≤60 min | 100 (31.3) | 219 (68.7) | 1.83 (0.67,5.00) | 0.47 (0.11,2.06) | 0.339 |
| >60 min | 5 (20) | 20 (80) | 1 | 1 | |
| Age of partner | |||||
| <20 | 5 (38.5) | 8 (61.5) | 2.54 (0.72,8.98) | ~ | 0.999 |
| 20-34 | 83 (33.5) | 165 (66.5) | 2.05 (1.08,3.89) | 2.05 (0.84,5.01) | 0.10 |
| >=35 | 14 (19.7) | 57 (80.3) | 1 | 1 | |
| Occupation of partner | |||||
| Government employee | 29 (27.9) | 75 (72.1) | 1 | 1 | |
| Daily laborer | 17 (29.8) | 40 (70.2) | 1.10 (0.54,2.24) | 1.19 (0.41,3.42) | 0.749 |
| Merchant | 17 (40.5) | 25 (59.5) | 1.76 (0.83,3.73) | 3.47 (1.15,10.46)* | 0.027 |
| Private employed | 20 (30.3) | 46 (69.7) | 1.12 (0.57,2.21) | 1.74 (0.67,4.53) | 0.260 |
| Farmer | 11 (22) | 39 (78) | 0.73 (0.33,1.62) | 0.67 (0.20,2.26) | 0.520 |
| Others | 6 (54.5) | 5 (45.5) | 3.10 (0.88,10.96) | 5.16 (0.91,29.23) | 0.164 |
| Knowledge of ANC visit | |||||
| Poor knowledge | 63 (25.3%) | 186 (74.7%) | 1 | 1 | |
| Good knowledge | 42 (44.2%) | 53 (55.8%) | 2.34 (1.43,3.84) | 2.25 (1.06,4.78)* | 0.015 |
| Gravidity | |||||
| Primigravida | 56 (33.7%) | 110 (66.3%) | 1.34 (0.85,2.12) | 2.52 (1.20,5.32)* | 0.015 |
| Multigravida | 49 (27.5%) | 129 (72.5%) | 1 | ||
| Planned pregnancy | |||||
| Yes | 93 (32.9) | 190 (67.1) | 2.0 (1.01,3.94) | 2.86 (1.05,7.81)* | 0.040 |
| No | 12 (19.7) | 49 (80.3) | 1 | 1 | |
| Wanted pregnancy | |||||
| Yes | 92 (32.6% | 190 (67.4%) | 1.83 (0.94,3.53) | 1.62 (0.40,6.57) | 0.160 |
| No | 13 (21%) | 49 (79%) | 1 | 1 | |
| Know available services on ANC service | |||||
| Yes | 68 (38.9) | 107 (61.1) | 2.27 (1.41,3.65) | 3.00 (1.31,6.88)* | 0.009 |
| No | 37 (21.9) | 132 (78.1) | 1 | 1 | |
| Got advice from health professionals | |||||
| Yes | 48 (39%) | 75 (61%) | 1.95 (1.06,3.60) | 2.27 (1.05,4.89)* | 0.036 |
| No | 21 (24.7%) | 64 (75.3%) | 1 | 1 | |
| Got advice from health extension workers | |||||
| Yes | 12 (24) | 38 (76) | 0.56 (0.27,1.16) | 0.73 (0.30,1.76) | 0.093 |
| No | 57 (36.1) | 101 (63.9) | 1 | 1 | |
| Attitudes towards ANC | |||||
| Unfavorable | 34 (25) | 102 (75) | 1 | 1 | |
| Favorable | 71 (34.1) | 137 (65.9) | 1.55 (0.96,2.52) | 1.18 (0.53,2.61) | 0.693 |
Keys: *Indicates significant association at P <0.05 in multivariate, 1=Reference category, COR=crude odd ratio, AOR=adjusted odd ratio
Discussion
The findings of this study showed that 105 (30.5%; 95% CI 25.63%, 35.41%) of respondents initiated first ANC early (before 16 weeks) while 69.5% of them booked lately (at the fourth month of pregnancy and above).
WHO recommends that pregnant mothers, especially those who are living in developing countries shall start ANC booking in the first 4 months of pregnancy.[7] In Ethiopia, it is suggested that pregnant mothers should start their first ANC booking early (before 16 weeks of pregnancy).[9,26] Even though WHO and Ethiopian guidelines recommend ANC booking before 16 weeks, in this study, only 30.5% of pregnant mothers initiated their first ANC early (before sixteen weeks of pregnancy). These differences might be due to poor implementation of focused ANC in the study areas.
This study’s result was relatively lower compared to the findings of other studies which reported 70% in Nepal,[28] 46% in South Africa,[29] 44.1% by Ethiopian Demographic Health Survey (EDHS) 2016 on urban women,[10] 58% in Addis Ababa,[19] 41% in Tigray Central Zone,[20] and 66.6% in Debre Markos.[30] Such a relatively high difference in the prevalence of early initiation of first ANC is largely due to variation in socio-demographic features of the study participants, the difference in health information and communication on the timing of first ANC among healthcare providers, the cut point of gestational week difference, and knowledge of mothers on the importance of early ANC booking.
But, this result is higher when compared with a study done in Arba Minch town and district.[21] This inconsistency may be due to the research done in Arba Minch covering participants from rural areas and due to the socio-demographic characteristics of the respondents.
On the other hand, this finding is nearly in line with a study conducted in south-eastern Tanzania (29%),[27] Dilla town (35.4%), Debra Markos (33.4%), and Debre Berhan town (26.2%).[22,30,31] This consistency might be due to the similarity of the cut point of gestational age sixteen weeks and year of study.
In this study, planned pregnancy was significantly associated with early initiation of first ANC. This finding was in line with a study conducted in Addis Ababa,[19] Arba Minch town and district,[21] and Debre Berhan town.[31] This might be because when mothers had planned a pregnancy, they are interested in the search for health information and communicate with concerned bodies to visit health facility timely.
Gravidity was associated with the early initiation of the first ANC visit. This study is also consistent with the study done in the Central Tigray zone[20] and data review which indicated that multi-gravida had higher odds of delayed initiation of ANC visit when compared to the primigravida.[32] This study is also supported by a study done in Boricha district, Southern Ethiopia.[33] This could be due to primigravida mothers may be younger and have access to the different health information on the advantages of early initiation of first ANC follow-up.
Mothers who had good knowledge of ANC follow-up were more likely to make an early first ANC visit. This finding was supported by a study done in Southern Ethiopia.[34] Similarly, studies done in Dilla town showed that pregnant mothers who know the importance of timely booking booked the first ANC within recommended time as compared to referents.[22] In the same manner, a study done in Debre Berhan town and a systematic review done on ANC initiation in Ethiopia showed that mothers who had good knowledge of early ANC visits were more likely to book their first ANC early.[31,35] This might be due to those pregnant mothers who know the exact time coming early than those without information.
Mothers whose partners’ occupation was merchant initiate first ANC early. This result was supported by a study done in the Tigray region.[36] This might be due to the life status of the family; they gave more attention to the pregnancy to seek and checked their pregnancy status early.
The result of the study indicates that mothers who got advice on ANC booking time from health professionals before visiting a health facility initiated first ANC early than those who did not get advice. This study is supported by a study conducted in northern Jordan.[37] Similarly, studies conducted on health facilities in Central Zone, Tigray, and Southern Ethiopia showed that pregnant mothers were advised on the timing of their first ANC booked early.[20,34] This might be because pregnant mothers accept and implement the advice given by health professionals than by health extension workers and mass media.
Conclusion and Recommendation
Conclusion
Early initiation of first ANC was relatively low in Ambo town health facilities. So, the majority of the pregnant mothers did not get the services based on the recommendation of ANC guidelines. This study indicated that planned pregnancy, number of pregnancies, knowledge of ANC follow-up, occupation of respondents’ partner, and having advice from health professionals had a significant association with early initiation of ANC.
Recommendation
All concerned bodies should strengthen and maintain a local information dissemination network on early initiation of first ANC and should develop a clear structure that will advance knowledge of reproductive age women on the timing of ANC. Community-based information, education, and communication on ANC and its right time of beginning should be organized and implemented by both health extension workers (HEWs) and health professionals.
Health professionals should provide full information, advice, and the importance of early ANC for every eligible mother. It is important to provide continuous public health education on the importance of early initiation of the first ANC visit at a health facility. Researchers should do further studies both with qualitative and quantitative researches to improve the ANC service quality and the importance of early first ANC booking. Community-based cross-sectional studies should be done in the study area.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We would like to thank the Department of Public Health, School of Health Science, Ambo University for providing permission to conduct this study. We would also like to extend our appreciation to health workers in the Ambo Town Health office and facilities for their cooperation and facilitation by providing baseline information. We would like to thank all study participants and data collectors for their contribution to the success of our work.
References
- 1.Tuncalp O, Were WM, MacLennan C, Oladapo OT, Gulmezoglu AM, Bahl R, et al. Quality of care for pregnant women and newborns-the WHO vision. BJOG. 2015;122:1045–9. doi: 10.1111/1471-0528.13451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO . Geneva, Switzerland: WHO Document Production Services; WHO; 2016. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience; p. 105. [Google Scholar]
- 3.CSA[Ethiopia], ICF. Ethiopia Demographic and Health Survey 2011. Addis Ababa: Ethiopia and Calverton; Central Statistical Agency and ICF International; 2012. p. 121. [Google Scholar]
- 4.CSA[Ethiopia], ICF. Ethiopia Mini Demographic and Health Survey 2014. Addis Ababa: Ethiopia and calverton; CSA (Ethioia) and ICF international; 2014. p. 49. [Google Scholar]
- 5.WHO. Packages of Interventions, for Family Planning, Safe Abortion Care, Maternal, Newborn and Child Health. Geneva, Switzerland: WHO Document Production Services; 2010. [Google Scholar]
- 6.Belayneh T, Adefris M, Andargie G. Previous early antenatal service utilization improves timely booking:cross-sectional study at university of Gondar hospital, northwest Ethiopia. J pregnancy. 2014;2014 doi: 10.1155/2014/132494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Villar J, Ba'aqeel H, Piaggio G, Lumbiganon P, Miguel BJ, Farnot U, et al. WHO antenatal care randomised trial for the evaluation of a new model of routine antenatal care. Lancets. 2001;357:1551–64. doi: 10.1016/s0140-6736(00)04722-x. [DOI] [PubMed] [Google Scholar]
- 8.Villar J, Bergsjo P. WHO antenatal care randomized trial:Manual for the implementation of the new model. WHO/RHR. 2002;130:7. [Google Scholar]
- 9.Mistry Health of Ethiopia. Revised Health Management Information System Indicator Reference Guide. Addis Ababa: Minstry of Health; 2017. [Google Scholar]
- 10.WHO, UNFPA, The World Bank. Trends in maternal mortality: 1990 to 2010. World health organization, UNICEF, UNFPA, and the World Bank; 2012. [Google Scholar]
- 11.Mehboob R, Gilani SA, Khalid S, Hassan A, Alwazzan A. In: Global Women's Health. IntechOpen, United Kingdom; 2021. Maternal mortality ratio in low income developing countries. [Google Scholar]
- 12.Musarandega R, Nyakura M, Machekano R, Pattinson R, Munjanja SP. Causes of maternal mortality in sub-Saharan Africa:A systematic review of studies published from 2015 to 2020. J Glob Health. 2021;11:04048. doi: 10.7189/jogh.11.04048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO. World Health Statistics 2015. Switzerland: Luxembourg; 2015. p. 18. [Google Scholar]
- 14.Ethiopian Public Health Institute (EPHI) [Ethiopia] and ICF. Ethiopia Mini Demographic and Health Survey 2019: Final Report. Rockville, Maryland, USA: EPHI and ICF; 2021. [Google Scholar]
- 15.WHO, UNICEF, UNFPA, World, Bank. Trends in Maternal Mortality: 1990 to 2010. World Health Organization; France: 2012. [Google Scholar]
- 16.Bain LE, Aboagye RG, Dowou RK, Kongnyuy EJ, Memiah P, Amu H. Prevalence and determinants of maternal healthcare utilisation among young women in sub-Saharan Africa:Cross-sectional analyses of demographic and health survey data. BMC Public Health. 2022;22:1–20. doi: 10.1186/s12889-022-13037-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang W, Alva S, Wang S, Fort A. Calverton, Maryland, USA: ICF Macro; 2011. Levels and Trends in the Use of Maternal Health Services in Developing Countries: DHS Comparative Reports 26. [Google Scholar]
- 18.Sinyange N, Sitali L, Jacobs C, Musonda P, Michelo C. Factors associated with late antenatal care booking:Population based observations from the 2007 Zambia demographic and health survey. Pan Afr Med J. 2016;25:109. doi: 10.11604/pamj.2016.25.109.6873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gulema H, Berhane Y. Timing of first antenatal care visit and its associated factors among pregnant women attending public health facilities in Addis Ababa, Ethiopia. Ethiop J Health Sci. 2017;27:139–46. doi: 10.4314/ejhs.v27i2.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gidey G, Hailu B, Nigus K, Hailu T, G/Her W, Gerensea H. Timing of first focused antenatal care booking and associated factors among pregnant mothers who attend antenatal care in Central Zone, Tigray, Ethiopia. BMC Res Notes. 2017;10:608. doi: 10.1186/s13104-017-2938-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gebremeskel F, Dibaba Y, Admassu B. Timing of first antenatal care attendance and associated factors among pregnant women in Arba Minch Town and Arba Minch District, Gamo Gofa Zone, south Ethiopia. J Environ Public Health. 2015;2015:971506. doi: 10.1155/2015/971506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abuka T, Alemu A, Birhanu B. Assessment of timing of first antenatal care booking and associated factors among pregnant women who attend antenatal care at health facility in Dilla town, Gedeo Zone, Souther nations, nationalities and peoples region, Ethiopia 2014. J Pregnancy Child Health. 2016;3:258. [Google Scholar]
- 23.Guevarra MV, Stubbs JM, Assareh H, Achat HM. Risk factors associated with late entry to antenatal care visits in NSW in 2014. Aust N Z J Public Health. 2017;41:543–4. doi: 10.1111/1753-6405.12668. [DOI] [PubMed] [Google Scholar]
- 24.Kisuule I, Kaye DK, Najjuka F, Ssematimba SK, Arinda A, Nakitende G, et al. Timing and reasons for coming late for the first antenatal care visit by pregnant women at Mulago hospital, Kampala Uganda. BMC Pregnancy Childbirth. 2013;13:121. doi: 10.1186/1471-2393-13-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.FDRE , Commission C. Summary and Statistical Report of the 2007 Population and Housing Census. Central Statistical Authority: Addis Ababa. 2008 [Google Scholar]
- 26.FMOH. Ethiopian basic emergency obstetric & newborn care (BEmONC) Training Manual 2013 [Google Scholar]
- 27.Gross K, Alba S, Glass TR, Schellenberg JA, Obrist B. Timing of antenatal care for adolescent and adult pregnant women in south-eastern Tanzania. BMC Pregnancy Childbirth. 2012;12:16. doi: 10.1186/1471-2393-12-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Paudel YR, Jha T, Mehata S. Timing of first antenatal care (ANC) and inequalities in early initiation of ANC in Nepal. Front Public Health. 2017;5:242. doi: 10.3389/fpubh.2017.00242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Muhwava LS, Morojele N, London L. Psychosocial factors associated with early initiation and frequency of antenatal care (ANC) visits in a rural and urban setting in South Africa:A cross-sectional survey. BMC Pregnancy Childbirth. 2016;16:18. doi: 10.1186/s12884-016-0807-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ewunetie AA, Munea AM, Meselu BT, Simeneh MM, Meteku BT. DELAY on first antenatal care visit and its associated factors among pregnant women in public health facilities of Debre Markos town, North West Ethiopia. BMC Pregnancy Childbirth. 2018;18:173. doi: 10.1186/s12884-018-1748-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zegeye AM, Bitew BD, Koye DN. Prevalence and determinants of early antenatal care visit among pregnant women attending antenatal care in Debre Berhan Health Institutions, Central Ethiopia. Afr J Reprod Health. 2013;17:130–6. [PubMed] [Google Scholar]
- 32.Ebeigbe PN, Igberase GO. Reasons given by pregnant women for late initiation of antenatal care in the niger delta, Nigeria. Ghana Med J. 2010;44:47–51. [PMC free article] [PubMed] [Google Scholar]
- 33.Dulla D, Daka D, Wakgari N. Antenatal care utilization and its associated factors among pregnant women in Boricha District, Southern Ethiopia. Divers Equal Health Care. 2017;14:76–84. [Google Scholar]
- 34.Geta MB, Yallew WW. Early Initiation of antenatal care and factors associated with early antenatal care initiation at health facilities in Southern Ethiopia. Adv Public Health. 2017;10:6. [Google Scholar]
- 35.Yesuf EA, Calderon-Margalit R. Disparities in the use of antenatal care service in Ethiopia over a period of fifteen years. BMC Pregnancy Childbirth. 2013;13:131. doi: 10.1186/1471-2393-13-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tsegay Y, Gebrehiwot T, Goicolea I, Edin K, Lemma H, Sebastian MS. Determinants of antenatal and delivery care utilization in Tigray region, Ethiopia:A cross-sectional study. Int J Equity Health. 12:30. doi: 10.1186/1475-9276-12-30. 213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hijazi HH, Alyahya MS, Sindiani AM, Saqan RS, Okour AM. Determinants of antenatal care attendance among women residing in highly disadvantaged communities in northern Jordan:A cross-sectional study. Reprod Health. 2018;15:106. doi: 10.1186/s12978-018-0542-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


