ABSTRACT
Introduction:
There is a continuous and increasing trend in sexually transmitted infections (STIs) worldwide. There are severe consequences of STI especially among women practicing high-risk behavior. Control of STI among women practicing high-risk behavior is an important strategy to reduce HIV transmission. In the present study, STIs and reproductive tract infections (RTI) were assessed among bar girls in an urban metro city.
Methods:
The cross-sectional study was conducted among bar girls residing in an urban settlement from May 2018 to December 2018. 195 bar girls randomly selected from among the registered bar girls for HIV prevention services with a local NGO and willing to participate were enrolled after obtaining informed consent. They were interviewed in person and clinical examination was conducted for assessing symptoms and signs of STI and RTI.
Results:
The median age of women was 26 years. 45% women reported sexual activity 3–6 times/week. 49.7% women reported symptom of vaginal discharge in the preceding 3 months, 52.3% women reported pain in lower abdomen, 10.2% women complained of genital ulcer disease, 67.2% women reported itching in the genital area, and 36.4% women had complaint of dyspareunia. 90.2% women in the present study had at least one symptom of STI/RTI.
Conclusion:
High-risk sexual behavior of bar girls with their regular clients puts them at a higher risk of acquiring HIV/AIDS. Focused efforts need to be put in to encourage reporting of symptoms for early diagnosis and management of STI/RTIs.
Keywords: Bar girls, community based organizations (CBO), human immunodeficiency virus (HIV), reproductive tract infection (RTI), sexually transmitted infection (STI)
Introduction
Reproductive tract infections (RTI) including sexually transmitted infections (STI) present a huge burden of diseases and adversely impact reproductive health. STI are of public health concern not only because of their high prevalence worldwide, but also because of their potential to cause serious and permanent complications in infected people who are not treated in a timely and effective way (National health program (NHP) STI). On average, approximately 1 in 25 people globally have at least one of the four STIs, which include trichomoniasis, bacterial vaginosis, chlamydia, and gonorrhea.
Many STIs can be identified and treated on the basis of characteristic symptoms and signs. Syndromic management refers to approach of treating STI symptoms and signs based on the organism most commonly responsible for such syndrome. WHO recommends the syndromic approach for diagnosis and management of RTI/STIs as it was observed that in many public health facilities, symptoms of these infections were going unrecognized. White discharge was reported to be the major complaint regarding STI/RTI and women referred to the problem indirectly by using the terms such as “backache” and “weakness” for white discharge.[1]
Bar girls have been categorized as “Sex Workers,” whose primary occupational identity may vary, but as a large proportion of their occupation group, but not all, often engage in commercial sex regularly and in significant volumes.[2] The sex workers are considered a high-risk group for the acquisition of STI, due to their social vulnerability and factors associated with their work like a history of multiple sex partners, inconsistent condom use, or coinfection with other STI. Bar girls remain a high-risk group for STI transmission to their numerous clients.
Under National AIDS Control Program in India, ensuring clinical service provision for groups practicing high-risk behaviors such as sex workers, men having sex with men, and intravenous drug users for RTI/STI case management is one of the strategies for the prevention and control of HIV/AIDS.
There are hardly any studies on STI syndromes among the bar girls in Mumbai. The present study was undertaken among bar girls residing in the urban resettlement slum of Mumbai to assess their sociodemographic and sexual risk profile and to determine the signs and symptoms associated with STI.
Materials and Methods
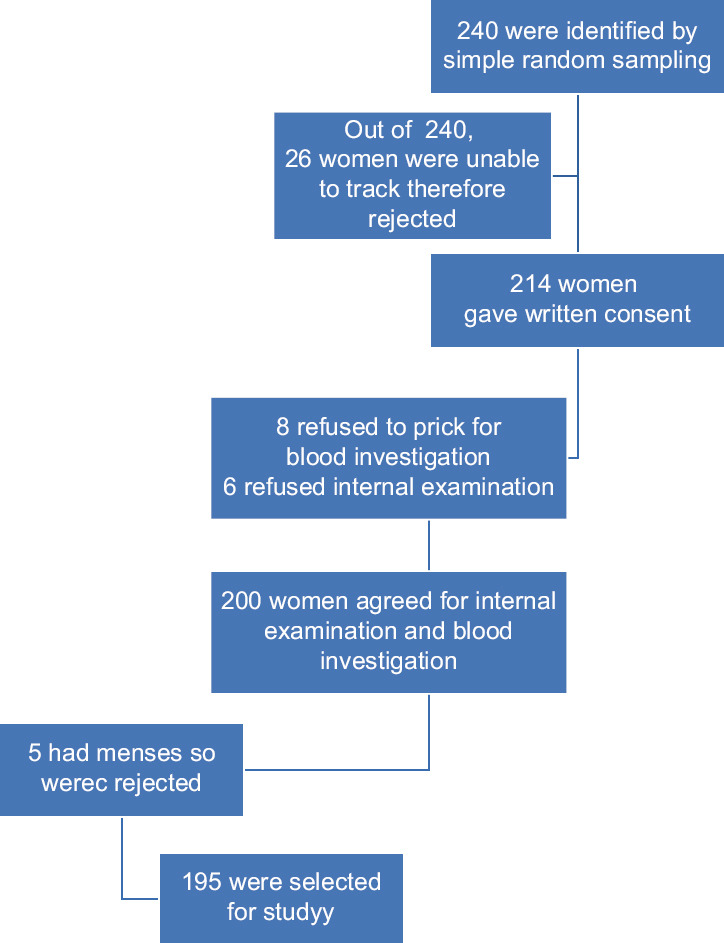
The urban slum community at our urban health center has a significant presence of bar girls residing in the area. These women are registered with a local NGO for HIV prevention services under targeted intervention from Mumbai Districts AIDS Control Society. A designated STI/RTI clinic with a trained counselor is also set up in the urban health center for regular medical check-up and management of patients with STI/RTI in the community. Approval from IRB was sought for the collaborative study with MDACS and NGO. A simple random sampling method by random number tables was used to identify the study participants from the list of registered bar girls with the local NGO. These women were contacted with help of peer educator and outreach worker and explained the purpose of the study. 240 bar girls willing to participate in the study after informed consent process were interviewed using a pretested semistructured questionnaire. The study was carried out from May 2018 to December 2018.
The bar girls were contacted at their residence with the help of outreach workers/peers; the women who agreed to participate were interviewed and examined at an urban health center. Demographic and socioeconomic characteristics including age, education, religion, and marital status were obtained. These women were subjected to thorough clinical examination. The investigator was trained to elicit signs of cervical infection (cervical discharge, friability, or ectopy) and pelvic inflammatory disease (cervical motion or adnexal tenderness). External genitalia, perianal region, and genital lesions and inguinal lymph nodes were palpated and findings were recorded. Vagino-cervical discharge (VCD) includes symptomatic vaginal discharge, asymptomatic discharge on examination, and cervical discharge on speculum. Lower abdominal pain (LAP) syndrome includes lower abdominal pain with cervical motion tenderness. Findings were recorded in a clinical assessment form.
Data Analysis was done using Microsoft Excel 2007 software and SPSS software version 22.0. Data was summarized using percentages and contingency tables.
Results and Analysis
The median age of the bar girls was 26 years. 41.6% bar girls were unable to read and write, while 74.3% were currently married. The majority belonged to lower socioeconomic class [Table 1].
Table 1.
Association of sociodemographic characteristics with weekly sexual activity
| Sexual activity/week | Total | P | |||
|---|---|---|---|---|---|
|
| |||||
| 1-2/week | 3-6/week | >6/week | |||
| Age group in years | |||||
| 18-24 | 22 (47.8%) | 12 (26.1%) | 12 (26.1%) | 46 (23.5%) | Chi: 0.002, df: |
| 25-34 | 52 (51.4%) | 33 (32.7%) | 16 (15.8%) | 101 (51.8%) | 1, P=0.4818 |
| 35-44 | 16 (44.5%) | 14 (38.8%) | 6 (16.7%) | 36 (18.4%) | |
| 45-55 | 6 (50%) | 3 (25%) | 3 (25%) | 12 (6.1%) | |
| Total | 96 (49.2%) | 62 (31.8%) | 37 (19%) | 195 | |
| Per capita income | |||||
| More than Rs 6528 | 02 (33.3%) | 02 (33.3%) | 02 (33.3%) | 6 (3%) | Chi: 4.27 |
| Rs 3264-6527 | 05 (33.3%) | 05 (33.3%) | 5 (33.3%) | 15 (7.7%) | Df: 2 P=0.118 |
| Rs 1959-3263 | 26 (44.8%) | 21 (36.2%) | 11 (19%) | 58 (29.7%) | |
| Rs 979-1958 | 62 (53.4%) | 37 (31.9%) | 17 (14.6%) | 116 (59.4%) | |
| Total | 95 (48.8) | 65 (33.4) | 35 (18) | 195 (100) | |
Figures in parentheses indicate percentage
41.5% bar girls had sexual relations with spouse and clients both, while 40.5% had sexual relation with spouse only. 26.6% bar girls reported sexual activity once-twice/week, while 45% bar girls reported sexual activity 3–6 times/week. 41% bar girls reported the use of condoms during sexual activity. Among the bar girls not using condom, 58.2% did not use a condom with regular or known clients.
We found that among all age groups, maximum women were engaged in having once-twice sexual activity/week. Among all the per capita income range stated, maximum women were engaged in having once-twice sexual activity/week. There was no significant association between sociodemographic characteristics and weekly sexual activity.
66.2% of women having vaginal discharge were illiterate. 81.8% of women having vaginal discharge had sexual relations with spouse and clients both. Of those women, with sexual activity more than six times per week, 91.3% had vaginal discharge. We found a significant association between the educational status of women, sexual relation with the type of clients, and sexual activity per week and discharge on examination to be statistically significant (P = 0.01) [Table 2].
Table 2.
Sociodemographic profile association with symptom of sexually transmitted disease
| Vaginal discharge on examination | Total | P | ||
|---|---|---|---|---|
|
| ||||
| Yes | No | |||
| Age group in years | ||||
| 18-24 | 30 (65.2) | 16 (34.7) | 46 (23.5) | P=0.44 |
| 25-34 | 74 (73.3) | 27 (26.7) | 101 (51.8) | |
| 35-44 | 23 (63.9) | 13 (36.1) | 36 (18.4) | |
| 45-55 | 8 (66.7) | 4 (33.3) | 12 (6.1) | |
| Educational status | ||||
| Illiterate | 53 (66.2) | 27 (33.8) | 80 (41.02) | P=0.0023 |
| 1st-4th std | 18 (64.2) | 10 (35.8) | 28 (14.3) | |
| 5th-7th std | 45 (73.8) | 16 (26.2) | 61 (31.2) | |
| 8th-10th std | 18 (75) | 06 (25) | 24 (12.3) | |
| More than 10th std | 01 (50) | 01 (50) | 02 (1) | |
| Per capita income | ||||
| More than Rs 6528 | 5 (83.3) | 1 (16.7) | 6 (3) | P=0.365 |
| Rs 3264-6527 | 12 (80) | 3 (20) | 15 (8) | |
| Rs 1959-3263 | 41 (70.6) | 17 (29.3) | 58 (30) | |
| Rs 979-1958 | 77 (66.3) | 39 (33.7) | 116 (59) | |
| Sexual Relation | ||||
| Only spouse | 27 (67.5) | 13 (32.5) | 40 (20.5) | P<0.01 |
| Spouse and client | 63 (81.8) | 14 (18.1) | 77 (39.5) | |
| Relation with clients only | 45 (57.7) | 33 (42.3) | 78 (40) | |
| Sexual activity/week | ||||
| Once-twice | 33 (66) | 17 (34) | 50 (26) | P<0.001 |
| 3-6 times | 48 (56.3) | 38 (43.6) | 87 (44) | |
| More than 6 times | 54 (91.3) | 05 (8.6) | 58 (30) | |
| Total | 135 (69.8) | 60 (30.2) | 195 (100) | |
Figures in parentheses indicate percentage
We found that 51.8% having vaginal discharge belong to the age group 25–34 years. 66.3% having vaginal discharge on examination were in the income range of Rs 979–1958 per capita. There was no significant association of age of women and per capita income with vaginal discharge on examination.
52.3% of women reported pain in lower abdomen, 10.2% genital ulcer disease, and 67.2% reported itching in the genital area were having vaginal discharge on examination. All the women who complained of vaginal discharge also had symptoms of burning micturition. 36.4% women had complaint of dyspareunia. 90.2% women had at least one symptom of STI/RTI. There was a significant association between pain in lower abdomen and itching in genital area and the presence of vaginal discharge on examination. Women not using condoms also showed a significant association with vaginal discharge on examination (P < 0.001).
49% of women had history of past vaginal discharge. There was a significant association between history of vaginal discharge and discharge on examination (P < 0.001) [Table 3].
Table 3.
Association between symptoms of sexually transmitted infections/RTI and signs
| Discharge on examination | Total | P df=1 | ||
|---|---|---|---|---|
|
| ||||
| Yes | No | |||
| Pain in abdomen | ||||
| Yes | 79 (77.4) | 23 (22.6) | 102 (52.3) | Chi: 6.784, P=0.0045 |
| No | 56 (60.2) | 37 (39.8) | 93 (47.7) | |
| Genital ulcer | ||||
| Yes | 13 (65) | 7 (35) | 20 (10) | Chi: 0.187, P=0.332 |
| No | 122 (69.8) | 53 (30.2) | 175 (90) | |
| Itching in genital area | ||||
| Yes | 75 (57.2) | 56 (42.8) | 131 (67.1) | Chi: 26.89, P<0.001 |
| No | 60 (93.8) | 4 (6.2) | 64 (32.9) | |
| Burning micturition | ||||
| Yes | 71 (73.9) | 25 (26.1) | 97 (49.8) | P=0.079 Chi: 1.985 |
| No | 64 (64.6) | 35 (35.4) | 98 (50.2) | |
| Total | 135 (69.2) | 60 (30.8) | 195 | |
Figures in parentheses indicate percentage
On internal examination, among women who had vaginal discharge, 33.3% women had yellow color discharge and 66.7% women had white discharge. 20% women had foul smelling discharge. Among 24.4% women, discharge was profuse and among 75.6% women, scanty discharge was observed. 15.4% women had yellow, foul smelling, and profuse vaginal discharge.
Discussion
The study was conducted with the help of pretested interview schedule to assess the symptoms and signs of STI, and the risk factors associated with STI in girls with high-risk behavior (FSW) by personal interview method. Data was collected from 195 participants during the period from May 2018 to December 2018. Data was summarized using percentages and contingency tables. Chi-square test was used for statistical inferences.
26.6% bar girls reported sexual activity once-twice/week, while 45% bar girls reported sexual activity 3–6 times/week. Hassan Taghizadeh et al.[3] found that average sexual activity was 1–10 per week. Nasirian et al.[4] found that number of sexual partners in a week ranged from 1 to 30. Desai et al.[5] found that the mean number of different sexual partners of sex workers per day was 5.
49.7% women reported symptom of vaginal discharge in the preceding 3 months. Desai et al.[5] found abnormal vaginal discharge in 12.7% women and the prevalence of vaginocervical discharge (VCD) was found in 51.7% women. Prabhakar et al.[6] found that, in 78.5% women had vaginal discharge and 52.3% women had pain in lower abdomen as most common symptom. Desai et al.[5] found lower abdominal pain in 19.5% girls. Prabhakar et al.[6] found lower abdominal pain in 18.7% women. Ghebremichael[7] found that the most prevalent STI symptom was lower abdominal pain and it was in 16% of women. 10.2% women complained of genital ulcer disease in our study, whereas Desai et al.[5] found genital ulcer in 5.9% girls, Ghebremichael[7] found genital ulcers in 1.1% of girls, and Prabhakar et al.[6] found genital ulcer in 5.8% of girls.
67.2% women reported itching in genital area. Ghebremichael reported[7] itching in the genital area in 15% of women. Desai et al.[5] found itching around the genital area in 10.2% women. All women who complained of vaginal discharge also had symptoms of burning micturition 49.7%. Desai et al.[5] found painful micturition in 11.0% women. Ghebremichael[7] found burning or pain on micturition in 6% women.
36.4% had complaint of dyspareunia. A study by Ghebremichael[7] showed that 9.4% had pain during intercourse. Desai et al.[5] found painful sexual intercourse in 12.7% women.
90.2% women had atleast one symptom of STI means vaginal discharge or foul smell etc. 27.1% had atleast one STI means they have lab confirmed STI syndrome, whereas Desai et al.[5] found that 47.5% had at least one STI, Nasirian et al.[4] found that 84.9% had at least one STI, Verscheijden et al.[8] found that 11.7% had at least one STI, Passey et al.[9] found that 59% of the women had at least one STD, and Behets et al.[10] found that 77.5% had at least one STI.
15.4% women had yellow, foul smelling, and profuse vaginal discharge. A study by Ghebremichael[7] found that 3.2% women had foul smell in genital area.
Conclusion
This study will help health care providers a picture that why there is a need to give special attention to health needs of bar girls. Young age, lack of proper education, uncertainty about future, and low income along with discrimination and stigma attached to their profession puts them in neglected section of society. High-risk sexual behavior of bar girls with their regular clients puts them at a higher risk of acquiring HIV/AIDS.
Ethical approval
Study was ethically approved by the Instituitional Ethics Committe of Seth GS Medical College and KEM Hospital Mumbai.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We are really thankful to the entire team of CBO, peer educators, and outreach workers for their immense help. Without them, it would have been impossible to complete this huge project. We would also like to acknowledge our gratitude toward DSRC staff for providing all the equipment required for internal examination.
References
- 1.Desai GS, Patel RM. Incidence of reproductive tract infections and sexually transmitted diseases in India:Levels and differentials. J Fam Welf. 2011;57:48–60. [Google Scholar]
- 2.Nirgude A, Solanki M, Shinde R, Naik P. Study of sexual behaviour of bar-girls residing in an urban slum area of Mumbai. Indian J Community Med. 2011;36:31–5. doi: 10.4103/0970-0218.80790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taghizadeh H, Taghizadeh F, Fathi M, Reihani P, Shirdel N, Rezaee SM. Drug use and high-risk sexual behaviors of women at a drop-in center in Mazandaran Province, Iran, 2014. Iran J Psychiatry Behav Sci. 2015;9:e1047. doi: 10.17795/ijpbs1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nasirian M, Kianersi S, Hoseini SG, Kassaian N, Yaran M, Shoaei P, et al. Prevalence of sexually transmitted infections and their risk factors among female sex workers in Isfahan, Iran:A cross-sectional study. J Int Assoc Provid AIDS Care. 2017;16:608–14. doi: 10.1177/2325957417732836. [DOI] [PubMed] [Google Scholar]
- 5.Desai VK, Kosambiya JK, Thakor HG, Umrigar DD, Khandwala BR, Bhuyan K. Prevalence of sexually transmitted infections and performance of STI syndromes against aetiological diagnosis, in female sex workers of red light area in Surat, India. Sex Transm Infect. 2003;79:111–5. doi: 10.1136/sti.79.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Das A, Prabhakar P, Narayanan P, Neilsen G, Wi T, Kumta S, et al. Prevalence and assessment of clinical management of sexually transmitted infections among female sex workers in two cities of India. Infect Dis Obstet Gynecol. 2011;2011:494769. doi: 10.1155/2011/494769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghebremichael M. The syndromic versus laboratory diagnosis of sexually transmitted infections in Resource-Limited settings. Int Sch Res Notices. 2014;2014 doi: 10.1155/2014/103452. Article ID 103452, 5 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Verscheijden MMA, Woestenberg PJ, Götz HM, Van Veen MG, Koedijk FDH, Van Benthem BHB. Sexually transmitted infections among female sex workers tested at STI clinics in the Netherlands, 2006-2013. Emerg Themes Epidemiol. 2015;12:12. doi: 10.1186/s12982-015-0034-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Passey M, Mgone CS, Lupiwa S, Suve N, Tiwara S, Lupiwa T, et al. Community based study of sexually transmitted diseases in rural women in the highlands of Papua New Guinea:Prevalence and risk factors. Sex Transm Infect. 1998;74:120–7. doi: 10.1136/sti.74.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Behets FMTF, Rasolofomanana JR, Van Damme K, Vaovola G, Andriamiadana J, Ranaivo A, et al. Evidence-based treatment guidelines for sexually transmitted infections developed with and for female sex workers. Trop Med Int Health. 2003;8:251–8. doi: 10.1046/j.1365-3156.2003.01017.x. [DOI] [PubMed] [Google Scholar]


