Abstract
Context
Clinical management of sport-related concussion requires the assessment of various factors, including motor performance. The tandem gait test, a measure of postinjury motor performance, has demonstrated clinical utility but is limited by time availability and test uniformity.
Objective
To assess intrasession reliability between tandem gait test trials and determine the number of trials necessary for optimal utility and feasibility in clinical decision-making after concussion.
Design
Cross-sectional study.
Setting
Pediatric sport medicine clinic.
Patients or Other Participants
Adolescent athletes who recently sustained a concussion (n = 44; age = 15.4 ± 1.8 years; 39% females) and were seen for care within 14 days (7.3 ± 3.2 days) of their injury as well as uninjured control participants (n = 73; age = 15.8 ± 1.3 years; 41% females). All individuals completed 3 single-task and 3 dual-task tandem gait trials.
Main Outcome Measure(s)
We collected test completion time and cognitive performance for each trial and calculated Pearson correlation coefficients between trials and intraclass correlation coefficients (ICCs) to determine intrasession reliability. We also compared performance between groups and calculated area under the curve (AUC) values to identify the ability of each trial to distinguish between groups.
Results
Both the concussion and control groups demonstrated high intrasession reliability between tandem gait trials under single- (R ≥ 0.82, ICC ≥ 0.93) and dual- (R ≥ 0.79, ICC ≥ 0.92) task conditions. The greatest group classification values were obtained from the second single-task trial (AUC = 0.89) and first dual-task trial (AUC = 0.83). Test completion time provided excellent between-groups discrimination in single- and dual-task conditions. However, cognitive performance during dual-task trials demonstrated only marginally significant clinical utility (AUC ≤ 0.67).
Conclusions
Tandem gait assessments may only require 2 trials under single-task and 1 trial under dual-task conditions to effectively discriminate between concussion and control groups. This approach may improve the feasibility (ie, time requirement) of the test while maintaining excellent discriminatory ability.
Keywords: mild traumatic brain injury, adolescent, evaluation, SCAT5, standardized assessment
Key Points
Tandem gait assessment may require fewer than 3 trials to effectively discriminate between concussion and control groups. This approach may improve the feasibility of the test in many clinical settings.
Tandem gait motor performance during the words-backward cognitive task demonstrated the greatest group classification accuracy among dual-task conditions. Clinicians should consider using this task to detect identifiable concussion-related impairments in motor performance.
Test completion time provided the best between-groups discrimination in single- and dual-task conditions. Thus, motor performance impairment, as measured by time to completion during tandem gait, may be a more accurate diagnostic approach than cognitive performance under this specific dual-task paradigm.
The diagnosis and management of patients with sport-related concussion requires assessment of an array of factors, including symptom severity, injury history, neurocognitive disruption, and motor performance impairment (eg, balance or gait instability).1 One factor particularly affected by concussion is motor performance.2–4 Various measures of motor performance impairment are included in the most recent edition of the Sport Concussion Assessment Tool (SCAT5) to assist physicians, athletic trainers, and physical therapists in complex concussion management and decision-making.1 One such measure of postinjury motor performance, the tandem gait test, has demonstrated excellent clinical utility for the management of concussion.5
According to the SCAT5, tandem gait testing requires patients to walk in a heel-toe pattern along a 3-m line1; complex motor control is assessed as complex motor control as the individual ambulates with a narrow base of support. This test can be performed under single-task (with undivided attention) and dual-task (in which the individual is asked to simultaneously complete a cognitive task) conditions.5–7 Single-task tandem gait time, the total number of seconds from start to finish, has demonstrated the capacity to distinguish patients with concussion from healthy control individuals when testing occurs within 1 week of injury.6,8,9 Furthermore, dual-task tandem gait time can differentiate patients with concussion from healthy control participants even after symptom resolution, confirming its ability to provide useful information for concussion management beyond that of typically used measures, such as symptom severity.6,8,9 When compared with their preinjury scores, collegiate athletes who sustained a concussion performed significantly slower on tandem gait testing within 48 hours of injury, as opposed to their nonconcussed peers, who showed no difference relative to baseline scores, indicating that baseline testing may be useful when assessing and interpreting postinjury tandem gait.5
Tandem gait assessment was first presented in the SCAT3; performance was quantified as the best (fastest) time among 4 total trials.10 Despite emerging research demonstrating the utility of a timed tandem gait in the assessment of patients with concussion,5,6,8,9 the most recent SCAT5 transitioned to a pass/fail evaluation,1,11 defining a failing score as separation between the heel and toe, stepping off the line, or using the administrator to regain balance. Regardless of this transition to a pass/fail system, recent authors5,8,9 have quantified single- and dual-task tandem gait performance among patients with concussion as either the average or the best time to completion for 3 trials under each condition. Furthermore, the SCAT5 offers no direction on or standardization of the cognitive task for use in dual-task conditions.1,11 As such, incorporating a question-and-answer cognitive task during tandem gait trials represents a feasible option for increasing task complexity, creating a more challenging and sportlike test environment, and better detecting identifiable concussion-related motor performance impairments.6,8,9,12
However, the feasibility of the clinical assessment of tandem gait may be restricted by a variety of factors. Primarily, clinician time availability is limited, given the numerous other recommended assessments performed during a clinical examination of an individual with concussion.1 A single tandem gait trial can last approximately 20 to 30 seconds after concussion.8,9 With intermittent preparation, instruction, and transition, a full assessment that contains multiple trials and conditions may take up to 10 minutes. Furthermore, previous researchers5 observed a difference between postinjury tandem gait times and preinjury baseline scores. As such, the inclusion of the tandem gait assessment in preinjury baseline testing is further limited by test administration time. This constraint is intensified when baseline testing is performed in 1 session for a large number of athletes, as is the case for many adolescent school and club sports. By reducing the time clinicians spend on test administration, test feasibility can improve, specifically in time-limited situations such as sideline assessment, baseline testing, or clinical evaluation.
Concomitantly, the lack of uniformity in tandem gait testing, specifically for cognitive task use in dual-task testing and in the optimal number of trials, can create unnecessary variability among clinicians evaluating patients with sport-related concussions. Therefore, establishing a uniform tandem gait protocol, which is currently missing from the SCAT5,1,11 can improve test feasibility and reduce test variability. Although high test-retest reliability of tandem gait has been established for pediatric patients,7 the intrasession reliability of the assessment is currently unknown.
Therefore, the purpose of our investigation was to determine the number of tandem gait test trials necessary for optimal clinical feasibility (the number of trials required and intrasession reliability) and utility (discriminatory ability) to assist in clinical decision-making after concussion. A secondary objective was to evaluate the discriminatory ability of 3 cognitive tests within the dual-task framework.
METHODS
Participants and Study Design
We conducted a cross-sectional study of youth athletes aged 13 to 17 years who had recently sustained a concussion or were uninjured control participants. Concussion participants were seen for care at the institution's Sports Medicine Center and diagnosed with a concussion within 14 days of their injury. All concussions were diagnosed by Board-certified sports medicine physicians, consistent with the definition provided by the most recent international consensus statement on concussion in sport at the time of data collection.1 Participants completed the Post-Concussion Symptom Inventory (PCSI), a validated measure of concussion-related symptoms,13 at the time of assessment. Individuals with concussion reported higher PCSI scores, indicating an elevated level of concussion-related symptoms, than healthy control individuals. Recruits in the concussion group were excluded if they received a diagnosis for any injury other than a concussion or related sequelae (eg, neck strain) at the time of assessment. Control recruits were tested during routine preparticipation sport physical evaluations. All control group participants received clearance to engage in sport without restriction from a physician at the time of assessment, thus confirming their healthy status. No patients in the concussion group were among those tested during the preparticipation physical evaluations. Exclusion criteria for both groups were a history of epilepsy or seizure, preexisting neurologic or psychiatric disorder, or a diagnosed concussion within 6 months of the assessment (other than the injury for which the concussion group was being seen). Before the study, the local institutional review board approved the protocol, and all participants and their parents or legal guardians provided written informed assent and consent, respectively, to be involved in the study.
Tandem Gait Protocol
Tandem gait assessments were conducted during the visit at which the patient presented for evaluation (concussion group) or as part of a preparticipation physical evaluation (control group). The testing environment for tandem gait was a space free from clutter, furniture, or equipment that might interfere with gait; large enough for participants to comfortably ambulate without nearing walls or doorways; and secluded from obvious noise or distraction. Before test initiation, a study or clinical team member affixed a 3-m length of sports tape linearly to the ground in the testing area to delineate the test distance.
Participants received oral instruction from a clinical or research team member before the start of the test. They were instructed to walk using an alternating heel-to-toe pattern along the entire length of sports tape, complete a 180° turn with both feet still on the tape, and then continue the gait pattern back to the starting position without interruption. Individuals were asked to perform this task as quickly as possible, without separation of the heel and toe during gait, stepping off the tape, or relying on the test administrator to regain balance. During both single- and dual-task trials, the test administrator told participants when to begin each trial. The primary outcome measure was time to completion, measured in seconds by the administrator using a stopwatch or smartphone timer. The timer started as soon as the administrator instructed the person to begin the trial and stopped when the back foot reached the end of the sports tape. The test administrator recorded the time to completion during a 5- to 15-second break between trials.
Dual-task conditions mirrored those of a single task with the addition of a simultaneous cognitive task. The test administrator informed individuals that, for the next 3 trials, they were to respond aloud to cognitive tasks while simultaneously completing the tandem gait protocol. Three cognitive tasks were used in the dual-task condition, consistent with previous research6,7,12: (1) backward spelling of a simple 5-letter word, (2) serial subtraction by 6 or 7 from a 2-digit number, and (3) reciting the months in reverse order. All participants completed the dual-task trials in the same order of cognitive task completion (ie, trial 1 = words backward, trial 2 = serial subtraction, trial 3 = months in reverse).
Before each trial in the dual-task condition, individuals were informed of the cognitive task to be completed, and an oral description of the task was provided. If needed, they were offered a simplified practice prompt of a similar nature to that for the task used in the trial (eg, backward spelling of the word cat or subtraction of 7 from 14) to ensure comprehension. No instructions were given regarding the prioritization of either gait or the cognitive response. The primary outcome measure in the dual-task condition remained time to completion. The test administrator also recorded cognitive task accuracy (the number of correct responses divided by the total number of responses) and response rate (the number of seconds per response, calculated as trial time divided by the total number of responses) as secondary outcomes. Failed trials—defined as separation between the heel and toe in tandem gait, stepping off the tape, or relying on the administrator to regain balance—were not included in the subsequent analysis. In the event of a failed trial, the participant was asked to perform the trial again until 3 trials in each condition were successful. An inability to accurately respond to cognitive tasks was not considered a failed trial.
This protocol is consistent with procedures used in previous studies.5–7 Psychometric properties for tandem gait have been established, with reported sensitivity of 0.63, specificity of 0.61, and area under the curve (AUC) of 0.70.5 In addition, the tandem gait test in single-task (intraclass correlation coefficient [ICC] = 0.86) and dual-task (ICC = 0.84) conditions has demonstrated suitable levels of test-retest reliability for repeat clinical assessments over multiple sessions on different days.7
Statistical Analysis
Data are presented as mean ± SD for continuous variables and the number included (corresponding percentage) for categorical variables. We compared demographic and medical history characteristics between groups using independent-samples t tests and χ2 analyses. To assess test completion time and cognitive performance differences for each individual trial, we compared the concussion and control groups using independent-samples t tests. To adjust for multiple comparisons, we defined a significant difference between groups as P < .01. To assess within-session test reliability, we calculated Pearson correlation coefficients (r values) between trials 1 and 2 and between trials 2 and 3 separately for the concussion and control groups and for the single- and dual-task conditions. To interpret correlations between trials, we used the following values: <0.39, low correlation; 0.4 to 0.59, moderate correlation; 0.60 to 0.79, moderately high correlation; and ≥0.80, high correlation.14 Furthermore, we calculated the ICC [2,k] values across the 3 trials using a 2-way random-effects, absolute agreement, multiple raters and measurements approach15 separately for the concussion and control groups and for the single- and dual-task conditions.
To examine the ability of the obtained measures to discriminate between the concussion and control groups, we also calculated AUC values from receiver operating characteristic curves for each trial separately. We defined AUC values as outstanding (>0.9), excellent (0.8–0.9), acceptable (0.7–0.8), or poor (<0.7).16
Finally, to compare concussion and control group performances for each trial while adjusting for potential confounders, we constructed a series of multivariable linear regression models. The outcome variable in each model was tandem gait completion time in each trial; the predictor variable was group assignment; and covariates were height, concussion history, and symptom severity (PCSI rating). Any missing data were treated as such, and no imputations were performed. All statistical tests were 2 sided and conducted using Stata Statistical Software (version 15; StataCorp, LLC).
RESULTS
A total of 117 participants completed the study protocol: n = 44 had sustained a concussion within 2 weeks of the assessment (mean = 7.3 ± 3.2 days, range = 2–14 days) and n = 73 were uninjured. The concussion group was shorter, had a greater proportion of individuals with a previously diagnosed concussion, and reported greater symptom severity than the control group (Table 1).
Table 1.
Concussion and Control Group Participant Characteristics
| Variable |
Group |
P Value |
|
| Concussion (n = 44) |
Control (n = 73) |
||
| Age, y (mean ± SD) | 15.4 ± 1.8 | 15.8 ± 1.3 | .12 |
| Sex (female), No. (%) | 19 (39) | 30 (41) | .87 |
| Height, cm (mean ± SD) | 166.7 ± 9.7 | 171.8 ± 9.1 | .005a |
| Mass, kg (mean ± SD) | 66.0 ± 23.6 | 63.5 ± 17.7 | .52 |
| History of previous concussion, No. (%) | 23 (52) | 17 (23) | .002a |
| Attention-deficit or attention-deficit/hyperactivity disorder diagnosis, No. (%) | 5 (11) | 4 (5) | .25 |
| Symptom severity (Post-Concussion Symptom Inventory rating), mean ± SD | 50.0 ± 27.1 | 5.8 ± 8.1 | <.001a |
Significant difference (P < .05).
The concussion group completed the tandem gait test more slowly than the control group during both the single- and dual-task conditions for all 3 trials (Figure 1). In addition, the single-task tandem gait test demonstrated excellent discriminatory ability between groups during all 3 trials (AUC ≥ 0.85; Figure 1). Both groups displayed high correlations and ICC values across all single-task trials (Figure 1). Similarly, the concussion group performed the dual-task tandem gait test more slowly than the control group on all 3 trials, and the dual-task condition revealed excellent discriminatory ability between groups (AUC ≥ 0.80; Figure 2). The concussion and control groups demonstrated high correlations and ICC values across all dual-task trials (Figure 2). Classification accuracy was high between groups at the following cut points for the single-task (trial 1: 20.3 seconds = 82% accuracy; trial 2: 20.8 seconds = 82% accuracy; trial 3: 17.1 seconds = 83% accuracy) and dual-task (words backward: 29.2 seconds = 80% accuracy; subtraction: 26.8 seconds = 79% accuracy; months backward: 27.6 seconds = 75% accuracy) conditions.
Figure 1.
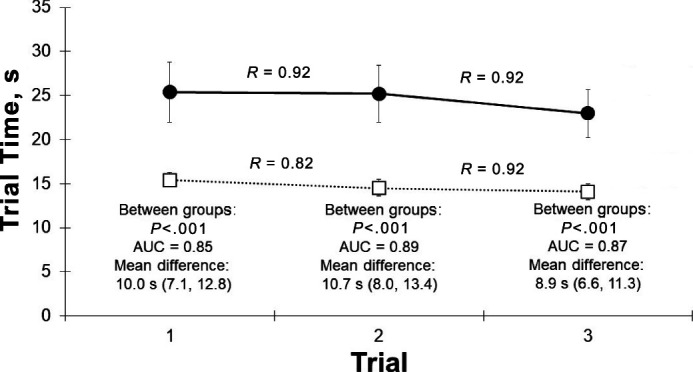
Single-task tandem gait performance. Data are presented as means; error bars represent 95% CIs. The concussion group is represented as black circles, and the control group is represented as white squares. AUC = area under the curve (derived from receiver operating characteristic analysis). The R values represent the trial-to-trial correlation within each group. Intraclass correlation coefficients (2,k) = 0.92 (0.96, 0.98) for the concussion group and 0.93 (0.90, 0.95) for the control group.
Figure 2.
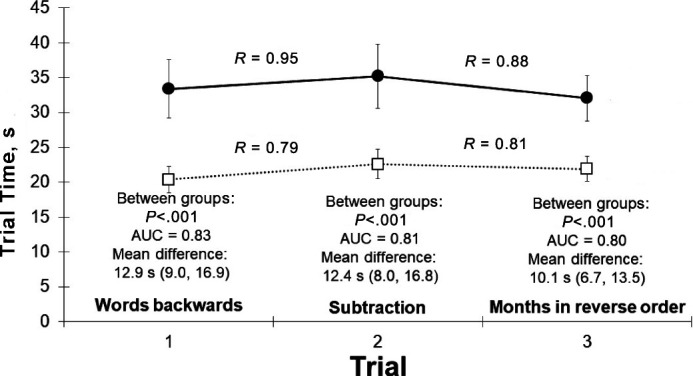
Dual-task tandem gait performance. Data are presented as means; error bars represent 95% CIs. The concussion group is represented as black circles, and the control group is represented as white squares. AUC = area under the curve (derived from receiver operating characteristic analysis). The R values represent the trial-to-trial correlation within each group. Intraclass correlation coefficients (2,k) = 0.94 (0.91, 0.97) for the concussion group and 0.92 (0.88, 0.95) for the control group.
No differences in cognitive performance were observed during the tandem gait test (Table 2). Specifically, no accuracy or response rate differences existed between groups for any of the 3 cognitive tasks, and AUC values were low (0.61–0.64).
Table 2.
Cognitive Performance During Dual-Task Tandem Gait Trials for the Concussion and Control Groups
| Task |
Group, Mean ± SD |
P Value |
Area Under the Curve Value |
|
| Concussion |
Control |
|||
| Words backward | ||||
| Accuracya | 67.2 ± 34.2 | 83.6 ± 29.4 | .013 | 0.67 |
| Response rateb | 9.8 ± 4.5 | 8.6 ± 5.9 | .28 | 0.64 |
| Serial subtraction | ||||
| Accuracya | 83.1 ± 25.6 | 79.2 ± 26.8 | .48 | 0.54 |
| Response rateb | 7.9 ± 6.2 | 6.2 ± 4.4 | .11 | 0.61 |
| Months-in-reverse | ||||
| Accuracya | 94.2 ± 10.2 | 93.6 ± 10.8 | .82 | 0.53 |
| Response rateb | 3.0 ± 2.2 | 2.2 ± 1.2 | .04 | 0.63 |
Percentage of questions answered correctly.
Seconds per response.
After adjusting for the potential confounding variables of height, concussion history, and symptom severity, we found significant associations between the concussion group and slower tandem gait test times for all 3 single-task trials and for the dual-task trials in which participants completed the words-backward and months-in-reverse tasks (Table 3).
Table 3.
Multiple Regression Results Describing the Expected Differences Between the Concussion and Control Groups (β Coefficient Value) for Each Tandem Gait Trial After Adjusting for Height, Concussion History, and Symptom Severity
| Condition |
β Coefficient |
95% CI |
P Value |
| Single task | |||
| Trial 1 | 7.87 | 3.33, 12.40 | .001a |
| Trial 2 | 7.76 | 3.30, 12.22 | .001a |
| Trial 3 | 5.73 | 1.75, 9.70 | .005a |
| Dual task | |||
| Trial 1 (words backward) | 9.40 | 3.11, 15.70 | .004a |
| Trial 2 (serial subtraction) | 8.44 | 1.37, 15.52 | .020 |
| Trial 3 (months in reverse) | 7.33 | 1.86, 12.80 | .009a |
Significant difference (P < .05).
DISCUSSION
Our data support those of previous researchers5,6,8,9 regarding the capacity of the tandem gait test to identify concussion-related motor performance impairment after a concussion. Although all trials were able to distinguish between groups, the most accurate group classification was obtained from tandem gait time-to-completion values during the second single-task trial and the first dual-task trial (words backward). Additionally, under both conditions, tandem gait time showed high intrasession reliability, demonstrating that values obtained from 1 test trial did not differ from those of another trial within the same testing session. This builds on earlier work7 that illustrated high test-retest reliability between sessions approximately 2 weeks apart. As such, our data suggest that a tandem gait protocol for use in concussion assessment among adolescent patients may only require 2 single-task trials and 1 dual-task trial with the concurrent words-backward test.
Under single-task conditions, the second trial (in which the greatest AUC value occurred) provided the best discriminatory ability, indicating that 2 timed trials may be adequate for clinical examination purposes. In dual-task conditions, tandem gait time to completion during the words-backward cognitive task most accurately predicted group classification (concussed versus nonconcussed). This indicates that only 1 dual-task trial with this cognitive cue may be required for clinicians to obtain clinically relevant information during concussion assessment. Therefore, the previously accepted quantification of motor performance as the best (ie, fastest) or average time to completion among 4 separate trials, as used in prior studies,8–10 may not be necessary. Our data suggest that 1 to 2 trials per condition may be sufficient in providing clinically useful information and the most streamlined protocol for tandem gait testing. This trial reduction is particularly significant under dual-task conditions, which require additional cognitive task instruction between trials. The clinical utility of these data thus offer an option for clinicians to reduce the time required for the tandem gait test in concussion evaluations.
A slight learning effect for tandem gait time to completion was observed as participants marginally improved in later trials, similar to the learning effects demonstrated for other concussion measures, such as the Modified Balance Error Scoring System (mBESS).17 This further supports the use of fewer trials in single- and dual-task tandem gait tests to reduce the influence of potential practice effects. Previous repeated-measure designs have identified high reliability across time for the tandem gait test (ICC values > 0.8),7,18 reflecting small learning effects across time. Our results endorse these findings but within the existing testing session when trials are administered consecutively. Furthermore, earlier investigators5 have supported the ability of tandem gait tests to identify concussion-related impairments in motor control beyond those detected by the Balance Error Scoring System (BESS) and mBESS (tandem gait, AUC = 0.704; BESS, AUC = 0.508; mBESS, AUC = 0.535). Although the tandem gait test may be slightly more complex in preparation, instruction, and administration than the mBESS, our results align with previous outcomes in further supporting the use of the tandem gait test as the primary assessment in motor control evaluations, particularly with improved test feasibility. Given that mean differences for each trial exceeded 95% confidence reliable change values (>5.3 seconds for the single task, >8.5 seconds for dual tasks),7 our data suggest this approach confers utility in the assessment of athletes with a concussion.
We noted no differences in cognitive performance during the tandem gait test. Specifically, no accuracy or response rate differences were identified between groups for any of the 3 cognitive tasks, and AUC values were low. Moreover, tandem gait time to completion appeared to be a stronger discriminator between groups than cognitive performance. Thus, motor performance impairment, as measured by time to completion during tandem gait, may be a more accurate diagnostic approach than cognitive performance under this specific dual-task paradigm. In addition, prior authors19 determined that athletes displayed worse cognitive performance than control individuals on the words-backward test during a steady-state gait task. These findings, paired with our observations, suggest the utility of this cognitive task as an appropriate dual-task cognitive cue for concussion management.
Our study had limitations that should be considered while interpreting the results. Our cross-sectional study design did not allow us to generalize to postinjury tests that are performed closer to clinical recovery (eg, at return-to-play clearance) rather than our assessment timeframe of approximately 1 week postinjury. Furthermore, we recruited both participants with concussion and control participants from 1 geographic area, within a relatively small age range, and only through our sports medicine clinic and community partnerships. Our results, therefore, may not be generalizable to other geographic locations, practice settings, or age groups.
In addition, lower intrasession reliability in tandem gait time to completion between trials was demonstrated for the concussion group than the control group. Although this variability can likely be explained, at least in part, by differences in sample sizes between groups, it may also be that individuals with concussion experience greater variation in tandem gait times. Thus, it may be relevant to investigate the clinical significance of this variability in future studies. Moreover, the order of cognitive task completion in dual-task conditions remained unchanged in our research, such that all individuals performed the cognitive tasks in the same trial order. Hence, although we indicated that cognitive task complexity and novelty may be an appropriate explanation for group classification (AUC) differences among dual-task trials, we could not determine the effect of cognitive task order on tandem gait performance with our current methods. It is possible that the AUC values obtained during dual-task trials were not due to the specific cognitive task used but rather to the trial number during which that cognitive task occurred (eg, first, second, or third trial).
The clinical utility of the tandem gait test for concussion decision making is well established,5–8 yet limitations of the test include the time to administer a series of trials within a comprehensive multifaceted concussion evaluation and the lack of uniformity among cognitive tasks used in dual-task paradigms and optimal number of trials required. Our results indicate that multiple (ie, 6) trials may not be required to obtain useful clinical information under each condition, thereby improving the feasibility of the test while maintaining group classification ability. Similarly, the words-backward cognitive task demonstrated the greatest group classification accuracy among dual-task conditions. Specific cognitive tasks may be more useful for dual-task testing, and their incorporation into standardized evaluations may improve uniformity of tandem gait assessment among clinicians, thus improving overall test feasibility beyond reducing the time requirements. Consequently, clinicians seeking valuable information on postinjury motor performance should consider using 2 single-task trials and 1 dual-task trial (words backward) in tandem gait for an appropriate balance between test feasibility and clinical utility during concussion evaluation.
Funding Statement
FINANCIAL DISCLOSURE Dr Howell has received research support from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (Award No. R03HD094560), the National Institute of Neurological Disorders and Stroke (Award Nos. R01NS100952, R03HD094560, and R43NS108823), and MINDSOURCE Brain Injury Network.
REFERENCES
- 1.McCrory P, Meeuwisse W, Dvořák J, et al. Consensus statement on concussion in sport-the 5th International Conference on Concussion in Sport held in Berlin, October 2016. Br J Sports Med . 2017;51(11):838–847. doi: 10.1136/bjsports-2017-097699. [DOI] [PubMed] [Google Scholar]
- 2.Quatman-Yates CC, Hunter-Giordano A, Shimamura KK, et al. Physical therapy evaluation and treatment after concussion/mild traumatic brain injury. J Orthop Sports Phys Ther . 2020;50(4):CPG1–CPG73. doi: 10.2519/jospt.2020.0301. [DOI] [PubMed] [Google Scholar]
- 3.Manaseer TS, Gross DP, Dennett L, Schneider K, Whittaker JL. Gait deviations associated with concussion: a systematic review. Clin J Sport Med . 2020;30(Suppl 1):S11–S28. doi: 10.1097/JSM.0000000000000537. [DOI] [PubMed] [Google Scholar]
- 4.Fino PC, Parrington L, Pitt W, et al. Detecting gait abnormalities after concussion or mild traumatic brain injury: a systematic review of single-task, dual-task, and complex gait. Gait Posture . 2018;62:157–166. doi: 10.1016/j.gaitpost.2018.03.021. [DOI] [PubMed] [Google Scholar]
- 5.Oldham JR, Difabio MS, Kaminski TW, Dewolf RM, Howell DR, Buckley TA. Efficacy of tandem gait to identify impaired postural control after concussion. Med Sci Sports Exerc . 2018;50(6):1162–1168. doi: 10.1249/MSS.0000000000001540. [DOI] [PubMed] [Google Scholar]
- 6.Howell DR, Osternig LR, Chou LS. Single-task and dual-task tandem gait test performance after concussion. J Sci Med Sport . 2017;20(7):622–626. doi: 10.1016/j.jsams.2016.11.020. [DOI] [PubMed] [Google Scholar]
- 7.Howell DR, Brilliant AN, Meehan WP., 3rd Tandem gait test-retest reliability among healthy child and adolescent athletes. J Athl Train . 2019;54(12):1254–1259. doi: 10.4085/1062-6050-525-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Howell DR, Wilson JC, Brilliant AN, Gardner AJ, Iverson GL, Meehan WP., 3rd Objective clinical tests of dual-task dynamic postural control in youth athletes with concussion. J Sci Med Sport . 2019;22(5):521–525. doi: 10.1016/j.jsams.2018.11.014. [DOI] [PubMed] [Google Scholar]
- 9.Howell DR, Lugade V, Potter MN, Walker G, Wilson JC. A multifaceted and clinically viable paradigm to quantify postural control impairments among adolescents with concussion. Physiol Meas . 2019;40(8):084006. doi: 10.1088/1361-6579/ab3552. [DOI] [PubMed] [Google Scholar]
- 10.McCrory P, Meeuwisse WH, Aubry M, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med . 2013;47(5):250–258. doi: 10.1136/bjsports-2013-092313. [DOI] [PubMed] [Google Scholar]
- 11.Echemendia RJ, Meeuwisse W, McCrory P, et al. The Sport Concussion Assessment Tool 5th Edition (SCAT5): background and rationale. Br J Sports Med . 2017;51(11):848–850. doi: 10.1136/bjsports-2017-097506. [DOI] [PubMed] [Google Scholar]
- 12.Howell DR, Osternig LR, Koester MC, Chou LS. The effect of cognitive task complexity on gait stability in adolescents following concussion. Exp Brain Res . 2014;232(6):1773–1782. doi: 10.1007/s00221-014-3869-1. [DOI] [PubMed] [Google Scholar]
- 13.Sady MD, Vaughan CG, Gioia GA. Psychometric characteristics of the postconcussion symptom inventory in children and adolescents. Arch Clin Neuropsychol . 2014;29(4):348–363. doi: 10.1093/arclin/acu014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Safrit M, Wood TM. Introduction to Measurement in Physical Education and Exercise Science 3rd ed. CV Mosby Co. 71. 1995.
- 15.Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med . 2016;15(2):155–163. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mandrekar JN. Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol . 2010;5(9):1315–1316. doi: 10.1097/JTO.0b013e3181ec173d. [DOI] [PubMed] [Google Scholar]
- 17.Valovich TC, Perrin DH, Gansneder BM. Repeat administration elicits a practice effect with the Balance Error Scoring System but not with the Standardized Assessment of Concussion in high school athletes. J Athl Train . 2003;38(1):51–56. [PMC free article] [PubMed] [Google Scholar]
- 18.Schneiders AG, Sullivan SJ, McCrory PR, et al. The effect of exercise on motor performance tasks used in the neurological assessment of sports-related concussion. Br J Sports Med . 2008;42(12):1011–1013. doi: 10.1136/bjsm.2007.041665. [DOI] [PubMed] [Google Scholar]
- 19.Brilliant AN, Meehan WP, 3rd, Howell DR. Static and dynamic cognitive performance in youth and collegiate athletes with concussion. Clin J Sport Med . 2021;31(5):442–447. doi: 10.1097/JSM.0000000000000779. [DOI] [PubMed] [Google Scholar]


