The worldwide burden of adult cardiometabolic diseases such as hypertension, diabetes, obesity, and dyslipidaemia continues its relentless increase. Scaling up the prevention, management, and control of cardiometabolic diseases is cost-effective but requires strong health systems.1 As we have previously argued in this journal,2 building these health systems requires data that is accurate, timely, and transparent. Data from high-quality population-based surveys are particularly essential, as they reflect the spectrum of adults living in communities, including those who are not reached by their health system.
Tremendous progress has been made in making population-based survey data on cardiometabolic diseases available; for example, the release of the WHO Non-communicable Disease (NCD) Microdata Repository in 2018. This repository hosts over 130 surveys conducted with the WHO Stepwise Approach to NCD Risk Factor Surveillance (STEPS) methodology. These surveys are now available to researchers after a brief application. Most STEPS surveys are conducted in low-income and middle-income countries (LMICs), where a the vast majority of the cardiometabolic disease burden occurs.3 Therefore, this repository fills a crucial gap in openly accessible, population-based survey data on cardiometabolic risk factors and health-care access in LMICs.
Despite this progress, more work is needed. Although necessary, the availability of population-based data is insufficient by itself to ensure effective use of the data to shape programmes, strategies, and policies that address cardiometabolic diseases. In this Comment, we highlight three other important actions needed to maximise the use of population data: harmonisation, alignment with monitoring indicators to benchmark health system performance, and capacity-building initiatives to democratise data use by giving people the tools to use the data (figure).
Figure:
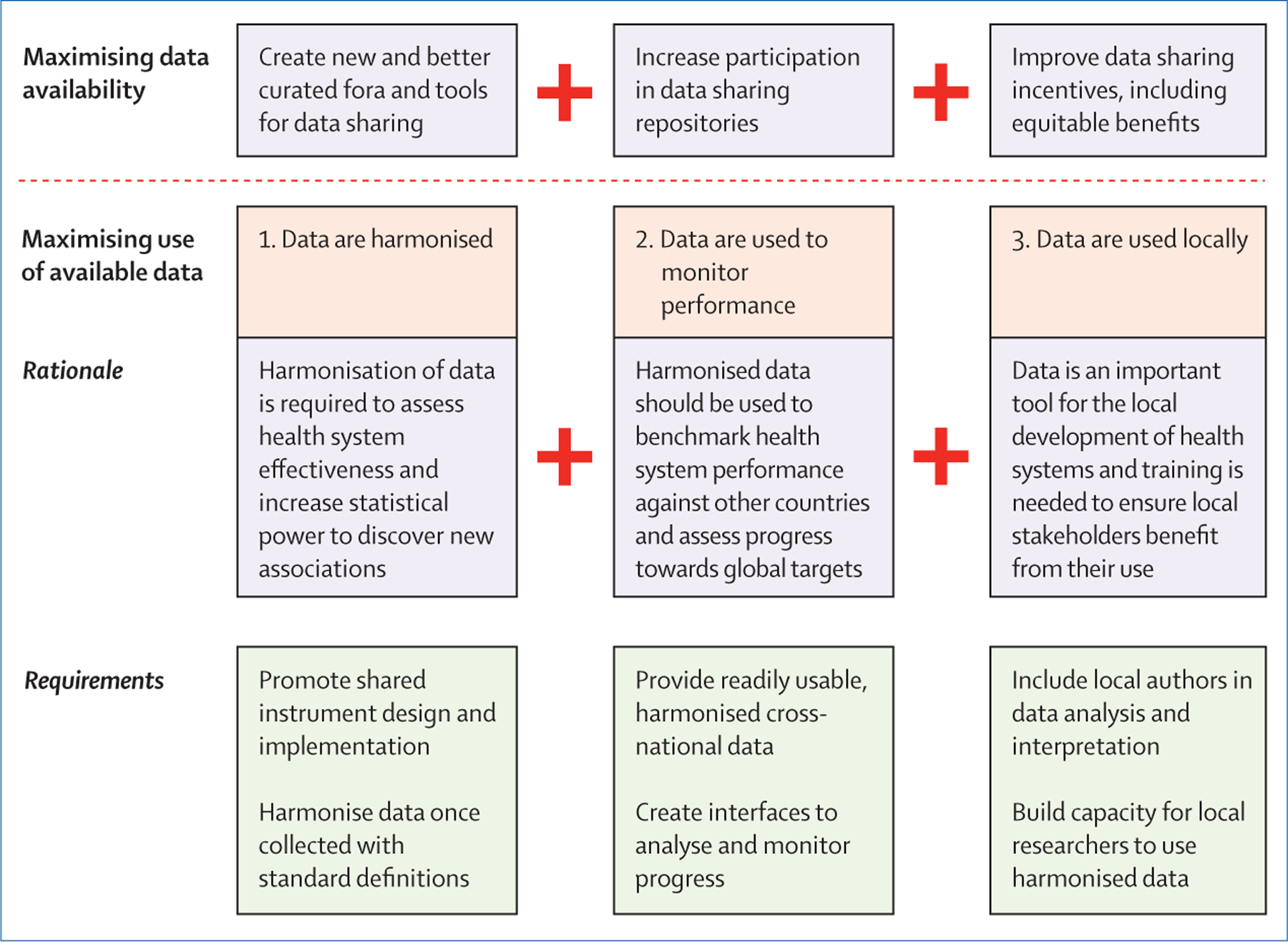
Steps to maximising data availability and its use.
Our perspective is informed by our experience as collaborators in the Global Health and Population Project on Access to Care for Cardiometabolic Diseases (HPACC), an international research consortium. The HPACC has collaborators in more than 30 countries and represents 1∙3 million individuals, including more than 50 STEPS surveys.
First, although population-based data should be used at the national level, these data should also be harmonised to maximise use by international advocacy organisations, policymakers, and researchers. Harmonisation refers to the process of bringing distinct data sources together in a single comparable format. Harmonised data are available for maternal and child health surveys, but not for cardiometabolic diseases. Harmonised data allows assessment of health system effectiveness, as our study on the state of hypertension care in 44 LMICs illustrates.4 Harmonisation increases the size and diversity of samples, giving added power to study variations in cardiometabolic risk factors. These variations include biological risk factors such as blood glucose concentration and behavioural risk factors such as physical activity and diet. Understanding these variations is important, as the epidemiological patterns of risk factors of clinical relevance observed in well-studied, high-income countries might not be conserved in LMICs. Indeed, we have found that the association between diabetes and BMI is highly variable across world regions and suggests that BMI thresholds generated with European or North American data cannot be applied elsewhere.5 Harmonisation also allows for the construction of sophisticated clinical and policy models to predict effects of change in risk factor prevention or management.1,6 Importantly, to ensure data are useful for cross-country comparisons, survey instruments and data collection methods should be standardised and aligned with the highest-priority global health metrics, for example those in the Sustainable Development Goals, before data collection.
Second, population data on cardiometabolic diseases should be used to benchmark and monitor health system performance. At present, these data are underutilised for this purpose. Harmonised data from STEPS surveys and similar surveys can reveal progress on the monitoring of indicators in the WHO NCD Global Monitoring Framework. Harmonised data can also inform new targets such as those proposed by the WHO Global Diabetes Compact, a recently established initiative to improve global diabetes care.7 To show global variation in health system performance, harmonised data from high-income countries should be included as well as from LMICs, although we acknowledge that data from high-income countries are currently less available.
Third, there is a need to build capacity of local researchers and policy-makers in LMICs to ensure the wide usability of population data on cardiometabolic diseases by people in the countries in which it was collected. Local researchers—especially those in LMICs—who design and conduct surveys should be empowered to use harmonised population data to answer policy-relevant questions, conduct independent analyses, and publish in lead-author roles.8 In addition to this harmonisation being a step towards decolonising global health, local collaborators that use this data can provide contextual interpretation for results that might not be fully understood by individuals outside their settings.
Although this Comment focuses on maximising use of available population data on cardiometabolic diseases, data sharing efforts also need to be improved and continued. Many STEPS and comparable household surveys remain unavailable, as do more than 20 nationally representative health facility surveys conducted using the WHO Service Availability Readiness Assessment (SARA) methodology.9 Many other data sources, for example, from subnational research studies, also remain inaccessible. Furthermore, cardiometabolic disease epidemiology is rapidly evolving, but data is often outdated as it is not regularly collected. As is the case for HIV, data collection for cardiometabolic diseases needs to be ongoing to assess temporal trends in disease prevalence and health system performance.
The staggering burden of cardiometabolic diseases brings an imperative to maximise the use of population-based data. These data are a global, public good, with many countries and individuals investing substantial resources in their production. However, although the data are increasingly available, in practice they remain too sparse and underutilised given the toll of these diseases on populations worldwide. We call on funders and international health organisations to invest in efforts to collect, harmonise, and make these data available with an urgency reflecting the global burden of cardiometabolic diseases.
Supplementary Material
Acknowledgments
No support was received for writing this manuscript. Authors declare the following support or relationships within 36 months of submitting the work. DF reports a Pilot and Feasibility Grant funded by the Michigan Center for Diabetes Translational Research (US National Institutes of Health grant P30-DK092926) and a grant from the Swinmurn Foundation to implement a sustainable diabetes clinic in Guatemala. DF also reports volunteer affiliations with Wuqu’ Kawoq and GlucoSalud. DF has received research fellowship funding from the National Clinician Scholars Program at the University of Michigan Institute for Healthcare Policy and Innovation. TB reports grants from the Alexander von Humboldt Foundation, Wellcome Trust, and US National Institutes of Health. RA reports contracts with Novo Nordisk, the Union for International Cancer Control, Novo Nordisk, Hoffman-La Roche, and Sloan Memorial Kettering Hospital. RA also reports payments or honorario from Merck and Hoffmann-La Roche. JD reports grants from UK MRC and National Institute for Health Research, and US National Institute of Health. All other authors declare no competing interests.
Footnotes
For the harmonised international survey data on maternal, child, and reproductive health see https://globalhealth.ipums.org/
For the WHO NCD Microdata Repository see https://extranet.who.int/ncdsmicrodata/index.php/catalog
For more on WHO NCD Global Monitoring Framework see https://www.who.int/teams/ncds/surveillance/monitoring-capacity/gmf
References
- 1.Basu S, Flood D, Geldsetzer P, et al. Estimated impact of increased diagnosis, treatment, and control of diabetes mellitus among low-and middle-income countries: a microsimulation model. Lancet Glob Health 2021; 9: e1539–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davies J, Yudkin JS, Atun R. Liberating data: the crucial weapon in the fight against NCDs. Lancet Diabetes Endocrinol 2016; 4: 197–8. [DOI] [PubMed] [Google Scholar]
- 3.GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020. 396: 1223–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Geldsetzer P, Manne-Goehler J, Marcus ME, et al. The state of hypertension care in 44 low-income and middle-income countries: a cross-sectional study of nationally representative individual-level data from 1∙1 million adults. Lancet 2019; 394: 652–62. [DOI] [PubMed] [Google Scholar]
- 5.Teufel F, Seiglie JA, Geldsetzer P, et al. Body-mass index and diabetes risk in 57 low-income and middle-income countries: a cross-sectional study of nationally representative, individual-level data in 685 616 adults. Lancet 2021; 398: 238–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO. Noncommunicable Diseases Global Monitoring Framework: Indicator Definitions and Specifications. 2014. https://www.who.int/nmh/ncd-tools/indicators/GMF_Indicator_Definitions_Version_NOV2014.pdf (accessed Sept 29, 2021).
- 7.Hunt D, Hemmingsen B, Matzke A, et al. The WHO Global Diabetes Compact: a new initiative to support people living with diabetes. Lancet Diabetes Endocrinol 2021; 9: 325–7. [DOI] [PubMed] [Google Scholar]
- 8.Wang W, Assaf S, Pullum T, Kishor S. The Demographic and Health Surveys Faculty Fellows Program: Successes, Challenges, and Lessons Learned. Glob Health Sci Pract 2021; 9: 390–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mangipudi S, Leather A, Seedat A, Davies J. Oxygen availability in sub-Saharan African countries: a call for data to inform service delivery. Lancet Glob Health 2020; 8: e1123–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


