ABSTRACT
Bowel perforation of biliary stents is a rare complication of biliary stenting. We report the successful endoscopic treatment of a 78-year-old man with a straight biliary plastic stent perforating the ascending colon without underlying structural abnormality in the affected segment. Perforation was detected incidentally during computed tomography; the patient had been under continued antibiotic therapy for liver abscess. Stent extraction was performed by using an endoscopic snare; the site of perforation was closed with through-the-scope clips. The patient remained asymptomatic. In addition, we reviewed published cases of perforated biliary stents and outlined that most perforations are caused by straight plastic stents.
KEYWORDS: biliary stent, perforation, endoscopic treatment
INTRODUCTION
Biliary stenting is a common procedure to treat a variety of benign and malignant conditions, most notably common bile duct stones, acute cholangitis, and benign or malignant strictures of the common bile duct. Stent migration occurs in 3%–21%1–5 of patients, the rate being highly dependent on the etiology of the stricture, stent type used, and length of follow-up. Although stent migration is not uncommon, serious complications due to this are rare. Duodenal perforation vis-à-vis of the papilla by straight biliary stents ranges from 1 in 2,2936 to 2.1%.7 The majority was managed with endoscopic removal and closure, with however high mortality (3 of 116 vs 4 of 13 cases7). While migration to unusual sites, such as the pericardium,8–10 bronchial system,11 and perforation of small bowel,12,13 is limited to few case reports, colonic perforation has been reported in 32 cases since 2000 (Table 1), with only 5 cases outside the rectosigmoid colon, in which most perforations occurred because of impaction in thin-walled diverticula.
Table 1.
Reported colonic perforations of biliary stents from 2000
| Year | Author | Indication for ERCP | Stent | Location | Manifestation | Treatment | Outcome |
| 2000 14 | Størkson | Malignant stenosis | Straight | Ileum | Pain/abscess | Laparotomy | Died after surgery |
| 200014 | Størkson | CBD stone/cholangitis | Straight | Sigmoid | Pain/free perforation | Surgical primary closure | Uneventful |
| 200114 | Figueiras | Benign stricture | Straight | Left flexure | Cutaneous fistula | Removal through colocutaneous fistula | Uneventful |
| 200114 | Klein | CBD stone | Straight | Sigmoid | Pain/peritonitis | Surgery | Uneventful |
| 200314 | Elliott | CBD stone/cholangitis | Straight | Sigmoid | Pain/ileus | Hartmann procedure | Uneventful |
| 200314 | Diller | Benign stricture | Straight | Sigmoid | Asymptomatic | Endoscopic removal and sigmoidectomy | Perforation after endoscopic removal |
| 200314 | Wilhelm | CBD stone | Straight | Sigmoid | Pneumaturia/enterovesical fistula | Sigmoidectomy | Uneventful |
| 200315 | Cerisoli | Postoperative bile leakage | Straight | Cecum | Pain/serosa not perforated | Cecotomy | Uneventful |
| 200416 | Blake | CBD stone | Straight | Sigmoid | Colovaginal fistula | Low anterior resection | Uneventful |
| 200714 | Anderson | CBD stone | Straight | Sigmoid | Pain/abscess | Endoscopic removal | Uneventful |
| 200714 | Namdar | Postoperative bile leakage | Straight | Rectum | Pain/peritonitis | Rectal resection | Uneventful |
| 200917 | Brinkley | Malignant stenosis | Straight | Right flexure | Fever/abscess | Percutaneous removal | Uneventful |
| 201114 | Jafferbhoy | Postoperative bile leakage | Straight | Sigmoid | Pain w/o peritonitis | Endoscopic removal and clip closure | Uneventful |
| 201114 | Lankisch | Malignant stenosis | Straight | Sigmoid | Pain/abscess | Surgery | Uneventful |
| 201114 | Malgras | Malignant stenosis | Straight | Sigmoid | Pain/peritonitis | Hartmann procedure | N/A |
| 201214 | Alcaide | CBD stone/stricture | Straight | Sigmoid | Pain/peritonitis | Endoscopic removal and clip closure | Abscess (day 5, treated with antibiotics) |
| 201218 | Depuydt | Post-LT bile duct stricture | Straight | Rectum | Fever/minimal perirectal inflammation | Peranal stent removal | Uneventful |
| 201314 | Jones | Benign stricture | Straight | Cecum | Pain/no peritonitis | Endoscopic removal | Uneventful |
| 201614 | Chittleborough | CBD stone/cholangitis | Straight | Sigmoid | Sepsis/peritonitis | Hartmann procedure | Prolonged ileus, discharged after 18 d |
| 201714,19 | Siaperas | Postoperative CBD stricture | Straight | Sigmoid | Pain/peritonitis | Hartmann procedure with colostomy | Uneventful |
| 201819 | Cano-Hoz | CBD stone/stricture | Straight | Sigmoid | Fever/hydronephrosis | Endoscopic removal and clip closure | Uneventful |
| 201914 | Riccardi | CBD stone | Straight | Sigmoid | Pain/peritonitis | Hartmann procedure with colostomy | Perioperative NSTEMI |
| 201920 | Ramani | CBD stone | Straight | Sigmoid | Pain/impaction in sacral foramen | Endoscopic removal | Uneventful |
| 202014 | Marcos | CBD stone | Straight | Sigmoid | Asymptomatic | Surgical primary closure | N/A |
| 202114 | Pengermä | Benign stricture | Straight | Appendix | Pain/appendicitis | Appendectomy | Abscess (day 10, treated with antibiotics) |
| 202114 | Tao | CBD stone/cholangitis | Straight | Sigmoid | Pain/free perforation | Sigmoidectomy + colostomy | Uneventful |
| 202114 | Park | CBD stone/cholangitis | Straight | Left colon | Pain/localized peritonitis | Right hemicolectomy | Uneventful |
| 201114 | Wagemakers | CBD stone | N/A | Sigmoid | Urinary tract infection/enterovesical fistula | Sigmoidectomy | Uneventful |
| 201514 | Mady | Malignant stenosis | N/A | Sigmoid | Sepsis/abscess | Hartmann procedure | Died from MOF |
| 201514 | Virgilio | CBD stone | N/A | Sigmoid | Pain/covered perforation | Endoscopic removal | N/A |
| 201514 | Virgilio | CBD stone | N/A | Sigmoid | Pain/free perforation | Hartmann procedure | N/A |
| 201714 | Chou | CBD stone | N/A | Sigmoid | Asymptomatic | Endoscopic removal and clip closure | Uneventful |
| 201014 | Bagul | Benign stricture | Pigtail | Sigmoid | Pain and groin abscess | Abscess exploration and stent removal | Uneventful |
CBD, common bile duct; ERCP, endoscopic retrograde cholangiopancreatography; LT, liver transplantation; MOF, multiple organ failure; N/A, not available; NSTEMI, non-ST segment elevation myocardial infarction; op, operation.
CASE REPORT
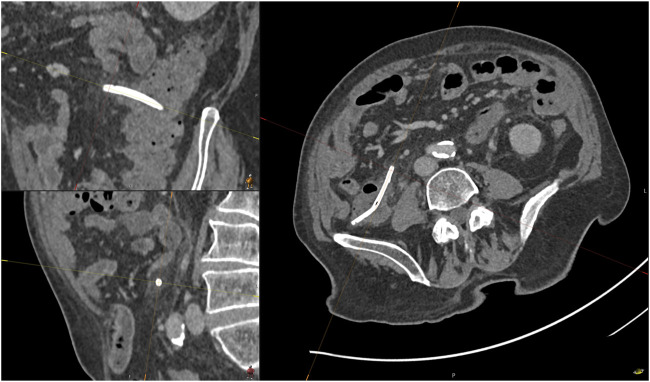
A 78-year-old man underwent scheduled abdominal computed tomography during a follow-up of liver abscess diagnosed 1 month earlier. Colon perforation due to a migrated stent in the ascending colon was suspected with the stent protruding 3 cm beyond the colonic lumen and surrounding fat imbibition while no free air was detected (Figure 1). The patient was without symptoms and afebrile, and the abdominal examination was without tenderness or localized resistance. His laboratory results showed no leukocytosis, but mild C-reactive protein elevation (19.7 mg/L, reference: <10).
Figure 1.
Computed tomography showing perforation of the ascending colon.
One month before colonic perforation, the patient underwent urgent endoscopic retrograde cholangiography with endoscopic papillotomy and placing of a straight biliary stent because of ascending cholangitis with worsening sepsis complicated by polymicrobial liver abscess and severe pancreatitis with disseminated intravasal coagulation and portal vein thrombosis. Choledocholithiasis was neither present on magnetic resonance imaging conducted 3 days earlier nor noted during endoscopic retrograde cholangiopancreatography. After stent placement, fever resolved within 3 days; jaundice had not been present. His course was complicated by vancomycin-associated acute kidney injury. He was discharged after de-escalation of antibiotic therapy 16 days after stent placement. At the time of colonic perforation, he was still on antibiotic therapy with linezolid and amoxicillin/clavulanic acid as the ongoing treatment of liver abscess; he had remained asymptomatic since discharge.
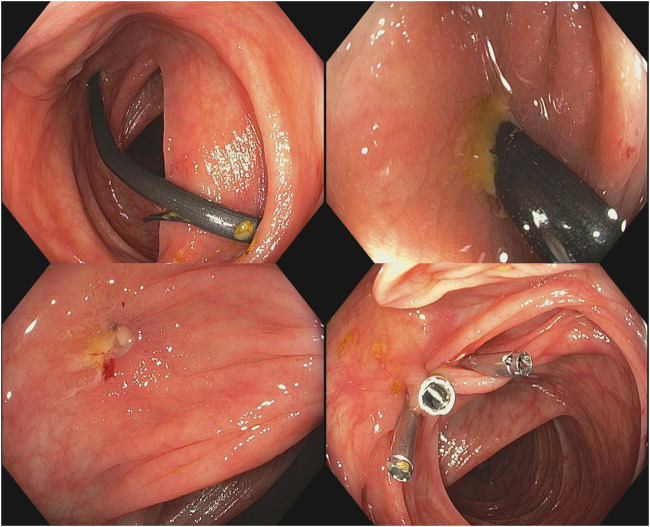
During colonoscopy, the stent was found to be lodged transversely in the ascending colon, penetrating the bowel wall with one end of the flap not visible; near the other end, a superficial, fibrin-covered ulceration was present (Figure 2). The stent was retrieved with a snare; the site of perforation showed only traces of purulent discharge and was closed with 3 through-the-scope metal clips. Antibiotic therapy was continued for 1 week after removal of the stent, and the patient remained asymptomatic on follow-up (Figures 3 and 4).
Figure 2.
Endoscopic removal of the affected biliary stent.
Figure 3.
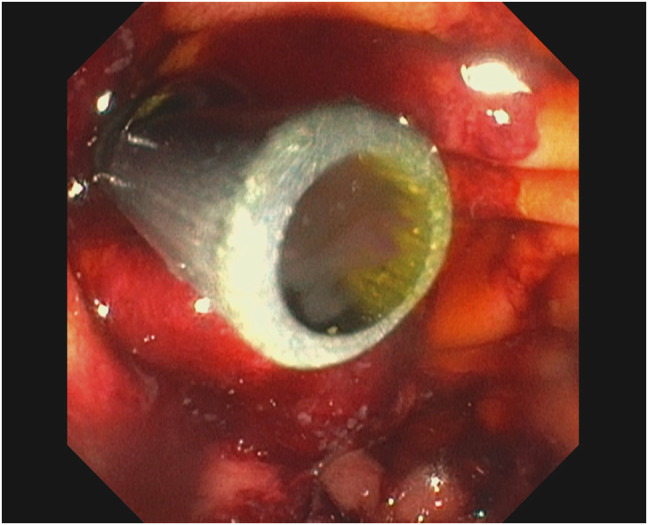
Duodenoscopic view of the biliary stent.
Figure 4.
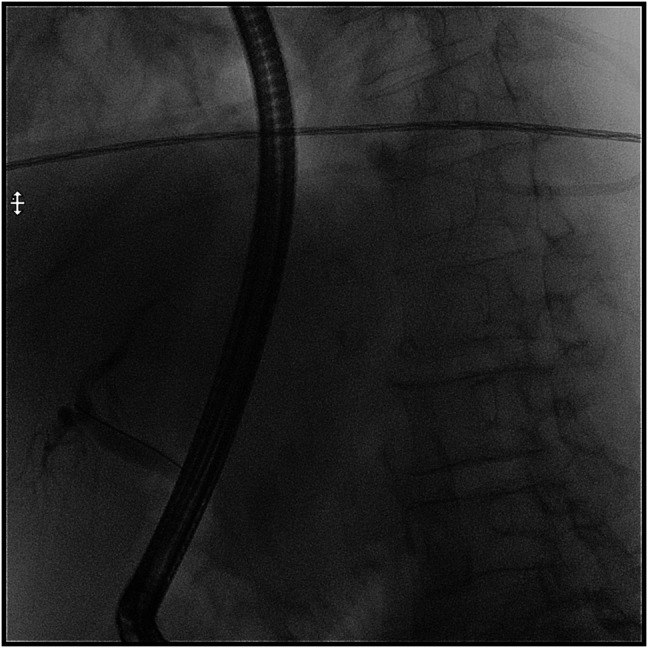
Cholangiogram during endoscopic retrograde cholangiopancreatography.
DISCUSSION
Our patient benefited from the incidental discovery of his asymptomatic colonic perforation and from being on broad-spectrum antibiotic therapy for his liver abscess. Owing to the absence of clinical and radiographic signs of peritonitis, we deemed endoscopic removal to be the appropriate therapy, in accordance with previous reports that demonstrated successful endoscopic treatment in the absence of peritonitis or penetration of other organs, in which case surgery is required. To our knowledge, this case is the first reported colonic perforation of a biliary plastic stent outside anatomically predisposed sites, such as diverticula or colonic flexures, and shows feasibility of endoscopic removal and closure of the fistula in an asymptomatic patient.
Colonic perforation is a rare complication of biliary stenting. Reviewing reported cases of colonic perforations of biliary stents from 2000 to 2022 (Table 1), we found that unlike in duodenal perforation, which carries a high risk of mortality,6,7 mortality in reported cases of colonic perforation is low (1 of 32). Of note, only 1 perforation was confirmed to be due to a pigtail stent while 31 of 32 perforations were caused by straight stents (25 of 32) or the type of stent was not mentioned (5 of 32). Nevertheless, colonic perforation was associated with additional interventions and hospital-prolonged hospital stay. Most cases were managed surgically (20 of 32), and endoscopic therapy was performed in 10 of 32 cases; 2 stents were removed through a colocutaneous fistula. Of those treated endoscopically, 1 patient developed a small abscess that was successfully treated conservatively and 1 patient had a colonic perforation after stent removal and required surgery. Mortality in colonic perforations seems to be low (1 of 32).
The almost exclusive causation of colonic and duodenal perforations by straight plastic stents should be kept in mind when choosing a biliary stent, and risk factors of stent migration should be considered. Whether reported higher rates of migration in pigtail stents3 is compensated for by less complications from perforation remains unclear. Consequent follow-up of implanted stents until their removal or excretion is documented should be assured by keeping records of implanted stents.
DISCLOSURES
Author contributions: F. Rybinski: endoscopy and care of the patient, drafting of the manuscript, and is the article guarantor. H. Heinrich: endoscopy supervision and drafting of the manuscript. M. Zimmerli: review of the literature and revision of the manuscript. S. Kahl: revision of the manuscript.
Financial disclosure: None to report.
Previous presentations: Accepted abstract for poster presentation: 52. Annual conference of the German Society for Endoscopy and Imaging Procedures; March 1–3, 2023; Cologne, Germany. Submitted abstract for poster presentation: ESGE Days; April 20–22, 2023; Dublin, Ireland.
Informed consent was obtained for this case report.
Contributor Information
Henriette Heinrich, Email: henriettesophie.heinrich@clarunis.ch.
Marius Zimmerli, Email: marius.zimmerli@clarunis.ch.
Stefan Kahl, Email: stefan.kahl@clarunis.ch.
REFERENCES
- 1.Arhan M, Odemiş B, Parlak E, et al. Migration of biliary plastic stents: Experience of a tertiary center. Surg Endosc. 2009;23:769–75. [DOI] [PubMed] [Google Scholar]
- 2.Emara MH, Ahmed MH, Mohammed AS, et al. Biliary stent migration: Why, how, and what? Eur J Gastroenterol Hepatol. 2021;33:967–73. [DOI] [PubMed] [Google Scholar]
- 3.Paspatis GA, Papastergiou V, Mpitouli A, et al. Distal biliary stent migration in patients with irretrievable bile duct stones: Long-term comparison between straight and double-pigtail stents. Dig Dis Sci. 2022;67:4557–64. [DOI] [PubMed] [Google Scholar]
- 4.Taj MA, Ghazanfar S, Qureshi S, et al. Plastic stent migration in ERCP; a tertiary care experience. J Pak Med Assoc. 2019;69:1099–102. [PubMed] [Google Scholar]
- 5.Katsinelos P, Kountouras J, Paroutoglou G, et al. Migration of plastic biliary stents and endoscopic retrieval: An experience of three referral centers. Surg Laparosc Endosc Percutan Tech. 2009;19:217–21. [DOI] [PubMed] [Google Scholar]
- 6.Gromski MA, Bick BL, Vega D, et al. A rare complication of ERCP: Duodenal perforation due to biliary stent migration. Endosc Int Open. 2020;8:E1530–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stassen PMC, Jong DMde, Poley J-W, et al. Prevalence of and risk factors for stent migration-induced duodenal perforation. Endosc Int Open. 2021;9:E461–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee V, Woldman S, Meier P. Biliary stent migration as a cause of cardiac tamponade. J Cardiovasc Med (Hagerstown). 2013;14:750–2. [DOI] [PubMed] [Google Scholar]
- 9.Simeon K, Wright A, Browne V. Cardiac tamponade and septic pericarditis caused by biliary stent migration. Am J Emerg Med. 2022;63:181.e1–3. [DOI] [PubMed] [Google Scholar]
- 10.Chao HY, Li CH, Chen SY. Bacterial pericarditis caused by penetration of a migrated biliary stent from the lateral segment of the liver: A case report. Medicina (Kaunas). 2022;58:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Queirós T, Castro B, Ferreira A, et al. Bronchobiliary fistula after stenting of biliary duct as the management of iatrogenic bile duct injury during elective cholecystectomy. Acta Chir Belg. 2022;2022:1–6. [DOI] [PubMed] [Google Scholar]
- 12.Barranco Castro D, Aparcero López R, Domínguez Amodeo A, et al. Biliary stent migration as a rare cause of ileal perforation. Rev Esp Enferm Dig. 2022;13:54–5. [DOI] [PubMed] [Google Scholar]
- 13.Zorbas KA, Ashmeade S, Lois W, et al. Small bowel perforation from a migrated biliary stent: A case report and review of literature. World J Gastrointest Endosc. 2021;13:543–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park TY, Hong SW, Oh H-C, et al. Colonic diverticular perforation by a migrated biliary stent: A case report with literature review. Medicine (Baltimore). 2021;100:e28392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cerisoli C, Diez J, Giménez M, et al. Implantation of migrated biliary stents in the digestive tract. HPB (Oxford). 2003;5:180–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blake A-M, Monga N, Dunn EM. Biliary stent causing colovaginal fistula: Case report. JSLS. 2004;8:73–5. [PMC free article] [PubMed] [Google Scholar]
- 17.Brinkley M, Wible BC, Hong K, et al. Colonic perforation by a percutaneously displaced biliary stent: Report of a case and a review of current practice. J Vasc Interv Radiol. 2009;20:680–3. [DOI] [PubMed] [Google Scholar]
- 18.Depuydt P, Aerts R, van Steenbergen W, et al. An unusual case of rectal perforation after liver transplantation. Acta Chir Belg. 2012;112:232–3. [PubMed] [Google Scholar]
- 19.Cano-Hoz M, Carrascosa MF, Pérez AD, et al. Migrated biliary stent. Lancet Gastroenterol Hepatol. 2018;3:288. [DOI] [PubMed] [Google Scholar]
- 20.Ramani AS, Mandrekar S, Samant D, et al. An unusual case of biliary stent migration in sacrum. Niger J Surg. 2019;25:104–6. [DOI] [PMC free article] [PubMed] [Google Scholar]