Abstract
Background
In response to a growing cancer burden and need for improved coordination among stakeholders in Kenya, the US National Cancer Institute and the Kenya Ministry of Health collaboratively hosted a stakeholder meeting in 2014 which identified four priority areas of need (research capacity building, pathology and cancer registries, cancer awareness and education, and health system strengthening) and developed corresponding action plans.
Methods
Surveys were conducted with participants to collect input on the progress and impact of the 2014 stakeholder meeting.
Findings
Of 69 eligible participants, 45 responded from academia, healthcare institutions, civil society, government, and international agencies. Of the four technical focus areas, three have continued to conduct working group meetings and two have conducted in-person meetings to review and update their respective action plans. Accomplishments linked to or enhanced by t meeting include: Kenyan and international support for expansion of population-based cancer registries, increased availability of prioritized diagnostic tests in selected regional referral hospitals, a greater focus on development of a national cancer research agenda, strategic planning for a community education strategy for cancer awareness, and improved coordination of partners through in-country technical assistance.
Interpretation
The Stakeholder Program has successfully united individuals and organizations to improve cancer control planning in Kenya, and has enhanced existing efforts and programs across the country. This model of partners working in parallel on prioritized track activities has supported development of long term coordination of cancer research and control activities sustainable by the Kenyan government and Kenyan institutions.
Keywords: Health Planning, Health Policy, Kenya, Pathology, Registries, Community Health Education
Introduction
The increasing burden of non-communicable diseases (NCDs) presents a global health challenge. In particular, cancer incidence is expected to rise by 70% in the next 20 years, with a majority of cases occurring in low-and middle-income countries [1]. Consequently, countries need to begin shifting resources toward this imminent burden [2]. In Kenya, many institutions including the Ministry of Health (MoH), academia, civil society, the US Government (the US National Institutes of Health, Centers for Disease Control and Prevention, and US Agency for International Development), and international partners, have been working to address this public health issue, but more efforts are needed to increase integration with Kenya’s National Cancer Control Strategy (NCCS) [3].
To improve coordination among cancer-related stakeholders in Kenya, the US National Cancer Institute (NCI)’ s Center for Global Health (CGH) and the MoH hosted a two-day workshop in 2014 [4]. The meeting focused around three primary objectives: (1) to foster a network of incountry contacts; (2) to leverage infrastructure and relationships to improve alignment with the MoH and implementation of the NCCS; and (3) to integrate NCI and global cancer control efforts into MoH priorities.
Stakeholders in Kenya identified four areas critical to advancing cancer control and care, which provided the structure for grouping participants within their areas of expertise: research capacity building (Track 1), pathology and cancer registries (Track 2), cancer awareness and education (Track 3), and health system strengthening (Track 4). The program intentionally drew stakeholders from different sectors, to ensure useful dialogue and outputs that ultimately implemented the goals of the NCCS nation-wide.
The two-day meeting has evolved into the Stakeholder Program, a bi-lateral partnership between the NCI and the Government of Kenya to accelerate implementation of the action plans of each technical working group (TWG) (Figure 1). This has included an NCI-supported technical advisor to the MoH and the recently inaugurated National Cancer Institute of Kenya (I), as well as support for specific projects. Nearing the three-year mark of bilateral engagement, NCI initiated an evaluation of the program to gauge progress and to assess the Stakeholder Program model as a means of NCI investment toward cancer research and control in a partner country.
Figure 1.
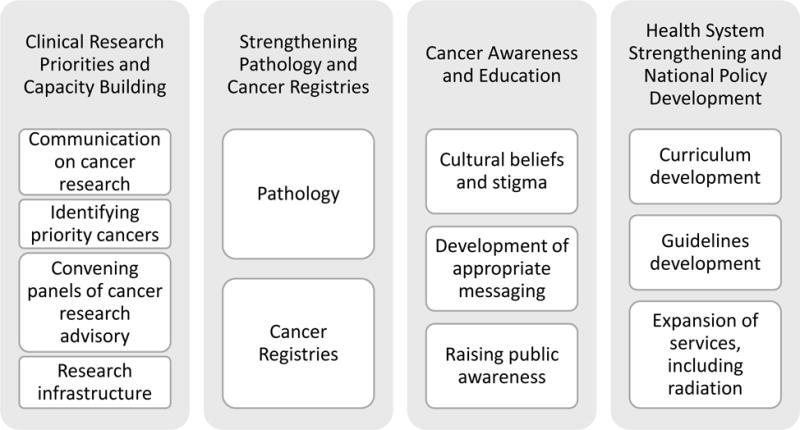
Technical working groups and respective subtopics
Methodology
NCI developed a set of survey questions to address the three key objectives of the meeting and the activities of the four technical tracks. Two survey instruments were used, one for Kenyan MoH participants (13 questions: 8 closed-ended, 5 open-ended) and one for non-MoH participants (27 questions: 18 closed-ended, 9 open-ended), to assess the degree of strategic alignment between the groups. Questions on both surveys addressed activities completed since the 2014 meeting, scope of partnerships formed through the program, progress on action plan implementation, alignment between MoH and non-MoH partners, and successes and challenges of the program. Both surveys were developed using Questionnaire Development System (QDS, NOVA Research, v3.0), which were administered through a web-link sent to stakeholders by email. As CGH was the primary funder of the 2014 meeting, CGH staff members were excluded from participation in the survey. Data collection took place during a five-week period, with follow-up at two, three, and four weeks. After closure of the web-based survey, a CGH staff member conducted semi-structured face-to-face and telephone interviews with nonrespondents, using the same survey questions administered in the web version. Stakeholders from the 2014 meeting who are active in at least one of the four technical tracks or currently holding positions relating to cancer were prioritized for these follow-ups.
Two CGH staff members used thematic coding to analyze responses to each open-ended question. After review, the open-ended questions were coded according to major thematic categories by using a combined inductive/deductive approach based upon the objectives of the program and common areas of interest that arose from the data. A team of reviewers examined the codes to determine the final set of themes.
Results
In total, 54 Kenyan (13 MoH, 41 non-MoH) and 15 international participants were eligible to be surveyed. Of those, 33 Kenyan (9 MoH, 24 non-MoH) and 12 international participants responded in the evaluation (Table 2), for an overall response rate of 65%.
Table 2.
Survey responses
| Kenyan | Foreign | Total | ||
|---|---|---|---|---|
| MoH | Non-MoH | |||
| Eligible survey recipients | 13 | 41 | 15 | 69 |
| Total respondents | 9 (69%) | 24 (59%) | 12 (80%) | 45 (65%) |
| Self-administered | 4 (44%) | 18 (75%) | 10 (84%) | 32 (71%) |
| Interviewer-administered (phone) | 0 (0%) | 2 (8%) | 1 (8%) | 3 (7%) |
| Interviewer-administered (in person) | 5 (55%) | 4 (17%) | 1 (8%) | 10 (22%) |
| Non-respondents | 4 (31%) | 17 (36%) | 3 (20%) | 24 (35%) |
Evaluation of Meeting Objectives
(1) To foster a network of in-country contacts, and (2) to leverage infrastructure and relationships to improve alignment with the MoH and implementation of the NCCS
Success of the first two meeting objectives was assessed in part by the number and types of new partnerships that stakeholders formed as a result of the meeting. Of the 45 respondents, 35 (77%) reported forming at least one new partnership. The partnerships described were commonly cross-sector, many being across public and private institutions. For non-MoH partners, the extent to which new relationships were formed with MoH stakeholders reflected both a stronger network and an increased alignment with the MoH. Of the 36 non-MoH respondents, 26 (72%) stated that the meeting increased their level of interaction with the MoH, reflecting both a stronger network and increased alignment with MoH priorities. Specifically, the meeting allowed the relationship with the MoH to be “more focused and intense, and more productive—less combative and more collaborative.” Many participants noted that the meeting yielded a “strong synergy” between MoH and non-MoH stakeholders, with non-MoH respondents reporting that the interest and active involvement of MoH officials engendered a sense of confidence in being viewed as partners in cancer control efforts, and that the government considers cancer an important issue. The utility of the technical track structure of the program was also viewed as a success. With key guiding principles for cancer control that include “ownership, partnership, coordination, systematic and integrated approach” [3], the NCCS itself was enhanced by this stakeholders meeting and subsequent engagement of stakeholders within the technical tracks.
As cancer is addressed by multiple MoH units (NCD, Reproductive Health, Oncology, and Health Promotion), strengthening relationships within the MoH is another important aspect of fostering an effective incountry network. Redeployment within the Kenyan government is another barrier to coordination within the MoH: of the thirteen MoH participants at the 2014 meeting, five have transitioned to new positions, some outside of cancer or outside of the MoH entirely. Because of this reality, partnerships at the organizational level, not only among individuals, are crucial to the strength of the in-country network and the continuity of efforts.
“Partners (are) very important for the MoH. Over time, different partners have different strengths and different mandates, and not everyone can do (the same) thing. Consensus takes time but once you have it, you move at very fast speed.”-Kenyan-based MoH respondent
Following the meeting, several specific projects were cited as examples of improved coordination between stakeholders and the MoH. Examples include: enhanced cancer registry efforts broadly, specific support for the Kisumu registry, the building of a national registry, and the expansion of efforts to create Cancer Centers of Excellence. Another example cited was the Epidemiology of Burkitt Lymphoma in East-African Children and Minors (EMBLEM) study [5]. EMBLEM was a case-control epidemiological study of Burkitt Lymphoma that required collaboration between the NGO, Academic Model Providing Access to Healthcare (AMPATH) [6], and the MoH to expand cancer care capacity at participating hospitals.
(3) Integration of NCI and US government (USG) cancer control efforts into MoH priorities
The formation of the technical tracks also successfully formalized the connectivity between MoH and non-MoH stakeholders, including NCI and USG stakeholders. The track structure was subsequently formalized into a set of MoH Technical Working Groups (TWGs). These TWGs now function as a framework for the MoH to engage with non-MoH stakeholders on national cancer priorities (Figure 1). Furthermore, the track structure serves as a forum for stakeholders to address and update one another and the MoH on their ongoing activities. Following the 2014 meeting, NCI and the MoH recognized that dedicated staff time was needed to solidify the track structure into the TWGs. In response, the NCI supported a technical advisor to sit within the MoH and facilitate and sustain progress of the TWGs. As the TWG framework becomes more standardized and self-sustaining, the focus of this advisory role will shift to strategy and policy level considerations.
Evaluation of the Stakeholder Program: Progress of Technical Tracks
Track 1
Track 1, Clinical Research Priorities and Capacity Building, was established to increase capacity for oncology research in Kenya. Following the meeting, an advisory board was established to set specific priorities. In December 2015, the working group initiated an in-person meeting and launched four priority areas: channels of communication for cancer research; cancer research advisory; convening panels for priority cancers; and resource mobilization for cancer research. Specific activities within Track 1 are highlighted in Table 3.
Table 3.
Progress across the four technical tracks since 2014
| Track | Progress in Kenya to-date | Long term goals |
|---|---|---|
| Track 1: Clinical research priorities and capacity building |
|
|
| Track 2a: Pathology |
|
|
| Track 2b: Cancer Registries |
|
|
| Track 3: Cancer awareness and education |
|
|
| Track 4: Health System Strengthening and National Policy Development |
|
|
MOU= Memorandum of Understanding
MoH= Ministry of Health
Track 2
Track 2, Strengthening Pathology and Cancer Registries, focused on improving access to accurate and timely pathology for cancer diagnosis in areas outside of Nairobi, and expanding registration of cancer cases nationally. This track and its subsequent TWG has split into two sub-groups, one for each of these areas (Figure 1), but they continue to hold joint quarterly meetings.
Pathology
Acknowledging the scarcity of pathologists in Kenya outside of Nairobi, the Pathology subgroup prioritized access to accurate diagnostic testing for cancer. Specifically, access to simple but valuable diagnostic tests by developing a program to train medical officers in regional referral hospitals to perform and technical staff to process high quality fine needle aspirates (FNA), bone marrow aspirates (BMA) and bone marrow trephine biopsies. In a CGH-sponsored program, pathology residents and technicians from the University of Nairobi (UON, a public institution) and Aga Khan University (AKU, a not-for-profit private institution) were trained by Kenyan and international experts to be certified trainers of these techniques, and these new “trainers” then trained medical officers and technicians from five tertiary referral county public hospitals and helped them set up or expand existing FNA and BMA/Trephine biopsy clinics. Periodic on-site supervision and reinforcement of the training, as well as monitoring and evaluation of the program, are planned for the next 3–5 years, and the local hospitals have agreed to support the expense of ongoing supplies to ensure program sustainability beyond the project lifetime. The Pathology subgroup is now considering options for expanding this program to other sites [7].
Cancer Registries
This sub-group has made progress toward building a representative national cancer registry system. Although cancer registries have existed in Kenya since 1999, the scope and impact of these registries have not reached full implementation. The 2014 meeting helped to define national needs, including consistent funding of full-time staff and standardization of reporting forms for health facilities and laboratories. As a result of the meeting, CGH funded a proposal for strengthening three existing population-based cancer registries (Nairobi, Eldoret and Kisumu), which included a match in funding by the Government of Kenya (GOK) for training, increasing human resource capacity, cancer registry awareness workshops, and other needs. The cancer registry program is planning expansion to ten additional counties in order to develop a representative population-based national cancer registry. This will require training in data collection and data standardization.
Track 3
Track 3, Cancer Awareness and Education (CAE), had three objectives: (1) to understand community cultural beliefs and to identify key drivers of stigma in adults and children about cancer; (2) to develop and/or adapt culturally appropriate messages to destigmatize cancer; and (3) to raise public awareness of cancer prevention and early detection (in locations where primary prevention and early detection services exist), with a goal of reaching 60% of the population by 2018. Achieving consensus among the multitude of organizations working in this area was a priority for the follow-up CAE TWG meetings. The CAE TWG invited experts to the subsequent quarterly meetings for updates on ongoing knowledge, attitudes, and practices (KAP) studies, current education materials and other messages. These discussions served as the foundation for a systematic review of cancer education materials. In April 2016, the track held a regroup meeting in Nairobi to update the action plan and determine a revised course forward.
Survey respondents reported that the 2014 meeting helped to ensure that MoH and non-MoH partners reached consensus before implementing specific activities around cancer education and awareness. Furthermore, several respondents noted that awareness is the area of cancer control that has made visible progress in recent years, reflecting the need for coordination (see text box). Overall, respondents reported that the CAE TWG activities have been particularly important in improving stakeholder communication and determining opportunities for coordination of new and existing efforts to raise cancer awareness and reduce stigma. As funding for implementation of the CAE plan was a major obstacle reported, respondents agreed that future objectives need to be considered within the context of available resources.
“A lot has gone on since - so much on awareness. And much on prevention. A few years ago most people would run away from you if you talked about cancer. Now women are going to be checked. People are now aware.”-Kenya-based, non-MoH respondent
Track 4
Kenya’s decentralized health system relies upon policies and guidelines which emanate from the central government to ensure that prevention, screening, diagnosis, and treatment services are evidence-based, equitable, and disseminated throughout the country. To be successful, the health system requires significant coordination, commitment, and communication among the counties, where local implementation and budget priorities are decided. As such, Track 4, Health System Strengthening and National Policy Development, featured most prominently those organizations working at the county level.
While this track has not subsequently convened regular working group meetings, stakeholders have contributed to MoH-led national policy development through participation in working groups of relevant technical experts. This work has accelerated progress on the development of cancer treatment protocols and cancer center guidelines. These technical experts were consulted during the development of a plan to include cancer drugs in the recently updated Kenyan essential medicines list [8]. This process has involved consultation with multi-lateral partners, cancer treatment experts in Kenya, and key MoH stakeholders.
The operationalization of the NCI-K represents a much needed central coordinating body at the MoH level. NCI-K is charged with supporting the renewal and implementation of the NCCS by strengthening cancer research, cancer surveillance and community awareness, and by mobilizing resources to support cancer care and control. The establishment of this body, which did not exist at the time of the 2014 meeting, will strengthen Kenyan health systems related to cancer control and care [9]. In December 2016, NCI signed an MOU with NCI-K to continue to provide technical assistance to do this work.
Discussion
This evaluation of the Kenya Cancer Stakeholder Program highlights several key points about its structure and successes as well as future areas for improvement. The role of NCI’s Kenya-based technical adviser was repeatedly cited as a reason for progress, implementation, and success of the program. Liaising with all groups, especially the MoH and NCI-K, this position has been crucial in fostering relationships formed at the stakeholder meeting and assisting with the follow-through of action plans. This technical advisor provides content expertise, and ensures continuity of work and preservation of institutional knowledge, especially in a setting of high turnover of staff from both countries.
Our assessment elucidated two primary structural critiques of the program: 1) the breadth of topics addressed; and 2) the need for improved information dissemination across technical tracks. The agenda of the program spanned six thematic areas (research, training, pathology, cancer registries, community education, health systems), which in retrospect may have been overly ambitious and strained feasibility. The working groups have since tempered expectations, with the understanding that nearly all group members serve on a volunteer/inkind basis and participate in group activities in addition to their primary job responsibilities. Secondly, while each track has had structured follow-up calls and meetings to some extent, no program-wide follow-up meeting had been originally planned. The timing of a scheduled followup meeting within a few years would allow stakeholders to revisit the original meeting priorities and to strategize and plan for the next NCCS (2017–2022). With the recent establishment of the NCI-K and the increased capacity in cancer research and control, the MoH may now be able to organize such a forum.
Important to note is that the Stakeholder Program is not the sole catalyst of progress against cancer in Kenya and builds on previous efforts supported by domestic and international government and non-government organizations [10]. The First Lady of Kenya called for further action on stigma of cancer, which she described as the “foremost” of the “social challenges” that remain [11]. This is an example of high level recognition of the cancer problem nationwide, beyond the Stakeholder Program. Likewise, in 2016 the National Hospital Insurance Fund expanded coverage to include chemotherapy, radiation therapy and surgery for cancer care (up to a specified limit) [12]. This expansion of coverage has the potential to significantly impact the level of access to cancer treatment. Currently treatment is limited to patients who can afford to pay directly for services and who can afford the associated indirect costs (including time and transportation) required to undergo cancer treatment. Though not a direct outcome of the health system strengthening working group, this measure contributes to the improvement of treatment access, the reduction of loss to follow-up, as well as other related efforts in cancer control. Additionally, increased media attention to these cancer topics has kept the cancer agenda active in the public and policy domains to further impact the health policy movement.
In August 2016, the International Atomic Energy Agency (IAEA) led an imPACT mission in Kenya, an assessment in which the IAEA evaluates national cancer control capabilities and provides recommendations for improving capacity [13, 14]. NCI participated alongside the MoH and several key cancer stakeholders in this imPACT mission. Similar to a previous imPACT assessment in May 2010, this mission had a specific intent of informing the next phase of the national cancer strategy. The alignment of the NCI with other international partners like IAEA is a benefit to the MoH, which works with a multitude of partners, and avoids duplication of resources for cancer control.
Finally, several limitations in our survey-based evaluation should be acknowledged: first, stakeholder input was voluntary and self-reported, which may introduce response bias. Secondly, cancer stakeholders who were not present at the original stakeholders meeting were ineligible to be surveyed, despite any current involvement in the program. And finally, no premeeting survey was conducted, so we were unable to assess change over time without consideration of recall bias.
Conclusion
Though coordinated USG disease-specific programs are well-documented in infectious disease control efforts, the Kenya Cancer Stakeholder Program represents one of the first of its kind addressing an NCD. The successes of burgeoning partnerships, and the momentum generated in cancer research and control from the TWGs, suggest that this program can serve as an effective model for the control of cancer, and potentially other NCDs. Several elements contributed to this program’s success, including existing infrastructure, political will, fiscal and coordination support for workshop planning meetings, and an in-country technical adviser, which may be adopted in future NCD programs.
The progress in cancer over the past few years is based on the creation of a platform for key existing organizations and individuals to unite their efforts into a synergistic response. Through the planning efforts, leaders in research, pathology, cancer registries, awareness, and health systems, common objectives are now guiding cancer control efforts which begin in the central ministries of government and extend outward to the counties and to individual health facilities and communities. The collaborative Stakeholder Program has helped bring clarity and integration to this process, as partners move forward to prevent and control cancer in Kenya.
Table 1.
Organizations represented at the 2014 Kenya Stakeholder Meeting
| Organization Type | Kenya | Foreign | |
|---|---|---|---|
| Ministry of Health |
|
||
| NonMinistry of Health | Government |
|
|
| Research Institutions |
|
|
|
| Academia |
|
|
|
| Cancer Care |
|
|
|
| NGO |
|
|
|
| Multi-lateral |
|
|
|
Partnership between Kenyan and foreign entities
Highlights.
Four technical areas provide a structure for organizing partners and efforts across the country.
Political will around cancer and multi-sectoral momentum laid groundwork for a cohesive program.
An NCI-supported technical adviser embedded in the Ministry of Health has enabled follow-through.
This model offers a replicable strategy for organizing non-communicable disease programs.
Acknowledgments
The study was reviewed and approved by the United States Office of Management and Budget (OMB # 0925-0722, expiration date: 06/30/2018). The NCI Center for Global Health and the Kenyan Ministry of Health acknowledge the efforts and contributions of all stakeholders who participated in the 2014 meeting and all individuals who are engaged in the ongoing efforts of the Stakeholder Program. The NCI and MoH notably thank those who assisted in the planning, implementation, and evaluation of the program, and the co-chairs of each technical track. Lastly, the authors acknowledge Catherine Hildago for her efforts in obtaining OMB clearance for this evaluation, and Karen Haney for her contributions in coding survey responses.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.WHO. Updated February 2015. Cancer Fact Sheet N°297. http://www.who.int/mediacentre/factsheets/fs297/en/. Accessed September 26, 2016.
- 2.Kanavos P. The rising burden of cancer in the developing world. Annals of Oncology. 2006;17:viii15–viii23. doi: 10.1093/annonc/mdl983. [DOI] [PubMed] [Google Scholar]
- 3.Ministry of Medical Services (MOMS) and Ministry of Public Health & Sanitation (MOPHS), Kenya. National Cancer Control Strategy, 2011–2016. http://www.ipcrc.net/pdfs/Kenya-National-Cancer-Control-strategy.pdf (accessed 12.16.16)
- 4.Topazian H, Cira M, Dawsey SM, et al. Joining forces to overcome cancer: The Kenya cancer research and control stakeholder program. Journal of Cancer Policy. 2016;7:36–41. doi: 10.1016/j.jcpo.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simbiri KO, Biddle J, Kinyera T, et al. Burkitt lymphoma research in East Africa: highlights from the 9th African organization for research and training in cancer conference held in Durban, South Africa in 2013. Infectious Agents and Cancer. 2014;9:32. doi: 10.1186/1750-9378-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Academic Model Providing Access to Healthcare. http://www.ampathkenya.org/ (accessed 12.16.16)
- 7.Shahin S. Manuscript in preparation. 2016. Creation and pilot testing of cases for case-based learning: A pedagogical approach for pathology cancer diagnosis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ministry of Health, Kenya. Kenya Essential Medicines List 2016. Published June 2016. http://apps.who.int/medicinedocs/documents/s23035en/s23035en.pdf (accessed 12.16.16)
- 9.Makumi D. Finally Kenya gets a statutory cancer body to unify efforts. The East African, Opinion and Editorial. Feb 7, 2015. http://www.theeastafrican.co.ke/OpEd/comment/Finally-Kenya-gets-a-statutory-cancer-body-to-unify-efforts-/-/434750/2616574/-/lr2ycd/-/index.html .
- 10.Cira Mishka. Report on Cervical Cancer Activity in Kenya, January 2015. American Cancer Society, Global Health Department; http://rho.org/files/ACS_Kenya_report_2015.pdf (accessed 12.16.16) [Google Scholar]
- 11.The Official Website of the President, Statements and Speeches. Speech by HE Margaret Kenyatta, The First Lady of the Republic of Kenya, During the Ministry of Defence Cancer Awareness Month on Wednesday, October 28, 2015 at Moi Air Base, Nairobi, Kenya. http://www.president.go.ke/2015/10/28/speech-by-h-e-margaret-kenyatta-the-first-lady-of-the-republic-of-kenya-during-the-ministry-of-defence-cancer-awareness-month-on-wednesday-october-28-2015-at-moi-air-base-nairobi-kenya/ (accessed 12.16.16)
- 12.National Hospital Insurance Fund (NHIF) http://www.nhif.or.ke/healthinsurance/ (accessed 12.16.16)
- 13.International Atomic Energy Agency (IAEA) Programme of Action for Cancer Therapy (PACT), 2014. http://cancer.iaea.org/impact.asp (accessed 12.16.16)
- 14.International Atomic Energy Agency (IAEA), Integrated Missions of PACT. Together Against Cancer. https://cancer.iaea.org/documents/imPACTBrochure.pdf (accessed 12.16.16)


