Abstract
To improve the success of mechanical thrombectomy, three-dimensional turbo spin-echo (3D-TSE) sequences on T2WI can be employed to estimate the vascular structure of the posterior circulation. In addition to the short imaging time of 3D-TSE T2WI (33 sec), it can visualize the outer diameter of the main cerebral artery, including the occluded vessels. However, to date, the efficacy of mechanical thrombectomy in the posterior circulation remains unclear, and safer and more efficient mechanical thrombectomy procedures are required. Assessment of the anatomical variations in the posterior circulation using 3D-TSE T2WI is valuable for access decisions, device selection, and safe device guidance and retrieval techniques to the target vessel. Herein, we present representative cases of basilar artery and posterior cerebral artery occlusions in our institute and describe the utility of preoperative 3D-TSE T2WI in these patients.
Keywords: 3D turbo spin-echo magnetic resonance imaging, mechanical thrombectomy, posterior circulation ischemia
Introduction
Approximately 20% of all ischemic strokes occur in the posterior circulation.1) Among these, basilar artery occlusion is a serious condition with a poor prognosis in 70%-90% of patients receiving standard medical treatment.2) Although the superiority of mechanical thrombectomy for large vessel occlusion in the anterior circulation is well established, a meta-analysis and two randomized controlled trials (RCTs) have failed to demonstrate the efficacy of mechanical thrombectomy for acute basilar artery occlusion.3-6)
Stent-based thrombus retrieval procedures require blind guidance of a wire and microcatheter over the thrombus, followed by dragging of the deployed stent. Recent RCTs suggested that 5%-29% of patients receiving mechanical thrombectomy exhibit device-related complications, such as arterial perforation and dissection.7) Furthermore, these complications may be more frequent for basilar artery occlusions than for anterior circulation occlusions.8)
A few studies of mechanical thrombectomy have employed magnetic resonance imaging (MRI) to detect occluded vessels in the anterior circulation, and we have demonstrated the efficacy of three-dimensional turbo spin-echo (3D-TSE) sequences using T1WI and T2WI to evaluate both thrombus configuration and arterial anatomy at the middle cerebral artery bifurcations.9-11) In this study, we applied 3D-TSE T2WI to examine the vascular structure of the posterior circulation, including a comparison of vessel diameters between the posterior communicating artery (PCoA) and the P1 segment of the posterior cerebral artery (PCA). Our findings indicate the utility of 3D-TSE T2WI for identifying the mechanism of posterior circulation cerebral ischemia and achieving a safe and efficient mechanical thrombectomy.
Method
We used MRI as a first-line imaging modality for all 133 cases of acute stroke due to large vessel occlusion between February 2021 and July 2022. A total of 11 patients with acute basilar artery occlusion during this period underwent the following MRI protocol.11) Using 3.0 T MRI (Skyra system; Siemens, Erlangen, Germany), patients with acute ischemic stroke underwent diffusion-weighted imaging (DWI), 3D time-of-flight magnetic resonance angiography (MRA), T2*WI, fluid-attenuated inversion recovery, and 3D-TSE T1WI and T2WI. The total scan time of our stroke protocol was 9 min and 47 sec. The parameters for 3D-TSE T2WI (slice thickness, 0.6 mm; no gap) were TR/TE = 1300/98 msec, voxel size = 0.5 × 0.5 × 0.6 mm, ETL = 165, FOV = 140 mm, and acquisition time = 33 sec. In some cases, the fusion images of 3D-TSE T2WI and MRA were generated preoperatively on a workstation (Syngo. via VE11, Siemens, Germany).
Case 1
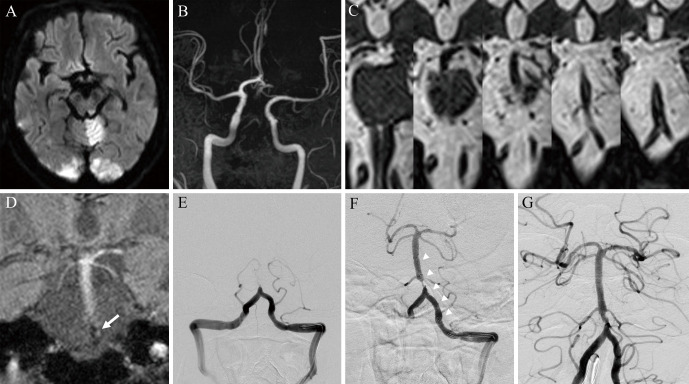
The patient was a 68-year-old man. He was found collapsed at home and was urgently transported to our hospital. His National Institute of Health Stroke Scale (NIHSS) score was 24 due to severe consciousness impairment. DWI revealed new infarcts in the left cerebellum and the bilateral occipital lobes (Fig. 1A). MRA showed occlusion of the basilar artery from the bilateral vertebral arteries, a small left PCoA, and slight blood flow at the tip of the basilar artery (Fig. 1B). The penumbra was located in the brainstem and other territories in the posterior circulation. Thus, thrombus retrieval therapy was performed for acute basilar artery occlusion.
Fig. 1.
Use of three-dimensional turbo spin-echo (3D-TSE) T2WI in mechanical thrombectomy for basilar artery occlusion. Diffusion-weighted imaging revealed areas of high signal intensity in the left cerebellum and bilateral occipital lobes (A). Magnetic resonance angiography revealed basilar artery occlusion (B). 3D-TSE T2WI visualized the arterial configuration of the occluded vertebral arteries and basilar artery (C). T2*WI depicted the thrombus with a low intensity, which was located in the lower segment of the basilar artery (arrow indicates the thrombus) (D). Successful recanalization was achieved after the endovascular procedure (E: pre-operation, F: post-stent deployment, G: post-percutaneous transluminal angioplasty).
3D-TSE T2WI revealed the vascular anatomy of the basilar artery, including the PCA origin (Fig. 1C). In addition, although MRA did not show the bilateral vertebral arteries, a left-sided vertebral artery approach was selected as the bilateral vertebral arteries were equally developed on both sides in 3D-TSE T2WI. The wire was safely advanced beyond the thrombus into the right PCA, and a microcatheter was then inserted. T2*WI showed that the thrombus was located in the lower basilar artery (Fig. 1D). Thus, a Solitaire device (4 × 40 mm; Medtronic, Irvine, CA, USA) was deployed from the middle segment of the basilar artery. Good revascularization was achieved after additional percutaneous transluminal angioplasty (Unryu balloon catheter, 2.5 × 10 mm; Kaneka Medix, Osaka, Japan) (Fig. 1E-G).
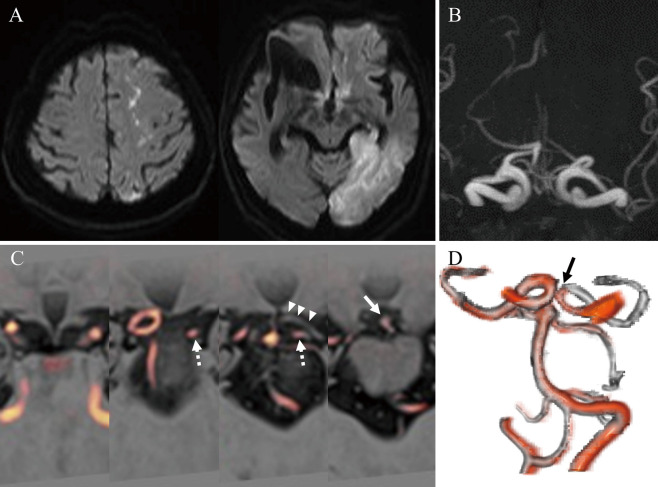
Case 2
The patient was a 79-year-old woman who presented with disturbed consciousness, aphasia, and right upper extremity motor impairment (NIHSS score of 26). DWI demonstrated high-intensity areas in the left anterior cerebral artery/middle cerebral artery watershed territory and the left occipital lobe (Fig. 2A). MRA revealed occlusion of the left PCA (Fig. 2B). The infarct image was seen in both the anterior and posterior circulations. Although the potential for multiple cerebral embolisms was considered, fused 3D-TSE T2WI with MRA revealed fetal PCA occlusion with a small P1 segment (Fig. 2C, D). Thus, we concluded that the occluded internal carotid artery (ICA) had recanalized, and the thrombus remained only in the fetal PCA. We considered that mechanical thrombectomy via the ICA would be appropriate for revascularization of the PCA region. In this case, the infarction in the left PCA territory had already been completed, and medical treatment was chosen.
Fig. 2.
Utility of three-dimensional turbo spin-echo (3D-TSE) T2WI in determining the pathophysiology in patients with posterior circulation ischemic stroke. Diffusion-weighted imaging revealed a fresh infarction in both the anterior and posterior circulations (A). Magnetic resonance angiography (MRA) showed left posterior cerebral artery (PCA) occlusion (B). 3D-TSE T2WI (grayscale) and MRA (red) fusion imaging revealed fetal PCA occlusion with a small P1 segment (the dotted arrow indicates the posterior communicating artery; the arrowhead indicates the occluded P2 segment of the PCA; the solid arrow indicates the occlusion site) (C). Three-dimensional reconstruction of the fused 3D-TSE T2WI and MRA images (D).
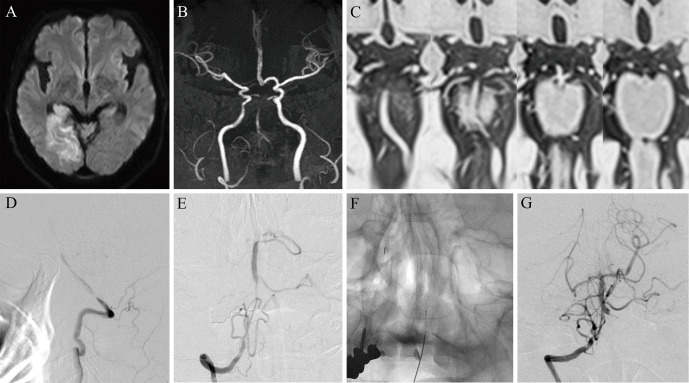
Case 3
The patient was a 60-year-old man. He suffered from dizziness, sensory disturbance on the left side, and dysarthria. His NIHSS score was 6. DWI revealed a fresh cerebral infarction in the right occipital lobe, thalamus, and right cerebellum (Fig. 3A). MRA showed a small right P1 segment and left PCA delineation, along with upper basilar artery occlusion (Fig. 3B). 3D-TSE T2WI identified vascular structures around the tip of the basilar artery, as well as a bilateral hypoplastic PCoA (Fig. 3C). Angiography revealed atherosclerotic stenosis in the V4 segment of the left vertebral artery (Fig. 3D). The patient was diagnosed with basilar artery occlusion due to artery-to-artery embolism from the left vertebral artery stenosis. A mechanical thrombectomy was performed using the right vertebral artery approach. The right PCA territory was already infarcted, and the microcatheter was intentionally guided into the right superior cerebellar artery. The Embotrap III device (5 × 37 mm; CERENOVUS, Irvine, CA, USA) was placed from the right superior cerebellar artery to the lower basilar artery, and thrombus retrieval was performed, which resulted in good revascularization after a single pass (Fig. 3E-G). The right PCA was terminated with occlusion. Percutaneous transluminal angioplasty for the left vertebral artery stenosis was successfully conducted in the subacute phase of ischemic stroke.
Fig. 3.
The application of three-dimensional turbo spin-echo (3D-TSE) T2WI was effective in mechanical thrombectomy for basilar artery occlusion. Diffusion-weighted imaging demonstrated high-intensity areas in the right occipital lobe, thalamus, and right cerebellum (A). Magnetic resonance angiography revealed upper basilar artery occlusion (B). 3D-TSE T2WI revealed vascular structures around the tip of the basilar artery, with the bilateral hypoplastic posterior communicating artery (C). Cerebral angiography detected atherosclerotic stenosis in the left vertebral artery and basilar artery occlusion (D). After a single pass of mechanical thrombectomy from the right superior cerebellar artery, successful recanalization was achieved with the right posterior cerebral artery remaining occluded (E–G).
Discussion
Compared with anterior circulation, posterior circulation ischemia is characterized by a short time to infarction due to a lack of collateral blood flow and a range of symptoms that take time to be accurately diagnosed.1) Recanalization is important for good prognosis in basilar artery occlusion.12) However, futile recanalization of the posterior circulation could not improve functional outcomes compared with the anterior circulation.13) The heterogeneity evident in studies to date, such as differences in baseline NIHSS values, the device used, site of occlusion, and etiology of cerebral ischemia, may have contributed to the range of outcomes of mechanical thrombectomy.6)
Because successful recanalization in anterior circulation stroke with a single thrombectomy device pass is associated with a good functional outcome, there is increasing interest in the efficacy of the first-pass effect for basilar artery occlusion.14) An accurate understanding of the stroke mechanism and precise endovascular recanalization therapy is required to achieve a first-pass effect. There are numerous anatomical variations in the posterior circulation.15) In cases with a fetal PCA, thromboembolism in the anterior circulation can cause infarction in the PCA territory. Acute arterial occlusions or infarcts in both the anterior and posterior circulations make it difficult to determine a single-vessel occlusion or a multiple embolism etiology. Of note, the vascular structure alone cannot completely determine the mechanism of cerebral ischemia. Nevertheless, understanding the anatomical variations in the posterior circulation using 3D-TSE T2WI can help understand the pathophysiology of ischemic stroke.
Vascular variations in the circle of Willis can also affect thrombus retrieval techniques. Mechanical thrombectomy via the ICA is appropriate for PCA occlusion in patients with a fetal PCA. Blindly probing a small or absent P1 segment via the basilar artery with a wire, pushing a microcatheter forward, or deploying a stent can cause serious complications, including arterial perforation or dissection. Numerous perforating branches of the P1 segment (e.g., thalamoperforating arteries) run in the same direction as the occluded basilar artery. These anatomical characteristics at the tip of the basilar artery provide an additional risk of arterial perforation. Apart from noting a change in resistance or behavior during wire insertion, it cannot be confirmed whether the wire located beyond the occlusion site is located in the main trunk of the posterior circulation. Patients must abandon recanalization therapy if an arterial perforation occurs and the prognosis is extremely poor.16) It should be noted that 3D-TSE T2WI-based imaging of the arterial structure allows the target vessel to be selected, and the wires and microcatheters can be inserted along the estimated vascular run to avoid vascular damage.
Regarding the first-line choice of thrombus retrieval technique for posterior circulation stroke, direct aspiration was reported to have better results than stent retrieval.17) However, it was recently reported that a combination of both aspiration and stent retrieval was more effective than direct aspiration alone.18) Expanded indications of mechanical thrombectomy for more distal PCA occlusions have been attempted. In addition, a larger catheter-to-vessel ratio is more effective for thrombus retrieval in direct aspiration procedures.19) Thus, efficient thrombectomy procedures in the posterior circulation require appropriately sized devices to be safely guided to the distal vessel. A particular advantage of 3D-TSE T2WI about device selection is that it provides anatomical information on occluded vessels, including vessel diameter, which is not depicted by cerebral angiography, computed tomography angiography, or other devices.
In conclusion, 3D-TSE T2WI can rapidly visualize the vasculature of the main cerebral arteries, including vessels distal to the occlusion site. 3D-TSE T2WI is useful for estimating the pathophysiology of posterior circulation ischemic stroke and for an efficient mechanical thrombectomy.
Conflicts of Interest Disclosure
All authors declare no conflicts of interest associated with this manuscript.
Acknowledgments
We thank Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
References
- 1). Markus HS, van der Worp HB, Rothwell PM: Posterior circulation ischaemic stroke and transient ischaemic attack: Diagnosis, investigation, and secondary prevention. Lancet Neurol 12: 989-998, 2013 [DOI] [PubMed] [Google Scholar]
- 2). Mattle HP, Arnold M, Lindsberg PJ, Schonewille WJ, Schroth G: Basilar artery occlusion. Lancet Neurol 10: 1002-1014, 2011 [DOI] [PubMed] [Google Scholar]
- 3). Powers WJ, Rabinstein AA, Ackerson T, et al. : Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 50: 344-418, 2019. 30626290 [Google Scholar]
- 4). Liu X, Dai Q, Ye R, et al. : Endovascular treatment versus standard medical treatment for vertebrobasilar artery occlusion (BEST): an open-label, randomised controlled trial. Lancet Neurol 19: 115-122, 2020 [DOI] [PubMed] [Google Scholar]
- 5). Langezaal LCM, van der Hoeven EJRJ, Mont'Alverne FJA, et al. : Endovascular therapy for stroke due to basilar-artery occlusion. N Engl J Med 384: 1910-1920, 2021 [DOI] [PubMed] [Google Scholar]
- 6). Zhao Y, Zhao W, Guo Y, Li Y: Endovascular thrombectomy versus standard medical treatment for stroke patients with acute basilar artery occlusion: a systematic review and meta-analysis. J Neurointerv Surg 14: 1173-1179, 2022 [DOI] [PubMed] [Google Scholar]
- 7). Balami JS, White PM, McMeekin PJ, Ford GA, Buchan AM: Complications of endovascular treatment for acute ischemic stroke: Prevention and management. Int J Stroke 13: 348-361, 2018 [DOI] [PubMed] [Google Scholar]
- 8). Alonso De Leciñana M, Kawiorski MM, Ximénez-Carrillo Á, et al. : Mechanical thrombectomy for basilar artery thrombosis: A comparison of outcomes with anterior circulation occlusions. J Neurointerv Surg 9: 1173-1178, 2017 [DOI] [PubMed] [Google Scholar]
- 9). Kuribara T, Haraguchi K, Ogane K, Matsuura N, Ito T: 3D-FIESTA magnetic resonance angiography fusion imaging of distal segment of occluded middle cerebral artery. Neurol Med Chir (Tokyo) 55: 805-808, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10). Sato K, Hijikata Y, Omura N, et al. : Usefulness of three-dimensional fast imaging employing steady-state acquisition MRI of large vessel occlusion for detecting occluded middle cerebral artery and internal carotid artery before acute mechanical thrombectomy. J Cerebrovasc Endovasc Neurosurg 23: 201-209, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11). Ohara J, Fujimoto M, Tani S, et al. : 3D Turbo spin-echo MRI-based mechanical thrombectomy at middle cerebral artery bifurcations. Neurol Med Chir (Tokyo) 62: 149-155, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12). Kumar G, Shahripour RB, Alexandrov AV: Recanalization of acute basilar artery occlusion improves outcomes: A meta-analysis. J Neurointerv Surg 7: 868-874, 2015 [DOI] [PubMed] [Google Scholar]
- 13). Meinel TR, Kaesmacher J, Chaloulos-Iakovidis P, et al. : Mechanical thrombectomy for basilar artery occlusion: Efficacy, outcomes, and futile recanalization in comparison with the anterior circulation. J Neurointerv Surg 11: 1174-1180, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14). Pop R, Finitsis SN, Arquizan C, et al. : Poor clinical outcome despite successful basilar occlusion recanalization in the early time window: Incidence and predictors. J Neurointerv Surg. doi: org/10.1136/neurintsurg.2022-018769 Epub 2022 Apr 15 [DOI] [PubMed] [Google Scholar]
- 15). Gunnal SA, Farooqui MS, Wabale RN: Anatomical variability of the posterior communicating artery. Asian J Neurosurg 13: 363-369, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16). Happi Ngankou E, Gory B, Marnat G, et al. : Thrombectomy complications in large vessel occlusions: Incidence, predictors, and clinical impact in the ETIS registry. Stroke 52: e764-e768, 2021 [DOI] [PubMed] [Google Scholar]
- 17). Ye G, Wen X, Wang H, et al. : First-line contact aspiration versus first-line stent retriever for acute posterior circulation strokes: An updated meta-analysis. J Neurointerv Surg 14: 457-463, 2022 [DOI] [PubMed] [Google Scholar]
- 18). Abdelrady M, Ognard J, Cagnazzo F, et al. : Frontline thrombectomy strategy and outcome in acute basilar artery occlusion. J Neurointerv Surg. doi: org/10.1136/neurintsurg.2021-018180 Epub 2022 Jan 6 [DOI] [PubMed] [Google Scholar]
- 19). Kyselyova AA, Fiehler J, Leischner H, Flottmann F, Buhk JH, Frölich AM: Vessel diameter and catheter-to-vessel ratio affect the success rate of clot aspiration. J Neurointerv Surg 13: 605-608, 2021 [DOI] [PubMed] [Google Scholar]