Abstract
We compared the treatment satisfaction of patients who had undergone surgery for tarsal tunnel syndrome (TTS) and carpal tunnel syndrome (CTS). We enrolled 44 patients in this study; 23 were operated for CTS and 21 for TTS. All patients had received surgery under a microscope and under local anesthesia. Using the numerical rating scale (NRS) for numbness/pain (range 0-10) we compared their preoperative outcome expectations with their satisfaction with our treatment 6 months after the operation. We also recorded their pre- and postoperative EuroQol 5-dimension 5-level (EQ-5D-5L) scale for their health-related quality of life (QOL). The subjective assessment of their QOL showed that it was significantly lower in TTS- than CTS patients both pre- and postoperatively. Six months after the operation, the NRS for symptoms and the (EQ-5D-5L) scale for the QOL were significantly improved in TTS- and CTS patients; however, these scores were significantly better after CTS- than TTS surgery. Also, the postoperative NRS was significantly lower in the CTS- than the TTS patients. Our comparison of the patients' expected- and actual surgical outcome showed that the result was better than expected after CTS- and TTS surgery; in CTS patients the difference was significant. Overall, CTS- were more satisfied than TTS patients with the treatment outcome. Satisfaction with the treatment was greater after CTS- than TTS surgery. TTS- experienced less symptom relief than CTS patients although the actual- exceeded the expected outcome in patients operated for TTS.
Keywords: surgical satisfaction, tarsal tunnel syndrome, carpal tunnel syndrome
Introduction
Tarsal tunnel syndrome (TTS) is an entrapment neuropathy of the posterior tibial nerve at the tarsal tunnel, and symptoms that lower the patients' quality of life (QOL),1-4) being sole numbness, a foreign body- and a cold sensation, and pain.
Symptomatic TTS can be due to space-occupying lesions such as ganglia or schwannoma; it can be diagnosed by MRI and high-resolution ultrasound,5-10) and the surgical results are relatively good.5,11-13) Idiopathic TTS is elicited by physiological changes such as adhesions due to trauma, distortion of an artery, dilation of a vein, or hypertrophy of the flexor retinaculum.1,2,5,10) Currently there is no gold-standard examination for idiopathic TTS. Because the results of electrophysiologic examination are not reliable,1,11,14-18) and because its diagnosis tends to be based on clinical findings,5,14-16) the postoperative outcome may be unsatisfactory. The success rate of TTS surgery ranged from 44% to 96%,1,2,5,11,12,14) however, besides the patients' post-treatment health status,19-22) their postoperative satisfaction plays an important role in value-based patient care.
Carpal tunnel syndrome (CTS) is the most common and well-studied peripheral entrapment neuropathy. Finger numbness and motor weakness of the thenar eminence associated with median nerve entrapment affect the patients' QOL; surgery is a viable treatment option.3,23-25)
In this retrospective study we compared the surgical results and the degree of postoperative satisfaction in patients operated for TTS and CTS.
Materials and Methods
Our retrospective study was approved by the ethics committee of Chiba Hokuso Hospital. Patients written informed consent for inclusion in the study was waived because an opt-out option was provided on our hospital homepage, with prior written consent for the surgery was obtained from all patients.
Patients
Between January 2020 and December 2021 we treated 54 consecutive patients who presented with CTS (n = 26) or TTS (n = 28). Not included in this study were patients who improved with conservative therapy consisting of medication and physiotherapy lasting at least 3 months, patients who refused surgery or presented with severe dementia, psychological problems, and malignant disease. We excluded 10 patients (CTS n = 3, TTS = 7) because they had had surgery for entrapment neuropathy or spinal disease within the past 6 months or they did not fulfill our inclusion criteria. Consequently, the final study population was comprised of 44 patients who did not improve by conservative treatment; their characteristics are presented in Table 1.
Table 1.
CTS and TTS patients’ characteristics and surgical results
| CTS | TTS | p value | |
|---|---|---|---|
| Cases | 23 | 21 | ns |
| Age (years) | 72 | 73 | ns |
| Male:Female | 5:18 | 10:11 | ns |
| Preoperative symptom (NRS) | 6.2 ± 1.7 | 6.6 ± 1.5 | ns |
| Postoperative symptom (NRS) | 0.6 ± 0.8* | 2.7 ± 1.5 | p < 0.01 |
| Preoperative QOL* | 0.82 ± 0.11 | 0.71 ± 0.16 | p = 0.01 |
| Postoperative QOL* | 0.95 ± 0.1 | 0.81 ± 0.11 | p < 0.01 |
| Postoperative satisfaction (NRS) | 9.4 ± 0.9 | 6.6 ± 2.1 | p < 0.01 |
Abbreviations:
CTS = carpal tunnel syndrome
TTS = tarsal tunnel syndrome
NRS = numerical rating scale
QOL* = quality of life based on the EuroQol 5-dimension 5-level scale
Diagnosis
The CTS diagnosis was based on pain and numbness in the distribution of the median nerve (palmar aspect of the thumb, index and middle fingers, radial half of the ring finger), atrophy of the thenar eminence in patients with progressive symptoms, and the results of the Tinel sign- and Phalen tests. The median nerve at the carpal tunnel was subjected to electrodiagnostic study; a distal motor latency longer than 4.2 ms and a sensory distal latency longer than 3.5 ms were considered diagnostically positive.26) All 23 CTS patients fulfilled electrodiagnostic criteria; in 2 patients with motor nerve conduction velocity and in 6 with sensory nerve conduction velocity (SCV) were evoked.
All 21 patients with TTS had sole symptoms consistent with TTS (numbness, pain, coldness, foreign-body sensation). On 16 sides a Tinel-like sign was recorded at the tarsal tunnel. The SCV at the tarsal tunnel was measured and terminal latencies of the abductor hallucis muscle exceeding 5.8 ms and side-to-side variations in the amplitude decrease exceeding 50% of the same-branch27,28) were considered to be positive findings. Only one TTS patient did not fulfill electrodiagnostic criteria; 8 SCV patients manifested no evocation.
In one SCV patient there was no significant latency prolongation (medial plantar nerve 5.4 ms, lateral plantar nerve 5.2 ms), and surgery was performed in accordance with the patient's wish and with prior informed consent, although we noted typical clinical symptoms of TTS.
Of the 21 TTS patients, all but one who harbored a ganglion, presented with idiopathic TTS. No patient harbored mass lesions. All 21 patients underwent MRI studies to look for lumbar spine lesions. In relatively elderly individuals we noted lumbar degenerative diseases such as lumbar spine canal stenosis. In patients with both TTS and lumbar spine canal stenosis, because there are few symptoms due to lumbar spine canal stenosis along the dermatome, our treatment focused on their TTS when the main symptom involved the sole.
Surgery
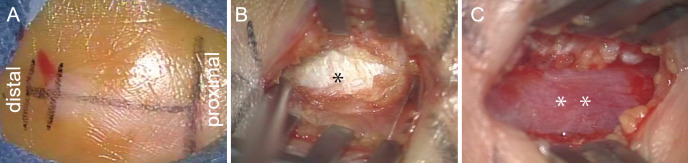
CTS: The patient was placed under local anesthesia; no tourniquet was used. Under a microscope, a 20-mm linear skin incision was made on the carpal tunnel and the flexor retinaculum was opened. The median nerve was decompressed by external neurolysis, the perineural synovium was dissected (Fig. 1).
Fig. 1.
Photographs of our surgery for carpal tunnel syndrome.
A A 20-mm linear skin incision is made on the carpal tunnel.
B The flexor retinaculum (*) is exposed.
C The median nerve (**) is decompressed.
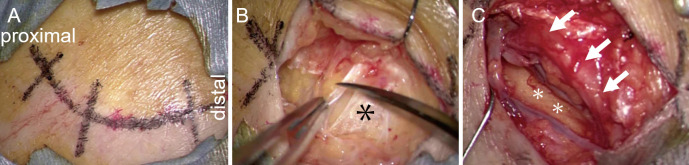
TTS: Surgery was under local anesthesia using a microscope. The posterior tibial artery was sutured to the superficial part of the flexor retinaculum using a 4-0 nylon suture,27) and a 25-mm bow-like skin incision was made on the tarsal tunnel and the flexor retinaculum was opened. The nerve was decompressed by transposing the posterior tibial artery to the side of the medial malleolus in the tarsal tunnel; small arterial branches and veins were cut as needed (Fig. 2).
Fig. 2.
Photographs of our surgery for tarpal tunnel syndrome.
A A 25-mm bow-like skin incision is made on the tarpal tunnel.
B The flexor retinaculum (*) is exposed and opened.
C The posterior tibial nerve (**) is decompressed by transposing the posterior tibial artery (arrows).
Outcome evaluation
When acquiring the patients' informed consent for surgery, we explained that postoperative symptom improvement could be expected but that numbness would remain. We suggested that, if their current symptoms were tolerable, they undergo conservative treatment, stressing that if their preoperative expectations were too high, they may not be satisfied with the treatment outcome. We also explained that subsequent treatment such as tendon transplantation may be necessary for further symptom alleviation, and that it would take time postoperatively to resolve localized paralysis or muscle atrophy due to CTS.
Six months after the operation, the pre- and postoperative severity of numbness/pain (0 = no pain, 10 = great pain) was compared with the patients' subjective satisfaction (10 = great satisfaction, 0 = complete dissatisfaction). Their pre- and postoperative health-related QOL was evaluated using the EuroQol 5-dimension 5-level (EQ-5D-5L) scale. It ranges from 0 to 1 with 1 indicating perfect health.
For statistical analyses we used IBM SPSS for Windows ver. 25.0 (IBM Corp., Armonk, NY, USA). Intra-group comparisons were performed with the Wilcoxon signed-rank- and the Mann-Whitney U-test. Differences of p < 0.05 were considered statistically significant. All values are expressed as the mean ± standard deviation.
Results
There was no significant difference between TTS- and CTS patients with respect to the number of patients, the gender ratio, mean age, and the NRS for preoperative symptoms. The preoperative QOL rated on the EQ-5D-5L scale was significantly lower in TTS- than CTS patients (p < 0.05, Table 1). Although surgery yielded significantly better results in CTS- than TTS patients (p < 0.05) and the level of patient satisfaction was significantly higher in patients operated for CTS than TTS, as shown in the table, 6 months postoperatively, the NRS for symptoms and the QOL based on the EQ-5D-5L score were significantly improved in TTS and CTS patients. In the TTS patient harboring a ganglion, the degree of postoperative satisfaction was rated as 8, showing a good surgical result.
Table 2 shows that in patients operated for CTS, but not in TTS patients, the actual- was significantly better than the expected treatment outcome (p < 0.05).
Table 2.
CTS or TTS patients’ preoperative expectations and actual outcomes
| CTS | TTS | |||||
|---|---|---|---|---|---|---|
| Expected | Actual | Expected | Actual | |||
| NRS | 2.04 ± 2.49 | 0.61 ± 0.78 | p < 0.05 | 3.10 ± 1.87 | 2.79 ± 1.51 | ns |
| QOL* | 0.92 ± 0.08 | 0.96 ± 0.05 | p < 0.05 | 0.85 ± 0.15 | 0.80 ± 0.11 | ns |
Abbreviations:
CTS = carpal tunnel syndrome
TTS = tarsal tunnel syndrome
NRS = numerical rating scale
EQ-5D-5 L = EuroQol 5-dimension 5-level scale
QOL* = quality of life based on the EuroQol 5-dimension 5-level scale
Discussion
Our study showed that patients operated for CTS tended to be satisfied with the treatment results. Similar findings have been reported by others.23-25) While surgery for TTS improved the NRS for symptoms and the QOL score, operated TTS patients were less satisfied than CTS patients with the treatment outcome. Although the preoperative NRS was not significantly different between CTS- and TTS patients, the latter were less satisfied with our treatment than were the CTS patients. Others22,29-32) documented that improvement in the pain- and disability scores correlated with postoperative patient satisfaction. Those patients operated for TTS expressed less satisfaction than CTS patients, while the postoperative QOL was improved in both our TTS and CTS patients.
This study compared the expected- and the actual outcome after surgery for TTS and CTS. We found that exceeding the expectation of patients scheduled for CTS surgery led to a high degree of postoperative satisfaction. Others19,21,23,33) reported that patients experiencing a postoperative reduction in pain and disability were satisfied with their treatment although their symptom improvement did not meet their preoperative expectations.
In earlier series the surgical success rate in patients with TTS was reported.1,2,5,11,14) According to Pfeiffer and Cracchiolo34) only 44% of TTS patients benefited markedly from surgery. On the other hand, Bouysset et al.11) found that 51% of their operated TTS patients were willing to undergo another surgery to further improve their condition. Kim et al2) reported that, while 22% of TTS patients found the results acceptable, and 10% were dissatisfied, 68% of these patients were satisfied with the surgical treatment outcome.
The postoperative prognosis is good in patients with compressive space-occupying lesions.11,34) Factors such as plantar fasciitis, prolonged symptom duration, positive Tinel signs, ankle disorders, electrophysiological findings, and the surgical procedure affect the surgical outcome in patients with idiopathic TTS.1,11,13,14,25,35)
Marked hindfoot valgus/varus, bone-nerve contact, and accessory muscle fasciitis were associated with unsatisfactory surgical results.11) None of our patients presented with accessory muscle- or plantar fasciitis; we did not evaluate marked hindfoot valgus/varus and bone-nerve contact.
Ankle-joint eversion or inversion increases tarsal tunnel pressure; in neutral ankle-joint position, the intra-tunnel pressure and tibial nerve entrapment are decreased.36) Neurolysis decreases tarsal tunnel pressure but it may not decrease nerve stretching in the static state of marked hindfoot valgus/varus. Such management may affect the bone-nerve contact due to morphological anomalies of the posteromedial tubercle of the talus, imaging scans must be inspected to alert to such changes,11) as the recommended management in patients with mobile joint- and hindfoot deformities is the wearing of appropriate footwear and plantar ortheses.11)
As there is no diagnostic gold standard for the identification of idiopathic TTS, its diagnosis tends to rely on clinical findings5,14-16) and patients may not be satisfied with the surgical results. According to others,37,38) negative electrophysiological findings did not rule out surgery and electrophysiological findings did not correlate with surgical outcomes.39)
Seidel et al.40) reported that the findings of preoperative electrophysiologic studies predicted postoperative symptom improvement in TTS patients and in patients with plantar tibial nerve symptoms. With the false-positive and false-negative rate in their study population requiring further investigation, their studies recorded mixed nerve action potentials that include a large number of sensory and motor axons contributing to the measured waveforms, where actual improvement was recorded in 92% of patients suspected of TTS and in 77% of patients with no TTS.
Unlike earlier patients,27) none of our current patients underwent decompression of the distal tarsal tunnel. Heimkes et al.41) reported distal tarsal tunnel involvement in some TTS patients. Because in our patients reporting low satisfaction with the operation, we may have overlooked distal tarsal tunnel entrapment, we now recommend extension of the skin incision and distal tarsal tunnel decompression, ad in our patients reporting low satisfaction with our operation, we may have overlooked distal tarsal tunnel entrapment.
Our study has some limitations. It was retrospective, involved a single institution, and the study population was small. We think that the following factors had no significant effect on our findings, although we did not evaluate the possible impact these patient-ages, race, education, economic status, mental state, employment, insurance, the preoperative diagnosis, and communication with physicians.33,42-45)
Conclusions
Although the surgical outcome among TTS patients met their preoperative expectation, they were less satisfied with their treatment outcome than patients operated for CTS. Patients contemplating TTS surgery must be informed that the operation may not yield a completely satisfactory result.
Conflicts of Interest Disclosure
The authors declare they have no conflicts of interest and no commercial relationships and received no support from pharmaceutical or other companies. All authors are members of The Japan Neurosurgical Society (JNS) and have completed the Self-reported COI Disclosure Statement Forms available at the website for JNS members.
References
- 1). Ahmad M, Tsang K, Mackenney PJ, Adedapo AO: Tarsal tunnel syndrome: A literature review. Foot Ankle Surg 18: 149-152, 2012 [DOI] [PubMed] [Google Scholar]
- 2). Kim K, Isu T, Morimoto D, et al. : Neurovascular bundle decompression without excessive dissection for tarsal tunnel syndrome. Neurol Med Chir 54: 901-906, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3). Kokubo R, Kim K, Isu T, Morimoto D, Iwamoto N, Morita A: Quality of life effects of pain from para-lumbar- and lower extremity entrapment syndrome and carpal tunnel syndrome and comparison of the effectiveness of surgery. Acta Neurochir 162: 1431-1437, 2020 [DOI] [PubMed] [Google Scholar]
- 4). Kokubo R, Kim K, Isu T, et al. : The impact of tarsal tunnel syndrome on cold sensation in the pedal extremities. World Neurosurg 92: 249-254, 2016 [DOI] [PubMed] [Google Scholar]
- 5). McSweeney SC, Cichero M: Tarsal tunnel syndrome - A narrative literature review. Foot 25: 244-250, 2015 [DOI] [PubMed] [Google Scholar]
- 6). Iborra A, Villanueva M, Barrett SL, Rodriguez-Collazo E, Sanz P: Anatomic delineation of tarsal tunnel innervation via ultrasonography. J Ultrasound Med 37: 1325-1334, 2018 [DOI] [PubMed] [Google Scholar]
- 7). Kinoshita M, Okuda R, Morikawa J, Jotoku T, Abe M: The dorsiflexion-eversion test for diagnosis of tarsal tunnel syndrome. J Bone Joint Surg Am 83: 1835-1839, 2001 [DOI] [PubMed] [Google Scholar]
- 8). Moroni S, Zwierzina M, Starke V, Moriggl B, Montesi F, Konschake M: Clinical-anatomic mapping of the tarsal tunnel with regard to Baxter's neuropathy in recalcitrant heel pain syndrome: Part I. Surg Radiol Anat 41: 29-41, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9). Nariai M, Kim K, Kawauchi M, et al. : [Magnetic resonance imaging conditions for imaging of the tarsal tunnel]. No Shinkei Geka 46: 11-19, 2018(in Japanese with English abstract) [DOI] [PubMed] [Google Scholar]
- 10). Kim K, Kokubo R, Isu T, et al. : Magnetic Resonance Imaging findings in patients with Tarsal Tunnel Syndrome. Neurol Med Chir. doi: 10.2176/jns-nmc.2022-0118 Epub 2022 Sep 30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11). Bouysset M, Denarié D, Coillard JY, et al. : Predictive factors of effective tibial nerve release in tarsal tunnel syndrome. Foot Ankle Surg 28: 610-615, 2022 [DOI] [PubMed] [Google Scholar]
- 12). Mullick T, Dellon AL: Results of decompression of four medial ankle tunnels in the treatment of tarsal tunnels syndrome. J Reconstr Microsurg 24: 119-126, 2008 [DOI] [PubMed] [Google Scholar]
- 13). Sammarco GJ, Chang L: Outcome of surgical treatment of tarsal tunnel syndrome. Foot Ankle Int 24: 125-131, 2003 [DOI] [PubMed] [Google Scholar]
- 14). Doneddu PE, Coraci D, Loreti C, Piccinini G, Padua L: Tarsal tunnel syndrome: Still more opinions than evidence. Status of the art. Neurol Sci 38: 1735-1739, 2017 [DOI] [PubMed] [Google Scholar]
- 15). Vega-Zelaya L, Iborra Á, Villanueva M, Pastor J, Noriega C: Ultrasound-guided near-nerve needle sensory technique for the diagnosis of tarsal tunnel syndrome. J Clin Med 10: 3065, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16). Sakamoto K, Isu T, Kim K, et al. : Treatment of coexisting paralumbar spine diseases in patients with lumbar disc herniation. Neurol Med Chir 60: 368-372, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17). Gould JS: Tarsal tunnel syndrome. Foot Ankle Clin 16: 275-286, 2011 [DOI] [PubMed] [Google Scholar]
- 18). Patel AT, Gaines K, Malamut R, et al. : Usefulness of electrodiagnostic techniques in the evaluation of suspected tarsal tunnel syndrome: An evidence-based review. Muscle Nerve 32: 236-240, 2005 [DOI] [PubMed] [Google Scholar]
- 19). Geoghegan CE, Mohan S, Cha EDK, Lynch CP, Jadczak CN, Singh K: Achievement of a minimum clinically important difference for back disability is a suitable predictor of patient satisfaction among lumbar fusion patients. World Neurosurg 152: e94-e100, 2021 [DOI] [PubMed] [Google Scholar]
- 20). Mooney J, Michalopoulos GD, Alvi MA, et al. : Minimally invasive versus open lumbar spinal fusion: A matched study investigating patient-reported and surgical outcomes. J Neurosurg Spine 14: 1-14, 2021 [DOI] [PubMed] [Google Scholar]
- 21). Yoo JS, Patel DV, Mayo BC, et al. : Postoperative satisfaction following lumbar spinal fusion surgery: Patient expectation versus actuality. J Neurosurg Spine 26: 1-7, 2019 [DOI] [PubMed] [Google Scholar]
- 22). Gepstein R, Arinzon Z, Adunsky A, Folman Y: Decompression surgery for lumbar spinal stenosis in the elderly: Preoperative expectations and postoperative satisfaction. Spinal Cord 44: 427-431, 2006 [DOI] [PubMed] [Google Scholar]
- 23). Kadzielski J, Malhotra LR, Zurakowski D, Lee SGP, Jupiter JB, Ring D: Evaluation of preoperative expectations and patient satisfaction after carpal tunnel release. J Hand Surg Am 33: 1783-1788, 2008 [DOI] [PubMed] [Google Scholar]
- 24). Li Y, Luo W, Wu G, Cui S, Zhang Z, Gu X: Open versus endoscopic carpal tunnel release: A systematic review and meta-analysis of randomized controlled trials. BMC Musculoskelet Disord 21: 272, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25). Gerritsen AA, de Vet HC, Scholten RJ, Bertelsmann FW, de Krom MC, Bouter LM: Splinting vs surgery in the treatment of carpal tunnel syndrome: A randomized controlled trial. JAMA 288: 1245-1245, 2002 [DOI] [PubMed] [Google Scholar]
- 26). Basiri K, Katirji B: Practical approach to electrodiagnosis of the carpal tunnel syndrome: A review. Adv Biomed Res 4: 50, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27). Fujihara F, Isu T, Kim K, et al. : Transposition using indocyanine green for tarsal tunnel decompression. World Neurosurg 141: 142-148, 2020 [DOI] [PubMed] [Google Scholar]
- 28). Kim K, Isu T, Morimoto D, Kokubo R, Fujihara F, Morita A: Perioperative complications and adverse events after surgery for peripheral nerve- and para-lumbar spine diseases. Neurol Med Chir 62: 75-79, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29). Rönnberg K, Lind B, Zoëga B, Halldin K, Gellerstedt M, Brisby H: Patients' satisfaction with provided care/information and expectations on clinical outcome after lumbar disc herniation surgery. Spine 32: 256-261, 2007 [DOI] [PubMed] [Google Scholar]
- 30). Krauss P, Sonnleitner C, Reinartz F, Meyer B, Meyer HS: Patient-reported expectations, outcome and satisfaction in thoracic and lumbar spine stabilization surgery: A prospective study. Surgeries 1: 63-76, 2020 [Google Scholar]
- 31). McKinley RK, Stevenson K, Adams S, Manku-Scott TK: Meeting patient expectations of care: The major determinant of satisfaction with out-of-hours primary medical care? Fam Pract 19: 333-338, 2002 [DOI] [PubMed] [Google Scholar]
- 32). Jackson JL, Kroenke K: The effect of unmet expectations among adults presenting with physical symptoms. Ann Intern Med 134: 889-897, 2001 [DOI] [PubMed] [Google Scholar]
- 33). Soroceanu A, Ching A, Abdu W, McGuire K: Relationship between preoperative expectations, satisfaction, and functional outcomes in patients undergoing lumbar and cervical spine surgery: A multicenter study. Spine 37: E103-E108, 2012 [DOI] [PubMed] [Google Scholar]
- 34). Pfeiffer WH, Cracchiolo A 3rd: Clinical results after tarsal tunnel decompression. J Bone Joint Surg Am 76: 1222-1230, 1994 [DOI] [PubMed] [Google Scholar]
- 35). Reichert P, Zimmer K, Wnukiewicz W, Kuliński S, Mazurek P, Gosk J: Results of surgical treatment of tarsal tunnel syndrome. Foot Ankle Surg 21: 26-29, 2015 [DOI] [PubMed] [Google Scholar]
- 36). Bracilovic A, Nihal A, Houston VL, Beattie AC, Rosenberg ZS, Trepman E: Effect of foot and ankle position on tarsal tunnel compartment volume. Foot Ankle Int 27: 431-437, 2006 [DOI] [PubMed] [Google Scholar]
- 37). Skalley TC, Schon LC, Hinton RY, Myerson MS: Clinical results following revision tibial nerve release. Foot Ankle Int 15: 360-367, 1994 [DOI] [PubMed] [Google Scholar]
- 38). Jerosch J, Schunk J, Khoja A: Results of surgical treatment of tarsal tunnel syndrome. Foot Ankle Surg 12: 205-208, 2006 [Google Scholar]
- 39). Bailie DS, Kelikian AS: Tarsal tunnel syndrome: Diagnosis, surgical technique, and functional outcome. Foot Ankle Int 19: 65-72, 1998 [DOI] [PubMed] [Google Scholar]
- 40). Seidel GK, Jamal SA, Weidert E, et al. : Predictive outcome modeling of preoperative clinical symptoms and electrodiagnostic data in tarsal tunnel surgery. J Brachial Plex Peripher Nerve Inj 16: e37-e45, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41). Heimkes B, Posel P, Stotz S, Wolf K: The proximal and distal tarsal tunnel syndromes. Int Orthop 11: 193-196, 1987 [DOI] [PubMed] [Google Scholar]
- 42). Cook C, Baxendale S: Preoperative predictors of postoperative satisfaction with surgery. Epilepsy Behav 129: 108612, 2022 [DOI] [PubMed] [Google Scholar]
- 43). Jackson JL, Chamberlin J, Kroenke K: Predictors of patient satisfaction. Soc Sci Med 52: 609-620, 2001 [DOI] [PubMed] [Google Scholar]
- 44). Rethorn ZD, Cook CE, Park C, et al. : Social risk factors predicting outcomes of cervical myelopathy surgery. J Neurosurg Spine 28: 1-8, 2022 [DOI] [PubMed] [Google Scholar]
- 45). Rethorn ZD, Garcia AN, Cook CE, Gottfried ON: Quantifying the collective influence of social determinants of health using conditional and cluster modeling. PLoS One 15: e0241868, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]