Abstract
Background and study aims Gastric per-oral endoscopic myotomy (G-POEM) has been recently compared with surgical techniques (i. e. pyloromyotomy and pyloroplasty) for managing patients with refractory gastroparesis. Given the varying results, we performed a systematic review and meta-analysis of available studies to assess the safety and efficacy of each technique.
Patients and methods A comprehensive review of the literature using the following databases was undertaken through July 29, 2022: MEDLINE, Embase, Web of Science, KCI – Koran Journal index, Global Index Medicus, and Cochrane. Comparative studies including case-control, cohort and randomized controlled trials (RCTs) were included. Random effects model using DerSimonian laird approach was used to compare outcomes. Relative risk (RR) and mean difference (MD) were calculated for binary and continuous outcomes respectively.
Results A total of four studies with 385 patients (216 in the G-POEM group and 169 in the surgical group were included. The mean age was 46.9 (± 3.41) and 46.2 (± 0.86) and the female proportion was 79.6 % and 74.0 % for the G-POEM and surgery group respectively. The mean procedural time (MD: –59.47 mins, P < 0.001) and length of hospital stay (MD: –3.10 days, P < 0.001) was significantly lower for G-POEM compared to surgery. The post procedure GCSI score (MD: –0.33, P = 0.39) and reduction in GCSI score preoperatively and postoperatively (MD: 0.27, P = 0.55) was not significantly different.
Conclusions G-POEM appears promising as it may provide a cost-effective approach for managing refractory gastroparesis compared to surgical techniques. RCTs are needed to further confirm these results.
Introduction
Gastroparesis is a functional disorder that is characterized by delayed gastric emptying in the absence of mechanical gastric outlet obstruction leading to symptoms including nausea, vomiting, pain, early satiety, and bloating 1 . The underlying etiologies can be multifactorial; however, the most observed are diabetes, postsurgical, or idiopathic 2 . Ye et al. demonstrated that the overall prevalence of gastroparesis was 267.7 per 100,000 US adults 3 . The management of gastroparesis entails lifestyle modification and/or use of prokinetic agents as first line therapy. In many patients, these agents tend to lose efficacy over time and patients require additional modalities for persistent or refractory symptoms. These include use of gastric stimulators, Roux-en-Y gastric bypass, pyloroplasty/pyloromyotomy, gastrojejunostomy, and/or subtotal gastrectomy 4 .
An endoscopic approach called gastric per-oral endoscopic myotomy (G-POEM) has been evaluated in patients with refractory gastroparesis with notable clinical success 5 . During G-POEM, submucosal gastric tunneling is performed to approach, identify, and incise the musculature of the pylorus, similar to technique employed for POEM in the esophagus to treat patients with achalasia 6 . Recent meta-analyses have demonstrated varying clinical success and efficacy for G-POEM in managing refractory gastroparesis. Meyboodi et al. demonstrated that G-POEM was associated with reduction of mean Gastroparesis Cardinal Symptom Index (GCSI) value by –1.57 (confidence interval (CI): –2.2 to –0.9) and mean gastric emptying by 22.3 % (CI: –32.9 %–11.6 %) after 5 days 7 . Similarly, Kamal et al. showed reduction of GCSI by –1.4 (CI: –1.9–0.9) at 1-year follow-up 8 . Neither of these meta-analyses compared G-POEM to surgical approach.
Given the lack of comparative data, we sought to perform a systematic review and meta-analysis of studies comparing the endoscopic approach i. e. G-POEM, to the surgical pyloromyotomy for managing refractory gastroparesis.
Patients and methods
Search strategy
This meta-analysis was conducted in accordance to guidelines provided by Preferred Reporting items for Systematic Review and Meta-Analysis (PRISMA) 9 . A detailed search of the following databases was undertaken from inception through July 29, 2022: MEDLINE (PubMed interface, National Center for Biotechnology Information), Embase (Elsevier), Web of Science Core Collection (Clarivate), KCI – Koran Journal index, Global Index Medicus, and Cochrane Central Register of Controlled Trials (Cochrane/Wiley). The initial search strategy was suggested by lead investigator (M.A.) that was further refined and executed by expert medical librarian (W.L.-S.) using appropriate medical subject headings and related vocabulary and syntax. The following keywords were utilized: “Pyloromyotomy,” “POEM,” “Endoscopy,” “Surgery,” and “Gastroparesis.” A sample search strategy using PubMed is highlighted in Supplementary Table 1. Our search was not restricted to language. Citations were imported and deduplicated using EndNote X9 bibliographic management software (Clarivate, Philadelphia, Pennsylvania, United States). We did not prepare a review protocol prior to screening/data extraction process.
Study definitions
Symptoms related to gastroparesis were quantified using Gastroparesis Cardinal Symptom Index (GCSI) score, a previously validated survey that scores on post-prandial fullness, nausea/vomiting, and bloating 10 . Clinical success was defined as improved gastric emptying study (GES) and/or improvement in GCSI score based on individual study defined criteria on follow-up. The surgical group included patients that underwent either pyloromyotomy and/or pyloroplasty using any approach (open, laparoscopic, robotic).
Inclusion/exclusion criteria
The studies were included based on following parameters: (1) Patients: Adult patients (≥ 18 years old with refractory gastroparesis of any etiology; (2) Intervention: G-POEM; (3) Control: Surgical pyloromyotomy (laparoscopic, robotic, and/or open) and (4) Outcomes: Procedure duration, length of stay (LOS), complications, clinical success, post operative GCSI score. We included comparative studies i. e. case-control, retrospective/prospective cohort and/or randomized controlled trials (RCTs). We included abstracts if they met all study criteria. We excluded case reports, case series < 10 patients, single arm studies, guidelines, and reviews. If more than one publication was notable for overlapping data, we included the most recent and updated study to capture the most comprehensive data.
Screening and data collection
Study screening and data extraction was performed by two independent reviewers (M.A.) and (M.G). The initial screening was performed using titles and abstracts. Pertinent studies were then further screened using full texts (where applicable). Data was extracted using Microsoft Excel (Microsoft, Redmond, Washington, United States). Data regarding demographics (age, gender), etiology of gastroparesis (diabetic, postsurgical, and unknown/idiopathic), type of surgery (robotic, laparoscopic, open), and outcomes (LOS, procedure duration, complications, clinical success, post operative GCSI score) were collected. Any discrepancy during screening and data extraction was resolved through mutual discussion.
Data synthesis and analysis
Given the presumed heterogeneity of different surgical approaches and etiology of gastroparesis, Random effects model using DerSimonian-Laird approach was used a priori for pooling and comparing outcomes. A correction factor of “0.5” was added when outcomes were 0 for a given study. Relative risk (RR) for dichotomous outcomes and mean difference (MD) for continuous outcomes were calculated along with 95 % confidence interval (CI) and P value. P < 0.05 was considered significant for all assessed outcomes. Study heterogeneity was assessed using the I 2 statistical and value > 50 % was considered substantial heterogeneity 11 . Statistical analysis was performed using Open Meta Analyst (CEBM, University of Oxford, Oxford, United Kingdom).
The GCSI score was calculated for each group preoperatively and postoperatively. Comparison was made between postoperative GCSI score directly between the two groups as well as between the reduction/mean difference (MD) of preoperative and postoperative GCSI between the two groups.
A subgroup analysis was performed based on individual surgical techniques i. e. pyloroplasty or pyloromyotomy if two or more studies were available reporting outcomes.
Bias assessment
The risk of bias for individual studies was performed using Newcastle Ottawa scale (NCOS) for observational/cohort studies and Cochrane risk of bias tool for RCTs 12 13 . Publication bias was undertaken via funnel plot for qualitative assessment and Egger’s regression analysis for quantitative assessment using P value. If publication bias was noted, we attempted the “trim-and-fill” method to assess the changes in effect size for respective outcome.
Results
A total of 516 studies were identified, of which 324 remained after machine deduplication was undertaken. After rigorous screening, a total of four studies (1 abstract and 3 full texts) were selected for inclusion in the meta-analysis 14 15 16 17 . The details of study selection are highlighted in the PRISM flow diagram ( Fig. 1 ). Of the included studies, all were observational. G-POEM was used as an intervention in all studies. For surgical techniques, two studies used pyloromyotomy 14 16 and two studies used pyloroplasty 15 17 . The demographic details and patient characteristics of included studies are summarized in Table 1 .
Fig. 1.
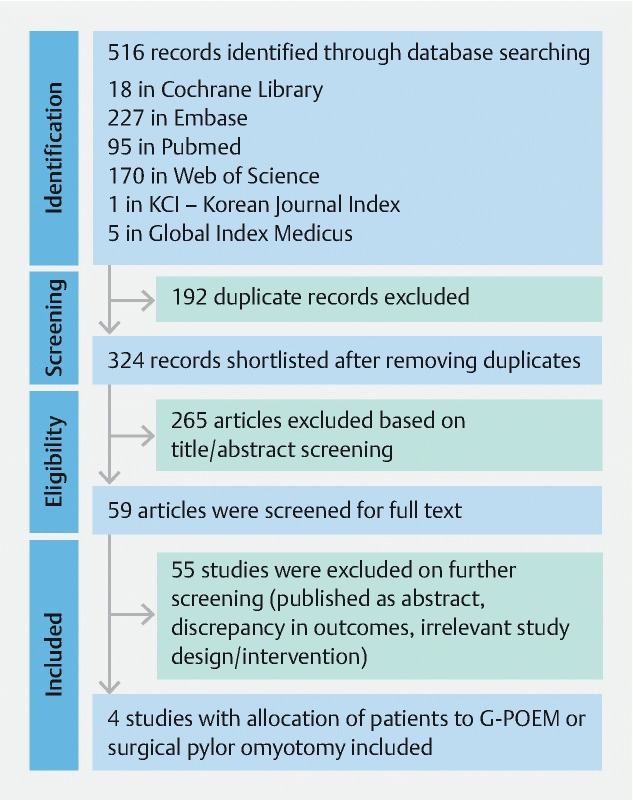
PRISMA flow diagram (G-POEM: Gastric per-oral endoscopic myotomy). From: Page MJ, McKenzie JE, Bossuyt PM et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71.
Table 1. Study details and demographics of included patients.
| Study, year | Landreneau, 2019 | Pioppo, 2021 | AbiMansour, 2020 | Clapp, 2022 | |
| Type of study | Case control study | Retrospective | Retrospective | Prospective | |
| Interventions | Group 1: G-POEM Group 2: Laparoscopic pyloroplasty |
Group 1: G-POEM Group 2: Laparoscopic pyloromyotomy |
Group 1: G-POEM Group 2: pyloromyotomy |
Group 1: G-POEM Group 2: Robotic pyloromyotomy |
|
| Total patients | Group 1: 30 Group 2: 30 |
Group 1: 39 Group 2: 63 |
Group 1: 84 Group 2: 28 |
Group 1: 63 Group 2: 48 |
|
| Mean age, (SD) | Group 1: 44.1 (13.5) Group 2: 45.4 (14.5) |
Group 1: 49 (16.5) Group 2: 45.8 (10.3) |
Group 1: 50.6 (16.9) Group 2: 46.2 (17.4) |
Group 1: 43.9 (14.1) Group 2: 47.4 (12.4) |
|
| Female (%) | Group 1: 23 (76.7 %) Group 2: (76.7 %) |
Group 1: 33 (84.6 %) Group 2: 36 (57.1 %) |
Group 1: 63 (75.0 %) Group 2: 22 (78.6 %) |
Group 1: 53 (84.1 %) Group 2: 44 (91.7 %) |
|
| Mean BMI, (SD) | Group 1: 24.9 (7.1) Group 2: 26.1 (6.7) |
Group 1: 27.7 (7.7) Group 2: 27.6 (7.5) |
Group 1: 6.09 (25.1) Group 2: 25.1 (5.2) |
Group 1: 28.7 (8.2) Group 2: 27.3 (5.5) |
|
| Etiology of Gastroparesis | Diabetic | Group 1: 5 Group 2: 5 |
Group 1: 13 Group 2: 14 |
Group 1: 23 Group 2: 3 |
Group 1: NR Group 2: NR |
| Postsurgical | Group 1: 6 Group 2: 6 |
Group 1: 4 Group 2: 16 |
Group 1: 23 Group 2: 12 |
Group 1: NR Group 2: NR |
|
| Idiopathic/ unknown | Group 1: 19 Group 2: 19 |
Group 1: 22 Group 2: 33 |
Group 1: 38 Group 2: 13 |
Group 1: NR Group 2: NR |
|
| Length of follow-up | 90 days | Postoperative | NR | 90 days |
BMI, body mass index; G-POEM, gastric per-oral endoscopic myotomy; NR, not reported; SD, standard deviation.
A total of 385 patients were included (216 in the G-POEM group and 169 in the surgical group). The mean age was 46.9 (± 3.41) and 46.2 (± 0.86) for G-POEM and surgery, respectively. The female proportion was 79.6 % and 74.0 % for G-POEM and surgery, respectively. The outcomes for individual studies are shown in Table 2 .
Table 2. Outcomes for individual studies.
| Study, year | Mean procedure duration, mins (SD) | Mean LOS, days (SD) | Mean Postoperative GCSI score, (SD) | Mean reduction in GCSI pre/post, (SD) | Clinical success | Normal GES | Complication rates | Reintervention rates | Readmisson rates |
| Landreneau, 2019 | G-POEM: 33.9 (18.8) Surgery: 99.9 (41.8) |
G-POEM: 1.4 (1.0) Surgery: 4.6 (5.6) |
G-POEM: 2.4 (1.5) Surgery: 2.3 (1.5) |
G-POEM: 1.6 (0.3) Surgery: 1.7 (0.3) |
G-POEM: 6 Surgery: 5 |
G-POEM: 8 Surgery: 7 |
G-POEM: 1 Surgery: 5 |
G-POEM: 1 Surgery: 1 |
G-POEM: 2 Surgery: 5 |
| Pioppo, 2021 | G-POEM: 58.0 (27.6) Surgery: 78.4 (13.1) |
G-POEM: 1.3 (1.0) Surgery: 4.2 (0.7) |
G-POEM: 1 (0.8) Surgery: 1.7 (0.6) |
G-POEM: 2.8 (0.8) Surgery: 1.5 (0.7) |
G-POEM: 36 Surgery: 52 |
G-POEM: NR Surgery: NR |
G-POEM: 5 Surgery: 21 |
G-POEM: NR Surgery: NR |
G-POEM: NR Surgery: NR |
| AbiMansour, 2020 | G-POEM: 60.6 (29.6) Surgery: 151.8 (72.0) |
G-POEM: 1.5 (2.4) Surgery: 10.9 (20.8) |
G-POEM: 1.1 (1.3) Surgery: 2.3 (1.1) |
G-POEM: 1.8 (1.6) Surgery: 1 (0.9) |
G-POEM: 24 Surgery: 9 |
G-POEM: 12 Surgery: 6 |
G-POEM: 9 Surgery: 11 |
G-POEM: 8 Surgery: 2 |
G-POEM: NR Surgery: NR |
| Clapp, 2022 | G-POEM: 25.3 (6.1) Surgery: 91.5 (10.4) |
G-POEM: NR Surgery: NR |
G-POEM: 2.5 (1.2) Surgery: 2.0 (1.1) |
G-POEM: 0.9 (1.2) Surgery: 1.9 (1.2) |
G-POEM: NR Surgery: NR |
G-POEM: NR Surgery: NR |
G-POEM: 12 Surgery: 6 |
G-POEM: NR Surgery: NR |
G-POEM: 12 Surgery: 3 |
GCSI, Gastroparesis Cardinal Symptom Index; GES, gastric emptying study; G-POEM, gastric per-oral endoscopic myotomy; LOS, length of stay; lNR, not reported; SD, standard deviation.
Procedure duration
The mean procedure time was significantly lower for G-POEM compared to surgery (MD: –59.47 min, CI: –87.57 to –31.37 min, P < 0.001, I 2 = 96.6 %) ( Fig. 2a ). Consistent results were obtained on subgroup analysis for patients that underwent surgical pyloroplasty (MD: –66.24 min, CI: –69.84 to –62.64 min, P < 0.001, I 2 = 0 %). The subgroup analysis although showed shorter duration for G-POEM compared to surgical pyloromyotomy however this result was not statistically significant (MD: –54.59 min, CI: –123.95–14.78 min, P = 0.12, I 2 = 95.65 %).
Fig. 2.
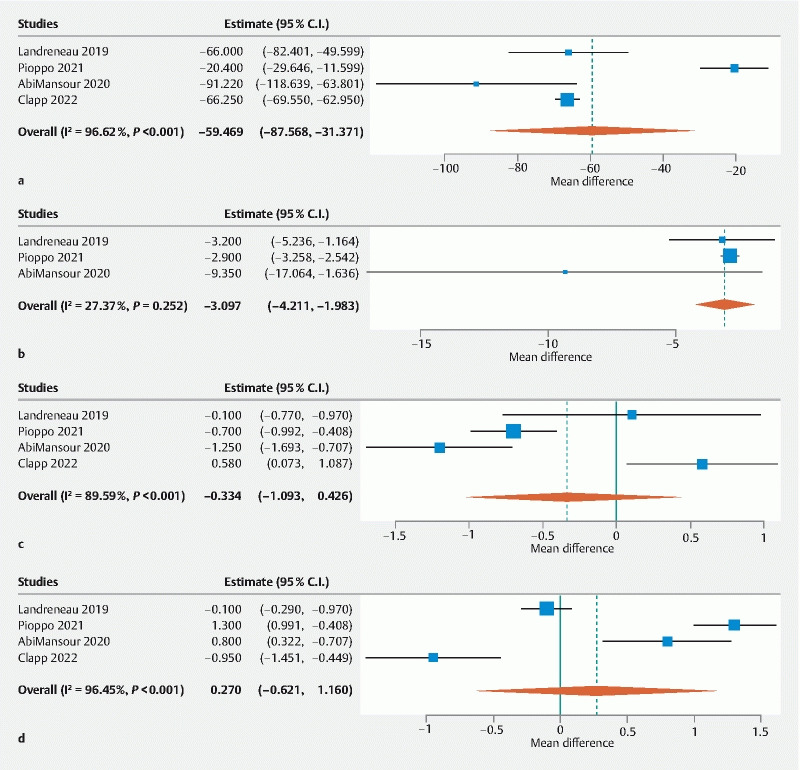
Mean difference for a procedure duration, b LOS, c postoperative GCSI, d preoperative/postoperative difference in GCSI between G-POEM and surgical group. CI, confidence interval; LOS, length of stay.
Length of stay
The LOS was significantly shorter for the G-POEM group compared to the surgical group (MD: –3.10 days, CI: –4.21 to –1.98 days, P < 0.001, I 2 = 27.4 %) ( Fig. 2b ). The subgroup analysis was possible for surgical pyloromyotomy only. Although lower LOS was noted for G-POEM, the result did not achieve statistical significance (MD: –4.93, CI: –10.80–0.94, P = 0.10, I 2 = 62.7 %).
Post-GCSI score
The post-procedure GCSI was evaluated by all four studies and was not significantly different (MD: –0.33, CI: –1.09–0.43, P = 0.39, I 2 = 89.6 %) ( Fig. 2c ). The subgroup analysis demonstrated higher post operative GCSI score for G-POEM group compared to surgical pyloroplasty group (MD: 0.46, CI: 0.02–0.90, P = 0.04, I 2 = 0 %). However, G-POEM showed lower post operative GCSI score compared to surgical pyloromyotomy group (MD: – 0.91, CI: –1.39 to –0.43, P < 0.001, I 2 = 65.82 %).
The reduction in the GCSI score preoperatively and postoperatively between the G-POEM and surgical groups was compared and no difference was observed (MD: 0.27, CI: –0.62 – 1.16, P = 0.55, I 2 = 96.45 %) ( Fig. 2d ). Consistent result was obtained when G-POEM was compared to surgical pyloroplasty only (MD: –0.49, CI: –1.32–0.34, P = 0.25, I 2 = 89.7 %). G-POEM showed higher reduction of GCSI postoperatively compared to surgical pyloromyotomy group (MD: 1.09, CI: 0.60–1.57, P < 0.001, I 2 = 66.32 %).
Clinical success/normal GES
Three studies assessed clinical success on follow-up. No significant difference in clinical success was noted for either group (OR: 0.98, CI: 0.32–3.00, P = 0.98, I 2 = 49.34 %) ( Fig. 3a ). Subgroup analysis between surgical pyloromyotomy group and G-POEM was also consistent (OR: 0.95, CI: 0.14–6.69, P = 0.96, I 2 = 74.7 %).
Fig. 3.
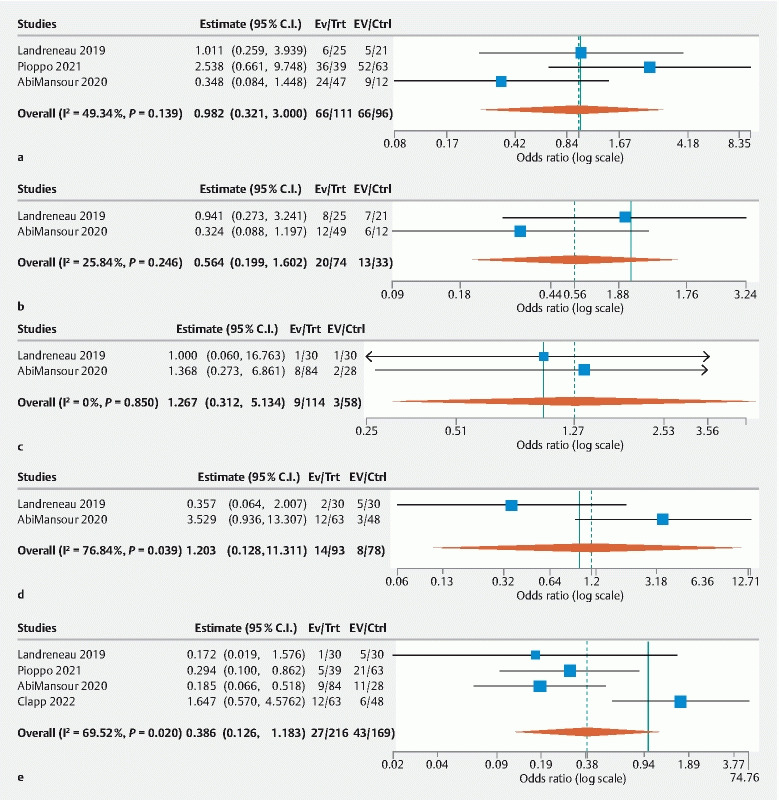
Odds ratio for a clinical success, b normal GES, c reintervention rate, d readmission rate, and e any complication rates between G-POEM and surgical group. CI, confidence interval.
The postoperative rate of normal GES was assessed by two studies and was not significantly different between the G-POEM and surgical groups (OR: 0.56, CI: 0.20–1.60, P = 0.28, I 2 = 25.84 %) ( Fig. 3b ).
Readmission/reintervention rate
Only two studies assessed the reintervention rates, and no significant difference was noted between the G-POEM and surgical group (OR: 1.27, CI: 0.31–5.13, P = 0.74, I 2 = 0 %). A subgroup analysis was not applicable ( Fig. 3c ).
Only two studies assessed readmission rate and no significant difference was noted between the G-POEM and surgical groups (OR: 1.20, CI: 0.13–11.31, P = 0.87, I 2 = 76.5 %) ( Fig. 3 d ). Both studies used pyloroplasty and hence subgroup analysis for pyloromyotomy was not applicable.
Adverse events
The overall rates of adverse events (AEs) were assessed by all studies and no significant difference was noted between G-POEM and surgery (OR: 39, CI: 0.13–1.18, P = 0.10, I2 = 69.5 %) ( Fig. 3e ). Subgroup analysis was consistent for G-POEM and surgical pyloroplasty (OR: 0.66, CI: 0.08–5.80, P = 0.71, I 2 = 69.2 %). Lower overall rates of AEs were noted for G-POEM compared to pyloromyotomy (OR: 023, CI: 0.11–0.49, P < 0.001, I 2 = 0 %).
Risk of bias
The risk of bias using the NCOS is highlighted in Supplementary Table 2. The risk of bias was applicable for three studies with full text, and each had a score of 6 or more signifying moderate to low risk 15 16 17 . One study was an abstract and hence risk of bias assessment was not possible 14 .
Discussion
Gastroparesis is a debilitating disease that severely impairs the quality of life of affected patients. Unfortunately, there are limited interventions for the management of gastroparesis. The alteration of pyloric musculature via mechanical disruption, to reduce barriers to gastric outflow, using surgical and endoscopic techniques have been explored.
The approaches that have been performed to achieve pyloric muscle disruption include pyloroplasty or pyloromyotomy. The difference between the two techniques is that in pyloromyotomy, a longitudinal incision is made in the avascular plane after the duodenum is grasped just distal to the level of pylorus. The muscle fibers are spread with a spreader and pyloric edges are mobilized thus confirming successful pyloromyotomy 16 . In pyloroplasty, a longitudinal incision is performed through the pylorus and the incision is then closed using Heineke-Mikulicz technique 15 . A previous retrospective study comparing these two techniques in children with delayed gastric emptying and gastroesophageal reflux did not find an advantage of one over the other 18 . Toro et al. assessed the impact of laparoscopic pyloroplasty on patients with gastroparesis and noted improvement of symptoms in 82 % of patients postoperatively 19 . Similarly, Shada et al. described the largest single center experience for pyloroplasty and noted a 90 % improvement in GES among affected patients following the procedure 20 . G-POEM has shown promise with similar efficacy compared to surgical techniques. Landreneau et al. demonstrated that G-POEM and laparoscopic pyloroplasty were similar in terms of postoperative GCSI score (2.4 ± 1.5 vs 2.3 ± 1.5, P = 0.85) and improved GES (85.7 % vs 83.3 %, P = 0.91) 15 . In this study, we demonstrated that G-POEM resulted in similar efficacy to surgery with regard to the following parameters: postoperative GCSI score (MD: –0.33, CI: –1.09–0.43), reduction in GCSI score preoperatively and postoperatively (MD: 0.27, CI: –0.62–1.16), and similar rates of obtaining a normal GES (OR: 0.56, CI: 0.20–1.60).
The major attractiveness of G-POEM is its cost-effectiveness. A previous study showed that G-POEM overall had a 26 % lower procedural cost than surgical pyloroplasty 21 . In this study, we further demonstrated that G-POEM also reduced the overall procedure time compared to surgery (MD: –59.47 min, CI: – 87.57 to –31.37 min) and overall length of hospital stay (MD: –3.10 days, CI: –4.21 to –1.98), both of which may contribute to further reducing the cost. The overall lower procedural time reduces the risk of prolonged anesthesia as well.
We compare our study to a previously published article on similar topic by Mohan et al. The authors performed systematic review, pooled analysis and comparison between the two groups i. e. G-POEM and surgical pyloroplasty. The authors demonstrated similar clinical success between surgical pyloroplasty, and G-POEM based on GES and GCSI score which is in line with our analysis 22 . However, the authors could not perform the analysis of mean difference between pre- and post-GCSI score between the two groups due to lack of data. Further, the comparison of clinical success between two groups was made indirectly as all included studies except one were single arm. Our study only included comparative studies and hence we were able to perform comparative meta-analysis on more outcomes.
Interestingly, a lower overall postoperative GCSI was noted for surgical pyloroplasty compared to G-POEM, however, the reduction in GCSI preoperatively and postoperatively were comparable between the two groups. One major limitation of this analysis was that only two studies utilized pyloroplasty. Furthermore, one of the studies explored the efficacy of pyloroplasty using a laparoscopic approach and other study used a robotic technique. We were unable to account for this heterogeneity in our outcome. Future RCTs, directly comparing individual surgical approaches, can further expand on the relative benefits and efficacy of each technique.
Our study had some notable limitations. The most important limitations were the lack of RCTs as well as low number of included studies with lower overall patients included in respective intervention groups. We were unable to account for outcomes based on specific etiology of gastroparesis, surgical access (open, laparoscopic, robotic), and prior exposure to other interventions such as medications (metoclopramide, erythromycin, domperidone) or botulinum toxin injection. Further, the included studies mostly included patients at highly advanced tertiary care centers, and hence the generalizability of the results is questionable. Lastly, the follow-up of patients was not consistent across the studies and hence important outcomes such as duration and timing of improvement in symptoms, GES and reduction in GCSI were not consistently assessed. All these aspects can explain the high heterogeneity noted in our outcomes. Despite the limitations, this study provides the largest comprehensive comparative analysis currently available between G-POEM and surgery. We performed subgroup analysis based on type of surgery i. e., pyloroplasty vs pyloromyotomy and although few outcomes were different owing to the low number of studies, these were not clinically significant.
Conclusions
In conclusion, G-POEM may be favored over surgical approach for refractory gastroparesis as it was more cost-effective while demonstrating comparable efficacy. Future randomized controlled trials (RCTs) should be performed to confirm these results.
Footnotes
Competing interests The authors declare that they have no conflict of interest.
Supplementary material :
References
- 1.Camilleri M, Bharucha A E, Farrugia G. Epidemiology, mechanisms and management of diabetic gastroparesis. Clin Gastroenterol Hepatol. 2011;9:e5–e7. doi: 10.1016/j.cgh.2010.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Waseem S, Moshiree B, Draganov P V. Gastroparesis: current diagnostic challenges and management considerations. World J Gastroenterol. 2009;15:25–37. doi: 10.3748/wjg.15.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ye Y, Yin Y, Huh S Y et al. Epidemiology, etiology, and treatment of gastroparesis: real-world evidence from a large US national claims database. Gastroenterology. 2022;162:109–1.21E7. doi: 10.1053/j.gastro.2021.09.064. [DOI] [PubMed] [Google Scholar]
- 4.Jones M P, Maganti K. A systematic review of surgical therapy for gastroparesis. Am J Gastroenterol. 2003;98:2122–2129. doi: 10.1111/j.1572-0241.2003.07721.x. [DOI] [PubMed] [Google Scholar]
- 5.Tan J, Shrestha S M, Wei M et al. Feasibility, safety, and long-term efficacy of gastric peroral endoscopic myotomy (G-POEM) for postsurgical gastroparesis: a single-center and retrospective study of a prospective database. Surg Endosc. 2021;35:3459–3470. doi: 10.1007/s00464-020-07793-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu J, Chen T, Elkholy S et al. Gastric peroral endoscopic myotomy (G-POEM) as a treatment for refractory gastroparesis: long-term outcomes. Can J Gastroenterol Hepatol. 2018;2018:6.409698E6. doi: 10.1155/2018/6409698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aghaie Meybodi M, Qumseya B J, Shakoor D et al. Efficacy and feasibility of G-POEM in management of patients with refractory gastroparesis: a systematic review and meta-analysis. Endosc Int Open. 2019;7:E322–E329. doi: 10.1055/a-0812-1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kamal F, Khan M A, Lee-Smith W et al. Systematic review with meta-analysis: one-year outcomes of gastric peroral endoscopic myotomy for refractory gastroparesis. Aliment Pharmacol Ther. 2022;55:168–177. doi: 10.1111/apt.16725. [DOI] [PubMed] [Google Scholar]
- 9.Page M J, McKenzie J E, Bossuyt P M et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Revicki D A, Rentz A M, Dubois D et al. Development and validation of a patient-assessed gastroparesis symptom severity measure: the Gastroparesis Cardinal Symptom Index. Aliment Pharmacol Ther. 2003;18:141–150. doi: 10.1046/j.1365-2036.2003.01612.x. [DOI] [PubMed] [Google Scholar]
- 11.Shuster J. Review: Cochrane handbook for systematic reviews for interventions, Version 5.1.0, published 3/2011. Julian P.T. Higgins and Sally Green, Editors. Res Synth Methods. 2011;2:126–130. [Google Scholar]
- 12.Deeks J, Dinnes J, D'Amico R.Evaluating non-randomised intervention studies Health Technol Assess 200373–10., 1–173 [DOI] [PubMed] [Google Scholar]
- 13.Higgins J, Altman D, Gotzsche P et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928–d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.AbiMansour J P, Meybodi M A, Ichkhanian Y et al. Gastric peroral endoscopic myotomy compared to surgical pyloromyotomy in the treatment of gastroparesis: A case-matched multicenter study. Gastrointest Endosc. 2020;91:AB6. [Google Scholar]
- 15.Landreneau J P, Strong A T, El-Hayek K et al. Laparoscopic pyloroplasty versus endoscopic per-oral pyloromyotomy for the treatment of gastroparesis. Surg Endosc. 2019;33:773–781. doi: 10.1007/s00464-018-6342-6. [DOI] [PubMed] [Google Scholar]
- 16.Pioppo L, Reja D, Gaidhane M et al. Gastric per-oral endoscopic myotomy versus pyloromyotomy for gastroparesis: An international comparative study. J Gastroenterol Hepatol. 2021;36:3177–3182. doi: 10.1111/jgh.15599. [DOI] [PubMed] [Google Scholar]
- 17.Clapp J H, Gaskins J T, Kehdy F J. [S156] Comparing outcomes of per-oral pyloromyotomy and robotic pyloroplasty for the treatment of gastroparesis. Surg Endosc. 2022 doi: 10.1007/s00464-022-09437-x. [DOI] [PubMed] [Google Scholar]
- 18.Okuyama H, Urao M, Starr G A et al. A comparison of the efficacy of pyloromyotomy and pyloroplasty in patients with gastroesophageal reflux and delayed gastric emptying. J Pediatr Surg. 1997;32:316–320. doi: 10.1016/s0022-3468(97)90201-3. [DOI] [PubMed] [Google Scholar]
- 19.Toro J P, Lytle N W, Patel A D et al. Efficacy of laparoscopic pyloroplasty for the treatment of gastroparesis. J Am Coll Surg. 2014;218:652–660. doi: 10.1016/j.jamcollsurg.2013.12.024. [DOI] [PubMed] [Google Scholar]
- 20.Shada A L, Dunst C M, Pescarus R et al. Laparoscopic pyloroplasty is a safe and effective first-line surgical therapy for refractory gastroparesis. Surg Endosc. 2016;30:1326–1332. doi: 10.1007/s00464-015-4385-5. [DOI] [PubMed] [Google Scholar]
- 21.Mekaroonkamol P, Dacha S, Christofaro S et al. Cost-effectiveness analysis of gastric peroral endoscopic pyloromyotomy (GPOEM) in treatment of refractory gastroparesis 1135. Am J Gastroenterol. 2017;112:S619. [Google Scholar]
- 22.Mohan B P, Chandan S, Jha L K et al. Clinical efficacy of gastric per-oral endoscopic myotomy (G-POEM) in the treatment of refractory gastroparesis and predictors of outcomes: a systematic review and meta-analysis using surgical pyloroplasty as a comparator group. Surg Endosc. 2020;34:3352–3367. doi: 10.1007/s00464-019-07135-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


