Abstract
Functional bladder disorders including overactive bladder and interstitial cystitis may induce problems in many other parts of our body such as brain and gut. In fact, diagnosis is often less accurate owing to their complex symptoms. To have correct diagnosis of these diseases, we need to understand the pathophysiology behind overlapped clinical presentation. First, we focused on reviewing literatures that have reported the link between bladder and brain, as the patients with bladder disorders frequently accompanied mood disorders such as depression and anxiety. Second, we reviewed literatures that have described the relationship between bladder and gut. There exist many evidences of patients who suffered from both bladder and intestinal diseases, such as irritable bowel syndrome and inflammatory bowel disease, at the same time. Furthermore, the interaction between brain and gut, well-known as brain-gut axis, might be a key factor that could change the activity of bladder and vice versa. For example, the affective disorders could alter the activity of efferent nerves or autonomic nervous system that modulate the gut itself and its microbiota, which might cause the destruction of homeostasis in bladder eventually. In this way, the communication between bladder and brain-gut axis might affect permeability, inflammation, as well as infectious etiology and dysbiosis in bladder diseases. In this review, we aimed to find an innovative insight of the pathophysiology in the functional bladder disorders, and we could provide a new understanding of the overlapped clinical presentation by elucidating the pathophysiology of functional bladder disorders.
Keywords: Urinary bladder diseases, Mood disorders, Intestinal diseases, Brain-gut axis
INTRODUCTION
Overactive bladder (OAB)—a complex of symptoms—is defined by the International Continence Society as “urinary urgency with or without incontinence, usually accompanied by increased daytime urinary frequency and nocturia.” OAB can affect the quality of life by interfering with work, social, and other daily activities [1]. Interstitial cystitis/bladder pain syndrome (IC/BPS) has been one of the most commonly diagnosed diseases in the fourth decade or after, although the diagnosis may be delayed depending upon the index of suspicion for the disease. IC/BPS can coexist with other medical conditions, such as fibromyalgia, irritable bowel syndrome (IBS), chronic fatigue syndrome, and Sjögren syndrome. Patients with OAB and IC/BPS frequently exhibit mental health disorders, such as depression and anxiety [2]. Moreover, the disorders are often overlapped with each other. Patients with OAB have a high risk of developing IC/BPS, and vice versa [3].
The current concept of functional bladder disorders is directed away from organ-centered diseases towards symptom-based syndromes, owing to its complex and elusive pathophysiology. Until now, the underlying mechanism and treatment refractoriness of patients with functional bladder disorders has not been clearly understood. Therefore, elucidating a mechanism that causes functional bladder disorders is essential. In this study, we introduce a mechanism that links bladder and brain-gut axis has an important role in causing functional bladder disorder-associated symptoms.
THE COMMUNICATION BETWEEN BLADDER AND BRAIN
Significance of Stress and Corticotropin-Releasing Factor in Bladder Disease
Corticotropin-releasing factor (CRF)—a stress-related peptide that acts in hypothalamic-pituitary-adrenal axis—mainly functions as a hormone that causes secretion of cortisol. CRF is secreted from hypothalamus in response to stress, allowing the body to respond appropriately to a stressful stimulus. Barrington’s nucleus (pontine micturition center) controls micturition [4], and its neurons are considered as one of the sources that release CRF [5]. This indicates that the CRF released from Barrington’s nucleus neurons plays a crucial role in micturition.
It has been reported that CRF secretion influences micturition. When patients with OAB were exposed to stress, they manifested deterioration of symptoms such as frequent urination, urinary urgency, and nocturia, and when 60% of patients with IC/BPS were exposed to stress, bladder pain was exacerbated [6–8]. The results from animal studies were consistent with that from patient-based researches. In animal studies, rats exposed to repeated social stress exhibited worsened urinary tract symptoms [9]. A study that conducted water avoidance test also demonstrated that stress-exposed rats showed increased urinary frequency and shortened voiding interval [10].
Alterations in urodynamic functions, increased levels of CRF receptor (CRF-R) expression, and mRNA in stress-exposed rats were observed when CRF level was increased by CRF administration [11,12]. Given these findings, it is reasonable to say that CRF-R activation followed by a specific signaling pathway plays a crucial role in bladder control. For example, considerable increase in CRF-R2 expression was detected in bladder after 48 hours of cyclophosphamide (CYP) treatment [13]. When rats were treated with a CRF-R antagonist intrathecally, the intercontraction interval and micturition volume were markedly lower than those of rats in the control group [14]. In addition, experiments involving CRF-R agonist or antagonist demonstrated the role of CRF-R signaling. CRF-R1 antagonist-treated rats showed an increased micturition frequency and a decreased bladder capacity [15,16]. Visceromotor responses of rats to urinary bladder distension were elevated when treated with a CRF-R2 agonist (urocortin), and this elevation was suppressed when treated together with a CRF-R2 antagonist (antisauvagine-30) [12] (Fig. 1).
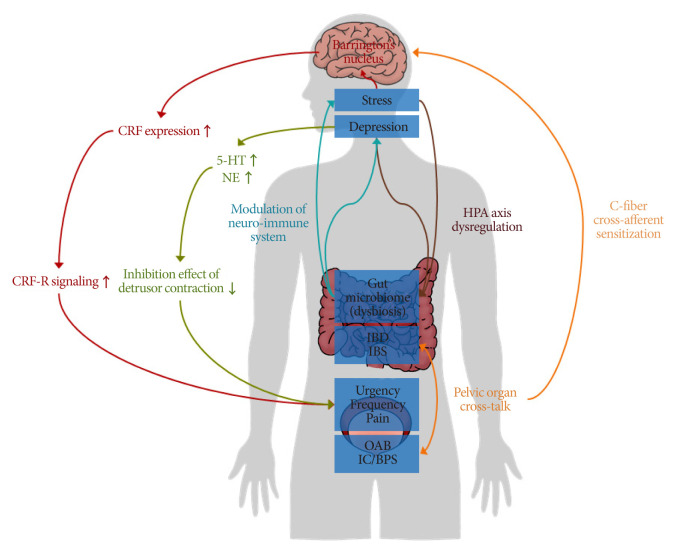
Fig. 1.
Functional bladder disorders have close relationship with brain-gut axis. Stress/depression usually induces overexpression of corticotropin-releasing factor (CRF), and this makes urinary urgency, frequency, and pain. The affective disorders in brain induce dysregulation of serotonin (5-hydroxy tryptamine, 5-HT) and norepinephrine (NE), and altered levels of these neurotransmitters could decrease inhibition effect of detrusor contraction. It could also increase risks of urinary urgency, frequency and pain. The noxious signal from bladder can affect the sensitivity of gut afferent through cross-sensitization. Cross-sensitization is one evidence of cross-talk between bladder and gut. Bladder has unique bacterial community, called urobiome. Interstitial cystitis/bladder pain syndrome (IC/BPS) and overactive bladder (OAB) patients have altered urobiome composition, called dysbiosis. Dysbiosis in bladder could affect gut microbiome and vice versa. Inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS) could affect brain through brain-gut axis such as hypothalamic/pituitary/adrenal axis (HPA axis).
Significance of Serotonin and Norepinephrine in Functional Bladder Disease
Serotonin or 5-hydroxy tryptamine (5-HT)—a neurotransmitter in the central nervous system (CNS) that regulates various neurological activities—is produced mainly from the raphe nuclei of brainstem [17,18]. 5-HT has an important role in regulating emotion, especially its association with the development of depression. It is well known that the expression levels of 5-HT were remarkably low in the brain of depressed patients [19]. Norepinephrine (NE) is primarily synthesized in neurons that originate from locus coeruleus [20]. As a neurotransmitter in sympathetic nervous system, NE is recognized to play a crucial role in regulating blood pressure, heart rate, and muscles during fight-or-flight response [21]. Similar to 5-HT, a decreased level of NE is associated with depression [22].
Functional bladder disorders are caused by the comorbid of psychiatric symptoms such as depression and anxiety, which eventually affects patients in their quality of life and financial aspects. Of the 274 women diagnosed with OAB, many of them developed depression or anxiety, accounting for 59.8% and 62.4%, respectively [23]. In the Hospital Anxiety and Depression Scale - Depression subscale scoring of 2 groups—51 OAB patients and 30 controls—OAB patients had 90% higher score than that of controls [24]. Moreover, in these OAB patients, depression turned out to induce deterioration of incontinence symptom and in quality of life [24]. In addition, depression levels were high in women with urinary urgency or stress incontinence [25]. Moreover, the patients with severe depression scored higher in International Consultation on Incontinence Questionnaire-OAB and complained more of serious discomfort like enuresis and urge incontinence than those with mild depression, and this aspect was also observed in the patients with severe and mild anxiety [23]. Correlation analysis showed that depression and urinary symptoms were positively correlated [23], corroborating the p association between functional bladder and mood disorders. Given these findings, 5-HT and NE are considered as factors that regulate the correlation between functional bladder and psychiatric disorders.
The role of 5-HT and NE in controlling micturition was supported by in vivo experiments in which the effects of the administered drug on urination were observed. Mice with altered micturition pattern caused by moderate spinal contusion injury exhibited enhanced micturition after the administration of selective serotonin reuptake inhibitor (SSRI; fluoxetine) and 5-HT2A agonist (quipazine and 8-hydroxy-2-(di-n-propylamino)tetralin) [26]. Cats treated with a serotonin antagonist (methysergide), showed reduced micturition threshold [27]. Moreover, a study using SSRI, serotonin and norepinephrine reuptake inhibitors (SNRI), and their metabolites demonstrated the alleviation in the micturition pattern of CYP-induced OAB mice model [28].
Antidepressant injection was administered 24 hours post OAB induction and its effect was observed after 24 and 48 hours of administration [28]. Both observations exhibited an increase in first voiding latency and a reduction in number of urine spots and urine volume [28]. Moreover, the administration of corticosterone injection for the signs of depression and detrusor overactivity displayed a remarkable remission in SNRI (duloxetine)-treated mice [29]. Depressogenic-like behavior, cystometric parameters, altered concentration of proinflammatory cytokines, and other parameters of depression were almost recovered to normal levels [29–31]. Moreover, cats with reduced bladder capacity and abnormal pattern of electromyography (EMG) that resulted from the contraction of external urethral sphincter caused by acetic acid infusion were improved after the treatment with duloxetine [32]. Treatment of a patient suffering from OAB and OAB-related anxiety and depression with duloxetine ameliorated both bladder and mood disorders [33]. There are numerous 5-HT receptor subtypes, and the effect of agonists/antagonists binding varies depending on the subtypes and location of receptors, subjects, and signaling pathway triggered—which implies the need for further investigation [34,35] (Fig. 1).
THE RELATIONSHIP BETWEEN BLADDER AND GUT DISORDERS
Evidences for the Co-occurrence of Bladder and Gut Disorders
Patients with gut disorders were frequently accompanied by urinary disorders including urinary urgency, increased frequency of urination, straining to begin or finish voiding [36]. Approximately 20% of the 504 women with urinary incontinence suffered from fecal incontinence [37]. In addition, voiding frequency and urgency were often found in patients with IBS when compared with that in controls [38]. The prevalence rate of inflammatory bowel disease (IBD) was almost 100 times higher in IC/BPS patients than in healthy control group, and IBS was found to be the second most common concomitant disease in IC/BPS patients [39]. Furthermore, the extent of voiding symptoms depended on acute colitis severity [40].
Experimental animal models were similar to humans. Mice with 2, 4, 6-trinitrobenzene sulfonic acid (TNBS)-induced colitis were examined after 7 days of TNBS administration. It showed a reduced void volume and substantially high urinary frequency when compared with that in control groups [41]. TNBS-treated rats also showed altered micturition patterns, including decreased voiding intervals and increased micturition rate of 40% and above. Similarly, CYP-induced cystitis magnified the visceromotor responses to colonic distension, which suggests that dysfunction in bladder might cause colorectal disorders [42].
These outcomes imply that colonic dysfunction affects bladder functions (urodynamic changes) and thereby, causing different voiding patterns in patients. Therefore, given that the comorbidity of urinary and colonic dysfunctions is found to be quite common, and pathology in one organ may give rise to functional changes in the other, it is reasonable to say that there is a cross-talk between these 2 organs. The most well-known hypothesis of bladder-gut cross-talk is cross-afferent sensitization.
The contribution of afferent sensitization in bladder-gut cross-talk was illuminated by several experiments. In colitis-induced animal models, the activity of neurons was enhanced by urinary bladder distention when compared with that in control [43], and there was an increase in the amplitude of sodium ion current in bladder afferent after the induction of colitis [44,45]. Moreover, in a study that measured the firing rate of bladder afferent, especially C-fiber, there was a substantial difference in response to mechanical or chemical stimulation between the pre-intracolonic and postintracolonic administration of TNBS [46]. Similarly, rats with TNBS-induced colitis displayed a decreased bladder pain in response to capsaicin, followed by the denervation of capsaicin-sensitive afferent [47]. When the abdominal EMG for colorectal distension was measured in an acute cystitis-induced rat model, EMG activity was exhibited at a lower pressure than in control [48]. Moreover, TNBS-induced colitis model showed cystometric changes including decreased bladder contraction interval [48]. Therefore, we can suggest that the sensitivity of afferent changes depending on the presence of urinary or colonic irritation (Fig. 1).
Microbiome - the Key Player of Communication
The microorganisms living in the specific locations of host’s body regulate organ homeostasis, physiology, and interaction with other organs. The definition of human microbiome includes the genome, collection of microorganisms, and their ecology in human body (Table 1). The microbiota refers to the microbes found in specific niche [49]. Most of the microbiota are found in gastrointestinal tract, especially in large intestine. It is reasonable to say that the gut microbiome regulates the health of host as well as intestine, thereby maintaining a symbiotic relation with the host. Moreover, alterations in the population of gut microorganisms affect host gene expressions, metabolisms, physiological functions, and immune system—eventually exacerbating infectious diseases. Although the physiological correlation between gut microbiome and bladder disorder is not clearly understood, the overlap of several microorganisms in diverse symptoms was observed in both gut and bladder diseases (Fig. 2).
Table 1.
Representative microbiota in bladder and gut
| Bladder | Gut | ||
|---|---|---|---|
|
|
|
||
| Phylum | Genus | Phylum | Genus |
| Firmicute | Aerococcus [60] | Firmicute | Clostridium [61] |
|
| |||
| Anaerococcus [60] | Eubacterium [61] | ||
|
| |||
| Lactobacillus [60,62] | Lactobacillus [63] | ||
|
| |||
| Bacillus [62] | Bacillus [63] | ||
|
| |||
| Enterococcus [60] | Enterococcus [64] | ||
|
| |||
| Staphylococcus [60] | Staphylococcus [63] | ||
|
| |||
| Dialister [60] | Dialister [61] | ||
|
| |||
| Facklamia [60] | Faecalibacterium [61] | ||
|
| |||
| Bacteroidete | Bacteroides [62] | Bacteroidete | Bacteroides [61] |
|
| |||
| Porphyromonas [60] | Tannerella [61] | ||
|
| |||
| Proteiniphilum [60] | Parabacteroides [64] | ||
|
| |||
| Prevotella [60,62] | Prevotella [61] | ||
|
| |||
| Proteobacteria | Enterobacter [60] | Proteobacteria | Escherichia [64] |
|
| |||
| Methylovirgula [60] | Shigella [61] | ||
|
| |||
| Microvirgula [60] | Desulfovibrio [61] | ||
|
| |||
| Pelomonas [60] | Bilophila [61] | ||
|
| |||
| Helicobacter [61] | |||
|
| |||
| Actinobacteria | Bifidobacterium [65] | Actinobacteria | Bifidobacterium [61,64] |
|
| |||
| Atopobium [60] | Collinsella [61] | ||
|
| |||
| Corynebacterium [60,62] | |||
|
| |||
| Fusobacteria | Fusobacterium [60] | Fusobacteria | Fusobacterium [61] |
|
| |||
| Verrucomicrobia | Akkermansia [61] | ||
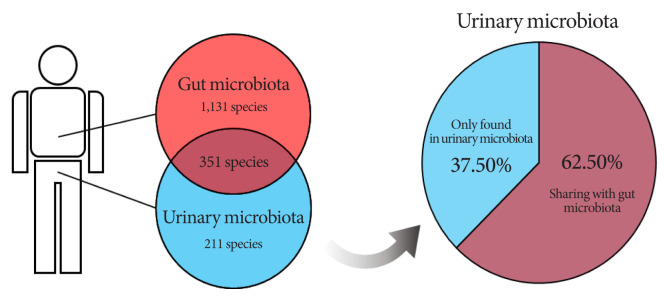
Fig. 2.
Bladder and gut share the common microbiota in species level. When identifying microbiota in catheterized urine and stool samples with 16S rRNA sequencing, 562 species and 1,482 species were found, respectively. Among the urine microbiota, about 62.5% (351 species) were commonly identified in stool sample [50].
The Problem Is Dysbiosis
“Urinary microbiome,” or “urobiome,” is the collective genome of microorganisms in urine collected from the bladder [50,51]. It contains fungi, virus, and mainly bacteria. Some of these microorganisms can be pathogenic (uropathogen) and were isolated from urine [52]. Dysbiosis is the alteration of normal composition and function of microbiome in specific environments [53]. The changes in bacterial composition of urine samples collected from patients with bladder disease were observed, suggesting that these alterations can be associated with the development of functional bladder diseases [54]. In dysbiosis, the total microbial diversity was decreased, and some bacterial taxa were identified in increased or decreased concentration in urine samples of the patients with bladder diseases. When comparing with the healthy group, the IC/BPS and OAB groups commonly have a reduced microbial concentration and diversity in urine [55,56]. In case of IC/BPS, the Streptococcus, Bifidobacterium, Candida, and Lactobacillus genera concentration were increased, while the Burkholderia, Staphylococcus, Propionbacterium, Listeria, Finegoldia, and Corynebacterium genera concentration were decreased [57]. In the OAB urine sample, 7 genera including Sneathia, Staphylococcus, Proteus, Helococcus, Gemella, Mycoplasma, and Aerococcus were in high concentration [56]. Symptom severity and incontinence in bladder diseases is remarkably correlated with urinary dysbiosis. The OAB patients with a decrease in microbial diversity of urinary bacterial species showed increased incontinence and symptom severity [58]. Furthermore, OAB patients with depression or anxiety showed different bacterial genera in urine when compared with that in OAB patients without mental disorders.
Understanding the link between bladder and brain-gut axis, and the discovery of urinary microbiota can bring profound clinical implications in future. Many researchers suggest that the interaction between bladder and brain-gut axis is bidirectional. Efferent nerves of the CNS modulate the gut including microbiota via autonomic nervous system and hypothalamic/pituitary/adrenal axis. The interaction of the brain-gut (microbiota) axis is observed in chronic intestinal disorders such as IBS or IBD. These disorders are also associated with cognitive disorders (anxiety, depression, or stress). In note, the affective disorders and chronic gut disorders are frequently associated with functional bladder disorders. The communication between bladder and brain-gut axis might affect permeability, inflammation, as well as infectious etiology and dysbiosis in bladder diseases [59].
CONCLUSIONS
A new hypothesis should be put forth to understand the functional bladder disorders that often show various overlapping symptoms. In the present review, we suggest that other etiologies may exist in addition to neuromuscular dysfunction and inflammation. We focused on the importance and possible role of the bladder and brain-gut axis. In regard to this insight, innovative therapeutic strategies targeting the microbiota and the integration of many overlapping symptoms could be developed for the proper management of functional bladder disorders. Instead of a therapy focused on decreasing urinary frequency or reducing bladder pain, evolving therapies are focused on enhancing the role of integrated care and beneficial microorganisms in the urinary ecosystem.
Footnotes
Grant/Fund Support
This research was supported by the Basic Science Research Program (NRF-2015R1A6A3A04058568, NRF-2020R1F1A 1076240, and NRF-2021R1C1C1009743, NRF-2019R1I1A2A01063045) and by the Korea Health Technology R&D Project (HU21C0161) through the Korea Health Industry Development Institute (KHIDI) and Korea Dementia Research Center (KDRC).
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTION STATEMENT
• Conceptualization: JJ, AK, SHY
• Funding acquisition: AK, SHY
• Project administration: AK, SHY
• Writing - original draft: JJ, AK, SHY
• Writing - review & editing: JJ, AK, SHY
REFERENCES
- 1.Brown JS, McGhan WF, Chokroverty S. Comorbidities associated with overactive bladder. Am J Manag Care. 2000;6(11 Suppl):S574–9. [PubMed] [Google Scholar]
- 2.Hanno PM, Erickson D, Moldwin R, Faraday MM, American Urological A Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol. 2015;193:1545–53. doi: 10.1016/j.juro.2015.01.086. [DOI] [PubMed] [Google Scholar]
- 3.Warren JW, Brown J, Tracy JK, Langenberg P, Wesselmann U, Greenberg P. Evidence-based criteria for pain of interstitial cystitis/painful bladder syndrome in women. Urology. 2008;71:444–8. doi: 10.1016/j.urology.2007.10.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pavcovich LA, Valentino RJ. Central regulation of micturition in the rat the corticotropin-releasing hormone from Barrington’s nucleus. Neurosci Lett. 1995;196:185–8. doi: 10.1016/0304-3940(95)11873-u. [DOI] [PubMed] [Google Scholar]
- 5.McFadden K, Griffin TA, Levy V, Wolfe JH, Valentino RJ. Overexpression of corticotropin-releasing factor in Barrington’s nucleus neurons by adeno-associated viral transduction: effects on bladder function and behavior. Eur J Neurosci. 2012;36:3356–64. doi: 10.1111/j.1460-9568.2012.08250.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koziol JA, Clark DC, Gittes RF, Tan EM. The natural history of interstitial cystitis: a survey of 374 patients. J Urol. 1993;149:465–9. doi: 10.1016/s0022-5347(17)36120-7. [DOI] [PubMed] [Google Scholar]
- 7.Chess-Williams R, McDermott C, Sellers DJ, West EG, Mills KA. Chronic psychological stress and lower urinary tract symptoms. Low Urin Tract Symptoms. 2021;13:414–24. doi: 10.1111/luts.12395. [DOI] [PubMed] [Google Scholar]
- 8.Lutgendorf SK, Kreder KJ, Rothrock NE, Ratliff TL, Zimmerman B. Stress and symptomatology in patients with interstitial cystitis: a laboratory stress model. J Urol. 2000;164:1265–9. [PubMed] [Google Scholar]
- 9.Wood SK, Baez MA, Bhatnagar S, Valentino RJ. Social stress-induced bladder dysfunction: potential role of corticotropin-releasing factor. Am J Physiol Regul Integr Comp Physiol. 2009;296:R1671–8. doi: 10.1152/ajpregu.91013.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith AL, Leung J, Kun S, Zhang R, Karagiannides I, Raz S, et al. The effects of acute and chronic psychological stress on bladder function in a rodent model. Urology. 2011;78:967.e1–7. doi: 10.1016/j.urology.2011.06.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Valentino RJ, Wood SK, Wein AJ, Zderic SA. The bladder-brain connection: putative role of corticotropin-releasing factor. Nat Rev Urol. 2011;8:19–28. doi: 10.1038/nrurol.2010.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robbins MT, Ness TJ. Footshock-induced urinary bladder hypersensitivity: role of spinal corticotropin-releasing factor receptors. J Pain. 2008;9:991–8. doi: 10.1016/j.jpain.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.LaBerge J, Malley SE, Zvarova K, Vizzard MA. Expression of corticotropin-releasing factor and CRF receptors in micturition pathways after cyclophosphamide-induced cystitis. Am J Physiol Regul Integr Comp Physiol. 2006;291:R692–703. doi: 10.1152/ajpregu.00086.2006. [DOI] [PubMed] [Google Scholar]
- 14.Klausner AP, Streng T, Na YG, Raju J, Batts TW, Tuttle JB, et al. The role of corticotropin releasing factor and its antagonist, astressin, on micturition in the rat. Auton Neurosci. 2005;123:26–35. doi: 10.1016/j.autneu.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 15.Wood SK, McFadden K, Griffin T, Wolfe JH, Zderic S, Valentino RJ. A corticotropin-releasing factor receptor antagonist improves urodynamic dysfunction produced by social stress or partial bladder outlet obstruction in male rats. Am J Physiol Regul Integr Comp Physiol. 2013;304:R940–50. doi: 10.1152/ajpregu.00257.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kiddoo DA, Valentino RJ, Zderic S, Ganesh A, Leiser SC, Hale L, et al. Impact of state of arousal and stress neuropeptides on urodynamic function in freely moving rats. Am J Physiol Regul Integr Comp Physiol. 2006;290:R1697–706. doi: 10.1152/ajpregu.00742.2005. [DOI] [PubMed] [Google Scholar]
- 17.Berger M, Gray JA, Roth BL. The expanded biology of serotonin. Annu Rev Med. 2009;60:355–66. doi: 10.1146/annurev.med.60.042307.110802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Groat WC. Influence of central serotonergic mechanisms on lower urinary tract function. Urology. 2002;59:30–6. doi: 10.1016/s0090-4295(01)01636-3. [DOI] [PubMed] [Google Scholar]
- 19.Blier P, El Mansari M. Serotonin and beyond: therapeutics for major depression. Philos Trans R Soc Lond B Biol Sci. 2013;368:20120536. doi: 10.1098/rstb.2012.0536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hamon M, Blier P. Monoamine neurocircuitry in depression and strategies for new treatments. Prog Neuropsychopharmacol Biol Psychiatry. 2013;45:54–63. doi: 10.1016/j.pnpbp.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 21.Tank AW, Lee Wong D. Peripheral and central effects of circulating catecholamines. Compr Physiol. 2015;5:1–15. doi: 10.1002/cphy.c140007. [DOI] [PubMed] [Google Scholar]
- 22.Nemeroff CB. The neurobiology of depression. Sci Am. 1998;278:42–9. doi: 10.1038/scientificamerican0698-42. [DOI] [PubMed] [Google Scholar]
- 23.Melotti IGR, Juliato CRT, Tanaka M, Riccetto CLZ. Severe depression and anxiety in women with overactive bladder. Neurourol Urodyn. 2018;37:223–8. doi: 10.1002/nau.23277. [DOI] [PubMed] [Google Scholar]
- 24.Lai HH, Shen B, Rawal A, Vetter J. The relationship between depression and overactive bladder/urinary incontinence symptoms in the clinical OAB population. BMC Urol. 2016;16:60. doi: 10.1186/s12894-016-0179-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee HY, Rhee Y, Choi KS. Urinary incontinence and the association with depression, stress, and self-esteem in older Korean Women. Sci Rep. 2021;11:9054. doi: 10.1038/s41598-021-88740-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ma L, Tang JY, Zhou JY, Zhu C, Zhang X, Zhou P, et al. Fluoxetine, a selective serotonin reuptake inhibitor used clinically, improves bladder function in a mouse model of moderate spinal cord injury. Neural Regen Res. 2021;16:2093–8. doi: 10.4103/1673-5374.308667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Espey MJ, Downie JW, Fine A. Effect of 5-HT receptor and adrenoceptor antagonists on micturition in conscious cats. Eur J Pharmacol. 1992;221:167–70. doi: 10.1016/0014-2999(92)90788-6. [DOI] [PubMed] [Google Scholar]
- 28.Redaelli M, Ricatti MJ, Simonetto M, Claus M, Ballabio M, Caretta A, et al. Serotonin and noradrenaline reuptake inhibitors improve micturition control in mice. PLoS One. 2015;10:e0121883. doi: 10.1371/journal.pone.0121883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wrobel A, Serefko A, Wozniak A, Kociszewski J, Szopa A, Wisniewski R, et al. Duloxetine reverses the symptoms of overactive bladder co-existing with depression via the central pathways. Pharmacol Biochem Behav. 2020;189:172842. doi: 10.1016/j.pbb.2019.172842. [DOI] [PubMed] [Google Scholar]
- 30.Levine J, Barak Y, Chengappa KN, Rapoport A, Rebey M, Barak V. Cerebrospinal cytokine levels in patients with acute depression. Neuropsychobiology. 1999;40:171–6. doi: 10.1159/000026615. [DOI] [PubMed] [Google Scholar]
- 31.Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, et al. A meta-analysis of cytokines in major depression. Biol Psychiatry. 2010;67:446–57. doi: 10.1016/j.biopsych.2009.09.033. [DOI] [PubMed] [Google Scholar]
- 32.Thor KB, Katofiasc MA. Effects of duloxetine, a combined serotonin and norepinephrine reuptake inhibitor, on central neural control of lower urinary tract function in the chloralose-anesthetized female cat. J Pharmacol Exp Ther. 1995;274:1014–24. [PubMed] [Google Scholar]
- 33.Wang SM, Lee HK, Kweon YS, Lee CT, Lee KU. Overactive bladder successfully treated with duloxetine in a female adolescent. Clin Psychopharmacol Neurosci. 2015;13:212–4. doi: 10.9758/cpn.2015.13.2.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cheng CL, de Groat WC. Role of 5-HT1A receptors in control of lower urinary tract function in anesthetized rats. Am J Physiol Renal Physiol. 2010;298:F771–8. doi: 10.1152/ajprenal.00266.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ramage AG. The role of central 5-hydroxytryptamine (5-HT, serotonin) receptors in the control of micturition. Br J Pharmacol. 2006;147(Suppl 2):S120–31. doi: 10.1038/sj.bjp.0706504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Klingele CJ, Lightner DJ, Fletcher JG, Gebhart JB, Bharucha AE. Dysfunctional urinary voiding in women with functional defecatory disorders. Neurogastroenterol Motil. 2010;22:1094–e284. doi: 10.1111/j.1365-2982.2010.01539.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Malykhina AP, Wyndaele JJ, Andersson KE, De Wachter S, Dmochowski RR. Do the urinary bladder and large bowel interact, in sickness or in health? ICI-RS 2011. Neurourol Urodyn. 2012;31:352–8. doi: 10.1002/nau.21228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Monga AK, Marrero JM, Stanton SL, Lemieux MC, Maxwell JD. Is there an irritable bladder in the irritable bowel syndrome? Br J Obstet Gynaecol. 1997;104:1409–12. doi: 10.1111/j.1471-0528.1997.tb11013.x. [DOI] [PubMed] [Google Scholar]
- 39.Alagiri M, Chottiner S, Ratner V, Slade D, Hanno PM. Interstitial cystitis: unexplained associations with other chronic disease and pain syndromes. Urology. 1997;49:52–7. doi: 10.1016/s0090-4295(99)80332-x. [DOI] [PubMed] [Google Scholar]
- 40.Franco I. Overactive bladder in children. Part 1: Pathophysiology. J Urol. 2007;178(3 Pt 1):761–8. doi: 10.1016/j.juro.2007.05.014. discussion 768. [DOI] [PubMed] [Google Scholar]
- 41.Lei Q, Pan XQ, Villamor AN, Asfaw TS, Chang S, Zderic SA, et al. Lack of transient receptor potential vanilloid 1 channel modulates the development of neurogenic bladder dysfunction induced by cross-sensitization in afferent pathways. J Neuroinflammation. 2013;10:3. doi: 10.1186/1742-2094-10-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bielefeldt K, Lamb K, Gebhart GF. Convergence of sensory pathways in the development of somatic and visceral hypersensitivity. Am J Physiol Gastrointest Liver Physiol. 2006;291:G658–65. doi: 10.1152/ajpgi.00585.2005. [DOI] [PubMed] [Google Scholar]
- 43.Qin C, Malykhina AP, Akbarali HI, Foreman RD. Cross-organ sensitization of lumbosacral spinal neurons receiving urinary bladder input in rats with inflamed colon. Gastroenterology. 2005;129:1967–78. doi: 10.1053/j.gastro.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 44.Malykhina AP, Qin C, Foreman RD, Akbarali HI. Colonic inflammation increases Na+ currents in bladder sensory neurons. Neuroreport. 2004;15:2601–5. doi: 10.1097/00001756-200412030-00008. [DOI] [PubMed] [Google Scholar]
- 45.Lei Q, Malykhina AP. Colonic inflammation up-regulates voltage-gated sodium channels in bladder sensory neurons via activation of peripheral transient potential vanilloid 1 receptors. Neurogastroenterol Motil. 2012;24:575–85.e257. doi: 10.1111/j.1365-2982.2012.01910.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ustinova EE, Fraser MO, Pezzone MA. Colonic irritation in the rat sensitizes urinary bladder afferents to mechanical and chemical stimuli: an afferent origin of pelvic organ cross-sensitization. Am J Physiol Renal Physiol. 2006;290:F1478–87. doi: 10.1152/ajprenal.00395.2005. [DOI] [PubMed] [Google Scholar]
- 47.Yoshikawa S, Kawamorita N, Oguchi T, Funahashi Y, Tyagi P, Chancellor MB, et al. Pelvic organ cross-sensitization to enhance bladder and urethral pain behaviors in rats with experimental colitis. Neuroscience. 2015;284:422–9. doi: 10.1016/j.neuroscience.2014.08.064. [DOI] [PubMed] [Google Scholar]
- 48.Pezzone MA, Liang R, Fraser MO. A model of neural cross-talk and irritation in the pelvis: implications for the overlap of chronic pelvic pain disorders. Gastroenterology. 2005;128:1953–64. doi: 10.1053/j.gastro.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 49.Berg G, Rybakova D, Fischer D, Cernava T, Verges MC, Charles T, et al. Microbiome definition re-visited: old concepts and new challenges. Microbiome. 2020;8:103. doi: 10.1186/s40168-020-00875-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Perez-Carrasco V, Soriano-Lerma A, Soriano M, Gutierrez-Fernandez J, Garcia-Salcedo JA. Urinary microbiome: Yin and Yang of the urinary tract. Front Cell Infect Microbiol. 2021;11:617002. doi: 10.3389/fcimb.2021.617002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pohl HG, Groah SL, Perez-Losada M, Ljungberg I, Sprague BM, Chandal N, et al. The urine microbiome of healthy men and women differs by urine collection method. Int Neurourol J. 2020;24:41–51. doi: 10.5213/inj.1938244.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Barnett BJ, Stephens DS. Urinary tract infection: an overview. Am J Med Sci. 1997;314:245–9. doi: 10.1097/00000441-199710000-00007. [DOI] [PubMed] [Google Scholar]
- 53.Levy M, Kolodziejczyk AA, Thaiss CA, Elinav E. Dysbiosis and the immune system. Nat Rev Immunol. 2017;17:219–32. doi: 10.1038/nri.2017.7. [DOI] [PubMed] [Google Scholar]
- 54.Mueller ER, Wolfe AJ, Brubaker L. Female urinary microbiota. Curr Opin Urol. 2017;27:282–6. doi: 10.1097/MOU.0000000000000396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Siddiqui H, Lagesen K, Nederbragt AJ, Jeansson SL, Jakobsen KS. Alterations of microbiota in urine from women with interstitial cystitis. BMC Microbiol. 2012;12:205. doi: 10.1186/1471-2180-12-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wu P, Chen Y, Zhao J, Zhang G, Chen J, Wang J, et al. Urinary microbiome and psychological factors in women with overactive bladder. Front Cell Infect Microbiol. 2017;7:488. doi: 10.3389/fcimb.2017.00488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nickel JC, Stephens-Shields AJ, Landis JR, Mullins C, van Bokhoven A, Lucia MS, et al. A culture-independent analysis of the microbiota of female interstitial cystitis/bladder pain syndrome participants in the MAPP research network. J Clin Med. 2019;8:415. doi: 10.3390/jcm8030415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Karstens L, Asquith M, Davin S, Stauffer P, Fair D, Gregory WT, et al. Does the urinary microbiome play a role in urgency urinary incontinence and its severity? Front Cell Infect Microbiol. 2016;6:78. doi: 10.3389/fcimb.2016.00078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ringel Y, Ringel-Kulka T. The intestinal microbiota and irritable bowel syndrome. J Clin Gastroenterol. 2015;49(Suppl 1):S56–9. doi: 10.1097/MCG.0000000000000418. [DOI] [PubMed] [Google Scholar]
- 60.Lewis DA, Brown R, Williams J, White P, Jacobson SK, Marchesi JR, et al. The human urinary microbiome; bacterial DNA in voided urine of asymptomatic adults. Front Cell Infect Microbiol. 2013;3:41. doi: 10.3389/fcimb.2013.00041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Arumugam M, Raes J, Pelletier E, Le Paslier D, Yamada T, Mende DR, et al. Enterotypes of the human gut microbiome. Nature. 2011;473:174–80. doi: 10.1038/nature09944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kogan MI, Naboka YL, Ibishev KS, Gudima IA, Naber KG. Human urine is not sterile - shift of paradigm. Urol Int. 2015;94:445–52. doi: 10.1159/000369631. [DOI] [PubMed] [Google Scholar]
- 63.Tap J, Mondot S, Levenez F, Pelletier E, Caron C, Furet JP, et al. Towards the human intestinal microbiota phylogenetic core. Environ Microbiol. 2009;11:2574–84. doi: 10.1111/j.1462-2920.2009.01982.x. [DOI] [PubMed] [Google Scholar]
- 64.Kurokawa K, Itoh T, Kuwahara T, Oshima K, Toh H, Toyoda A, et al. Comparative metagenomics revealed commonly enriched gene sets in human gut microbiomes. DNA Res. 2007;14:169–81. doi: 10.1093/dnares/dsm018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pearce MM, Hilt EE, Rosenfeld AB, Zilliox MJ, Thomas-White K, Fok C, et al. The female urinary microbiome: a comparison of women with and without urgency urinary incontinence. mBio. 2014;5:e01283–14. doi: 10.1128/mBio.01283-14. [DOI] [PMC free article] [PubMed] [Google Scholar]